- 1Department of Laboratory Medicine, The People’s Hospital of Guangxi Zhuang Autonomous Region, Guangxi Academy of Medical Sciences, Nanning, China
- 2Department of Gastroenterology, The People’s Hospital of Guangxi Zhuang Autonomous Region, Guangxi Academy of Medical Sciences, Nanning, China
- 3Department of Microbiology, Guangzhou Baochuang Biotechnology Co., Ltd., Guangzhou, China
Background: Community-acquired pneumonia is primarily caused by Acinetobacter baumannii, Pseudomonas aeruginosa, Klebsiella pneumoniae, Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus aureus, Mycoplasma pneumoniae, and Chlamydia pneumoniae, leading to severe illness and death in developing countries.
Methods: A rapid, straightforward, sensitive, high-throughput, and precise multiplex PCR-dipstick DNA chromatography assay was devised. This innovative technique was specifically engineered for the immediate and efficient detection of the aforementioned eight respiratory pathogens, with particular emphasis on scenarios involving co-infections. Custom-designed specific primers were employed, wherein the 5′ end of the forward primers was tagged with oligonucleotide tags (Tag) and the 5′ end of the reverse primers was conjugated with biotin. A C3 spacer was incorporated to bridge the Tag and the forward primer. Complementary oligonucleotides (cTag) corresponding to each of the eight pathogens were immobilized within the test area of the test strip. Meanwhile, biotin was strategically utilized to create an internal control line at the distal end of the test strip. The biotin moiety at the 5′ end of the reverse primer was engineered to interact with blue latex microspheres coated with streptavidin, thereby triggering a detectable signal. Following the PCR amplification of the target DNA fragments, during the membrane strip chromatography hybridization process, the Tag- and biotin-labeled target DNA engaged in a dual interaction. First, it bound to the blue latex microspheres via streptavidin–biotin binding, and second, it hybridized with the cTag on the membrane strip. This led to the accumulation of captured blue latex microspheres at both the test line and the internal control line, manifesting as visible blue bands. A total of 186 respiratory sputum or bronchoalveolar lavage fluid specimens were collected and analyzed. The multiplex PCR-dipstick DNA chromatography assay was deployed for detection, while traditional bacterial culture was also carried out in parallel for comparative purposes. To rigorously validate the accuracy of the multiplex PCR-dipstick DNA chromatography assay in identifying PCR products, DNA sequencing was performed on all PCR products derived from the clinical samples.
Results: The multiplex PCR-dipstick DNA chromatography assay demonstrated remarkable efficacy, being capable of specifically discriminating among the eight pathogens within a remarkably short timeframe of 40 minutes. The detection limit for individual bacterial species ranged from 10 to 102 CFU/mL. Notably, no cross-reactions were observed among the eight target bacteria, nor with other representative respiratory bacteria, including Acinetobacter junii, Enterobacter cloacae, Klebsiella oxytoca, Haemophilus parainfluenzae, Pseudomonas fluorescens, Aeromonas hydrophila, and Staphylococcus epidermidis. The concordance between the results obtained from the multiplex PCR-dipstick DNA chromatography assay and those from DNA sequencing was absolute, with a kappa value of 1.00.
Conclusion: A successful multiplex PCR-dipstick DNA chromatography assay was established for the simultaneous detection of eight respiratory bacterial pathogens and was effectively applied in clinical sample analysis. This indicates that this single-use device has promising potential for analyzing the microbial composition related to respiratory infections and is also suitable for small laboratories and field diagnostics.
Introduction
Lower respiratory tract infection remains one of the primary causes of hospitalization and death worldwide (Vink et al., 2014; Simpson et al., 2015; Beck et al., 2015; Noviello and Huang, 2019). Diverse etiologies have been linked to acute respiratory infections, with bacteria being significant causative agents of lower respiratory tract infections (Price et al., 2019; Uzoamaka et al., 2017; He et al., 2017; Liu et al., 2018; Carvalhaes et al., 2019). Acinetobacter baumannii, Pseudomonas aeruginosa, Haemophilus influenzae, Staphylococcus aureus, Streptococcus pneumoniae, Klebsiella pneumoniae, Mycoplasma pneumoniae, and Chlamydia pneumoniae were identified as the responsible pathogens causing pneumonia (He et al., 2017; Khadanga et al., 2014; Yun et al., 2019; Wang et al., 2019). The prompt identification and treatment of bacterial pathogens are crucial, as these pathogens can lead to severe, complicated pneumonia and even mortality. Co-infections of respiratory pathogens occur frequently (Liu et al., 2018; Kotula et al., 2018). There is an urgent need for a rapid, straightforward, sensitive, high-throughput, and accurate diagnostic technique for respiratory pathogens, especially for co-infections involving these agents. However, the traditional microbial culture method is time-consuming and labor-intensive and generally can only identify dominant pathogens.
Multiplex polymerase chain reaction (PCR), owing to its advantages of speed, sensitivity, and specificity, is anticipated to become the most efficacious method for detecting respiratory pathogens. Nevertheless, real-time PCR methods have a narrow diagnostic scope, as they can only detect two or three pathogens concurrently in a single reaction due to the limited recognition capabilities of the instrument (van de Pol et al., 2007; Mangold et al., 2011). With the swift development of molecular biology technology, specific probe hybridization technology (Chen et al., 2020), PCR technology for amplifying specific nucleic acid fragments (Chen et al., 2019), and 16S rRNA sequence analysis (Menon et al., 2017) have also been applied to the detection of pathogenic microorganisms. These methods are sensitive, specific, and rapid, but they all depend on expensive equipment and trained laboratory technicians, which limits their widespread application in small community hospitals and remote areas.
Thanks to its rapidity, sensitivity, and ease of automation, the paper-based microfluidic DNA biosensor has emerged as a promising approach for detecting pathogenic microorganisms in recent years (Özgür et al., 2020; Abdelrasoul et al., 2020; Song et al., 2019). In particular, paper-based microfluidic DNA biosensors used gold nanoparticles (Chen et al., 2020, 2019; Menon et al., 2017; Özgür et al., 2020; Bahavarnia et al., 2020) and color polystyrene beads (Abdelrasoul et al., 2020; Cao et al., 2009) as signal generators to realize the visual detection of target. Accordingly, paper-based microfluidic DNA biosensors can also provide semi-quantitative results for bacterial targets through intensity reading or coupling with other agents like enzymes (Chen et al., 2019), fluorescent dye (Huang et al., 2020; Fadlalla et al., 2020), or radioactive binding compound (Banakar et al., 2022). Given its rapid, compact, sensitive, cost-effective, and disposable nature (Chen et al., 2019; Menon et al., 2017; Özgür et al., 2020; Abdelrasoul et al., 2020; Huang et al., 2020; Ang et al., 2012), an increasing number of paper-based microfluidic DNA biosensors have been designed for point-of-care diagnosis. Moreover, the paper-based microfluidic DNA biosensor does not require complex equipment, reagents, or a power supply, minimizing the demands on laboratory personnel. The test strip DNA biosensor platform can be constructed as needed, enabling the intuitive display of detection results for different pathogens. It holds significant potential for application in the analysis of pathogenic microorganisms and antimicrobial resistance (Tian et al., 2016; Liles et al., 2019; Shanmugakani et al., 2017; Hayashi et al., 2013; Tian et al., 2014).
This study aimed to develop a simple, rapid, and sensitive PCR-dipstick chromatography method and achieve the simultaneous detection of respiratory bacterial co-infections by combining PCR and paper-based microfluidic bioassay.
Materials and method
Standard strain
Standard strains of A. baumannii (ATCC19606), P. aeruginosa (ATCC9027), K. pneumoniae (ATCC13883), S. pneumoniae (ATCC49619), H. influenzae (ATCC49766), S. aureus (ATCC6538), M. pneumoniae (ATCC15531), and C. pneumoniae (ATCC53592) were purchased from the Guangdong Microbiological Culture Collection Center.
Clinical samples
The study was approved by the medical ethics committee of the People’s Hospital of Guangxi Zhuang Autonomous Region, and all the subjects provided informed consent. A total of 186 specimens of sputum or bronchoalveolar lavage fluid (BALF) were collected from pneumonia patients at the People’s Hospital of Guangxi Zhuang Autonomous Region between December 2023 and December 2024. The collected sputum/BALF samples were characterized by a white blood cell count exceeding 25 and an epithelial cell count of less than 10 under ×10 magnification. These 186 sputum/BALF specimens were evaluated using the PCR-dipstick chromatography assay and were also subjected to culture. To further assess the accuracy of the PCR-dipstick chromatography assay, all PCR products were sent for sequencing.
Sample preparation
The sample preparation process for the multiplex PCR-dipstick DNA chromatography assay was as follows: equal volumes of 4% sodium hydroxide were added to the sputum/BALF samples, which were then incubated for 10 minutes. Subsequently, the samples were transferred to 1.5-mL centrifuge tubes and centrifuged at 15,000 rpm for 5 minutes, after which the supernatant was discarded. Next, 1 mL of sterile physiological saline was added, and the pellet was resuspended by gentle shaking. The samples were then centrifuged again at 15,000 rpm for 5 minutes, and the supernatant was discarded as completely as possible. Finally, 1 mL of sterile physiological saline was added. The pretreated sputum/BALF samples were stored in tubes at −80°C. Genomic DNA was extracted from the sputum/BALF samples using Magen HiPure Bacterial DNA kits according to the manufacturer’s instructions. For the bacterial culture methods, a sterile swab was used to obtain an appropriate amount of purulent sputum, which was then inoculated onto blood agar, MacConkey agar, and chocolate agar, with sector lines carefully drawn. BALF samples were centrifuged at 13,000 rpm for 5 minutes, and the sediment at the bottom was collected and inoculated onto the same types of agar plates, also with sector lines drawn. All media were incubated at 35°C in an atmosphere containing 5% CO2 for 48 hours. After 48 hours, matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI–TOF MS) was employed to identify the isolated strains. The specific steps were as follows: A single colony was carefully picked and spotted onto a MALDI target plate, dried at room temperature, then covered with 1 µL of α - Cyano - 4 - hydroxycinnamic acid (HCCA) matrix solution, and subsequently dried at room temperature again before being placed into the instrument for analysis. Protein spectra were analyzed using the FlexControl™ software in conjunction with the MBT compass software (Bruker, Billerica, MA, USA) and compared against the Mass Spectrometry Identification (MSI) platform database 2. Identification was confirmed when the MSI score was greater than or equal to 2.0. If multiple identification results were suggested for the same colony, only the result with the highest score was retained.
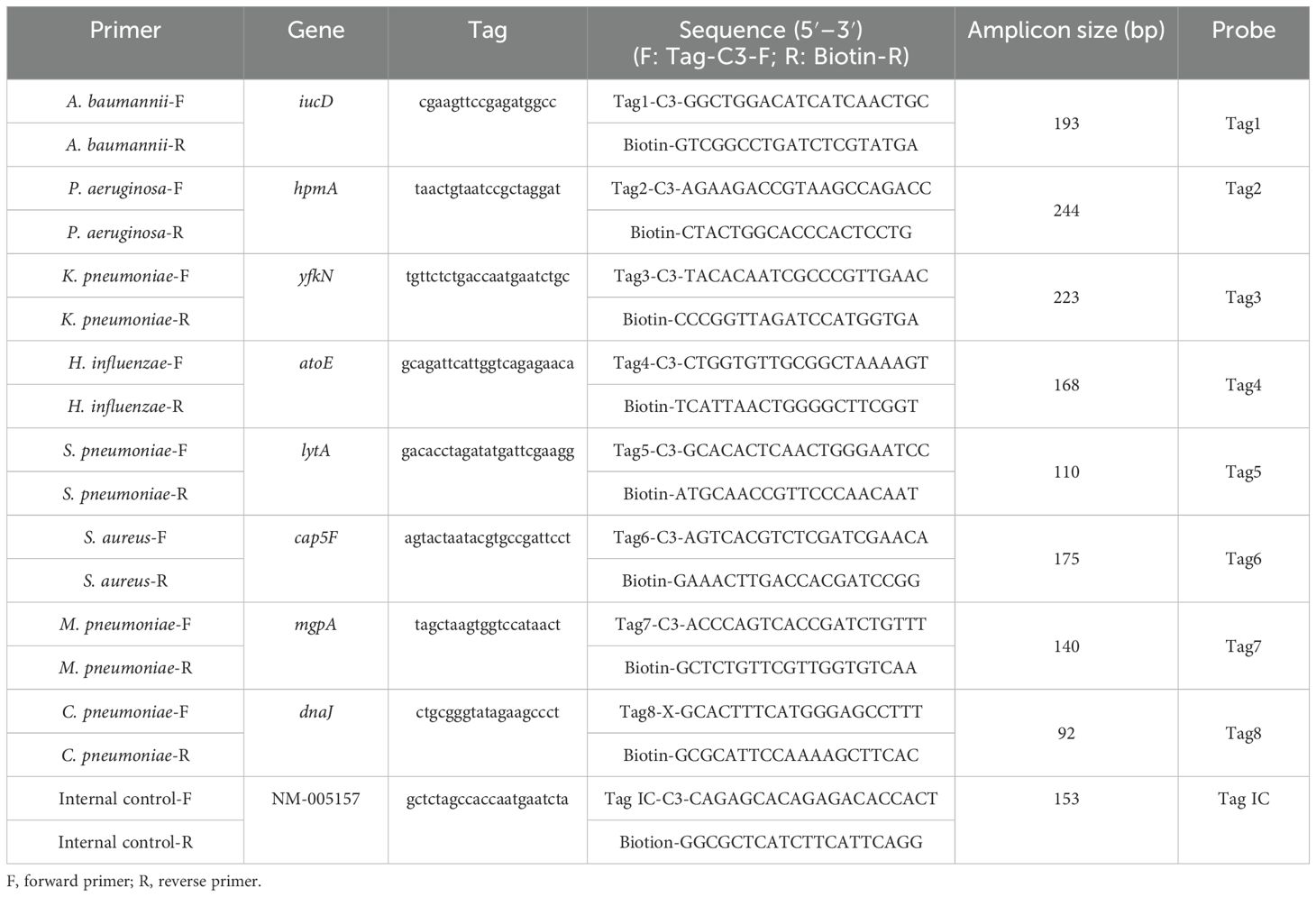
Primer and probe design
In multiplex PCR reactions, the presence of multiple pairs of primers can potentially lead to non-specific amplification. In this experiment, 10 pairs of specific primers for each bacterium were found from published literature for preliminary screening. These primers were further tested using the NCBI BLAST to ensure their specificity. Subsequently, the eight bacterial primer sets were incorporated into the multiplex PCR system using a stepwise sequential approach. Real-time PCR with melting curve analysis was performed to verify the specificity of the primers through characteristic melting temperature (Tm) profiles (Hu et al., 2020). Eventually, eight bacterial primers were selected based on their excellent amplification efficiency and the absence of non-specific primer amplicons (Hu et al., 2020; Luo et al., 2021) (Table 1). The 5′ terminus of the forward primer was tagged with a segment of oligonucleotides (tag) uniquely linked by C3 spacer (Niwa et al., 2014), in which C3 spacer was used to ensure that the tag remains a single strand during amplification. The 5′ terminus of the reverse primer was labeled with biotin.
Additionally, the inclusion of an internal control (IC) was crucial to ensure the reliability of the results and minimize the impact of sample variability, instrument performance, reagent quality, and operational errors. The IC was a synthetic sequence (CAGAGCACAGAGACACCACTGACGTGCCTGAGATGCCTCACTCCAAGGGCCAGGGAGAGAGCGATCCTCTGGACCATGAGCCTGCCGTGTCTCCATTGCTCCCTCGAAAAGAGCGAGGTCCCCCGGAGGGCGGCCTGAATGAAGATGAGCGCC) (Luo et al., 2021). The homology of the IC with the target genes was extremely low, indicating that it would not trigger cross-reactions. A pair of primers was also designed for the IC (Luo et al., 2021). The primers and the probes (Table 1) were synthesized by TBA (Tohoku Bio-Array, TBA, Sendai, Japan).
Detection principle of multiplex PCR-dipstick DNA chromatography
The dipstick strips produced by Tohoku Bio-Array, Co., contain three main components: a polyvinyl chloride (PVC) membrane that provides stability and adhesion, an absorbent area made of filter paper, and a sample application area made of nitrocellulose (NC) membrane. Complementary oligonucleotides (cTag) are fixed on the NC membrane, forming detection lines for eight pathogens, along with an IC line. Additionally, four red positioning lines are printed on the sample application area. These red lines serve as markers for locating different bacterial detection lines. For each pair of primers of eight bacteria, the 5′ terminus of the forward primer was tagged with eight different oligonucleotides (Tag), and the 5′ terminus of the reverse primer was tagged with biotin. The order of the cTag on the dipstick strip from the downside to the upside is A. baumannii, P. aeruginosa, K. pneumoniae, H. influenzae, S. pneumoniae, S. aureus, M. pneumoniae, C. pneumoniae, and internal control line. The terminal of the forward primer was connected with a tag by C3 spacer. The insertion of C3 spacer terminates DNA synthesis of Taq DNA polymerase at the insertion site so that tag is left as a single strand in the PCR (Niwa et al., 2014). Target DNA amplicons with an oligonucleotide-tagged terminus and a biotinylated terminus were coupled with latex beads through a streptavidin–biotin interaction and then hybridized with complementary oligonucleotides on the strip. The accumulation of captured latex beads on the test and internal control lines produced blue bands, enabling the judging of the result just by the naked eye (Figure 1).
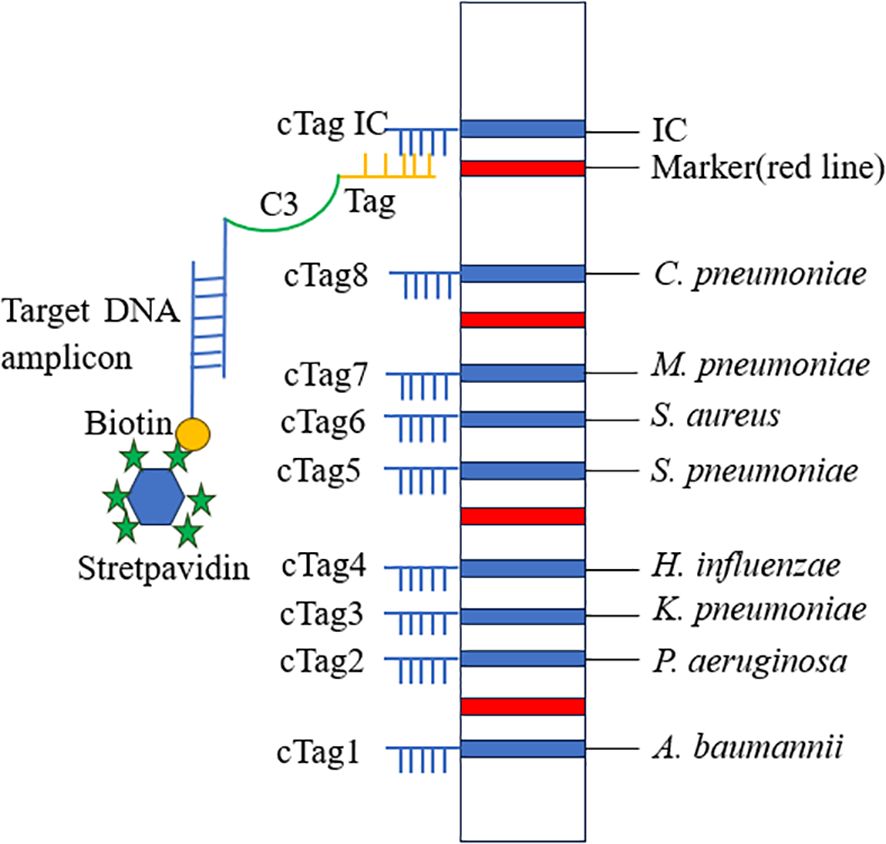
Figure 1. Schematic diagram of PCR-dipstick chromatography assay. Tag, oligonucleotide strand; cTag, complementary oligonucleotide strand.
After PCR amplification, 10 μL of PCR product was mixed with 9 μL of eluent (containing detergents, blocking agents, phosphate buffered saline (PBS), and salt solution) and 1 μL of streptavidin-coated blue latex suspension. A dipstick strip was then inserted into the mixture. After 10 minutes, the corresponding test lines and internal control lines were clearly visible as blue lines, indicating that the target bacterium amplicon was positive. It is of utmost importance to note that, regardless of the sample outcome, the IC line must always display a visible blue band. This serves as a critical quality control measure, confirming that the strips are operating correctly and that the assay conditions are suitable for reliable results. If the IC line fails to show a blue band, it signals a potential issue with the strip, the reagents, or the assay procedure, and the results obtained should be considered unreliable.
Optimization of PCR reaction system and procedure
S. aureus was selected as the representative species for optimizing the reaction program and conditions. To ascertain the most suitable reaction system and procedure for the multiplex PCR-dipstick DNA chromatography assay, the standard strains of S. aureus (105, 104, and 103 CFU/mL) were amplified by any combination of reaction procedures 1 and 2 and reaction systems 1 and 2. PCR amplification products were analyzed by dipstick chromatography and 3% agarose gel electrophoresis. Reaction system 1 and system 2 were identical in composition, with the exception of the buffers employed. The multiplex PCR was carried out in a total volume of 25 μL. In reaction system 1, the buffer was self-produced 10 × PCR buffer, with a volume of 2.5 μL. In contrast, reaction system 2 utilized 10 × Takara PCR buffer, also at a volume of 2.5 μL. The remaining components of the reaction systems were as follows: 1 μL of dUTPmix (100 mM); 0.4 μL each of the forward and reverse primers (10 μM) specific to the eight pathogens; 0.3 μL of the IC forward primer (2 μM) and 0.3 μL of the IC reverse primer (2 μM); and 1 μL of IC DNA (1 nM), 0.02 μL of UNG, 0.3 μL of Hs-Taq, and 5 μL of DNA template. Deionized water was added to bring the total volume up to 25 μL. Reaction procedure 1 was 95°C for 3 minutes and the following amplification program for a total of 40 cycles: 95°C for 5 s and 60°C for 20 s. Procedure 2 was 95°C for 3 minutes and the following amplification program for a total of 40 cycles: 95°C for 5 s and 60°C for 30 s.
Sensitivity of multiplex PCR-dipstick chromatography
To evaluate the limit of detection (LOD) of the PCR-dipstick chromatography assay, serial 10-fold dilutions of the DNA from standard strains of A. baumannii, P. aeruginosa, K. pneumoniae, S. pneumoniae, H. influenzae, S. aureus, M. pneumoniae, and C. pneumoniae were prepared, ranging from 10 to 107 CFU/mL. These diluted samples were then analyzed using the PCR-dipstick DNA chromatography assay to determine the assay’s sensitivity. The lowest concentration at which a visible blue band appeared at the corresponding detection line was deemed the LOD of the PCR-dipstick chromatography assay.
Results
Determination of reaction system and procedure
The standard strains of S. aureus (with concentrations of 105, 104, and 103 CFU/mL) were amplified through all possible combinations of reaction procedures 1 and 2, as well as reaction systems 1 and 2. As illustrated in Figure 2, no non-specific bands were detected in any of the three combinations. This demonstrated that the combination of reaction procedure 1 and reaction system 2 yielded the optimal dipstick DNA chromatography performance and the highest sensitivity in 3% agarose gel electrophoresis (as indicated by B and D).
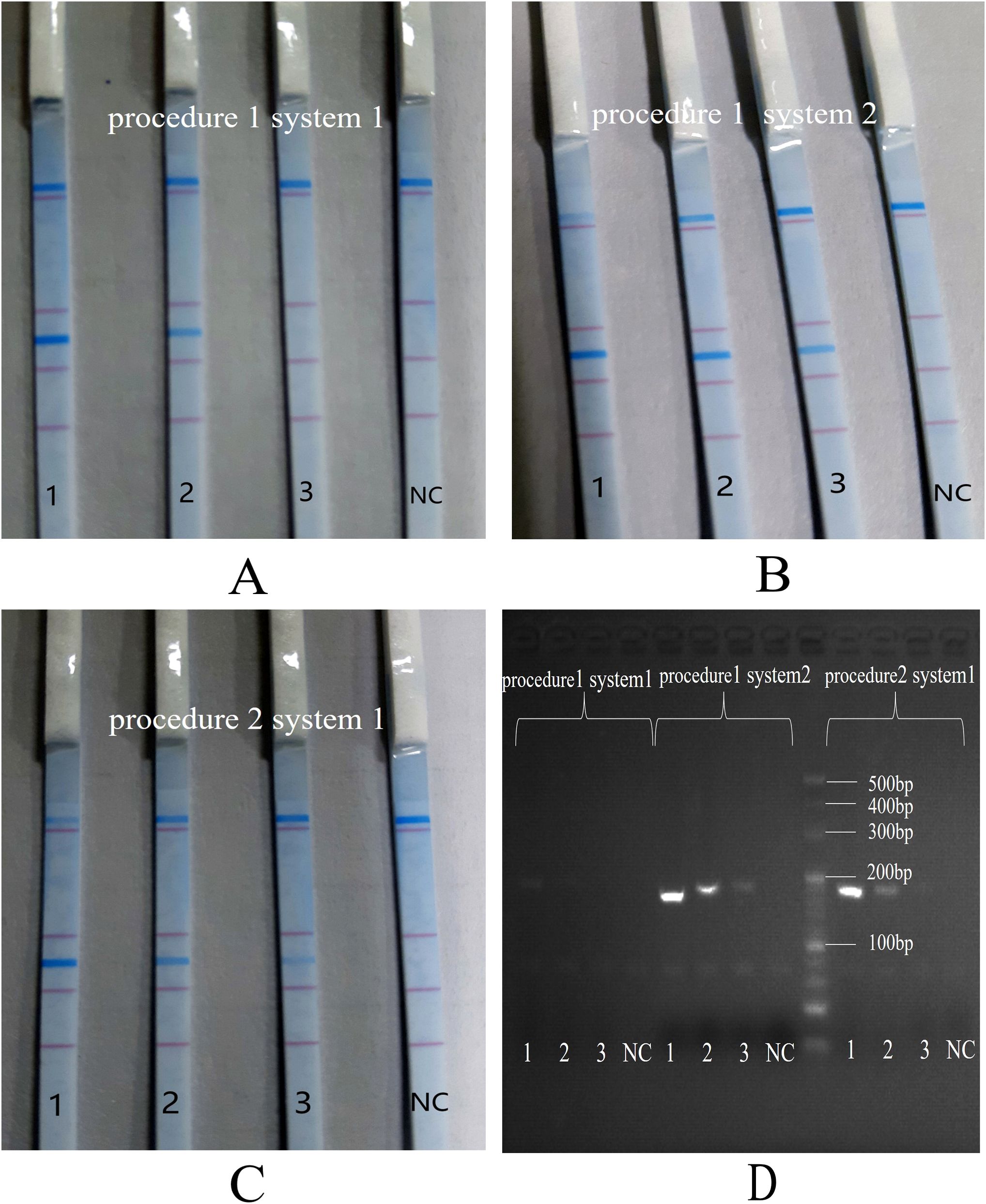
Figure 2. Comparison of PCR procedures and reaction systems. 1: 105 CFU/mL of S. aureus; 2: 104 CFU/mL of S. aureus; 3: 103 CFU/mL of S. aureus; NC, negative control. (A): reaction procedure 1 and reaction system 1; (B): reaction procedure 1 and reaction system 2; (C): reaction procedure 2 and reaction system 1; (D): 3% agarose gel electrophoresis.
Consequently, the finalized PCR-dipstick chromatography reaction protocol was 95°C for 3 minutes and the following amplification program for a total of 40 cycles: 95°C for 5 s and 60°C for 20 s. The final reaction mixture was formulated to contain 2.5 μL of 10 × Takara PCR buffer, 1 μL of dUTP mix (100 mM), 0.4 μL each of the forward and reverse primers (10 μM) specific for eight pathogens, 0.3 μL each of the IC forward and reverse primers (2 μM), 1 μL of IC DNA (1 nM), 0.02 μL of UNG, 0.3 μL of Hs-Taq, and 5 μL of DNA template, and deionized water was added to adjust the total volume to 25 μL.
Specificity of PCR-dipstick DNA chromatography
Initially, the specificity of the multiplex PCR-dipstick DNA chromatography assay was assessed to ascertain whether the eight pairs of primers could amplify effectively. The detailed procedure was as follows: each bacterial standard strain (at a concentration of 106 CFU/mL) was detected using the PCR-dipstick DNA chromatography assay to monitor whether blue bands corresponding to the other seven bacteria would appear at their respective detection sites. Sterile purified water served as the negative control. A visible blue band was present at the corresponding test line for the detection of each bacterium, while no non-specific amplification was observed, indicating that there was no cross-reaction among the eight bacteria (Figure 3A).
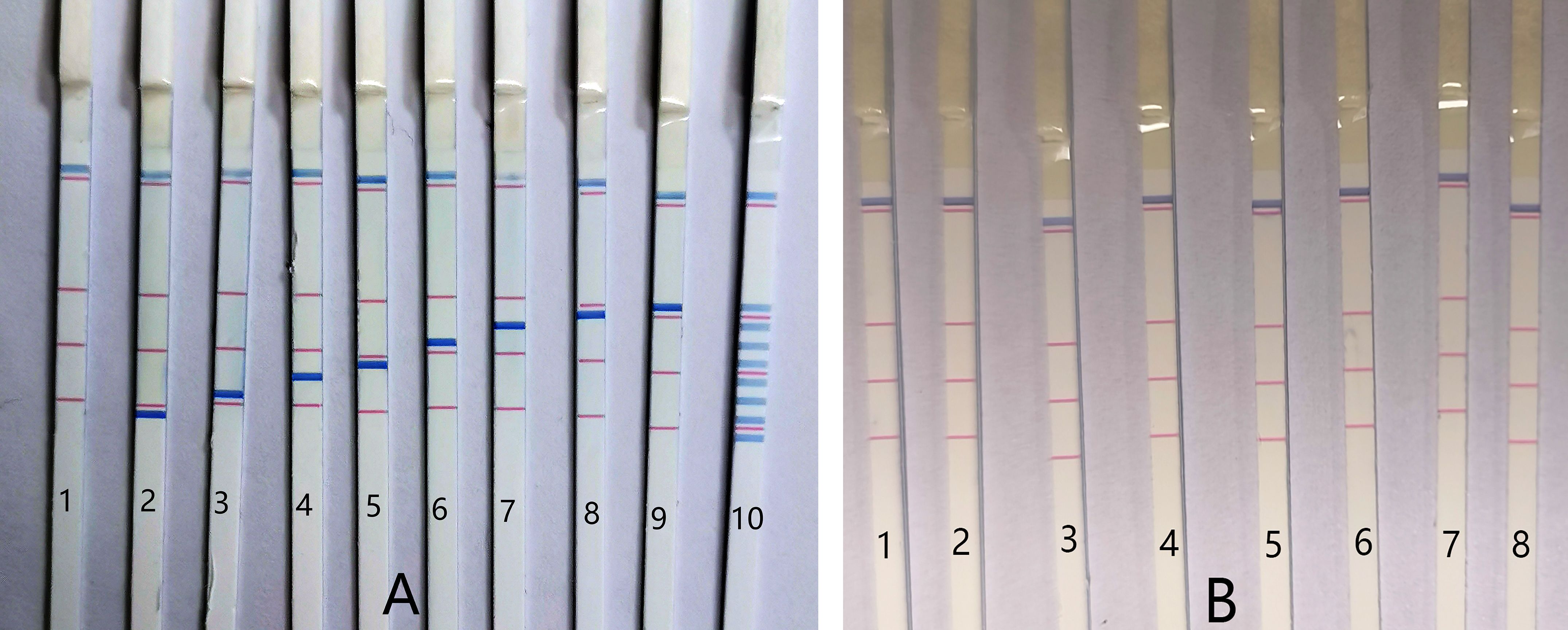
Figure 3. The specificity of PCR-dipstick DNA chromatography. (A) 1: negative control; 2: Acinetobacter baumannii; 3: Pseudomonas aeruginosa; 4: Klebsiella pneumoniae; 5: Haemophilus influenzae; 6: Streptococcus pneumoniae; 7: Staphylococcus aureus, 8: Mycoplasma pneumoniae; 9: Chlamydia pneumoniae; 10: multiplex detection, detect equivalent mixture of eight bacterial standard strains DNA (at a concentration of 106 CFU/mL). (B) 1: negative control; 2: Acinetobacter junii; 3: Enterobacter cloacae; 4: Klebsiella oxytoca; 5: Haemophilus parainfluenzae; 6: Pseudomonas fluorescens; 7: Aeromonas hydrophila; 8: Staphylococcus epidermidis.
Furthermore, the PCR-dipstick DNA chromatography assay was employed to detect an equivalent mixture of the DNA of eight bacterial standard strains (at a concentration of 106 CFU/mL). It was discovered that each test line corresponded to a specific bacterial standard strain DNA, and there was no false positive in the negative control (Figure 3A). These results suggest that this assay is suitable for multiplex analysis. Representative respiratory bacteria, including Acinetobacter junii, Enterobacter cloacae, Klebsiella oxytoca, Haemophilus parainfluenzae, Pseudomonas fluorescens, Aeromonas hydrophila, and Staphylococcus epidermidis, were also examined using the PCR-dipstick chromatography assay to verify the specificity of the primers against other bacteria. All the results were negative (Figure 3B), further demonstrating that the PCR-dipstick DNA chromatography method possesses excellent specificity.
Sensitivity of PCR-dipstick DNA chromatography
The single-bacterium sensitivity of the PCR-dipstick DNA chromatography assay was determined as follows: for A. baumannii, P. aeruginosa, K. pneumoniae, S. pneumoniae, S. aureus, M. pneumoniae, and C. pneumoniae, the detection limit was 10 CFU/mL; for H. influenzae, it was 102 CFU/mL (Figure 4).
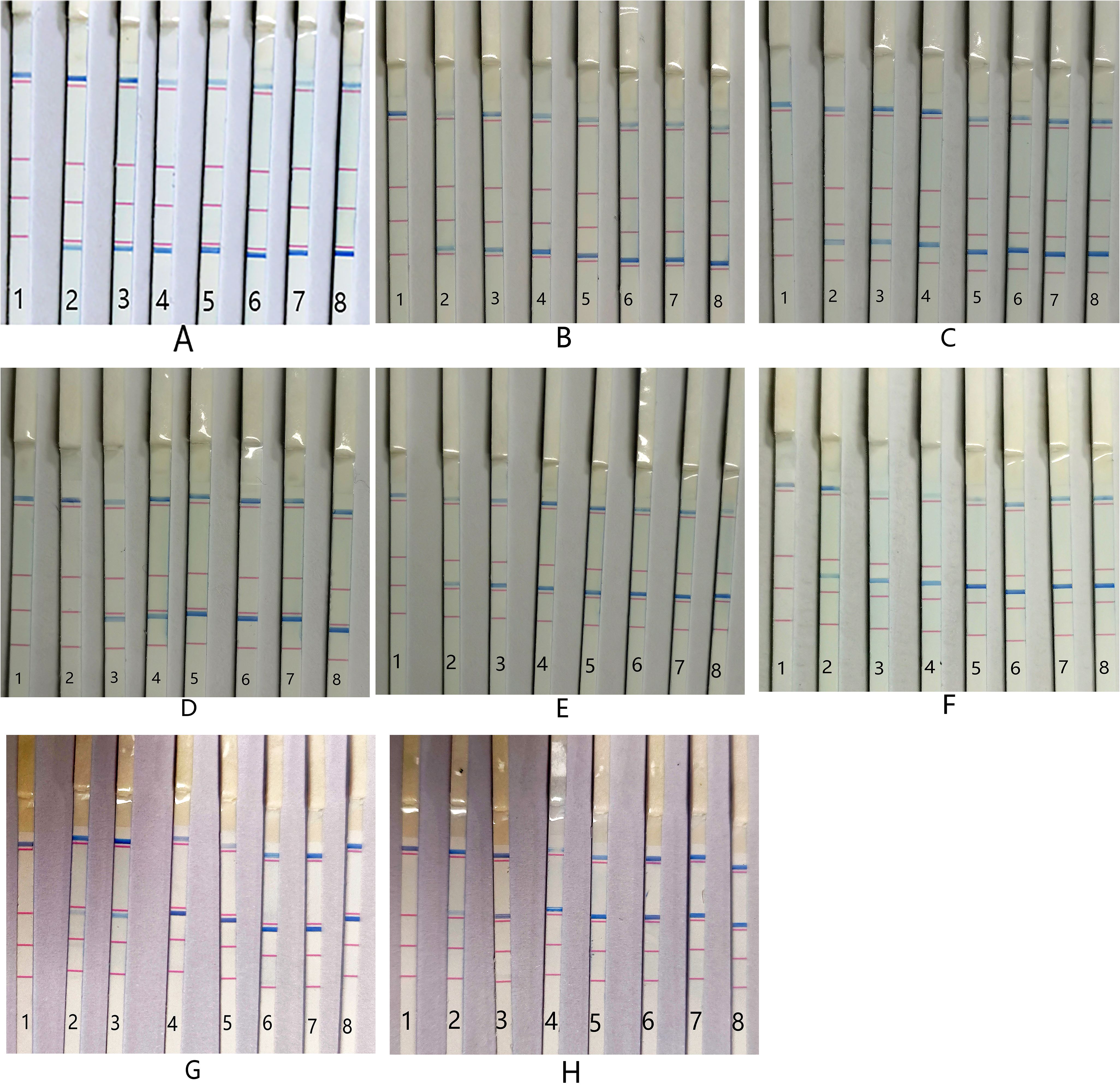
Figure 4. Sensitivity of PCR-dipstick chromatography assay for detection of single bacterium. (A) Acinetobacter baumannii, (B) Pseudomonas aeruginosa, (C) Klebsiella pneumoniae, (D) Haemophilus influenzae, (E) Streptococcus pneumoniae, (F) Staphylococcus aureus, (G) Mycoplasma pneumoniae, and (H) Chlamydia pneumoniae. 1: negative control; 2: 10 CFU/mL; 3: 102 CFU/mL; 4: 103 CFU/mL; 5: 104 CFU/mL; 6: 105 CFU/mL; 7: 106 CFU/mL; 8: 107 CFU/mL.
Clinical sample testing and qualitative analysis
A total of 186 sputum/BALF samples were analyzed using the PCR-dipstick DNA chromatography assay, and the results were compared with those obtained from the conventional culture method. The outcomes of the multiplex PCR-dipstick DNA chromatography method when testing the 186 clinical samples were as follows: A. baumannii was detected in 23 cases (Figure 5A), P. aeruginosa in 22 cases (Figure 5B), K. pneumoniae in 21 cases (Figure 5C), H. influenzae in 4 cases (Figure 5D), S. pneumoniae in 12 cases (Figure 5E), S. aureus in 14 cases (Figure 5F), M. pneumoniae in 15 cases (Figure 5G), C. pneumoniae in 11 cases (Figure 5H), and mixed infections in 17 cases (Figure 5I), with 47 cases yielding negative results (Figure 5J).
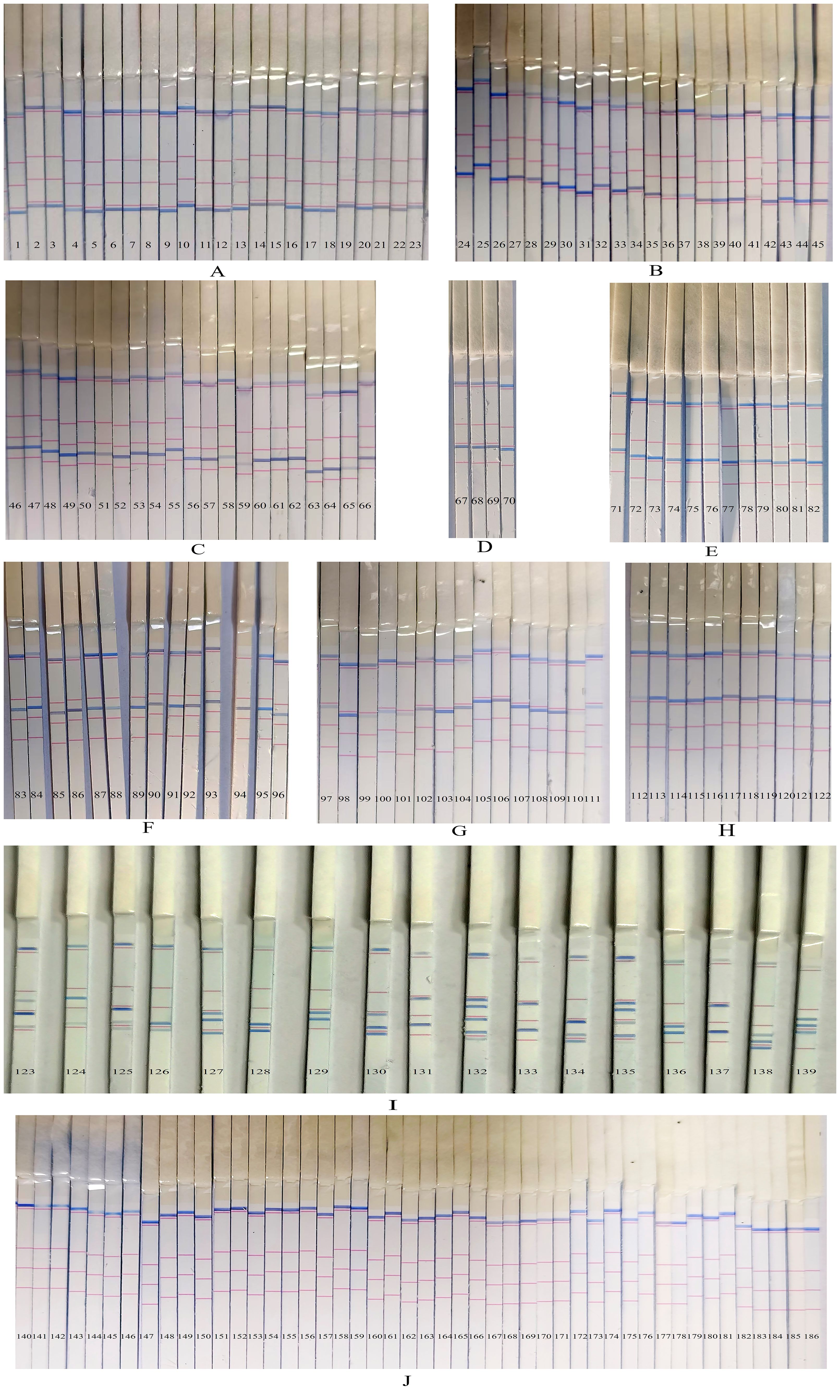
Figure 5. The results of the multiplex PCR-dipstick DNA chromatography method in testing clinical samples. (A) Acinetobacter baumannii in 23 cases, (B) Pseudomonas aeruginosa in 22 cases, (C) Klebsiella pneumoniae in 21 cases, (D) Haemophilus influenzae in 4 cases, (E) Streptococcus pneumoniae in 12 cases, (F) Staphylococcus aureus in 14 cases, (G) Mycoplasma pneumoniae in 15 cases, (H) Chlamydia pneumoniae in 11 cases, (I) 17 multiple pathogens cases, and (J) negative sample in 47 cases.
Conventional bacterial culture was also performed on all 186 samples. Among them, 24 samples grew A. baumannii. In one sample, the results differed from those of the PCR-dipstick DNA chromatography method, which detected a mixed infection of A. baumannii, P. aeruginosa, and K. pneumoniae (Figure 5I—138). This discrepancy between the two methods is due to the fact that the sensitivity of the PCR-dipstick DNA chromatography method was higher than that of traditional bacterial culture. Bacterial culture mainly isolates dominant bacteria, while other bacteria present at lower concentrations may be masked by the dominant ones. A total of 23 cases of P. aeruginosa were cultured, and in one case, the result was inconsistent with that of the PCR-dipstick DNA chromatography method. The PCR-dipstick DNA chromatography method detected a mixed infection of P. aeruginosa and A. baumannii (Figure 5I—126). It is presumed that the low concentration of A. baumannii in the sample was overshadowed by the dominant P. aeruginosa during cultivation. Additionally, 24 cases of K. pneumoniae were cultured, and in three cases, the results differed from those of the PCR-dipstick DNA chromatography method (Figure 5I—131, 133, 137). In these three cases, the PCR-dipstick DNA chromatography method indicated a mixed infection of K. pneumoniae and M. pneumoniae. The inconsistency arose because the culture conditions for M. pneumoniae were stringent, and conventional bacterial culture failed to cultivate it. Therefore, even if the bacterial concentration of M. pneumoniae was high in these samples, conventional culture methods may still miss it. A total of six cases of H. influenzae were cultured, and in two cases, the results were inconsistent with those of the PCR-dipstick DNA chromatography method (Figure 5I—123, 125). These two cases were detected as mixed infections by PCR-dipstick DNA chromatography, but the presence of other bacteria at low concentrations led to their overshadowing by the dominant H. influenzae during cultivation. Additionally, 12 cases of S. pneumoniae and 15 cases of S. aureus were cultured, and in one case, the result was inconsistent with that of the PCR-dipstick DNA chromatography method (Figure 5I—124). The PCR-dipstick DNA chromatography detected a mixed infection of S. aureus and P. aeruginosa, but the growth of P. aeruginosa was obscured by the dominant S. aureus, resulting in a false negative. In total, nine cases of mixed infections were identified via bacterial culture, and these samples also indicated mixed infections through PCR-dipstick DNA chromatography (Figure 5I—127, 128, 129, 130, 132, 134,135, 136, 139). However, bacterial cultures failed to detect M. pneumoniae in Figure 5I (132 and 135), while the low concentration of A. baumannii in Figure 5I (132) also went undetected. The results of the 17 cases of mixed-infection samples tested by the PCR-dipstick DNA chromatography assay and their corresponding bacterial culture results are presented in Table 2. Out of the 186 samples, 73 were negative for bacterial culture, primarily because the culturing conditions for M. pneumoniae were stringent and C. pneumoniae is an intracellular microorganism that cannot be cultured in vitro, making traditional culturing methods ineffective for detecting these pathogens.
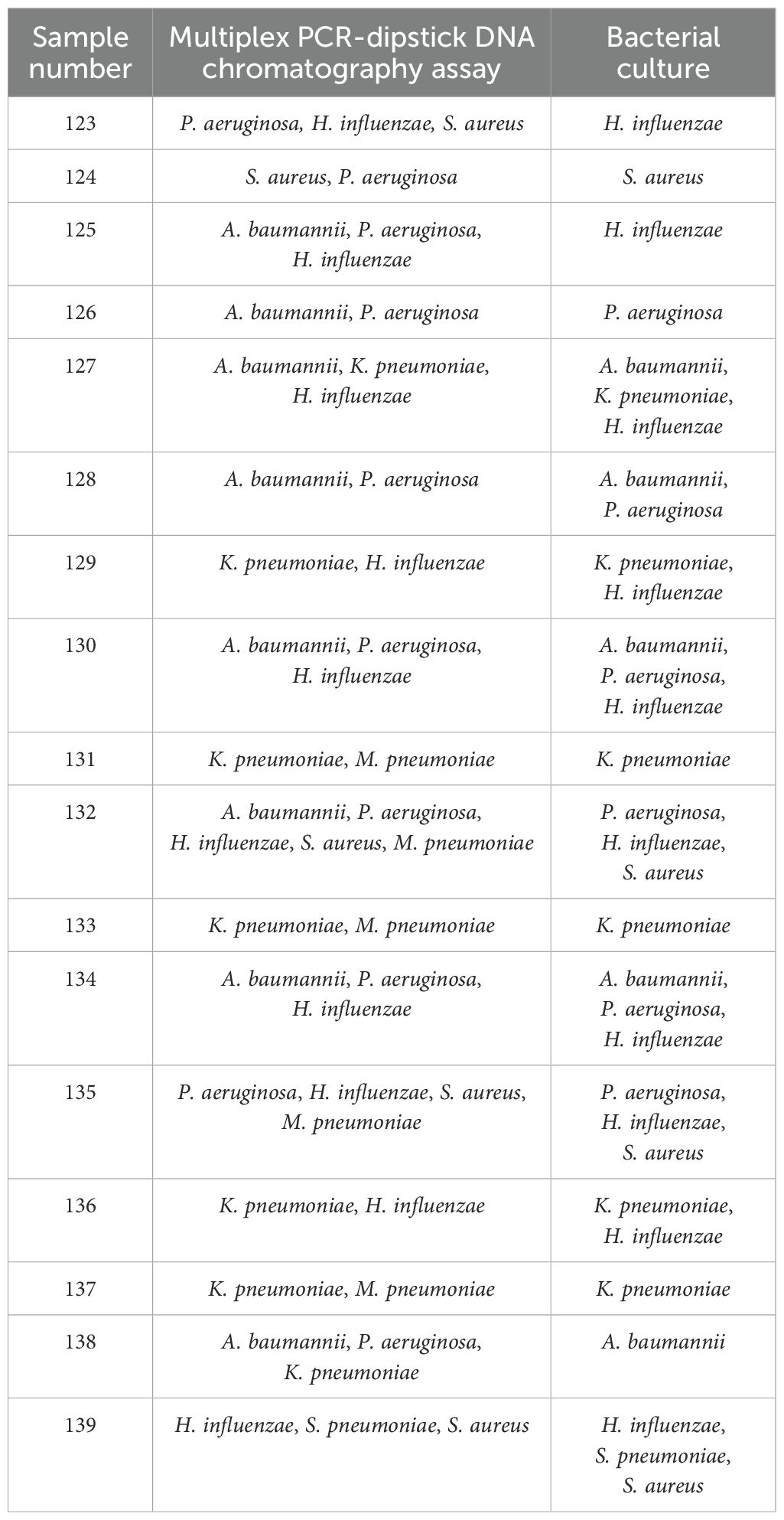
Table 2. The results of 17 cases of mixed-infection samples tested by the PCR-dipstick DNA chromatography assay and their corresponding bacterial culture results.
DNA sequencing
In order to verify the accuracy of the PCR-dipstick chromatography method for detecting PCR products, the PCR products of all clinical samples were subjected to DNA sequencing. DNA sequencing results were completely consistent with the qualitative results of PCR-dipstick chromatography assay, which proves no false negative and false positive for target detection. Consequently, the consistency between PCR-dipstick chromatography assay and DNA sequencing was 100%, and the kappa value was 1.00.
Discussion
In the present study, a PCR-dipstick chromatography assay capable of simultaneously detecting eight respiratory bacterial pathogens was successfully developed. The results demonstrated that all eight target bacteria could be precisely identified using PCR-dipstick chromatography, and no cross-reactivity was observed. The LOD of PCR-dipstick chromatography for individual bacteria ranges from 10 to 102 CFU/mL. There was no cross-reaction among the eight bacteria, nor among representative respiratory bacteria such as A. junii, E. cloacae, K. oxytoca, H. parainfluenzae, P. fluorescens, A. hydrophila, and S. epidermidis, highlighting the excellent specificity of the PCR-dipstick DNA chromatography method. The concordance rate between PCR-dipstick chromatography and DNA sequencing was 100%, indicating that the PCR-dipstick chromatography assay is simple, rapid, high-throughput, sensitive, and accurate and exhibits good diagnostic performance.
One of the prominent advantages of the PCR-dipstick chromatography method lies in its capacity to detect mixed pathogens within a single sample. We applied this assay to evaluate 186 clinical sputum/BALF samples and identified 17 cases of multiple pathogen infections. In contrast, the traditional bacterial culture method, regarded as the gold standard for diagnosis, detected only nine cases of mixed infections. Moreover, for bacteria present at low concentrations, dominant species during culture can mask their detection, leading to false negatives. This not only hampers clinicians’ ability to prescribe appropriate antibiotics but also prolongs the duration of patient infections. Importantly, in recent years, infections caused by M. pneumoniae and C. pneumoniae have become increasingly prevalent in respiratory infections, accounting for approximately 10%–40% and 5%–10% of infections in children, respectively, with a 1%–2% co-infection rate of both pathogens (Chen et al., 2013; Defilippi et al., 2008; Hamano-Hasegawa et al., 2008). However, the cultivation conditions for M. pneumoniae are stringent and time-consuming and yield low positivity rates, rendering traditional bacterial culture inadequate for meeting the rapid diagnostic requirements of clinical practice (Zhao et al., 2020; Qu et al., 2022). As an intracellular microorganism, C. pneumoniae cannot be cultured in vitro. Consequently, traditional bacterial culture failed to detect M. pneumoniae and C. pneumoniae infections in the 186 samples analyzed. In our study, the PCR-dipstick chromatography method performed well in detecting infections caused by these two pathogens, with a sensitivity of 10 CFU/mL.
Quantifying the target pathogen is essential for differentiating the relative abundance of bacterial infections since changes in bacterial concentration before and after treatment can signify the effectiveness of the therapy. In the current study, when the bacterial concentration was between 10 and 107 CFU/mL, the intensity of the color of the single-bacterial detection line increased with the rise in bacterial concentration (Figure 4). Therefore, we could approximately determine the change in single-bacterial concentration of the sample based on the color intensity of the DNA detection line for each order of magnitude. However, we noted that the relationship between the color intensity of the detection line and the bacterial concentration was weakened in the multi-target pathogen response. This could be attributed to the competition between streptavidin-coated blue latex microspheres. For bacteria of the same order, the detection line color of single bacteria was stronger than that of multiple target bacteria. The semi-quantitative results for multiple pathogens were lower than the actual bacterial concentration. Nevertheless, even though the semi-quantitative results of multiple infection samples were not accurate, as a qualitative analysis, the PCR-dipstick chromatography assay could still indicate which bacteria dominated in the same sample, which is of significant clinical value.
The most conspicuous limitation of the PCR-dipstick chromatography assay was the inaccurate quantification of multiple pathogens in a sample. Consequently, clinicians must make a comprehensive judgment based on the sample source, disease conditions, and the relative concentrations of multiple pathogens. To overcome this drawback, we will further investigate the relationship between the detection line color intensity of multiple infections and the concentration of bacteria by analyzing a large number of multiple infection clinical samples. Additionally, the PCR-dipstick chromatography method can only analyze a limited number of species, while the bacteria associated with respiratory infection are complex and diverse. A single strip could only identify eight related bacterial pathogens, which oversimplified the actual microflora of respiratory tract infection. Therefore, a negative sample identified by the PCR-dipstick chromatography method could only indicate the absence of the eight bacterial infections, but other pathogenic microorganisms could not be excluded. In fact, the defined bacterial species may not be directly involved in the etiology of a disease, and pathogens other than these eight bacteria may also be the main causative agents. Although the test strip DNA biosensor platform can be constructed according to different needs and used for multiple detections of different pathogens, with the continuous addition of targets in a strip, the competition between target primers and non-specific amplifications will increase, and sensitivity and specificity will decline, making it difficult to achieve ultra-high-throughput detection. With the development of the signal processing, probe, and multiplex PCR technologies of the strip biosensor, additional bacterial species related to respiratory tract infections should be incorporated into the PCR-dipstick chromatography method.
Conclusion
A highly effective multiplex PCR-dipstick DNA chromatography assay was successfully established. This assay enabled the simultaneous detection of eight respiratory bacterial pathogens and was seamlessly integrated into clinical sample analysis. The results unequivocally suggest that this single-use, disposable device holds substantial promise for dissecting the microbial composition associated with respiratory infections. Its simplicity and portability make it an ideal choice for small laboratories and field diagnostics, potentially revolutionizing the way respiratory infections are diagnosed and managed.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Medical ethics committee of the People’s Hospital of Guangxi Zhuang Autonomous Region. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LH: Conceptualization, Funding acquisition, Investigation, Writing – original draft, Writing – review & editing, Software. XW: Investigation, Methodology, Validation, Writing – review & editing, Data curation, Formal analysis, Project administration, Resources, Supervision, Visualization. QL: Data curation, Formal analysis, Methodology, Project administration, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Guangxi Natural Science Foundation under Grant No. 2024GXNSFBA010122.
Conflict of interest
Author QL was employed by Guangzhou Baochuang Biotechnology Co., Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abdelrasoul, G. N., Anwar, A., MacKay, S., Tamura, M., Shah, M. A., Khasa, D. P., et al. (2020). DNA aptamer-based non-faradaic impedance biosensor for detecting E. coli. Anal. Chim. Acta 1107, 135–144. doi: 10.1016/j.aca.2020.02.004
Ang, G. Y., Yu, C. Y., and Yean, C. Y. (2012). Ambient temperature detection of PCR amplicons with a novel sequence-specific nucleic acid lateral flow biosensor. Biosens. Bioelectron. 38, 151–156. doi: 10.1016/j.bios.2012.05.019
Bahavarnia, F., Mobed, A., Hasanzadeh, M., Saadati, A., Hassanpour, S., and Mokhtarzadeh, A. (2020). Bio-assay of Acintobacter baumannii using DNA conjugated with gold nano-star: A new platform for microorganism analysis. Enzyme Microb. Technol. 133, 109466. doi: 10.1016/j.enzmictec.2019.109466
Banakar, M., Hamidi, M., Khurshid, Z., Zafar, M. S., Sapkota, J., Azizian, R., et al. (2022). Electrochemical biosensors for pathogen detection: an updated review. Biosensors 12. doi: 10.3390/bios12110927
Beck, A. F., Florin, T. A., Campanella, S., and Shah, S. S. (2015). Geographic variation in hospitalization for lower respiratory tract infections across one county. JAMA Pediatr. 169, 846–854. doi: 10.1001/jamapediatrics.2015.1148
Cao, Y. C., Wang, Z., Wang, H. Q., Wang, J. H., Hua, X. F., Jin, X., et al. (2009). Enhanced optical property of Au coated polystyrene beads for multi-color quantum dots encoding. J. nanoscience nanotechnology 9, 1778–1784. doi: 10.1166/jnn.2009.396
Carvalhaes, C. G., Huband, M. D., Reinhart, H. H., Flamm, R. K., and Sader, H. S. (2019). Antimicrobial activity of omadacycline tested against clinical bacterial isolates from hospitals in mainland China, Hong Kong, and Taiwan: results from the SENTRY antimicrobial surveillance program, (2013 to 2016). Antimicrob. Agents Chemother. 63. doi: 10.1128/AAC.02262-18
Chen, F., Di, T., Yang, C. T., Zhang, T., Thierry, B., and Zhou, X. (2020). Naked-eye enumeration of single chlamydia pneumoniae based on light scattering of gold nanoparticle probe. ACS sensors 5, 1140–1148. doi: 10.1021/acssensors.0c00150
Chen, Z., Ji, W., Wang, Y., Yan, Y., Zhu, H., Shao, X., et al. (2013). Epidemiology and associations with climatic conditions of Mycoplasma pneumoniae and Chlamydophila pneumoniae infections among Chinese children hospitalized with acute respiratory infections. Ital. J. Pediatr. 39, 34. doi: 10.1186/1824-7288-39-34
Chen, X., Liu, N., Liu, L., Chen, W., Chen, N., Lin, M., et al. (2019). Thermodynamics and kinetics guided probe design for uniformly sensitive and specific DNA hybridization without optimization. Nat. Commun. 10, 4675. doi: 10.1038/s41467-019-12593-9
Defilippi, A., Silvestri, M., Tacchella, A., Giacchino, R., Melioli, G., Di Marco, E., et al. (2008). Epidemiology and clinical features of Mycoplasma pneumoniae infection in children. Respir. Med. 102, 1762–1768. doi: 10.1016/j.rmed.2008.06.022
Fadlalla, M. H., Ling, S., Wang, R., Li, X., Yuan, J., Xiao, S., et al. (2020). Development of ELISA and lateral flow immunoassays for ochratoxins (OTA and OTB) detection based on monoclonal antibody. Front. Cell. infection Microbiol. 10, 80. doi: 10.3389/fcimb.2020.00080
Hamano-Hasegawa, K., Morozumi, M., Nakayama, E., Chiba, N., Murayama, S. Y., Takayanagi, R., et al. (2008). Comprehensive detection of causative pathogens using real-time PCR to diagnose pediatric community-acquired pneumonia. J. infection chemotherapy 14, 424–432. doi: 10.1007/s10156-008-0648-6
Hayashi, M., Natori, T., Kubota-Hayashi, S., Miyata, M., Ohkusu, K., Kawamoto, K., et al. (2013). A new protocol to detect multiple foodborne pathogens with PCR dipstick DNA chromatography after a six-hour enrichment culture in a broad-range food pathogen enrichment broth. BioMed. Res. Int. 2013, 295050. doi: 10.1155/2013/295050
He, X., Xie, M., Li, S., Ye, J., Peng, Q., Ma, Q., et al. (2017). Antimicrobial resistance in bacterial pathogens among hospitalized children with community acquired lower respiratory tract infections in Dongguan, China, (2011-2016). BMC Infect. Dis. 17, 614. doi: 10.1186/s12879-017-2710-4
Hu, L., Han, B., Tong, Q., Xiao, H., and Cao, D. (2020). Detection of eight respiratory bacterial pathogens based on multiplex real-time PCR with fluorescence melting curve analysis. Can. J. Infect. Dis. Med. Microbiol. = J. canadien Des. maladies infectieuses la microbiologie medicale 2020, 2697230. doi: 10.1155/2020/2697230
Huang, L., Tian, S., Zhao, W., Liu, K., Ma, X., and Guo, J. (2020). Multiplexed detection of biomarkers in lateral-flow immunoassays. Analyst 145, 2828–2840. doi: 10.1039/C9AN02485A
Khadanga, S., Karuna, T., Thatoi, P. K., and Behera, S. K. (2014). Changing bacteriological profile and mortality trends in community acquired pneumonia. J. Glob. Infect. Dis. 6, 186–188. doi: 10.4103/0974-777X.145251
Kotula, J. J., 3rd, Moore, W. S., 2nd, Chopra, A., and Cies, J. J. (2018). Association of procalcitonin value and bacterial coinfections in pediatric patients with viral lower respiratory tract infections admitted to the pediatric intensive care unit. J. Pediatr. Pharmacol. therapeutics: JPPT: Off. J. PPAG 23, 466–472. doi: 10.5863/1551-6776-23.6.466
Liles, V. R., Pangilinan, L. S., Daroy, M. L. G., Dimamay, M. T. A., Reyes, R. S., Bulusan, M. K., et al. (2019). Evaluation of a rapid diagnostic test for detection of dengue infection using a single-tag hybridization chromatographic-printed array strip format. Eur. J. Clin. Microbiol. Infect. Dis. 38, 515–521. doi: 10.1007/s10096-018-03453-3
Liu, P., Xu, M., He, L., Su, L., Wang, A., Fu, P., et al. (2018). Epidemiology of respiratory pathogens in children with lower respiratory tract infections in Shanghai, China, from 2013 to 2015. Jpn. J. Infect. Dis. 71, 39–44. doi: 10.7883/yoken.JJID.2017.323
Luo, L., Chen, Q., Qin, S., Luo, Q., Liu, Z., Li, Q., et al. (2021). Design and evaluation of multiplex one-step reverse transcription PCR-dipstick chromatography method for the analysis of seven respiratory pathogens. Curr. Microbiol. 78, 3656–3666. doi: 10.1007/s00284-021-02621-7
Mangold, K. A., Santiano, K., Broekman, R., Krafft, C. A., Voss, B., Wang, V., et al. (2011). Real-time detection of blaKPC in clinical samples and surveillance specimens. J. Clin. Microbiol. 49, 3338–3339. doi: 10.1128/JCM.00268-11
Menon, T., Gopalakrishnan, S. N., Balasubramanian, R., and Justin, S. R. (2017). Characterisation of the human oral microbiome in patients with coronary artery disease using next-generation sequencing of 16SrRNA amplicons. Indian J. Med. Microbiol. 35, 101–104. doi: 10.4103/ijmm.IJMM_16_370
Niwa, K., Oribe, A., Okumura, H., Shimono, M., Nagai, K., Hirota, T., et al. (2014). Tag/hybridization-based sensitive detection of polymerase chain reaction products. Anal. Biochem. 464, 12–16. doi: 10.1016/j.ab.2014.07.010
Noviello, S. and Huang, D. B. (2019). The basics and the advancements in diagnosis of bacterial lower respiratory tract infections. Diagnostics (Basel Switzerland) 9. doi: 10.3390/diagnostics9020037
Özgür, E., Topçu, A. A., Yılmaz, E., and Denizli, A. (2020). Surface plasmon resonance based biomimetic sensor for urinary tract infections. Talanta 212, 120778. doi: 10.1016/j.talanta.2020.120778
Price, O. H., Sullivan, S. G., Sutterby, C., Druce, J., and Carville, K. S. (2019). Using routine testing data to understand circulation patterns of influenza A, respiratory syncytial virus and other respiratory viruses in Victoria, Australia. Epidemiol. infection 147, e221. doi: 10.1017/S0950268819001055
Qu, J., Zhang, J., Chen, Y., Huang, Y., Xie, Y., Zhou, M., et al. (2022). Aetiology of severe community acquired pneumonia in adults identified by combined detection methods: a multi-centre prospective study in China. Emerging microbes infections 11, 556–566. doi: 10.1080/22221751.2022.2035194
Shanmugakani, R. K., Akeda, Y., Yamamoto, N., Sakamoto, N., Hagiya, H., Yoshida, H., et al. (2017). PCR-dipstick chromatography for differential detection of carbapenemase genes directly in stool specimens. Antimicrob. Agents Chemother. 61. doi: 10.1128/AAC.00067-17
Simpson, C. R., Steiner, M. F., Cezard, G., Bansal, N., Fischbacher, C., Douglas, A., et al. (2015). Ethnic variations in morbidity and mortality from lower respiratory tract infections: a retrospective cohort study. J. R. Soc Med. 108, 406–417. doi: 10.1177/0141076815588321
Song, C., Chorath, J., Pak, Y., and Redjal, N. (2019). Use of dipstick assay and rapid PCR-DNA analysis of nasal secretions for diagnosis of bacterial sinusitis in children with chronic cough. Allergy rhinology (Providence R.I.) 10, 2152656718821281. doi: 10.1177/2152656718821281
Tian, L., Sato, T., Niwa, K., Kawase, M., Mayanagi, G., Washio, J., et al. (2016). PCR-dipstick DNA chromatography for profiling of a subgroup of caries-associated bacterial species in plaque from healthy coronal surfaces and periodontal pockets. Biomed. Res. 37, 29–36. doi: 10.2220/biomedres.37.29
Tian, L., Sato, T., Niwa, K., Kawase, M., Tanner, A. C., and Takahashi, N. (2014). Rapid and sensitive PCR-dipstick DNA chromatography for multiplex analysis of the oral microbiota. BioMed. Res. Int. 2014, 180323. doi: 10.1155/2014/180323
Uzoamaka, M., Ngozi, O., Johnbull, O. S., and Martin, O. (2017). Bacterial etiology of lower respiratory tract infections and their antimicrobial susceptibility. Am. J. Med. Sci. 354, 471–475. doi: 10.1016/j.amjms.2017.06.025
van de Pol, A. C., van Loon, A. M., Wolfs, T. F., Jansen, N. J., Nijhuis, M., Breteler, E. K., et al. (2007). Increased detection of respiratory syncytial virus, influenza viruses, parainfluenza viruses, and adenoviruses with real-time PCR in samples from patients with respiratory symptoms. J. Clin. Microbiol. 45, 2260–2262. doi: 10.1128/JCM.00848-07
Vink, M. A., Bootsma, M. C., and Wallinga, J. (2014). Serial intervals of respiratory infectious diseases: a systematic review and analysis. Am. J. Epidemiol. 180, 865–875. doi: 10.1093/aje/kwu209
Wang, Q. Y., Li, C. R., Guo, J., and Tang, K. W. (2019). Bacteriologic profile and drug resistance in children with respiratory infection from 2016 to 2018. Zhongguo Dang Dai Er Ke Za Zhi 21, 1182–1187.
Yun, K. W., Wallihan, R., Juergensen, A., Mejias, A., and Ramilo, O. (2019). Community-acquired pneumonia in children: myths and facts. Am. J. Perinatol 36, S54–s57. doi: 10.1055/s-0039-1691801
Keywords: multiplex PCR-dipstick DNA chromatography assay, lower respiratory tract infection, eight respiratory bacterial pathogens, rapid detection, multiple detection
Citation: Hu L, Wang X and Li Q (2025) Methodology and application of multiplex PCR-dipstick DNA chromatography for the detection of eight respiratory bacterial pathogens. Front. Cell. Infect. Microbiol. 15:1558612. doi: 10.3389/fcimb.2025.1558612
Received: 10 January 2025; Accepted: 17 April 2025;
Published: 27 May 2025.
Edited by:
Michael Marceau, Université Lille Nord de France, FranceCopyright © 2025 Hu, Wang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiuri Wang, Mjg2NDE1MjA5NEBxcS5jb20=
†These authors have contributed equally to this work and share first authorship
 Liuyang Hu
Liuyang Hu Xiuri Wang2*†
Xiuri Wang2*†