Abstract
Objective:
Traditional Chinese exercises (TCE) are excellent cardiac rehabilitation (CR) training that can effectively improve cardiorespiratory fitness. However, there is no published meta-analysis of TCE on CR in patients with myocardial infarction (MI). Therefore, this study aimed to provide a comprehensive evaluation from multiple perspectives.
Methods:
This meta-analysis is based on the Cochrane Handbook of Systematic Reviews. Eight databases were searched from the date of database construction to March 15, 2023. Two investigators independently screened the literature and assessed their quality. The meta-analysis was performed with RevMan5.4 software.
Results:
A total of 21 articles involving 1,890 patients were included. N-terminal pro-brain natriuretic peptide (NT-proBNP) in the TCE group were lower than the control group (MD = −96.34, 95%CI: −140.69 ∼−51.98, P < 0.00001, I2 = 96%), the left ventricular ejection fraction (LVEF) in the TCE group was higher than the control group (MD = 4.58, 95%CI: 3.28–5.88, P < 0.00001, I2 = 79%), the left ventricular end diastolic dimension (LVDD) in TCE group was lower than the control group (MD = −3.83, 95%CI: −5.27 ∼−2.38, P < 0.00001, I2 = 94%), the left ventricular end systolic diameter (LVESD) in TCE group was lower than the control group (MD = −2.17, 95%CI: −4.10 ∼−0.24, P < 0.00001, I2 = 96%), The 6-minute walk test (6MWT) in the TCE group was higher than the control group (MD = 69.60, 95%CI: 34.59–104.60, P < 0.00001, I2 = 99%), the oxygen uptake (VO2) in the TCE group was higher than the control group (MD = 4.38, 95%CI: 2.25–6.51, P < 0.00001, I2 = 94%), the 36-item short form survey (SF-36) in the TCE group was higher than the control group (MD = 13.34, 95%CI: 9.25–17.42, P = 0.008, I2 = 75%), the Hamilton Anxiety Scale (HAMA) in the TCE group was lower than the control group (MD = −4.34, 95%CI: −5.18 ∼−3.50, P = 1.00, I2 = 0%), the Hamilton Depression Scale (HAMD) in the TCE group was lower than the control group (MD = −3.48, 95%CI: −5.35 ∼−1.61, P = 0.0002, I2 = 88%), the incidence of major adverse cardiac events (MACEs) in the TCE group was lower than the control group (RR = 0.31, 95%CI: 0.20–0.47, P = 0.52, I2 = 0%). Subgroup analysis revealed differences in TCE types could be a potential source of heterogeneity.
Conclusion:
MI patients who used TCE have not only notable improvements in cardiopulmonary function, physical function, quality of life, and emotions but also reduced the incidence of MACEs. Tai Chi might be more efficient than Ba Duan Jin.
Systematic Review Registration:
https://www.crd.york.ac.uk/PROSPERO/, identifier CRD42023408675.
1. Introduction
Cardiovascular disease (CVD) accounts for a large proportion of a range of non-communicable diseases. Acute myocardial infarction (AMI), one of the primary causes of death from coronary heart disease (CHD) (1), affects approximately 11.39 million individuals in China, where the prevalence of CVD is continually rising (2). The usual treatment for AMI often involves percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG), which can enhance the quality of life for myocardial infarction (MI) patients by restoring perfusion. However, how to recover the pre-morbid health status remains an urgent public health issue (2). Cardiac rehabilitation (CR) is a comprehensive multidisciplinary program specifically designed for patients with CVD. The main objectives are to increase daily function and lessen cardiovascular risk factors (3). The European Society of Cardiology, American Heart Association, and American College of Cardiology all suggest utilizing CR as a Class I standard of care following an AMI (4).
Traditional Chinese Exercise (TCE) is a type of therapeutic, aerobic, mind-body exercise that has a history dating back over 3,000 years from traditional Chinese medicine (5). TCE mainly includes Tai Chi, Ba Duan Jin, Qi Gong, Yi Jin Jing, Wu Qin Xi, and other low to medium-intensity exercises (6). As a mild muscle-strengthening sport, TCE combines spiritual meditation with moderate postures, musculoskeletal stretching, and deep breathing (7, 8). It has been shown in numerous studies to be an effective exercise for CR and to enhance cardiorespiratory health (9, 10).
Early and appropriate CR not only improves cardiac function and quality of life but also prognosis in MI patients. However, there is no published meta-analysis evaluating the effect of TCE in these patients. Accordingly, the purpose of this study is to systematically evaluate the effects from multiple perspectives and provide a resource for future clinical advice.
2. Materials and methods
The Cochrane Handbook of Systematic Reviews served as the foundation for our meta-analysis. The results of this study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. This meta-analysis has been registered in PROSPERO (registration number: CRD42023408675).
2.1. Search strategy
The relevant literature published in Pubmed, Web of Science, Cochrane Library, Embase, China Knowledge Network (CNKI), Vipshop database (VIP), Wanfang Knowledge Service Platform, and Sinomed Database from inception to March 15, 2023, were searched. The following search terms were utilized: (((((((traditional Chinese exercise [Title/Abstract]) OR (tai chi [Title/Abstract])) OR (tai ji [Title/Abstract])) OR (ba duan jin [Title/Abstract])) OR (yi jin jing [Title/Abstract])) OR (wu qin xi [Title/Abstract])) OR (qi gong [Title/Abstract])) AND (myocardial infarction [Title/Abstract]) AND (randomized [Title/Abstract]).
2.2. Study eligibility
Inclusion criteria: (1) The type of study is a randomized controlled trial (RCT). (2) The subjects were patients with a definite diagnosis of MI. (3) The intervention in the treatment group was TCE, such as Tai Chi, Ba Duan Jin, Qi Gong, Wu Qin Xi, or Yi Jin Jing. (4) The control group received conventional treatment or other exercises. (5) The effectiveness outcomes included N-terminal pro-brain natriuretic peptide (NT-proBNP), left ventricular ejection fraction (LVEF), left ventricular end diastolic dimension (LVDD), left ventricular end systolic diameter (LVESD), 6-minute walk test (6MWT), oxygen uptake(VO2), the 36-item short form survey (SF-36), Hamilton Depression Scale (HAMD), Hamilton Anxiety Scale (HAMA) and major adverse cardiac events (MACEs).
Exclusion criteria: (1) Duplicate literature. (2) Animal experiments, meta-analyses, and systematic reviews. (3) Studies with insufficient data, such as those in which the data could not be combined with other outcome indicators.
2.3. Data extraction
Two investigators independently screened the retrieved literature. Firstly, eliminate duplicate publications. Then read titles and abstracts to exclude the literature not relevant to the topic. Finally read the full text to identify whether the literature met the inclusion criteria and establish the information base, including author, country, year of publication, general information, interventions, outcomes, and indicators for conducting the quality evaluation. Discrepancies between investigators were resolved by discussion or a third independent reviewer.
2.4. Quality assessment
Cochrane Handbook (11) was used to assess the quality of the included literature for random sequence generation, allocation concealment, blinding, incomplete outcome data, selective reporting, and other biases. Each entry was evaluated for one of low risk, high risk, and unclear risk.
2.5. Statistical analysis
The meta-analysis was performed with the RevMan5.4 software. Dichotomous variables were expressed as relative risk (RR) and 95% confidence interval (CI), and continuous variables were expressed as mean difference (MD) and 95% CI. I2 was used to determine the heterogeneity. Meta-analysis was conducted using the fixed-effects model if P > 0.1 and I2 < 50%. Meta-analysis was conducted using the random-effects model if P ≤ 0.1 and I2 ≥ 50%. Sensitivity analysis and subgroup analysis were used to examine the source of heterogeneity. The publication bias was displayed in a funnel plot. The test level of the meta-analysis was set as α = 0.05.
3. Results
3.1. Search results and population characteristics
The study screening process is illustrated in Figure 1. A total of 258 articles were searched through the databases (21 from Pubmed, 28 from Web of Science, 20 from Embase, 29 from Cochrane Library, 48 from CNKI, 33 from Wan Fang, 49 from VIP, and 30 from Sinomed). After removing duplicates and screening, 21 articles revolving 1,890 patients were eligible for meta-analysis. The general characteristics are summarized in Table 1. According to the table, 17 studies were from China and one was from Brazil. Interventions included Ba Duan Jin, Tai Chi Quan, and Tai Chi Ball. Intervention duration ranged from two weeks to one year.
Figure 1
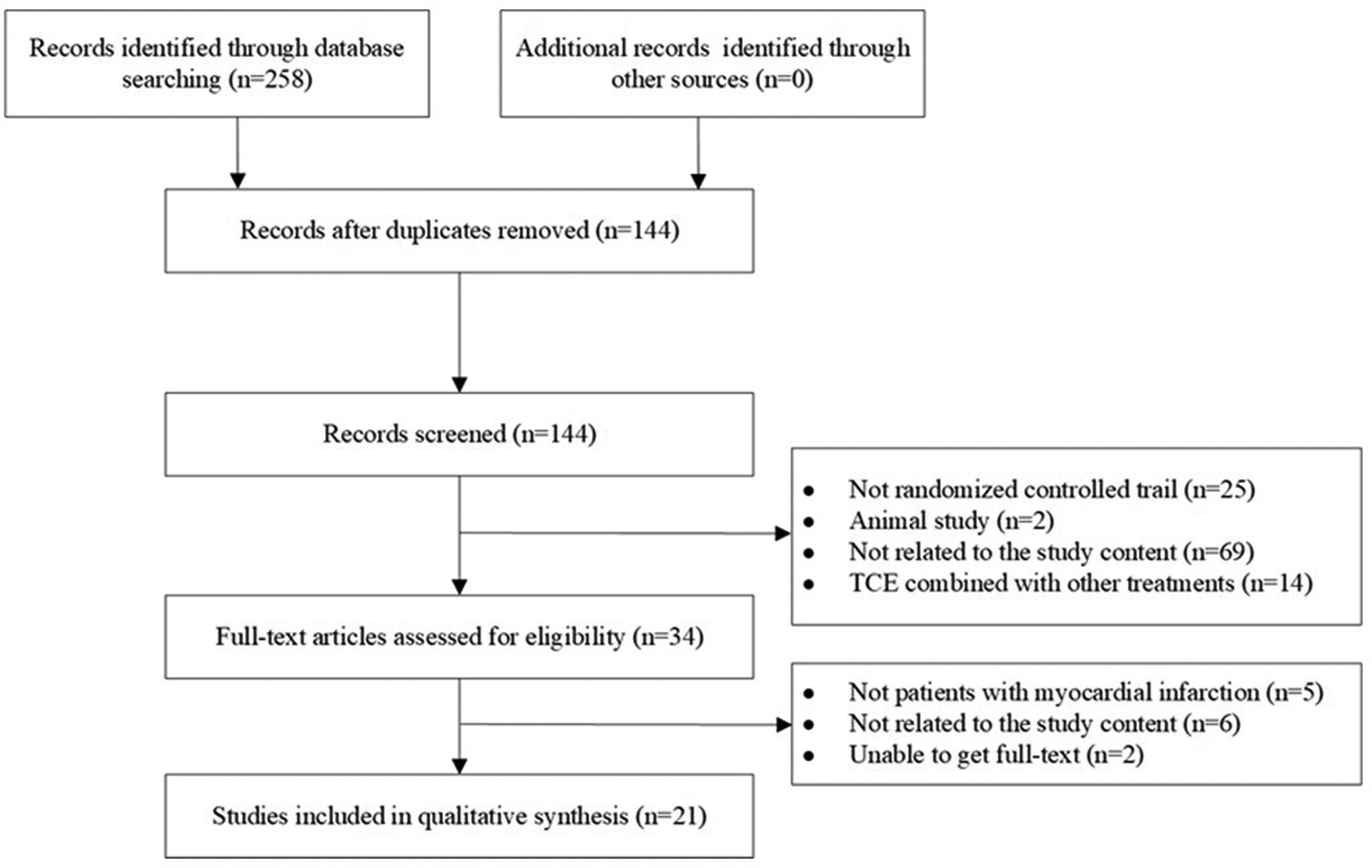
Flow chart of the search strategy.
Table 1
| Number | Study | Country | Patients | n (T/C) | Age (T/C, years old) | Intervention (T/C) | Duration | Outcomes |
|---|---|---|---|---|---|---|---|---|
| 1 | Wang et al. (12) | China | AMI | 75/75 | 59.3 ± 15.4/58.8 ± 12.5 | CT and Ba Duan Jin/CT and conventional exercise | 6 months | ①③④⑤⑩ |
| 2 | Cai et al. (13) | China | AMI | 45/45 | 49.58 ± 9.41/49.47 ± 9.32 | CT and Ba Duan Jin/CT | 2 weeks | ⑤⑥ |
| 3 | Wang et al. (14) | China | AMI | 40/40 | 59.54 ± 14.78/58.65 ± 17.38 | CT and Ba Duan Jin/CT | 2 weeks | ⑦ |
| 4 | Zhang et al. (15) | China | AMI | 35/35 | 59.42 ± 7.022/58.65 ± 7.027 | CT and Ba Duan Jin/CT | 8 weeks | ①② |
| 5 | Zhou et al. (16) | China | AMI | 50/50 | 57.87 ± 4.61/58.41 ± 4.52 | CT and Ba Duan Jin/CT | 3 months | ①③④⑤ |
| 6 | Zong et al. (17) | China | AMI | 50/50 | 57.26 ± 6.84/56.91 ± 7.34 | CT and Ba Duan Jin/CT | 2 weeks | ①③④⑥⑦⑩ |
| 7 | Kang et al. (18) | China | AMI | 30/30 | 51.27 ± 10.62/51.33 ± 9.95 | CT and Ba Duan Jin/CT | 2 months | ①③⑤⑧⑨ |
| 8 | Liu et al. (19) | China | STEMI | 30/30 | 56.21 ± 10.44/57.32 ± 11.36 | CT and Ba Duan Jin/CT | 12 weeks | ①②⑤ |
| 9 | Guo and Jia (20) | China | AMI | 60/60 | 58.21 ± 8.12/58.01 ± 9.54 | CT and Ba Duan Jin + Tai Chi Ball/CT | 1 month | ①②⑨⑩ |
| 10 | Li (21) | China | AMI | 30/30 | 60.33 ± 12.34/60.13 ± 9.78 | CT and Ba Duan Jin + Tai Chi Ball/CT | 2 months | ①②⑥⑧⑨ |
| 11 | Yang (22) | China | AMI | 69/69 | 63.19 ± 5.62/64.11 ± 5.64 | CT and Tai Chi Ball/CT | 4 weeks | ⑥ |
| 12 | Yu et al. (23) | China | AMI | 32/32 | 65.36 ± 4.12/66.33 ± 5.35 | CT and Tai Chi Quan/CT | 4 months | ①②③⑤ |
| 13 | Zhang and Chan (24) | China | AMI | 66/66 | 56.4 ± 4.3/55.7 ± 4.26 | CT and Tai Chi Quan/CT | 1 year | ①⑤⑦ |
| 14 | Wang et al. (25) | China | STEMI | 30/30 | 55.25 ± 11.13/54.86 ± 12.05 | CT and Tai Chi Quan/CT | 6 months | ②⑦ |
| 15 | Liu et al. (26) | China | AMI | 40/40 | <60 years old, 60–70 years old, ≥70 years old: 18, 8, 14/16, 9, 15 | CT and Tai Chi Quan/CT | 12 weeks | ①②⑩ |
| 16 | Lu (27) | China | AMI | 48/48 | 65.30 ± 2.45/66.07 ± 2.84 | CT and Tai Chi Quan + Ba Duan Jin/CT | 3 months | ①③⑤⑩ |
| 17 | Yu et al. (28) | China | AMI | 53/53 | 61.13 ± 11.06/60.4 ± 11.37 | CT and Ba Duan Jin/CT | 6 months | ①③④⑤ |
| 18 | Li et al. (29) | China | AMI | 29/28 | 58.52 ± 5.95/57.57 ± 6.69 | CT and Tai Chi Quan/CT | 6 months | ⑤ |
| 19 | Mao et al. (30) | China | AMI | 56/54 | 60.43 ± 10.21/61.30 ± 11.12 | CT and Ba Duan Jin/CT | 12 weeks | ①③ |
| 20 | Chen et al. (31) | China | AMI | 48/48 | 59.98 ± 10.86/61.49 ± 11.54 | CT and Ba Duan Jin/CT | 24 weeks | ① |
| 21 | Rosane et al. (32) | Brazil | AMI | 31/31 | 56 ± 9/60 ± 9 | CT and Tai Chi Quan/CT + spinal stretching exercise | 12 weeks | ⑥ |
Characteristics of the clinical trials included in the meta-analysis.
AMI, acute myocardial infarction; STEMI, ST-segment elevation myocardial infarction; T, traditional Chinese exercise rehabilitation group; C, control group; CT, conventional treatment; ① LVEF ② NT-proBNP ③ LVDD ④ LVESD ⑤ 6MWT ⑥ VO2 ⑦ SF-36 ⑧ HAMA ⑨ HAMD ⑩ MACEs.
3.2. Quality assessment
The results of the risk of bias evaluation of the included literature are presented in Supplementary Table S1. Two studies (12, 28) employed random samplings, 16 studies utilized random number table grouping and three studies (24–26) did not describe the randomization method. Only Rosane (32) used blinding of outcome assessment.
3.3. Meta analysis
3.3.1. Effects of TCE on Nt-proBNP
Seven articles involving 514 patients reported NT-proBNP levels. The NT-proBNP of patients who engaged in TCE was significantly less compared with the control group based on a random-effects model (MD = −96.34, 95%CI: −140.69–−51.98, P < 0.00001, I2 = 96%) (Figure 2).
Figure 2
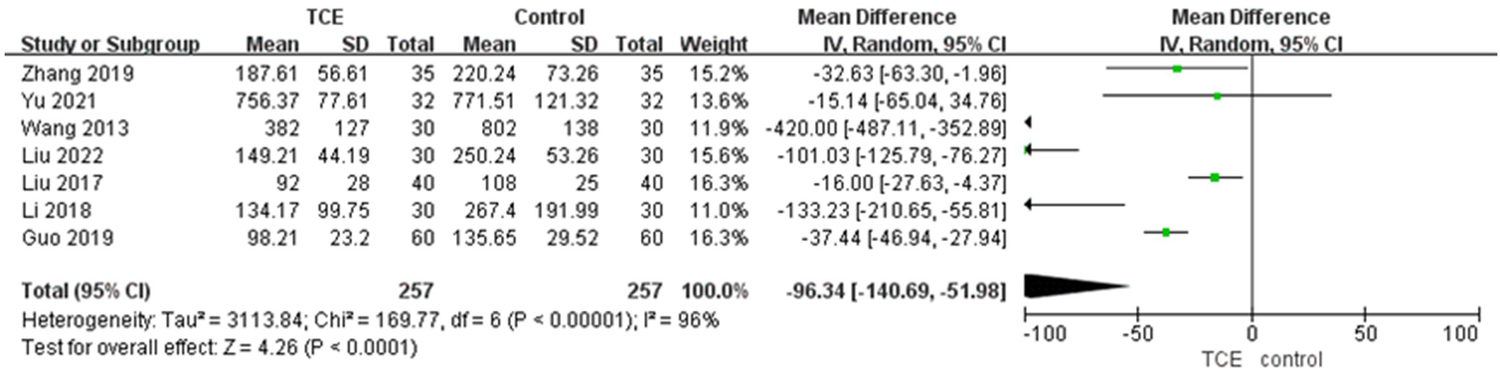
The forest plot of NT-proBNP.
3.3.2. Effects of TCE on echocardiographic indicators of cardiac function
15 articles involving 1,404 patients reported the LVEF outcome. The LVEF of patients who engaged in TCE was significantly improved compared with the control group based on a random-effects model (MD = 4.58, 95%CI: 3.28–5.88, P < 0.00001, I2 = 79%) (Figure 3A).
Figure 3
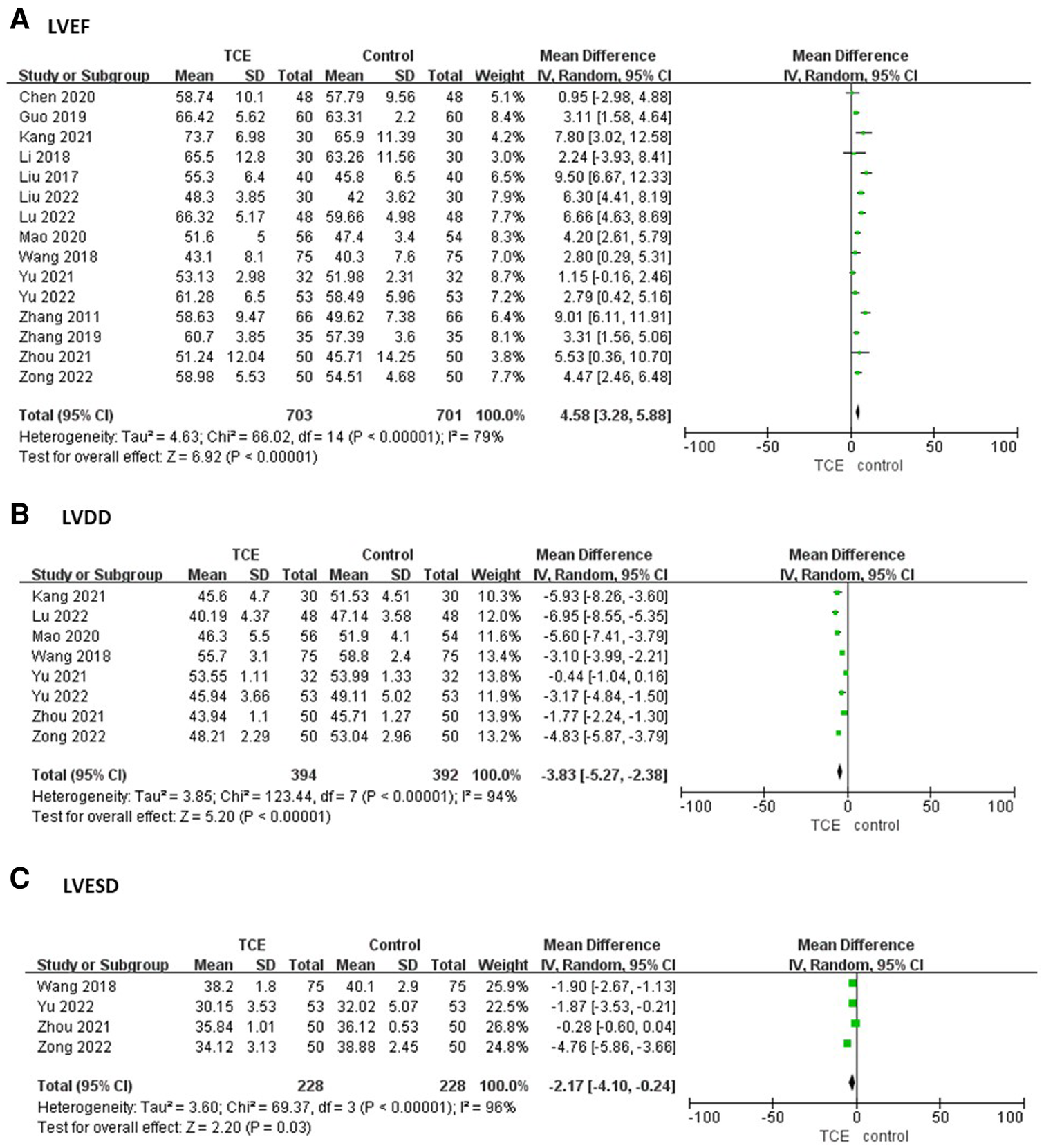
The forest plots of (A) LVEF, (B) LVDD, (C) LVESD.
Eight studies involving 786 patients reported the LVDD outcome. The LVDD of patients who engaged in TCE was significantly less compared with the control group based on a random-effects model (MD = −3.83, 95%CI: −5.27–−2.38, P < 0.00001, I2 = 94%) (Figure 3B).
Four studies involving 456 patients reported the LVESD outcome. The LVESD of patients who engaged in TCE was significantly less compared with the control group based on a random-effects model (MD = −2.17, 95%CI: −4.10–−0.24, P < 0.00001, I2 = 96%) (Figure 3C).
3.3.3. Effects of TCE on physical function
Ten studies involving 915 patients reported the 6MWT outcome. The 6MWT of patients who engaged in TCE was significantly improved compared with the control group based on a random-effects model (MD = 69.60, 95%CI: 34.59–104.60, P < 0.00001, I2 = 99%) (Figure 4A).
Figure 4
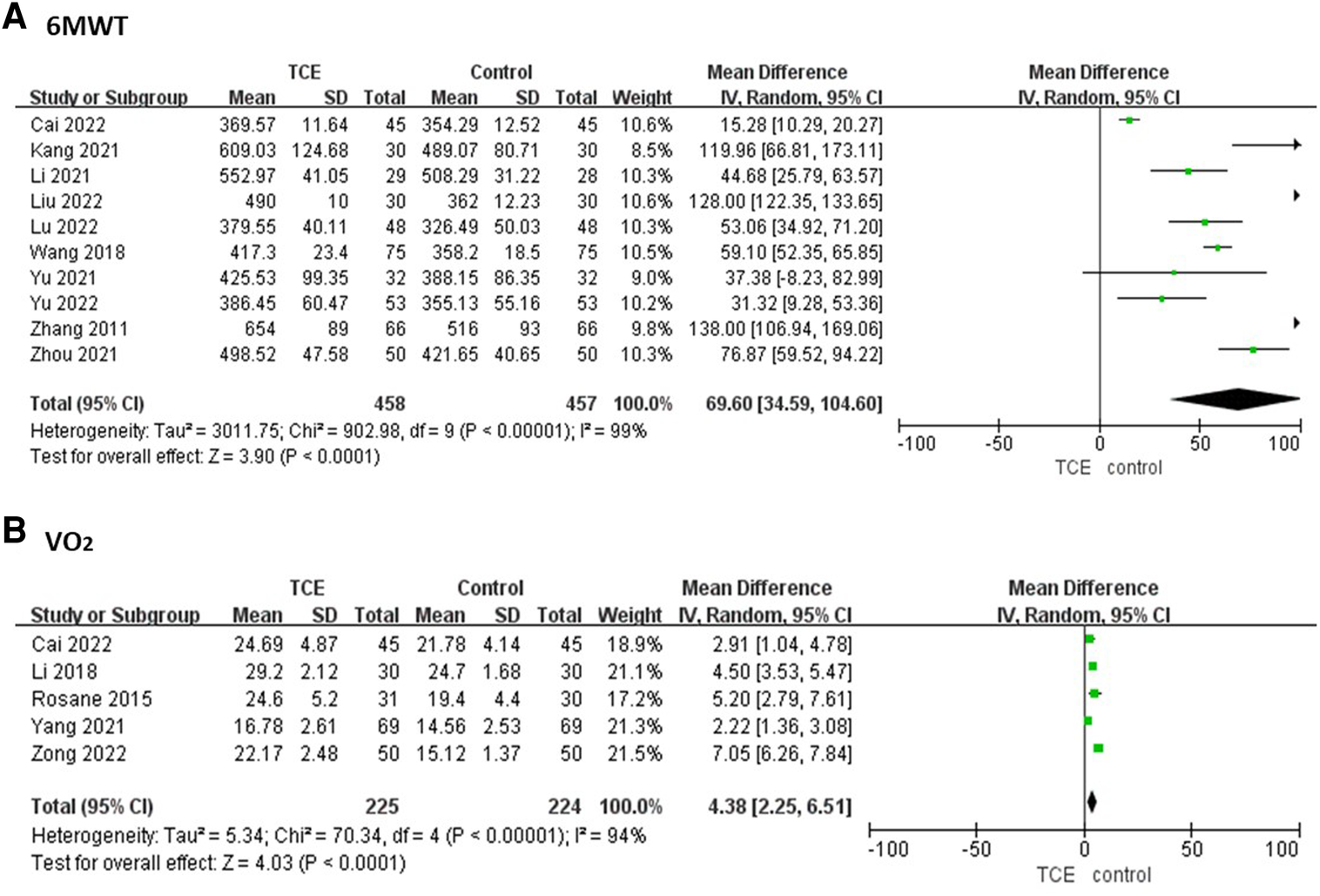
The forest plots of (A) 6MWT, (B) VO2.
Five studies involving 448 patients reported the VO2 outcome. The VO2 of patients who engaged in TCE was significantly improved compared with the control group based on a random-effects model (MD = 4.38, 95%CI: 2.25–6.51, P < 0.00001, I2 = 94%) (Figure 4B).
3.3.4. Effects of TCE on quality of life
Four studies involving 372 patients estimated the quality of life with SF-36 outcome. The SF-36 score of patients who engaged in TCE was significantly improved compared with the control group based on a random-effects model (MD = 13.34, 95%CI: 9.25–17.42, P = 0.008, I2 = 75%) (Figure 5).
Figure 5
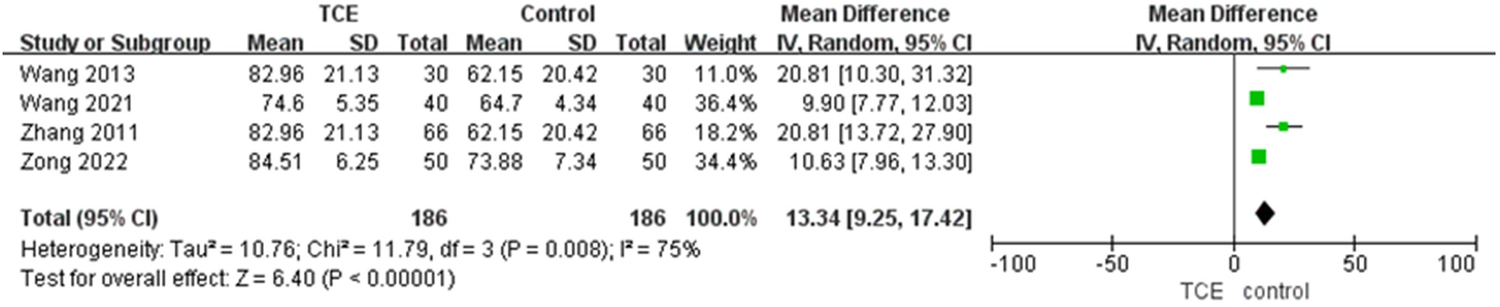
The forest plot of SF-36.
3.3.5. Effects of TCE on emotional distress
Two studies involving 120 patients reported the HAMA outcome. The HAMA of patients who engaged in TCE was significantly less compared with the control group based on a fixed-effects model (MD = −4.34, 95%CI: −5.18–−3.50, P = 1.00, I2 = 0%) (Figure 6A).
Figure 6
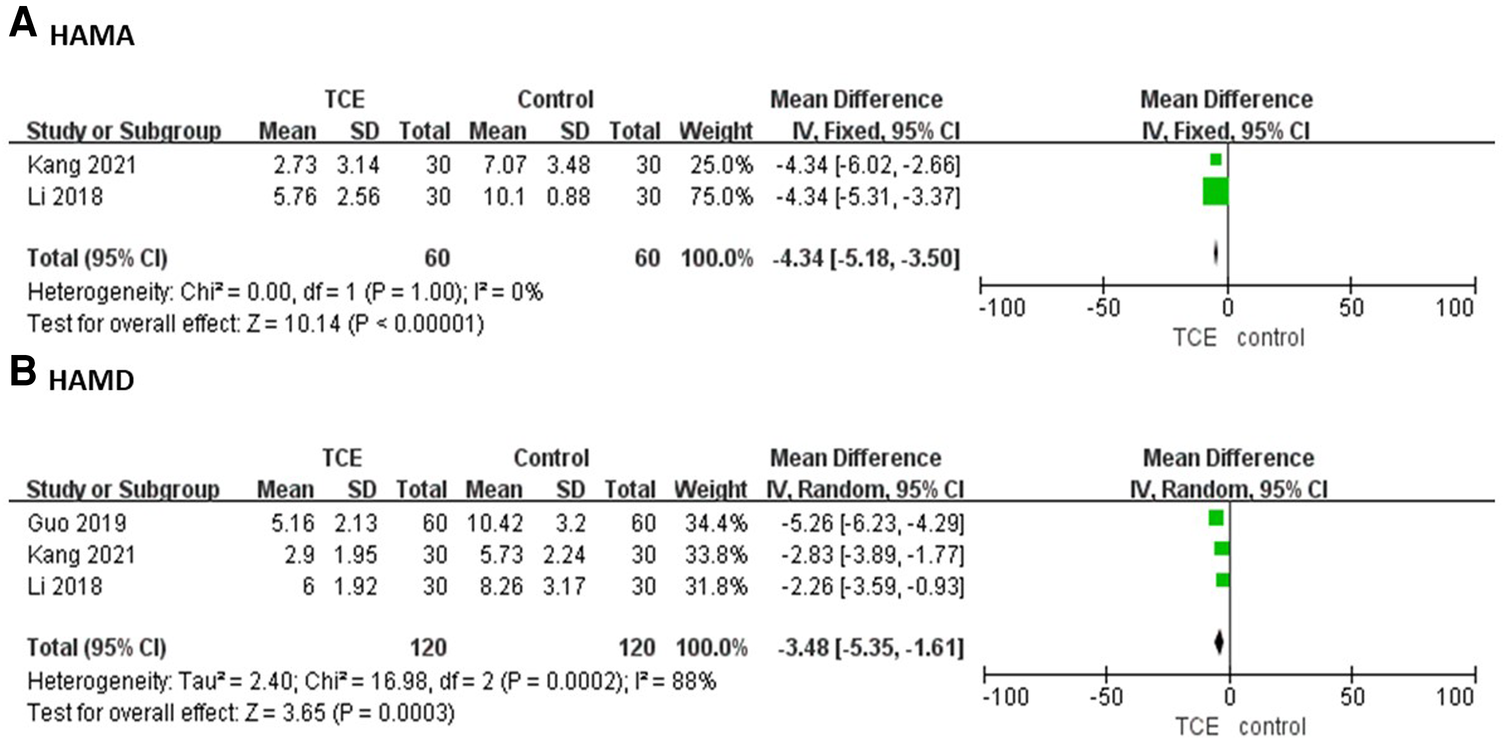
The forest plots of (A) HAMA, (B) HAMD.
Three studies involving 240 patients reported the HAMD outcome. The HAMD of patients who engaged in TCE was significantly less compared with the control group based on a random-effects model (MD = −3.48, 95%CI: −5.35–−1.61, P = 0.0002, I2 = 88%) (Figure 6B).
3.3.6. Effects of TCE on MCAEs
Five articles involving 526 patients reported the MACEs outcome. The incidence of MACEs of patients who engaged in TCE was significantly less compared with the control group based on a fixed-effects model (RR = 0.31, 95%CI: 0.20–0.47, P = 0.52, I2 = 0%) (Figure 7).
Figure 7
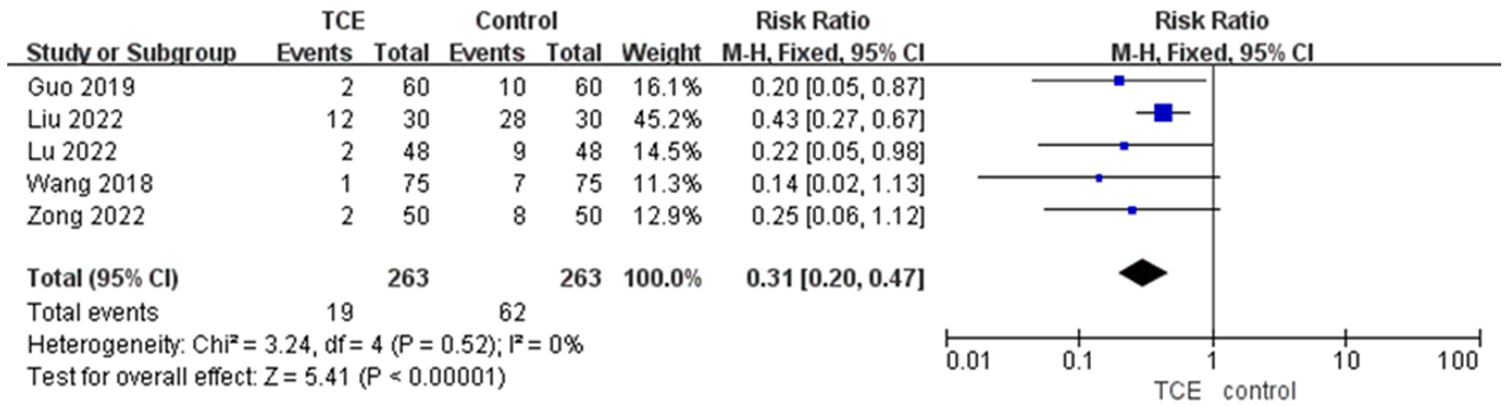
The forest plot of MCAEs.
3.4. Sensitivity analysis and subgroup analysis
Sensitivity analyses were performed by excluding each study one by one. The results revealed NT-proBNP, LVEF, LVDD, LVESD, 6MWT, and VO2 outcomes were not significantly altered. The sensitivity of the SF-36 outcome decreased when Zhang's study (24) was removed (I2 changed to 50%), and the sensitivity of the HAMD outcome decreased when Guo's study (20) was excluded (I2 changed to 0%).
Meanwhile, we implemented subgroup analyses of NT-proBNP, LVEF, 6MWT, VO2, and SF-36 outcomes according to the type of TCE in Table 2. There are three subgroups depending on the type of exercise: Tai Chi, Ba Duan Jin, and Tai Chi combined Ba Duan Jin. As shown the heterogeneity of subgroup analyses in NT-proBNP, LVEF and SF-36 outcomes significantly decreased.
Table 2
| Outcome | Subgroup | Number of studies | Sample size | MD (95%CI) | Statistical method | P value for heterogeneity | I 2 |
|---|---|---|---|---|---|---|---|
| NT-proBNP | Ba Duan Jin | 4 | 310 | −67.85 [−107.84, −27.87] | Random-effects | <0.00001 | 89% |
| Tai Chi | 3 | 204 | −147.93 [−344.66, 48.81] | Random-effects | <0.00001 | 99% | |
| LVEF | Ba Duan Jin | 10 | 972 | 3.93 [3.25, 4.61] | Fixed-effects | 0.10 | 39% |
| Tai Chi | 3 | 276 | 6.45 [0.25, 12.65] | Random-effects | <0.00001 | 95% | |
| Ba Duan Jin and Tai Chi | 2 | 156 | 6.23 [4.30, 8.16] | Fixed-effects | 0.18 | 44% | |
| 6MWT | Ba Duan Jin | 6 | 602 | 54.57 [29.03, 80.11] | Random-effects | <0.00001 | 97% |
| Tai Chi | 3 | 253 | 73.86 [9.35, 138.36] | Random-effects | <0.00001 | 93% | |
| VO2 | Ba Duan Jin | 2 | 190 | 5.07 [1.02, 9.21] | Random-effects | <0.00001 | 94% |
| Tai Chi | 2 | 199 | 3.49 [0.60,6.38] | Random-effects | 0.02 | 81% | |
| SF-36 | Ba Duan Jin | 2 | 180 | 10.18 [8.52, 11.85] | Fixed-effects | 0.68 | 0% |
| Tai Chi | 2 | 192 | 20.81 [14.93, 26.69] | Fixed-effects | 1.0 | 0% |
Subgroup analyses.
4. Publication bias
Funnel plots were used to assess the publication bias of the 21 included articles. We drew a funnel plot with the LVEF outcome divided into three subgroups as an example. As seen in Figure 8, all studies were relatively evenly distributed and located on both sides of the axis, and the bias was acceptable.
Figure 8
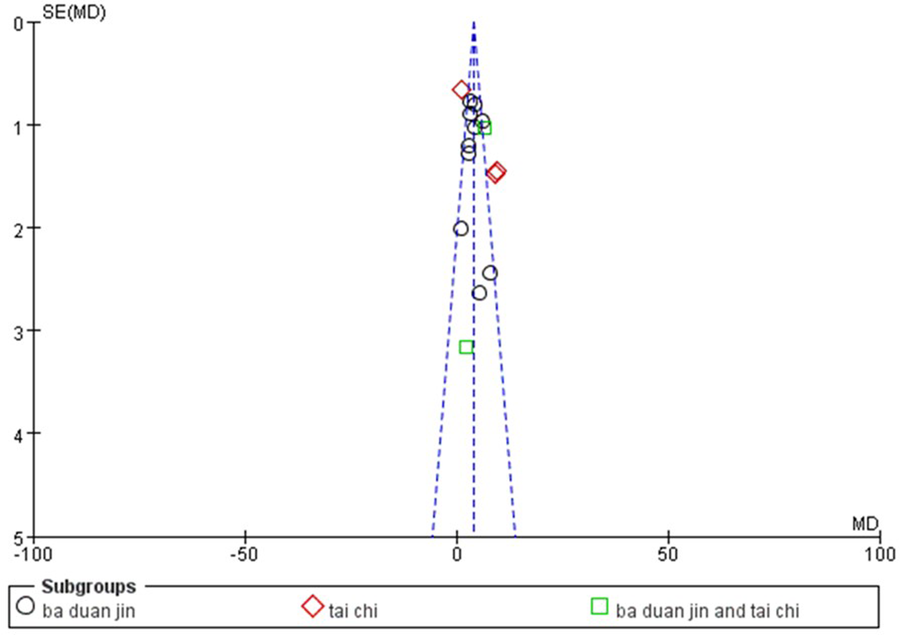
Funnel plot of LVEF.
5. Discussion
MI is a high-incidence disease worldwide, bringing a heavy social burden, especially for low and middle-income countries (33). Numerous studies have indicated that PCI only solves the blockage problem of blood vessels, but long-term rehabilitation exercises are still needed to restore myocardial function (34, 35). The common belief among patients is that after a MI, exercise should be avoided. However, patients who have undergone PCI or CABG should participate in a clinically supervised exercise program. According to Fernandez's study (36), patients who engage in CR have a 26% reduction in mortality and an 18% reduction in hospital readmission rates compared to patients who do not participate in CR. Exercises for post-MI rehabilitation are a crucial part of enhancing patients' quality of well-being and long-term prognosis following drug and surgical treatment. Additionally, it plays a key role in cardiac remodeling and cardiovascular regulation (37). Although CR is strongly recommended as a post-MI treatment, the current underuse is concerning (38, 39). Thus, our meta-analysis focused on MI patients. In recent years, TCEs such as Tai Chi, Qi Gong, and Ba Duan Jin have become increasingly popular around the world because of their gentle movements, low-risk, easy training, ancd long-term adherence. TCE is not only effective in regulating the physical condition and mental health of patients with Parkinson's disease, type 2 diabetes, chronic obstructive pulmonary disease, chronic pain disorders, and cancer but also beneficial in improving the cardiopulmonary function and quality of life (7).
A total of 21 RCTs comprising 1,890 patients were included for the first time to perform the meta-analysis. Unfortunately, Tai Chi and Ba Duan Jin were the only TCEs included. In comparison to the control group, patients in the TCE group demonstrated better results in NT-proBNP, LVEF, LVDD, LVESD, 6MWT, VO2, SF-36 scores, HAMA, and HAMD scale outcomes, and showed a decrease in the MACEs outcome. In addition, Ba Duan Jin and Tai Chi were likewise discovered to be safe, with no instances of TCE-related adverse events. This is consistent with Ting Liu's meta-analysis, Tai Chi increases social well-being and physical endurance in CHD patients (40). A randomized controlled trial reported that adapted personalized motor activity could improve health in individuals with mental disorders and physical comorbidities (41). Notably, our study further demonstrated that TCE improved the emotions of patients with MI as well. About 50% of patients experience anxiety after MI (42). Due to diminished cardiopulmonary function, which affects their capacity for employment and social contact as well as their long-term drug dependence, frequent hospitalizations, and significant financial stress, they are more prone to anxiety, depression, and other negative emotions. Therefore, TCE is very suitable and effective for MI patients to improve their mental and physical function. Apart from that, some researchers believed that TCE might influence cholesterol (18) and myocardial fibrosis levels (23) throughout the screening. However, the number of studies was not enough to perform a meta-analysis.
Furthermore, we conducted sensitivity analysis and subgroup analysis to investigate the source of heterogeneity. Except for HAMA and MACEs outcomes, some heterogeneity in the results of other outcomes may be due to certain clinical and methodological variations in different trials. Subgroup analysis revealed differences in TCE types as a potential source of heterogeneity and suggested that Tai Chi might be more efficient than Ba Duan Jin.
TCE involves the purposeful regulation of breath and thought, in harmony with the control of the body. Combining self-awareness with physical posture, the flow of breath, and stillness of thought is considered an exercise that activates the natural self-regulatory capacity to stimulate a balanced release of endogenous neurohormones (43). Overall, our meta-analysis provided reliable results in terms of TCE improving CR in patients with MI.
5.1. Limitations
This study has several limitations. Firstly, there is a lack of gray literature. If the findings from unpublished studies differ from the published data, the meta-analysis may become biased. Secondly, most of the included literature did not explicitly mention allocation concealment and only one study was blinded, so selection bias may be present. Finally, only Ba Duan Jin and Tai Chi were discussed in this essay. The majority of the included RCTs were Chinese, so language restrictions might lead to publication bias.
6. Conclusion
In conclusion, the use of TCE in MI patients showed significant improvements in cardiac function, physical function, quality of life, and mental health, also reduced the incidence of MACEs, which has good clinical application value and is recommended as a complementary therapy for CR in MI patients. It was found that Tai Chi might be more efficient than Ba Duan Jin. However, the above findings still need to be verified by more high-quality RCTs. The specific frequency and duration of different exercises should be analyzed to prescribe the most appropriate exercise prescription in the future.
Statements
Data availability statement
Publicly available datasets were analyzed in this study. The data analyzed in this article can be found here: PubMed (https://pubmed.ncbi.nlm.nih.gov/). Web Of Science (https://clarivate.com/products/web-of-science/). Cochrane library (https://www.cochranelibrary.com/). Embase (https://www.embase.com/). CNKI (https://www.cnki.net/). VIP (http://Lib.cqvip.com/). Wan Fang Databases (https://www.wanfangdata.com.cn/index.html). SinoMed (http://www.sinomed.ac.cn/index.jsp).
Author contributions
JZ: Study design, data analysis, and writing the original draft. JW and MY: Paper screening and data extraction. XCS and YW: Quality assessment. XXS: Writing-review and editing. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by the 2023 Science and Technology Innovation Special Project of Dongzhimen Hospital of Beijing University of Chinese Medicine, Grant/Award Number: DZMKJCX-2023-030.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1223677/full#supplementary-material
References
1.
The Writing of Committee Report on Cardiovascular Health and Diseases in China. Interpretation of report on cardiovascular health and diseases in China 2021. Chin J Cardiovasc Med. (2022) 27(04):305–18. 10.12114/j.issn.1007-9572.2022.0506
2.
Stevens W Peneva D Li JZ Liu LZ Liu G Gao RL et al Estimating the future burden of cardiovascular disease and the value of lipid and blood pressure control therapies in China. BMC Health Serv Res. (2016) 16(1):1–10. 10.1186/s12913-016-1420-8
3.
Servey JT Stephens MB . Cardiac rehabilitation: improving function and reducing risk. Am Fam Physician. (2016) 94(1):37–43.
4.
Prabhakaran D Chandrasekaran AM Singh K Mohan B Chattopadhyay K Chadha DS et al Yoga-based cardiac rehabilitation after acute myocardial infarction: a randomized trial. J Am Coll Cardiol. (2020) 75(13):1551–61. 10.1016/j.jacc.2020.01.050
5.
Li RJ Chen HW Feng JH Xiao Y Zhang HY Lam CWK et al Effectiveness of traditional Chinese exercise for symptoms of knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Int J Environ Res Public Health. (2020) 17(21):7873. 10.3390/ijerph17217873
6.
Jiang BC Feng CY Hu HL George D Huang TL Li ZH . Traditional Chinese exercise for neurodegenerative diseases: a bibliometric and visualized analysis with future directions. Front Aging Neurosci. (2022) 14:932924. 10.3389/fnagi.2022.932924
7.
Zeng ZP Liu YB Fang JJ Liu Y Luo J Yang M . Effects of baduanjin exercise for knee osteoarthritis: a systematic review and meta-analysis. Complement Ther Med. (2020) 48:102279. 10.1016/j.ctim.2019.102279
8.
Zhou ZL Zhou RZ Li KP Zhu Y Zhang ZQ Luo Y et al Effects of tai chi on physiology, balance and quality of life in patients with type 2 diabetes: a systematic review and meta-analysis. J Rehabil Med. (2019) 51(6):405–17. 10.2340/16501977-2555
9.
Yang YL Wang YH Wang SR Shi PS Wang C . The effect of tai chi on cardiorespiratory fitness for coronary disease rehabilitation: a systematic review and meta-analysis. Front Physiol. (2018) 8:1091. 10.3389/fphys.2017.01091
10.
Gu Q Wu SJ Zheng Y Zhang Y Liu C Hou JC et al Tai chi exercise for patients with chronic heart failure: a meta-analysis of randomized controlled trials. Am J Phy Med Rehabil. (2017) 96(10):706–16. 10.1097/PHM.0000000000000723
11.
Higgins J Thomas J Chandler J Cumpston M Li TJ Page M et al Cochrane handbook for systematic reviews of interventions (version 6.4). Chichester, UK: John Wiley & Sons, Ltd. (2023). https://training.cochrane.org/handbook/current
12.
Wang JM Liang C Wang B Pan DD He ZQ Li N et al The effect of sitting ba duan jin on post-intervention cardiac rehabilitation in patients with acute myocardial infarction. Chin J Integr Med Cardio Cerebrovasc Dis. (2018) 16(08):1082–5. 10.12102/j.issn.1672-1349.2018.08.027
13.
Cai Y Zheng HY Zhou YY Yang C Wang Y Yin J . Effect of ba duan jin Ⅰ cardiac rehabilitation exercises on cardiopulmonary function and sleep quality of patients after percutaneous coronary intervention for acute myocardial infarction. China Med Herald. (2022) 19(25):172–5. 10.20047/j.issn1673-7210.2022.25.39
14.
Wang XJ Liu Q Lian YH Tan JJ Li FQ . The effect of ba duan jin on the recent quality of life after emergency percutaneous coronary intervention in patients with acute myocardial infarction. Guangxi Med J. (2021) 43(02):245–7. 10.11675/j.issn.0253-4304.2021.02.28
15.
Zhang ZL . Efficacy evaluation of ba duan jin on stage II cardiac rehabilitation in patients after emergency. Fujian Univ Tradit Chin Med. (2019).
16.
Zhou YX Li SJ Xia WM Liu YY Cao QQ Wu KQ . Effect of baduanjin exercise on cardiac function and quality of life in patients with heart failure after myocardial infarction. China Modern Med. (2021) 28(25):73–75+79. 10.3969/j.issn.1674-4721.2021.25.019
17.
Zong S Cao J Sun WN Zhao P Hai X . Effects of baduanjin combined with cardiac exercise rehabilitation on cardiac function, exercise endurance and quality of life in patients with acute myocardial infarction after emergency PCI. Prog Modern Biomed. (2022) 22(21):4081–5. 10.13241/j.cnki.pmb.2022.21.014
18.
Kang L . To investigate the effect of baduanjin exercise therapy on cardiac rehabilitation of patients with acute myocardial infarction after PC. Guangzhou Univ Tradit Chin Med. (2021). 10.27044/d.cnki.ggzzu.2021.000768
19.
Liu GG Si T Shi L Zhang M Long WP . Efficacy of baduanjin in phase Ⅱ cardiac rehabilitation after PCI for acute myocardial infarction. World Chin Med. (2022) 17(19):2781–6. 10.3969/j.issn.1673-7202.2022.19.018
20.
Guo X Jia Y . The effect of taijiquan combined with ba duan jin on cardiac rehabilitation in patients with acute myocardial infarction after PCI. Henan Tradit Chin Med. (2019) 39(08):1247–51. 10.16367/j.issn.1003-5028.2019.08.0308
21.
Li GB . A clinical study of the effect of tai ji ball combined with ba duan jin on cardiac rehabilitation in patients with acute myocardial infarction after PCI. Guangzhou Univer Tradit Chin Med. (2018).
22.
Yang CY . Effect of tai ji ball exercise therapy on cardiopulmonary function and exercise function of patients with acute myocardial infarction in recovery period. Reflexol Rehabil Med. (2021) 2(4):18–21.
23.
Yu DM Deng XJ Zhou SH . To investigate the effect of taijiquan rehabilitation exercise on myocardial fibrosis markers in elderly patients with acute myocardial infarction after PCI. Chin J Integr Med Cardio Cerebrovasc Dis. (2021) 19(17):2960–3. 10.12102/j.issn.1672-1349.2021.17.017
24.
Zhang SQ Chen XH . Effect of taijiquan exercise on rehabilitation in patients with acute myocardial infarction. Chin Manip Rehabil Medieiqn. (2011) 7(56):32–3.
25.
Wang XK Zhang XL Ding FM Jiang WQ . Effects of taijiquan exercise on quality of life and BNP concentration in patients with STEMI after percutaneous coronary intervention. Guide China Med. (2013) 11(12):659–61. 10.3969/j.issn.1671-8194.2013.12.520
26.
Liu J Wang B Liang C Li H . Influence of tai chi exercise program on cardiac rehabilitation in patients with acute myocardial infarction undergoing percutaneous coronary intervention. Chin Nurs Res. (2017) 31(09):1043–8. 10.3969/j.issn.1009-6493.2017.09.007
27.
Lu M . Observation on the application effect of tai chi exercise combined with baduanjin in rehabilitation nursing of patients with acute myocardial infarction. Reflexol Rehabil Med. (2022) 3(10):28–31.
28.
Yu YY Jin DD Zhu YJ Zhai CL . Effects of sitting baduanjin on cardiac function rehabilitation in patients with acute anterior myocardial infarction after PCI. Chin J Tradit Med Sci Technol. (2022) 29(06):988–91.
29.
Li LY Zheng G Zhu FY Che DY . Application of tai chi in stage Ⅱ cardiac rehabilitation after acute myocardial infarction: a case series. Asian J Surg. (2021) 44(10):1322–3. 10.1016/j.asjsur.2021.06.037
30.
Mao S Zhang XX Chen MG Wang CY Chen QB Guo LH et al Beneficial effects of baduanjin exercise on left ventricular remodelling in patients after acute myocardial infarction: an exploratory clinical trial and proteomic analysis. Cardiovasc Drugs Ther. (2021) 35:21–32. 10.1007/s10557-020-07047-0
31.
Chen MG Liang XF Kong LL Wang JJ Wang FF Hu XY et al Effect of baduanjin sequential therapy on the quality of life and cardiac function in patients with AMI after PCI: a randomized controlled trial. Evid Based Complement Alternat Med. (2020) 2020:8171549. 10.1155/2020/8171549
32.
Nery RM Zanini M De Lima JB Bühler RP Da Silveira AD Stein R . Tai chi chuan improves functional capacity after myocardial infarction: a randomized clinical trial. Am Heart J. (2015) 169(6):854–60. 10.1016/j.ahj.2015.01.017
33.
Timmis A Townsend N Gale CP Torbica A Lettino M Petersen SE et al European society of cardiology: cardiovascular disease statistics 2019. Eur Heart J. (2020) 41(1):12–85. 10.1093/eurheartj/ehz859
34.
Batista DF Polegato BF Da Silva RC Claro RT Azevedo PS Fernandes AA et al Impact of modality and intensity of early exercise training on ventricular remodeling after myocardial infarction. Oxid Med Cell Longevity. (2020) 2020:5041791. 10.1155/2020/5041791
35.
Otto CM . Heartbeat: exercise improves quality of life after acute myocardial infarction. Heart. (2020) 106(22):1705–6. 10.1136/heartjnl-2020-318432
36.
Fernandez AB Thompson PD . Exercise training in athletes with heart disease. Prog Cardiovasc Dis. (2017) 60(1):121–9. 10.1016/j.pcad.2017.05.004
37.
Moraes-Silva IC Rodrigues B Coelho HJ Feriani DJ Irigoyen MC . Myocardial infarction and exercise training: evidence from basic science. Adv Exp Med Biol. (2017) 999:139–53. 10.1007/978-981-10-4307-9_9
38.
Ambrosetti M Abreu A Corrà U Davos CH Hansen D Frederix I et al Secondary prevention through comprehensive cardiovascular rehabilitation: from knowledge to implementation. 2020 update. A position paper from the secondary prevention and rehabilitation section of the European association of preventive cardiology. Eur J Prev Cardiol. (2021) 28(5):460–95. 10.1177/2047487320913379
39.
Kotseva K Wood D De Bacquer D . Determinants of participation and risk factor control according to attendance in cardiac rehabilitation programmes in coronary patients in Europe: EUROASPIRE IV survey. Eur J Prev Cardiol. (2018) 25(12):1242–51. 10.1177/2047487318781359
40.
Liu T Chan AWK Liu YH Taylor-Piliae RE . Effects of tai chi-based cardiac rehabilitation on aerobic endurance, psychosocial well-being, and cardiovascular risk reduction among patients with coronary heart disease: a systematic review and meta-analysis. Eur J Cardiovasc Nurs. (2018) 17(4):368–83. 10.1177/1474515117749592
41.
Lamberti V Palermi S Franceschin A Scapol G Lamberti V Lamberti C et al The effectiveness of adapted personalized motor activity (AMPA) to improve health in individuals with mental disorders and physical comorbidities: a randomized controlled trial. Sports. (2022) 10(3):30. 10.3390/sports10030030
42.
Wen Y Yang Y Shen J Luo SX . Anxiety and prognosis of patients with myocardial infarction: a meta-analysis. Clin Cardiol. (2021) 44(6):761–70. 10.1002/clc.23605
43.
Jahnke R Larkey L Rogers C Etnier J Lin F . A comprehensive review of health benefits of qigong and tai chi. Am J Health Promot. (2010) 24(6):e1–e25. 10.4278/ajhp.081013-LIT-248
Summary
Keywords
traditional Chinese exercise, tai chi, ba duan jin, cardiac rehabilitation, myocardial infarction, meta-analysis
Citation
Zhang J, Weng J, Yuan M, Shen X, Weng Y and Shen X (2023) Effects of traditional Chinese exercises on cardiac rehabilitation in patients with myocardial infarction: a meta-analysis of randomized controlled trials. Front. Cardiovasc. Med. 10:1223677. doi: 10.3389/fcvm.2023.1223677
Received
16 May 2023
Accepted
18 September 2023
Published
02 October 2023
Volume
10 - 2023
Edited by
Panagiotis Xaplanteris, Université Libre de Bruxelles, Belgium
Reviewed by
Stefano Palermi, University of Naples Federico II, Italy Thomas P. Olson, Mayo Clinic, United States
Updates
Copyright
© 2023 Zhang, Weng, Yuan, Shen, Weng and Shen.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Xiaoxu Shen shenxiaoxupaper@sina.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.