- 1School of Public Health, Xuzhou Medical University, Xuzhou, China
- 2Department of Physiology, Basic Medical School, Xuzhou Medical University, Xuzhou, China
- 3School of Basic Medical Sciences, Southwest Medical University, Luzhou, China
- 4Department of Cardiology, Institute of Cardiovascular Research, The Affiliated Hospital, Southwest Medical University, Luzhou, China
- 5College of Life Science, Xuzhou Medical University, Xuzhou, China
- 6Department of Physiology, School of Basic Medical Sciences, Southwest Medical University, Luzhou, China
Importance: Obese patients are mostly accompanied by various cardiovascular diseases (CVDs), which is a major global health challenge and has important clinical significance. The global burden of CVDs caused by high body mass index (BMI) is still not well known.
Objective: To determine the global burden of high BMI-related CVDs from 1990 to 2023.
Methods: Following the methodological framework and analytical strategy used in the 2023 global burden of disease study (GBD 2023), we examined the death and disability-adjusted life years (DALYs) of CVDs associated with high BMI in the global population considering year, gender, age, socio-demographic index (SDI), income, and geographic location. We also calculated the annual percentage change (APC) to quantify the trends over time.
Results: From 1990 to 2023, high BMI significantly contributed to over a 2-fold increase in global deaths and DALYs due to CVDs, particularly affecting ischemic heart disease (IHD), hypertensive heart disease (HHD), ischemic stroke (IS), and intracranial hemorrhage. IHD saw a doubling of deaths and DALYs, with males being more affected, and the age group with the highest deaths in over 70 years old, while DALYs peaked in the 50–69 age group. The deaths of IHD moved from high SDI to upper-middle SDI countries. Deaths and DALYs for HHD, IS, and intracranial hemorrhage also doubled, with females being slightly more affected. These conditions maintained their highest death in those over 70, but DALYs were highest in the 50–69 age group. The fastest-growing APC of deaths and DALYs were observed in low SDI countries and regions, as well as lower-middle income countries and regions, indicating a significant shift in the geographic distribution of CVD death.
Conclusion: High BMI is a major contributor to CVDs globally, leading to significant increases in deaths and DALYs over the past three decades. The impact varies by age, gender, income level, and geographic region, with the APC growing most rapidly in lower-middle income populations. IHD is particularly concerning, with notable gender and age-specific trends. Addressing high BMI and its associated cardiovascular risks, especially in vulnerable populations, is crucial to mitigating the growing impact of obesity-related CVDs.
1 Introduction
Cardiovascular diseases (CVDs), have become a major public health challenge, with WHO data indicating in 2022, nearly 20 million deaths were attributed to CVDs, representing approximately 32% of all global deaths (1). The increasing prevalence of high body mass index (BMI) is a significant contributor to this trend, with 2.2 billion adults worldwide classified as having a high BMI in 2020, a number expected to rise to 3.3 billion by 2035, or 54% of the global adult population (2). Among children aged 5–19, the proportion with a high BMI is projected to increase from 22% to 39% by 2035 (2). High income regions like North America and parts of Europe have particularly high rates of high BMI among adults (3). The issue affects all age groups, with a notable increase in adolescents, and is economically pronounced in lower-middle income countries. High BMI individuals are at a higher risk of developing various diseases, including CVDs, type 2 diabetes, and chronic kidney disease, underscoring the urgency for in-depth research into CVDs and their risk factors (2, 4).
Unhealthy lifestyle habits like high-calorie diets, lack of exercise, smoking, and sedentary behavior contribute to the rise in high BMI and are key risk factors for CVDs (5–7), including ischemic heart disease (IHD), ischemic stroke (IS), and coronary artery disease, are leading causes of global death, challenging the health system (8, 9). Understanding the link between high BMI and CVDs is crucial for developing prevention strategies. The global burden of disease(GBD), injuries, and risk factors study 2023 data, released in 2025, provides a comprehensive assessment of the global impact of health challenges, including the burden of CVDs attributable to high BMI, such as IHD, hypertensive heart disease (HHD), IS, and intracerebral hemorrhage, over the past decades (10). This information is vital for crafting effective public health interventions to address the escalating threat of CVDs associated with high BMI.
This study aims to utilize the latest GBD data to analyze, for the first time, the relationship between the high BMI population and several common CVDs, as well as the global burden, during the period from 1990 to 2023. Special emphasis will be placed on regional, age, and gender differences. Through this research, we expect to provide a scientific basis for the prevention and control of CVDs among the global high BMI population and offer support for formulating effective public health strategies.
2 Methods
2.1 Data sources
The GBD 2023 study is a comprehensive multinational research estimating global burden using data from various sources and tools (http://ghdx.healthdata.org/gbd-results-tool). It analyzed burden globally, regionally, and nationally, stratified by socio-demographic index (SDI). Disability-adjusted life-years (DALYs) measure healthy life years lost due to disease, including years of life lost (YLL) and years lived with disability (YLD). The study provided estimates for incidence, prevalence, DALYs, and death for each disease and risk factor, focusing on CVDs related to high BMI.
2.2 Definitions in GBD 2023
The four-level classification system for risk factors in the GBD 2023 is as follows: the first level is divided into three major categories, namely behavioral, metabolic, and environmental and occupational factors; the second level covers 20 risk clusters; the third level consists of 42 specific risk factors; and the fourth level includes 22 distinct factors. Notably, the metabolic category does not involve further subdivision into the third and fourth levels. Metabolic risk factors encompass high fasting plasma glucose, high systolic blood pressure, high BMI, low bone mineral density, kidney dysfunction, and high low density lipoprotein cholesterol. In total, this classification system encompasses 88 modifiable risk factors. Further details on these five risk factors are available in the GBD 2023 online resources (https://ghdx.healthdata.org/gbd-2023/sources?components.6&risks.367&location). It examines the global burden of CVDs attributable to high BMI across all ages, using deaths and DALYs as metrics. The cause-of-death ensemble model estimates high BMI-attributable deaths by incorporating predictive covariates, accounting for location, age, sex, and year.
2.3 Deaths, DALYs, and annual percentage change (APC)
From 1990 to 2023, the GBD study measured the global, regional, and national burden of metabolic diseases using deaths and DALYs for all age groups. It assessed the impact of high BMI on global burden by calculating potential DALY changes at the theoretical minimum risk level. The GBD 2023 Disease and Injury Collaborators performed 500 iterations for each calculation to produce sample-level estimates, reporting the meaning of these samples as the final estimate. The 95% uncertainty intervals were determined by the 2.5th and 97.5th percentiles of the samples. Data visualization and tabular results (https://vizhub.healthdata.org/gbd-results/) are available online, with analyses following GBD's established rules and procedures. The APC is a widely used indicator to measure the trend of standardized rates over a specific period, and was calculated by Joinpoint regression analysis.
3 Results
3.1 Overview
In 2023, the numbers of deaths and DALYs of all disease sub-categories increased by 1–3 times compared to 1990 (Supplementary Table S1). Among diseases attributable to high BMI, CVDs account for the highest of deaths, diabetes and kidney diseases account for the highest of DALYs. In 1990, Central Europe, Eastern Europe and Central Asia were the regions with the top of deaths and DALYs attributable to high BMI. By 2023, the region with the top of deaths remained unchanged, while China became the territory with the highest of DALYs. (Figure 1). In 2023, the other two territories with the top of deaths also included India and China. Further ranking analysis of deaths and DALYs of various CVDs caused by BMI showed that the top four were IHD, HHD, IS, and intracerebral hemorrhage. The rankings remained stable in 1990 and 2023 (Supplementary Figure S1). Therefore, we mainly analyzed the impact of BMI on the global burden of these four CVDs.
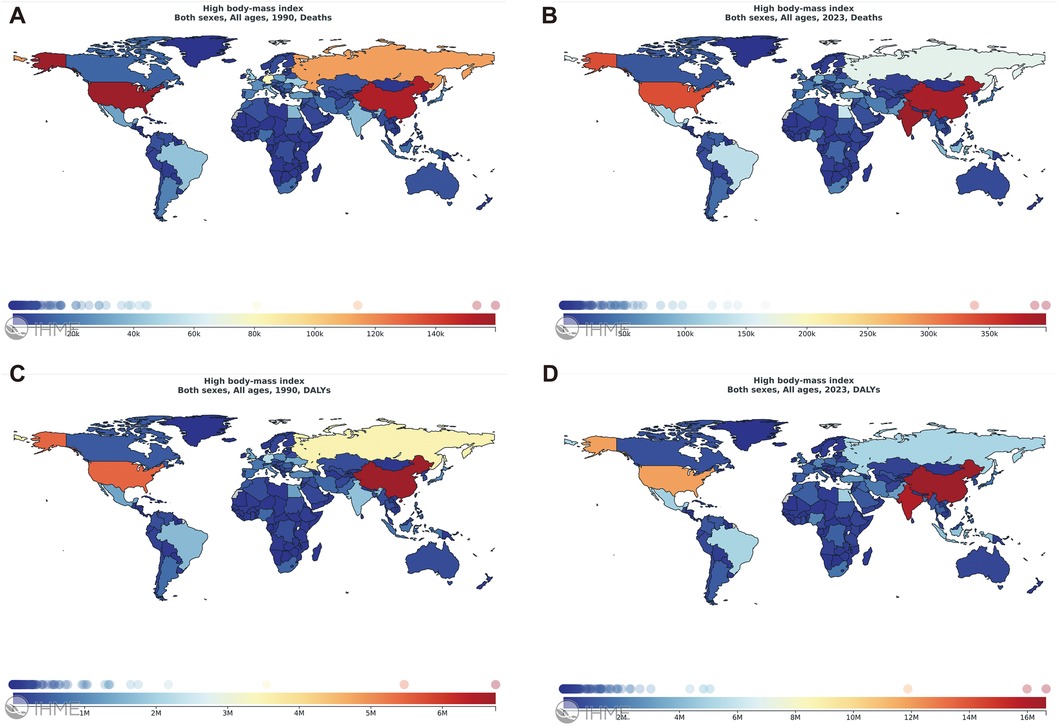
Figure 1. Global distribution of disease burden of high BMI in 1990 and 2023. Global maps of high BMI deaths (A) and DALYs (C) in 1990, and deaths (B) and DALYs (D) in 2023. Maps reproduced from the GBD database, Institute for Health Metrics and Evaluation (https://vizhub.healthdata.org/), licensed under CC BY-NC-ND 4.0.
3.2 Ischemic heart disease
IHD has the heaviest burden among high BMI-related CVDs. It has a high probability of causing heart failure (11). Among middle-aged and older adult people, the numbers of deaths caused by it shows a trend of getting younger. Tobacco, hypertension, hyperlipidemia, and high BMI are the main risk factors for IHD (12, 13). In 2023, 8.90 million (95% UI: 8.04–9.65) deaths were related to IHD, and 0.94 million (95% UI: 0.43–1.47) deaths were related to IHD caused by high BMI, accounting for 10.6%. In 2023, it was estimated that 24.56 million (95% UI: 11.44–37.26) DALYs of all age groups were caused by IHD due to high BMI, doubling compared to 33 years ago (Table 1). Males accounted for 59.6% (14.65 million) of these DALYs, and females accounted for 40.4% (9.91 million). Among all age groups, the over 70 years old group had the highest of deaths [0.45 million (95% UI: 0.20–0.73)], and the 50–69-year-old group had the highest of DALYs [12.25 million (95% UI: 5.81–18.26)].
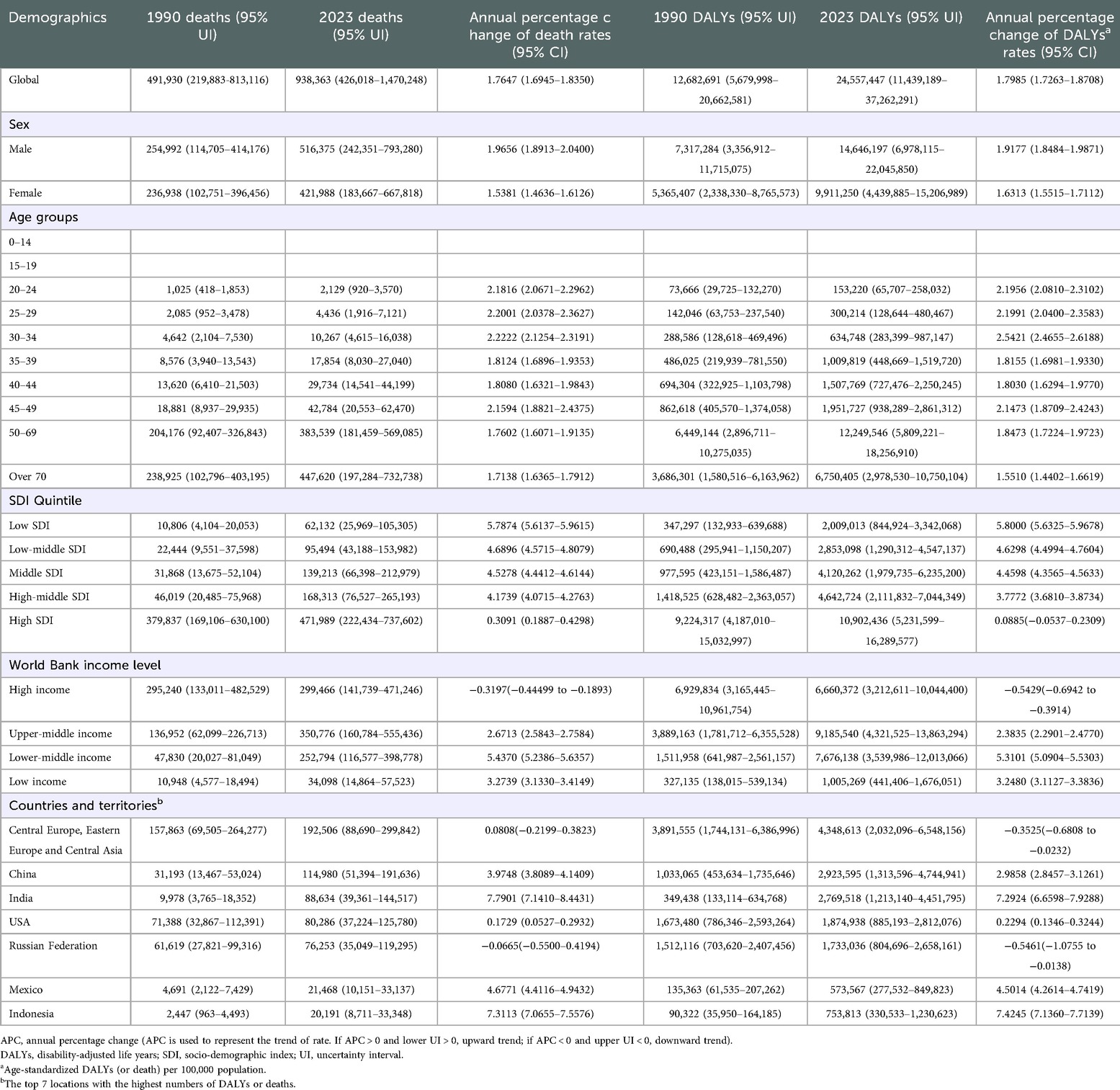
Table 1. The burden attributable to BMI risks in ischemic heart disease in 1990 and 2023 and the temporal trends from 1990 to 2023.
The death and the DALYs were the highest in high SDI [0.47 million (95% UI: 0.22–0.74) for deaths, 10.90 million (95% UI: 5.23–12.69) for DALYs]. The number of deaths was the highest among the upper-middle income population [0.35 million (95% UI: 0.16–0.56)], as well as the number of DALYs [9.19 million (95% UI: 4.32–13.86)]. In 2023, the number of IHD deaths in China [0.11 million (95% UI: 0.05–0.19)] exceeded that of the United States of America (USA) [0.08 million (95% UI: 0.04–0.13)]. Meanwhile, Central Europe, Eastern Europe and Central Asia had the top of DALYs of IHD over 33 years ago [4.35 million (95% UI: 2.03–6.55)] (Supplementary Figure S2). The other three territories with the top numbers of DALYs of high BMI-related IHD in 2023 were China [2.92 million (95% UI: 1.31–4.74)], India [2.77 million (95% UI: 1.21–4.45)], and the USA [1.87 million (95% UI: 0.89–2.81)].
3.3 Hypertensive heart disease
Research shows that an increase in BMI leads to fat accumulation in the body, triggering a series of metabolic disorders and activating the renin-angiotensin-aldosterone system, which promotes an increase in blood pressure (14). The long-term state of high blood pressure increases the afterload of the heart, causing myocardial cells to undergo compensatory hypertrophy and gradually develop into HHD (15). The probability of high BMI people suffering from hypertension is several times higher than that of people with normal weight, which significantly increases the risk of HHD (16).
In 2023,1.48 million (95% UI: 1.18–1.82) deaths were related to HHD, and 0.60 million (95% UI: 0.37–0.81) deaths were related to HHD caused by high BMI, accounting for 40.5%. In 2023, it was estimated that 13.18 million (95% UI: 10.09–16.94) DALYs of all age groups were caused by HHD due to high BMI. Males accounted for 46.6% (6.14 million) of these DALYs, and females accounted for 53.4% (7.04 million) (Table 2). Among all age groups, the number of deaths was the highest among those over 70 years old [0.37 million (95% UI: 0.17–0.56)], and the number of DALYs was the highest in the 50–69-year-old group [5.70 million (95% UI: 4.09–7.63)].
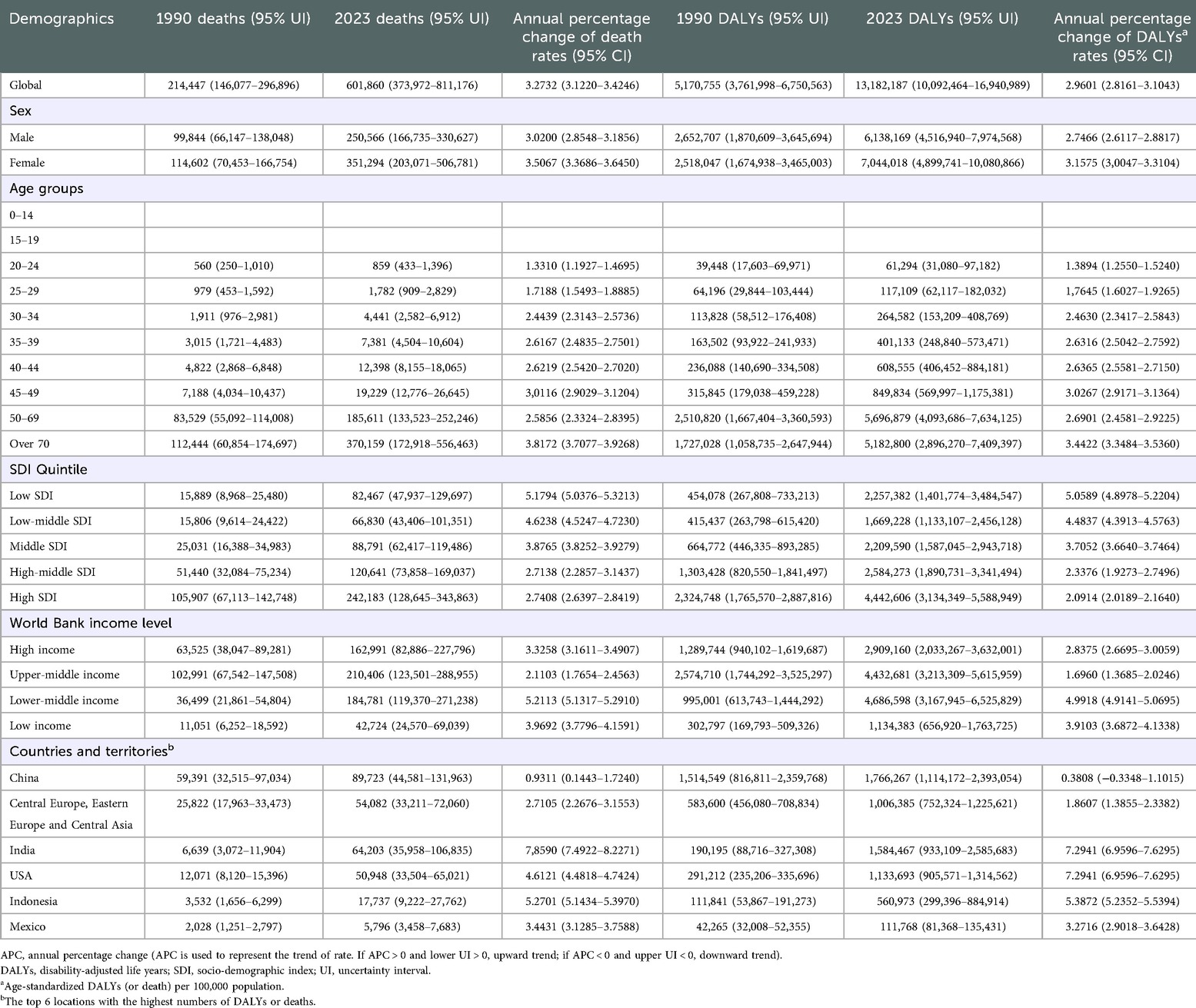
Table 2. The burden attributable to BMI risks in Hypertensive heart disease in 1990 and 2023 and the temporal trends from 1990 to 2023.
From 1990 to 2023, the DALYs of HHD caused by high BMI globally increased 2.5 times that of 33 years ago. Over the past 33 years, China has been the territory with the highest DALYs of HHD (Supplementary Figure S3). The top three countries and territories with the top of deaths of high BMI-related HHD were China [0.09 million (95% UI: 0.04–0.13)], Central Europe, Eastern Europe and Central Asia [0.05 million (95% UI: 0.03–0.07)], and India [0.06 million (95% UI: 0.04–0.11)]. The death and DALYs were the highest in high SDI countries and regions (0.24 million (95% UI: 0.13–0.34) for death, [4.44 million (95% UI: 3.12–5.59) for DALYs]. The number of DALYs was the highest among the lower-middle income population [4.69 million (95% UI: 3.17–6.53)], and the number of deaths was the highest among the upper-middle income population [0.21 million (95% UI: 0.12–0.29)].
3.4 Ischemic stroke
In 2023, 3.27 million (95% UI: 2.87–3.68) deaths were related to IS, while 0.15 million (95% UI: 0.03–0.29) deaths were caused by IS due to high BMI, accounting for 4.6%. From 1990 to 2023, the global DALYs of IS caused by high BMI increased approximately 1.75-fold (Table 3). Males accounted for 48.8% (2.00 million) of the DALYs, while females accounted for 51.2% (2.09 million) of the DALYs. Among all age groups, the number of deaths was the highest in the population over 70 years old [0.09 million (95% UI: 0.01–0.18)], and the number of DALYs was the highest in the 50–69-year-old population [1.95 million (95% UI: 0.38–3.59)].
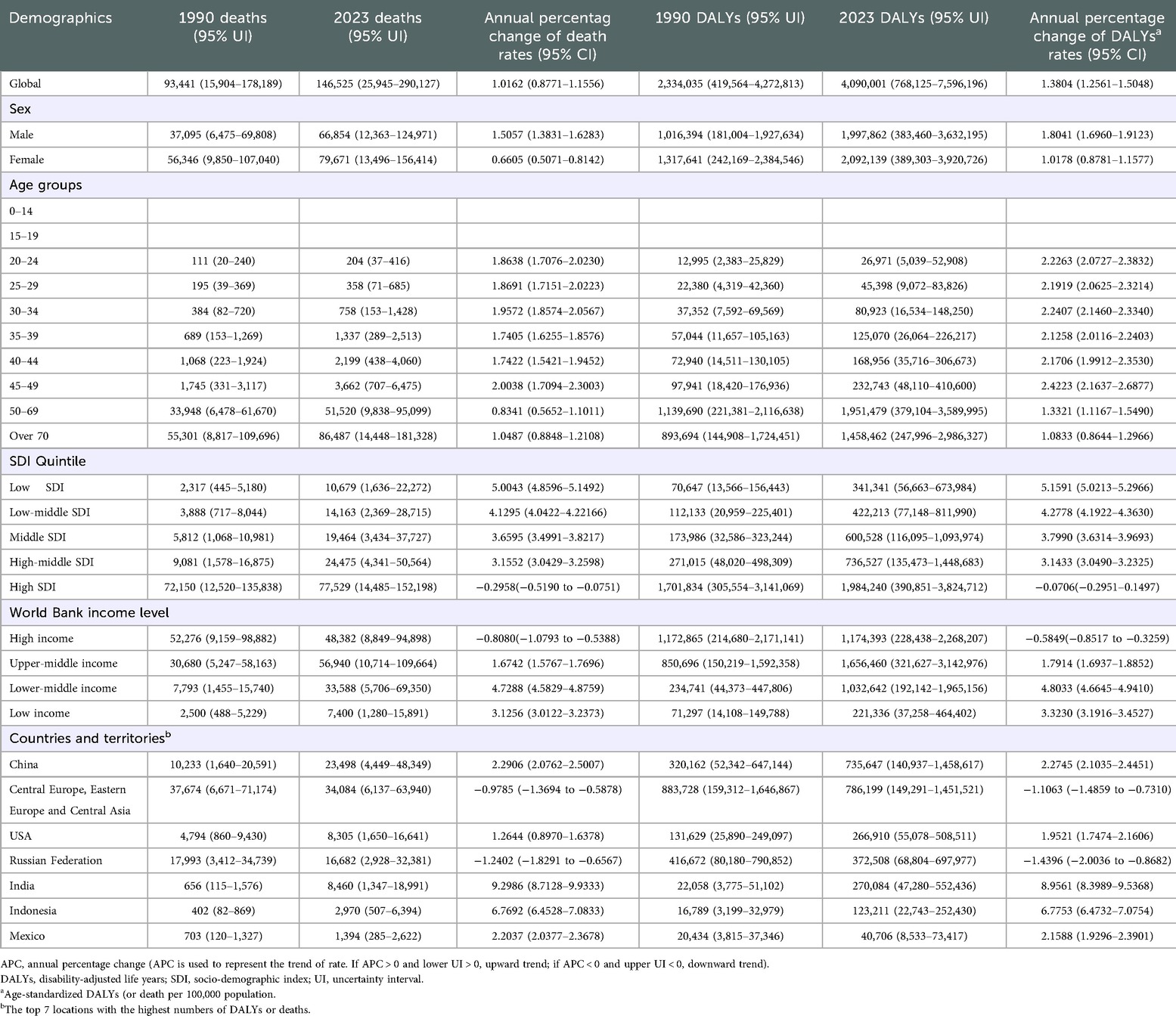
Table 3. The burden attributable to BMI risks in ischemic stroke in 1990 and 2023 and the temporal trends from 1990 to 2023.
The death [0.08 million (95% UI: 0.01–0.15)] and DALYs [1.98 million (95% UI: 0.39–3.82)] were the highest in high SDI. The upper-middle income population had the top numbers of deaths [0.06 million (95% UI: 0.01–0.11)] and DALYs [1.66 million (95% UI: 0.32–3.14)]. Over the past three decades, China has been the territory with the heaviest burden of IS Supplementary Figure S4). Globally, the top three countries and territories with the top numbers of deaths and DALYs of high BMI-related IS were Central Europe, Eastern Europe and Central Asia, China, and Russia.
3.5 Intracerebral hemorrhage
Intracerebral hemorrhage refers to the bleeding caused by the rupture of blood vessels within the non-traumatic brain parenchyma. It is an acute cerebrovascular disease characterized by high incidence, high disability rate, and high death. High BMI has a significant impact on the global burden of intracerebral hemorrhage.
In 2023, 3.16 million (95% UI: 2.75–3.55) deaths were related to intracerebral hemorrhage, while 0.07 million (95% UI: −6,116–162,868) deaths were caused by intracerebral hemorrhage due to high BMI. In 2023, it was estimated that 2.33 million (95% UI: −0.12–5.46) DALYs across all age groups were caused by intracerebral hemorrhage resulting from high BMI (Table 4). From 1990 to 2023, the global DALYs of intracerebral hemorrhage caused by high BMI increased approximately 3.13-fold. Males accounted for 45.2% (1.05 million) of the DALYs, and females accounted for 54.8% (1.28 million) of the DALYs. Among all age groups, globally, the 50–69-year-old population had the top numbers of deaths [0.04 million (95% UI: −1,383–91,102)] and DALYs [1.24 million (95% UI: −0.04–2.86)]. The death [0.03 million (95% UI: 487–58,815)] and DALYs [0.81 million (95% UI: 10,620–1,729,374)] were the highest in high SDI. The upper-middle income population had the top numbers of deaths [0.03 million (95% UI: −4,265–73,914)] and DALYs [1.06 million (95% UI: −64,348–2,415,566)].
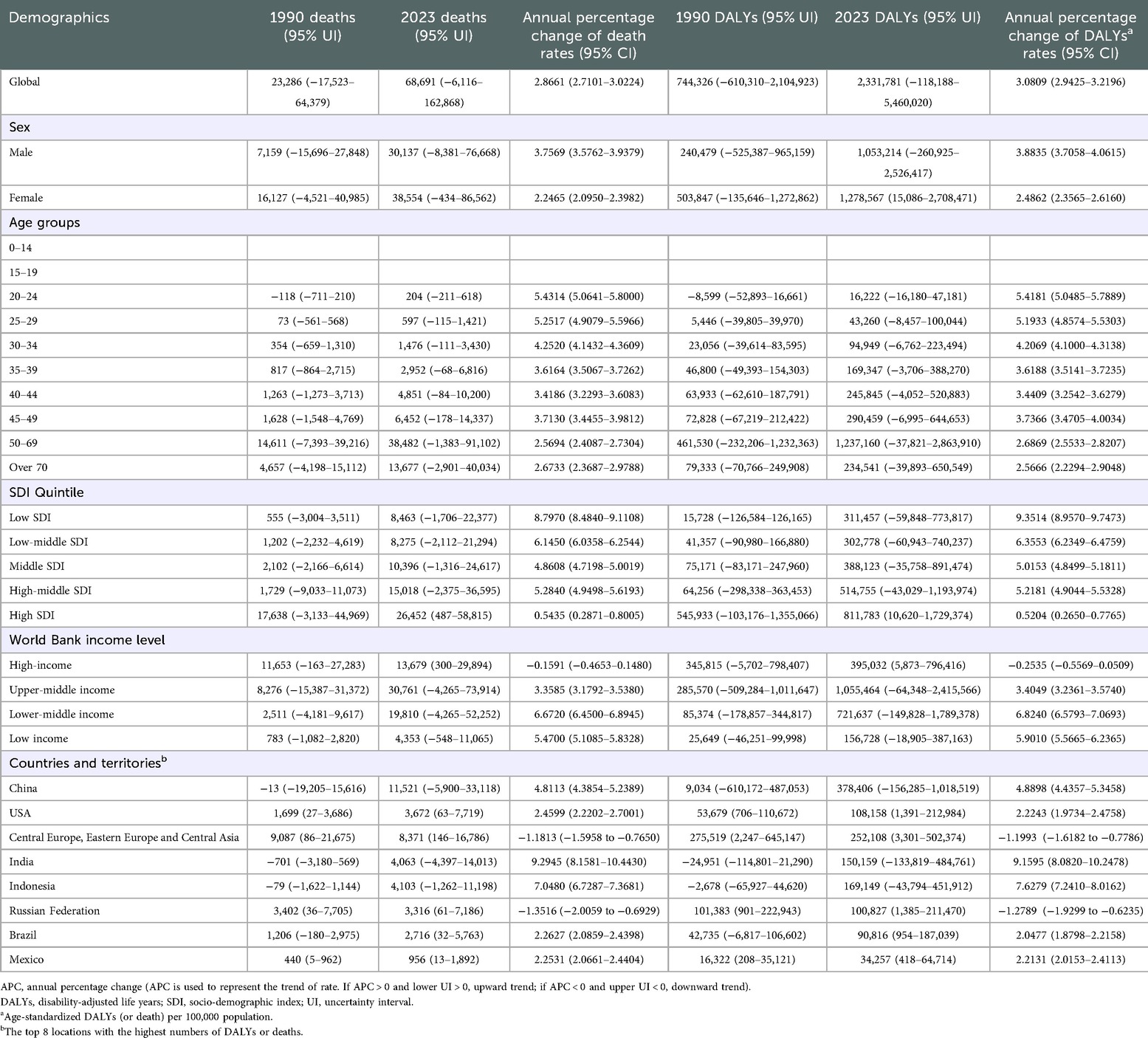
Table 4. The burden attributable to BMI risks in intracerebral hemorrhage in 1990 and 2023 and the temporal trends from 1990 to 2023.
Over the past 33 years, China has been the territory with the highest deaths and DALYs of intracerebral hemorrhage (Supplementary Figure S5). The other regions with the top absolute global burden of high BMI-related intracerebral hemorrhage were Central Europe, Eastern Europe and Central Asia.
4 Discussion
High BMI significantly raises the risk of CVDs, with each 1 kg/m2 increase in BMI associated with a 10%–15% rise in hypertension risk (17). Individuals with high BMI are more prone to high cholesterol, triglycerides, and high-density lipoprotein cholesterol, which accelerates atherosclerosis and coronary heart disease risk (18). Obesity also alters cardiac structure and function, increasing the incidence of heart failure and arrhythmia (19). The risk of coronary heart disease in obese individuals is directly proportional to the incidence of obesity (20). High BMI not only raises the risk of CVD occurrence but also exacerbates disease severity and treatment difficulty, imposing a heavy burden on personal health, families, and the healthcare system. It increases both direct medical costs, such as hospitalization and medication, and indirect costs, like reduced working hours and labor ability, placing significant pressure on the social economy (21).
Our results show that high BMI has a profound impact on the global burden of CVDs across all age groups, and it has increased significantly from 1990 to 2023, especially in territories and countries with a high SDI and among high and upper-middle income groups in China, India, and Central Europe, Eastern Europe and Central Asia. The incidence of high BMI-related IHD is lower in women than males, likely due to estrogen's protective effect and men's social and psychological burden (22, 23). However, females have higher incidence rates of high BMI-related hypertension, IHD, and intracerebral hemorrhage. This may be due to the decrease in estrogen levels with age, particularly after women reach menopause (24).
Additionally, the death of high BMI-related IHD is highest in the over 70 age group. In certain regions with high SDI, the death and DALYs associated with high BMI-related IHD rank first. In some upper-middle income populations, the death and DALYs related to high BMI-related IHD are rising rapidly. This is closely linked to the natural environment and the social and psychological pressures faced by these populations. However, for high BMI-related HHD, and IS, the death is highest in those over 70 years old, while DALYs are most significant in the 50–69 age group. In this age group, physical function begins to decline, and the metabolic rate slows down, which means the adverse effects of high BMI are more likely to accumulate, greatly increasing their risk (25–29). In high SDI regions and countries, DALYs from BMI-related HHD are higher. However, DALYs show an upward trend among lower-middle income populations. For high BMI-related intracerebral hemorrhage, the death and DALYs are heaviest in the 50–69 age group. Overall, the global burden of high BMI-related CVDs is highest in high SDI.
Regional differences are significant in the burden of CVDs linked to high BMI. Countries and territories like China, India, the USA, and Central Europe, Eastern Europe and Central Asia face a heavy burden, especially in areas with rapid economic growth and Western-style diets, which increase high-calorie food intake and reduce physical activity, leading to higher BMI and CVD incidence (19, 30). In China, urban areas with high obesity prevalence have higher hospitalization and death for CVDs, while regions with traditional healthy lifestyles see a lighter burden of CVD, despite hypertensive patients (31). Additionally, China's aging population exacerbates the burden. In the USA, the high-calorie diet and sedentary lifestyle make obesity a major CVD risk factor (32, 33).
High BMI contributes significantly to the burden of CVDs by triggering metabolic disorders, insulin resistance, inflammation, and oxidative stress, which promote atherosclerosis and endothelial damage (34, 35). It also leads to cardiac structural changes, increasing heart burden and impairing function over time (36). Obesity worsens heart function, elevates the risk of arrhythmia and heart failure, and reduces the heart's energy metabolism, worsening disease progression and prognosis (37, 38). Patients with high BMI face greater treatment challenges, prolonged recovery, and higher death and DALYs due to associated complications.
Preventing and controlling CVDs is challenging, particularly in regions with limited medical resources and low awareness, leading to delayed diagnoses and poor management (39). Global population aging exacerbates the issue, as the older adult are at high risk for CVDs (40). The complex etiology of CVDs, influenced by genetics, lifestyle, and environment, complicates prevention and treatment (41). To reduce the burden of high BMI-related CVDs, it's essential to strengthen health education, raise awareness, and promote lifestyle changes such as balanced diets, exercise, smoking cessation, and alcohol reduction (13, 42–44). In Northeast China, high BMI from unhealthy diets leads to IHD, which can be mitigated by dietary adjustments (45). The Mediterranean diet, rich in nuts, can lower blood pressure, lipids, and glucose, and improve heart health (46).
For individuals with high BMI, regular check-ups are essential to monitor blood pressure, lipids, glucose, and manage CVD risk factors. Obesity can also complicate imaging, hindering the assessment of internal injuries (47). Higher BMI in early adulthood (18–34 years) increases CVD risk, particularly IHD (28). It contributes to early vascular and metabolic issues, such as dyslipidemia and hypertension, accelerating CVD progression (48). Overweight or obese individuals face a higher lifetime risk of CVDs, with BMI strongly linked to heart failure (32). BMI-stratified criteria can improve diagnosis and guide exercise testing for potential heart failure (49). Central fat measurements like waist-to-height ratio are more closely associated with heart failure risks than BMI (50, 51). Fat redistribution to the trunk during adolescence emphasizes the need for both BMI and waist-to-height ratio in early CVD intervention.
Patients with high BMI face increased higher postoperative complications, slower recovery, and poorer neurological outcomes (52, 53). This affects their quality of life and places a care burden on families and society (54). Treatment for HHD includes antihypertensive drugs, metabolic therapies, and weight management, with tailored plans to improve metabolic profiles and reduce IS recurrence. Nutritional support and rehabilitation improve physical function, enhance survival, and reduce societal disease burden. Comprehensive interventions that combine medical and lifestyle factors can significantly reduce disease risk and global burden, improving patient outcomes (55–57).
To prevent and reduce the global burden of CVDs associated with high BMI, targeted interventions tailored to economic status, age, and gender are essential. Low income countries and regions should strengthen free primary-level screening and affordable drug supply, while coordinating efforts to control both infectious and chronic diseases (58). High income countries and regions should build sports-friendly cities, reduce health disparities through healthcare incentives and programs for vulnerable populations (59), and help young people develop healthy habits through campus and workplace interventions (60). Men should control their tobacco and alcohol consumption and adopt a healthy diet (61), while women should avoid extreme dieting and focus on postpartum weight management. For older adults, prioritizing smoking cessation, balanced nutrition, and regular exercise can slow age-related declines in cardiovascular function (62). Additionally, at the global level, equitable access to new drugs such as glucagon-like peptide-1 receptor agonists should be promoted (63), and costs should be reduced through technological innovation to benefit low income countries and regions.
China, as a populous nation with a large population base, has the world's highest number of people who are overweight or obese. The China Nutrition and Chronic Disease Report (2020) indicates that among residents aged 18 and above, the rates of overweight and obesity are 34.3% and 16.4%, respectively, with the combined overweight and obesity rate among adults exceeding half (50.7%). The World Obesity Atlas 2024, released by the World Obesity Federation, indicates that China's overweight and obese adult population is projected to grow at an annual rate of 2.8%. By 2030, obesity-related healthcare expenditures in China are expected to account for approximately 22% of the nation's total medical costs, significantly impacting both livelihood and economy (64, 65). By 2030, the rates of overweight and obesity among adults in China is projected to reach 70.5%. Based on the 2024 edition of the Weight Management Guidelines, China has established a standardized weight management protocol for adults, primarily focusing on diet and exercise. Dietary recommendations for overweight and obese individuals are set at 85% and 80% of intake standards, respectively, based on individual basal metabolic rates and actual energy requirements corresponding to physical activity levels. Staple foods should primarily consist of whole grains, with reduced consumption of high-sugar, high-fat, and high-salt foods. Alcohol intake should be strictly limited, and meals should be consumed at regular times and in consistent quantities. Regarding physical activity, overweight and obese individuals should prioritize fat loss as the primary goal and learn mass maintenance as the secondary goal. This involves engaging in prolonged, moderate-to-low intensity aerobic exercise combined with resistance training, performed once or twice daily (66). The standardized weight management protocols for adults developed in China offer valuable reference points for other developing countries in terms of exercise and dietary recommendations.
This study has certain limitations. Regarding data sources, it primarily relies on a single source—GBD 2023—which has limited sample coverage and insufficient representativeness. Additionally, the data suffers from temporal lag and information gaps, affecting the robustness of conclusions. In terms of analytical methods, the use of before-and-after comparisons and Joinpoint analysis for APC calculations lacks explanatory power regarding deep causal relationships between variables and dynamic evolutionary processes. Regarding research content, specific weight management recommendations were not provided for overweight and obese populations across different genders, age groups, or countries and territories. Given the variations in national contexts, cultural practices, and dietary habits worldwide, we only offered general advice on exercise and diet suitable for most individuals.
In future related research, a hybrid data system combining “primary research + multi-source database integration + big data scraping” can be established to expand sample coverage. Research boundaries should be broadened to incorporate diverse subjects and external influencing factors, while adding cross-temporal and spatial comparison dimensions to deepen core issues. Integrating qualitative and quantitative methods alongside interdisciplinary technologies will enhance the scientific rigor and explanatory power of conclusions.
5 Conclusion
High BMI significantly contributes to the global burden of CVDs, with disparities in impact across gender, age, and regions, particularly severe in upper-middle income countries and regions with middle SDI. To combat this, comprehensive measures are needed, including health education, lifestyle promotion, disease surveillance, and early diagnosis and treatment, especially in lower-middle income countries and regions. International cooperation is crucial to achieving Sustainable Development Goal 3.4, reducing premature death from non-communicable diseases. Future research should explore factors influencing the global burden of CVDs due to high BMI, assess prevention measures, and inform global health strategies.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
MS: Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Investigation, Methodology, Resources, Visualization. YS: Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Investigation, Methodology, Resources, Visualization. NL: Writing – review & editing, Data curation, Formal analysis. ZZ: Writing – review & editing, Data curation, Formal analysis. JL: Writing – review & editing, Data curation, Formal analysis. ZC: Writing – original draft. DL: Writing – original draft. RT: Writing – original draft, Writing – review & editing, Conceptualization, Funding acquisition, Project administration, Supervision, Validation.
Funding
The author(s) declared that financial support was received for this work and/or its publication. The authors would like to acknowledge the National Natural Science Foundation of China (81700055, RT); the Outstanding Talent Research Funding of Xuzhou Medical University (D2016021, RT); the Natural Science Foundation of Jiangsu Province (BK20160229, RT); Jiangsu Province College Students' Innovative Entrepreneurial Training Plan Program (202310313127Y); Postdoctoral degree foundation of Xuzhou Medical University (RC5052112).
Conflict of interest
The author(s) declared that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declared that generative AI was not used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2026.1689708/full#supplementary-material
References
1. Organization WH. Cardiovascular diseases (CVDs) (2025). Available online at: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (Accessed December 30, 2025).
2. Lobstein T, Powis J, Jackson-Leach R. World obesity atlas 2024 (2024). Available online at: https://s3-eu-west-1.amazonaws.com/wof-files/WOF_Obesity_Atlas_2024.pdf (Accessed January 01, 2026).
3. Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet. (2011) 377:557–67. doi: 10.1016/s0140-6736(10)62037-5
4. Garland JS. Elevated body mass index as a risk factor for chronic kidney disease: current perspectives. Diabetes Metab Syndr Obes. (2014) 7:347–55. doi: 10.2147/dmso.S46674
5. Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. (2012) 70:3–21. doi: 10.1111/j.1753-4887.2011.00456.x
6. Koskinas KC, Van Craenenbroeck EM, Antoniades C, Blüher M, Gorter TM, Hanssen H, et al. Obesity and cardiovascular disease: an ESC clinical consensus statement. Eur Heart J. (2024) 45:4063–98. doi: 10.1093/eurheartj/ehae508
7. Zhu S, Gao J, Zhang L, Wanguo SW, Heng G, Tianfeng H, et al. Global, regional, and national cardiovascular disease burden attributable to smoking from 1990 to 2021: findings from the GBD 2021 study. Tob Induc Dis. (2025) 23:11. doi: 10.18332/tid/200072
8. Tan SCW, Zheng BB, Tang ML, Chu H, Zhao Y-T, Weng C. Global burden of cardiovascular diseases and its risk factors, 1990–2021: a systematic analysis for the global burden of disease study 2021. QJM. (2025) 118:411–22. doi: 10.1093/qjmed/hcaf022
9. Lee H, Rhee TM, Choi JM, Kim DW. The close link between obesity and cardiovascular disease: current insights and remaining challenges. Endocrinol Metab Clin North Am. (2025) 54:175–92. doi: 10.1016/j.ecl.2024.10.005
10. Collaborators GRF. Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990–2021: a systematic analysis for the global burden of disease study 2021. Lancet. (2024) 403:2162–203. doi: 10.1016/s0140-6736(24)00933-4
11. Zhang H, Zheng X, Huang P, Guo L, Ma X. The burden and trends of heart failure caused by ischemic heart disease at the global, regional, and national levels from 1990 to 2021. Eur Heart J Qual Care Clin Outcomes. (2024) 11:186–96. doi: 10.1093/ehjqcco/qcae094
12. Zhang MN, Li MT, Zhi XY, Zhu H, Zhang X, Xie J. Trends of a burden on atherosclerotic cardiovascular disease and its related risk factors in China, 1990 to 2019. Zhonghua Liu Xing Bing Xue Za Zhi. (2021) 42:1797–803. doi: 10.3760/cma.j.cn112338-20201208-01390
13. Wang Y, Li Q, Bi L, Lv T, Zhang P. Global trends in the burden of ischemic heart disease attributable to smoking from 1990 to 2021: a systematic analysis of the global burden of disease study 2021. Tob Induc Dis. (2025) 23(January):7. doi: 10.18332/tid/199931
14. Hall JE, da Silva AA, do Carmo JM, Dubinion J, Hamza S, Munusamy S, et al. Obesity-induced hypertension: role of sympathetic nervous system, leptin, and melanocortins. J Biol Chem. (2010) 285:17271–6. doi: 10.1074/jbc.R110.113175
15. Frohlich ED. Cardiac hypertrophy in hypertension. N Engl J Med. (1987) 317:831–3. doi: 10.1056/nejm198709243171310
16. Xu RY, Zhou YQ, Zhang XM, Wan YP, Gao X. Body mass index, waist circumference, body fat mass, and risk of developing hypertension in normal-weight children and adolescents. Nutr Metab Cardiovasc Dis. (2018) 28:1061–6. doi: 10.1016/j.numecd.2018.05.015
17. Williams PT. Increases in weight and body size increase the odds for hypertension during 7 years of follow-up. Obesity (Silver Spring). (2008) 16:2541–8. doi: 10.1038/oby.2008.396
18. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/national heart, lung, and blood institute scientific statement. Circulation. (2005) 112:2735–52. doi: 10.1161/circulationaha.105.169404
19. Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association scientific statement on obesity and heart disease from the obesity committee of the council on nutrition, physical activity, and metabolism. Circulation. (2006) 113:898–918. doi: 10.1161/circulationaha.106.171016
20. Yusuf S, Hawken S, Ôunpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. (2004) 364:937–52. doi: 10.1016/s0140-6736(04)17018-9
21. Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood). (2009) 28:w822–31. doi: 10.1377/hlthaff.28.5.w822
22. Wang Z, Liu J, Chen Y, Tang Y, Chen T, Zhou C, et al. From physiology to pathology: emerging roles of GPER in cardiovascular disease. Pharmacol Ther. (2025) 267:108801. doi: 10.1016/j.pharmthera.2025.108801
23. Qu S, Zhang Z, Ju R, Leng J, Xue Z, Tao S, et al. Association between the female hormone intake and cardiovascular disease in the women: a study based on NHANES 1999–2020. BMC Public Health. (2024) 24:3578. doi: 10.1186/s12889-024-21001-x
24. Manson JE, Woodruff TK. Reproductive health as a marker of subsequent cardiovascular disease: the role of estrogen. JAMA Cardiol. (2016) 1:776–7. doi: 10.1001/jamacardio.2016.2662
25. Du Z, Zhu W, Zhao Y, Liu S, Chu H, Sun Z, et al. The epidemic of stroke mortality attributed to high body mass index in mainland China: current trends and future prediction. Front Public Health. (2022) 10:1021646. doi: 10.3389/fpubh.2022.1021646
26. Javed F, Aziz EF, Sabharwal MS, Nadkarni GN, Khan SA, Cordova JP, et al. Association of BMI and cardiovascular risk stratification in the elderly African-American females. Obesity (Silver Spring). (2011) 19:1182–6. doi: 10.1038/oby.2010.307
27. Zhou M, Offer A, Yang G, Smith M, Hui G, Whitlock G, et al. Body mass index, blood pressure, and mortality from stroke: a nationally representative prospective study of 212,000 Chinese men. Stroke. (2008) 39:753–9. doi: 10.1161/strokeaha.107.495374
28. Chen Y, Yu W, Lv J, Sun D, Pei P, Yang L, et al. Early adulthood BMI and cardiovascular disease: a prospective cohort study from the China Kadoorie biobank. Lancet Public Health. (2024) 9:e1005–e13. doi: 10.1016/s2468-2667(24)00043-4
29. Zhou XD, Chen QF, Yang W, Zuluaga M, Targher G, Byrne CD, et al. Burden of disease attributable to high body mass index: an analysis of data from the global burden of disease study 2021. EClinicalMedicine. (2024) 76:102848. doi: 10.1016/j.eclinm.2024.102848
30. Monteiro CA, Moubarac JC, Cannon G, Popkin B. Ultra-processed products are becoming dominant in the global food system. Obes Rev. (2013) 14:21–8. doi: 10.1111/obr.12107
31. Tian Y, Zhao Z, Cao X, Kang Y, Wang L, Yin P, et al. Rapid increasing burden of diabetes and cardiovascular disease caused by high body mass index in 1.25 million Chinese adults, 2005–2018. Med. (2023) 4:505–25.e3. doi: 10.1016/j.medj.2023.05.008
32. Khan SS, Ning H, Wilkins JT, Allen N, Carnethon M, Berry JD, et al. Association of body mass index with lifetime risk of cardiovascular disease and compression of morbidity. JAMA Cardiol. (2018) 3:280–7. doi: 10.1001/jamacardio.2018.0022
33. Mozaffarian D, Afshin A, Benowitz NL, Bittner V, Daniels SR, Franch HA, et al. Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation. (2012) 126:1514–63. doi: 10.1161/CIR.0b013e318260a20b
34. Saltiel AR, Kahn CR. Insulin signalling and the regulation of glucose and lipid metabolism. Nature. (2001) 414:799–806. doi: 10.1038/414799a
35. Steven S, Frenis K, Oelze M, Kalinovic S, Kuntic M, Bayo Jimenez MT, et al. Vascular inflammation and oxidative stress: major triggers for cardiovascular disease. Oxid Med Cell Longev. (2019) 2019:7092151. doi: 10.1155/2019/7092151
36. Balaji S, DiLorenzo MP, Fish FA, Etheridge SP, Aziz PF, Russell MW, et al. Impact of obesity on left ventricular thickness in children with hypertrophic cardiomyopathy. Pediatr Cardiol. (2019) 40:1253–7. doi: 10.1007/s00246-019-02145-9
37. Powell-Wiley TM, Poirier P, Burke LE, Després J-P, Gordon-Larsen P, Lavie CJ, et al. Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. (2021) 143:e984–e1010. doi: 10.1161/cir.0000000000000973
38. Güven B, Sun Q, Wagg CS, Almeida de Oliveira A, Silver H, Persad KL, et al. Obesity is a major determinant of impaired cardiac energy metabolism in heart failure with preserved ejection fraction. J Pharmacol Exp Ther. (2024) 388:145–55. doi: 10.1124/jpet.123.001791
39. Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. (2005) 111:1233–41. doi: 10.1161/01.Cir.0000158136.76824.04
40. Sun N, Jia X, Shi X, Jiang F, Yang C, Yang Y, et al. A global decomposition analysis of the effect of population aging on disability-adjusted life years associated with cardiovascular disease—204 countries and territories, 1990–2021. China CDC wkly. (2024) 6:1004–10. doi: 10.46234/ccdcw2024.209
41. Govindarajan G, Whaley-Connell A, Mugo M, Stump C, Sowers JR. The cardiometabolic syndrome as a cardiovascular risk factor. Am J Med Sci. (2005) 330:311–8. doi: 10.1097/00000441-200512000-00009
42. Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Miller NH, Hubbard VS, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American college of cardiology/American heart association task force on practice guidelines. Circulation. (2014) 129:S76–99. doi: 10.1161/01.cir.0000437740.48606.d1
43. Agarwal K, Demiral SB, Manza P, Volkow ND, Joseph PV. Relationship between BMI and alcohol consumption levels in decision making. Int J Obes. (2021) 45:2455–63. doi: 10.1038/s41366-021-00919-x
44. Butler L, Popkin BM, Poti JM. Associations of alcoholic beverage consumption with dietary intake, waist circumference, and body mass index in us adults: national health and nutrition examination survey 2003–2012. J Acad Nutr Diet. (2018) 118:409–20.e3. doi: 10.1016/j.jand.2017.09.030
45. Liu C, Zhang Z. Assessing the health impact of low seafood omega-3 intake on ischemic heart disease: trends, demographic disparities, and forecasts. Eur Heart J Qual Care Clin Outcomes. (2025) 11:792–805. doi: 10.1093/ehjqcco/qcaf006
46. Whayne TF Jr. Ischemic heart disease and the Mediterranean diet. Curr Cardiol Rep. (2014) 16:491. doi: 10.1007/s11886-014-0491-6
47. Miller B, Chalfant H, Thomas A, Wellberg E, Henson C, McNally MW, et al. Diabetes, obesity, and inflammation: impact on clinical and radiographic features of breast cancer. Int J Mol Sci. (2021) 22:2757. doi: 10.3390/ijms22052757
48. Ryder JR, Xu P, Inge TH, Xie C, Jenkins TM, Hur C, et al. Thirty-year risk of cardiovascular disease events in adolescents with severe obesity. Obesity (Silver Spring). (2020) 28:616–23. doi: 10.1002/oby.22725
49. Reddy YNV, Tada A, Obokata M, Carter RE, Kaye DM, Handoko ML, et al. Evidence-based application of natriuretic peptides in the evaluation of chronic heart failure with preserved ejection fraction in the ambulatory outpatient setting. Circulation. (2025) 151(14):976–89. doi: 10.1161/circulationaha.124.072156
50. Peikert A, Vaduganathan M, Claggett BL, Kulac IJ, Litwin S, Zile M, et al. Near-universal prevalence of central adiposity in heart failure with preserved ejection fraction: the PARAGON-HF trial. Eur Heart J. (2025) 46:2372–90. doi: 10.1093/eurheartj/ehaf057
51. Butt JH, Petrie MC, Jhund PS, Sattar N, Desai AS, Køber L, et al. Anthropometric measures and adverse outcomes in heart failure with reduced ejection fraction: revisiting the obesity paradox. Eur Heart J. (2023) 44:1136–53. doi: 10.1093/eurheartj/ehad083
52. Tjeertes EK, Hoeks SE, Beks SB, Valentijn TTM, Hoofwijk AAGM, Stolker RJRJ. Obesity–a risk factor for postoperative complications in general surgery? BMC Anesthesiol. (2015) 15:112. doi: 10.1186/s12871-015-0096-7
53. Capodaglio P, Cimolin V, Tacchini E, Parisio C, Galli M. Balance control and balance recovery in obesity. Curr Obes Rep. (2012) 1:166–73. doi: 10.1007/s13679-012-0018-7
54. O'Brien PD, Hinder LM, Callaghan BC, Eva L. Neurological consequences of obesity. Lancet Neurol. (2017) 16:465–77. doi: 10.1016/s1474-4422(17)30084-4
56. Zhang L, Zou W, Hu Y, Wu H, Gao Y, Zheng J. Voluntary wheel running ameliorated the deleterious effects of high-fat diet on glucose metabolism, gut microbiota and microbial-associated metabolites. Food Science and Human Wellness. (2024) 13:1672–84. doi: 10.26599/FSHW.2022.9250142
57. Müller TD, Blüher M, Tschöp MH, DiMarchi RD. Anti-obesity drug discovery: advances and challenges. Nat Rev Drug Discov. (2022) 21:201–23. doi: 10.1038/s41573-021-00337-8
58. Chiu C, Omaya M, Uwinkindi F, Tang D, Mwubahamana S, Miller F, et al. Pharmacy-based non-communicable diseases screening has high potential for reach: lessons from Rwanda. Front Public Health. (2025) 13:1684688. doi: 10.3389/fpubh.2025.1684688
59. WHO. How can cities shape up? Encouraging healthy diets and active lifestyles in urban environments (2022). Available online at: https://www.who.int/europe/news/item/31-08-2022-how-can-cities-shape-up-encouraging-healthy-diets-and-active-lifestyles-in-urban-environments#:∼:text=A%20new%20report%20prepared%20by%20WHO%2FEurope%20in%20collaboration,and%20well-being%20at%20the%20centre%20of%20city%20planning (Accessed January 01, 2026).
60. Nally S, Carlin A, Blackburn N, Baird J, Salmon J, Murphy M, et al. The effectiveness of school-based interventions on obesity-related behaviours in primary school children: a systematic review and meta-analysis of randomised controlled trials. Children. (2021) 8:489. doi: 10.3390/children8060489
61. Najman JM, Kisely S, Scott JG, Ushula TW, Williams GM, Clavarino AM, et al. Gender differences in cardiovascular disease risk: adolescence to young adulthood. Nutr Metab Cardiovasc Dis. (2024) 34:98–106. doi: 10.1016/j.numecd.2023.09.024
62. Townsend N, Timmis A, Erglis A, Miličić D, Perrone-Filardi P, Weidinger F, et al. Challenges in the prevention, treatment and management of cardiovascular disease among older adults. Lancet Reg Health—Eur. (2025) 56:101372. doi: 10.1016/j.lanepe.2025.101372
63. Schutte AE. Addressing obesity and subsequent cardiovascular risk in primary care: the relevance of high- and low-resource settings. Cardiovasc Res. (2025) 121:1135–7. doi: 10.1093/cvr/cvaf094
64. Sun X, Yan AF, Shi Z, Zhao B, Li K, Gao L, et al. Health consequences of obesity and projected future obesity health burden in China. Obesity (Silver Spring). (2022) 30:1724–51. doi: 10.1002/oby.23472
65. Obesity W. Obesity Atlas 2024 (2024). Available online at: https://data.worldobesity.org/publications/?cat=22 (Accessed January 02, 2026).
Keywords: body mass index, cardiovascular diseases, disability-adjusted life years, global burden of disease, regional disparities
Citation: Sun M, Shi Y, Li N, Zhou Z, Luo J, Chen Z, Lin D and Tan R (2026) The global burden of cardiovascular diseases attributable to high body mass index, 1990–2023. Front. Cardiovasc. Med. 13:1689708. doi: 10.3389/fcvm.2026.1689708
Received: 21 August 2025; Revised: 10 January 2026;
Accepted: 26 January 2026;
Published: 13 February 2026.
Edited by:
Abbas F. Almulla, Chulalongkorn University, ThailandReviewed by:
Vibha Sinha, Guru Ghasidas Vishwavidyalaya, IndiaShuyi Wu, Fujian Provincial Cancer Hospital, China
Copyright: © 2026 Sun, Shi, Li, Zhou, Luo, Chen Z, Lin and Tan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rubin Tan, dGFucnViaW4xMUAxMjYuY29t
†These authors have contributed equally to this work
 Manqi Sun
Manqi Sun Yue Shi2,†
Yue Shi2,† Rubin Tan
Rubin Tan