- 1Department of Joint Surgery, The First Affiliated Hospital of Sun Yat-Sen University, Guangzhou, China
- 2Guangdong Provincial Key Laboratory of Orthopedics and Traumatology, The First Affiliated Hospital of Sun Yat-Sen University, Guangzhou, China
- 3Department of Orthopaedics, West China Hospital, Sichuan University, Chengdu, China
Background: Previous studies have identified some risk factors of dislocation after total hip arthroplasty (THA). However, there are many vital preoperative patient risk factors remaining unknown. This study aimed to investigate comprehensively patient risk factors to reduce the dislocation rate after THA.
Methods: We retrospectively reviewed patients who underwent primary THA in our department between January 2016 to December 2020. All readmissions related to postoperative dislocation were recorded, and each patient who dislocated was matched with three patients who did not dislocate according to date of operation, operative time and follow-up time. Patient risk factors were initially analyzed by univariate analyses, and independent risk factors for dislocation were identified by multivariate logistic regression.
Results: A total of 5,133 patients were reviewed and 76 patients were readmitted with postoperative dislocations in follow-up time (1.5%). Age (odds ratio [OR], 1.027; 95% confidence interval [CI], 1.000–1.055; P = 0.049), rheumatoid arthritis (OR, 7.976; 95% CI, 1.419–44.827; P = 0.018), low serum calcium level (OR, 0.009; 95% CI, 0.000–0.211; P = 0.003) and poor education degree (OR, 0.847; 95% CI, 0.770–0.932; P = 0.001) were determined as independent predictors associated with dislocation after THA.
Conclusion: Patients with older age, rheumatoid arthritis, low serum calcium level, and poor education degree require targeted optimization of preoperative planning and should be performed by appropriate surgical techniques and hip prostheses to prevent dislocation after THA and revision surgeries.
Introduction
Total hip arthroplasty (THA) is a common surgical procedure used to treat end-stage joint diseases that may cause severe pain, deformities and bodily dysfunction (Mercurio et al., 2020; Saiz et al., 2019). Although the improvement of prosthesis design and surgical techniques has reduced the incidence of dislocation after THA to 0.05%–3.9%, the volume of THA is also on the rise and dislocation remains one of the most common reasons for failure and indication for early revision (Saiz et al., 2019; Dargel et al., 2014; Ding et al., 2020; Buckland et al., 2017; Malkani et al., 2010; Liu et al., 2019; Rowan et al., 2018). Most patients with a first dislocation have an increased factor for multiple occurrences, and subsequent treatment including reduction and revision THA, would bring higher charges to the patient and more complex surgery procedure to surgeons (Rowan et al., 2018; Kotwal et al., 2009; Abdel et al., 2015). Therefore, reducing the risk of dislocation after THA is essential to the orthopedists and the healthcare system (Saiz et al., 2019; Rowan et al., 2018).
In order to prevent of dislocation, risk factors for postoperative instability need to be identified (Rowan et al., 2018). Etiology of dislocation after primary THA is multifactorial, and risk factors are generally divided into four categories: patient risk factors, surgical techniques, implant design and management strategies (Saiz et al., 2019). The main risk factors of dislocation that have been identified are as follows: 1) patient risk factors: neuromuscular and cognitive disorders including cerebral palsy, Parkinson disease and dementia, cognitive dysfunction from aging, alcoholism and psychiatric diseases, prior hip fractures or surgical procedures, spinopelvic malalignment from spinal arthrodeses (fusions), degeneration or deformities, and decreased compliance (Dargel et al., 2014; Meek et al., 2006; von Knoch et al., 2002; Perfetti et al., 2017; Sing et al., 2016; DelSole et al., 2017; Kanawade et al., 2014; Zeng et al., 2023); 2) surgical techniques: less-experienced surgeons, posterior approach, unnormal femoral offset, component malposition, soft tissue imbalance, abnormal combined anteversion and prosthesis impingement (Charney et al., 2020; Forde et al., 2018; Lewinnek et al., 1978; Nakashima et al., 2014; Miki et al., 2013; Vaishya et al., 2015; Hedlundh et al., 1996; Zhang et al., 2015; Ji et al., 2012); 3) implant factors: without use of the elevated or constrained liner in patients considered to be at high risk for dislocation, smaller-diameter femoral head (Gill et al., 2016; Pace et al., 2015; Girard et al., 2013; Hailer et al., 2012; Howie et al., 2012; Tidermark et al., 2003; Munro et al., 2013); and 4) management strategies including lack of preoperative education to patients (Peter et al., 2011).
Although many risk factors of dislocation after THA are universally acknowledged, most previous studies were focused on the surgical techniques and implant factors such as component malposition and soft tissue imbalance, and it is obvious that there are some unknown factors involved (Liu et al., 2019; Dorr et al., 1983). Before surgeons perform the surgery procedures, detailing the patient risk factors of dislocation after primary THA could help them evaluate optimal surgical techniques and prosthesis selection to provide the best treatment for patients and decrease the likelihood of dislocations following primary THA (Saiz et al., 2019).
Therefore, based on the hypothesis that there are some unknown patient risk factors of dislocation after primary THA, we conducted a retrospective study aimed to determine undetected patient risk factors to reduce the rate of postoperative dislocation.
Materials and methods
Ethics statements
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the institutional review board. Informed consent and patients’ consent to participate were obtained from all participants.
Cohort selection
All patients undergoing elective primary THA in our institution from January 2016 to December 2020 were reviewed retrospectively. Elective primary THA was defined by using International Classification of Disease-9th Edition (ICD-9) codes, and excluded patients with concomitant infection, hip fracture, tumor, or undergoing revision THA. A readmission that involved a hip dislocation or reduction of a hip dislocation was assessed as the primary outcome.
Surgical technique
All primary THAs were performed via a posterolateral approach by five senior surgeons who performed more than 200 total hip arthroplasties per year. The patient was placed in the lateral decubitus position and the skin of the hip was incised through the fascia above the greater trochanter. The gluteus maximus was then divided and the external rotators were isolated. The specific procedures in the posterolateral approach were as described previously (Li et al., 2022). The acetabular implant was expected to be positioned in the “safe zone” of 40° ± 10° abduction and 15° ± 10° anteversion (Lewinnek et al., 1978). The hip capsule and external rotators were repaired. Senior surgeons explained the postoperative precautions to the patient and family in detail. After surgery, patients were encouraged to take limb exercises early, especially to strengthen hip abduction function exercises, and to perform partial weight-bearing walking for about 2 weeks, and gradually resume full weight-bearing walking 4–6 weeks after surgery. Each patient was followed up for at least 6 months after discharge.
Statistical methods
All data management and statistical analyses were conducted using SPSS version 22.0 software (IBM Corp.). Continuous variables were calculated as means ± standard deviations, and they were analyzed using an independent Student’s t-test or a nonparametric test depending on normality of the data. Categorical variables were described as numbers and percentages. The Pearson chi-square test or Fisher exact test was used to analyze categorical variables according to whether the expected frequencies were greater than five. Univariate analyses were initially used to compare data between the dislocation group and the non-dislocation group. Then variables that had a p-value <0.1 in the univariate analyses were analyzed in a multivariate logistic regression analysis to determine independent patient risk factors for dislocation after THA. The significance level was set at p < 0.05.
Results
In total, 5,360 primary THAs (5,174 patients) were performed in our department between January 2016 to December 2020. Among those patients, there were 19 patients were lost to follow-up and 22 mortalities during the follow-up period. Ultimately, a total of 5,133 patients were reviewed and 76 patients were readmitted with postoperative dislocations in follow-up time (1.5%). Twenty-six of those patients had more than 1 readmission for dislocation (0.5% of all patients undergoing elective THAs, 34.2% of patients who are readmitted for dislocation). Each patient who dislocated was matched with three patients who did not dislocate according to date of operation, operative time and follow-up time. Therefore, 76 patients who dislocated were included in this study, and 228 patients who did not dislocate were identified as controls.
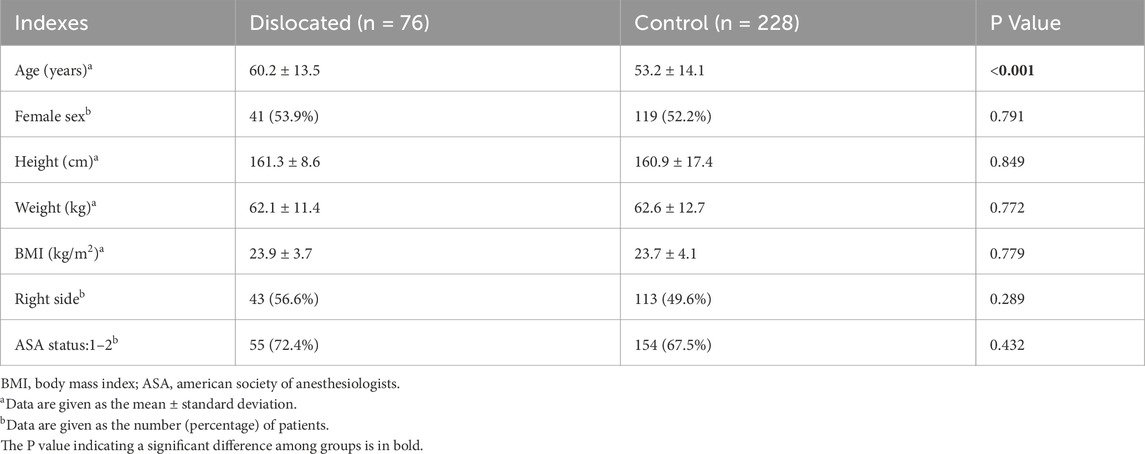
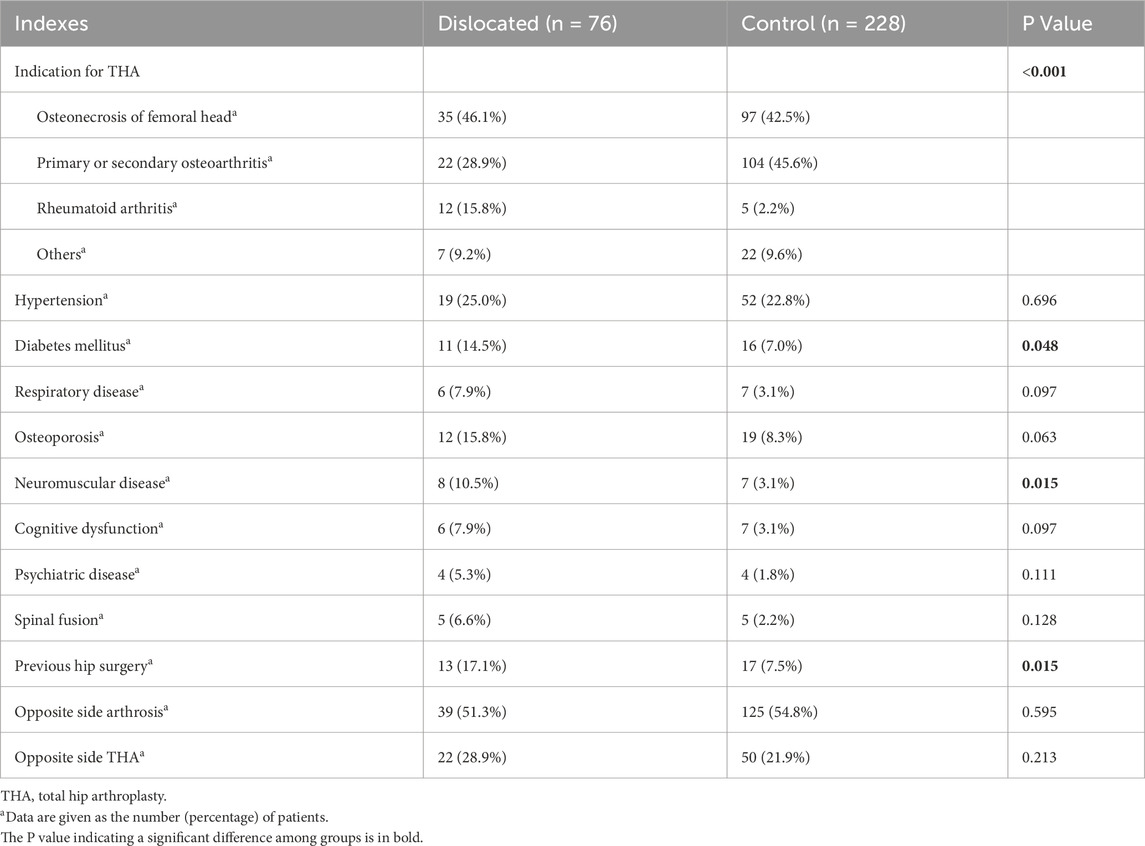
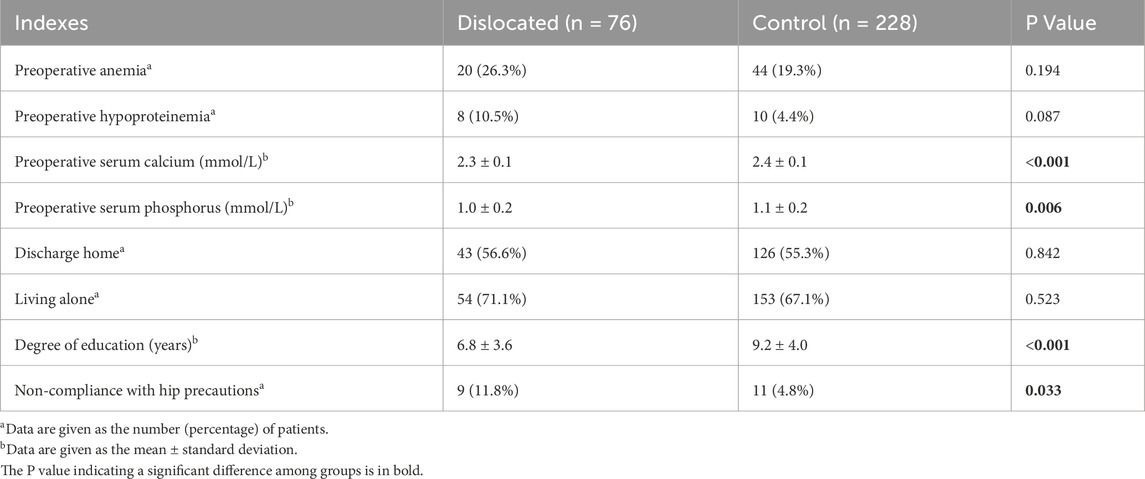
Table 1 demonstrates the demographic characteristics of the patients. On average, patients in the dislocated group had an older age (60.2 ± 13.5) than those (53.2 ± 14.1) in the control group (P < 0.001). There was no significant difference in sex, height, weight, body mass index (BMI), body side and American Society of Anesthesiologists (ASA) status. The variables regarding indication, comorbidities and surgical history are summarized in Table 2. There was a significant difference (P < 0.001) between two groups in the indication for THA, revealing that the disease type is a dislocation risk factor. Moreover, the dislocated group had significantly higher proportion of patients with diabetes mellitus (14.5% vs. 7.0%, P = 0.048), neuromuscular disease (10.5% vs. 3.1%, P = 0.015) and previous hip surgery (17.1% vs. 7.5%, P = 0.015) than the control group. The preoperative laboratory values and social support of patients for risk evaluation are summarized in Table 3. Patients who dislocated had significantly lower levels of serum calcium (2.3 ± 0.1 vs. 2.4 ± 0.1, P < 0.001) and phosphorus (1.0 ± 0.2 vs. 1.1 ± 0.2, P = 0.006) than those who did not experience a dislocation. Additionally, patients in the dislocated group had lower education degree and poorer compliance with hip precautions during the postoperative period than patients in the control group (P < 0.001 and = 0.033, respectively).
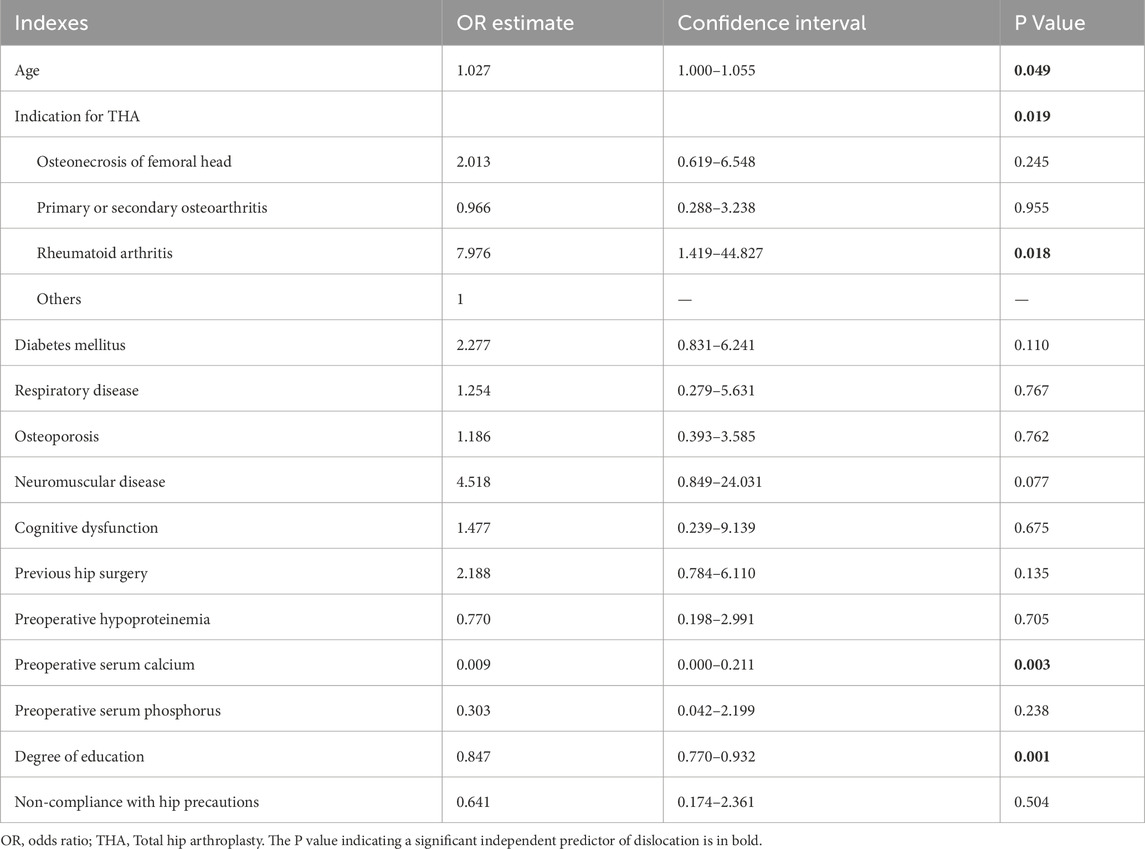
Then the multivariate logistic analysis was used to identify independent predictors of hip dislocation after THA (Table 4). Age was assessed and determined as an independent predictor associated with dislocation (odds ratio [OR], 1.027; 95% confidence interval [CI], 1.000–1.055; P = 0.049).The indication for the primary THA was a significant independent predictor of dislocation, as patients with rheumatoid arthritis had higher dislocation rates after adjusting for other variables (OR, 7.976; 95% CI, 1.419–44.827; P = 0.018). A lower serum calcium level was also related to increased risk of dislocation (OR, 0.009; 95% CI, 0.000–0.211; P = 0.003). Moreover, lower education degrees showed significantly higher risk of dislocation (OR, 0.847; 95% CI, 0.770–0.932; P = 0.001). Diabetes mellitus, respiratory disease, osteoporosis, neuromuscular disease, cognitive dysfunction, previous hip surgery, preoperative hypoproteinemia, serum phosphorus and non-compliance with hip precautions were not identified as independent risk factors of hip dislocation after THA in this multivariate logistic analysis.
Discussion
Dislocation following primary THA is a well-known and potentially devastating complication (Wright-Chisem et al., 2022). Since the introduction of THA, orthopedists provided a number of strategies to prevent dislocation (Wera et al., 2012). While modern surgical techniques, hip prosthesis and postoperative care have attracted much attention, particular emphasis should be placed on preoperative planning in the prevention of dislocation. This study aimed to identify comprehensively patient risk factors to assist orthopedists in the preoperative planning to evaluate optimal surgical techniques and prosthesis to reduce the risk of postoperative dislocations. The most important finding of this study was that patients with older age, indication for rheumatoid arthritis, low serum calcium level and poor education degree had higher risk of dislocation following THA. These patients require targeted optimization of preoperative planning and should be performed by appropriate surgical techniques and hip prostheses to prevent dislocation after THA and revision surgeries.
The overall dislocation rate in this study was 1.5%, which is lower than the 2.84% reported by Goel et al., in 2015, which was limited in the Medicare population over the study period (1997–2011) (Goel et al., 2015). The lower dislocation rate in this study can be attributed to the improvement of surgical techniques and prosthesis, while the additional emphasis is still required to further eliminate the dislocation rate.
In the previous literature, older age was generally considered as an independent risk factor for hip dislocation (Ding et al., 2020; Malkani et al., 2010; Rowan et al., 2018; Jørgensen et al., 2014; Malkani et al., 2017). This result may be attributed to the weakness of the abductor muscles in the elderly (Ding et al., 2020; Falez et al., 2017). However, the cutoff age for postoperative THA dislocation is not consistent in the previous studies (Esposito et al., 2015). In a retrospective review of 22,097 THAs, the authors found that patients aged over 70 years had a significantly higher rate of dislocation than those aged 50–69 years (Esposito et al., 2015). Our study also found that patients who dislocated were older than those who did not dislocate.
Patients with rheumatoid arthritis have a greater demand for THA than those without rheumatoid arthritis because the disease is characterized by joint destruction and bone erosion (Zhou et al., 2022). Our study found that rheumatoid arthritis was an independent risk factor for dislocation after THA, which is consistent with the results of a previous study published in 2023 (Jiang et al., 2023). The study included patients undergoing THA for rheumatoid arthritis or osteoarthritis at their hospital between 2011 and 2021, and demonstrated that patients with rheumatoid arthritis showed significantly higher rates of wound aseptic complications, hip prosthesis dislocation, homologous transfusion, and albumin use. Patients with rheumatoid arthritis have a high prevalence of small femoral head, acetabular protrusion, suboptimal hip abductor strength and soft tissue laxity, which cannot provide adequate posterolateral support for the hip prosthesis (Ravi et al., 2014). Moreover, cortical thinning associated with long-term corticosteroid use and bone loss in patients with rheumatoid arthritis may be linked to increased incidence of hip prosthesis dislocation (Zhu et al., 2015).
The major finding of our study was the new identification of two risk factors for dislocation: low serum calcium level and poor education degree. Calcium is the core component of bone matrix mineralization, which is essential for bone formation and bone repair, and calcium deficiency may lead to osteoporosis and increase the risk of delayed fracture union, muscle spasms, periprosthetic osteolysis and aseptic loosening (Ciosek et al., 2021). However, maintenance of normal blood calcium levels is often neglected, even in patients diagnosed with osteoporosis. In a study including 505 patients with osteoporosis undergoing total joint arthroplasty, less than two-thirds of patients with osteoporosis or osteopenia received calcium or vitamin D treatments (Wang et al., 2022). In another study aimed at exploring the relationship between mortality and low bone mass density at the femoral neck and vertebra among patients self-discontinuing anti-osteoporosis medication, lower serum calcium levels were associated with higher mortality risk (Hsu et al., 2021). However, Okyaya et al. reported that serum calcium and ionized calcium levels were not associated with the development of osteoporosis (Okyay et al., 2013). Lower patient education degree is also an independent risk factor for dislocation after THA. Different from the lack of patient education and poor compliance with hip precautions during the postoperative period increasing the risk of dislocation (Dargel et al., 2014; Peter et al., 2011), low education levels make it difficult for patients to comprehensively understand the orthopedists’ instructions and inadvertently ignore the dislocation-prone movements. There is a significant relationship between knowledge level and education degree, but in a cross-sectional study involving 268 patients, the authors found that although adults with higher education levels had significantly more knowledge about healthy lifestyle habits than those with lower education levels, there was no significant relationship between education degree and osteoporosis lifestyle habits such as exercise, calcium and vitamin intake in patients’ daily lives (Etemadifar et al., 2013). In our study, after adjusting for other potential risk factors, osteoporosis was not an independent risk factor for dislocation after THA, so the reason why low blood calcium and poor education degree increase dislocation after THA may be unrelated to osteoporosis, and further research is needed to confirm our findings. For patients with low serum calcium level, orthopedists should pay attention to their bone density and guide them in calcium supplementation. For patients with low education levels, we need to explain to patients and their families in a more understandable way, such as drawing or animation, and actively communicate to prevent patients from doing actions that are prone to dislocation.
In order to reduce the dislocation rate after THA, orthopedists have made numerous attempts in surgical approach and prosthesis design. The posterolateral approach is a classic approach for THA, while great interest has been directed toward anterior approaches because of lower dislocation risk without increasing the risk of early revision (Sheth et al., 2015). Constrained liner is also an efficient way to reduce dislocation rate after THA. As displayed by Pace in a study, the impetus for using the constrained liner primarily was associated with significant decreases in the risk of dislocation following constrained THA (Pace et al., 2015). Therefore, for patients with the above patient risk factors of dislocation after primary THA, orthopedic surgeons can select appropriate approaches and prostheses to prevent dislocation.
The present study had several limitations. First, this is a retrospective study, which may lead to inevitable patient selection bias. In order to further thoroughly analyze the patient risk factors of dislocation after THA, more prospective studies with larger samples are needed in the future. Second, the indications for THA are not subdivided enough. For example, primary osteoarthritis and secondary osteoarthritis are classified into one category, and diseases other than osteoarthritis, femoral head necrosis and rheumatoid arthritis are collectively referred to as others. If the diseases are further subdivided, the interference of confounding factors may be further reduced, and more diseases may be identified as risk factors related to dislocation. Third, this study was a single-center study, which may reduce the generalizability of the research results. However, the generalizability will also be affected by different factors such as the center and individual. Therefore, the results in this study may be beneficial to extrapolate the results to a wider range of clinical practices involving different surgeons or settings. Finally, the muscles around the hip joint are easily affected by various factors such as diseases and age. However, the muscle strength was not compared due to the retrospective study design. In the future, more studies are needed to verify these theoretical hypotheses and further validate our results.
Conclusion
Dislocation after THA remains a major challenge for orthopedists and is caused by multiple factors. Older age, rheumatoid arthritis, low serum calcium level, and poor education degree are independent risk factors for hip dislocation. Awareness of preoperative patient risk factors to predict dislocation can help orthopedists identify high-risk patients, make more accurate preoperative plans and select optimal surgical techniques and hip prostheses to prevent dislocation after THA and revision surgeries.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Medical Ethical Committee for Clinical Research and Animal Trials of the First Affiliated Hospital of Sun Yat-sen University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
HL: Data curation, Conceptualization, Writing – review and editing, Writing – original draft. JX: Conceptualization, Writing – review and editing, Data curation. XL: Writing – review and editing, Data curation. SL: Data curation, Writing – review and editing. WL: Writing – review and editing, Supervision, Conceptualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by SunYat-sen University 5010 Clinical Research Project (2013002).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abdel, M. P., Cross, M. B., Yasen, A. T., and Haddad, F. S. (2015). The functional and financial impact of isolated and recurrent dislocation after total hip arthroplasty. bone and Jt. J. 97-b (8), 1046–1049. doi:10.1302/0301-620X.97B8.34952
Buckland, A. J., Puvanesarajah, V., Vigdorchik, J., Schwarzkopf, R., Jain, A., Klineberg, E. O., et al. (2017). Dislocation of a primary total hip arthroplasty is more common in patients with a lumbar spinal fusion. bone and Jt. J. 99-b (5), 585–591. doi:10.1302/0301-620X.99B5.BJJ-2016-0657.R1
Charney, M., Paxton, E. W., Stradiotto, R., Lee, J. J., Hinman, A. D., Sheth, D. S., et al. (2020). A comparison of risk of dislocation and cause-specific revision between direct anterior and posterior approach following elective cementless total hip arthroplasty. J. arthroplasty 35 (6), 1651–1657. doi:10.1016/j.arth.2020.01.033
Ciosek, Ż., Kot, K., Kosik-Bogacka, D., Łanocha-Arendarczyk, N., and Rotter, I. (2021). The effects of calcium, magnesium, phosphorus, fluoride, and lead on bone tissue. Biomolecules 11 (4), 506. doi:10.3390/biom11040506
Dargel, J., Oppermann, J., Brüggemann, G. P., and Eysel, P. (2014). Dislocation following total hip replacement. Dtsch. Arztebl Int. 111 (51-52), 884–890. doi:10.3238/arztebl.2014.0884
DelSole, E. M., Vigdorchik, J. M., Schwarzkopf, R., Errico, T. J., and Buckland, A. J. (2017). Total hip arthroplasty in the spinal deformity population: does degree of sagittal deformity affect rates of safe zone placement, instability, or revision? J. arthroplasty 32 (6), 1910–1917. doi:10.1016/j.arth.2016.12.039
Ding, Z. C., Zeng, W. N., Mou, P., Liang, Z. M., Wang, D., and Zhou, Z. K. (2020). Risk of dislocation after total hip arthroplasty in patients with crowe type IV developmental dysplasia of the hip. Orthop. Surg. 12 (2), 589–600. doi:10.1111/os.12665
Dorr, L. D., Wolf, A. W., Chandler, R., and Conaty, J. P. (1983). Classification and treatment of dislocations of total hip arthroplasty. Clin. Orthop. Relat. Res. 173, 151–158. doi:10.1097/00003086-198303000-00019
Esposito, C. I., Gladnick, B. P., Lee, Y. Y., Lyman, S., Wright, T. M., Mayman, D. J., et al. (2015). Cup position alone does not predict risk of dislocation after hip arthroplasty. J. Arthroplasty 30 (1), 109–113. doi:10.1016/j.arth.2014.07.009
Etemadifar, M. R., Nourian, S. M., Fereidan-Esfahani, M., Shemshaki, H., Nourbakhsh, M., and Zarezadeh, A. (2013). Relationship of knowledge about osteoporosis with education level and life habits. World J. Orthop. 4 (3), 139–143. doi:10.5312/wjo.v4.i3.139
Falez, F., Papalia, M., Favetti, F., Panegrossi, G., Casella, F., and Mazzotta, G. (2017). Total hip arthroplasty instability in Italy. Int. Orthop. 41 (3), 635–644. doi:10.1007/s00264-016-3345-6
Forde, B., Engeln, K., Bedair, H., Bene, N., Talmo, C., and Nandi, S. (2018). Restoring femoral offset is the most important technical factor in preventing total hip arthroplasty dislocation. J. Orthop. 15 (1), 131–133. doi:10.1016/j.jor.2018.01.026
Gill, K., Whitehouse, S. L., Hubble, M. J., and Wilson, M. J. (2016). Short-term results with a constrained acetabular liner in patients at high risk of dislocation after primary total hip arthroplasty. Hip Int. J. Clin. Exp. Res. hip pathology Ther. 26 (6), 580–584. doi:10.5301/hipint.5000396
Girard, J., Kern, G., Migaud, H., Delaunay, C., Ramdane, N., Hamadouche, M., et al. (2013). Primary total hip arthroplasty revision due to dislocation: prospective French multicenter study. Orthop. and traumatology, Surg. and Res. OTSR 99 (5), 549–553. doi:10.1016/j.otsr.2013.03.026
Goel, A., Lau, E. C., Ong, K. L., Berry, D. J., and Malkani, A. L. (2015). Dislocation rates following primary total hip arthroplasty have plateaued in the Medicare population. J. Arthroplasty 30 (5), 743–746. doi:10.1016/j.arth.2014.11.012
Hailer, N. P., Weiss, R. J., Stark, A., and Kärrholm, J. (2012). The risk of revision due to dislocation after total hip arthroplasty depends on surgical approach, femoral head size, sex, and primary diagnosis. An analysis of 78,098 operations in the Swedish Hip Arthroplasty Register. Acta Orthop. 83 (5), 442–448. doi:10.3109/17453674.2012.733919
Hedlundh, U., Ahnfelt, L., Hybbinette, C. H., Weckstrom, J., and Fredin, H. (1996). Surgical experience related to dislocations after total hip arthroplasty. J. Bone Jt. Surg. Br. 78 (2), 206–209. doi:10.1302/0301-620x.78b2.0780206
Howie, D. W., Holubowycz, O. T., and Middleton, R.Large Articulation Study Group (2012). Large femoral heads decrease the incidence of dislocation after total hip arthroplasty: a randomized controlled trial. J. bone Jt. Surg. Am. volume 94 (12), 1095–1102. doi:10.2106/JBJS.K.00570
Hsu, C. S., Chang, S. T., Cheng, Y. Y., Lee, H. T., Chen, C. H., Deng, Y. L., et al. (2021). Low bone mineral density and calcium levels as risks for mortality in patients with self-discontinuation of anti-osteoporosis medication. Int. J. Environ. Res. Public Health 19 (1), 197. doi:10.3390/ijerph19010197
Ji, H. M., Kim, K. C., Lee, Y. K., Ha, Y. C., and Koo, K. H. (2012). Dislocation after total hip arthroplasty: a randomized clinical trial of a posterior approach and a modified lateral approach. J. arthroplasty 27 (3), 378–385. doi:10.1016/j.arth.2011.06.007
Jiang, W., Xu, H., Wang, X., Jia, Z., Liao, C., Huang, Q., et al. (2023). More complications and higher transfusion rate in patients with rheumatoid arthritis than osteoarthritis undergoing total hip arthroplasty. Int. Orthop. 47 (5), 1189–1196. doi:10.1007/s00264-023-05728-7
Jørgensen, C. C., Kjaersgaard-Andersen, P., Solgaard, S., and Kehlet, H.Lundbeck Foundation Centre for Fast-track Hip and Knee Replacement Collaborative Group (2014). Hip dislocations after 2,734 elective unilateral fast-track total hip arthroplasties: incidence, circumstances and predisposing factors. Arch. Orthop. Trauma Surg. 134 (11), 1615–1622. doi:10.1007/s00402-014-2051-3
Kanawade, V., Dorr, L. D., and Wan, Z. (2014). Predictability of acetabular component angular change with postural shift from standing to sitting position. J. bone Jt. Surg. Am. volume 96 (12), 978–986. doi:10.2106/JBJS.M.00765
Kotwal, R. S., Ganapathi, M., John, A., Maheson, M., and Jones, S. A. (2009). Outcome of treatment for dislocation after primary total hip replacement. J. Bone Jt. Surg. Br. 91 (3), 321–326. doi:10.1302/0301-620X.91B3.21274
Lewinnek, G. E., Lewis, J. L., Tarr, R., Compere, C. L., and Zimmerman, J. R. (1978). Dislocations after total hip-replacement arthroplasties. J. Bone Jt. Surg. Am. 60 (2), 217–220. doi:10.2106/00004623-197860020-00014
Li, H., Xie, J. W., Ding, Z. C., Yuan, M. C., Lai, Y. H., and Zhou, Z. K. (2022). Evaluation of the rate of post-operative dislocation in patients with ipsilateral valgus knee deformity after primary total hip arthroplasty. Int. Orthop. 46 (7), 1507–1514. doi:10.1007/s00264-022-05372-7
Liu, Q., Cheng, X., Yan, D., and Zhou, Y. (2019). Plain radiography findings to predict dislocation after total hip arthroplasty. J. Orthop. Transl. 18, 1–6. doi:10.1016/j.jot.2018.12.003
Malkani, A. L., Dilworth, B., Ong, K., Baykal, D., Lau, E., Mackin, T. N., et al. (2017). High risk of readmission in octogenarians undergoing primary hip arthroplasty. Clin. Orthop. Relat. Res. 475 (12), 2878–2888. doi:10.1007/s11999-017-5241-9
Malkani, A. L., Ong, K. L., Lau, E., Kurtz, S. M., Justice, B. J., and Manley, M. T. (2010). Early- and late-term dislocation risk after primary hip arthroplasty in the Medicare population. J. Arthroplasty 25 (6 Suppl. l), 21–25. doi:10.1016/j.arth.2010.04.014
Meek, R. M., Allan, D. B., McPhillips, G., Kerr, L., and Howie, C. R. (2006). Epidemiology of dislocation after total hip arthroplasty. Clin. Orthop. Relat. Res. 447, 9–18. doi:10.1097/01.blo.0000218754.12311.4a
Mercurio, M., Gasparini, G., Carbone, E. A., Galasso, O., and Segura-Garcia, C. (2020). Personality traits predict residual pain after total hip and knee arthroplasty. Int. Orthop. 44 (7), 1263–1270. doi:10.1007/s00264-020-04553-6
Miki, H., Sugano, N., Yonenobu, K., Tsuda, K., Hattori, M., and Suzuki, N. (2013). Detecting cause of dislocation after total hip arthroplasty by patient-specific four-dimensional motion analysis. Clin. Biomech. (Bristol, Avon) 28 (2), 182–186. doi:10.1016/j.clinbiomech.2012.11.009
Munro, J. T., Vioreanu, M. H., Masri, B. A., and Duncan, C. P. (2013). Acetabular liner with focal constraint to prevent dislocation after THA. Clin. Orthop. Relat. Res. 471 (12), 3883–3890. doi:10.1007/s11999-013-2858-1
Nakashima, Y., Hirata, M., Akiyama, M., Itokawa, T., Yamamoto, T., Motomura, G., et al. (2014). Combined anteversion technique reduced the dislocation in cementless total hip arthroplasty. Int. Orthop. 38 (1), 27–32. doi:10.1007/s00264-013-2091-2
Okyay, E., Ertugrul, C., Acar, B., Sisman, A. R., Onvural, B., and Ozaksoy, D. (2013). Comparative evaluation of serum levels of main minerals and postmenopausal osteoporosis. Maturitas 76 (4), 320–325. doi:10.1016/j.maturitas.2013.07.015
Pace, T., Finley, S., Snider, R., Looper, J., and Tanner, S. (2015). Short-term results of novel constrained total hip arthroplasty. Orthop. Rev. (Pavia). 7 (2), 5779. doi:10.4081/or.2015.5779
Perfetti, D. C., Schwarzkopf, R., Buckland, A. J., Paulino, C. B., and Vigdorchik, J. M. (2017). Prosthetic dislocation and revision after primary total hip arthroplasty in lumbar fusion patients: a propensity score matched-pair analysis. J. arthroplasty 32 (5), 1635–1640.e1. doi:10.1016/j.arth.2016.11.029
Peter, R., Lübbeke, A., Stern, R., and Hoffmeyer, P. (2011). Cup size and risk of dislocation after primary total hip arthroplasty. J. Arthroplasty 26 (8), 1305–1309. doi:10.1016/j.arth.2010.11.015
Ravi, B., Croxford, R., Hollands, S., Paterson, J. M., Bogoch, E., Kreder, H., et al. (2014). Increased risk of complications following total joint arthroplasty in patients with rheumatoid arthritis. Arthritis Rheumatol. 66 (2), 254–263. doi:10.1002/art.38231
Rowan, F. E., Benjamin, B., Pietrak, J. R., and Haddad, F. S. (2018). Prevention of dislocation after total hip arthroplasty. J. Arthroplasty 33 (5), 1316–1324. doi:10.1016/j.arth.2018.01.047
Saiz, A. M., Lum, Z. C., and Pereira, G. C. (2019). Etiology, evaluation, and management of dislocation after primary total hip arthroplasty. JBJS Rev. 7 (7), e7. doi:10.2106/jbjs.rvw.18.00165
Sheth, D., Cafri, G., Inacio, M. C., Paxton, E. W., and Namba, R. S. (2015). Anterior and anterolateral approaches for THA are associated with lower dislocation risk without higher revision risk. Clin. Orthop. Relat. Res. 473 (11), 3401–3408. doi:10.1007/s11999-015-4230-0
Sing, D. C., Barry, J. J., Aguilar, T. U., Theologis, A. A., Patterson, J. T., Tay, B. K., et al. (2016). Prior lumbar spinal arthrodesis increases risk of prosthetic-related complication in total hip arthroplasty. J. arthroplasty 31 (9 Suppl. l), 227–232.e1. doi:10.1016/j.arth.2016.02.069
Tidermark, J., Ponzer, S., Svensson, O., Söderqvist, A., and Törnkvist, H. (2003). Internal fixation compared with total hip replacement for displaced femoral neck fractures in the elderly. A randomised, controlled trial. J. Bone Jt. Surg. Br. 85 (3), 380–388. doi:10.1302/0301-620x.85b3.13609
Vaishya, R., Vijay, V., and Vaish, A. (2015). Successful salvage of an unstable Girdlestone's excision arthroplasty with a megaprosthesis of the hip. J. Clin. Orthop. trauma 6 (4), 269–272. doi:10.1016/j.jcot.2015.03.005
von Knoch, M., Berry, D. J., Harmsen, W. S., and Morrey, B. F. (2002). Late dislocation after total hip arthroplasty. J. bone Jt. Surg. Am. volume 84 (11), 1949–1953. doi:10.2106/00004623-200211000-00007
Wang, Z., Levin, J. E., Amen, T. B., Arzani, A., Manzi, J. E., and Lane, J. M. (2022). Total joint arthroplasty and osteoporosis: looking beyond the joint to bone health. J. Arthroplasty 37 (9), 1719–1725.e1. doi:10.1016/j.arth.2022.04.010
Wera, G. D., Ting, N. T., Moric, M., Paprosky, W. G., Sporer, S. M., and Della Valle, C. J. (2012). Classification and management of the unstable total hip arthroplasty. J. Arthroplasty 27 (5), 710–715. doi:10.1016/j.arth.2011.09.010
Wright-Chisem, J., Elbuluk, A. M., Mayman, D. J., Jerabek, S. A., Sculco, P. K., and Vigdorchik, J. M. (2022). The journey to preventing dislocation after total hip arthroplasty: how did we get here? Bone Jt. J. 104-b (1), 8–11. doi:10.1302/0301-620X.104B1.BJJ-2021-0823.R1
Zeng, Y., Prasad, R., King, R. D., Joshi, R., Lane, J., Shriber, S., et al. (2023). AIDS-related kaposi sarcoma associated with steroid-unresponsive periorbital lymphedema that responded to chemotherapy. Am. J. Case Rep. 24, e938801. doi:10.12659/AJCR.938801
Zhang, D., Chen, L., Peng, K., Xing, F., Wang, H., and Xiang, Z. (2015). Effectiveness and safety of the posterior approach with soft tissue repair for primary total hip arthroplasty: a meta-analysis. Orthop. and traumatology, Surg. and Res. OTSR 101 (1), 39–44. doi:10.1016/j.otsr.2014.10.015
Zhou, V. Y., Lacaille, D., Lu, N., Kopec, J. A., Garbuz, D. S., Qian, Y., et al. (2022). Has the incidence of total joint arthroplasty in rheumatoid arthritis decreased in the era of biologics use? A population-based cohort study. Rheumatol. Oxf. 61 (5), 1819–1830. doi:10.1093/rheumatology/keab643
Zhu, T. Y., Griffith, J. F., Qin, L., Hung, V. W., Fong, T. N., Au, S. K., et al. (2015). Cortical thinning and progressive cortical porosity in female patients with systemic lupus erythematosus on long-term glucocorticoids: a 2-year case-control study. Osteoporos. Int. 26 (6), 1759–1771. doi:10.1007/s00198-015-3077-2
Keywords: total hip arthroplasty, postoperative dislocation, patient risk factors, risk factors for dislocation, preoperative planning
Citation: Li H, Xie J, Lu X, Li S and Liao W (2025) Findings of preoperative patient risk factors to predict dislocation following total hip arthroplasty. Front. Cell Dev. Biol. 13:1601997. doi: 10.3389/fcell.2025.1601997
Received: 28 March 2025; Accepted: 05 May 2025;
Published: 15 May 2025.
Edited by:
Liao Zhiwei, Huazhong University of Science and Technology, ChinaReviewed by:
Xiaofan Hu, Fourth Military Medical University, ChinaYuhao Zeng, University of Pittsburgh Medical Center, United States
Tuozhou Liu, Central South University, China
Copyright © 2025 Li, Xie, Lu, Li and Liao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weiming Liao, bGlhb3dtQG1haWwuc3lzdS5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
 Hao Li
Hao Li Jinwei Xie
Jinwei Xie Xiaomin Lu
Xiaomin Lu Shuai Li1
Shuai Li1