- 1National Institute for Health Innovation, University of Auckland, Auckland, New Zealand
- 2Waitemata District Health Board, Auckland, New Zealand
- 3Counties-Manukau District Health Board, Auckland, New Zealand
- 4Auckland Bioengineering Institute, University of Auckland, Auckland, New Zealand
- 5Health and Rehabilitation Research Institute, Auckland University of Technology, Auckland, New Zealand
- 6School of Computer Science, University of Auckland, Auckland, New Zealand
Background: Pulmonary rehabilitation (PR) has been proven effective but is not well accessed due to transport, time, cost, and physical limitations of patients. We have developed a mobile phone-based PR program (mPR) that could be offered as an alternative for those unable to attend in-person. This was developed following formative research with patients, their families and clinicians. mPR has a core text message program plus an app that includes an action plan, exercise videos, lung visualization, symptom score questionnaire and 1-min sit-to-stand test.
Aims: To determine the feasibility of delivering pulmonary rehabilitation by mobile phone.
Methods: A 9-week non-randomized (1-arm) pilot study was conducted. Participants were 26 adults with chronic obstructive pulmonary disease plus four family members, who were offered participation at first assessment or during group PR sessions. Outcomes included satisfaction, engagement with the program, and perceived impacts.
Results: Eight people (31%) opted for text messages only, and 18 (69%) chose text messages plus the app. Three people stopped the program early, 20 said they would recommend it to others, 19 said it helped them to feel more supported, 17 said it helped them to change their behavior.
Conclusion: It is feasible to deliver PR support via mobile phone, including exercise prescription and support. Our mPR program was appreciated by a small number of people with chronic respiratory disorders and family members. Suggestions for improvements are being used to inform the further development of the program, which will then be tested for effectiveness. Registered with the Australia New Zealand Clinical Trials Registry ACTRN12619000884101 (www.anzctr.org.au).
Introduction
Pulmonary rehabilitation (PR) has been shown to be effective in improving symptoms and quality of life in people with chronic respiratory disorders (McCarthy et al., 2015). PR is a structured program involving exercise training, education and behavior change, which is designed to improve a patient’s physical and psychological health (Spruit et al., 2013). However only a very small proportion of those eligible access PR for reasons including transport, time off work, difficulty attending due to symptoms of their illness, lack of perceived benefit, and depression (Hayton et al., 2013; Guo and Bruce, 2014; Harrison et al., 2015). In recent times, those with long term respiratory disorders may be even more reluctant to attend group sessions, particularly those based in hospitals, due to the risk of COVID-19 infection. To increase the accessibility of PR (and consequently reduce the risk to this vulnerable population) we wanted to determine whether many of the aspects of PR could be delivered using mobile phones, in the same way other long-term condition self-management support programs have successfully been delivered (Chow et al., 2015; Dobson et al., 2018; Dobson et al., 2019b).
This project aims to develop a mobile phone-based PR support program using the steps outlined in the mHealth Development and Evaluation Framework (Whittaker et al., 2012). Formative work undertaken for this project found high interest in mPR from both patients and healthcare professionals (Dobson et al., 2019a). Both patients and healthcare professionals identified potential for an mPR program to overcome current barriers to traditional PR programs but had concerns regarding technology and the lack of a group environment within a digital program. Differing technology access, digital literacy and patient characteristics highlighted the need for a range of solutions to meet individual needs. There were differing views on how a potential mPR program should be accessed or how the program should sit in relation to current PR models of care. The findings from the formative work has led to the development of an mPR prototype intervention including a personally tailored text message program (mPR-SMS) and a personally tailored smartphone app (mPR-app).
The mPR prototype is an individually tailored and theoretically based PR intervention designed to support people with chronic respiratory conditions to: 1) Increase exercise capacity; 2) Increase health related quality of life; and 3) Decrease hospitalisations for acute exacerbations. The program is designed to support people (and their families) before, during, or after PR, or as an alternative for those not able to access traditional PR services. mPR consists of a core text message program with an optional mPR-app. In line with the findings from the formative work, a core text message program ensures that the intervention is accessible to everyone regardless of level of digital access and digital literacy.
The aim of this study was to pilot the prototype to assess the feasibility, acceptability and usability of a prototype mPR intervention, in order to inform the potential further development of a comprehensive integrated and adaptive mPR intervention.
Methods
A nine-week, non-randomized one-arm pilot intervention study was conducted between July and November 2019. All study documents and procedures were approved by the Health and Disability Ethics Committee (19/NTA/74). It was registered with the Australia New Zealand Clinical Trials Registry (ACTRN12619000884101).
Intervention
The content for the mPR program was developed by a multidisciplinary team including physiotherapists, a respiratory physician, a health psychologist, a public health physician, mHealth behavior change experts, computer scientists, patients and engineers. The development of this program followed the mHealth Development and Evaluation framework (Whittaker et al., 2012), which provides a process to guide the development and testing of mHealth interventions with a focus on implementation, behavioral change theory, and involvement of the target population. The development of the content was informed by a review of current PR program content, literature, existing mHealth interventions, patient resources, and our formative research with the target audience (Dobson et al., 2019a). The program was informed by behavior change theories and incorporates behavior change techniques (BCTs) (Michie et al., 2013) including information about health consequences, social support, (practical) instructions on how to perform the behavior, and graded tasks.
Participants could stop the intervention and any of its components at any time by free texting back “STOP” and uninstalling the app.
mPR Text Messages
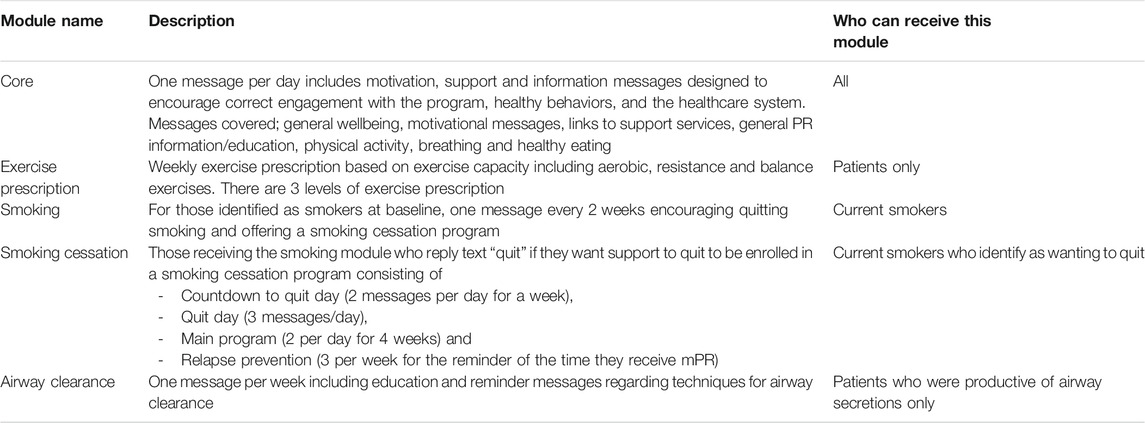
mPR consisted of a personally tailored package of text messages over a 9-week period. Different modules allowed content to be tailored to individual clinical characteristics, preferences and demographics. All participants received one mPR information/support message per day. In addition, smokers received a smoking module (encouraging consideration of quitting smoking) and an airway clearance module was available for participants who experienced increased respiratory secretions. All participants were also allocated an exercise prescription module based on their baseline exercise capacity and dyspnoea score as defined by the PR physiotherapist. Current smokers could opt to add a proven smoking cessation program (Bramley et al., 2005; Rodgers et al., 2005). Table 1 provides more specific detail of the content of the modules. Family members who signed up for the program received core messages and could also receive the smoking module if a smoker. Messages across all modules were tailored and personalized by culture, the person’s name, their motivations and the names of their support people.
Message delivery was managed by a specifically developed content management system, with messages sent and received through a gateway company to allow for participants to be registered with any New Zealand mobile network. The system maintained logs of all outgoing and incoming messages.
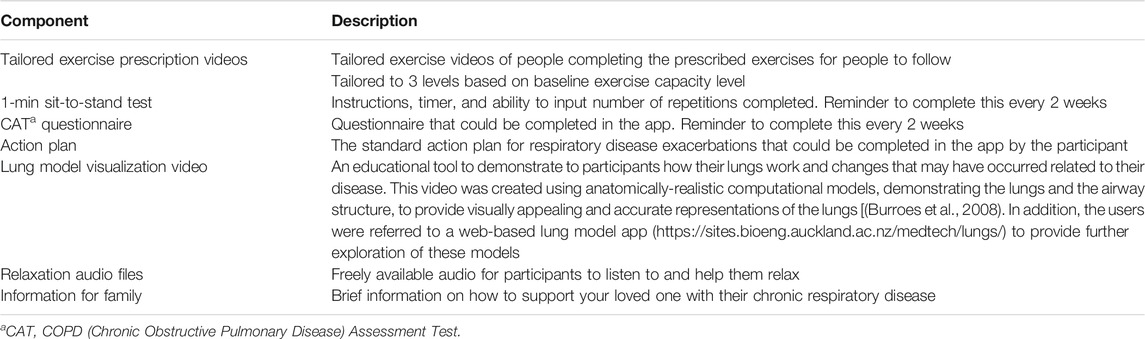
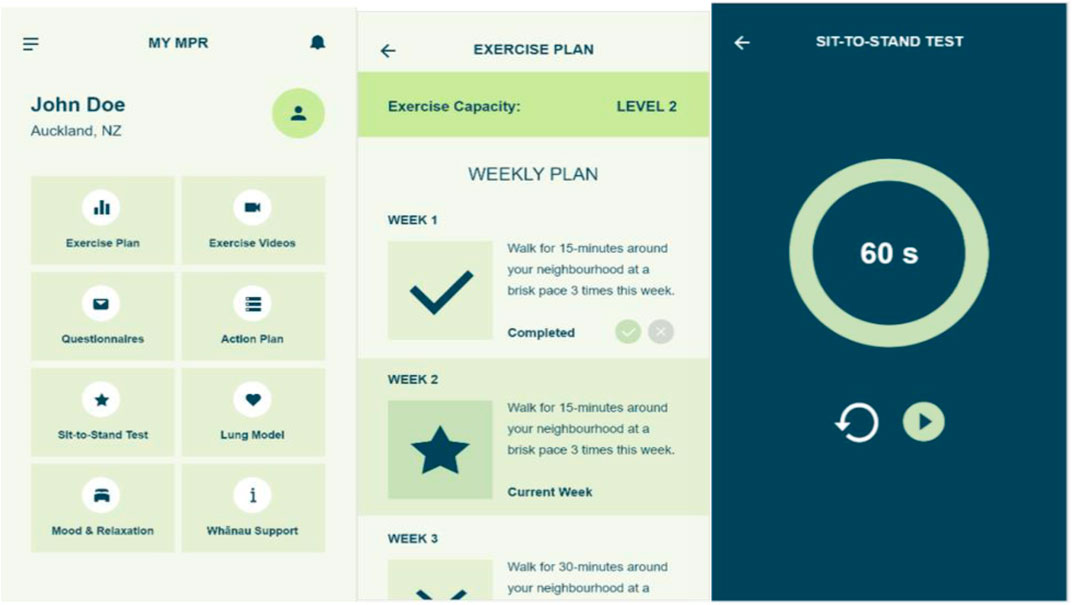
mPR app
The mPR app was designed to complement the text message program and was developed by students and staff under the supervision of the study team (see Table 2 for components and Figure 1 for screenshots). It was loaded onto the Apple and Play app stores for download and was accessed using a study specific code. Each individual’s profile was set up according to their baseline exercise prescription level.
Although no specific instructions were given to those choosing the app, participants may have been expected to use it approximately three times per week in order to view the exercise videos three times weekly and relaxation audio as needed. Other aspects of the app would expect to be used less frequently (for example, 1-min sit-to-stand test and CAT questionnaire every two weeks; lung model visualization and information for family only as desired).
Exercise Prescription
A key component of the mPR program is the exercise prescription. To ensure appropriateness, this was tailored to baseline exercise capacity. Participants were stratified to one of three exercise levels (1, 2, or 3). The exercise level was determined from their initial assessment findings, including; balance, dyspnoea score [MMRC Dyspnoea Scale Score (Bestall et al., 1999)] and functional exercise capacity [6-min walk test, 6 MWT (Holland et al., 2014)]. The exercise program included a generic warm up, walking program, and resistance training for upper and lower limbs using hand held weights. The level one program also included balance exercises. Participants were advised to exercise on five days of the week. The program was incremental - each week either the walking time, or the number of repetitions of strengthening exercises, increased. The progressed exercise prescription was sent to participants via SMS and updated on the mPR app. Participants were given instructions to use a scale of breathlessness (modified BORG scale) to guide the intensity of exercise. Participants were provided with instructions on how to complete each of the exercises as well as advice on when to stop exercise should they have pain or feel unwell.
The program was also adaptive to the patient’s current health state utilizing assessment via free reply message. From week 2, each week the participant received a message asking for their current rating of their health on a Visual Analogue Scale (VAS) from 1 to 10. If their health was rated three or above, they received a reply message with the exercise prescription recommendation for the week corresponding to the level associated with their baseline exercise capacity (level 1, 2, or 3). If their current health was rated less than three then no exercise prescription was sent, and a general self-care message sent instead. If people did not respond or reported ratings of less than three for three weeks in a row, a tailored message was sent to encourage them to engage with their clinical team.
The program was also designed to monitor compliance with exercise prescription by 2-way messaging. At the end of each week a message was sent asking how many times they completed the exercise prescription for that week. An automated response was sent based on the number of times they had completed the prescription designed to congratulate them and encourage continued engagement with the program.
Participants and Recruitment
Eligibility criteria included adults aged 16 years and over with a chronic respiratory disease e.g., chronic obstructive pulmonary disease (COPD), being eligible for PR, having completed a PR initial assessment by a PR clinician, being able to read and understand English, being able to provide informed consent, and owning or with regular access to a mobile phone. The only reason for exclusion aside from the above criteria was not being available for the duration of the study. Recruitment was carried out in two secondary care hospitals in Auckland, New Zealand. Clinicians at each site identified potential participants and gave them information about the study. Informed consent was obtained before the participant was registered for the study and baseline assessment completed. The clinician then explained the exercise prescription, including providing demonstrations of each exercise and written instructions on how to perform them correctly.
Participants were asked about their intervention preferences (whether they wanted the mPR app alongside the core text message program) and intervention tailoring factors including cultural version, preferred message delivery time, names of support people and motivations. Participants were asked if a family member would be interested in also receiving the program, and if so, they were contacted separately to inform them about the study and complete informed consent.
The program was completely free to receive (no costs for text messaging or apps). Participants were given a voucher at the conclusion of the study to reimburse them for their time.
Safety
Participants were advised to contact the study physiotherapist (SC) if there were any issues arising from participation in the program. Multiple contact methods were provided.
Measures
Baseline measures were those routinely collected at assessment including demographics, exercise capacity and clinical measures [MMRC Dyspnea Scale Score (Bestall et al., 1999), 6-min walk test (6 MWT) (Holland et al., 2014), 1 min sit-to-stand test (Vaidya et al., 2016)], plus symptom and quality of life measures [COPD Assessment Test, CAT (Jones et al., 2009)].
At the end of the nine-week program all participants (including those that stopped the intervention) were invited to complete questions about their satisfaction with the program, its usefulness and usability, and perceived impacts via a semi-structured telephone interview conducted by a research assistant. Engagement with the intervention was assessed using self-reports and system-recorded measures including text message responses and app data. In addition, participants were invited to repeat the exercise capacity and quality of life measures from baseline in person with the referring clinician for the purpose of assessing the feasibility of using these measures in the mPR context.
Statistical Analysis
Descriptive statistics were generated for baseline demographic and clinical characteristics, and measures of engagement with the system. Qualitative comments were analyzed using a simple, content analysis approach to identify common themes and meanings from the data.
Results
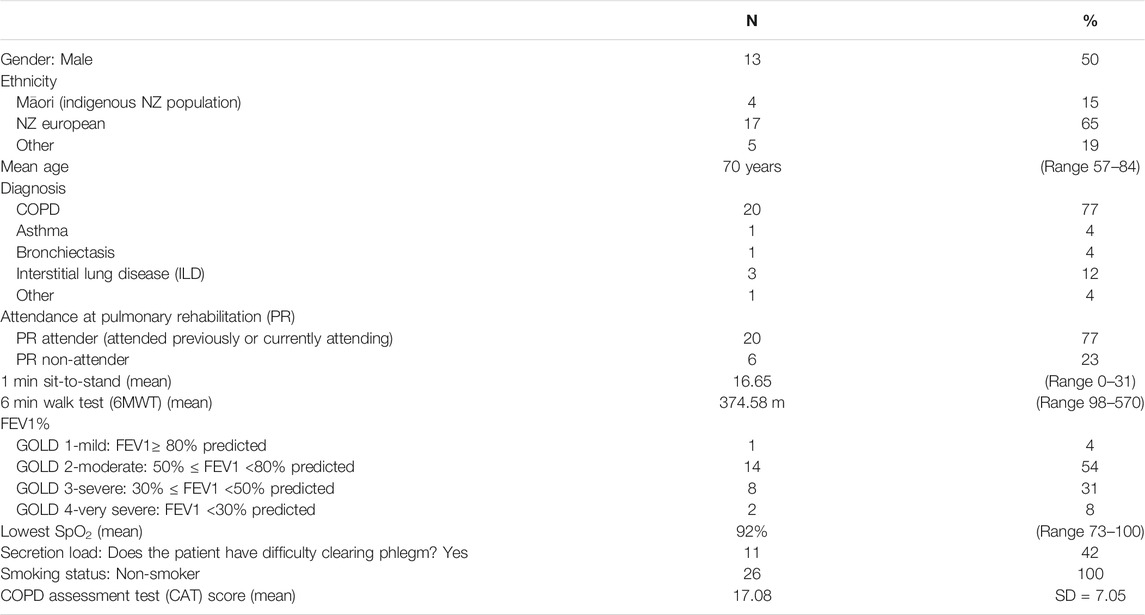
A total of 30 people registered for the mPR pre-testing study with 26 patients recruited and four of their whānau (family members) invited and consenting to participate. Table 3 presents characteristics of the patient participants only.
Three of the 26 (10%) participants requested to stop the program early, one during the second week of messages due to the program being too simple for what he wanted, and two in the eighth week of messages, one of which went overseas and one whose health deteriorated significantly.
Of the 26 patient participants enrolled, six (23%) were lost to follow-up: one was too unwell, one had a family bereavement, one was overseas during the follow up period, two were unable to be contacted and one declined due to commitments. The 20 who provided follow-up interviews were representative of the full group (that is, there were no major differences in demographics or condition).
Seventeen (85%) of the 26 participants completed the 1-min sit-to-stand at follow-up, 19 (95%) completed the 6-min walk test and 16 (80%) the CAT questionnaire, indicating that it was feasible for these outcome measures to be used as part of the mPR program. Due to this being a small pilot study, not powered for testing significance in these outcomes, change in the outcomes was not assessed.
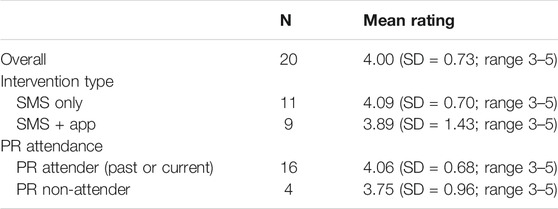
All participants (n = 20) reported that they would recommend the program to other people with chronic respiratory conditions. A total of 17 participants (85%) reported that the program had helped them to learn about their condition. Almost all reported the program made them feel more supported with their condition (19; 95%). All bar the participant who withdrew early due to the program being too simplistic, reported the program to be useful (19/20; 95%). Mean ratings of usefulness are shown in Table 4.
Participants were asked what they liked most about the program. The most common themes included that it was motivational and empowering (n = 8) and provided reminders and prompts (n = 8). Other themes included: that it was supportive (n = 3); it increased awareness and knowledge (n = 4); it increased confidence (n = 1); the exercise component and becoming more active (n = 2); and that you could do the program at your own pace (n = 1).
“Liked it because it motivated me, mostly when I got the texts every day, it was like they were there with me, I found it really good” (Female, 65–74 years, ID#20)
“Keeps it [exercising] in the front of your mind and you can’t ignore” (Female, 65–74 years, ID#3)
“Someone checking in on you.” (Female, 65–74 years, ID#12)
When asked what they liked least about the program, themes included: nothing (n = 5); the exercises were too hard, progressing too quickly or exercise frequency unrealistic (n = 5); that the messages were not personalized enough (e.g., not specific to condition, irrelevant/inappropriate messages, n = 4); lack of feedback during the program (n = 1).
“None. Should be compulsory with attending PR” (Male, 65–74 years, ID#10)
Exercise Prescription
There were three participants (12%) allocated to the level 1 exercise prescription, 20 (77%) level 2, and three (12%) level 3. Of the 26 patients receiving the program, there were four (15%) who did not respond to any of the question messages rating their health and therefore received no exercise prescriptions during the program, and eight (31%) who responded to all eight health ratings. There were two participants who rated their health at a level below the cut-off to get an exercise prescription for the week. On average participants received five exercise prescriptions (range 0–8).
At the end of each week that participants received an exercise prescription, they were asked to provide the number of times (0–5) they completed the prescription via reply message. Seven out of the 22 participants (32%) responded to all these questions, with participants responding on average to 64% of these question messages.
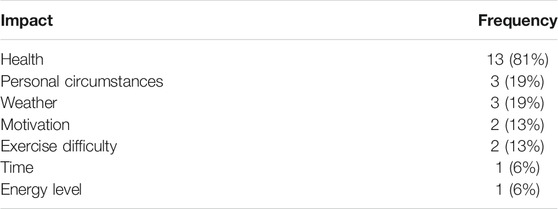
Participants stated that they liked the exercise program (n = 18, 2 did not answer this question) although 16 (80%) reported that there had been reasons that impacted their ability to perform the exercises. Table 5 presents the frequencies of reported impacts.
Engagement
At registration eight people (31%) opted for text messages only, and 18 (69%) chose to also download the mPR app. Participants reported that they read “all or nearly all of the messages” (19; 95%) or “most, more than half” of the messages (1; 5%). There were 12 (60%) participants who reported that they shared the messages with others. When asked about the dosage of messages, 12 (60%) felt that they received the right number of messages whereas seven (35%) reported that there were too many (one did not answer this question).
Of the 16 participants who selected to receive the app at registration, only 11 accessed the app (that is, completed app registration and logged in) according to system captured data. The mean number of days between users first logging into the app and their final visit was 39.2 (range 0–71). There was one user who only accessed the app on the day they first logged in. The mean number of unique days that a user accessed the app during this period was 13.3 (range 1–27).
The most viewed page in the app (excluding administration pages) was the Action Plan but only eight (73%) filled in their action plan. The individual exercise video pages were viewed a total of 88 times (11 people accessing these three times each week would mean an expected 297 times). All 11 participants who accessed the app completed the symptom score (CAT) questionnaire at least once with the average number of times completed per person being 3.1 (range 1–11; expected number of times would be at least 4). Four participants (36%) completed the 1-min sit-to-stand test through the app with the mean number of completions per participant for those that did complete it being 4.3 (range 2–6; expected number of times would be at least 4). Nearly all the participants (10, 91%) viewed the lung model visualization video page with a total of 25 views. Although nearly all of the participants viewed the mood and relaxation page (8; 82%) only three listened to one of the relaxation audio files.
In the follow up interview, participants who had not used the app stated their reasons, these included: forgetting (n = 2); difficulties downloading it or finding it on the app store (n = 3); that they did not feel it added anything above the messages so logged out (n = 1); and difficulties logging in (n = 1). Four participants felt that they needed more information on how to use the app. When asked for suggestions for how the app could be improved the following were suggested: warm up videos added; reminders to complete tasks; more consistency of information between app and text; adjustable plans and ability to go back into plans and edit; clearer instructions at the beginning; and more results reported back regularly to keep engaged.
Reported Impact
Seventeen (85%) participants reported that the program had impacted on how they managed their condition or helped them to change their behaviors.
“how to live with it generally. I had a negative attitude before it, but after it (I now know) you can pretty much still do everything as long as you pace yourself and breath carefully, it helped me a lot” (Female, 65–74 years, ID#20)
Self-reported positive impacts included: improved breathing, increased physical activity or exercise, and reduced inhaler use. They also reported changes in sedentary behavior and physical activity with 11 (58%) reporting spending less time sitting down since taking part in the program, 16 (84%) reporting more time being up and about, 16 (84%) doing more walking and 17 (89%) exercising more.
Family members’ feedback
All four patients who had family receiving the program reported that they found this beneficial and all reported that they felt it was beneficial to the family member.
“Made him (husband) more aware of what I go through.” (Female, 65–74 years, ID#9)
When interviewed, all four family members reported positive experiences with the program and that they appreciated being included. All said that it was useful to take part and would recommend it to other families.
“(it taught me) how to encourage her and support her willpower... to support her to move … I’ve noticed a change in her exercise since and her mentally coping.” (ID#23)
Safety
No adverse events were reported. Although alternatives were provided for anyone unable to comfortably complete the prescribed exercises, one participant did contact researchers about knee pain and was advised to stop lower limb exercises until the pain settled.
Suggestions for Improvement
Participants were asked to identify areas where mPR could be improved. Suggestions included: more condition specific information including more tailoring of the messages to conditions; and more details about the program and what it entails needs to be provided at registration including more information about what is included in the app and its functionality. It was suggested that the exercise component could be improved with more variability in exercises and more exercise options.
Discussion
This study found that it is feasible to deliver a pulmonary rehabilitation program solely by smart phone. There are currently no existing mPR programs being delivered in this way in New Zealand. There has been considerable scepticism from clinicians that a program developed for in-person group sessions could be adapted to be delivered over mobile phones. However, the lessons learned from the global COVID-19 pandemic have included the importance of remote delivery of support and services for vulnerable populations who do not want to or are not able to attend in person (Houchen-Wolloff and Steiner, 2020). This work will help to inform all future remote patient support programs.
Issues with digital literacy and confidence in using digital tools appear to remain with some in this patient cohort. Offering a text message only program, as well as a more integrated smartphone-based program, is therefore still worthwhile. Some people may require more instructions on using an app, regardless of its simplicity. Offering a version to patients’ family appears to be appreciated by both patients and their family members.
The exercise program was liked by participants, and they did report improvements in behaviors, however it seems that this may need further development. Future iterations of the mPR program will look to develop and strengthen the exercise component. This may include; increased feedback to the participant, resistance exercise prescription based on time rather than repetition, step counters and feedback loops, alternative exercises, and the possibility of a circuit option. We also intend to make the program more responsive and more tailored to the individual. More time is required to orientate participants to the program, especially the app, if they have low digital confidence.
Feedback from our participants aligns with our previous research in mHealth healthy behavior change (Bramley et al., 2005; Rodgers et al., 2005; Free et al., 2011), self-management support (Maddison et al., 2015; Dobson et al., 2018; Dobson et al., 2019b) and cardiac rehabilitation programs (Chow et al., 2015; Pfaeffli Dale et al., 2015). That is, that mHealth programs can be effective at improving health outcomes and that many people appreciate the motivation and support such programs are able to provide. Messages can provide timely reminders of desired behaviors and can align with existing in-person programs or act as an alternative where existing services are not accessible. To date, there has been less support for the effectiveness of smartphone apps than for mobile phone messaging in these areas (Whittaker et al., 2019). However, several current studies are investigating integrating the two forms of mHealth technology (Graham et al., 2016; Chen et al., 2020).
There is little other published research on mHealth pulmonary rehabilitation programs internationally. Bourne et al. (2017) completed a randomized control trial comparing the effectiveness of an online pulmonary rehabilitation program with a center-based program for people living with COPD. The exercise prescription included in the online program was a generic program and not individually prescribed or monitored. The authors found comparable improvements in exercise capacity and quality of life measures achieved from both programs, although it had a small sample size and recruitment was limited to participants who had internet access in their own home.
Chaplin et al. (2017) examined whether an interactive online web-based PR program was a feasible alternative to center-based PR in a randomized controlled feasibility study. Their program was individually tailored and intensely monitored. The study found comparable results for both groups. The authors noted the challenges associated with recruitment to the web-based program and the declining adherence to both programs. Parks et al. (Park et al., 2020) compared a smart phone app-based self management program with a control group for people living with COPD. Both groups started with a four week center based group exercise and education program. The app-based group had significant improvements in physical activity time compared to the control. The duration of program was six months, much longer than the previous trials, and the study showed adherence remained consistent throughout the six-month trial (Park et al., 2020).
The visualization included in the mPR app is novel and requires further investigation. One example from a clinically focused study identified that using visual images of the effect of skipping doses of anti-retroviral medication for the management of HIV, improved adherence (Jones et al., 2018). Another similar example has demonstrated the impact of model-based animation to improve recovery from acute coronary syndrome (Jones et al., 2016). Active visualization includes the application of live demonstrations or animations to communicate information about the effects of medication or other aspects of how the body works in a more impactful way (Perera et al., 2014). When information that is intangible, such as how our lungs work and what can go wrong in this complicated system, is presented visually with the assistance of computational modeling and/or animation, it may be easier for many people to process than factual material provided in text format.
Conclusions
A prototype mPR program was appreciated by a small number of patients and family members. More work is required to develop the next version of the mPR program based on the feedback from participants. We intend to develop a more integrated program, with the text messaging and app working together. It will also be a more adaptive and responsive program, tailored to the individual, their disease and their current condition. This will undergo more rigorous testing of effectiveness.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Health and Disability Ethics Committee (19/NTA/74), New Zealand. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
The intervention was designed by RW, RD, SC, JW, KB, TT, JR, DT, GH, JG, MT, SK, and FH. The study was designed and conducted by TT, SC, RD, and RW. Data collection by TT, RD, SC, and TW. Data analysis and interpretation by RW, RD, SC, JR, and GH. Manuscript prepared by RW, RD, SC and reviewed and edited by all.
Funding
This work was funded by the MedTech CoRE (Medical Technologies Center of Research Excellence), a collaboration of Universities and Callaghan Innovation in New Zealand (cmdt.org.nz).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors wish to acknowledge all the participants who contributed and participated in this work. We also would like to acknowledge the staff of NIHI, the PR and support staff at Waitemata and Counties-Manukau District Health Boards, and the Auckland region PR network.
References
Bestall, J. C., Paul, E. A., Garrod, R., Garnham, R., Jones, P. W., and Wedzicha, J. A. (1999). Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax 54, 581–586. doi:10.1136/thx.54.7.581
Bourne, S., DeVos, R., North, M., Chauhan, A., Green, B., Brown, T., et al. (2017). Online versus face-to-face pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: randomised controlled trial. BMJ open, 7 (7), e014580. doi:10.1136/bmjopen-2016-014580
Bramley, D., Riddell, T., Whittaker, R., Corbett, T., Lin, R. B., Wills, M., et al. (2005). Smoking cessation using mobile phone text messaging is as effective in Maori as non-Maori. N. Z. Med. J. 118, U1494.
Burrowes, K. S., Swan, A. J., Warren, N. J., and Tawhai, M. H. (2008). Towards a virtual lung: multi-scale, multi-physics modelling of the pulmonary system. Philos. Trans. A. Math. Phys. Eng. Sci. 366 (1879), 3247–3263. doi:10.1098/rsta.2008.0073
Chaplin, E., Hewitt, S., Apps, L., Bankart, J., Pulikottil-Jacob, R., Boyce, S., et al. (2017). Interactive web-based pulmonary rehabilitation programme: a randomised controlled feasibility trial. BMJ open 7, e013682. doi:10.1136/bmjopen-2016-013682
Chen, J., Ho, E., Jiang, Y., Whittaker, R., Yang, T., and Bullen, C. (2020). A mobile social network-based smoking cessation intervention for Chinese male smokers: protocol for a pilot randomized controlled trial. JMIR Res. Protoc. 9 (9), e18071. doi:10.2196/18071
Chow, C. K., Redfern, J., Hillis, G. S., Thakkar, J., Santo, K., Hackett, M. L., et al. (2015). Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease. JAMA 314 (12), 1255–1263. doi:10.1001/jama.2015.10945
Dobson, R., Herbst, P., Candy, S., Brott, T., Garrett, J., Humphrey, G., et al. (2019a). Understanding end-user perspectives of mobile pulmonary rehabilitation (mPR): cross-sectional survey and interviews. JMIR Form Res. 3 (4), e15466. doi:10.2196/15466
Dobson, R., Whittaker, R., Jiang, Y., McNamara, C., Shepherd, M., Maddison, R., et al. (2019b). Long‐term follow‐up of a randomized controlled trial of a text‐message diabetes self‐management support programme, SMS4BG. Diabet. Med. 37, 311. doi:10.1111/dme.14182
Dobson, R., Whittaker, R., Jiang, Y., Maddison, R., Shepherd, M., McNamara, C., et al. (2018). Effectiveness of text message based, diabetes self management support programme (SMS4BG): two arm, parallel randomised controlled trial. BMJ 361, k1959. doi:10.1136/bmj.k1959
Free, C., Knight, R., Robertson, S., Whittaker, R., Edwards, P., Zhou, W., et al. (2011). Smoking cessation support delivered via mobile phone text messaging (txt2stop): a single-blind, randomised trial. Lancet 378 (9785), 49–55. doi:10.1016/S0140-6736(11)60701-0
Graham, A. L., Jacobs, M. A., Cohn, A. M., Cha, S., Abroms, L. C., Papandonatos, G. D., et al. (2016). Optimising text messaging to improve adherence to web-based smoking cessation treatment: a randomised control trial protocol. BMJ Open 6, e010687. doi:10.1136/bmjopen-2015-010687
Guo, S. E., and Bruce, A. (2014). Improving understanding of and adherence to pulmonary rehabilitation in patients with COPD: a qualitative inquiry of patient and health professional perspectives. PLoS One 9 (10), e110835. doi:10.1371/journal.pone.0110835
Harrison, S. L., Robertson, N., Apps, L., Steiner, M. C., Morgan, M. D. L., and Singh, S. J. (2015). “We are not worthy”--understanding why patients decline pulmonary rehabilitation following an acute exacerbation of COPD. Disabil. Rehabil. 37 (9), 750–756. doi:10.3109/09638288.2014.939770
Hayton, C., Clark, A., Olive, S., Browne, P., Galey, P., Knights, E., et al. (2013). Barriers to pulmonary rehabilitation: characteristics that predict patient attendance and adherence. Respir. Med. 107 (3), 401–407. doi:10.1016/j.rmed.2012.11.016
Holland, A. E., Spruit, M. A., Troosters, T., Puhan, M. A., Pepin, V., Saey, D., et al. (2014). An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur. Respir. J. 44 (6), 1428–1446. doi:10.1183/09031936.00150314
Houchen-Wolloff, L., and Steiner, M. C. (2020). Pulmonary rehabilitation at a time of social distancing: prime time for tele-rehabilitation?. Thorax 75, 446–447. doi:10.1136/thoraxjnl-2020-214788
Jones, A. S. K., Coetzee, B., Kagee, A., Fernandez, J., Cleveland, E., Thomas, M., et al. (2018). The use of a brief, active visualisation intervention to improve adherence to antiretroviral therapy in non-adherent patients in South Africa. AIDS Behav. 23 (8), 2121–2129. doi:10.1007/s10461-018-2292-1
Jones, A. S., Ellis, C. J., Nash, M., Stanfield, B., and Broadbent, E. (2016). Using animation to improve recovery from acute coronary syndrome: a randomized trial. Ann. Behav. Medannals Behav. Med. 5050 (1), 108–118. doi:10.1007/s12160-015-9736-x
Jones, P. W., Harding, G., Berry, P., Wiklund, I., Chen, W. H., and Kline Leidy, N. (2009). Development and first validation of the COPD assessment test. Eur. Respir. J. 34 (3), 648–654. doi:10.1183/09031936.00102509
Maddison, R., Pfaeffli, L., Whittaker, R., Stewart, R., Kerr, A., Jiang, Y., et al. (2015). A mobile phone intervention increases physical activity in people with cardiovascular disease: results from the HEART randomized controlled trial. Eur. J. Prev. Cardiol. 22 (6), 701–709. doi:10.1177/2047487314535076
McCarthy, B., Casey, D., Devane, D., Murphy, K., Murphy, E., and Lacasse, Y. (2015). Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. (2), CD003793. doi:10.1002/14651858.CD003793.pub3
Michie, S., Richardson, M., Johnston, M., Abraham, C., Francis, J., Hardeman, W., et al. (2013). The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 46 (1), 81–95. doi:10.1007/s12160-013-9486-6
Park, S. K., Bang, C. H., and Lee, S. H. (2020). Evaluating the effect of a smartphone app-based self-management program for people with COPD: a randomized controlled trial. Appl. Nurs. Res. 52, 151231. doi:10.1016/j.apnr.2020.151231
Perera, A., Thomas, M. G., Moore, J. O., Faasse, K., and Petrie, K. J. (2014). Effect of a smartphone application incorporating personalized health-related imagery on adherence to antiretroviral therapy: a randomized clinical trial. AIDS Patient Care STDS 28 (11), 579–586. doi:10.1089/apc.2014.0156
Pfaeffli Dale, L., Whittaker, R., Jiang, Y., Stewart, R., Rolleston, A., and Maddison, R. (2015). Text message and internet support for coronary heart disease self-management: results from the Text4Heart randomized controlled trial. J. Med. Internet Res. 17 (10), e237. doi:10.2196/jmir.4944
Rodgers, A., Corbett, T., Bramley, D., Riddell, T., Wills, M., Lin, R. B., et al. (2005). Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. Tob. Control. 14 (4), 255–261. doi:10.1136/tc.2005.011577
Spruit, M. A., Singh, S. J., Garvey, C., ZuWallack, R., Nici, L., Rochester, C., et al. (2013). An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am. J. Respir. Crit. Care Med. 188 (8), e13–64. doi:10.1164/rccm.201309-1634ST
Vaidya, T., de Bisschop, C., Beaumont, M., Ouksel, H., Jean, V., Dessables, F., et al. (2016). Is the 1-minute sit-to-stand test a good tool for the evaluation of the impact of pulmonary rehabilitation? Determination of the minimal important difference in COPD. Int. J. Chron. Obstruct. Pulmon. Dis. 11, 2609. doi:10.2147/COPD.S115439
Whittaker, R., McRobbie, H., Bullen, C., Rodgers, A., Gu, Y., and Dobson, R. (2019). Mobile phone text messaging and app-based interventions for smoking cessation. Cochrane Database Syst. Rev. 10 (10), CD006611. doi:10.1002/14651858.CD006611.pub5
Keywords: mHealth, pulmonary rehabilitation (PR), COPD, COPD—chronic obstructive pulmonary disease, digital health (eHealth), mobile phone
Citation: Whittaker R, Dobson R, Candy S, Tane T, Burrowes K, Reeve J, Tawhai M, Taylor D, Robertson T, Garrett J, Humphrey G, Brott T, Khan SR, Hu F and Warren J (2021) Mobile Pulmonary Rehabilitation: Feasibility of Delivery by a Mobile Phone-Based Program. Front. Comput. Sci. 3:546960. doi: 10.3389/fcomp.2021.546960
Received: 30 March 2020; Accepted: 08 February 2021;
Published: 23 March 2021.
Edited by:
Bridget T. Kane, Karlstad University, SwedenReviewed by:
Jill Freyne, Commonwealth Scientific and Industrial Research Organization, AustraliaBjörn Nordlund, Karolinska Institutet, Sweden
Copyright © 2021 Whittaker, Dobson, Candy, Tane, Burrowes, Reeve, Tawhai, Taylor, Robertson, Garrett, Humphrey, Brott, Khan, Hu and Warren. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Robyn Whittaker, ci53aGl0dGFrZXJAYXVja2xhbmQuYWMubno=
 Robyn Whittaker
Robyn Whittaker Rosie Dobson
Rosie Dobson Sarah Candy3
Sarah Candy3 Merryn Tawhai
Merryn Tawhai Denise Taylor
Denise Taylor Trina Robertson
Trina Robertson Gayl Humphrey
Gayl Humphrey Sabaoon Raza Khan
Sabaoon Raza Khan Jim Warren
Jim Warren