- 1Institute of Cardiovascular Research and Sport Medicine, Department of Preventive and Rehabilitative Sport Medicine, German Sport University Cologne, Cologne, Germany
- 2Department of Fitness and Health, IST University of Applied Sciences, Düsseldorf, Germany
- 3Medical Center for Cardiology, Angiology, Pneumology and Rehabilitation Medicine, Cologne, Germany
- 4Department of Psychosomatics and Psychotherapy, University of Cologne, Cologne, Germany
- 5Fresenius University of Applied Sciences, Cologne, Germany
- 6Health Service of the Ford Motor Company GmbH, Cologne, Germany
- 7Institute of Medical Biometry and Epidemiology, University of Hamburg-Eppendorf, Hamburg, Germany
- 8HELIOS University Hospital Wuppertal, Wuppertal, Germany
- 9Witten/Herdecke University, Witten, Germany
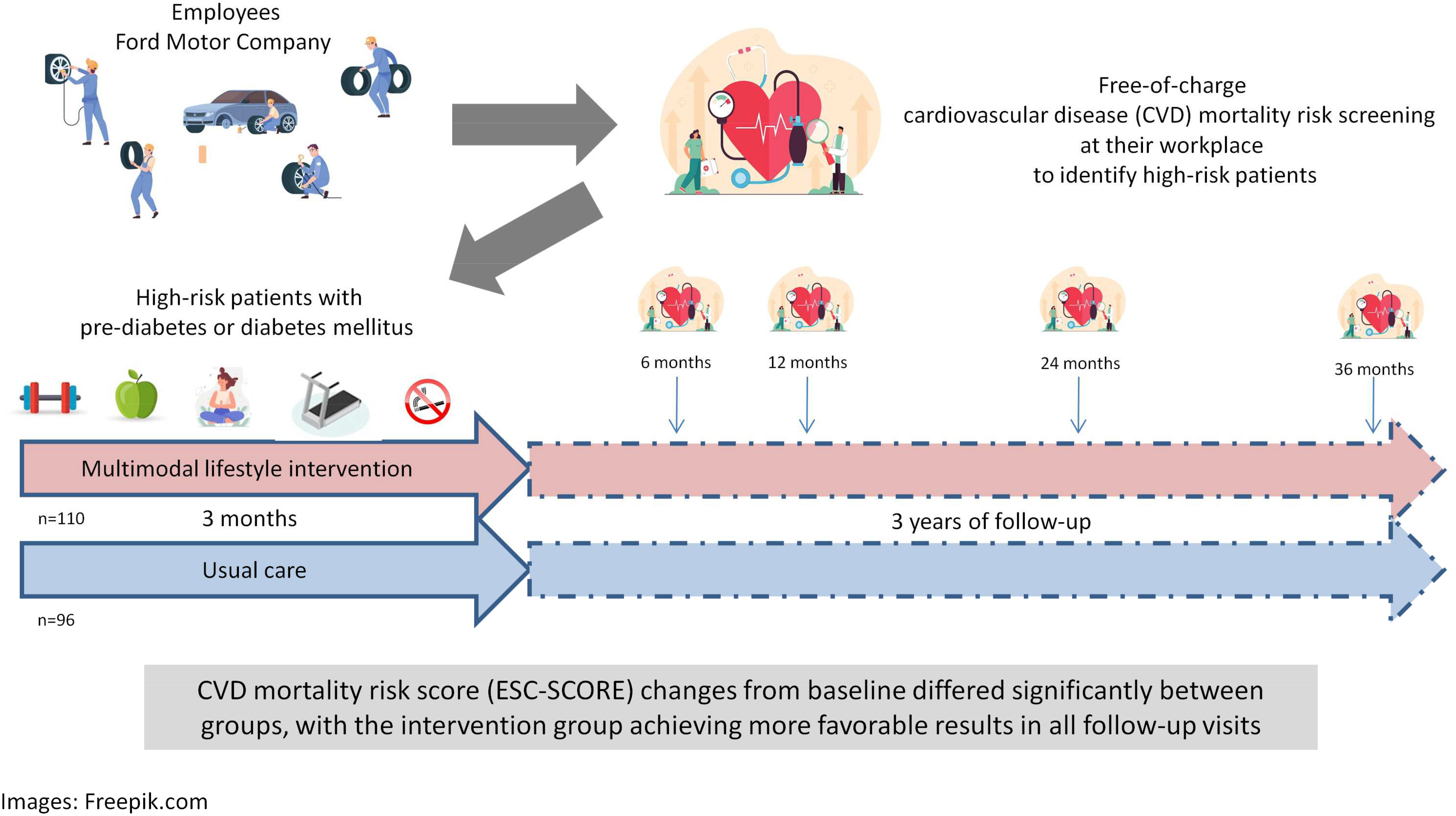
Aim: To evaluate the effects of a multimodal intervention (including exercise training, psychosocial interventions, nutrition coaching, smoking cessation program, medical care) on the health and long-term cardiovascular disease (CVD) mortality risk of company employees with pre-diabetes or diabetes mellitus (DM) at high CVD risk.
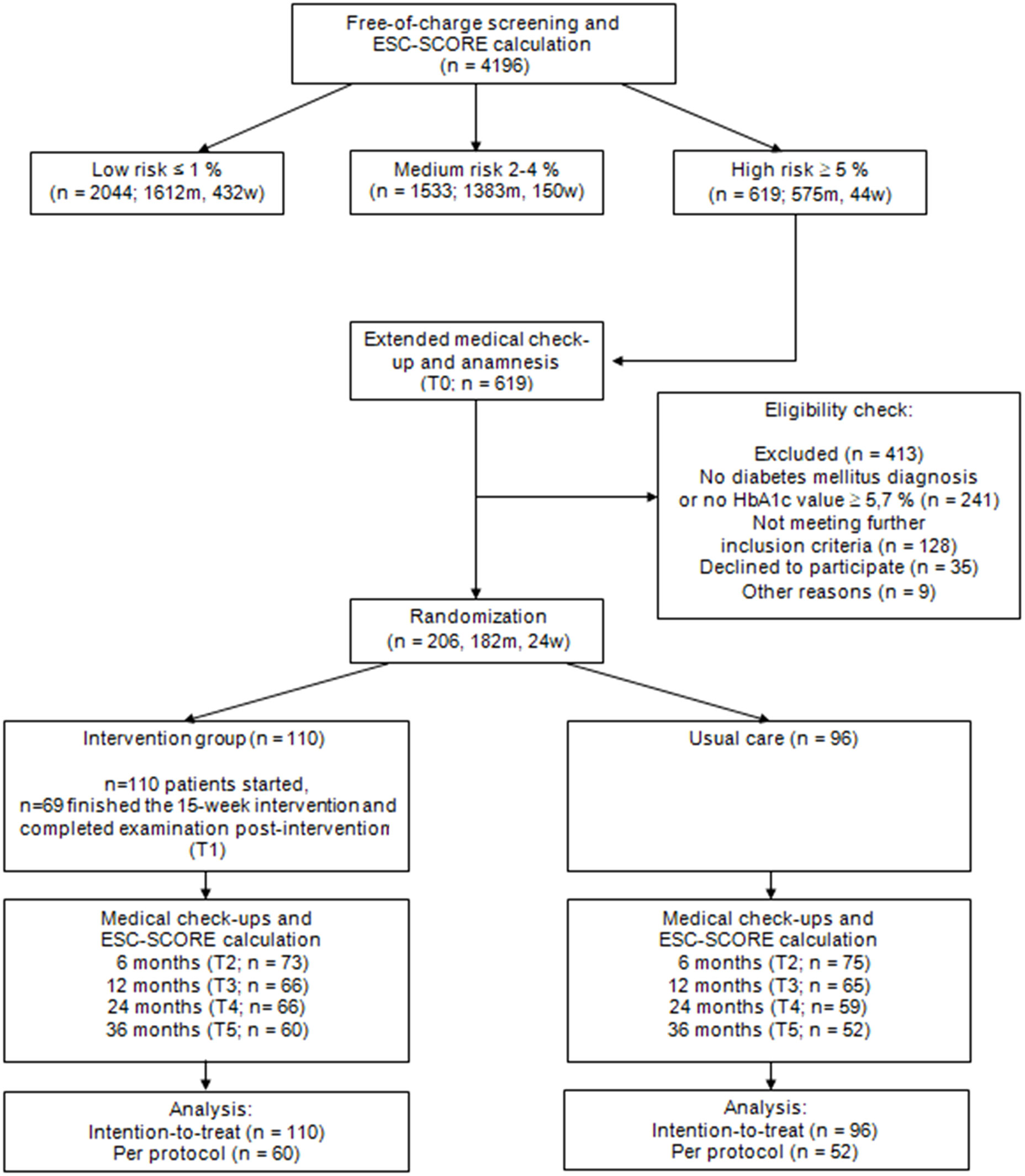
Methods: In the PreFord study, German company employees (n=4196) participated in a free-of-charge CVD mortality risk screening at their workplace. Based on their European Society of Cardiology – Systematic Coronary Risk Evaluation score (ESC-SCORE), they were subdivided into three risk groups. High-risk patients (ESC-SCORE≥5%) were randomly assigned to a 15-week lifestyle intervention or usual care control group. Data from patients with pre-DM/DM were analyzed intention-to-treat (ITT: n=110 versus n=96) and per protocol (PP: n=60 versus n=52).
Results: Body mass index, glycated hemoglobin, total cholesterol, low-density lipoprotein, triglyceride levels as well as systolic and diastolic blood pressure improved through the intervention (ITT, PP: p<0.001). The ESC-SCORE markedly decreased from pre- to post-intervention (ITT, PP: p<0.001). ESC-SCORE changes from baseline differed significantly between the groups, with the intervention group achieving more favorable results in all follow-up visits 6, 12, 24 and 36 months later (at each time point: ITT: p<0.001; PP: p ≤ 0.010).
Conclusion: The study demonstrates the feasibility of attracting employees with pre-DM/DM at high CVD mortality risk to participate in a multimodal lifestyle program following a free CVD mortality risk screening at their workplace. The lifestyle intervention used in the PreFord study shows high potential for improving health of company employees with pre-DM/DM in the long term. ISRCTN23536103.
1 Introduction
Cardiovascular diseases (CVDs) are the leading cause of premature death (1, 2). Thus, reducing the incidence of CVDs is of high public health importance. A meta-analysis from observational studies has shown that a healthy lifestyle can reduce the risk of developing CVDs by up to 66% (3). Preventive measures aimed at lifestyle changes can therefore be helpful to reduce individual mortality risk. In the PreFord study (4), German company employees of the Ford Motor Company (n=4196) participated in a free-of-charge CVD mortality risk screening at their workplace. The participants were then subdivided into three risk groups based on their risk factors, quantified by the European Society of Cardiology – Systematic Coronary Risk Evaluation score (ESC-SCORE), which is an established metric to estimate the risk of fatal cardiovascular events with a high accuracy for Germans and other Europeans (5, 6). Employees with a high risk score (ESC-SCORE ≥ 5%) were randomly assigned to a multimodal lifestyle intervention group (receiving exercise training, psychosocial interventions, nutrition coaching, smoking cessation program, medical care) or to a usual care group (receiving medical care only).
Large-scale observational studies show that patients with diabetes mellitus (DM) have a drastically increased risk of cardiovascular events and CVD mortality (7–9). As lifestyle changes can help reduce cardiovascular risk, patients with pre-DM and DM should optimize their lifestyle as early as possible. Unfortunately, these patients are often very difficult to motivate for lifestyle changes; moreover, there might be several psycho-social barriers (10). When they participate in an intervention program, achieving sustainable effects is usually challenging, due to low program adherence and high drop-out rates (11).
This secondary analysis of the PreFord study data explores the direct effects of the study’s 15-week multimodal lifestyle intervention on the ESC-SCORE and other health-related variables in the pre-DM/DM subgroup. Long-term effects on the individual cardiovascular risks and the program’s efficiency for patients with pre-DM/DM are discussed, considering that aggressive programs for lifestyle changes are urgently needed to account for an increasing incidence and prevalence of DM (12, 13).
2 Methods
2.1 PreFord study
2.1.1 Study design
The PreFord trial was designed as a randomized controlled, multicenter clinical study. The study design has already been described in detail (4). The study protocol in line with good clinical practice has been approved by the Ethics Committee of the University of Cologne (ref: 03-217) and the Ethics Committee of the North Rhine Medical Association (Ärztekammer Nordrhein, ref: 2004079). Subjects gave their written informed consent prior to the start of the study.
2.1.2 Subjects
Employees of the Ford Motor Company Germany (>15.000) were invited to participate in a free-of-charge cardiovascular medical check-up (T0) and to determine their ESC-SCORE which reflects personal risk of cardiovascular events. The score was calculated by an independent statistics institution (Institute of Medical Statistics, Informatics and Epidemiology, University of Cologne). Age, blood pressure, smoking habits and total cholesterol values were recorded for risk assessment. Inclusion criteria were defined as follows: an ESC-SCORE ≥ 5% (high-risk group) and the ability to exercise. Exclusion criteria were defined as follows: exercise-limiting diseases, history of cardiovascular disease, cancer, pregnancy or severe mental disorders.
2.1.3 Lifestyle intervention
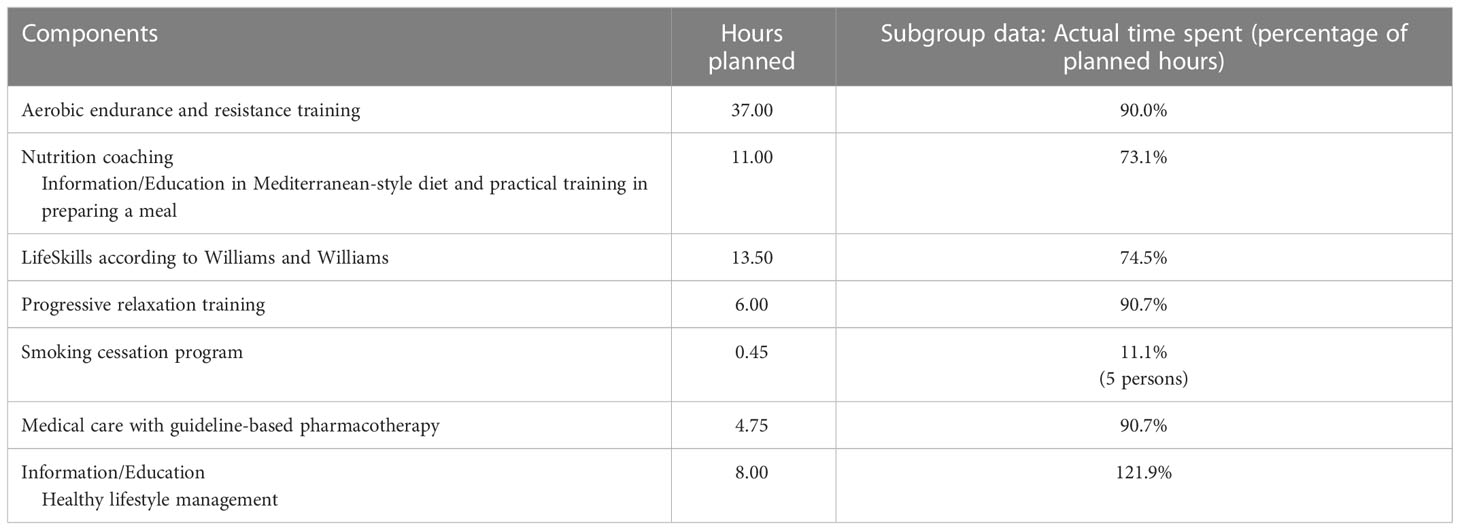
Subjects were randomly assigned to the intervention (INT) group or the usual care control (CON) group by block randomization 1:1. The computer-generated random list was provided by the Clinical Trial Center Cologne. Study personnel assigned participants to the INT or CON group according to this random list. The 15-week multimodal lifestyle intervention (Table 1) was supervised by professional health care specialists (medical doctors, exercise physiologists, psychologists, and nutritional coaches). The intervention was performed in small groups twice a week for 2.5-3 hours per session in two rehabilitation centers in Cologne, Germany. Further details about the program are available in the publication of Gysan et al. (4). All employees who participated in the intervention program were examined immediately after the intervention (T1). The CON group participants received usual care from their general practitioners.
2.1.4 Follow-up
All company employees who participated in the study, in either the INT or ON group, were invited for follow-up medical check-ups 6 (T2), 12 (T3), 24 (T4) and 36 (T5) months after start of the study. The study ended after completion of the last follow-up.
2.2 Secondary data analysis
2.2.1 Subjects
The secondary data analysis is reported in accordance with the CONSORT statement (14). Only employees diagnosed with diabetes mellitus (and receiving pharmacological treatment) and/or with glycated hemoglobin (HbA1c) levels ≥ 5.7% were included in this analysis (Figure 1). In total, the datasets of n=142 persons with pre-DM (HbA1c levels ≥ 5.7% and < 6.5% without anti-diabetic medication) and n=64 patients with manifest DM (HbA1c levels ≥ 6.5% and/or treated with anti-diabetic medication) were considered. The HbA1c thresholds correspond to the American Diabetes Association cutoffs for the diagnoses of pre-DM and DM (15).
2.2.2 Primary and secondary outcomes
The ESC-SCORE was defined as the primary outcome. It was determined in the INT and CON group at every follow-up examination and thus helped assess the long-term effectiveness of the intervention. The same ESC-SCORE algorithm in its initially published form was used throughout the study (5). The ESC-SCORE provides an accurate prediction of cardiovascular events in Europeans without a history of severe cardiovascular diseases (e.g., coronary heart disease, stroke, peripheral artery disease, heart failure, heart arrhythmia).
To determine the intervention’s direct effectiveness, body weight, body mass index (BMI), waist circumference, glycated hemoglobin (HbA1c), high-sensitive C-reactive protein (hsCRP), total cholesterol, high-density lipoprotein (HDL), low-density lipoprotein (LDL), triglycerides, systolic and diastolic blood pressure and exercise capacity pre- and post-intervention were defined as secondary outcomes.
2.2.3 Statistical analyses
Data are presented as mean values ± standard deviations (SD) and 95% confidence intervals (95%-CI). The “SPSS” program (v. 28.0, IBM Corporation, Armonk, New York, USA) was used for the statistical analyses. Parametric tests were used throughout. When assumptions were violated and when appropriate, non-parametric (rank-based) hypotheses tests were conducted. For baseline comparisons of interval-scaled variables between the two groups, the Student’s t test or the Mann-Whitney U test for unpaired samples were performed. The Chi2 test was used to assess differences in the distribution of nominal-scaled variables between the groups. For pre-post-comparisons of interval-scaled variables within the INT group, the Student’s t test or the Wilcoxon signed rank test for paired samples were used. For follow-up analyses within each group (INT and CON), the Friedman test was carried out. To compare changes from baseline between the two groups at the different follow-up time points, the Student’s t test or the Mann-Whitney U test for unpaired samples were used. Data were analyzed intention-to-treat and per protocol. The intention-to-treat cohort included all patients. Missing values in the intention-to-treat analysis were replaced by the last observation carried forward (29.9% missing ESC-SCORE data, 33.2% missing HbA1c data). The per protocol cohort included only those patients who fully adhered to the study protocol. In addition, data from all measurement time points had to be available. Significance was considered at p ≤ 0.05.
2.2.4 Sample size and power calculation
A sample size calculation was performed for the original study a priori (4). For this subgroup data analysis, a second power analysis was performed for the ESC-SCORE as the primary outcome a posteriori using G Power (v. 3.1.9.7., University of Düsseldorf, Düsseldorf, Germany). For the intention-to-treat analysis, a power of 100% was calculated for the comparison between the ESC-SCORE pre- and post-intervention of the INT group and a power of 94% for the comparison of ESC-SCORE changes from baseline between the INT and CON groups during the follow-up medical check-up 36 months later. For the per protocol analysis, statistical power values of 100% and 83% were calculated, respectively.
3 Results
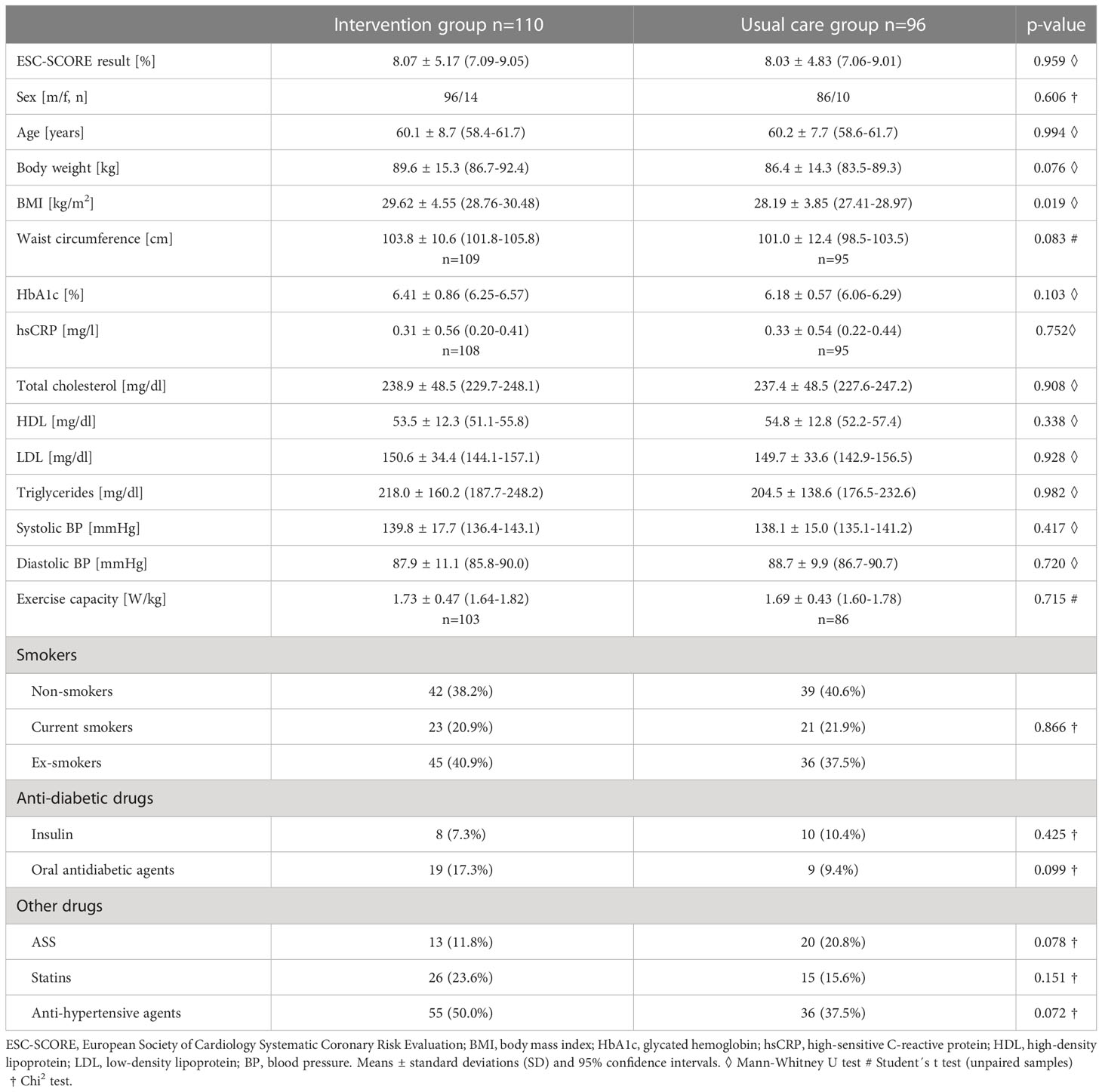
3.1 Baseline data
The baseline (T0) data of the subjects of the INT and CON groups are presented in Table 2. The ratio of men and women roughly reflects the ratio of employees in the company. The groups were almost perfectly matched for the ESC-SCORE and also did not significantly differ in any other variable, except BMI.
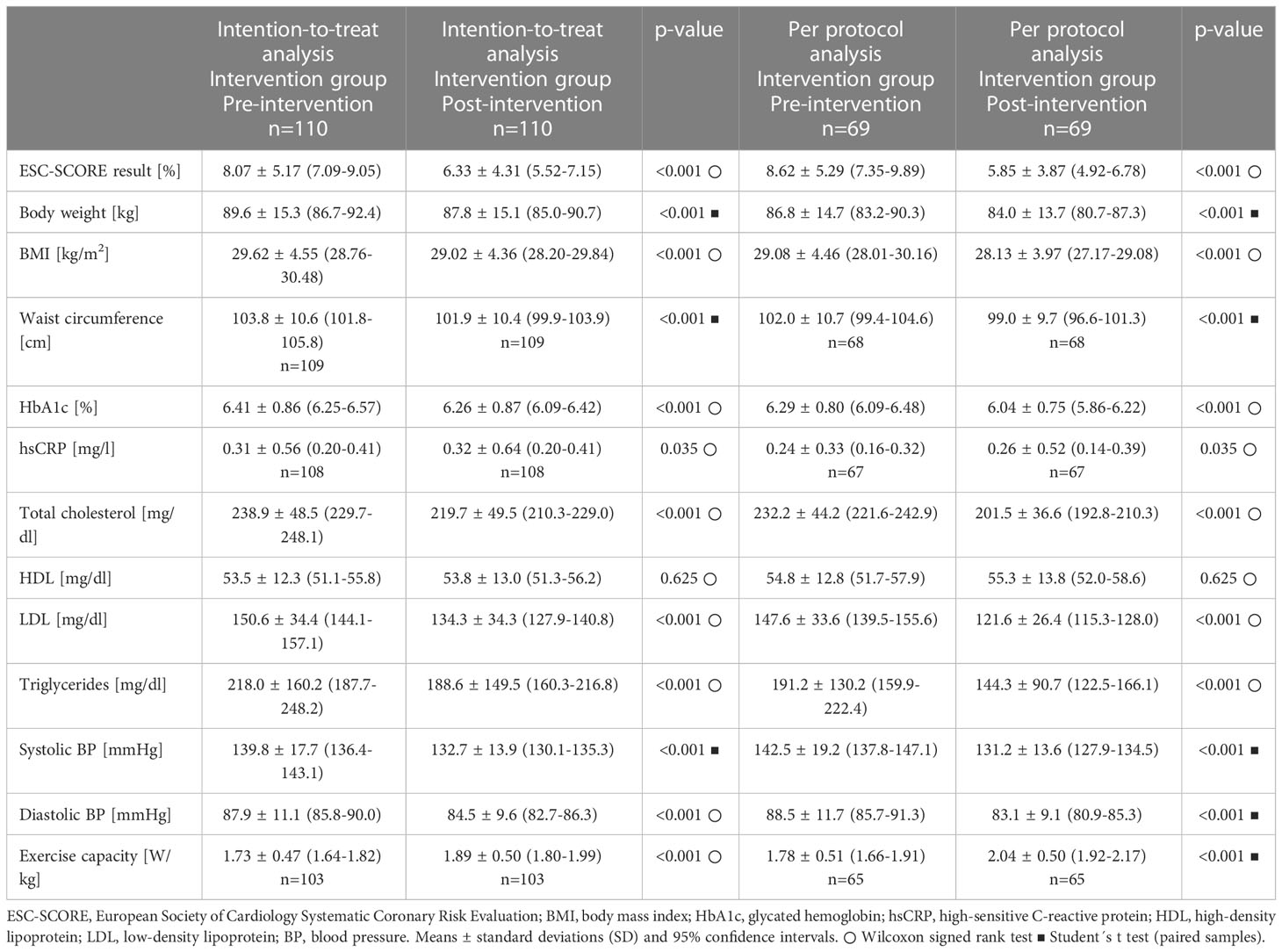
3.2 Direct effects of the multimodal lifestyle intervention on the ESC-SCORE and important health variables
Pre-post-intervention data (T0-T1) are presented in Table 3. The ESC-SCORE decreased significantly, irrespective of the type of analysis conducted (intention-to-treat or per protocol). Nearly all other health-related variables (body weight, BMI, waist circumference, HbA1c, total cholesterol, LDL, triglycerides, systolic and diastolic blood pressure, exercise capacity) also improved significantly. HDL levels remained unchanged and hsCRP levels increased significantly, but very slightly.
3.3 Follow-up and long-term effects of the multimodal lifestyle intervention on the ESC- SCORE
There was a significant overall time effect for the ESC-SCORE in each group (INT and CON) from T0 across all follow-up time points (T2, T3, T4, T5) (Friedman test: p<0.001), which was evident in both the intention-to-treat and per protocol analyses (Supplemental Data File: ESM 1). It appears that the ESC-SCORE of the INT group increased only very slightly in the long term after the intervention, while it increased more in the CON group. This is reflected in the changes from baseline. The delta values differed significantly between the groups (INT and CON) at each time point (T2, T3, T4, T5), with the intervention group achieving more favorable results in the intention-to-treat (Figure 2) as well as the per protocol analysis (Figure 3).
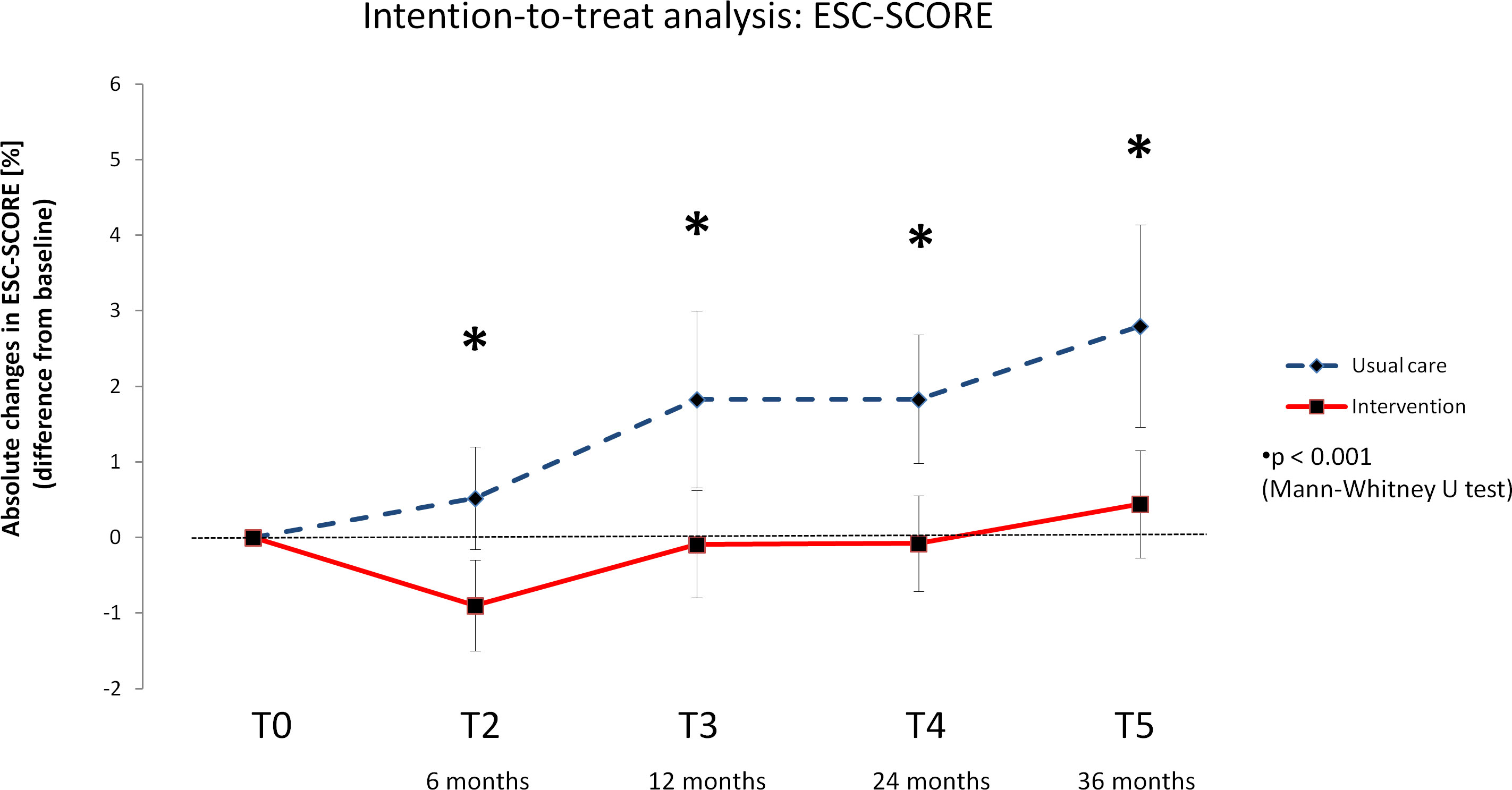
Figure 2 Delta values of the European Society of Cardiology – Systematic Coronary Risk Evaluation score (ESC-SCORE) – Intention-to-treat analysis. Means with 95% confidence intervals.
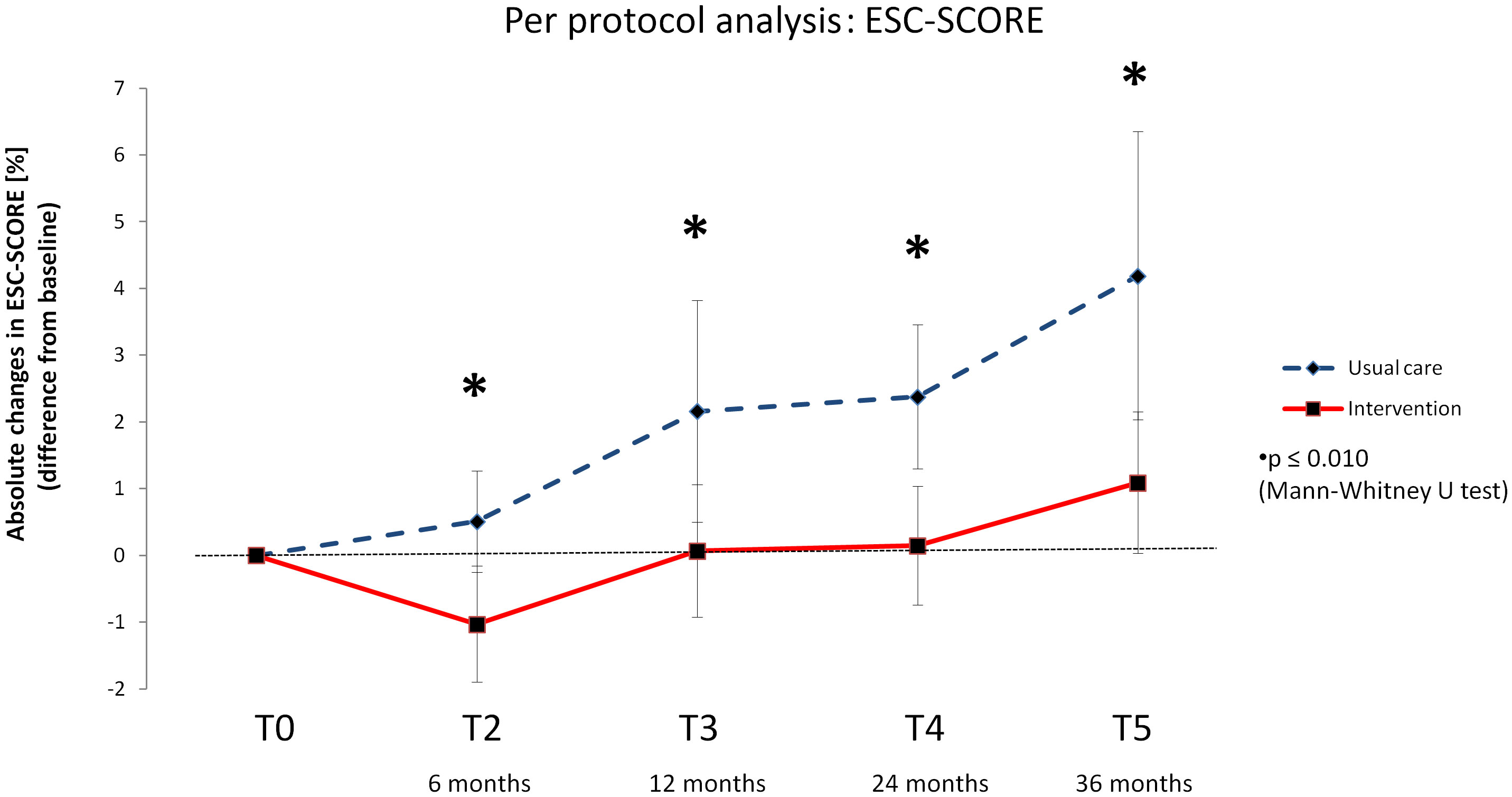
Figure 3 Delta values of the European Society of Cardiology – Systematic Coronary Risk Evaluation score (ESC-SCORE) –Per protocol analysis. Means with 95% confidence intervals.
To clarify whether there is a difference in the primary outcome between pre-DM and DM patients, a further subgroup analysis was performed for ESC-SCORE changes (Supplemental Data File: ESM 2). The intention-to-treat analysis revealed that the pre-DM patients’ (INT: n=72, CON: n=70) results were quite similar to those of all patients (pre-DM/DM patients). Delta values differed significantly between the groups (INT and CON) at each time point (T2, T3, T4, T5), with the intervention group achieving more favorable results. In DM patients (INT: n=38, CON: n=26), a significant difference in ESC-SCORE changes was evident after the lifestyle intervention, with better results in the INT group. However, from T3 onward, there was no longer a significant difference in delta values between the groups (INT and CON). It should be noted that ESC-SCORE baseline values were significantly higher in pre-DM than in DM patients in both groups (INT: pre-DM: 9.16 ± 4.99% (95%-CI: 7.99-10.33%), DM: 6.00 ± 4.95% (95%-CI: 4.38-7.63%), U test: p<0.001; CON: pre-DM: 8.54 ± 4.12% (95%-CI: 7.55-9.52%), DM: 6.67 ± 6.24% (95%-CI: 4.15-9.20%), U test: p=0.017). Due to the small number of included DM patients (INT: n=15, CON: n=12), no subgroup analysis was performed in the per protocol cohort.
3.4 Follow-up and long-term effects of the multimodal lifestyle intervention on glycemic control
There was a significant overall time effect for the HbA1c levels in the INT group from T0 across all follow-up time points (T2,T3,T4,T5) (Friedman test: p<0.001), which was evident in both the intention-to-treat and per protocol analyses (Supplemental Data File: ESM 3). There were no significant HbA1c changes in the CON group. Of all pre-DM patients from the per protocol cohort, 5% developed manifest DM in the INT and 22% in the CON group (from T0 to T5). Half of them started treatment with anti-diabetic medication.
3.5 Adverse events during the intervention
There were no adverse events during the intervention.
4 Discussion
DM can drastically increase the risk of CVDs. The INTERHEART study, which collected data from more than 27,000 subjects in 52 countries, identified DM as a strong risk factor for acute myocardial infarction (9). Other famous large-scale studies such as the Framingham study or the San Antonio Heart Study found increased CVD mortality rates in DM patients compared with non-diabetic subjects from the general population (7, 8). Furthermore, the understanding of the pathogenesis of CVDs in the context of DM improves continuously, with hyperglycemia, hyperinsulinemia and hypercoagulability playing important roles in increased CVD risk and mortality (16, 17). Lifestyle interventions that can prevent the development of CVDs or that have a positive effect on their progression should therefore be strongly recommended as preventive measures not only for patients with manifest DM, but also for those with pre-DM (18, 19).
The secondary data analysis of the PreFord study shows that the cardiovascular risk of persons with pre-DM/DM can be substantially reduced through the multimodal lifestyle program applied in the study. There was a direct effect on several health variables and the ESC-SCORE after 15 weeks. Over the next 3 years of follow-up, there were more favorable results in the INT group.
The ESC-SCORE reflects the probability of dying in the next 10 years from a cardiovascular event (5). The ESC-SCORE used in this study is calculated based on age, systolic blood pressure, smoking habits and total cholesterol values (5, 6). Although the algorithm does not consider pre-DM or diabetes status, the ESC-SCORE is nonetheless suitable for a rough assessment of the cardiovascular risk in the subgroup studied, because the relationship of the other risk factors with CVDs are almost parallel in individuals with and without DM (5, 20). However, the risk of persons with DM is generally higher. According to the ESC- SCORE’s instructions, it should be considered for the interpretation that the calculated risk at every risk factor combination can be at least twice as high in men and up to 4-fold higher in women with manifest DM (5). It must therefore be assumed that the actual CVD risk tends to be underestimated by the ESC-SCORE value for the subgroup studied, but because many more pre-DM patients than patients with manifest DM were included in the analysis, the underestimation should not be too far-reaching.
The overall results suggest a clear positive health effect of the intervention for the subgroup studied, which is very similar to the effect for the entire study cohort group (4). Persons in the intervention group generally benefited from the multimodal lifestyle program, which was reflected in more favorable ESC-SCORE changes compared to those in the usual care control group over the course of the study. Multimodal interventions that also target self-empowerment, such as the program in the PreFord study, promise long-term effectiveness, which in turn may also be cost-effective (21). Kähm et al. (22) estimated the costs for diabetic complications in German patients. End-stage renal disease, amputations, stroke, myocardial infarction and ischemic heart disease were deemed very cost-intensive. Indirect costs related to lost productivity and work ability due to diabetes and its complications are also very high (23). Magliano et al. (24) demonstrated that “productivity-adjusted life years” were reduced by 11.6% and 10.5% among men and women with DM, respectively. Interventions that focus on persons with pre-DM and DM and which are initiated early in working life could thus help reduce work absenteeism and protect the workforce by preventing the development of disease complications.
A closer look at the long-term effects on the ESC-SCORE changes (intention-to-treat analysis) implies that pre-DM patients in particular benefited from the lifestyle intervention. Further measures may be necessary to achieve more beneficial effects in patients with manifest DM. However, it should be noted that the pre-DM patients already had higher values at the beginning of the study, so that possible improvements may be more pronounced in them than in the DM patients. However, the result should not be overestimated, as only 42% of the DM patients of the intention-to-treat analysis fully adhered to the study protocol.
The strategy for raising awareness of CVD risk at the workplace through flyers and offering a quick medical check-up free of charge could—as demonstrated in the present study—motivate workers with pre-DM and DM to participate in multimodal therapy. Despite the noted drop-out rate during the intervention of 37% among those with pre-DM and DM (for all study participants, the rate was 32%), the intention-to-treat analysis nevertheless indicated significant and clinically meaningful improvements post-intervention, underscoring the program’s overall efficacy.
The PreFord study has some limitations, which have already been pointed out in the initial publication (4). One limitation, for example, is the fact that there could be concerns against the employer who pushed the study, so that some employees did not participate in the CVD mortality risk screening due to concerns that their health data could be misused. Therefore, the representativeness of the results for the entire company cannot be guaranteed. Another limitation is that very few women were included. Therefore, the question is to what extent the results are gender-specific. This cannot be clarified based on the present data.
An additional point that might be of interest, especially for the secondary analysis, is that no distinction was made between the types of DM. Among the 13 insulin-dependent patients, some patients with type 1 DM may have been included. However, Juutilainen et al. (25) showed in an 18-year observational study that there was no major difference between middle-aged individuals with T1DM and T2DM in terms of their CVD mortality risk (onset of the disease was > 30 years in both groups). However, other data suggest a greater mortality risk for T2DM patients compared with T1DM patients when the age of onset of the diabetic disease is earlier in both groups (15-30 years) (26).
Furthermore, there was a minor, but statistically significant difference in BMI values between the INT and CON group, which might have affected the development of health values. However, for the primary outcome (ESC-SCORE), the groups were almost perfectly matched.
5 Conclusion
In conclusion, attracting company employees who are at high CVD mortality risk to participate in a multimodal lifestyle program following a free CVD mortality risk screening at their workplace may be a successful strategy for CVD prevention, particularly in patients with pre-DM/DM. The multimodal intervention used in the PreFord study was suitable for improving the health of company employees with pre-DM/DM and for reducing their CVD mortality risk in the long term.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the University of Cologne. The patients/participants provided their written informed consent to participate in this study.
Author contributions
CB had the idea for this paper. CB and HH performed the statistical analyses. CB wrote and revised the manuscript. All other authors (D-BG, CA, SM, BB-W, JL, GH, KW, CH, MS, H-GP) have contributed substantially to the design, acquisition, analysis and interpretation of study data from the PreFord study and gave their intellectual input to the present manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors thank all volunteers from the Ford Motor Company who participated in the PreFord study.
Conflict of interest
CB is a member of the Abbott Diabetes Care Advisory Board and has received research grants and honoraria from Abbott. GH was employed by the Health Service of the Ford Motor Company GmbH.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2023.1106334/full#supplementary-material
References
1. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: A systematic analysis for the global burden of disease study 2017. Lancet (2018) 392:1736–88. doi: 10.1016/S0140-6736(18)32203-7
2. Jagannathan R, Patel SA, Ali MK, Narayan KMV. Global updates on cardiovascular disease mortality trends and attribution of traditional risk factors. Curr Diabetes Rep (2019) 19:44. doi: 10.1007/s11892-019-1161-2
3. Barbaresko J, Rienks J, Nöthlings U. Lifestyle indices and cardiovascular disease risk: A meta-analysis. Am J Prev Med (2018) 55:555–64. doi: 10.1016/j.amepre.2018.04.046
4. Gysan DB, Millentrup S, Albus C, Bjarnason-Wehrens B, Latsch J, Gohlke H, et al. Substantial improvement of primary cardiovascular prevention by a systematic score-based multimodal approach: A randomized trial: The PreFord-study. Eur J Prev Cardiol (2017) 24:1544–54. doi: 10.1177/2047487317718081
5. Conroy RM, Pyörälä K, Fitzgerald AP, Sans S, Menotti A, de BG, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur Heart J (2003) 24:987–1003. doi: 10.1016/S0195-668X(03)00114-3
6. Elsner LK, von JB, Grün D, JS W, Weferling M, Diouf K, et al. Prognostic performance of the ESC SCORE and its German recalibrated versions in primary and secondary prevention. Eur J Prev Cardiol (2020) 27:2166–9. doi: 10.1177/2047487319868034
7. Kannel WB. Diabetes and cardiovascular disease. JAMA (1979) 241:2035. doi: 10.1001/jama.1979.03290450033020
8. Wei M, Gaskill SP, Haffner SM, Stern MP. Effects of diabetes and level of glycemia on all-cause and cardiovascular mortality. San Antonio Heart Study Diabetes Care (1998) 21:1167–72. doi: 10.2337/diacare.21.7.1167
9. Yusuf S, Hawken S, Ôunpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet (2004) 364:937–52. doi: 10.1016/S0140-6736(04)17018-9
10. Fuller H, Alberti H. Barriers to lifestyle changes in people with diabetes. Br J Gen Pract (2017) 67:61. doi: 10.3399/bjgp17X689005
11. MacDonald CS, Ried-Larsen M, Soleimani J, Alsawas M, Lieberman DE, Ismail AS, et al. A systematic review of adherence to physical activity interventions in individuals with type 2 diabetes. Diabetes Metab Res Rev (2021) 37:e3444. doi: 10.1002/dmrr.3444
12. Echouffo-Tcheugui JB, Selvin E. Prediabetes and what it means: The epidemiological evidence. Annu Rev Public Health (2021) 42:59–77. doi: 10.1146/annurev-publhealth-090419-102644
13. Tinajero MG, Malik VS. An update on the epidemiology of type 2 diabetes: A global perspective. Endocrinol Metab Clin North Am (2021) 50:337–55. doi: 10.1016/j.ecl.2021.05.013
14. Begg C, Cho M, Eastwood S, Horton R, Moher D, Olkin I, et al. Improving the quality of reporting of randomized controlled trials: The CONSORT statement. JAMA (1996) 276:637–9. doi: 10.1001/jama.1996.03540080059030
15. ADA American Diabetes Association. 2. classification and diagnosis of diabetes: Standards of medical care in diabetes-2021. Diabetes Care (2021) 44:S15–33. doi: 10.2337/dc21-S002
16. Paul S, Ali A, Katare R. Molecular complexities underlying the vascular complications of diabetes mellitus – a comprehensive review. J Diabetes Complications (2020) 34:107613. doi: 10.1016/j.jdiacomp.2020.107613
17. Qazi MU, Malik S. Diabetes and cardiovascular disease: Original insights from the framingham heart study. Glob Heart (2013) 8:43–8. doi: 10.1016/j.gheart.2012.12.008
18. Narayan KMV, Imperatore G, Benjamin SM, Engelgau MM. Targeting people with pre-diabetes. BMJ (Clinical Res ed.) (2002) 325:403–4. doi: 10.1136/bmj.325.7361.403
19. Tuso P. Prediabetes and lifestyle modification: Time to prevent a preventable disease. Perm J (2014) 18:88–93. doi: 10.7812/TPP/14-002
20. Stamler J, Vaccaro O, Neaton JD, Wentworth D. The multiple risk factor intervention trial research group. diabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the multiple risk factor intervention trial. Diabetes Care (1993) 16:434–44. doi: 10.2337/diacare.16.2.434
21. Rodriguez-Mañas L, Laosa O, Vellas B, Paolisso G, Topinkova E, Oliva-Moreno J, et al. Effectiveness of a multimodal intervention in functionally impaired older people with type 2 diabetes mellitus. J Cachexia Sarcopenia Muscle (2019) 10:721–33. doi: 10.1002/jcsm.12432
22. Kähm K, Laxy M, Schneider U, Rogowski WH, Lhachimi SK, Holle R. Health care costs associated with incident complications in patients with type 2 diabetes in Germany. Diabetes Care (2018) 41:971–8. doi: 10.2337/dc17-1763
23. Riddle MC, Herman WH. The cost of diabetes care-an elephant in the room. Diabetes Care (2018) 41:929–32. doi: 10.2337/dci18-0012
24. Magliano DJ, Martin VJ, Owen AJ, Zomer E, Liew D. The productivity burden of diabetes at a population level. Diabetes Care (2018) 41:979–84. doi: 10.2337/dc17-2138
25. Juutilainen A, Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Similarity of the impact of type 1 and type 2 diabetes on cardiovascular mortality in middle-aged subjects. Diabetes Care (2008) 31:714–9. doi: 10.2337/dc07-2124
Keywords: exercise, nutrition, cardiovascular risk assessment, employees, diabetes
Citation: Brinkmann C, Hof H, Gysan D-B, Albus C, Millentrup S, Bjarnason-Wehrens B, Latsch J, Herold G, Wegscheider K, Heming C, Seyfarth M and Predel H-G (2023) Lifestyle intervention reduces risk score for cardiovascular mortality in company employees with pre-diabetes or diabetes mellitus – A secondary analysis of the PreFord randomized controlled trial with 3 years of follow-up. Front. Endocrinol. 14:1106334. doi: 10.3389/fendo.2023.1106334
Received: 23 November 2022; Accepted: 30 January 2023;
Published: 23 February 2023.
Edited by:
Gaetano Santulli, Albert Einstein College of Medicine, United StatesReviewed by:
Jaideep Menon, Amrita Institute of Medical Sciences and Research Centre, IndiaJuan Velasco, Yale University, United States
Copyright © 2023 Brinkmann, Hof, Gysan, Albus, Millentrup, Bjarnason-Wehrens, Latsch, Herold, Wegscheider, Heming, Seyfarth and Predel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christian Brinkmann, Y2guYnJpbmttYW5uQGdteC5uZXQ=
 Christian Brinkmann
Christian Brinkmann Hannah Hof1
Hannah Hof1 Birna Bjarnason-Wehrens
Birna Bjarnason-Wehrens Karl Wegscheider
Karl Wegscheider