Abstract
Objective:
The goals of this scoping review were to determine the source of data used to develop AI-based algorithms with emphasis on natural language processing, establish their application in different areas of vascular surgery and identify a target audience of published journals.
Materials and methods:
A literature search was carried out using established database from January 1996 to March 2023.
Results:
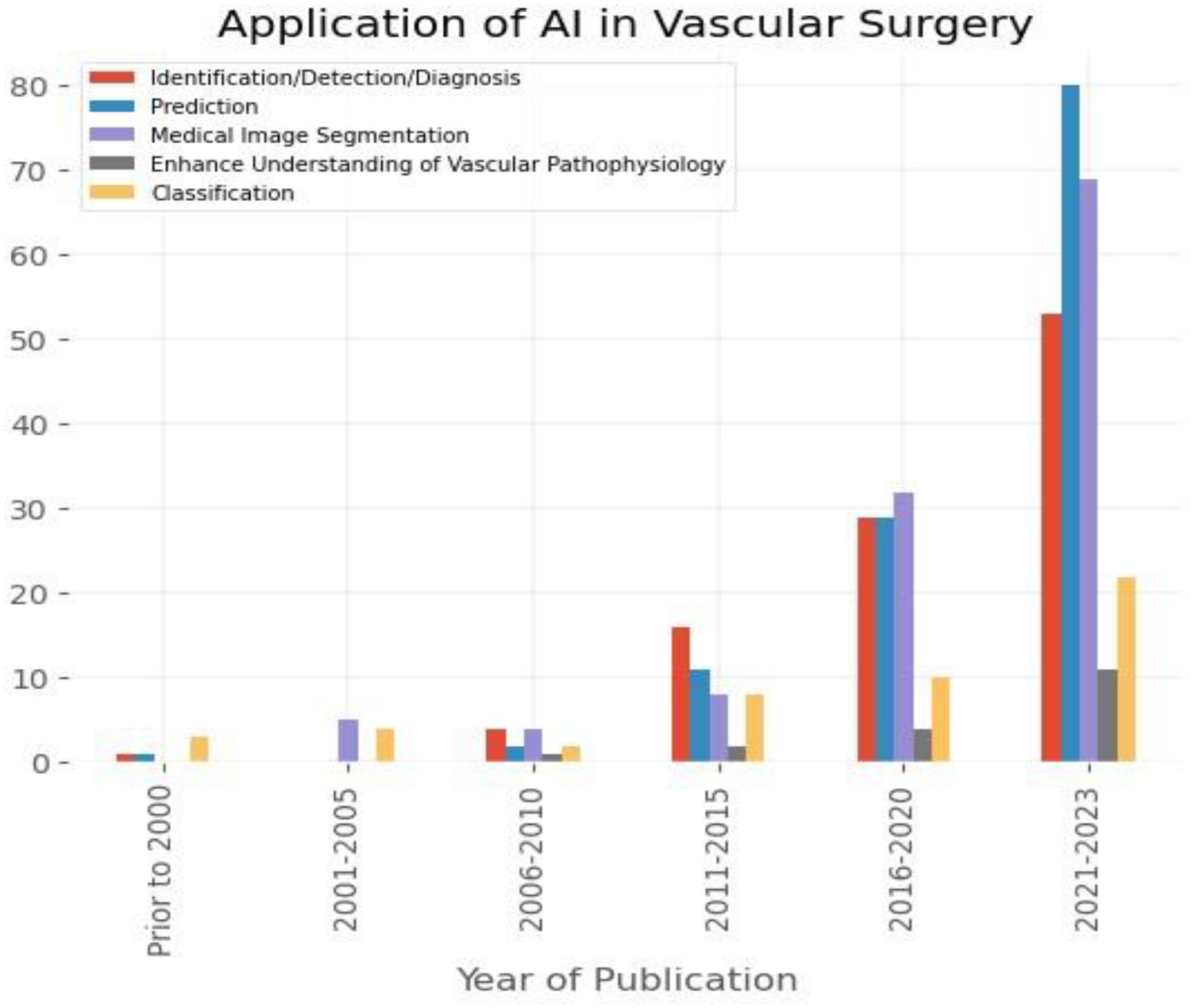
342 peer-reviewed articles met the eligibility criteria. NLP algorithms were described in 34 papers, while 115 and 193 papers focused on machine learning (ML) and deep learning (DL), respectively. The AI-based algorithms found widest application in research related to aorta (126 articles), carotid disease (85), and peripheral arterial disease (65). Image-based data were utilised in 216 articles, while 153 and 85 papers relied on medical records, and clinical parameters. The AI algorithms were used for predictive modelling (123 papers), medical image segmentation (118), and to aid identification, detection, and diagnosis (103).
Discussion:
Applications of Artificial Intelligence (AI) are gaining traction in healthcare, including vascular surgery. While most healthcare data is in the form of narrative text or audio recordings, natural language processing (NLP) offers the ability to extract information from unstructured medical records. This can be used to develop more accurate risk prediction models, support shared-decision model, and identify patients for trials to improve recruitment.
Conclusion:
Utilisation of different data sources and AI technologies depends on the purpose of the undertaken research. Despite the abundance of available of textual data, the NLP is disproportionally underutilised AI sub-domain in vascular surgery.
Introduction
The concept of artificial intelligence (AI) was first introduced in 1956 (1). According to the Commission Service on digital strategy for Europe, AI systems are software and hardware systems designed by humans that operate in digital and physical realms, gathering and interpreting data from their environment, to make decisions and take actions to achieve complex objectives (2, 3). Over the last two decades, an artificial intelligence technology has been increasingly utilised across the healthcare system to improve the quality of patients’ care and efficiency of medical resources and interventions (4). Electronic health records (EHR) allow for constantly growing collection of routine data including clinical notes, radiological reports, radiological and vascular images, physiological and physical metrics, laboratory and histopathology results, and administrative data. There is also an abundance of data derived from large-scale genetic studies and consumer devices such as wearables and smart phones. In many cases traditional statistical approaches fail to parse such large data to provide meaningful results, whereas AI algorithms can effectively handle large datasets and derive information, identifying complex non-linear relationships (5). Expeditious advancements in ML- and DL-based technologies could potentially be utilised in developing a more personalized therapeutic approach considering the patients’ general and clinical characteristics as well as a detailed characterization of the underlying cardio-vascular conditions.
The incorporation of digital technologies into health systems has transformed and rapidly increased in the last few years. It has been shown that incorporation of technologies such as remote monitoring, digital health applications, internet of things (IoT), and AI technologies during COVID-19 pandemic laid the groundwork for a more resilient and patient-centred healthcare system in the post-pandemic era (6, 7). Advancements in technology have expanded telemedicine capabilities with improved video and audio communication tools, remote monitoring devices, wearable devices, and health applications. These technologies enable remote diagnosis, monitoring, and managing various health conditions.
Constantly evolving AI technologies are utilised in disease identification, risk prediction and modelling, diagnosis, treatment planning, adverse events monitoring and follow up. Vascular surgery is not different in that respect. However, despite an increasing number of publications, there is a paucity of research exploring the source of information utilised to develop AI algorithms relevant to vascular surgery. To address this, we performed a scoping review that aimed to identify the source of input data utilised to develop AI algorithms with focus on NLP utilisation in vascular surgery. Our secondary goals include assessing application of AI algorithms across vascular surgery and identification of target audience of published results.
Methods
Machine learning (ML) is based on probabilistic and statistical techniques forming complex systems that can iteratively learn from data (8). Deep learning (DL), being a sub-field of ML, is a part of a wider family of artificial neural networks (ANN), defining an architecture that combines several processing layers to learn from data (9, 10). There are generally three approaches that ML and DL can utilise: supervised, unsupervised and reinforcement learning (9, 11). Natural language processing (NLP) refers to the machine's ability to identify, process, understand and/or generate information in written and spoken human communications (2). NLP applies computational techniques, that may include ML, or DL, or more basic statistical approaches to analyse speech and text and its tools have been used for information retrieval, classification, text extraction, text summarisation, question answering, and text generation utilising linguistics-focused or statistics-focused approaches, or a combination of these two (12, 13). A more extensive explanation of the principles of ML, DL and NLP is included in Appendix 1.
Cardiovascular diseases (CVDS) are the leading cause of death globally. According to World Health Organization (WHO) report published in 2021 [https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)], an estimated 17.9 million people's death was secondary to CVDs, representing 32% of global deaths. Brief description of clinical domains in vascular surgery where AI-based algorithms could be effectively utilised is provided in Appendix 2.
Data sources
This scoping review follows the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta Analyses extension for Scoping Reviews (PRISMA-ScR; https://www.equator-network.org/reportingguidelines/prismascr/). We conducted a literature search using the PubMed, EMBASE, and Google Scholar databases, covering the period from 01/01/1996 to 01/03/2023. No funding source supported this review.
Eligibility criteria
The predefined eligibility criteria encompassed literature in English or translated to English, published in peer reviewed journals, and met the population, intervention, comparison, and outcome criteria. Reviews, editorials, letters, and case reports were not considered for this review. For the population criteria, the exposure of interest included: aortic disease, carotid disease, peripheral artery disease (PAD), diabetic foot syndrome (DFS), vascular access surgery, arterial trauma, and lower limbs deep vein thrombosis. Articles referring to stroke management, ophthalmology, cardiac surgery, robotic surgery, education and diabetology were excluded. For the intervention criteria, studies were included if they evaluated AI-based algorithms, i.e., ML, DL, and NLP. For comparison and outcome criteria, there were no restrictions.
Search strategy and selection criteria
We used a combination of medical subjects’ headings, keywords, and other database-specific terminologies selected by a multidisciplinary team composed of AI experts (GG, LS) and vascular surgeons (MJ, MW, KP) to maximise the retrieval of relevant articles, including reference lists of related literature. Artificial intelligence constitutes an umbrella term and the keywords used in the search included “artificial intelligence”, “machine learning”, “deep learning”, “neural network”, and “natural language processing”. Clinical headings and key terms for non-cardiac vascular diseases included “aneurysm”, “carotid”, “peripheral arterial disease”, “revascularisation”, “dissection (artery or aorta)”, “vein”, “vessel trauma”, “venous”, “arterio-venous fistula”, vascular surgical procedures”, “vascular”, “diabetic foot” and “deep venous thrombosis”. We used the Boolean operator ‘NOT’ to exclude irrelevant to the focus of this review conditions, which were “cancer”, “oncological”, “tumour”, “cerebral”, “intracranial”, “heart”, “coronary”, “pulmonary”, “congenital” and “spinal”. The search queries (Boolean expressions) are presented in Figure 1.
Figure 1
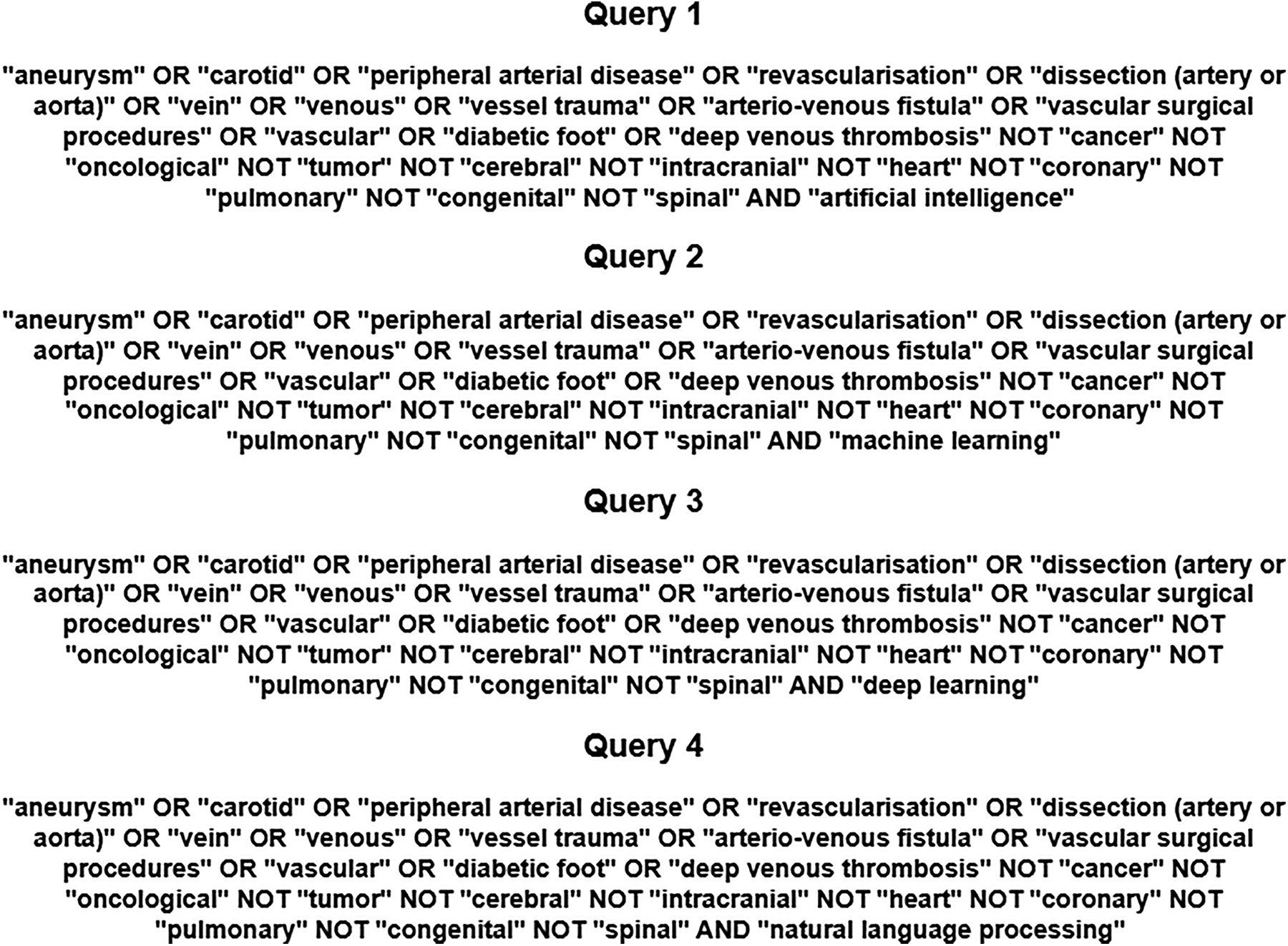
The search queries employed to screen the PUBMED, EMBASE and google scholar database.
Abstracts were reviewed independently by two authors (KP, KS), and any disagreement was resolved by arbitration (MJ, MW and GG). After identifying titles, full abstracts were reviewed and assessed for eligibility. All citations meeting the eligibility criteria were included in a second round of full-text article screening. Article selection, screening, and data extraction were completed by March 12, 2023. Data were tabulated, summarised, and gaps in AI utilisation in the healthcare system were identified.
Data analysis
Data that were extracted from the selected articles were stored in an Excel spreadsheet; this included: author, year of publication, journal, title, input data utilised for the AI algorithms development and their application in the vascular surgery.
We divided extracted articles into the following clinical subjects: aortic disease, carotid disease, peripheral arterial disease (PAD), diabetic foot syndrome (DFS), vascular access surgery, arterial trauma, and lower limb deep vein thrombosis.
The technologies covered by the umbrella term of AI were classified as machine learning (ML), deep learning (DL) and natural language processing (NLP).
The input data used to develop AI applications were categorised as:
- -
Image data [derived from computed tomography (CT), magnetic resonance (MR), Xray and ultrasound (US), thermograms, photographs, autofluorescence, microscopic analysis],
- -
Biological (peripheral blood sample, tissue samples),
- -
Genome database,
- -
Medical records (demographic data, medical background, radiology reports, medications, unstructured clinical text, discharge letters, surgical reports, socio-economic status, functional status, type of anaesthesia, medications, surveys results),
- -
Administrative records (procedure and admissions codes, physician claim codes, hospital volume, surgeon volume),
- -
Clinical parameters [blood results, heart rate, blood pressure, height and weight, BMI, intraoperative physiological measurements, wound characteristics, ankle-brachial pressure index (ABPI), transcutaneous oxygen pressure, haemodialysis parameters], and
- -
Devices data [tonometry, doppler sonograms, electrocardiogram (ECG), electromyogram (EMG), ground reaction force, photoplethysmography (PPG), phono-angiography, laser doppler flowmetry, spectrograms].
The intended application of AI-based technologies was classified into the following categories:
- -
Identification Detection Diagnosis,
- -
Prediction,
- -
Classification,
- -
Medical image segmentation, and
- -
Enhancement of understanding of pathophysiological mechanisms underlying vascular diseases.
We divided extracted articles into the following clinical themes: aortic disease, carotid disease, peripheral arterial disease (PAD), diabetic foot syndrome (DFS), vascular access surgery, arterial trauma, and lower limb deep vein thrombosis.
We summarised the literature in a narrative format for each domain of the vascular surgery focusing on the source of the input data and the intended application of the AI algorithms in the specific areas of the vascular surgery.
Statistical analysis
Statistical analyses were performed using SPSS (version 21, IBM, Chicago, IL, USA). Data were analysed using descriptive statistics. Results were expressed as counts and proportions/percentage as appropriate.
Results
We found 584 articles, out of which 342 papers met inclusion the criteria for our scoping review. The article selection is presented in the PRISMA flow diagram (Figure 2). Majority of articles were published after 2020. Articles considering aorta, carotid disease and peripheral arterial disease constituted most of analysed studies (79%).
Figure 2
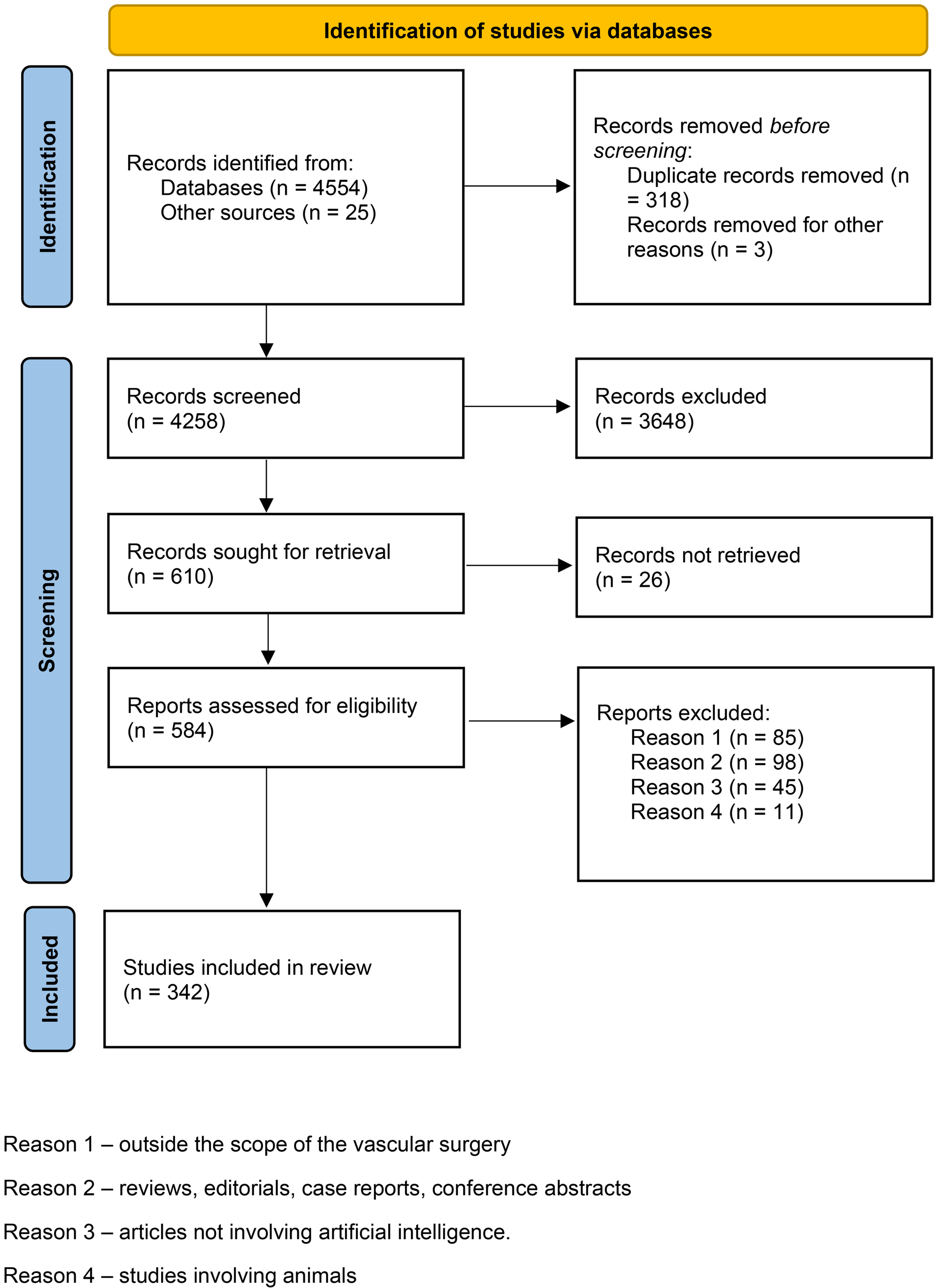
PRISMA diagram from initial literature search to final number of studies included in the analysis.
The most common data sources used for algorithm development were imaging (63.2% of studies), medical records (44.8%), and clinical parameters (24.8%). Biological databases (5.3%), genomic (1.7%) and administrative data (5.3%) were utilised the least (Figure 3). Distribution of AI-based technologies utilised across vascular conditions, based on description of population, intervention, comparison, and outcome criteria of 342 papers included in the review are provided in Table 1. Application of AI-based algorithms in different vascular conditions is depicted in Figure 4.
Figure 3
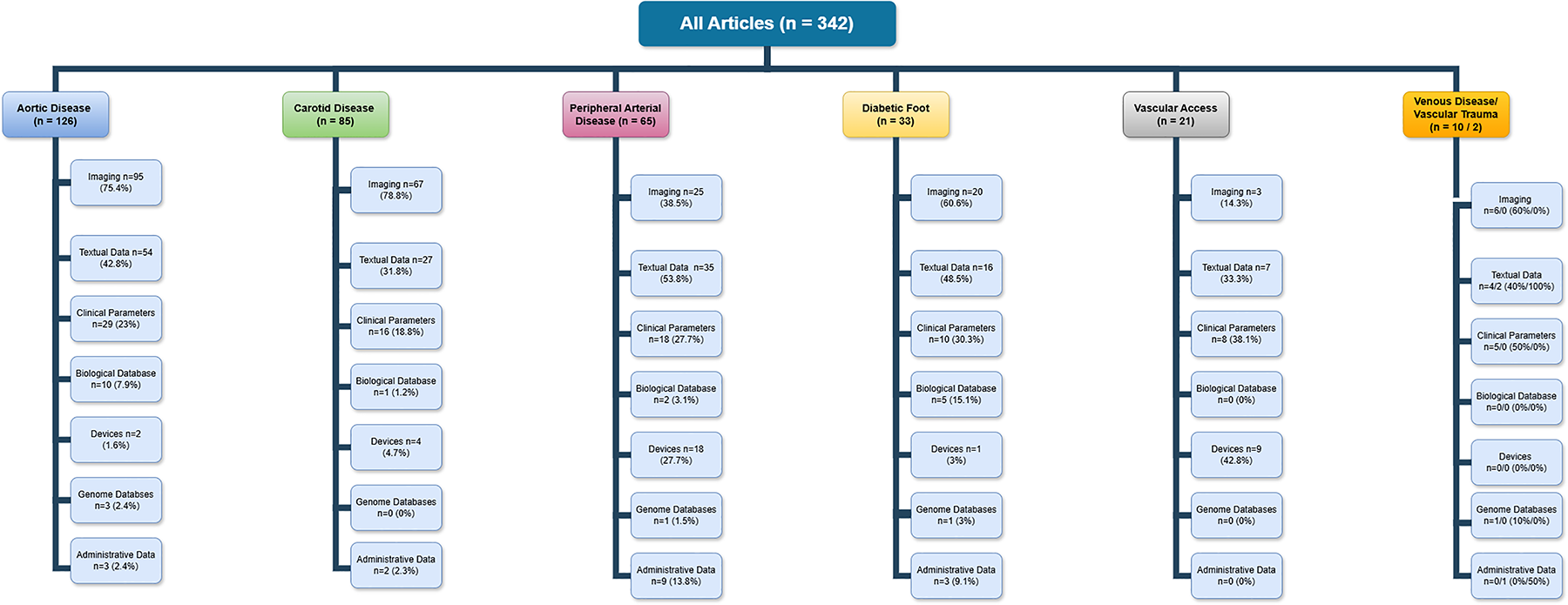
Input data for AI algorithms creation in vascular surgery.
Table 1
| PICO criteria | Articles, n (%) |
|---|---|
| Population | |
| Aortic disease | 126 (36.8%) |
| Carotid disease | 85 (24.8%) |
| Peripheral arterial disease | 65 (19%) |
| Diabetic foot syndrome | 33 (9.6%) |
| Vascular access surgery | 21 (6.1%) |
| Venous disease | 10 (2.9%) |
| Vascular trauma | 2 (0.6%) |
| Intervention | |
| Medical records | 153 (44.8%) |
| Imaging database | 216 (63.2%) |
| Clinical parameters | 85 (24.8%) |
| Biological database | 18 (5.3%) |
| Use of devices | 34 (9.9%) |
| Genome database | 6 (1.7%) |
| Administrative data | 18 (5.3%) |
| Comparison | |
| Machine learning vs. Deep learning | 42 (12.3%) |
| Outcome | |
| Identification/Detection/Diagnosis | 103 (30.1%) |
| Prediction | 123 (35.9%) |
| Medical image segmentation | 118 (34.5%) |
| Enhance understanding of pathophysiological processes | 18 (5.3%) |
| Classification | 49 (14.3%) |
Criteria based description of included articles.
Figure 4
Application of AI-based algorithms in vascular conditions.
Out of 342 articles, 126 (36.8%) were focused on aortic pathologies, 85 (24.8%) on carotid disease, 65 (19%) on peripheral arterial disease, 33 (6.1%) on diabetic foot syndrome, 21 (6.1%) on renal access surgery, 10 (2.9%) on lower limb venous disease and only 2 papers (0.6%) on vascular trauma.
Natural Language Processing technologies were employed in 34 studies (9.9%) utilising for development of the algorithm medical records (32 papers), administrative data (9), clinical data (5) and genomic database (2). NLP-based algorithms were mainly applied in research projects involving mainly peripheral arterial disease (15 studies; 44.1%).
Machine Learning algorithms were developed in 116 projects (33.9%) using as source of data medical records (65), imaging (51 papers), clinical data (49), medical device-derived data (15), biological information (11), administrative data (5) and genomic database (2). ML-based algorithms were mainly utilised in studies involving aortic pathologies (42 projects; 33.3%), carotid disease (24; 28.2%), and diabetic foot syndrome (16; 48.5%).
Deep Learning technologies were employed in 192 studies (56.2%) utilising as source of data imaging (157 papers), medical records (49), clinical data (30), medical device-derived data (18), biological data (7), administrative and genomic databases (3 and 2 studies, respectively). DL-based algorithms were predominantly applied in research projects focusing on aortic pathologies (76 studies; 60.3%), carotid disease (56; 66%), diabetic foot syndrome (16; 48.5%), and renal access surgery (9; 42.9%).
Majority of studies were published in technical peer-reviewed journals (230; 67.2%).
Discussion
We analysed 342 studies on application of AI technologies across different domains of the vascular surgery to assess the types of the data utilised in the development of AI-based algorithms. Most articles were published after 2020 and focused primarily on aortic pathology, carotid disease, and peripheral arterial disease; venous disease, vascular access, and vascular trauma constituted less than 10% of all studies. Despite an abundance of textual data which was used in over 50% of published projects, only one in ten papers described development of NLP algorithms, indicating its underutilisation.
Healthcare leaped forward in quality and complexity during the past two decades, characterised by an exponentially increasing use of information technology, and the vast amounts of data that information technology entails. It was estimated in 2020 that new information generated for every human being per second was around 1.7 megabytes (14). It has been shown that researchers often do not take full advantage of the diversity of data available in the EHR and frequently model development will only use a handful of variables pre-emptively identified by investigators. This limitation in data usage may unduly limit the accuracy of predictive models, especially where complex non-linear interactions are involved (5, 15). The textual data in medicine comprises a majority (80%) of information available for analysis (14). However, it is not effective in storing a quantifiable information. A well-designed NLP algorithm would be able to extract a large proportion of quantifiable data from a set of clinical notes without losing it context.
The volume of data and the velocity at which it is being generated exceeds the capabilities of traditional analytical tools. Novel analytical methods are dynamic and utilise advanced statistics, ML, DL, feedback, and NLP tools to mine through the data. These methods provide unparalleled capability in data exploration, analysis, and visualisation; they are robust and capable of seamlessly adapting models over time as new data comes in (14). Rapidly growing medical databanks that include clinical, genomic, imaging, and registries data, will only continue to increase. Thus, the future of medicine is likely to be even more data dependent, with the increasing convergence of medicine and AI technology (16).
The AI potential in healthcare has attracted significant attention from public and private sectors, amongst which Google Health has emerged as a major contributor to the development and deployment of AI-driven healthcare solutions, involving DL and NLP technologies (17). The growing demand for machines to handle complex language tasks, including translation, summarisation, information retrieval, and conversational interactions, has led to development of Large Language Models (LLMs; e.g., ChatGPT, MEDPalm 2) (18). They can be implemented in clinical, educational and research applications. However, since they still are lacking accuracy, they could be only deployed in assisting roles. Their adoption into medicine should be shaped by medical profession with careful clinical governance oversight pending further evaluation and fine tuning (19–21).
The increasing utilisation of telemedicine and telehealth technologies in cardiology in the last decade has shown efficiency and efficacy in the management of cardiovascular diseases risk factors such as obesity, vascular risk management and hypertension (22). The implementation of telemedicine in management of patients with chronic heart failure reduced short-term risk of cardiovascular-related hospitalisation and mortality in patients receiving combined remote disease monitoring and consultation (23). Digital health-based cardiac rehabilitation programs were shown to significantly reduce cardiovascular-related emergency department visits and unnecessary rehospitalization, however, further research is required to fully understand the clinical impact of digital health interventions (24). ML technologies, such as double machine learning (DML) have been utilised in target trial emulation (TTE), which is a powerful methodological bridge between traditional randomised control trials (RCTs) and observational studies. TTE applies the principles of RCTs to the observational studies in a structured approach. TTE, using DML to handle high-dimensional data, addresses RCTs limitations answering pressing clinical questions particularly in scenarios where conducting RCTs is impractical or ethically challenging (25).
Given the context of increasing attention to clinical NLP applications in recent years, we demonstrated that vascular surgery underutilises NLP (20). The narrative data from medical records, clinical parameters, biological and genomic databases were used in 280 (82%) articles, whereas image-based source was utilised in 216 (63%) papers. Despite abundance of narrative data NLP technologies were only utilised in 34 papers (9·9%), whereas ML- and DL-based algorithms were employed in 115 (33·6%), and 193 (56·4%) articles.
There are few reasons that could explain that low utilisation of NLP in vascular surgery. Firstly, vascular surgery is an image-driven specialty; most of decisions including diagnosis, planning of treatment and follow-up are based on various forms of imaging. Secondly, the importance of narrative data is not appreciated in the vascular community. Utilisation of NLP technologies require labelled data for supervised models, availability of annotators with clinical expertise, and appropriate computational environments. It is technically challenging to meet the hardware and software requirements within existing healthcare IT ecosystems. Additionally, access to patient-level data is controlled by complex information governance regulations, impeding development of efficient NLP algorithms (20). Despite increasing attention to clinical applications of NLP, the proportion of studies using text data in healthcare is low (20, 26, 27).
NLP holds immense promise in clinical research, with its potential ability to automatically identify cases for clinical studies and trials, drawing from sources like radiology reports. This is particularly important for rare diseases and studies where clinical diagnosis is entered in clinical notes in uncoded manner, and when the precision of diagnostic test is high, but pick up rate is low. Leveraging AI-driven NLP for participant screening using EHR could substantially reduce trials costs and expedite delivery (28, 29). This approach has been actively executed by pharmaceutical companies (30, 31).
Conclusions
Literature on AI-based technologies in vascular surgery is dominated by machine learning and deep learning that utilise primarily imaging and structured data. Although NLP holds immense promise, it is underutilised. It is likely that the primary reason for this underutilisation is a deficiency in understanding of this technology among clinicians and lack of adequate expertise. Close collaboration between clinicians and data scientists is mandatory to unlock and utilise NLP in the clinical and research fields.
Statements
Author contributions
KP: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing. KS: Data curation, Writing – review & editing. DB: Methodology, Writing – review & editing. MW: Writing – review & editing. GG: Writing – review & editing. MJ: Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. GVG acknowledges support from the NIHR Birmingham HPRU, NIHR Birmingham BRC, Nanocommons H2020-EU (731032), MAESTRIA (Grant agreement ID 965286), CRUCK (PRCNPG-Nov23/100001), HYPERMARKER (Grant agreement ID 101095480), PARC (Grant Agreement No 101057014), the MRC Heath Data Research UK (HDRUK/CFC/01) and the HDRUK midlands regional community project (HDRUK2023.0016), initiatives funded by UK Research and Innovation, Department of Health and Social Care (England) and the devolved administrations, and leading medical research charities. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research, the Medical Research Council or the Department of Health.
Acknowledgments
Thanks to HDRUK Midlands Regional Community Project [QQ2] Contract ID 2401346 that paid publication fee.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2025.1497822/full#supplementary-material
References
1.
Moor J . The dartmouth college artificial intelligence conference: the next fifty years. AI Mag. (2006) 27(4):87–91. 10.1609/aimag.v27i4.1911
2.
Samoli S Lopez Cobo M De Prato G Martinez-Plumed F Delipetrev B . AI watch—defining artificial intelligence: towards an operational definition and taxonomy of artificial intelligence. Joint Res Centre (Eur Commission). (2020):1–90. 10.2760/382730
3.
Lareyre F Lê CD Ballaith A Adam C Carrier M Amrani S et al Applications of artificial intelligence in non-cardiac vascular diseases: a bibliographic analysis. Angiology. (2022) 73(7):606–14. 10.1177/00033197211062280
4.
Hee Lee D Yoon SN . Application of artificial intelligence-based technologies in the healthcare industry: opportunities and challenges. Int J Environ Res Public Health. (2021) 18(1):1–18. 10.3390/ijerph18010271
5.
Flores AM Demsas F Leeper NJ Ross EG . Leveraging machine learning and artificial intelligence to improve peripheral artery disease detection, treatment, and outcomes. Circ Res. (2021) 128(12):1833–50. 10.1161/CIRCRESAHA.121.318224
6.
Ndwabe H Basu A Mohammed J . Post pandemic analysis on comprehensive utilization of telehealth and telemedicine. Clin EHealth. (2024) 7:5–14. 10.1016/j.ceh.2023.12.002
7.
Sharma K Patel Z Patel S Patel K Dabhi S Doshi J et al Repostioning of telemedicine in cardiovascular world post-COVID-19 pandemic. Front Cardiovasc Med. (2022) 9:1–5. 10.3389/fcvm.2022.910802
8.
Javidan AP Li A Lee MH Forbes TL Naji F . A systematic review and bibliometric analysis of applications of artificial intelligence and machine learning in vascular surgery. Ann Vasc Surg. (2022) 85:395–405. 10.1016/j.avsg.2022.03.019
9.
Sarker IH . Machine learning: algorithms, real-world applications and research directions. SN Comput Sci. (2021) 2(3):1–21. 10.1007/s42979-021-00592-x
10.
Yamashita R Nishio M Do RKG Togashi K . Convolutional neural networks: an overview and its applications in pattern recognition. Insights Imaging. (2018) 9:611–29. 10.1007/s13244-018-0639-9
11.
Vasilev I Slater D Spacagna G Roelants P Zocca V . Python Deep Learning. Birmingham: Packt Publishing Ltd (2019). p. 383.
12.
Linna N Kahn CE . Applications of natural language processing in radiology: a systematic review. Int J Med Inform. (2022) 163:104779. 10.1016/j.ijmedinf.2022.104779
13.
Wong A Plasek JM Montecalvo SP Zhou L . Natural language processing and its implications for the future of medication safety: a narrative review of recent advances and challenges. Pharmacotherapy. (2018) 38(8):822–41. 10.1002/phar.2151
14.
Ghavami P . Natural language processing. In: Big Data Analytics Methods. Berlin: De Gruyter (2019). p. 65–84.
15.
Ross EG Jung K Dudley JT Li L Leeper NJ Shah NH . Predicting future cardiovascular events in patients with peripheral artery disease using electronic health record data. Circ Cardiovasc Qual Outcomes. (2019) 12(3):1–20. 10.1161/CIRCOUTCOMES.118.004741
16.
Camara JR Tomihama RT Pop A Shedd MP Dobrowski BS Knox CJ et al Development of a convolutional neural network to detect abdominal aortic aneurysms. J Vasc Surg Cases, Innov Tech. (2022) 8(2):305–11. 10.1016/j.jvscit.2022.04.003
17.
George AS Hovan George AS Shahul A Baskar T . AI-driven breakthroughs in healthcare: google health’s advances and the future of medical AI. Partners Univ Int Innov J. (2023) 01(03):256–67. 10.5281/zenodo.8085221
18.
Naveed H Khan AU Qiu S Saqib M Anwar S Usman M et al A comprehensive overview of large language models. arXiv [Preprint]. arXiv: 2307.06435 (2023):1–35. 10.48550/arXiv.2307.06435
19.
Shah NH Entwistle D Pfeffer MA . Creation and adoption of large language models in medicine. JAMA. (2023) 330:866–9. 10.1001/jama.2023.14217
20.
Wu H Wang M Wu J Francis F Chang YH Shavick A et al A survey on clinical natural language processing in the United Kingdom from 2007 to 2022. npj Digit Med. (2022) 5(1):1–15. 10.1038/s41746-022-00730-6
21.
Thirunavukarasu AJ Ting DSJ Elangovan K Gutierrez L Tan TF Ting DSW . Large language models in medicine. Nat Med. (2023) 29(8):1930–40. 10.1038/s41591-023-02448-8
22.
Battineni G Sagaro GG Chintalapudi N Amenta F . The benefits of telemedicine in personalized prevention of cardiovascular diseases (CVD): a systematic review. J Pers Med. (2021) 11(7):1–12. 10.3390/jpm11070658
23.
Kuan PX Chan WK Fern Ying DK Rahman MAA Peariasamy KM Lai NM et al Efficacy of telemedicine for the management of cardiovascular disease: a systematic review and meta-analysis. Lancet Digit Heal. (2022) 4(9):e676–91. 10.1016/S2589-7500(22)00124-8
24.
Wongvibulsin S Habeos EE Huynh PP Xun H Shan R Porosnicu Rodriguez KA et al Digital health interventions for cardiac rehabilitation: systematic literature review. J Med Internet Res. (2021) 23(2):1–19. 10.2196/18773
25.
Yang J Wang L Chen L Zhou P Yang S Shen H et al A comprehensive step-by-step approach for the implementation of target trial emulation: evaluating fluid resuscitation strategies in post-laparoscopic septic shock as an example. Laparosc Endosc Robot Surg. (2025) 8(1):28–44. 10.1016/j.lers.2025.01.001
26.
Moazemi S Vahdati S Li J Kalkhoff S Castano LJV Dewitz B et al Artificial intelligence for clinical decision support for monitoring patients in cardiovascular ICUs: a systematic review. Front Med (Lausanne). (2023) 10:1007–15. 10.3389/fmed.2023.1109411
27.
Ford E Carroll JA Smith HE Scott D Cassell JA . Extracting information from the text of electronic medical records to improve case detection—a systematic review. J Am Inf Assoc. (2016) 23:1007–15. 10.1093/jamia/ocv180
28.
Wu K Wu E DAndrea M Chitale N Lim M Dabrowski M et al Machine learning prediction of clinical trial operational efficiency. AAPS J. (2022) 24(3):1–9. 10.1208/s12248-022-00703-3
29.
Askin S Burkhalter D Calado G El Dakrouni S . Artificial intelligence applied to clinical trials: opportunities and challenges. Health Technol (Berl). (2023) 13(2):203–13. 10.1007/s12553-023-00738-2
30.
Sahu A Mishra J Kushwaha N . Artificial intelligence (AI) in drugs and pharmaceuticals. Comb Chem High Throughput Screen. (2021) 25(11):1818–37. 10.2174/1386207325666211207153943
31.
Lamberti MJ Wilkinson M Donzanti BA Wohlhieter GE Parikh S Wilkins RG et al A study on the application and use of artificial intelligence to support drug development. Clin Ther. (2019) 41(8):1414–26. 10.1016/j.clinthera.2019.05.018
Summary
Keywords
natural language processing, artificial intelligence, source of data, vascular surgery, AI applications, identification, predictive modelling
Citation
Powezka K, Slater K, Brind D, Wall M, Gkoutos G and Juszczak M (2025) Data source and utilization of artificial intelligence technologies in vascular surgery—a scoping review. Front. Cardiovasc. Med. 12:1497822. doi: 10.3389/fcvm.2025.1497822
Received
17 September 2024
Accepted
05 March 2025
Published
07 May 2025
Volume
12 - 2025
Edited by
Robert Jeenchen Chen, Stanford University, United States
Reviewed by
Zhongheng Zhang, Sir Run Run Shaw Hospital, China
Nikolaos Patelis, Metropolitan General Hospital, Greece
Luminita Iliuta, Carol Davila University of Medicine and Pharmacy, Romania
Updates
Copyright
© 2025 Powezka, Slater, Brind, Wall, Gkoutos and Juszczak.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Katarzyna Powezka katarzyna.powezka1@nhs.net
†These authors share senior authorship
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.