Abstract
Background:
Acute type A aortic dissections (ATAAD) pose a challenge to surgeons due to high mortality, and decision making regarding the appropriate procedure is controversial. This study compared the outcomes of hemiarch and total arch replacement for ATAAD.
Methods:
The PubMed, Web of Science, Embase and Cochrane databases were searched for comparative studies on hemiarch versus total arch replacement that were published before May 1, 2022.
Results:
We included 23 observational studies with a total of 4,576 patients. Combined data analysis showed that early mortality (RR = 0.82; 95% CI: 0.70–0.97; P = 0.02), incidence of postoperative permanent neurological dysfunction (RR = 0.72; 95%CI:0.54∼0.94; P = 0.02), and incidence of renal failure and dialysis (RR = 0.82; 95%CI:0.71∼0.96; P = 0.01) were all lower for hemiarch than for total arch replacement. However, hemiarch replacement had a higher rate of late mortality (RR = 1.37; 95%CI:1.10∼1.71; P = 0.005). There were no statistically significant differences between the two groups in terms of re-operation for bleeding, aortic re-operation, or postoperative pneumonia.
Conclusion:
In this study, hemiarch replacement had better early outcomes but a higher late mortality rate than total arch replacement. Decisions regarding the extent of arch repair should be made according to location and extent of ATAAD and the experience of surgeons to ensure the most favorable prognosis.
Systematic review registration::
[INPLASY.COM], identifier [INPLASY202250088].
Introduction
Since acute aortic dissection was first described, it has been one of the most concerning emergent cardiac conditions owing to its high morbidity and mortality (1). Indeed, following symptom onset there is a 1–2% per hour increase in mortality rate during an ascending aortic dissection (2), which poses a great challenge for cardiac surgeons. Many patients with aortic dissection often experience a tear from the aortic intima to the arch, and the traditional surgical treatment for this has been to perform hemiarch replacement to reduce the inherent risks of surgery (3). However, this procedure may leave behind a residual false lumen in the distal aorta. Some researchers believe that total arch replacement combined with stented elephant trunk implantation is necessary for certain patients to address continued tearing of the intima to avoid subsequent reoperation (4). An intense discussion about which of the two treatments is favorable persists, as completion of the total arch replacement procedure requires personnel with rich surgical experience and expertise, and its prognosis remains relatively vague. Further, randomized controlled experiments are difficult, especially regarding ethics. Although there is an increasing trend in performing total arch replacement in patients with acute type A aortic dissections (ATAAD), controversy persists between choosing hemiarch and total arch replacement, as high-quality studies in this area are sparse. Some researchers have performed relevant meta-analyses previously (5), but newer studies have been published in the past few years, and thus these analyses require updating. In this study, we aimed to compare the early and long-term outcomes of hemiarch and total arch replacement for the treatment of ATAAD.
Patients and methods
Ethical statement
This study was a meta-analysis of the results of published retrospective cohort studies; therefore ethical approval and informed consent of patients were not required.
Search strategy and selection criteria
This study protocol followed the (Preferred Reporting Items for Systematic reviews and Meta-analyses) PRISMA-P guidelines. Two authors (LKM and TCC) searched the PubMed, Web of Science, Embase, and Cochrane Central Register of Controlled Trials databases for studies published in English before May 1, 2022. They also checked the references of related literature. Our search terms were: (“DeBakey type I aortic dissection” OR “type A aortic dissection”) AND (“total aortic arch replacement” OR “aggressive arch replacement” OR “extended repair”) AND (“hemiarch replacement” OR “conservative arch replacement” OR “limited repair”). We excluded medical record reports, abstracts, expert opinions, editorial comments, review articles, and articles that could not be found in full to ensure consistency in our studies.
Two authors (LM and TC) independently determined whether the identified articles fulfilled the inclusion criteria. All included studies were required to include postoperative short-, medium-, and long-term outcomes. All studies comparing the prognosis of hemiarch and total arch replacement were included. Hemiarch replacement refers to preserving the large curved side of the aortic arch without involving the arch vessels, removing the wall of the small curved side of the blood vessels, and cutting artificial blood vessels into a slope to create an anastomosis. Total arch replacement is the replacement of the superior aortic arch as a whole or using individual branched grafts, with or without an elephant trunk stent.
Participants included patients over 18 years of age who presented with ATAAD. If an institution published multiple observational studies, the largest and most informative study with complete follow-up data was selected. Where necessary, the researchers contacted the authors of these studies to obtain any necessary information.
Data extraction and appraisal
Data for all articles were independently collected and reviewed by two investigators (LM and TC). According to the Cochrane handbook for Systematic Reviews of Intervention, the qualities of papers were assessed independently by authors for suitability, consistency, and adequacy of study design and patient selection. For quality and bias assessment, we used the Newcastle-Ottawa Score (6) (9 = lowest risk of bias; 0 = highest risk of bias) to assess bias on three levels: selection, comparability and outcomes. The scoring was performed by two independent authors, and a score of ≥ 7 suggested no substantial bias. Finally, before the extracted data were analyzed; any discrepancies were resolved by consensus.
Statistical analysis
For this study, we assumed clinical differences between selected studies and evaluated studies using a fixed-effects model of inverse variance. Inter-study heterogeneity was assessed using chi-square tests and the I2 statistic, with fixed-effects models used for data with less heterogeneity (P > 0.1 or I2 < 50%), and random effects models used for data with high heterogeneity.
Dichotomous data were presented in the form of risk ratios (RRs) as a summary of statistics and effect measure with 95% confidence intervals (CI). RRs were derived from the relative frequencies of the studies where available. Publication bias was assessed using funnel plots comparing log risk estimates with their standard errors. The data were synthesized using Review Manager version 5.4 (Cochrane, London, United Kingdom). The GRADEpro GDT (McMaster University and Evidence Prime, 2022. Available from gradepro.org) was used to classify the certainty of evidence (Supplementary Figure 1).
Results
Quantity of studies and demographics
This study identified 23 retrospective observational studies that included 4,576 patients. Among them, 3,103 were hemiarch and 1,473 were total arch replacement patients. The literature selection process following the PRISMA checklist (7) is shown in Figure 1, and an overview of the selected studies is shown in Table 1. Basic patient characteristics such as age, sex, hypertension, diabetes mellitus, Marfan syndrome, renal insufficiency, and others are shown in Tables 2, 3.
FIGURE 1
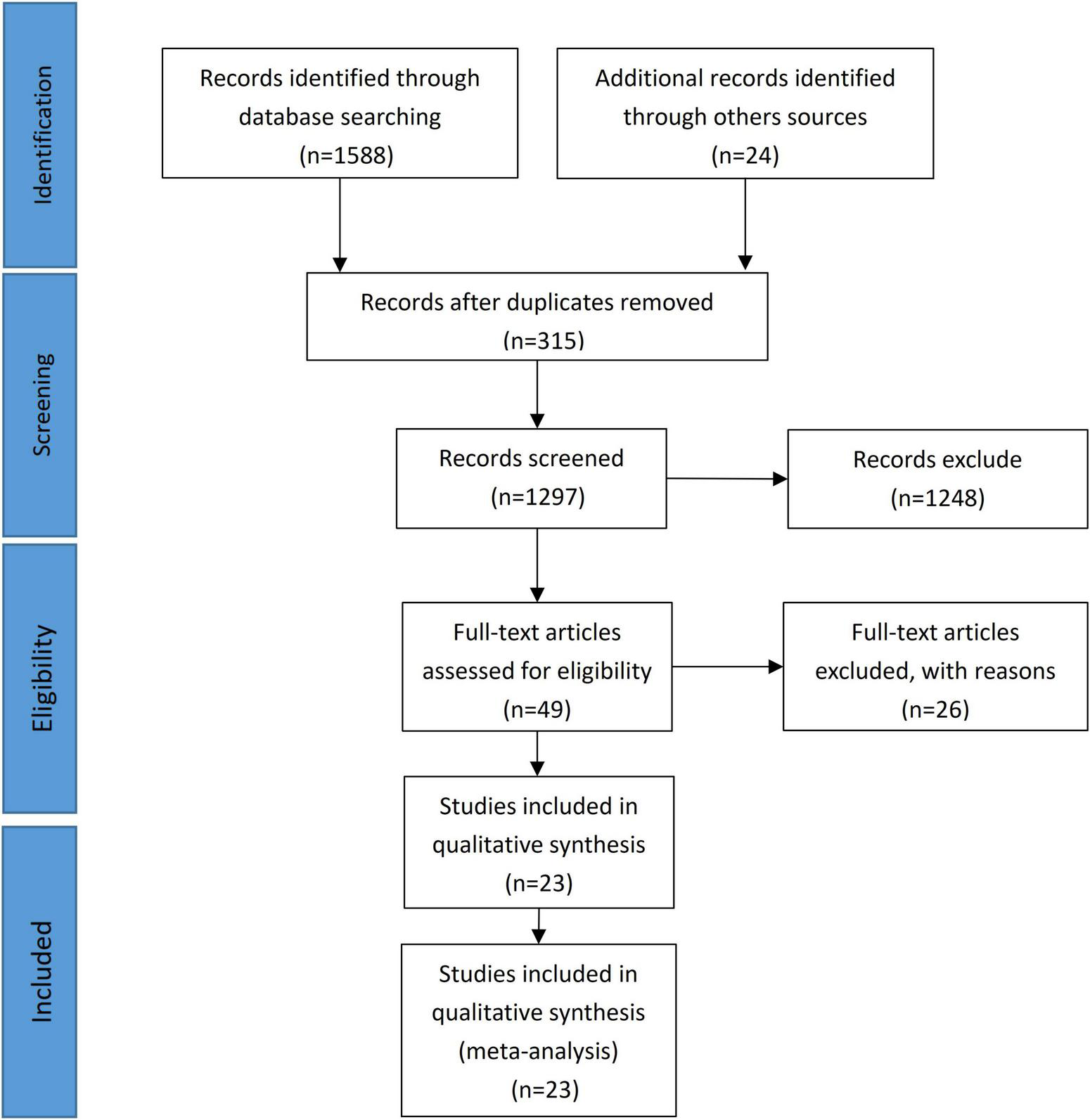
PRISMA flow diagram.
TABLE 1
| References | Study period | Country | Number of hemiarch | Number of total arch | Total sample size | Mean follow up time | Newcastle ottawa score |
| Aizawa et al. (17) | 2004–2014 | Japan | 225 | 42 | 267 | 57 ± 32 months | 9 |
| Chen et al. (18) | 2009–2013 | China | 21 | 63 | 84 | 7.6 ± 3.4 years | 7 |
| Colli et al. (19) | 1998–2015 | Italy | 114 | 21 | 135 | 5 ± 4 yesrs | 7 |
| Dai et al. (20) | 2008–2010 | China | 41 | 52 | 93 | 64 ± 5.3 months | 7 |
| Di Eusanio et al. (21) | 1997–2012 | Italy | 187 | 53 | 240 | 4.8 ± 3.9 years | 8 |
| Kim et al. (12) | 1999–2009 | Korea | 144 | 44 | 188 | 47.5 months | 9 |
| Lee et al. (22) | 2008–2018 | Korea | 82 | 16 | 98 | 48 months | 8 |
| Lio et al. (16) | 2006–2013 | Italy | 59 | 33 | 92 | 30.5 months | 8 |
| Merkle et al. (23) | 2006–2015 | Germany | 72 | 42 | 114 | up to 9 years | 7 |
| Ok et al. (24) | 1999–2019 | Korea | 248 | 117 | 265 | NS | 9 |
| Omura et al. (10) | 1999–2014 | Japan | 109 | 88 | 197 | 60 ± 48 months | 9 |
| Patel et al. (25) | 2004–2019 | USA | 397 | 107 | 504 | NS | 7 |
| Qin et al. (11) | 2001–2015 | China | 41 | 62 | 103 | 69.6 ± 19.2 months | 8 |
| Rice et al. (26) | 1999–2014 | USA | 440 | 49 | 489 | 49 months | 9 |
| Rylski et al. (27) | 2001–2003 | Germany | 37 | 14 | 51 | 4.9 years 45% >5 years | 9 |
| Shi et al. (28) | 2006–2011 | China | 71 | 84 | 155 | 42.7 ± 17.8 months | 8 |
| Shiono et al. (14) | 1995–2005 | Japan | 105 | 29 | 134 | up to 10 years | 8 |
| Sun et al. (4) | 2003–2008 | China | 66 | 148 | 214 | 42–49 months | 8 |
| Uchida et al. (29) | 1997–2008 | Japan | 55 | 65 | 120 | 67 months(3–124 months) | 7 |
| Vallabhajosyula et al. (30) | 2006–2013 | USA | 30 | 31 | 61 | 60 ± 41 months | 7 |
| Vendramin et al. (31) | 2006–2020 | Italy | 163 | 75 | 238 | 4.5 ± 3.5y ears | 9 |
| Yang et al. (32) | 1996–2017 | USA | 322 | 150 | 472 | 5.3 years | 9 |
| Zhang et al. (15) | 2002–2010 | China | 74 | 88 | 162 | 55.7 ± 33.1 months | 7 |
An overview of publication from selected studies.
NS, not specified.
TABLE 2
| References | Mean age |
Male sex |
Hypertension |
Diabetes mellitus |
||||
| HA | TA | HA | TA | HA | TA | HA | TA | |
| Aizawa et al. (17) | 66.0 ± 12.0 | 59.0 ± 12.0 | 103 (45.8%) | 31 (73.8%) | NS | NS | NS | NS |
| Chen et al. (18) | 51.0 ± 11.7 | 51.5 ± 10.5 | 9 (42.9%) | 29 (46%) | NS | NS | 1 (4.8%) | 4 (6.3%) |
| Colli et al. (19) | 63.0 ± 12.0 | 63.0 ± 13.0 | 49 (43%) | 9 (42.9%) | 61 (53.5%) | 15 (71.4%) | 6 (5.3%) | 0 (0%) |
| Dai et al. (20) | 49.1 ± 10.4 | 49.8 ± 9.6 | 25 (61%) | 29 (55.8%) | 40 (97.6%) | 49 (94.2%) | 1 (2.4%) | 1 (1.9%) |
| Di Eusanio et al. (21) | 64.4 ± 11.2 | 59.2 ± 12.3 | 125 (66.8%) | 41 (77.4%) | 138 (73.8%) | 40 (75.5%) | 8 (4.3%) | 1 (1.9%) |
| Kim et al. (12) | 57.6 ± 11.5 | 55.0 ± 12.1 | 69 (47.9%) | 26 (59.1%) | 92 (63.9%) | 24 (54.5%) | 6 (4.2%) | 2 (4.5%) |
| Lee et al. (22) | 60.1 ± 14.2 | 60.7 ± 14.3 | 38 (46.3%) | 8 (50.0%) | 45 (54.6%) | 9 (56.3%) | 6 (7.3%) | 0 (0%) |
| Lio et al. (16) | 66.0 ± 10.0 | 61.0 ± 12.0 | 43 (72.9%) | 28 (84.8%) | 51 (86.4%) | 30 (90.9%) | 2 (3.4%) | 1 (3.0%) |
| Merkle et al. (23) | 67.0 | 60.0 | 49 (68.1%) | 27 (64.3%) | 61 (84.7%) | 31 (73.8%) | 6 (8.3%) | 1 (2.4%) |
| Ok et al. (24) | 59.2 ± 11.9 | 51.9 ± 13.6 | 116 (46.8%) | 72 (61.5%) | 150 (60.5%) | 62 (53.0%) | 15 (6.0%) | 6 (5.1%) |
| Omura et al. (10) | 70.0 ± 11.0 | 61.0 ± 13.0 | 50 (45.9%) | 62 (70.5%) | NS | NS | NS | NS |
| Patel et al. (25) | 55.9 ± 14.1 | 55.3 ± 13.5 | 263 (66.2%) | 71 (66.4%) | 373 (94.0%) | 97 (90.7%) | 59 (14.9%) | 8 (7.5%) |
| Qin et al. (11) | 70.7 ± 3.8 | 69.5 ± 3.2 | 29 (70.7%) | 42 (67.7%) | 41 (100%) | 62 (100%) | 11 (26.8%) | 15 (24.2%) |
| Rice et al. (26) | 57.9 ± 14.8 | 62.4 ± 13.4 | 313 (71.1%) | 38 (77.6%) | 370 (84.1%) | 40 (81.6%) | NS | NS |
| Rylski et al. (27) | 66.0 | 55.0 | 21 (56.8%) | 8 (57.1%) | 31 (83.8%) | 13 (92.9%) | NS | NS |
| Shi et al. (28) | 55.9 ± 10.1 | 53.9 ± 12.2 | 53 (74.6%) | 57 (67.9%) | 55 (77.5%) | 67 (79.8%) | 12 (16.9%) | 19 (22.6%) |
| Shiono et al. (14) | 66.9 ± 13.0 | 59.5 ± 14.9 | 46 (43.8%) | 15 (51.7%) | NS | NS | NS | NS |
| Sun et al. (4) | 46.0 ± 13.0 | 45.0 ± 11.0 | 36 (54.5%) | 126 (85.1%) | 36 (54.5%) | 107 (72.3%) | 2 (3.0%) | 6 (4.1%) |
| Uchida et al. (29) | 72.3 | 64.4 | 25 (45.5%) | 28 (43.1%) | NS | NS | NS | NS |
| Vallabhajosyula et al. (30) | 58.0 ± 11.0 | 59 ± 12 | 20 (66.7%) | 20 (64.5%) | 26 (86.7%) | 28 (90.3%) | 2 (6.7%) | 2 (6.5%) |
| Vendramin et al. (31) | 69.0 | 58.0 | 106 (65.0%) | 57 (76.0%) | 124 (76.1%) | 58 (77.3%) | 11 (6.7%) | 2 (2.7%) |
| Yang et al. (32) | 61.0 | 57.0 | 226 (70.2%) | 104 (69.3%) | 230 (71.4%) | 107 (71.3%) | 21 (6.5%) | 9 (6.0%) |
| Zhang et al. (15) | 49.1 ± 12.6 | 45.5 ± 13.5 | 55 (74.3%) | 74 (84.1%) | 47 (63.5%) | 64 (72.7%) | 4 (5.4%) | 4 (4.5%) |
Patient’s demographics (part A).
NS, not specified; HA, hemiarch; TA, total arch.
TABLE 3
| References | Mafan syndrome |
Renal dysfunction |
Cardiogenic shock/Tamponade |
Cerebrovascular accident/Stroke |
||||
| HA | TA | HA | TA | HA | TA | HA | TA | |
| Aizawa et al. (17) | 3 (1.3%) | 0 (0%) | 2 (0.9%) | 3 (7.1%) | 38 (16.9%) | 4 (9.5%) | 37 (16.4%) | 5 (11.9%) |
| Chen et al. (18) | 2 (9.5%) | 7 (11.1%) | 0 (0%) | 1 (1.6%) | NS | NS | 1 (4.8%) | 2 (3.2%) |
| Colli et al. (19) | 3 (2.6%) | 0 (0%) | 5 (4.4%) | 0 (0%) | 15 (13.2%) | 2 (9.5%) | 31 (27.2%) | 3 (14.3%) |
| Dai et al. (20) | 2 (4.9%) | 3 (5.8%) | 1 (2.4%) | 2 (3.8%) | 2 (4.9%) | 1 (1.9%) | 0 (0%) | 1 (1.9%) |
| Di Eusanio et al. (21) | 5 (2.7%) | 3 (5.7%) | 8 (4.3%) | 3 (5.7%) | 25 (13.4%) | 2 (3.8%) | 11 (5.9%) | 4 (7.5%) |
| Kim et al. (12) | 7 (4.9%) | 1 (2.3%) | NS | NS | 13 (9.0%) | 4 (9.1%) | 4 (2.8%) | 3 (6.8%) |
| Lee et al. (22) | 4 (4.9%) | 1 (6.3%) | NS | NS | NS | NS | 4 (4.9%) | 0 (0%) |
| Lio et al. (16) | NS | NS | 1 (1.7%) | 0 (0%) | 5 (8.5%) | 4 (12.1%) | NS | NS |
| Merkle et al. (23) | NS | NS | NS | NS | NS | NS | 17 (23.6%) | 13 (31.0%) |
| Ok et al. (24) | 17 (6.9%) | 12 (10.3%) | NS | NS | 26 (10.5%) | 12 (10.3%) | NS | NS |
| Omura et al. (10) | NS | NS | NS | NS | 25 (22.9%) | 10 (11.4%) | NS | NS |
| Patel et al. (25) | NS | NS | 14 (3.5%) | 3 (2.8%) | 30 (7.6%) | 2 (1.9%) | 41 (10.3%) | 11 (10.3%) |
| Qin et al. (11) | NS | NS | NS | NS | 7 (17.1%) | 13 (21.0%) | 2 (4.9%) | 2 (3.2%) |
| Rice et al. (26) | 9 (2.0%) | 1 (2.0%) | 105 (23.9%) | 10 (20.4%) | 69 (15.7%) | 9 (18.4%) | 32 (7.3%) | 6 (12.2%) |
| Rylski et al. (27) | 2 (5.4%) | 0 (0%) | NS | NS | 3 (8.1%) | 1 (7.1%) | NS | NS |
| Shi et al. (28) | 10 (14.1%) | 22 (26.2%) | 5 (7.0%) | 4 (4.8%) | 13 (18.3%) | 12 (14.3%) | 2 (2.8%) | 2 (2.4%) |
| Qin et al. (14) | 5 (4.8%) | 3 (10.3%) | NS | NS | 49 (46.7%) | 8 (27.6%) | 11 (10.5%) | 0 (0%) |
| Sun et al. (4) | 5 (7.6%) | 19 (12.8%) | 1 (1.5%) | 4 (2.7%) | 8 (12.1%) | 3 (2.0%) | 1 (1.5%) | 1 (0.7%) |
| Qin et al. (29) | NS | NS | 5 (9.1%) | 2 (3.1%) | 21 (38.2%) | 21 (32.3%) | 12 (21.8%) | 6 (9.2%) |
| Vallabhajosyula et al. (30) | 10 (33.3%) | 7 (22.6%) | 3 (10.0%) | 2 (6.5%) | 7 (23.3%) | 3 (9.7%) | 1 (3.3%) | 5 (16.1%) |
| Vendramin et al. (31) | NS | NS | 16 (9.8%) | 12 (16.0%) | 61 (37.4%) | 20 (26.7%) | 28 (17.2%) | 19 (25.3%) |
| Yang et al. (32) | 16 (5.0%) | 5 (3.3%) | 40 (12.4%) | 26 (17.3%) | 67 (20.8%) | 16 (10.7%) | 13 (4.0%) | 7 (4.7%) |
| Zhang et al. (15) | 13 (17.6%) | 21 (23.9%) | 6 (8.1%) | 3 (3.4%) | 25 (33.8%) | 17 (19.3%) | 2 (2.7%) | 1 (1.1%) |
Patient’ s demographics (part B).
NS, not specified; HA, hemiarch; TA, total arch.
Surgical technique
In patients undergoing hemiarch replacement, most of the curvature of the lesser arch curvature was excised obliquely at the aortic arch. The greater curvature of the aortic arch was left and distal anastomosis was performed. In total arch replacement, the entire arch was excised, and arteries in the upper part of the aortic arch as a whole or branches were anastomosed with the graft. Some cardiac centers implanted stents into the lumen of the distal aorta. When the patient’s aortic intimal tear was located along the ascending aorta or the lesser curvature of the arch, hemiarch replacement was chosen. If the patient’s aortic intimal tear was located at the greater curvature of the arch or involved the upper arch artery, total arch replacement was performed. For total arch replacement with a frozen elephant trunk, the stent graft was inserted into the true lumen of the thoracic aorta until it reached the predetermined position. Then the distal aorta incorporating the stent graft was securely anchored to the distal trunk of the branched prosthetic graft. The neuroprotective strategies of each study are shown in Supplementary Figure 2.
Post-operative outcomes
Early mortality
Early mortality was defined as in-hospital and 30-day mortality. A pooled analysis of 23 studies showed lower early mortality in the hemiarch replacement group (HA) compared with that in the total arch replacement group (TA), RR = 0.82; 95% CI: 0.70–0.97; P = 0.02; I2 = 15% (Figure 2). According to statistics, the early mortality rate of hemiarch replacement was 12.71% (3.64–43.06%), and the total arch replacement was 17.39% (3.85–57.14%) (Supplementary Figure 3).
FIGURE 2
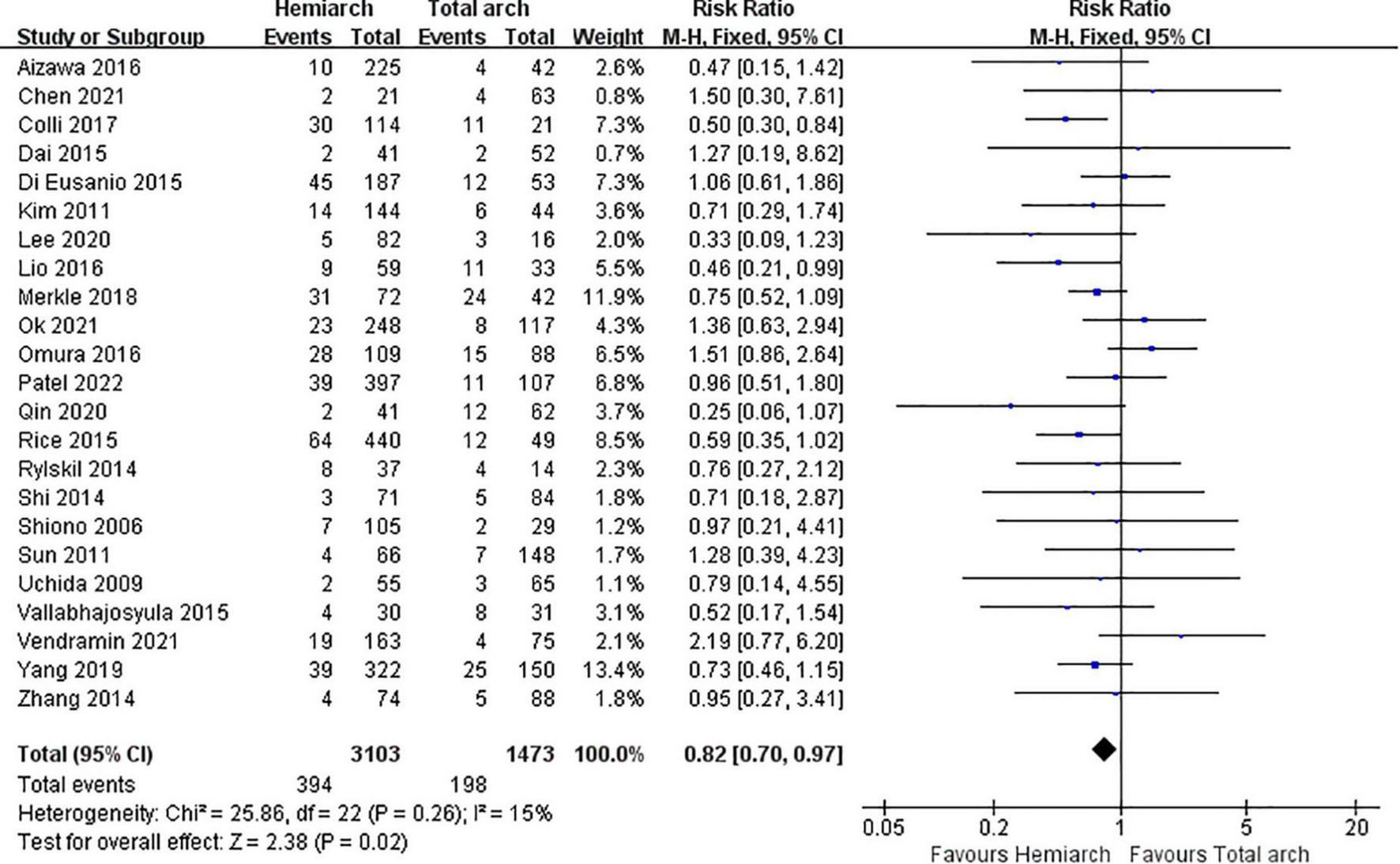
Forest plot of early mortality.
Neurological dysfunction
Patients with temporary neurological dysfunction may show slurred speech, poor response to instructions, visual field defects, or localized seizures. Data from 10 studies in a pooled analysis showed no statistical differences between the two groups, RR = 0.89; 95%CI:0.69∼1.14; P = 0.34; I2 = 0% (Supplementary Figure 4A). Permanent neurological dysfunction may take place if coma persists or stroke occurs after surgery. Data from 16 studies were pooled to show that hemiarch replacement had a lower risk of permanent neurological dysfunction than total arch replacement, RR = 0.72; 95%CI:0.54∼0.94; P = 0.02; I2 = 0% (Supplementary Figure 4B).
Renal failure and dialysis
According to the analysis of data from 22 studies, the incidence of acute renal failure and dialysis after hemiarch replacement was significantly lower, RR = 0.82; 95%CI:0.71∼0.96; P = 0.01; I2 = 0% (Supplementary Figure 4C).
Re-operation
There were 18 and 16 studies reporting re-operation for bleeding and aortic re-operation (proximal and distal). The analysis of the data showed no significant differences between hemiarch and total arch replacement regarding re-operation, RR = 0.89; 95% CI:0.72∼1.11; P = 0.30; I2 = 0% (Supplementary Figure 4D), and RR = 1.11; 95% CI:0.87∼1.41; P = 0.41; I2 = 17% (Supplementary Figure 4E), respectively.
Pneumonia
There were 10 studies that recorded the postoperative incidence of pneumonia in patients, and the aggregate data analysis found no significant statistical differences between the two groups, RR = 0.67; 95% CI:0.44∼1.04; P = 0.08; I2 = 60% (Supplementary Figure 4F).
Late mortality
Late mortality was defined as patient death that occurred during follow-up. Summarizing the data of 14 studies, we found that the late mortality of hemiarch replacement was higher than total arch replacement, RR = 1.37; 95% CI:1.10∼1.71; P = 0.005; I2 = 43% (Figure 3).
FIGURE 3
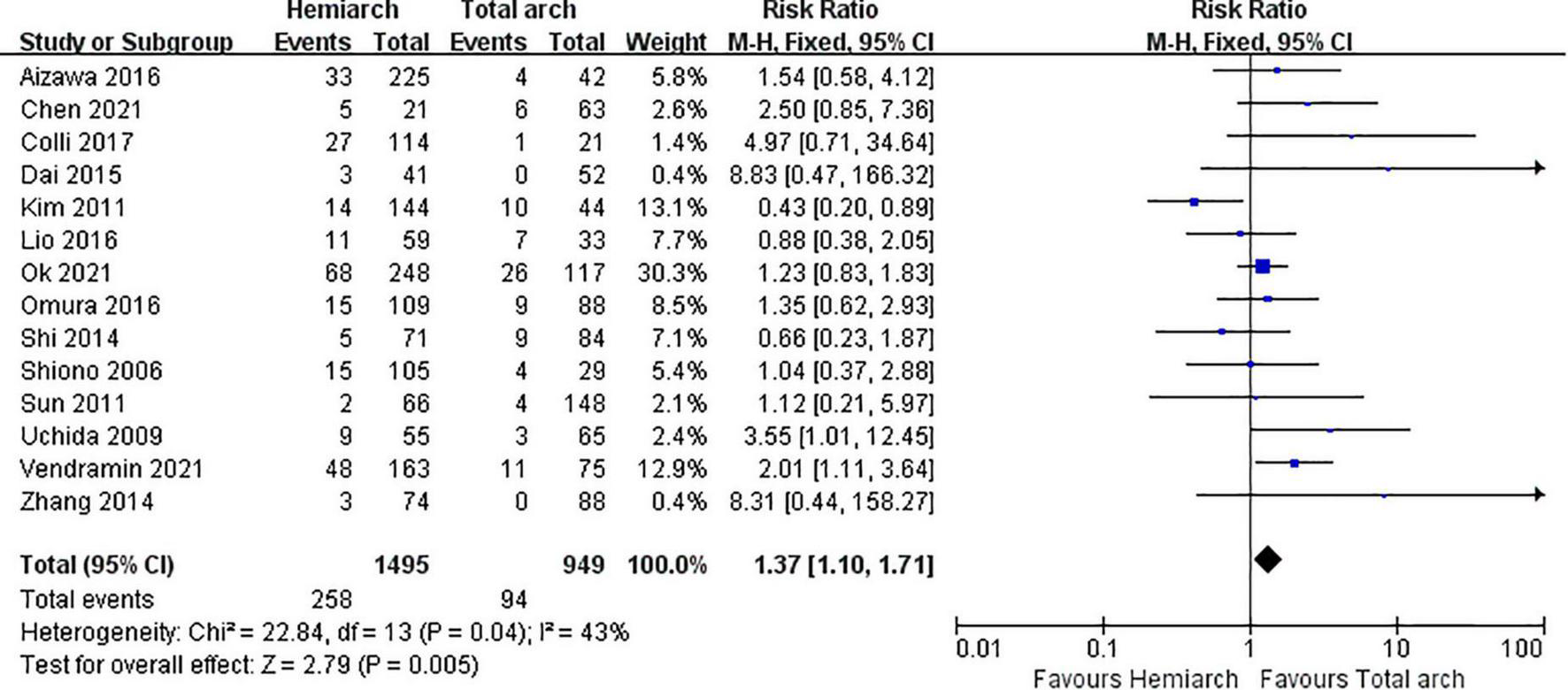
Forest plot of late mortality.
Publication bias
Funnel plots revealed no evidence of publication bias regarding early mortality (Supplementary Figure 5A), temporary neurological dysfunction, permanent neurological dysfunction, renal failure and dialysis, re-operation for bleeding, aortic re-operation, or late mortality. However, the funnel plots did suggest some publication bias regarding pneumonia (Supplementary Figure 5B). Thus, we used the trim-and-fill method to adjust the analysis, which did not significantly alter the findings.
Comment
In this study, results showed the incidences of early mortality, postoperative permanent neurological dysfunction, renal failure, and dialysis of hemiarch replacement to be lower than those in total arch replacement. However, the late mortality of hemiarch replacement was higher than that in total arch replacement, which differed from a previous study (5). We included up-to-date data in the English literature (Last Date access time as of May 2022). This may have been the reason for this difference.
Until recently, ATAAD was considered a severe and fatal disease. Thus, the selection of surgical strategy should be based not only on the general condition of patients and the extent of the dissection, but also the experience of cardiovascular surgeons. Cardiovascular surgeons have different views on the scope of arch surgeries for this condition. Ohtsubo (8), Westaby (9) and their colleagues have shown better early and late outcomes for hemiarch replacement. However, the results of Sun et al. (4) and Omura et al. (10) showed the ability for total arch replacement to completely repair the aorta and reduce the possibility of subsequent re-operation. In contrast, a recent study by Qin and his colleagues showed total arch replacement to have a higher mortality and surgical risk than hemiarch, and although the total arch replacement had reduced adverse arterial events later on, there was no difference in 5-year survival between the two groups (82.5 ± 60% vs. 75.2 ± 5.6%, P = 0.151) (11). These findings were based on data from their local hospitals, which inevitably carries the limitation of small sample size; further, differences in technique among surgical operators also has an impact on patient outcomes. In this analysis, data was pooled from 23 studies with a total of 4,576 patients from different countries, with the intent of eliminating these limitations and providing more credible findings.
Our results showed lower early mortality for hemiarch replacement, while there was no significant difference between the two procedures for re-operation rate. For emergency patients with aortic dissection, survival is the first priority, and thus the attending physician should treat the patient in the shortest possible time to avoid pericardial tamponade or rupture of the aorta, leading to death. Therefore, we believe that surgeons may perform hemiarch replacement in patients with intima tears in the root, the ascending aorta, or the proximal aorta to ensure greater chance of survival.
In addition, total arch replacement showed higher incidence of permanent neurological dysfunction, kidney failure, and dialysis in this study, which corresponds with previous reports (5, 12). In total arch replacement, longer cardiopulmonary bypass time, aortic cross-clamping time, and the selective antegrade cerebral perfusion time were was associated with ischemia reperfusion injury of the organs. Further, when the elephant trunk stent was inserted into the true lumen of the descending aorta during the total arch replacement procedure, the risk of paraplegia and spinal cord injury increased.
However, our findings also suggested that the hemiarch group had higher late mortality during follow-up, as any residual dissection may increase the risk of rupture or reoperation. In line with this finding, Omura et al. (10) reported that the incidence of distal aortic events may be lower in patients following total arch replacement, and Yoshitake et al. (13) reported that patients that underwent total arch replacement with a frozen elephant trunk stent performed better in long-term survival. Overall, total arch replacement can better repair the aorta, increase false lumen thrombosis, and reduce later aortic adverse events. Therefore, total arch replacement was a more favorable treatment choice for patients with intimal tears involving the large curvature and the thoracic-abdominal descending aorta.
For patients with Marfan syndrome, a total arch replacement may also be a better decision. Studies have shown Marfan syndrome as a statistically significant risk factor for re-operation (14), and Zhang et al. (15) has suggested that extensive arch replacement should be more actively used due to a weak aortic wall in patients with Marfan syndrome. Further, Lio et al. (16) also posited that total arch replacement or more aggressive approaches may be preferred in young patients and those with Marfan syndrome. Our research also showed that there was no significant difference in the rate of re-operation between hemiarch and total arch replacement, but total arch replacement did carry the advantage of lower late mortality. Therefore, it was more appropriate for younger patients and patients with Marfan syndrome to choose total arch replacement.
It must be stated that meta-analysis was a double-edged weapon. Meta-analysis was a reanalysis of existing research results, and its data source was limited by many factors, such as publication bias and small sample size. Moreover, some diseases were difficult to conduct randomized controlled trials, and the demonstration strength of meta-analysis was far less than that of large-scale randomized controlled trials. The lack of homogeneity among the selected studies is always a threat to the consistency of the conclusions. However, meta-analysis can analyze the differences and reasons of multiple similar studies. When the results of multiple clinical trials are inconsistent or divergent, more scientific conclusions can be drawn through combined analysis. Our research results were also ideal and may provide some guidance for the treatment of ATAAD in the future.
Limitations
Our study had several limitations. First, we were unable to guarantee that patients included in the study had the same baseline level, and inherent differences between patients could not be avoided. Second, we were unable to guarantee that the same surgical techniques existed in all centers, which may have affected the statistics for patient outcomes. Regarding multiple surgical procedures for total arch replacement, we did not perform a subgroup analysis to count prognostic outcomes for the different surgical procedures. There was also a treatment bias in different hospitals, as total arch replacement was more often used in younger patients and in patients with Marfan syndrome, and we struggled to remove this bias. Finally, patient loss to follow-up and unreported deaths and complications had an impact on the pooled statistical results. As healthcare advances, it may be possible that subsequent studies will yield different outcomes.
Conclusion
In conclusion, we found that hemiarch replacement had a lower incidence of early mortality, postoperative permanent neurological dysfunction, renal failure, and dialysis in patients with AAAD. However, the late survival of the total arch replacement was better than that for hemiarch replacement. As ATAAD can be a dangerous emergent condition, we believe that early survival is also important. For aortic intimal tears confined to the root, the ascending aorta, or the proximal aorta, hemiarch replacement was more desirable. When intimal tears involved the arch and the thoracic-abdominal descending aorta, total arch replacement were more appropriate, and may allow patients to obtain better long-term results. Surgical strategy was also based on the experience of surgeons. These findings should provide some guidance on choosing an appropriate approach for the treatment of ATAAD.
Statements
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
LM and ZQ contributed to conception and design of the study. LM and TC organized the database. LM performed the statistical analysis and wrote the first draft of the manuscript. XZ and QW wrote sections of the manuscript. LC contributed to supervision. ZQ revised the manuscript critically for important intellectual content. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This work was funded by the Natural Science Foundation of Fujian Province (2020J02056).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.988619/full#supplementary-material
Supplementary Figure 1GRADEpro GDT.
Supplementary Figure 2Neuroprotection strategies in hemiarch and total arch replacement.
Supplementary Figure 3Early mortality.
Supplementary Figure 4Forest plots. (A) Forest plot of temporary neurological dysfunction. (B) Forest plot of permanent neurological dysfunction. (C). Forest plot of renal failure and dialysis. (D) Forest plot of re-operation for bleeding. (E) Forest plot of aortic re-operation. (F) Forest plot of pneumonia.
Supplementary Figure 5Funnel plots. (A) Funnel plot of early mortality. (B) Funnel plot of pneumonia.
References
1.
Tsai TT Trimarchi S Nienaber CA . Acute aortic dissection: perspectives from the International Registry of Acute Aortic Dissection (IRAD).Eur J Vasc Endovasc Surg. (2009) 37:149–59. 10.1016/j.ejvs.2008.11.032
2.
Hirst JRAE Johns JRVJ Kime JRSW . Dissecting aneurysm of the aorta: a review of 505 cases.Medicine. (1958) 37:217. 10.1097/00005792-195809000-00003
3.
Malaisrie SC Duncan BF Mehta CK Badiwala MV Rinewalt D Kruse J et al The addition of hemiarch replacement to aortic root surgery does not affect safety. J Thorac Cardiovasc Surg. (2015) 150:118–24.e2. 10.1016/j.jtcvs.2015.03.020
4.
Sun L Qi R Zhu J Liu Y Zheng J . Total arch replacement combined with stented elephant trunk implantation.Circulation. (2011) 123:971–8. 10.1161/CIRCULATIONAHA.110.015081
5.
Poon SS Theologou T Harrington D Kuduvalli M Oo A Field M . Hemiarch versus total aortic arch replacement in acute type A dissection: a systematic review and meta-analysis.Ann Cardiothorac Surg. (2016) 5:156–73. 10.21037/acs.2016.05.06
6.
Wells G Shea B O’Connell D Peterson J Welch V Losos M et al The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analysis. Ottawa, ON: University of Ottawa (2013).
7.
Stroup DF Berlin JA Morton SC Olkin I Williamson GD Rennie D et al Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. (2000) 283:2008–12. 10.1001/jama.283.15.2008
8.
Ohtsubo S Itoh T Takarabe K Rikitake K Furukawa K Suda H et al Surgical results of hemiarch replacement for acute type a dissection. Ann Thorac Surg. (2002) 74:S1853–6. 10.1016/S0003-4975(02)04133-4
9.
Westaby S Saito S Katsumata T . Acute type A dissection: conservative methods provide consistently low mortality.Ann Thorac Surg. (2002) 73:707–13. 10.1016/S0003-4975(01)03449-X
10.
Omura A Miyahara S Yamanaka K Sakamoto T Matsumori M Okada K et al Early and late outcomes of repaired acute DeBakey type I aortic dissection after graft replacement. J Thorac Cardiovasc Surg. (2016) 151:341–8. 10.1016/j.jtcvs.2015.03.068
11.
Qin W Su C Li L Carmichael M Huang F Chen X . Is limited aortic resection more justified in elderly patients with type A acute aortic dissection?J Cardiothorac Surg. (2020) 15:183. 10.1186/s13019-020-01234-8
12.
Kim JB Chung CH Moon DH Ha GJ Lee TY Jung SH et al Total arch repair versus hemiarch repair in the management of acute DeBakey type I aortic dissection. Eur J Cardiothorac Surg. (2011) 40:881–9. 10.1016/j.ejcts.2010.12.035
13.
Yoshitake A Tochii M Tikunaga C Hayashi J Takazawa A Yamashita K et al Early and long-term results of total arch replacement with the frozen elephant turnk technique for acute type A aortic dissection. Eur J Cardiothorac Surg. (2020) 58:707–13. 10.1093/ejcts/ezaa099
14.
Shiono M Hata M Sezai A Niino T Yagi S Negishi N . Validity of a limited ascending and hemiarch replacement for acute Type A aortic dissection.Ann Thorac Surg. (2006) 82:1665–9. 10.1016/j.athoracsur.2006.05.112
15.
Zhang H Lang X Lu F Song Z Wang J Han L et al Acute type A dissection without intimal tear in arch: Proximal or extensive repair? J Thorac Cardiovasc Surg. (2014) 147:1251–5. 10.1016/j.jtcvs.2013.04.029
16.
Lio A Nicolò F Bovio E Serrão AC Zeitani J Scafuri AG et al Total arch versus hemiarch replacement for Type A acute aortic dissection: a single-center experience. Tex Heart Inst J. (2016) 43:488–95. 10.14503/THIJ-15-5379
17.
Aizawa K Kawahito K Misawa Y . Long-term outcomes of tear-oriented ascending/hemiarch replacements for acute type A aortic dissection.Gen Thorac Cardiovasc Surg. (2016) 64:403–8. 10.1007/s11748-016-0648-x
18.
Chen S-W Chen Y Ma W-G Zhong YL Qiao ZY Ge YP et al Limited vs. extended repair for acute type I aortic dissection: long-term outcomes over a decade in Beijing Anzhen Hospital. Chin Med J. (2021) 134:986–8. 10.1097/CM9.0000000000001416
19.
Colli A Carrozzini M Francescato A Galuppo M Comisso M Toto F et al Acute DeBakey type I aortic dissection without intimal tear in the arch: is total arch replacement the right choice? Interact Cardiovasc Thorac Surg. (2017) 26:84–90. 10.1093/icvts/ivx229
20.
Dai X-F Chen L-W Wu X-J Dong Y Wang Q-M . Total aortic arch reconstruction with triple-branched stent graft or hemiarch replacement for acute debakey type I Aortic Dissection: five-years experience with 93 patients.J Cardiac Surg. (2015) 30:749–55. 10.1111/jocs.12608
21.
Di Eusanio M Berretta P Cefarelli M Jacopo A Murana G Castrovinci S et al Total arch replacement versus more conservative management in type a acute aortic dissection. Ann Thorac Surg. (2015) 100:88–94. 10.1016/j.athoracsur.2015.02.041
22.
Lee CH Cho JW Jang JS Yoon TH . Surgical outcomes of type a aortic dissection at a small-volume medical center: analysis according to the extent of surgery.Korean J Thorac Cardiovasc Surg. (2020) 53:58–63. 10.5090/kjtcs.2020.53.2.58
23.
Merkle J Sabashnikov A Deppe A-C Zeriouh M Maier JA Weber C et al Impact of ascending aortic, hemiarch and arch repair on early and long-term outcomes in patients with Stanford A acute aortic dissection. Ther Adv Cardiovasc Dis. (2018) 12:327–40. 10.1177/1753944718801568
24.
Ok YJ Kang SR Kim HJ Kim JB Choo SJ . Comparative outcomes of total arch versus hemiarch repair in acute DeBakey type I aortic dissection: the impact of 21 years of experience.Eur J Cardiothorac Surg. (2021) 60:967–75. 10.1093/ejcts/ezab189
25.
Patel PM Dong A Chiou E Wei J Binongo J Leshnower B et al Aortic arch management during acute and subacute Type A aortic syndromes. Ann Thorac Surg. (2022) 114:694–701. 10.1016/j.athoracsur.2021.12.064
26.
Rice RD Sandhu HK Leake SS Afifi RO Azizzadeh A Charlton-Ouw KM et al Is total arch replacement associated with worse outcomes during repair of acute type A aortic dissection? Ann Thorac Surg. (2015) 100:2159–66. 10.1016/j.athoracsur.2015.06.007
27.
Rylski B Beyersdorf F Kari FA Schlosser J Blanke P Siepe M . Acute type A aortic dissection extending beyond ascending aorta: limited or extensive distal repair.J Thorac Cardiovasc Surg. (2014) 148:949–54. 10.1016/j.jtcvs.2014.05.051
28.
Shi E Gu T Yu Y Yu L Wang C Fang Q et al Early and midterm outcomes of hemiarch replacement combined with stented elephant trunk in the management of acute DeBakey type I aortic dissection: comparison with total arch replacement. J Thorac Cardiovasc Surg. (2014) 148:2125–31. 10.1016/j.jtcvs.2013.10.058
29.
Uchida N Shibamura H Katayama A Shimada N Sutoh M Ishihara H . Operative strategy for acute type A aortic dissection: ascending aortic or hemiarch versus total arch replacement with frozen elephant trunk.Ann Thorac Surg. (2009) 87:773–7. 10.1016/j.athoracsur.2008.11.061
30.
Vallabhajosyula P Gottret JP Robb JD Szeto WY Desai ND Pochettino A et al Hemiarch replacement with concomitant antegrade stent grafting of the descending thoracic aorta versus total arch replacement for treatment of acute DeBakey I aortic dissection with arch tear. Eur J Cardiothorac Surg. (2015) 49:1256–61. 10.1093/ejcts/ezv374
31.
Vendramin I Piani D Lechiancole A Sponga S Di Nora C Londero F et al Hemiarch versus arch replacement in acute Type A aortic dissection: is the occam’s razor principle applicable? J Clin Med. (2021) 11:114. 10.3390/jcm11010114
32.
Yang B Norton EL Shih T Farhat L Wu X Hornsby WE et al Late outcomes of strategic arch resection in acute type A aortic dissection. J Thorac Cardiovasc Surg. (2019) 157:1313–21.e2. 10.1016/j.jtcvs.2018.10.139
Summary
Keywords
hemiarch replacement, total arch replacement, type A aortic dissection, meta-analysis, adult
Citation
Ma L, Chai T, Yang X, Zhuang X, Wu Q, Chen L and Qiu Z (2022) Outcomes of hemi- vs. total arch replacement in acute type A aortic dissection: A systematic review and meta-analysis. Front. Cardiovasc. Med. 9:988619. doi: 10.3389/fcvm.2022.988619
Received
07 July 2022
Accepted
01 September 2022
Published
27 September 2022
Volume
9 - 2022
Edited by
Jinlin Wu, Guangdong Provincial People’s Hospital, China
Reviewed by
Randolph Wong, Prince of Wales Hospital, China; Carlo Bassano, University of Rome Tor Vergata, Italy
Updates
Copyright
© 2022 Ma, Chai, Yang, Zhuang, Wu, Chen and Qiu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liangwan Chen, chenliangwan@tom.comZhihuang Qiu, qzhflm@126.com
This article was submitted to Heart Surgery, a section of the journal Frontiers in Cardiovascular Medicine
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.