- 1Department of Cardiology, The First Hospital of Hebei Medical University, Shijiazhuang, Hebei, China
- 2Department of Cardiology, Beijing Genertec Aerospace Hospital, Beijing, China
Background: Radial artery pseudoaneurysm (RAP) is an uncommon but significant complication after transradial coronary procedures. This case demonstrates the efficacy of ultrasound-guided thrombin injection (UGTI) as a minimally invasive treatment.
Case presentation: A 65-year-old Chinese male developed a RAP two days after percutaneous coronary intervention. Diagnosis was confirmed by Doppler ultrasound. UGTI was performed, injecting 1.5 mL of thrombin. Complete thrombosis occurred within 30 s, with sustained occlusion confirmed at 24-hour follow-up.
Conclusions: UGTI is a highly effective and safe first-line treatment for iatrogenic RAP, enabling rapid resolution and avoiding the need for surgery. It represents a superior minimally invasive strategy for managing this vascular complication.
Introduction
Radial artery access has gained widespread preference over femoral access for coronary angiography and percutaneous coronary intervention (PCI) due to its association with fewer vascular complications, reduced bleeding risks, and enhanced patient comfort (1). Nonetheless, vascular complications such as radial artery pseudoaneurysm (RAP) may still occur, particularly among elderly patients with comorbidities such as atherosclerosis and hypertension (2, 3). RAP typically manifests as a painful, pulsatile mass at the puncture site and may lead to serious sequelae including nerve compression, distal ischemia, or rupture if left untreated (4, 5).
The management of RAP has evolved from primarily surgical repair, once considered a definitive treatment, to a spectrum of strategies including prolonged external compression, ultrasound-guided thrombin injection (UGTI), and endovascular exclusion techniques (6, 7). Small-neck pseudoaneurysms are often amenable to conservative or minimally invasive approaches, whereas those with wider necks or symptoms of compression may require more aggressive intervention (8, 9). UGTI, initially established for femoral pseudoaneurysms, has been increasingly applied in radial artery cases due to its minimally invasive nature and high technical success rates (10). However, its safety profile necessitates careful patient selection and operator expertise to avoid complications such as distal thromboembolism or radial artery occlusion (11). This case report illustrates the successful application of UGTI for a small-neck RAP in a 65-year-old male following coronary PCI, and discusses its role within contemporary treatment algorithms.
Case presentation
A 65-year-old Chinese male with a medical history of hypertension, dyslipidemia, and coronary artery disease was admitted due to unstable angina. Coronary angiography performed via right transradial access revealed significant triple-vessel disease, and PCI with drug-eluting stent implantation was successfully conducted. The procedure was uncomplicated, and hemostasis was achieved using a TR compression band device. On postoperative day 2, the patient reported swelling and tenderness at the right wrist. Physical examination identified a 2.5 × 2 cm pulsatile, tender mass with an audible bruit. Doppler ultrasonography confirmed the diagnosis of radial artery pseudoaneurysm, characterized by a narrow neck (2 mm) and a classic yin-yang flow pattern (Figure 1). After obtaining informed consent, UGTI was performed under continuous ultrasound guidance. A 21-gauge needle was used to inject 1.5 mL of purified human thrombin (500 IU/mL) into the pseudoaneurysm sac. Complete thrombosis occurred within 30 s (Figure 2). Post-procedurally, the mass became non-pulsatile, and follow-up ultrasound at 24 h confirmed sustained occlusion without recurrence (Figure 3). The patient remained asymptomatic and free of neurological or vascular complications.
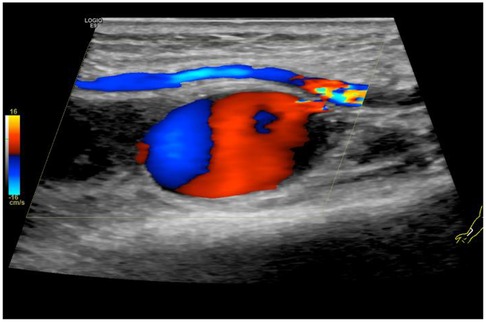
Figure 1. Doppler ultrasound of the right wrist was carried out, which confirmed the diagnosis of pseudoaneurysm of radial artery.
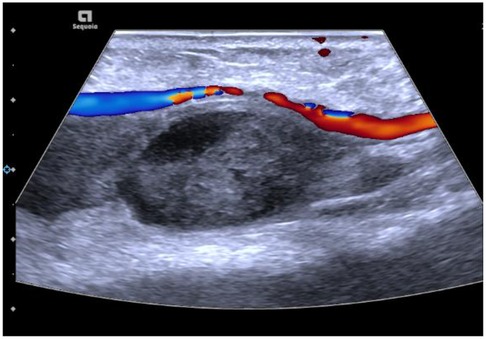
Figure 2. Ultrasound-guided injection of 1.5 mL of thrombin via a 21G needle. Immediate post-injection complete thrombosis on ultrasound imaging.
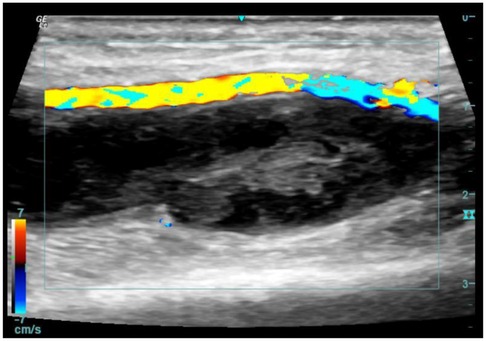
Figure 3. Ultrasound demonstrated sustained occlusion without evidence of recurrence at 24 h post-injection.
Discussion and conclusions
This case highlights the successful use of UGTI in managing iatrogenic RAP following transradial PCI, yet it also underscores the importance of appropriate patient selection and procedural nuance. Although RAP is uncommon, risk factors include advanced age, aggressive anticoagulation, and multiple puncture attempts. Traditional management options range from conservative measures such as prolonged external compression, often first-line for small, asymptomatic lesions, to surgical repair for larger or symptomatic aneurysms (12, 13).
As a superior alternative, UGTI offers a highly effective, minimally invasive approach, particularly in cases of narrow-necked pseudoaneurysms where compression therapy has failed. Critical technical considerations include precise needle placement within the aneurysm sac under continuous ultrasound guidance, avoiding injection into the neck or native artery to prevent distal thromboembolism (14). In our case, the pseudoaneurysm measured 2.5 × 2 cm with a 2 mm neck, making it suitable for UGTI. The procedure was performed by an interventional cardiologist with expertise in vascular ultrasound, in collaboration with a vascular radiologist, reflecting the multidisciplinary approach recommended for such interventions.
Despite its efficacy, UGTI is not without risks. Reported complications include thrombosis, distal embolism, allergic reactions to thrombin, and recurrence (11, 15). Therefore, UGTI should be considered after failure of conservative measures or when compression is deemed unlikely to succeed, rather than as a universal first-line option. Long-term follow-up is advised to monitor for recurrence, although most successfully thrombosed pseudoaneurysms remain stable.
In conclusion, UGTI represents a valuable minimally invasive strategy for managing eligible radial artery pseudoaneurysms, particularly those with narrow necks and symptomatic presentation. Its integration into clinical practice should be guided by lesion morphology, operator experience, and a balanced understanding of its risks and benefits, consistent with current guidelines that advocate for personalized, stepwise management of vascular complications.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
XL: Data curation, Writing – original draft. GQ: Data curation, Writing – original draft. LW: Writing – original draft, Funding acquisition, Writing – review & editing.
Funding
The author(s) declared that financial support was received for this work and/or its publication. This study was supported by the Hebei Provincial Administration of Traditional Chinese Medicine Research Foundation (Grant No. 2024266).
Acknowledgments
The authors would like to thank the nursing and ultrasonography staff of the Department of Cardiology for their excellent assistance and support in the management of this case.
Conflict of interest
The author(s) declared that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declared that generative AI was not used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Krittanawong C, Uppalapati L, Virk HUH, Qadeer YK, Irshad U, Wang Z, et al. Complications of radial vs femoral access for coronary angiography and intervention: what do the data tell US? Am J Med. (2024) 137(6):483–9. doi: 10.1016/j.amjmed.2024.02.022
2. Din JN, Murphy A, Chu K, Forman P, Mildenberger RD, Fretz EB, et al. Radial artery pseudoaneurysms after transradial cardiac catheterisation. Vasa. (2016) 45(3):229–32. doi: 10.1024/0301-1526/a000529
3. Roy S, Kabach M, Patel DB, Guzman LA, Jovin IS. Radial artery access complications: prevention, diagnosis and management. Cardiovasc Revasc Med. (2022) 40:163–71. doi: 10.1016/j.carrev.2021.12.007
4. Lee L, Blair J, Gupta S, Nathan S. Upper extremity vascular complications following transradial approach for cardiac catheterization and intervention: a focused review of diagnostic, prognostic and therapeutic considerations. Minerva Cardioangiol. (2016) 64(6):648–61.27175978
5. Mizuta H, Fujikawa H, Motomura H. Infected pseudoaneurysm of the radial artery. Arch Plast Surg. (2023) 50(3):325–8. doi: 10.1055/a-2039-3563
6. Gallinoro E, Natale F, D’Elia S, Golino P, Cimmino G. Radial pseudoaneurysm in elderly: a rare event with undefinied therapeutical approach. A case report and literature review. Monaldi Arch Chest Dis. (2019) 89(3):1109. doi: 10.4081/monaldi.2019.1109
7. Alqahtani NG. Radial artery pseudoaneurysm a rare complication after coronary angiography: a case report and systematic review of the reported cases. Clin Case Rep. (2024) 12(4):e8725. doi: 10.1002/ccr3.8725
8. Bortolini E, Leite TFO, Linard BRRG, Affonso BB, Nomura CH, Motta-Leal-Filho JMD. Ultrasound-guided thrombin injection for cardiac catheterization pseudoaneurysms: efficacy, safety, and predictors. Acta Radiol. (2025) 66(1):62–71. doi: 10.1177/02841851241292516
9. de Oliveira Leite TF, Bortolini E, Linard B, Boueri BA, Carnevale FC, Nomura CH, et al. Evaluation of morphological and clinical factors related to failure of percutaneous treatment with thrombin injection of femoral pseudoaneurysms from cardiac catheterization. Ann Vasc Surg. (2019) 59:173–83. doi: 10.1016/j.avsg.2019.01.013
10. Augustine MR, Atwell TD, Jundt MC, Schaller MS, Hibbert B, Schmitz JJ. Percutaneous ultrasound-guided thrombin injection for radial artery pseudoaneurysms. J Vasc Interv Radiol. (2025) 36(7):1224–6. doi: 10.1016/j.jvir.2025.03.019
11. Pająk M, Hasiura R, Stępień T. Safety evaluation of percutaneous ultrasound-guided thrombin injection into pseudoaneurysms. Pol Przegl Chir. (2019) 91(2):20–4. doi: 10.5604/01.3001.0012.8613
12. Nazer B, Boyle A. Treatment of recurrent radial artery pseudoaneurysms by prolonged mechanical compression. J Invasive Cardiol. (2013) 25(7):358–9.23813066
13. Tosti R, Özkan S, Schainfeld RM, Eberlin KR. Radial artery pseudoaneurysm. J Hand Surg Am. (2017) 42(4):295.e1–e6. doi: 10.1016/j.jhsa.2017.01.024
14. Hanson JM, Atri M, Power N. Ultrasound-guided thrombin injection of iatrogenic groin pseudoaneurysm: doppler features and technical tips. Br J Radiol. (2008) 81(962):154–63. doi: 10.1259/bjr/52029321
15. Willaert W, Petrovic M, Van Herzeele I, Randon C, Voet D, Vermassen F. Behandeling van iatrogene femorale pseudoaneurysmata door middel van echogeleide percutane trombine-injectie: doeltreffendheid en complicaties [treatment of iatrogenic femoral pseudoaneurysms by ultrasound-guided percutaneous thrombin injection: effectiveness and complications]. Acta Clin Belg. (2006) 61(1):19–23. doi: 10.1179/acb.2006.004
Keywords: complication, percutaneous coronary intervention, radial artery pseudoaneurysm, thrombosis, ultrasound-guided thrombin injection
Citation: Li X, Qi G and Wei L (2026) Case Report: Ultrasound-guided thrombin injection for the treatment of radial artery pseudoaneurysm after percutaneous coronary intervention. Front. Cardiovasc. Med. 13:1753285. doi: 10.3389/fcvm.2026.1753285
Received: 3 December 2025; Revised: 29 December 2025;
Accepted: 19 January 2026;
Published: 9 February 2026.
Edited by:
Gregor Leibundgut, University Hospital of Basel, SwitzerlandReviewed by:
Giuseppe Colletti, Cliniques du Sud-Luxembourg, BelgiumClaudiu Ungureanu, Hôpital de Jolimont, Belgium
Copyright: © 2026 Li, Qi and Wei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liye Wei, d2VpbGl5ZTEzMjBAaGVibXUuZWR1LmNu
 Xiaoyan Li1
Xiaoyan Li1 Liye Wei
Liye Wei