Abstract
Introduction:
: There is a possibility of ischemia-reperfusion injury following percutaneous coronary intervention (PCI). Traditional Chinese medicine (TCM) treatment features multi-target and multi-link interventions, along with relatively good safety profiles, making it a promising option for alleviating ischemia-reperfusion injury following PCI.
Methods:
We searched the China National Knowledge Infrastructure (CNKI), VIP Journal Database, China Biomedical Literature Database, Wanfang Medical Database, PubMed, Web of Science, Embase, and Cochrane Library for randomized controlled trials published in Chinese and English regarding Chinese herbal injections for treating no-reflow or slow-reflow after PCI, from database inception to November 30, 2024.
Results:
A total of 14 interventions were evaluated, involving 5,535 patients. The interventions encompassed 14 types, including Shenfu Injection, Ginseng Injection, Shengmai Injection, Tanshinone IIA Sodium Sulfonate Injection, Danhong Injection, Danshen Injection, Shuxuetong Injection, Tanshinone Injection, Salvianolate Lyophilized Injection, Xuesaitong Injection, Salvia Ligustrazine Injection, Ixeris Sonchifolia Injection, Ginkgo Damo Injection, and standard treatment. The results indicated that the combination of salvianolate lyophilized injection with standard treatment might provide the best efficacy in improving no-reflow or slow blood flow after PCI. For enhancing Left Ventricular Ejection Fraction (LVEF) and reducing Left Ventricular End-Diastolic Dimension (LVEDD), the effect of Danshen Injection combined with standard Western medicine treatment was the most significant. Regarding reducing Left Ventricular End-Systolic Diameter (LVESD) and decreasing the incidence of Major Adverse Cardiovascular Events (MACE), Shenfu Injection showed possibly the most ideal effect. Meanwhile, Danhong Injection combined with standard treatment significantly improved the incidence of no-reflow compared to standard treatment, while also exhibiting positive effects on LVEF, reducing LVESD, and effectively decreasing the occurrence of MACE.
Conclusion:
Traditional Chinese Medicine (TCM) injections demonstrate significant efficacy and a favorable safety profile in treating no-reflow or slow blood flow after PCI in patients with acute coronary syndrome.
Systematic Review Registration:
https://www.crd.york.ac.uk/PROSPERO/view/CRD42024497449, PROSPERO CRD42024497449.
Introduction
Acute Coronary Syndrome (ACS) is a group of clinical syndromes resulting from acute myocardial ischemia. Based on clinical presentation, electrocardiographic changes, and elevated cardiac troponin levels, ACS is categorized into unstable angina (UA), non-ST-segment elevation myocardial infarction (NSTEMI), and ST-segment elevation myocardial infarction (STEMI) (1, 2).
Percutaneous coronary intervention (PCI) is a crucial therapeutic approach for ACS that significantly improves myocardial blood flow and reduces mortality. However, complications such as the no-reflow phenomenon (NRP) and coronary slow-flow phenomenon (CSFP) can occur post-PCI, potentially enlarging the myocardial infarction area and worsening prognosis, thus increasing mortality and the risk of recurrent myocardial infarction (3). The incidence of NRP in selective PCI for Acute Myocardial Infarction (AMI) ranges from 0.6% to 6.0%, while it is higher (10.0% to 50.0%) in emergency settings (4). This underscores the substantial risk of NRP in this population and highlights the critical need for timely intervention to improve clinical outcomes. From the perspective of Traditional Chinese Medicine (TCM), no-reflow or slow flow after PCI in ACS patients falls under the categories of “chest bi” (chest obstruction) and “true heart pain”. The condition is primarily attributed to Qi Deficiency and Blood Stasis, often accompanied by Yang Collapse. The therapeutic principles are therefore to Supplement Qi, Warm Yang, Activate Blood Circulation, and Resolve Stasis. Modern pharmacological research has demonstrated that TCM injections developed under these principles exhibit multi-target effects, including anti-inflammatory, antiplatelet, antithrombotic, and vascular endothelial protective properties (5). These mechanisms align with the pathological processes of no-reflow, such as microvascular obstruction and ischemia-reperfusion injury, thereby providing a solid theoretical and mechanistic basis for the application of TCM injections in this context and for the subsequent network meta-analysis evaluating their comparative efficacy.
Current management strategies focus on dilating coronary and microvascular systems (6) and inhibiting platelet activation and aggregation to enhance myocardial perfusion and mitigate ischemia-reperfusion injury (7). Despite advancements in NRP management, the incidence of adverse cardiovascular events remains high. TCM offers a multi-target therapeutic approach with a favorable safety profile, making it a potential treatment strategy for no-reflow or slow flow post-PCI (5).
This study conducts a network meta-analysis to evaluate the efficacy of various TCM injections in reducing the incidence of no-reflow or slow flow after PCI for ACS and their role in minimizing adverse effects, thereby providing evidence to inform clinical practice and optimize treatment strategies.
Materials and methods
Retrieval strategy
According to the PRISMA guidelines (8), we conducted a systematic review, meta-analysis, and network meta-analysis of clinical trials related to treatment strategies for the incidence of no-reflow after PCI in patients with acute coronary syndrome. This evaluation protocol had been registered on the PROSPERO platform, with registration number CRD42024497449.
We searched for randomized controlled trials (RCTs) published in Chinese and English from database inception until November 30, 2024, we utilized the following databases: China National Knowledge Infrastructure (CNKI), VIP Journal Database, China Biomedical Literature Database, and Wanfang Medical Database, as well as English databases such as PubMed, Web of Science, Embase, and the Cochrane Library. The Chinese search terms for diseases included “No-Reflow Phenomenon”, “Slow-Flow Phenomenon”, “Acute Myocardial Infarction”, “Acute Coronary Syndrome”, and “Percutaneous Coronary Intervention”, The search terms for traditional Chinese medicine injections included “Chinese Medicine Injection”, “Traditional Chinese Medicine Injection”, and “Danhong Injection”, Research types were specified using terms such as “Randomized Controlled Trial”, “Randomized Controlled Study”, “Randomized Controlled Experiment”, and “Randomized Control”, The English search terms included “Acute Coronary Syndrome”, “No-Reflow Phenomenon”, “Slow-Flow Phenomenon”, “No Reflow”, “Cardiovascular Stroke”, “Chinese medicine injection”, “Traditional Chinese medicine”, “TCM injection”, “randomized controlled trial”, “RCT”, and “controlled clinical trial”, among others. As an example for PubMed, the search strategy is presented in Table 1.
Table 1
| Procedure | Search query |
|---|---|
| #1 | Acute Coronary Syndrome[Mesh] OR myocardial infarction[Title/Abstract] OR Infarction, Myocardial[Title/Abstract] OR Heart Attack[Title/Abstract] OR Myocardial Infarct[Title/Abstract] OR Cardiovascular Stroke[Title/Abstract] ORCoronary Syndrome, Acute[Title/Abstract] OR Syndrome, Acute Coronary[Title/Abstract] OR No-Reflow Phenomenon[Title/Abstract] OR Slow-Flow Phenomenon[Title/Abstract] OR No Reflow[Title/Abstract] |
| #2 | Chinese medicine injection[Title/Abstract] OR Traditional Chinese medicine[Title/Abstract] OR TCM injection[Title/Abstract] OR Traditional Chinese medicine injection[Title/Abstract] OR chinese patent medicine injection[Title/Abstract] OR salvia ligustrazine injection[Title/Abstract] OR sheng mei injection[Title/Abstract] OR shenfu injection[Title/Abstract] OR blood plug tong injection[Title/Abstract] OR blood circulation injection[Title/Abstract] OR danhong injection[Title/Abstract] OR danshen injection[Title/Abstract] OR tanshinone injection[Title/Abstract] OR tanshinone iia sodium sulfonate injection[Title/Abstract] OR compound injection of red sage root[Title/Abstract] OR ixeris sonchifolia injection[Title/Abstract] OR pulse-activating injection[Title/Abstract] OR ginkgo leaf extract dipyridamole injection[Title/Abstract] OR salvia ligustrazine injection[Title/Abstract] |
| #3 | Randomized controlled trial[Title/Abstract] OR RCT[Title/Abstract] OR controlled clinical trial[Title/Abstract] OR randomized[Title/Abstract] OR randomly[Title/Abstract] OR trial[Title/Abstract] |
| #4 | #1 AND #2 AND #3 |
Pubmed retrieval strategy.
Selection criteria
Studies were included if they met the inclusion criteria: (1) Eligible patients were those with acute coronary syndrome undergoing PCI; (2) The control group received standard treatments (conventional medical therapy according to contemporary clinical guidelines, typically including dual antiplatelet therapy [aspirin plus a P2Y₁₂ inhibitor (clopidogrel or ticagrelor)], statins, beta-blockers, angiotensin-converting enzyme inhibitors [ACEI] or angiotensin receptor blockers [ARB], and other necessary medications) alongside PCI. The experimental group received TCM injection formulations in addition to standard care, excluding studies that involved other TCM forms; (3) Key outcomes included the incidence of no-reflow or slow-reflow (TIMI flow grade ≤ II), Left Ventricular Ejection Fraction (LVEF), Left Ventricular End-Diastolic Dimension (LVEDD), Left Ventricular End-Systolic Diameter (LVESD), and the occurrence of Major Adverse Cardiovascular Events (MACE). The exclusion criteria were as follows: (1) Studies with fewer than 20 subjects per group to minimize potential bias from underpowered small-sample studies; (2) Studies from which key outcome data could not be extracted or calculated; (3) Patients with comorbidities such as end-stage renal disease, malignancies, or hematologic disorders; (4) Studies with unclear or inconsistent definitions of no-reflow; (5) Duplicately published studies; (6) Reviews, case reports, personal experience summaries, and meta-analyses; (7) Non-randomized controlled trials; (8) Publications in languages other than Chinese or English.
Data extraction and risks of bias assessment
Quality of included studies was assessed using the Cochrane Risk of Bias 2.0 tool (RoB 2.0) (9). RoB 2.0 comprised five domains: bias arising from the randomization process, deviation from intended interventions, missing outcome data, measurement of outcomes, and selection of reported results. A comprehensive assessment was conducted after evaluating these five domains to determine the overall risk of bias, categorized as low, high, or unclear risk (10).
Data extraction was performed using a standardized form in Microsoft Excel. Extracted data included, but were not limited to: study characteristics (publication year, authors, journal name), participants (total sample size, age, and gender distribution), intervention details (interventions for experimental and control groups, route of administration, dosage, timing, and duration), outcome measures (definition, measurement methods, and units for each outcome), and results data (event counts and totals for binary variables, sample size, mean, and standard deviation for continuous variables). Two researchers independently completed the data extraction and cross-checked their findings; discrepancies were resolved by consensus or by consulting a third reviewer (J.Z.).
Statistical analysis
In this network meta-analysis, various software and methods were employed to ensure the accuracy and visual representation of results. Core statistical analyses were performed using the Stata 18 software network package (11), which operates under a frequentist framework. Key indicators were calculated, and several significant visualizations were generated. The evidence network diagram intuitively displayed the relationships between different interventions, where dots represented interventions and their sizes indicated the sample sizes included; connecting lines represented direct comparisons between two interventions, with line thickness reflecting the number of studies using both interventions. The forest plot clearly illustrated the effect sizes and 95% confidence intervals (CIs) for each intervention. The surface under the cumulative ranking curve (SUCRA) was used to present the ranking of interventions (12), providing strong support for clinical decision-making. The funnel plot assessed publication bias to ensure the reliability of analytical results (13). The rank probability plot was created using the ggplot2 and ggalluvial packages in R 4.3.1 to display the probabilities of different interventions at specific ranking positions. A macro-enabled Excel file “RoB2_IRPG_beta_v9” was utilized to draw the risk of bias bar chart.
For statistics, odds ratios (ORs) and their 95% CIs were used to present results for the binary variables of no-reflow incidence and MACE incidence. The ORs effectively measured the impact of interventions on event probability, while the 95% CI provided a credible range for assessing result stability. For continuous variables such as LVEF, LVEDD, and LVESD, mean differences (MDs) served as effect analysis statistics. The MD intuitively reflected the average differences among interventions for these continuous variables, facilitating quantitative evaluation and comparison of intervention effects.
Results
Characteristics and quality evaluationof the included studies
A preliminary search identified 4,372 publications. After removing duplicates, 1,254 articles were screened. Following a review of titles and abstracts, 717 articles were excluded, leaving 537 for full-text review, ultimately resulting in the inclusion of 49 RCTs (14–62). The analysis included 5,535 patients and evaluated 14 different interventions: Shenfu injection, Shenmai injection, Shengmai injection, Danshenketo II A sulfonate injection, Danhong injection, Danshen injection, Shuxuetong injection, Danshenketo injection, Danshen polyphenol salt injection, Xuesaitong injection, Danshen Chuanxiong injection, Kudiezi injection, Ginkgo biloba injection, and standard treatment. The literature screening process is illustrated in Figure 1, and the basic characteristics of the included studies are detailed in Table 2.
Figure 1
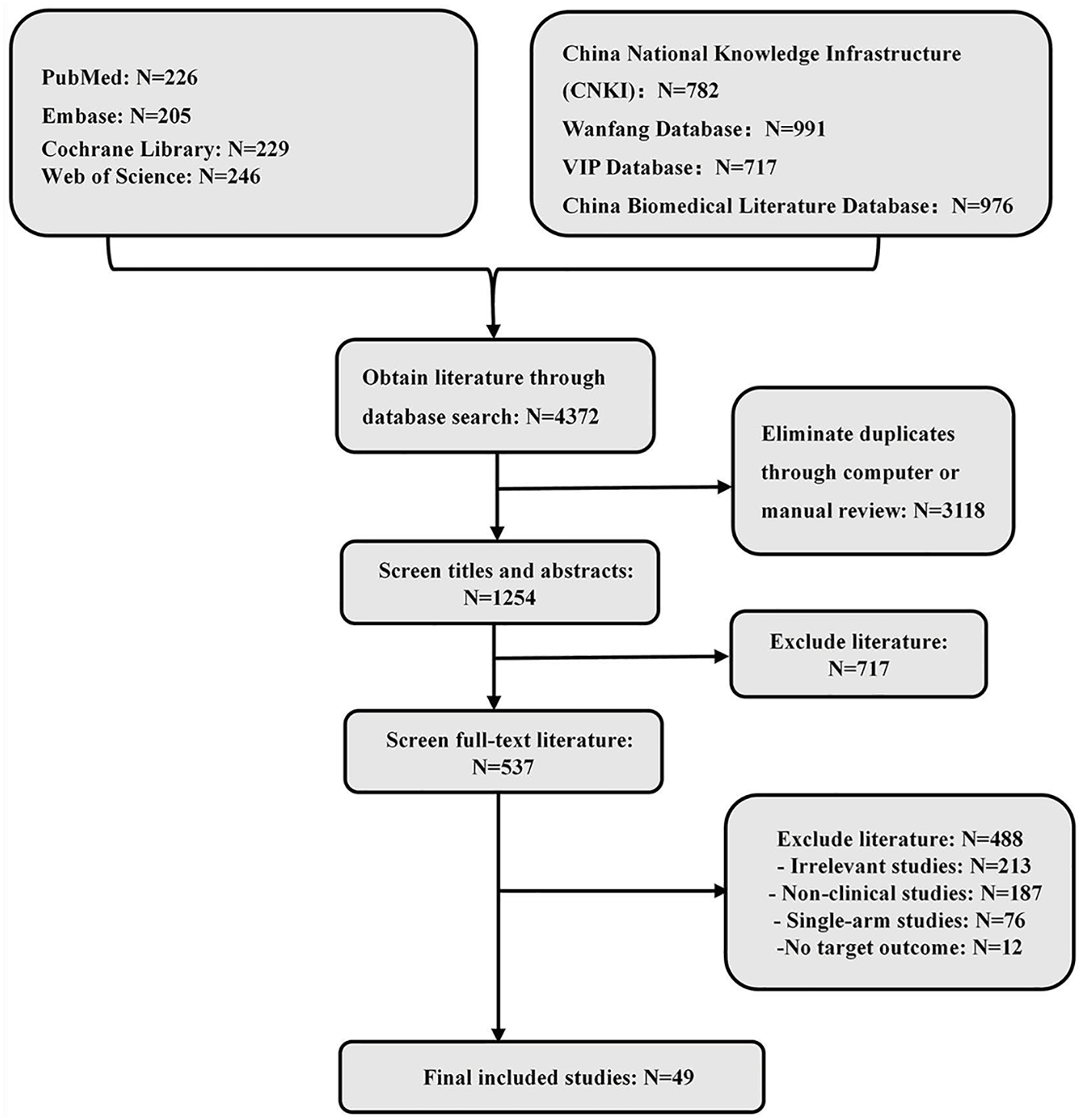
Literature screening flowchart.
Table 2
| Study (Author, Year https://www.ClinicalTrials.gov) | Sample size (male/female) | Mean age (Mean ± SD, year) | Intervention | Duration (day) | Outcomes | |||
|---|---|---|---|---|---|---|---|---|
| Teatment group | Control group | Teatment group | Control group | Teatment group (Drug dosage) | Control group | |||
| Xiao Wang 2024 NCT04493840 |
144 (121/23) | 151 (125/26) | 55.5 | 59.0 | Shenfu injection 80 ml |
Standard treatment | 5 days | ①② |
| Jiancheng Cao 2022 Not available |
41 (25/16) | 41 (22/19) | 52.75 ± 4.36 | 54.12 ± 3.19 | Ginseng injection 40 ml |
Standard treatment | 5 days | ①⑤ |
| Kai Xu 2022 Not available |
93 (52/41) | 93 (55/38) | 66.56 ± 3.35 | 66.69 ± 3.78 | Shengmai injection 60 ml |
Standard treatment | 7 days | ①②③④⑤ |
| Lu Yang 2021 Not available |
100 (58/42) | 100 (52/48) | 58.06 ± 4.84 | 58.13 ± 5.16 | Tanshinone IIA sodium sulfonate injection 80 mg |
Standard treatment | 7 days | ①③④⑤ |
| Qi Chen 2021 Not available |
46 (29/17) | 47 (27/20) | 62.9 ± 9.5 | 63.2 ± 8.5 | Danhong injection 40 ml |
Standard treatment | – | ①⑤ |
| Lina Hao 2021 Not available |
49 (22/27) | 48 (20/28) | 56.98 ± 4.02 | 57.47 ± 3.98 | Shenfu injection 40 ml |
Standard treatment | 7 days | ①⑤ |
| Xiuhua Zhu 2020 Not available |
70 (39/31) | 70 (43/27) | 65.07 ± 7.24 | 63.21 ± 6.63 | Shenfu injection 60 ml |
Standard treatment | 10 days | ①⑤ |
| Bin Huang 2020 Not available |
36 (24/12) | 36 (23/13) | 61.05 ± 3.64 | 62.74 ± 3.91 | Shengmai injection 60 ml |
Standard treatment | 7 days | ①②③④ |
| Donglang Chen 2020 Not available |
30 (17/13) | 30 (16/14) | 56.4 ± 5.2 | 56.8 ± 4.6 | Danshen injection 20mL |
Standard treatment | 7 days | ① |
| Mingyan Yao 2019 Not available |
47 (28/19) | 47 (30/17) | 67.47 ± 7.99 | 67.61 ± 8.07 | Shenfu injection 1 ml/kg |
Standard treatment | – | ① ⑤ |
| Qi You 2019 ChiCTR1800019451 |
57 (48/9) | 53 (47/6) | 56.8 ± 8.9 | 55.4 ± 9.5 | Danhong injection 40 ml |
Standard treatment | 7 days | ①⑤ |
| Jinghui Zhao 2019 Not available |
60 (43/26) | 60 (48/29) | 68 ± 5 | 65 ± 7 | Shuxuetong injection 8 ml |
Standard treatment | 7 days | ①②③④⑤ |
| Baixiang Yuan 2019 Not available |
60 (38/22) | 60 (41/19) | 60.2 ± 5.5 | 60.9 ± 5.0 | Danshen injection 30 ml |
Standard treatment | 3 days | ①②③④⑤ |
| Hongyan Ye 2019 Not available |
39 (23/16) | 39 (27/12) | 59.27 ± 8.11 | 59.22 ± 8.39 | Tanshinone injection 60 mg |
Standard treatment | 7 days | ①② |
| Qi You 2019 ChiCTR1800019451 |
62 (53/9) | 57 (50/7) | 58.1 ± 9.9 | 58.0 ± 9.7 | Danhong injection 40 ml |
Standard treatment | 7 days | ①⑤ |
| Yihui Zhang 2019 Not available |
100 (57/43) | 100 (59/41) | 62.45 ± 7.42 | 61.93 ± 7.74 | Shuxuetong injection 8 ml |
Standard treatment | 7 days | ①②③⑤ |
| Ying Zhang 2019 Not available |
102 (52/50) | 102 (50/52) | 56 ± 5.3 | 54 ± 6.3 | Tanshinone IIA sodium sulfonate injection 50 ml |
Standard treatment | 7 days | ①⑤ |
| Wenlu Chen 2018 Not available |
45 (26/19) | 45 (25/20) | 53.06 ± 1.29 | 52.11 ± 1.09 | Ginseng injection 40 ml |
Standard treatment | 5 days | ①⑤ |
| Hui Chang 2018 Not available |
55 (37/18) | 50 (31/19) | 61.38 ± 4.09 | 59.67 ± 5.02 | Danshen injection 20 ml |
Danshen polyphenolic acid salt | 3 days | ① |
| Xuan Wang 2018 Not available |
25 (20/5) | 25 (15/10) | 56.1 ± 5.3 | 55.8 ± 5.2 | Danshen injection 20 ml |
Standard treatment | 7 days | ①② |
| Li Qu 2018 Not available |
58 | 54 | – | – | Shenfu injection 60 ml |
Standard treatment | 10 days | ① |
| Hongmin Zhou 2018 Not available |
38 (25/13) | 38 (21/17) | 59.2 ± 5.4 | 58.7 ± 6.7 | Danhong injection 40 ml |
Standard treatment | 10 days | ①②⑤ |
| Lianren Wang 2018 Not available |
52 (31/21) | 52 (28/24) | 56.71 ± 6.25 | 57.29 ± 6.61 | Xuesaitong injection 8 ml |
Standard treatment | 14 days | ①②③ |
| Dongmei Zhang 2018 Not available |
60 (35/25) | 60 (33/27) | 62.97 ± 3.59 | 63.07 ± 3.60 | Shenfu injection 80 ml |
Standard treatment | – | ①⑤ |
| Shijing Na 2018 Not available |
40 (22/18) | 40 (24/16) | 62.9 ± 8.5 | 63.7 ± 9.0 | Shenfu injection 1 ml/kg |
Standard treatment | – | ①⑤ |
| Li qin 2018 Not available |
63 (29/34) | 63 (33/30) | 63.98 ± 1.25 | 63.41 ± 1.16 | Danhong injection 20 ml |
Standard treatment | 7 days | ①②③④⑤ |
| Lin Zhou 2017 Not available |
70 | 60 | 75 ± 9 | 74 ± 8 | Salvia ligustrazine injection 10 ml |
Standard treatment | 7 days | ①⑤ |
| Dongmei Zhang 2017 Not available |
40 (22/18) | 40 (25/15) | 61.6 ± 11.5 | 63.2 ± 11.2 | Shenfu injection 80 ml |
Standard treatment | – | ①⑤ |
| Jing Wu 2017 Not available |
44 | 36 | – | – | Danhong injection 20 ml |
Standard treatment | – | ① |
| Yujuan Wang 2017 Not available |
62 (35/27) | 62 (38/24) | 58.4 ± 9.6 | 57.6 ± 10.1 | Ixeris sonchifolia injection 40 ml |
Standard treatment | 14 days | ① |
| Wei Leng 2016 Not available |
120 (80/40) | 120 (77/43) | 56.9 ± 10.7 | 58.1 ± 11.2 | Danhong injection 20 ml |
Standard treatment | – | ① |
| Qiangfu Wu 2015 Not available |
40 | 40 | – | – | Shuxuetong injection 8 ml |
Standard treatment | 7 days | ①②③④⑤ |
| Junpeng Feng 2015 Not available |
34 (17/17) | 36 (18/18) | 62.5 ± 7.4 | 60.8 ± 10.0 | Xuesaitong injection 400 mg |
Standard treatment | 14 days | ① |
| Min Jia 2015 Not available |
60 (35/25) | 60 (40/20) | 62.23 ± 11.26 | 64.56 ± 12.85 | Danhong injection 20 ml |
Standard treatment | – | ① |
| Hanying Zhou 2015 Not available |
39 (27/12) | 40 (31/9) | 65 ± 11 | 62 ± 11 | Shuxuetong injection 8 ml |
Standard treatment | 7 days | ①②③④⑤ |
| Xiang Zhou 2014 Not available |
100 (71/29) | 100 (75/25) | 55.9 ± 1.48 | 56.0 ± 1.51 | Salvia ligustrazine injection 10 ml |
Standard treatment | – | ①⑤ |
| Sheng Guo 2014 Not available |
39 (26/13) | 39 | 55.6 ± 11.8 | – | Ginseng injection 50 ml |
Standard treatment | 7 days | ① |
| Xiaozheng Yang 2014 Not available |
30 (19/11) | 30 (17/13) | 57.77 ± 10.70 | 57.93 ± 10.37 | Ginseng injection 5 ml |
Standard treatment | 3 days | ①⑤ |
| Xiaozheng Yang 2014-2 Not available |
25 (17/8) | 25 (18/7) | 57.44 ± 11.09 | 59.40 ± 11.00 | Ginseng injection 30 ml |
Standard treatment | – | ①⑤ |
| Jing Wang, 2014 Not available |
138 (68/70) | 136 (66/70) | 59.32 ± 4.62 | 60.61 ± 4.61 | Salvia ligustrazine injection 40 ml |
Standard treatment | 14 days | ①⑤ |
| Xuguang Feng, 2013 Not available |
60 (32/28) | 36 (20/16) | 62.5 ± 10.1 | 61.6 ± 11.3 | Shuxuetong injection 6 ml |
Standard treatment | 14 days | ① |
| Baizhi Wang, 2013 Not available |
30 (23/7) | 30 (21/9) | 65.22 ± 7.54 | 63.61 ± 8.21 | Danhong injection 20 ml |
Standard treatment | – | ① |
| Rui Wang, 2011 Not available |
36 (27/12) | 37 (22/15) | – | – | Salvia ligustrazine injection 10 ml |
Standard treatment | 7–10 days | ① |
| Deqiang Zhao, 2010 Not available |
37 (29/8) | 37 (25/12) | 66.4 ± 10.4 | 66.2 ± 12.0 | Ginkgo damo injection 20 ml |
Standard treatment | 7 days | ①⑤ |
| Xuan Wang, 2010 Not available |
32 (19/13) | 30 (16/14) | 58.0 ± 14.9 | 54.9 ± 15.2 | shengmai injection 50 ml |
Standard treatment | 7 days | ①②③④ |
| Weiguo Shi, 2010 Not available |
55 | 51 | – | – | Danhong injection 40 ml |
Standard treatment | 10 days | ① |
| Xiaofei Wang, 2008 Not available |
30 (20/10) | 30 (24/6) | 54.0 ± 4.9 | 54.9 ± 5.2 | Shengmai injection 50 ml |
Standard treatment | 7 days | ①②③④ |
| Jinsong He, 2006 Not available |
68 (36/32) | 64 (30/34) | 61.18 ± 12.13 | 60.13 ± 11.15 | Shenfu injection 40 ml |
Standard treatment | 7 days | ① |
| Guohai Su, 2005 Not available |
47 (29/18) | 46 (30/16) | 61.8 ± 12.3 | 60.3 ± 11.5 | Shenfu injection 40 ml |
Standard treatment | 7 days | ① |
Baseline characteristics of the included studies.
Secondary endpoints: ① Incidence of no-reflow or slow-flow ② Left ventricular ejection fraction ③ Left ventricular end-diastolic internal diameter ④ Left ventricular end-systolic internal diameter ⑤ Incidence of major adverse cardiovascular events. Standard Treatment: dual antiplatelet therapy (aspirin plus a P2Y₁₂ inhibitor, either ticagrelor or clopidogrel), statins, beta-blockers, angiotensin-converting enzyme inhibitors (ACEI) or angiotensin receptor blockers (ARB), and other necessary medications per contemporary practice guidelines.
The risk of bias assessment for the 49 included studies revealed considerable variation in methodological quality. Of these, 41 studies explicitly employed random allocation methods, while the remaining 8 either allocated by treatment sequence or did not describe their allocation methods, resulting in a high risk rating for these studies in terms of randomization. Only 3 studies reported blinding of both participants and investigators, while the others did not mention the use of blinding. Additionally, 44 studies did not disclose whether outcome assessors were aware of the interventions received by the subjects, indicating potential risk. A more detailed presentation and analysis of the bias risk can be found in Figure 2.
Figure 2
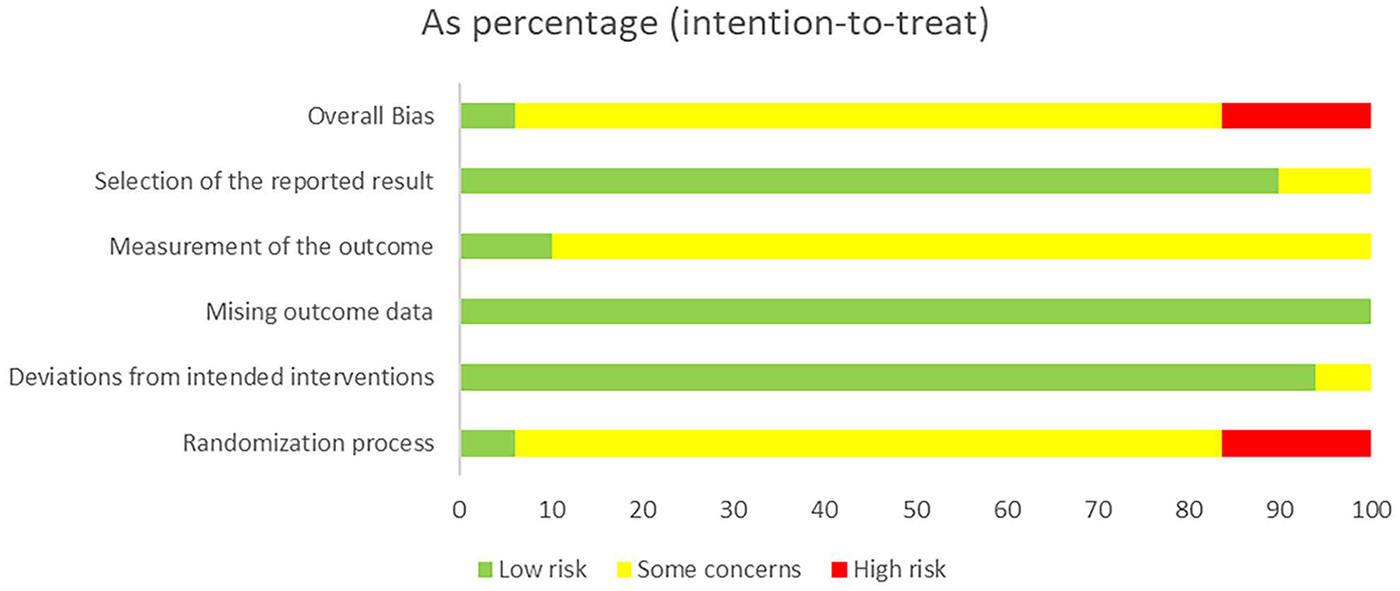
Risk of bias assessment.
Network meta-analysis in acute coronary syndrome with no-reflow or slow flow after PCI
A total of 49 studies evaluated the incidence of no-flow or slow flow, comparing 13 traditional Chinese medicine (TCM) injections (Shenfu, Ginseng, Shengmai, Tanshinone IIA, Danhong, Danshen, Shuxuetong, Tanshinone, Salvianolate, Xuesaitong, Salvia ligustrazine, Ixeris sonchifolia, and Ginkgo damo) with standard treatment. The evidence network is shown in Figure 3B. No closed loops were formed, eliminating the need for inconsistency testing. The results demonstrated that Salvianolate, Tanshinone, Danhong, Danshen, Ginseng, Shengmai, Xuesaitong, Shenfu, Tanshinone IIA, Shuxuetong, and Salvia ligustrazine significantly reduced the incidence of no-flow or slow flow compared to standard treatment, with odds ratios (ORs) ranging from 0.09 to 0.48. In contrast, Ginkgo damo and Ixeris sonchifolia showed no significant benefit (Figure 3A). Based on SUCRA rankings, Salvianolate was identified as the most effective TCM injection for reducing no-flow or slow flow incidence, followed by Tanshinone and Danhong. Standard treatment ranked the lowest in terms of efficacy (Figure 3C).
Figure 3
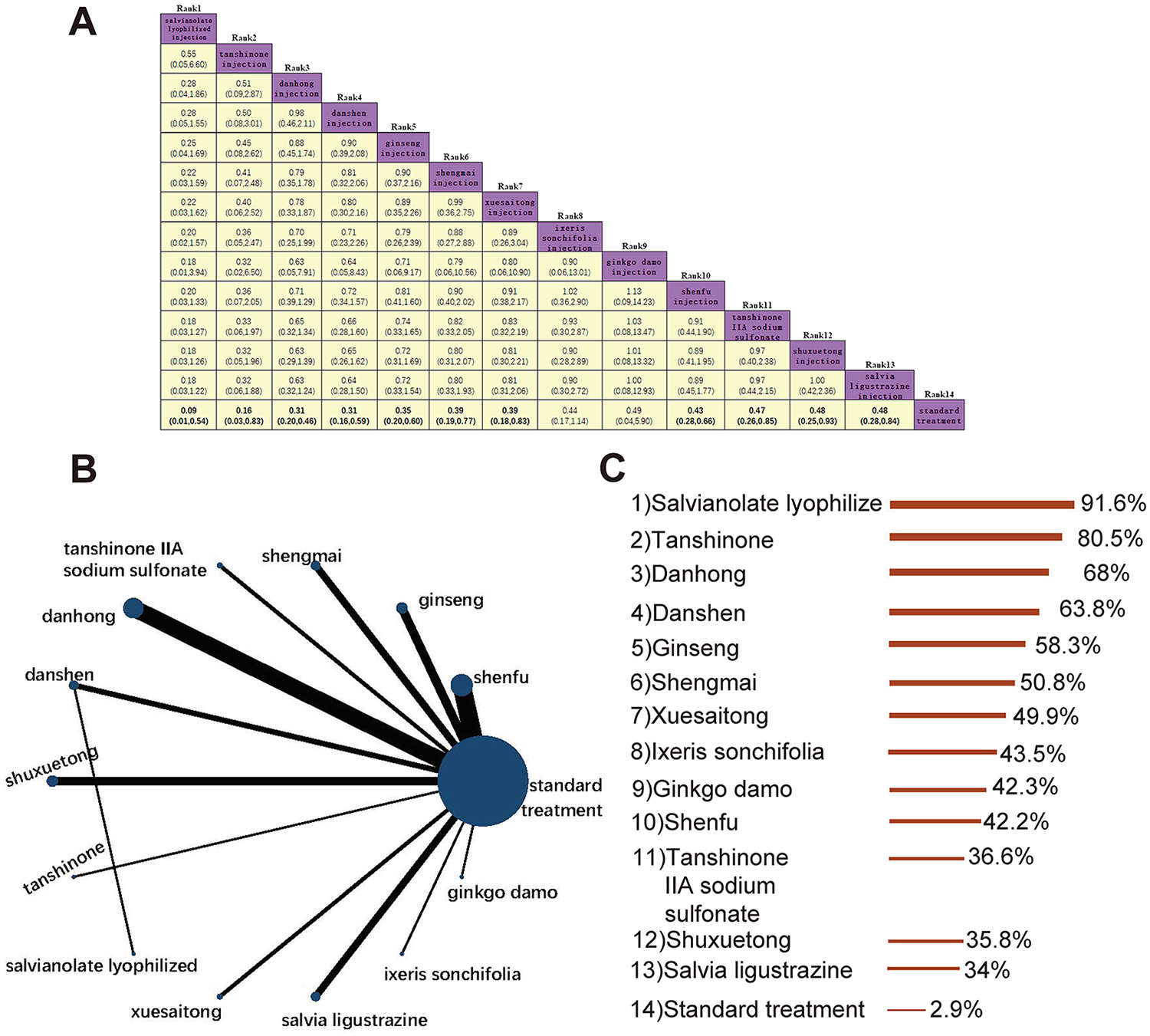
Incidence of no-flow or slow flow. (A) Pairwise comparisons of the incidence of no-reflow or slow flow. (B) Evidence network diagram of no-flow or slow flow incidence. (C) Treatment rankings (SUCRA).
A total of 15 studies evaluated LVEF outcomes, comparing standard treatment with Shenfu, Shengmai, Tanshinone IIA sodium sulfonate, Danhong, Danshen, Shuxuetong, and Xuesaitong injections (8 interventions in total). The evidence network is shown in Figure 4B. The results demonstrated that Danshen injection [MD = 8.40, 95% CI (4.03, 12.77)] and Danhong injection [MD = 6.95, 95% CI (1.72, 12.19)] significantly improved LVEF compared to standard treatment. Additionally, Danshen injection showed superior efficacy over Shuxuetong injection [MD = 6.46, 95% CI (0.52, 12.40)]. Other TCM injections did not exhibit significant advantages over standard treatment (Figure 4A). According to SUCRA rankings, Danshen injection was identified as the most effective intervention for improving LVEF, followed by Danhong injection and Tanshinone IIA sodium sulfonate injection. Standard treatment ranked the lowest in terms of efficacy (Figure 4C).
Figure 4
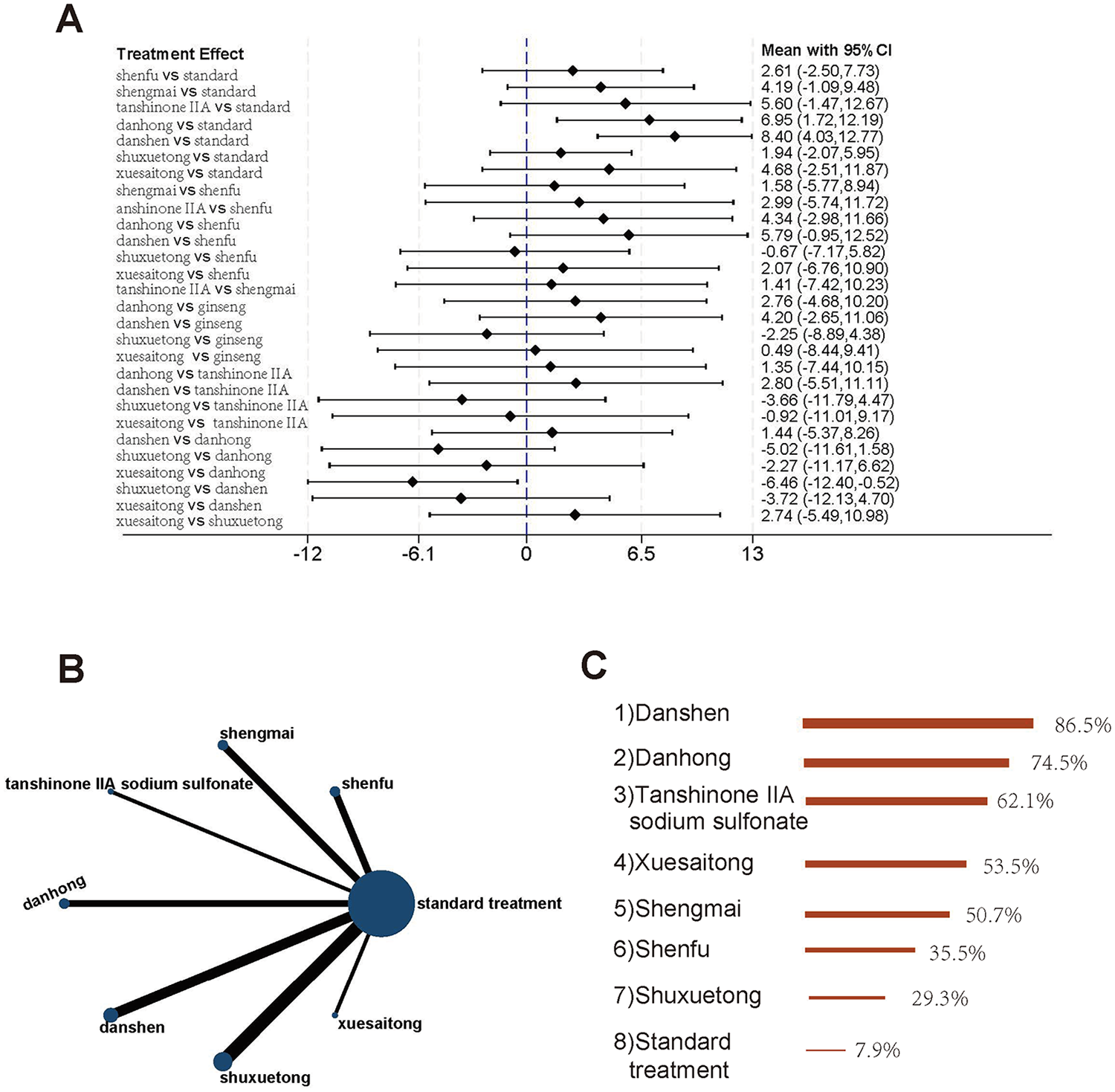
Studies involving LVEF (A) forest plot of pairwise comparisons for LVEF. (B) Evidence network diagram of LVEF. (C) Treatment rankings (SUCRA).
A total of 13 studies evaluated LVEDD outcomes, comparing standard treatment with Shenfu, Shengmai, Tanshinone IIA sodium sulfonate, Danhong, Danshen, Shuxuetong, and Xuesaitong injections (8 interventions in total). The evidence network is shown in Figure 5B. The analysis revealed that only Danshen injection [MD = −5.65, 95% CI (−9.58, −1.71)] combined with standard treatment significantly reduced LVEDD compared to standard treatment alone. Other TCM injections did not demonstrate a statistically significant advantage over standard treatment, and no notable differences were observed among the various TCM interventions (Figure 5A). According to SUCRA rankings, Danshen injection emerged as the most effective intervention for reducing LVEDD, followed by Shenfu injection and Danhong injection. Standard treatment ranked the lowest in terms of efficacy (Figure 5C).
Figure 5
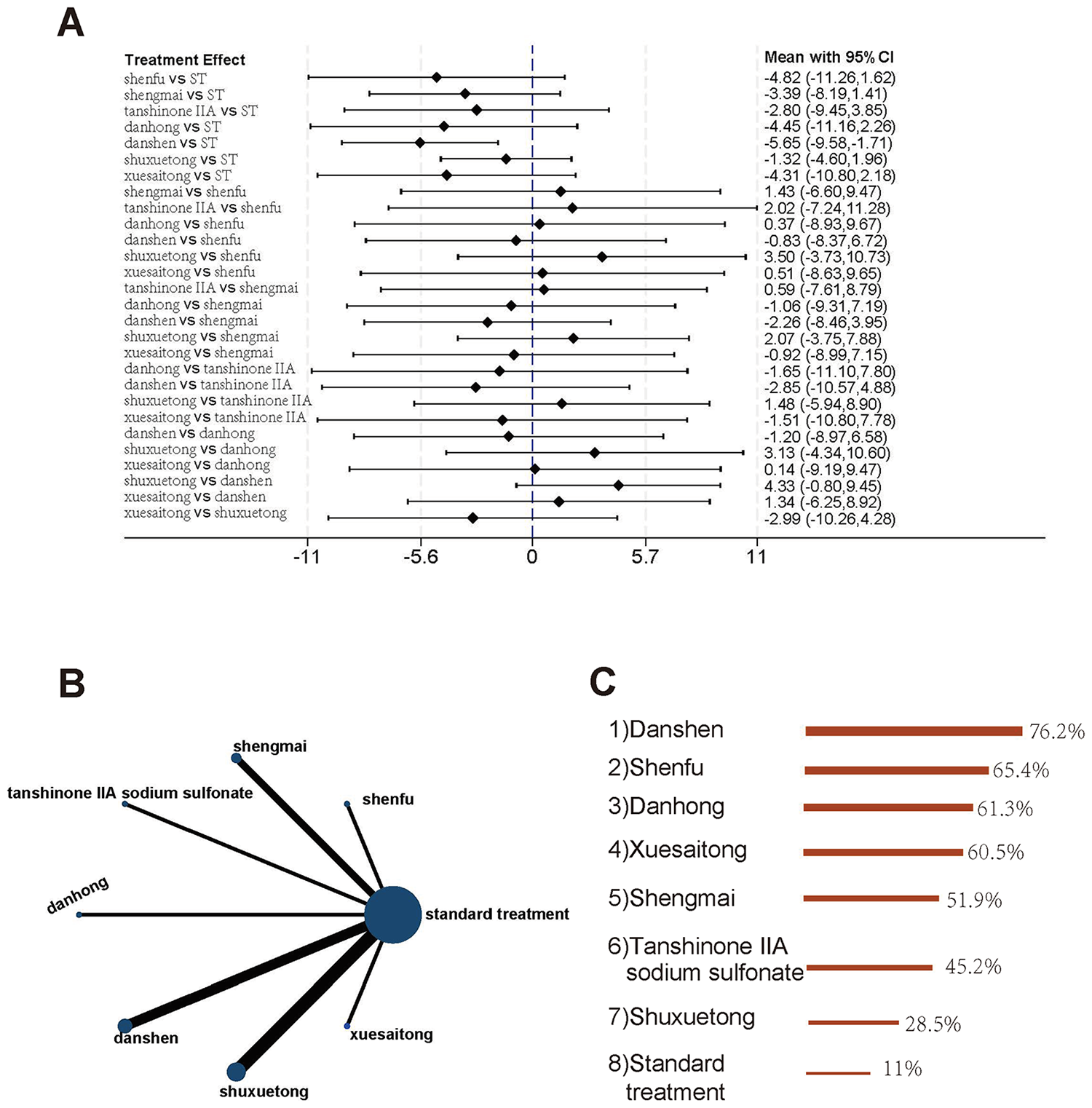
Studies involving LVEDD. (A) Forest plot of pairwise comparisons for LVEDD. (B) Evidence network diagram of LVEDD. (C) Treatment rankings (SUCRA).
A total of 11 studies involving 1,149 patients evaluated LVESD outcomes, comparing standard treatment with Shenfu, Shengmai, Tanshinone IIA sodium sulfonate, Danhong, Danshen, and Shuxuetong injections (7 interventions in total). The evidence network is shown in Figure 6B. The results demonstrated that Shenfu injection [MD = −5.37, 95% CI (−8.81, −1.93)], Danhong injection [MD = −4.38, 95% CI (−8.03, −0.73)], and Danshen injection [MD = −3.83, 95% CI (−6.13, −1.53)] significantly reduced LVESD compared to standard treatment. Furthermore, Shenfu injection [MD = −5.51, 95% CI (−9.75, −1.26)], Danhong injection [MD = −4.52, 95% CI (−8.93, −0.10)], and Danshen injection [MD = −3.97, 95% CI (−7.36, −0.57)] also showed superior efficacy over Shuxuetong injection, with statistically significant differences (Figure 6A). According to SUCRA rankings, Shenfu injection was identified as the most effective intervention for reducing LVESD, followed by Danhong injection and Danshen injection. Standard treatment ranked the lowest in terms of efficacy (Figure 6C).
Figure 6
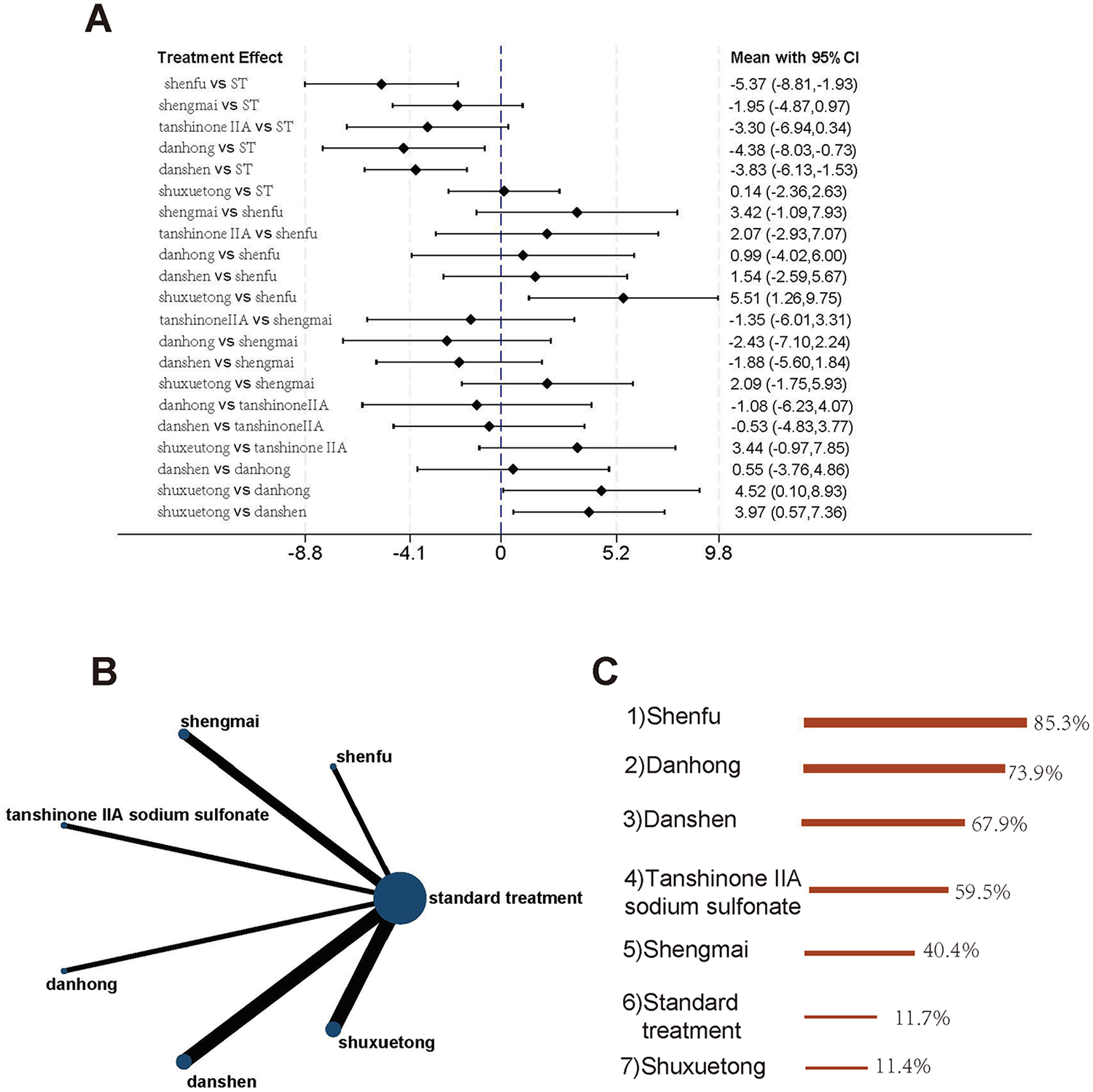
Studies involving LVESD (A) forest plot of pairwise comparisons for LVESD. (B) Evidence network diagram of LVESD. (C) Treatment rankings (SUCRA).
A total of 27 studies involving 3,368 participants evaluated MACE outcomes, comparing standard treatment with Shenfu, Ginseng, Shengmai, Tanshinone IIA sodium sulfonate, Danhong, Danshen, Shuxuetong, Tanshinone, Xuesaitong, Salvia ligustrazine, and Ginkgo damo injections (12 interventions in total). The evidence network is shown in Figure 7B. The results demonstrated that Shenfu injection [OR = 0.23, 95% CI (0.13, 0.43)], Tanshinone injection [OR = 0.21, 95% CI (0.07, 0.62)], Tanshinone IIA sodium sulfonate injection [OR = 0.27, 95% CI (0.16, 0.45)], Ginseng injection [OR = 0.33, 95% CI (0.18, 0.61)], Shuxuetong injection [OR = 0.35, 95% CI (0.19, 0.64)], and Danhong injection [OR = 0.36, 95% CI (0.20, 0.66)] significantly reduced the incidence of MACE compared to standard treatment. Additionally, these injections also showed superior efficacy over Salvia ligustrazine injection and Shengmai injection (Figure 7A). According to SUCRA rankings, Shenfu injection was identified as the most effective intervention for reducing MACE incidence, followed by Tanshinone injection and Danshen injection. Standard treatment ranked the lowest in terms of efficacy (Figure 7C).
Figure 7
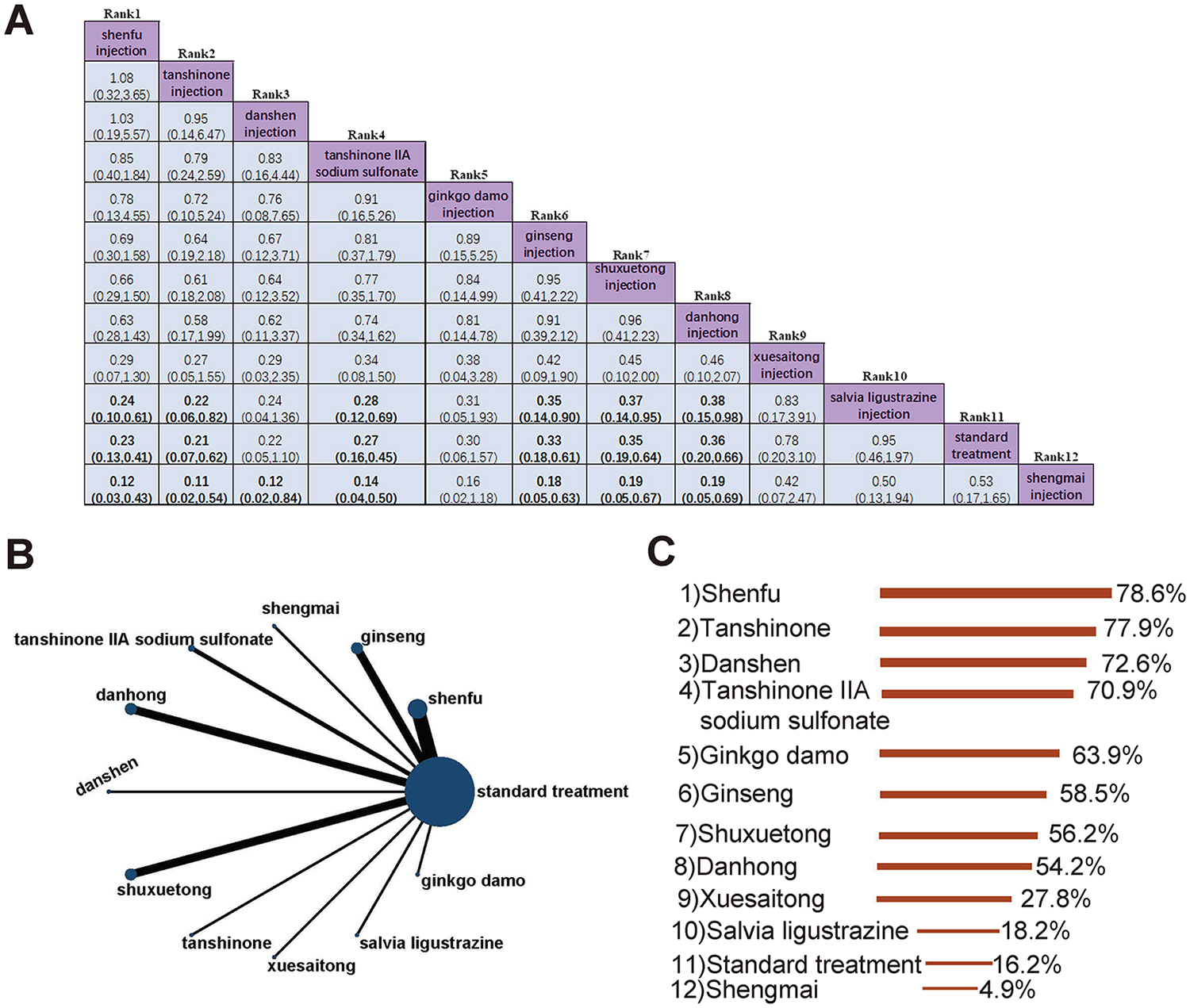
The incidence of MACE. (A) Pairwise comparisons of the incidence of MACE. (B) Evidence network diagram of MACE. (C) Treatment rankings (SUCRA).
In summary, by synthesizing the findings across all efficacy and safety endpoints, distinct profiles for the TCM injections emerge. Interventions such as Danhong Injection, Shenfu Injection, and Danshen Injection consistently demonstrated broad efficacy, appearing in the top ranks for multiple critical outcomes including no-reflow incidence, cardiac function (LVEF, LVESD), and MACE reduction. These can be considered “all-rounders” offering comprehensive benefits. In contrast, other injections showed more specialized effects; for instance, Salvianolate Lyophilized Injection was ranked highest specifically for preventing no-reflow, while Tanshinone Injection was particularly effective for MACE reduction. This synthesis provides clinicians with a practical hierarchy: for broad-spectrum improvement, Danhong, Shenfu, or Danshen are prominent choices, whereas for targeting a specific predominant concern like no-reflow, Salvianolate may be the optimal specialist agent.
Publication bias
In this study, five outcome indicators were set, with each indicator including more than 10 studies. By analyzing these data through funnel plots, we observed the distribution of the effect sizes on both sides of each study. The funnel plots of the outcomes can be seen in Figure 8. Specifically, in Figure 8E, all study points are neatly contained within the 95% confidence interval, with no points falling outside this range. Figures 8A,D show a similar situation, with only one point lying outside the 95% confidence interval. This indicates low heterogeneity among the studies assessing the outcomes of no-reflow, LVESD, and MACE. In other words, these studies yielded consistent results when evaluating the above outcome indicators, and there was little difference between them, which is beneficial for comprehensive analysis and interpretation of these indicators.
Figure 8
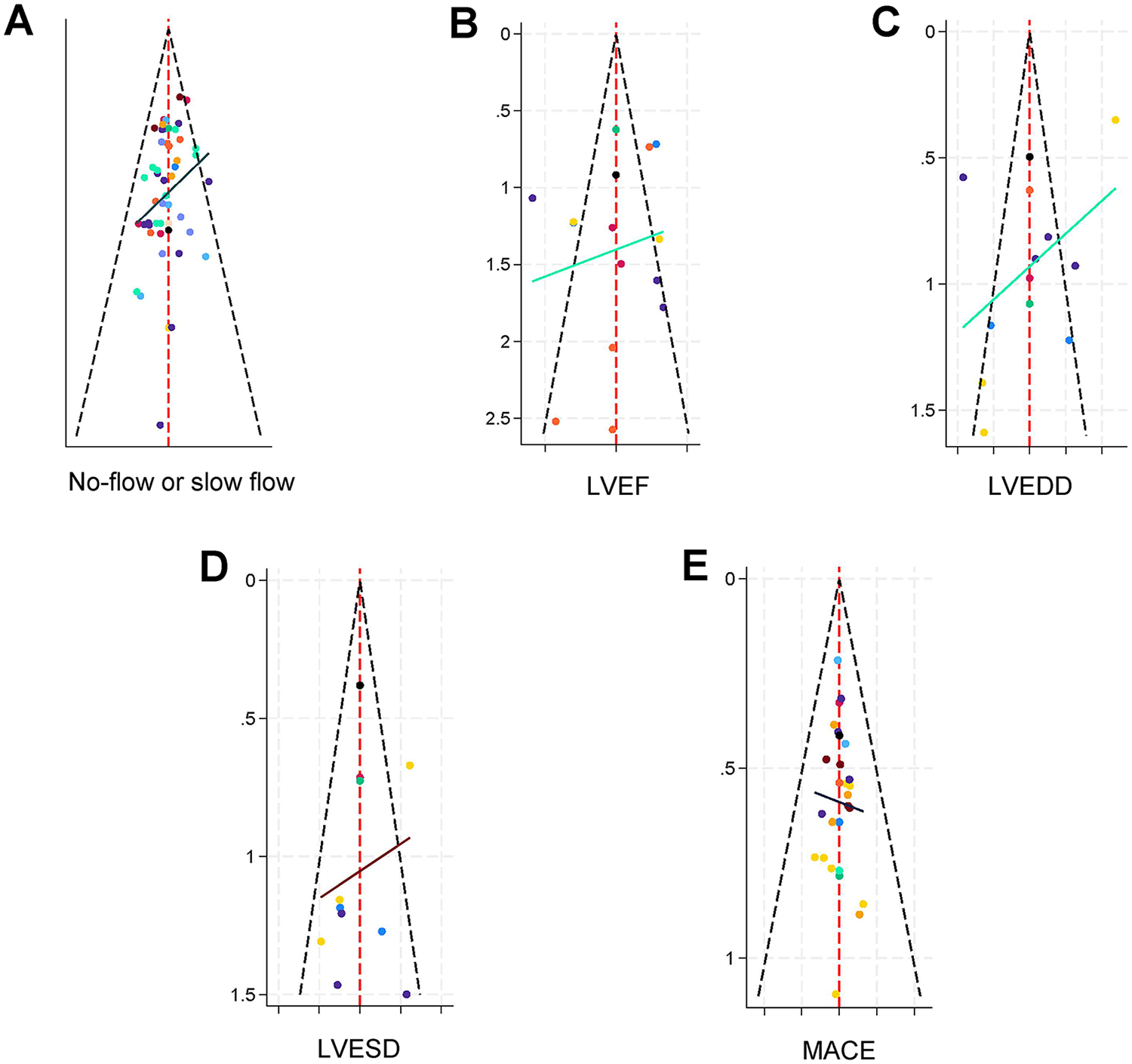
Funnel Plots for the Five Outcome Indicators. (A) No-reflow incidence. (B) Left ventricular ejection fraction (LVEF). (C) Left ventricular end-diastolic diameter (LVEDD). (D) Left ventricular end-systolic diameter (LVESD). (E) Major adverse cardiovascular events (MACE). Plots A, D, and E, with all or most data points within the 95% confidence intervals, indicate low heterogeneity. In contrast, plots B (LVEF) and C (LVEDD), showing a greater number of points outside the confidence intervals, suggest significant heterogeneity among the included studies).
However, Figures 8B,C show a different scenario. In these two funnel plots, a relatively larger number of study points fall outside the 95% confidence interval. This suggests that there is significant heterogeneity among the studies with LVEF and LVEDD as outcome indicators. In other words, different studies yielded markedly different results when assessing LVEF and LVEDD. This larger heterogeneity may be due to various factors, such as differences in the study populations included, the measurement methods used, and the specific implementation details of the interventions. These variations could lead to a greater degree of dispersion in the results for the LVEF and LVEDD indicators, increasing the difficulty of conducting a comprehensive analysis and interpretation of the findings related to these indicators.
Discussion
This network meta-analysis comprehensively evaluated the efficacy and safety of 13 TCM injections for ACS patients with no-reflow or slow flow after PCI. The most significant finding is that TCM injections, as adjuncts to standard therapy, are broadly effective, but they can be categorized into distinct efficacy profiles. Specifically, interventions like Danhong Injection, Shenfu Injection, and Danshen Injection emerged as consistent top performers across multiple endpoints, while others, such as Salvianolate Lyophilized Injection, demonstrated highly specific efficacy. This synthesis provides a practical, evidence-based hierarchy to guide clinical selection, moving beyond a one-size-fits-all approach.
A key insight from our analysis is the distinction between “all-rounder” and “specialist” interventions. Danhong Injection exemplified the “all-rounder” profile, showing significant benefits for improving no-reflow incidence, LVEF, LVESD, and reducing MACE. Similarly, Shenfu Injection ranked best for reducing LVESD and MACE, and Danshen Injection for improving LVEF and LVEDD, indicating their broad-spectrum cardioprotective effects. In contrast, Salvianolate Lyophilized Injection served as a “specialist”, ranking highest specifically for preventing the no-reflow phenomenon itself. This pattern suggests that the choice of TCM injection can be tailored to the patient's most pressing clinical need.
The clinical context of no-reflow phenomenon warrants emphasis. No-reflow or slow flow following PCI in ACS patients refers to impaired myocardial perfusion after successful revascularization, significantly increasing the risk of major cardiovascular events and mortality (3, 4). Current management strategies include vasodilators like nicorandil (63), antiplatelet agents such as ticagrelor (64), calcium channel blockers (e.g., verapamil (65), glycoprotein IIb/IIIa inhibitors like tirofiban (66), and non-pharmacological approaches including thrombus aspiration (67) and delayed stenting (68). Despite these available treatments, there remains substantial need for more effective interventions to address postoperative cardiac recovery limitations.
The distinct efficacy profiles observed in our analysis are supported by established pharmacological mechanisms. Danhong Injection's multi-target effects are attributed to its active components including danshenone, salvianolic acid, and hydroxy safflower yellow A, which collectively provide antioxidant, anti-inflammatory, antiplatelet aggregation, and anti-apoptotic benefits (69, 70). Shenfu Injection mediates mitochondrial autophagy to protect against ischemia-reperfusion injury through the HIF-1α/BNIP3 pathway (71), while Danshen Injection's tanshinones and salvianolic acids contribute to its anticoagulation, anti-inflammatory, and antioxidant properties (72). Salvianolate Lyophilized Injection exerts its specialized effects through potent microcirculation improvement and vascular endothelial protection (73, 74), directly addressing the core pathophysiology of no-reflow.
Our findings should be interpreted considering several limitations. First, the overall high risk of bias in many included studies, particularly concerning blinding, may have led to an overestimation of the treatment effects (9, 10). Second, the considerable heterogeneity observed in some outcomes (e.g., LVEF and LVEDD) likely stems from variations in patient demographics, PCI procedures, and TCM injection dosages, reducing the precision of these estimates. Third, the notable disparity in sample sizes across interventions means that rankings for less-studied injections (e.g., Salvianolate) should be considered exploratory, whereas those for extensively studied ones (e.g., Danhong) are more robust. Fourth, the lack of TCM syndrome differentiation in included studies limits our understanding of whether certain injections are more effective for specific patient subtypes. Finally, all participants were Chinese, potentially affecting the generalizability of our findings to other populations.
Notwithstanding these limitations, our study provides crucial evidence for personalizing TCM injection selection. For clinicians seeking comprehensive protection, Danhong Injection represents the most versatile choice. When targeting specific pathophysiological processes, Salvianolate Lyophilized Injection may be optimal for no-reflow prevention, Shenfu Injection for managing ventricular remodeling and MACE, and Danshen Injection for enhancing cardiac systolic function. Future research should prioritize large-scale, double-blind RCTs that directly compare these promising injections, incorporate TCM syndrome differentiation, explore potential synergistic combinations, and validate these findings in diverse ethnic populations.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
TC: Data curation, Methodology, Conceptualization, Writing – original draft, Formal analysis. WL: Writing – original draft, Data curation, Conceptualization, Methodology, Formal analysis. WX: Methodology, Writing – original draft, Data curation, Formal analysis. CL: Writing – review & editing, Data curation, Formal analysis. LL: Writing – review & editing, Data curation. DW: Data curation, Writing – review & editing. JZ: Conceptualization, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declared that financial support was received for this work and/or its publication. Guangxi Natural Science Foundation. Grant No. 2023GXNSFDA026029.
Acknowledgments
We sincerely acknowledge all the researchers and clinical trial investigators whose work contributed to the original studies included in this systematic review.
Conflict of interest
The author(s) declared that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declared that generative AI was used in the creation of this manuscript. Polish the manuscript language.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2025.1619345/full#supplementary-material
References
1.
Byrne RA Rossello X Coughlan JJ Barbato E Berry C Chieffo A et al 2023 ESC guidelines for the management of acute coronary syndromes. Eur Heart J (2023) 44(38):3720–826. 10.1093/eurheartj/ehad191
2.
Bergmark BA Mathenge N Merlini PA Lawrence-Wright MB Giugliano RP . Acute coronary syndromes. Lancet. (2022) 399(10332):1347–58. 10.1016/S0140-6736(21)02391-6
3.
Konijnenberg LSF Damman P Duncker DJ Kloner RA Nijveldt R van Geuns RM et al Pathophysiology and diagnosis of coronary microvascular dysfunction in ST-elevation myocardial infarction. Cardiovasc Res. (2020) 116(4):787–805. 10.1093/cvr/cvz301
4.
Zhao Q Zhao G . Research progress on predictors and prevention strategies for no-reflow phenomenon in patients with acute myocardial infarction undergoing percutaneous coronary intervention. Practical J Cardiac Cereb Pneumal Vasc Dis. (2019) 27(7):1–4.
5.
Yu Y Yang BP . Sodium nitroprusside injection immediately before balloon inflation during percutaneous coronary intervention. World J Clin Cases. (2021) 9(36):11248–54. 10.12998/wjcc.v9.i36.11248
6.
Zhou SS Tian F Chen YD Wang J Sun ZJ Guo J et al Combination therapy reduces the incidence of no-reflow after primary per-cutaneous coronary intervention in patients with ST-segment elevation acute myocardial infarction. J Geriatr Cardiol. (2015) 12(2):135–42. 10.11909/j.issn.1671-5411.2015.02.003
7.
Luo W Lu J Zhou J Yang M . Research progress in the prevention and treatment of coronary no-reflow after PCI with traditional Chinese medicine. Liaoning J Tradit Chin Med. (2023) 25(2):102–9. 10.13194/j.issn.1673-842x.2023.02.021
8.
Hutton B Salanti G Caldwell DM Chaimani A Schmid CH Cameron C et al The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. (2015) 162(11):777–84. 10.7326/M14-2385
9.
Sterne JAC Savović J Page MJ Elbers RG Blencowe NS Boutron I et al Rob 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. 10.1136/bmj.l4898
10.
Liu J Liu C Hua C . Interpretation of the revised tool for risk of bias in randomized trials (RoB2, 2019 version). Chin J Evidence Based Med. (2021) 21(6):737–44.
11.
Shim S Yoon BH Shin IS Bae JM . Network meta-analysis: application and practice using stata. Epidemiol Health. (2017) 39:e2017047. 10.4178/epih.e2017047
12.
Wang Z Carter RE . Ranking of the most effective treatments for cardiovascular disease using SUCRA: is it as sweet as it appears?Eur J Prev Cardiol. (2018) 25(8):842–3. 10.1177/2047487318767199
13.
Sterne JA Egger M . Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. (2001) 54(10):1046–55. 10.1016/s0895-4356(01)00377-8
14.
Wang X Guo R Guo Y Guo Q Yan Y Gong W et al Rationale and design of the RESTORE trial: a multicenter, randomized, double-blinded, parallel-group, placebo-controlled trial to evaluate the effect of shenfu injection on myocardial injury in STEMI patients after primary PCI. Am Heart J. (2023) 260:9–17. 10.1016/j.ahj.2023.02.005
15.
Xu K . Clinical Observation of Shengmai Injection in Acute Myocardial Infarction Patients After Emergency PCI. [Master’s thesis] Qingdao University (2022). 10.27262/d.cnki.gqdau.2022.002746
16.
Cao J Guo L Sun Q . Therapeutic effect of shenmai injection combined with western medicine on no-reflow after PCI in patients with acute myocardial infarction and its influence on myocardial injury and oxidative stress. J Chin Med. (2022) 54(15):48–52.
17.
Hao L Pei G Li Y . Effects of shenfu injection on TIMI blood flow grading and fibrinolysis indexes in patients with acute myocardial infarction undergoing PCI. Chin J Convalesc Med. (2021) 30(4):429–31. 10.13517/j.cnki.ccm.2021.04.035
18.
Chen Q Lin Z Ma T Liu Z . Efficacy of loading dose ticagrelor combined with danhong injection in preventing reperfusion arrhythmia after PCI in patients with acute anterior wall STEMI and its effect on myocardial injury markers. Modern J Integr Tradit Chinese West Med. (2021) 30(23):2555–60.
19.
Lu Y Yan Y Liu X . Effects of alprostadil combined with tanshinone IIa injection on microcirculation disorder, outcomes, and cardiac function in AMI patients after PCI. Ann Palliat Med. (2021) 10(1):97–103. 10.21037/apm-20-2147
20.
Zhu X Ye H Yang L . Effects of shenfu injection on myocardial TIMI flow grade during PCI and short-term major adverse cardiac events after surgery in patients with acute myocardial infarction. Chin J Integr Med Cardio Cerebrovasc Dis. (2020) 18(13):2107–11.
21.
Huang B Lu M . Effects of shengmai injection on cardiac autonomic nerve function and myocardial microcirculation in patients with three-vessel coronary artery disease after emergency PCI. Liaoning J Tradit Chin Med. (2020) 47(1):120–3. 10.13192/j.issn.1000-1719.2020.01.040
22.
Chen D Zou P Lu Y . Application effect of compound danshen injection in patients with acute ST-segment elevation myocardial infarction undergoing PCI. China Mod Med. (2020) 27(18):34–7.
23.
Zhao J Wu W Wang X Liu L . Clinical therapeutic effect and prognostic impact of shuxuetong injection in patients with acute ST-segment elevation myocardial infarction after PCI. Guide China Med. (2019) 17(20):154–5. 10.15912/j.cnki.gocm.2019.20.118
24.
Zhang Y Jin H . Effects of sodium tanshinone IIA sulfonate on myocardial function and prognosis in acute myocardial infarction with ischemia-reperfusion. Hebei Med J. (2019) 41(16):2424–7.
25.
Zhang Y Zeng J . Effects of shuxuetong on myocardial perfusion and adverse cardiovascular events in patients with acute myocardial infarction after PCI. Practical Clin J Integr Tradit Chin West Med. (2019) 19(3):64–5. 10.13638/j.issn.1671-4040.2019.03.031
26.
Yuan B Li S Wang Z . Effects of danshen injection combined with intracoronary injection of tirofiban hydrochloride on cardiac function, no-reflow, and prognosis in patients with acute myocardial infarction after emergency percutaneous coronary intervention. Eval Anal Drug Use Hospitals China. (2019) 19(11):1328–31. 10.14009/j.issn.1672-2124.2019.11.014
27.
You Q . Risk Prediction of no-reflow and Perioperative Myocardial Protection in Patients with Acute Myocardial Infarction Undergoing Emergency PCI [Doctoral dissertation] Chinese PLA Medical School (2019). 10.27637/d.cnki.gjyjc.2019.000065
28.
Ye H . Analysis of the therapeutic value of tanshinone injection after surgery for acute ST-segment elevation myocardial infarction. Clin Res. (2019) 27(11):129–30.
29.
Yao M Jia X Xie J Wang Y Zhao S Wu Y et al Observation on shenfu injection pretreatment combined with intracoronary injection of alprostadil in preventing no-reflow phenomenon during early percutaneous coronary intervention in acute coronary syndrome. Chin Arch Tradit Chin Med. (2019) 37(12):3021–5. 10.13193/j.issn.1673-7717.2019.12.049
30.
You Q Wang J Dong W Tian F Liu HX Jing J et al Protective effect of danhong injection in patients with acute myocardial infarction at a high risk of no-reflow during primary percutaneous coronary intervention. J Geriatr Cardiol (2019) 16(5):406–13. 10.11909/j.issn.1671-5411.2019.05.001
31.
Zhou L Li J Ren J Wang J Yang J Liao X . Effects of danshen chuanxiongqin combined with tirofiban on retinol binding protein 4 in patients with acute ST-segment elevation myocardial infarction after coronary intervention. Chin J Clin Healthcare. (2018) 21(1):51–4.
32.
Zhou H Zhang M Zhou S . Effects of danhong injection on coronary artery blood flow, left ventricular function, and myocardial function in patients with AMI after PCI. Chin J Integr Med Cardio Cerebrovasc Dis. (2018) 16(16):2296–9.
33.
Zhang D Sun D Sun C Du L Yao K Liu Y . Effect of pressurized rapid intravenous drip infusion of shenfu on hemodynamics in patients with acute inferior wall myocardial infarction. J Hebei Med Univ. (2018) 39(8):882–6.
34.
Wang X Cui J Cui X Li Y Hu J Wu Y . Effect of compound danshen injection on renal impairment in patients with acute ST-segment elevation myocardial infarction after PCI. Mod J Integr Tradit Chin West Med. (2018) 27(10):1035–7. 1042.
35.
Wang LR . The application value of Xuesaitong injection in patients undergoing interventional treatment for acute ST-segment elevation myocardial infarction. Int J Med Health Guid. (2018) 24(11):1679–82. 10.3760/cma.j.issn.1007-1245.2018.11.025
36.
Qu L Yuan T Fu R . Effects of shenfu injection on inflammatory factors, fibrinolytic activity, and myocardial reperfusion in patients undergoing elective PCI. Chin J Integr Med Cardio Cerebrovasc Dis. (2018) 16(17):2533–6.
37.
Qin L Zhao Y Zhang B . Effects of danhong injection combined with rosuvastatin on myocardial no-reflow, IL-6, cys-C, and hcy in patients with acute myocardial infarction after PCI. Chin J Integr Med Cardio Cerebrovasc Dis. (2018) 16(17):2453–6.
38.
Na S Li B Wei X Li Y Li D . Efficacy and mechanism of shenfu injection pretreatment combined with intracoronary injection of alprostadil in preventing no-reflow phenomenon after emergency PCI in patients with acute coronary syndrome. Mod J Integr Tradit Chin West Med. (2018) 27(12):1272–7.
39.
Chen W Zhang J Xu X . Efficacy of integrated Chinese and western medicine in preventing no-reflow after PCI in acute myocardial infarction and its effect on serological indicators. Mod J Integr Tradit Chin West Med. (2018) 27(32):3597–600.
40.
Chang H Ning X Han K Wang K Yue L . Effects of danshen injection and salvianolate injection on coronary microcirculation in patients with unstable angina pectoris. Prog Mod Biomed. (2018) 18(12):2294–7. 10.13241/j.cnki.pmb.2018.12.019
41.
Zhang D Wang L Sun D Sun C Du L Yao K et al Comparison of rapid intravenous infusion of shenfu and dopamine infusion in the interventional treatment of acute inferior myocardial infarction. Chin J Mod Nurs. (2017) 23(18):2383–7. Available online at:http://dx.chinadoi.cn/10.3760/cma.j.issn.1674-2907.2017.18.016
42.
Wu J Zheng Q Yan C Wang X Hu J . Efficacy and mechanism of danhong injection in preventing no-reflow after PCI in patients with acute myocardial infarction. Med J Nat Defend Forces Southwest China. (2017) 27(9):986–8.
43.
Wang Y Aimaiti M . Effect of kudiezi injection on patients with acute myocardial infarction undergoing percutaneous coronary intervention. Prac J Card Cereb Pneumal Vasc Dis. (2017) 25(4):81–4.
44.
Leng W . Effect of danhong injection combined with nitroglycerin on percutaneous coronary intervention in acute myocardial infarction. J Hubei Univ Chin Med. (2016) 18(5):18–21.
45.
Zhou H Zhang W Jin H Liu Z Yang W Wang W et al Effect of shuxuetong injection on myocardial perfusion and clinical prognosis in patients with ST-segment elevation myocardial infarction undergoing primary PCI. Chin Heart J. (2015) 27(4):431–3, 447. 10.13191/j.chj.2015.0121
46.
Wu Q Jin H Zhang W Li Y Liu Z . Clinical efficacy observation of shuxuetong injection in patients with acute myocardial infarction after PCI. Pharmacol Clin Chin Materia Medica. (2015) 31(2):112–3. 10.13412/j.cnki.zyyl.2015.02.048
47.
Jia M Liu J Gai F Wang Y Zhou F Zhang Y . Effects of danhong injection combined with nitroglycerin on no-reflow phenomenon and C-reactive protein in patients with acute myocardial infarction during PCI. J Hebei Tradit Chin Med Pharmacol. (2015) 30(1):5–7. 10.16370/j.cnki.13-1214/r.2015.01.002
48.
Feng J . Effects of Xuesaitong Injection on Cardiac Microcirculation and Short-term cardiac Function in Patients with STEMI After Emergency PCI [Master’s thesis] Henan University of Chinese Medicine. (2015). Available online at:https://kns.cnki.net/kcms2/article/abstract?v=VkQzIsHyPdhMlpJqz5N0kVARWmp3bxULTl-yDTixeDUG1mfNs-x43B4wLtvybZUZlpO7wKyRYTL-FTrTREJx7KTUoW3yjBKgaXvZ-uCI3AyMYly_xrY1LZgMz9DQXGNP_twwjPxodisDHT5RIy9yh-qfoNzMWExJ92AY4OVvbnNZudTWCy0sSA==&uniplatform=NZKPT&language=CHS
49.
Zhou X . Effects of Danshen Chuanxiongqin Injection on Myocardial Perfusion in Patients with Acute ST-segment elevation Myocardial Infarction [Master’s thesis] Liaoning University of Traditional Chinese Medicine]. (2014). Available online at:https://kns.cnki.net/kcms2/article/abstract?v=VkQzIsHyPdgRdON_-oi9gSNx1r_CMNpoXLCHF_l8PgHLBEPam9jQ1Y1bQ7WFLGCvTVQnUnHG-wGvu-KOSYfeG9lD0W7y4tny0wXdQIEXpd5MkogjeOfLBMPc4oKigAvtXszAVRbBlo7awyPt5D50hu82_o0DAMDPvWDF1cXPF7KrLtnPV2bF9Q==&uniplatform=NZKPT&language=CHS
50.
Yang X Zheng Y Guo S Li J Shang S . Clinical observation of 30 cases of intracoronary injection of shenmai injection combined with western medicine in the treatment of coronary no-reflow after interventional therapy for acute myocardial infarction. J Tradit Chin Med. (2014) 55(10):854–7. 10.13288/j.11-2166/r.2014.10.013
51.
Yang X Zheng Y Guo S Li J Shang S . Clinical observation of combined intracoronary Chinese and western medicine in preventing no-reflow during interventional procedures. J New Chin Med. (2014) 46(4):37–9. 10.13457/j.cnki.jncm.2014.04.016
52.
Wang J Yao Z Yin H Li Y . Clinical analysis of integrated Chinese and western medicine combined with emergency interventional therapy for acute coronary syndrome. Mod J Integr Tradit Chin West Med. (2014) 23(17):1901–2.
53.
Guo S . Application research on shenmai injection combined with western medicine in the treatment of acute myocardial infarction. Chin J Mod Drug Appl. (2014) 8(11):132–4. 10.14164/j.cnki.cn11-5581/r.2014.11.092
54.
Wang B Zhou C Guo M Li P Zhang X . Effect and mechanism of danhong on myocardial no-reflow after PCI in patients with ST-segment elevation acute myocardial infarction. J Qilu Med. (2013) 28(3):250–2.
55.
Feng X Na R . Effect of shuxuetong injection on slow flow and no-reflow during coronary intervention. Chin J Integr Med Cardio Cerebrovasc Dis. (2013) 12(12):1438–9.
56.
Wang R Han Q Jia Y Lu J . Effect of danshen chuanxiongqin injection on myocardial injury in patients with unstable angina after coronary intervention. Chin J Integr Med. (2011) 31(7):899–902.
57.
Zhao D Jin H Liu Z Shen J Yu H Gao J . Effect of yinxingdamo injection on myocardial perfusion and clinical prognosis in patients with acute myocardial infarction after primary percutaneous coronary intervention. Shanghai Medical Journal. (2010) 33(10):930–3.
58.
Wang X Wu Y Shen B Guo Z Wang X Cui X et al Clinical study on the prevention and treatment of reperfusion injury after interventional therapy for acute myocardial infarction with shengmai injection. Mod J Integr Tradit Chin West Med. (2010) 19(28):3553–4. 3561.
59.
Shi W Sun X Qu L Wang G . Effects of danhong injection on myocardial inflammatory response and coronary blood flow after percutaneous coronary intervention. Chin J Integr Tradit West Med Intensive Crit Care. (2010) 17(5):288–91. Available online at:http://dx.chinadoi.cn/10.3969/j.issn.1008-9691.2010.05.012
60.
Wang X . Clinical Study on the Prevention and Treatment of Reperfusion Injury After Interventional Therapy for Acute Myocardial Infarction with Shengmai Injection [Master’s thesis]. Beijing University of Chinese Medicine (2008). Available online at:https://kns.cnki.net/kcms2/article/abstract?v=VkQzIsHyPdgheW6pYs68MgUA8DaNEsHafrwLB65WtsW9KqMzzDwmgSRH4EEhVR5z8wLfXqzvqQwDrTKfrCeNRbstLeFTPEc5cWfPm2N5rQRGJqViM1p6h24xya8R5jaFKnQKIfJb8HU4o8Ih5TwI62DRskEgJGKF_gdnldZHtBgmYYKXAeUWWg==&uniplatform=NZKPT&language=CHS
61.
He J . Application of shenfu injection in emergency PCI. J Emerg Tradit Chin Med. (2006) (7):736–7.
62.
Su G Liu L Meng Q Wang L . Effect of shenfu injection on plasma brain natriuretic peptide and N-terminal propeptide of type III procollagen in patients with acute myocardial infarction undergoing interventional therapy. Chin J Integr Med. (2005) (5):422–4.
63.
Yoshinaga M Muramatsu T Ishikawa M Toriya T Uwatoko T Matsuwaki Y et al A pilot study of perfusion balloon predilatation in conjunction with intracoronary nicorandil administration for acute coronary syndrome. Cardiovasc Interv Ther. (2025) 40(1):45–56. 10.1007/s12928-024-01034-0
64.
Ndrepepa G Cassese S Xhepa E Joner M Sager HB Kufner S et al Coronary no-reflow and adverse events in patients with acute myocardial infarction after percutaneous coronary intervention with current drug-eluting stents and third-generation P2Y12 inhibitors. Clin Res Cardiol. (2024) 113(7):1006–16. 10.1007/s00392-023-02340-y
65.
Wang L Cheng Z Gu Y Peng D . Short-Term effects of verapamil and diltiazem in the treatment of No reflow phenomenon: a meta-analysis of randomized controlled trials. BioMed Res Int. (2015) 2015:382086. 10.1155/2015/382086
66.
Zeng Q Zhang LD Wang W . A meta-analysis of randomized controlled trials investigating tirofiban combined with conventional drugs by intracoronary administration for no-reflow prevention. Anatol J Cardiol. (2021) 25(1):7–16. 10.14744/AnatolJCardiol.2020.99469
67.
d'Entremont MA Alazzoni A Dzavik V Sharma V Overgaard CB Lemaire-Paquette S et al No-reflow after primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction: an angiographic core laboratory analysis of the TOTAL trial. EuroIntervention. (2023) 19(5):e394–401. 10.4244/EIJ-D-23-00112
68.
Pradhan A Bhandari M Vishwakarma P Sethi R . Deferred stenting for heavy thrombus burden during percutaneous coronary intervention for ST-elevation MI. European Cardiology. (2021) 16:e08. 10.15420/ecr.2020.31
69.
Feng X Li Y Wang Y Li L Little PJ Xu SW et al Danhong injection in cardiovascular and cerebrovascular diseases: pharmacological actions, molecular mechanisms, and therapeutic potential. Pharmacol Res. (2019) 139:62–75. 10.1016/j.phrs.2018.11.006
70.
Guo Y Yang JH Cao SD Gao CX He Y Wang Y et al Effect of main ingredients of danhong injection against oxidative stress induced autophagy injury via miR-19a/SIRT1 pathway in endothelial cells. Phytomedicine. (2021) 83:153480. 10.1016/j.phymed.2021.153480
71.
Chen Z Liu T Xiong L Liu Z . Shen-fu injection modulates HIF- 1α/BNIP3-mediated mitophagy to alleviate myocardial ischemia-reperfusion injury. Cardiovasc Toxicol. (2025) 25(6):898–914. 10.1007/s12012-025-09993-3
72.
MEIm XD Cao YF Che YY Li J Shang ZP Zhao WJ et al Danshen: a phytochemical and pharmacological overview. Chin J Nat Med. (2019) 17(1):59–80. 10.1016/S1875-5364(19)30010-X
73.
Gao F Li JM Xi C Li HH Liu YL Wang YP et al Magnesium lithospermate B protects the endothelium from inflammation-induced dysfunction through activation of Nrf2 pathway. Acta Pharmacol Sin. (2019) 40(7):867–78. 10.1038/s41401-018-0189-1
74.
Shen L Xu R Yin J Lu H Zhang S Huang Z et al Effects of salvianolate on myocardial perfusion after primary percutaneous catheter intervention in patients with ST-segment elevation myocardial infarction: a multicenter, randomized, double-blind, placebo-controlled study. Ann Transl Med. (2020) 8(18):1185. 10.21037/atm-20-6081
Summary
Keywords
percutaneous coronary intervention, no-reflow or slow blood flow, traditional Chinese medicine injection, network meta-analysis, ischemia-reperfusion injury
Citation
Cai T, Li W, Xu W, Lin C, Liang L, Wang D and Zheng J (2026) Efficacy and safety of Traditional Chinese Medicine injections for no-reflow or slow flow in patients with acute coronary syndrome after percutaneous coronary intervention: a systematic review and network meta-analysis. Front. Cardiovasc. Med. 12:1619345. doi: 10.3389/fcvm.2025.1619345
Received
06 August 2025
Revised
24 November 2025
Accepted
02 December 2025
Published
07 January 2026
Volume
12 - 2025
Edited by
DeLisa Fairweather, Mayo Clinic Florida, Jacksonville, United States
Reviewed by
Yu-Xi Huang, Peking University, China
Qian Li, Dali University, China
Updates
Copyright
© 2026 Cai, Li, Xu, Lin, Liang, Wang and Zheng.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Jinghui Zheng jinghuizheng@yeah.net
†These authors have contributed equally to this work and share first authorship
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.