- 1College of Medical and Dental Sciences, University of Birmingham, Birmingham, United Kingdom
- 2Department of Endocrinology and Diabetes, Clinic Neolab, Tbilisi, Georgia
- 3Institute of Metabolism and Systems Research, University of Birmingham, Birmingham, United Kingdom
- 4Royal College of Surgeons in Ireland (RCSI), University of Medicine and Health Sciences, Dublin, Ireland
- 5London Institute of Medical Sciences, Medical Research Council, London, United Kingdom
- 6Institute of Clinical Sciences, University of Birmingham, Birmingham, United Kingdom
- 7Institute of Applied Health Research, University of Birmingham, Birmingham, United Kingdom
- 8Queen Elizabeth Hospital, University Hospitals Birmingham National Health Service (NHS) Foundation Trust, Birmingham, United Kingdom
Objective: To understand and explore the perceptions and opinions of women with polycystic ovary syndrome (PCOS) and further delineate the variations across age and ethnicity.
Design: Qualitative survey focussed on lived experiences of people with PCOS. Participants could share their views either as written text or as voice note audio recording(s) on WhatsApp. The data from the audio were transcribed verbatim. Responses were coded by two study members independently, using a thematic inductive method with NVivo 12. Two senior study members then reviewed these codes to identify common themes.
Subjects: Women with PCOS aged 18-60 years.
Results: 43 of 45 participants had a formal diagnosis of PCOS, the remaining two had suspected PCOS which was under investigation. Four participants opted to share their views as voice note recordings. Poor mental health was the most reported (83.3% of participants), followed by dermatological (81.0%) and menstrual issues (76.2%). Participants were generally dissatisfied with the care they received (88.1%). A lengthy diagnostic journey was reported in 35.7% of cases. 52.6% felt less feminine, particularly regarding weight gain and infertility. As part of the recommendations by participants, it was emphasised that others with the condition should educate themselves and be proactive in their management. 46.3% reported that being more enlightened regarding their condition improved their health outcomes and enabled them to advocate for their own care. Women in their 20s expressed distress due to poor mental health, needing a longer time to get the diagnosis, and having weight and eating concerns. While women with PCOS in their 30s discussed their menstrual irregularities and fertility issues, those in their 40s expressed their concerns about the societal expectations of women when diagnosed with PCOS. The concerns varied across ethnicities as well.
Conclusion: PCOS has wide-ranging consequences for women living with the condition, with many dissatisfied with the clinical support they currently receive. The concerns and expectations vary across ages and ethnicities. Therefore, we propose involving women with PCOS to co-create clinical and educational resources informed by lived experiences to provide end-user-informed services.
1 Introduction
Polycystic ovary syndrome (PCOS) is one of the most common endocrine conditions affecting women of reproductive age with a global prevalence around 10% (1). It classically presents with oligomenorrhoea or amenorrhoea, infertility, hirsutism, acne, and obesity (2). The hallmarks of PCOS include hyperandrogenism, oligo/anovulation and polycystic ovarian morphology. It is also associated with cardio-metabolic diseases such as obesity and diabetes (3), psychological disorders (4) and increased cancer risk (5, 6). The disease is multifactorial, and its complex pathophysiology involves multiple pathways (7). A diagnosis of PCOS is made if other causes of patients’ symptoms are ruled out and patients fulfil two of the three diagnostic criteria (oligomenorrhoea or anovulatory cycles, biochemical or clinical hyperandrogenism, polycystic ovaries seen on ultrasound scan) (8).
PCOS often presents during puberty and the characteristic signs and symptoms coincide with the development of normal physiological findings during this period of life (9, 10), consequently complicating the diagnostic process. Despite its high prevalence, there is still lack of awareness among healthcare professionals regarding its long-term health consequences and its negative impact on mental health (11), consequently leading to delayed diagnosis and treatment. Gibson-Helm et al. reported that a third of women with PCOS reported that it took >2 years and >3 healthcare professionals to establish a diagnosis of PCOS (12). Another multi-methods study has shown that women with PCOS felt they were not taken seriously by their doctors (13). Additionally, women with PCOS often struggle to find reputable sources of information about their condition. Although physicians are integral in the education of patients, the latter often find resources accessed at home much more helpful. It is reported that 98.2% of patients search the internet for PCOS related information (14, 15). A recent systematic review by Lau et al. regarding the experiences of women and individuals with PCOS found that patients struggle to identify relevant, high quality educational resources regarding their condition (16). To date, existing educational and awareness resources for polycystic ovary syndrome (PCOS) have had limited inclusion of patient perspectives. Therefore, we conducted this mixed-methods study to understand the lived experiences, perceptions, and opinions on the current standard of care of women with PCOS which can then help us create a better-represented educational resource for the condition.
2 Methods
Women aged 18-60 years were invited to complete an online survey during April and May 2021. This survey was primarily promoted through patient support groups: PCOS Verity, DAISy-PCOS leadership group, and PCOS Vitality. The survey started with information about the study and a privacy statement. Interested participants had to complete an in-built consent form as part of the study before proceeding to answering the questions. Nine closed questions in this survey focused on participant demographics, such as age, gender, ethnicity, country of residence, and history of PCOS diagnosis. Participants with a formal diagnosis of PCOS were asked about the year of PCOS diagnosis, and a further four open-ended questions regarding their lived experiences at the onset of the symptoms of PCOS, their journey during diagnosis, an explanation of PCOS to their younger self, and any advice for their younger self (Supplementary Table 1). Participants had the option to share their views for the open-ended questions either as a written text or as a voice note on WhatsApp®. The data from the latter was transcribed verbatim. Phone numbers of participants obtained for collection of voice note data were removed after data collection was complete. All data were anonymised at the point of analysis. Data were then coded using NVivo 12 software and analysed using a combination of content analysis and thematic inductive qualitative methods (17–19). Authors GL and ME read through the data and independently identified and applied codes through open coding. Following this, GL and ME collaboratively organized the codes into themes, revised the codes as appropriate. This process until all data were coded and there was an agreement about the application of codes and themes to the whole data set. Authors PK and AL then reviewed the codes and themes to arrive at an agreement.
After synthesising the themes, we arranged the data into groups based on the participants’ age (20–29, 30–39, 40–49, 50–59) and ethnicity (White and Other). We then studied the frequency of various themes in these groups and highlighted the most commonly occurring themes from them.
3 Results
A total of 45 women completed the survey. 43 of 45 participants reported they had a formal diagnosis of PCOS; the remaining two had suspected PCOS which was under active investigation and hence excluded from further analysis. Four participants opted to share their views as voice note recordings; one of them could not be contacted as they had incorrectly indicated their phone number. As a result, data from 42 participants for the open question portion of the survey were analyzed, generating 1326 references towards their experiences and perception about PCOS in total (Supplementary 2).
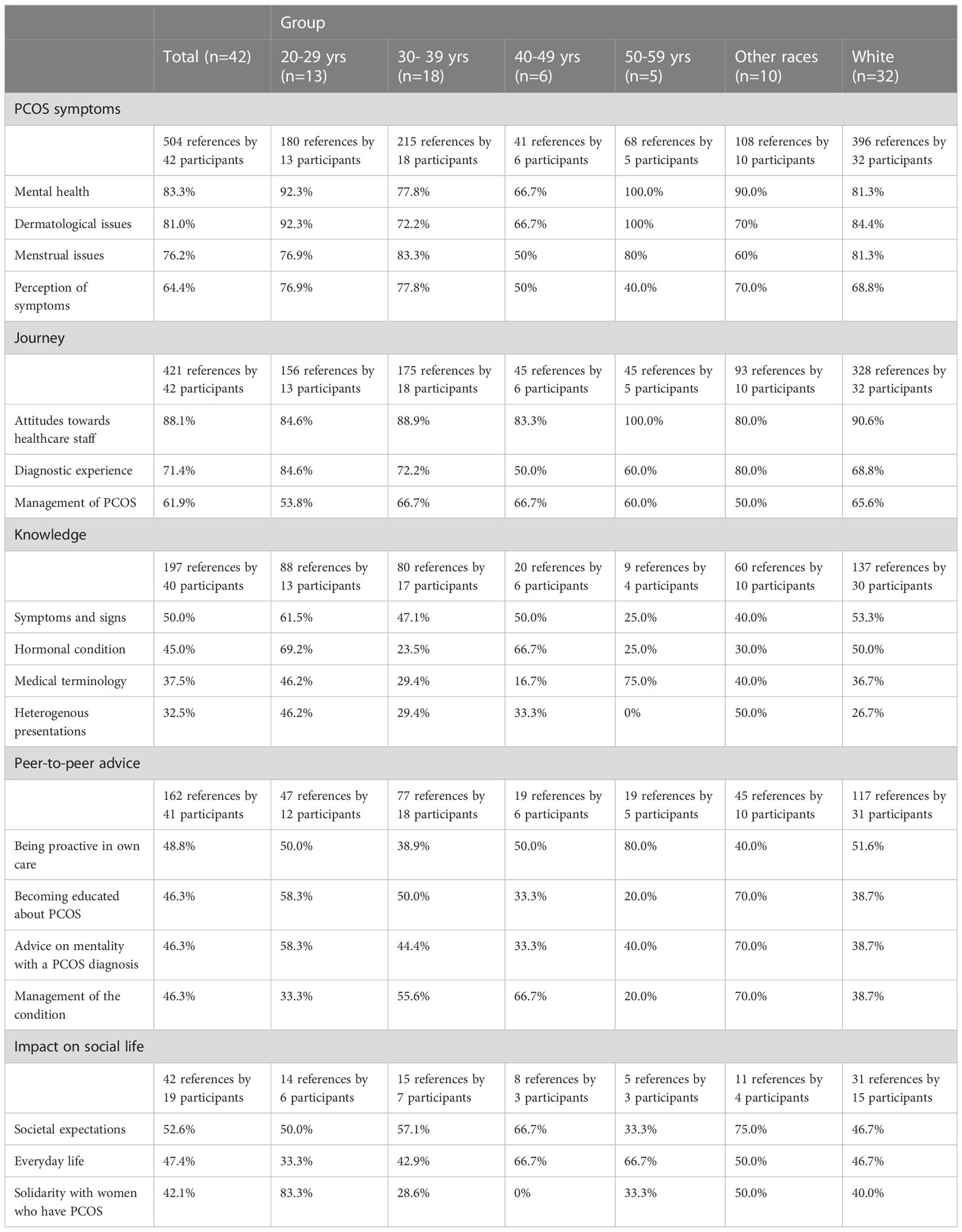
Overall, five common themes emerged: symptoms (504 references by 42 participants), patient journey (421 references by 42 participants), knowledge (197 references by 40 participants), peer-to-peer advice (162 references by 41 participants), and impact of PCOS on social aspects of life (42 references by 19 participants) (Table 1). The median and interquartile range of age in the White group was 37 (25.75-41.75) and in the other group was 27 (24–34). The various themes are discussed in greater detail below:
3.1 PCOS symptoms
The most common symptom participants reported was poor mental health. Within this theme, low mood or depression and a lack of self-worth were most notable. These were frequently discussed in connection with symptoms affecting participants’ outward appearance, particularly weight gain, hair growth, and acne. The second most reported symptom was dermatological issues, particularly hair related problems, namely hirsutism and alopecia, followed by menstrual irregularities. The latter was often the initial symptom prompting to seek professional advice. There were fewer reports of distress associated with this symptom compared to skin and hair concerns, except in the context of fertility. Many participants reported being on a form of contraceptive pill helped alleviate their menstrual irregularity symptoms. Below is an example quotation for PCOS related symptoms. More such examples are included in Supplementary Table 2.
Participant 19: “I stress myself out daily just looking at my knickers every time I go to the bathroom just hoping I’ve got a period. Knowing I’m not ovulating and don’t have enough progesterone again makes me feel I’m not a woman and confirms my body is not healthy”.
3.2 Patient journey
The most discussed theme within the patient journey domain were attitudes towards healthcare staff. 88.1% felt dissatisfied with PCOS-related healthcare support. Most women felt clinicians were dismissive and lacked empathy. Several participants were confused by their diagnosis and found explanations from clinicians unhelpful.
The second most common theme was diagnostic experience (71.4%). A lengthy diagnostic journey was most frequently reported (35.7%), with many finding it emotionally demanding as diagnosis often took years. Some reported that although clinicians suspected PCOS, their diagnosis was still delayed due to lack of timely investigations, which left women feeling isolated with little professional support.
The third most discussed theme was PCOS management (61.9%). Contraception (40.5%), lifestyle changes (21.4%), and management of dermatological symptoms (21.4%) were most common. Many participants described contraception use in their adolescence for menstrual cycle regulation. The most common contraception used was the oral pill. Lifestyle changes were usually focused on diet rather than exercise, with the aim of weight loss. A number of participants found lifestyle changes stressful. Methods, such as shaving, laser treatment, and using skincare products were reported for management of excess hair growth and acne.
Participant 21: “Terrible. I first went to the doctor about my periods when I was around 19, I had been in bed for a week because of the pain, I was prescribed painkillers, but no further investigation was completed. I went again a couple of years later and was advised that my periods would probably be irregular until I had a baby. I was generally prescribed contraceptive medication without any follow up for the reasons for needing it. In 2018 I went to the doctor to advise that I had come off contraceptive pills and was having issues again with my periods and a GP advised that they suspected PCOS, it then took two years until I had a five-minute appointment with a consultant that confirmed a. I had PCOS and b. There was nothing that I could be given to encourage me to ovulate as I was too fat.”
More examples are included in Supplementary Table 3.
3.3 Knowledge of PCOS
The most commonly discussed topic in the domain of knowledge of PCOS was signs and symptoms including menstrual symptoms (27.5%), weight and eating (22.5%), dermatological (17.5%), mental health (15.0%) and fertility issues (15.0%).
Some participants used medical terminology when discussing PCOS (37.5%). Notably, the term ‘hirsutism’ was the most frequently used. As expected, participants who employed medical terminologies in their answers, often used it on multiple occasions. Furthermore, 32.5% participants acknowledged the condition’s heterogeneous presentation and clearly understood what a syndrome was and described it accurately.
Participant 7: “… I would say that although the condition involves my ovaries, and that there would be potential implication when trying to get pregnant”.
More examples are included in Supplementary Table 4.
3.4 Peer-to-peer advice
A concept first established in mental health services, peer-to-peer advice can be defined as a form of social and emotional support that is mutually offered or provided by one person to another sharing a similar health condition to bring about a desired social or personal change (20).
The most common themes in peer-to-peer advice involved being proactive in own care (48.8%), becoming educated about PCOS (46.3%), mentality (46.3%), and management of the condition (46.3%). Many participants recommend being proactive early in one’s PCOS journey. Many considered education important to improve health in the long-term and to advocate for themselves in the future when meeting healthcare professionals. Most advice about mentality centered on remaining positive. Advice on management focused on lifestyle changes, particularly diet and exercise. Many acknowledged that lifestyle changes were not a cure but were associated with better control of the condition and, therefore, improved outcomes.
Participant 31: “It would be to take a driving seat approach, and to put myself at the forefront when it comes to communicating with doctors or telling them what I think is going on with my body”.
More examples are included in Supplementary Table 5.
3.5 Impact of PCOS on social aspects of life
Within this, the most common theme discussed was the societal expectations of women (52.6%). While all participants identified themselves as women, many believed PCOS rendered them less feminine due to the associated masculine appearance which did not align with current beauty ideals. Some women felt the pressure to bear children.
Another aspect discussed was the condition’s impact on everyday life, including school, career, and interactions with their partners (47.4%). Subfertility issues associated with PCOS were reported to cause strain on romantic relationships, with participants feeling inadequate as a partner.
The third most common theme was solidarity with other women with PCOS (42.1%). Some participants acknowledged the importance of bonding with others with PCOS not only to improve their emotional well-being but also to share experience and gain knowledge.
Participant 7: “I find that the pressures imposed by society on women to be thin and have beautiful hair are in direct opposition with the symptoms I have experienced as a result of PCOS.”
More examples are included in Supplementary Table 6.
3.5.1 Concerns and expectations across age groups and ethnicity
More women in their 20s expressed distress due to poor mental health, needing longer time to get diagnosis, and having weight and eating concerns. Interestingly, several women in this age group also acknowledged the condition’s heterogeneous presentation and understood what a syndrome was. While more women in their 30s discussed their menstrual irregularities and fertility issues, those in their 40s expressed their concerns about the societal expectations of women when diagnosed with PCOS.
While women of White ethnicity focused more on the distress due to poor mental health associated with PCOS, women from other ethnicities expressed their concerns with the time it took to get diagnosised and social consequences of the diagnosis.
4 Discussion
Seeking patients’ perspectives is vital to improve healthcare experiences and services. While themes regarding symptoms, the patient journey, and knowledge have been reported elsewhere, we report a number of new findings. Our findings emphasise the importance of peer-to-peer advice. Percy et al. found support networks led by specialist nurses to be a significant factor in mitigating the psychological impact of PCOS, especially for newly diagnosed women (21). In the internet era, online support groups have proved to be a versatile and easily accessible source for peer-to-peer support (15). With an ability to remain anonymous and to tap improved to resources from all over the world, online support groups are turning out to be a game-changer in managing chronic conditions like PCOS. Despite this, only 18.8% of patients joined an online PCOS support group or forum (14). It may be beneficial for clinicians to signpost these groups to patients in the future. However, some potential disadvantages should be considered with the use of online support groups, including anxiety because of hearing others’ negative experiences and feelings of being an outsider (22).
Our participants also emphasised the impact of PCOS on their social life. Sharma et al. and Carron et al. highlighted the difficulties women with PCOS encountered in communities where those who struggled to conceive children suffered from devaluation of their social status (23, 24). Some described menstrual symptoms to be debilitating, affecting their school life or career. Similarly, Native American women with PCOS reported being unable to attend tribal ceremonies for fear of unpredictable menses (24).
Women aged 20-29 are more knowledgeable compared to older participants in our study. This may be due to easier access to information on internet and social media. Social media influencers and public events such as PCOS awareness months may also have played a role in engaging the internet-active population (25, 26). Also, taboo may have played a role as topics such as fertility and femininity were not mainstream at the turn of the last century.
Women with PCOS, of non-White ethnicity reported greater delays in diagnosis and discussed mental health and societal pressures more than the rest of the group. To the best of our knowledge, this is the first study of its kind to explore the perception of women with PCOS across age and ethnicity in such detail.
Participants in our study considered some healthcare professionals to be dismissive, lacking clarity in their explanations and empathy. Dissatisfaction with care of women with PCOS may stem from lengthy diagnostic and management processes involved (12, 27) with similar findings reported within other literature (14, 28). PCOS can be difficult to identify due to its heterogenous presentation and presence of several controversies in the pathogenesis, diagnosis, and treatment of PCOS (29). It can also be difficult to manage the symptoms of PCOS once it is diagnosed as only the combined oral contraceptive pill is recommended for the condition. Other medications such as metformin and anti-androgen drugs may also be considered in the management although these are “off-label” uses (1). Longer treatment delay eventually leads to significant periods of time without support or management which can lead to dissatisfaction with care.
Participants in our study reported struggles at the start of their diagnostic journey and following their initial diagnosis of PCOS due to lack of information. Gibson-Helm et al. have reported similar findings, where 60% of women said they were not given information about PCOS when diagnosed, and 20% felt the information given was inadequate (30). Interestingly, the majority of participants in our study demonstrated rather in-depth understanding about PCOS. However, they reported this information was rarely received from healthcare professionals, and instead was a result of their own research.
Mental health was the most experienced symptom in women with PCOS across both non-White (90%) and White ethnicities (81.3%). According to Hillman et al., 74.9% of women with PCOS reported poor mental health due to the condition. Interestingly, they found that women of White ethnic background were more concerned about their mental health and subfertility (43.8% of White participants, compared to 0% non-White participants) than British Asian women (11). This may suggest an area to explore further, to ensure women of all races have adequate healthcare support for mental health and subfertility issues. Additionally, mitigating communication barriers for non-White groups is important to ensure support reaches communities who need it the most.
4.1 Strengths and weaknesses
While a sample size of 42 participants may be considered small for quantitative studies, it is considered large for the qualitative methodology we used in the study (31). The rich, detailed data obtained from these 42 participants ensured our ability to perform content analysis and delineate the differences in perception of women with PCOS across age groups and ethnic backgrounds. An average of ~400 words per participant (16,606 words in total) for the four open-ended questions in our survey depicts the long and in-depth answers from participants which adds strength to our findings. Further, all participants in our study came from a verified source, enabling us to confirm the diagnosis of PCOS.
The median time since diagnosis within the participants in this study was 22 years, which is both a strength and weakness; while the lived experience with PCOS over time can help understand the spectrum of PCOS’s impact across the lifespan, our findings may be limited by a recall bias. We also did not have sufficient representation from all the major ethnic groups; hence further studies with large and comprehensive samples are needed to delineate the differences in experience and perception of PCOS across various ethnicities. We acknowledge that the study was conducted during the COVID pandemic and thus opinions and perceptions of PCOS may have been impacted by limited access to clinics and outpatient services.
5 Conclusion
Women with PCOS were impacted physically and emotionally by their symptoms and many women felt dissatisfied with the support they received from healthcare professionals. Experiences varied across age and ethnicity further reaffirming the need for individualised approaches when managing PCOS. Therefore, we propose greater involvement of women with PCOS while designing clinical and educational resources to ensure these are acceptable to women living with the condition.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Health Research Authority (HRA). The patients/participants provided their written informed consent to participate in this study.
Author contributions
AL and PK conceptualised the study. ME and GL were involved in all stages of the study since conception, contributing equally to this work and sharing the first authorship. ME, GL, PK and AL conducted the thematic analysis of the data. MD conducted the searches alongside ME and GL and screened the data to ensure appropriateness and authenticity. CDTG provided critical insights during the execution of the study to ensure the voice of public was appropriately captured and recorded in the article. Members of the PCOS SEva team contributed substantially to the conception and design of the study and were involved in discussions at all stages of the study. The PCOS SEva team includes JJC, HKG, MH, SJ, HK, TL, EM, AN, LR, CS, JS, SW, and NZ. AL and PK supervised all stages of the study and share joint senior authorship of this article. ME and GL prepared the original draft of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work has been supported by the Wellcome Trust (investigator grant WT209492/Z/17/Z, to WA) and the Health Research Board (Emerging Clinician Scientist Award ECSA-FA-2020-001, to MWOR). WA receives support from the National Institute for Health and Care Research (NIHR) Birmingham Biomedical Research Centre at the University Hospitals Birmingham NHS Foundation Trust and the University of Birmingham (grant ref. no. BRC-1215-20009). The views expressed are those of the authors and not necessarily those of the NIHR UK or the Department of Health and Social Care UK.
Acknowledgments
We thank all women with PCOS who participated in our study and shared their lived experience. Throughout this manuscript we refer to individuals with PCOS as women; however, we acknowledge that not everyone with PCOS will identify as a woman.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2023.1175548/full#supplementary-material
References
1. Joham AE, Norman RJ, Stener-Victorin E, Legro RS, Franks S, Moran LJ, et al. Polycystic ovary syndrome. Lancet Diabetes Endocrinol (2022) 10(9):668–80. doi: 10.1016/S2213-8587(22)00163-2
2. P S. Polycystic ovary syndrome (PCOS), an inflammatory, systemic, lifestyle endocrinopathy. J Steroid Biochem Mol Biol (2018) 182:27–36. doi: 10.1016/j.jsbmb.2018.04.008
3. Elting MW, Korsen TJM, Bezemer PD, Schoemaker J. Prevalence of diabetes mellitus, hypertension and cardiac complaints in a follow-up study of a Dutch PCOS population. Hum Reprod (2001) 16(3):556–60. doi: 10.1093/humrep/16.3.556
4. Sheikh J, Khalil H, Shaikh S, Hebbar M, Zia N, Wicks S, et al. Emotional and psychosexual wellbeing is influenced by ethnicity and birthplace in women and individuals with polycystic ovary syndrome in the UK and India. BJOG (2023) 130(8):978–86. doi: 10.1111/1471-0528.17428
5. Johnson JE, Daley D, Tarta C, Stanciu P. Risk of endometrial cancer in patients with polycystic ovarian syndrome: A meta-analysis. Oncol Lett (2023) 25(4):168. doi: 10.3892/ol.2023.13754
6. Zhong X, Li Y, Liang W, Hu Q, Zeng A, Ding M, et al. Clinical and metabolic characteristics of endometrial lesions in polycystic ovary syndrome at reproductive age. BMC Womens Health (2023) 23(1):236. doi: 10.1186/s12905-023-02339-7
7. Khan MJ, Ullah A, Basit S. Genetic basis of polycystic ovary syndrome (PCOS): current perspectives. Appl Clin Genet (2019) 12:249. doi: 10.2147/TACG.S200341
8. Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group, Group RESPCW. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril (2004) 81(1):19–25. doi: 10.1016/j.fertnstert.2003.10.004
9. Roe AH, Dokras A. The diagnosis of polycystic ovary syndrome in adolescents. Rev Obstet Gynecol (2011) 4(2):45.
10. Agapova SE, Cameo T, Sopher AB, Oberfield SE. Diagnosis and challenges of polycystic ovary syndrome in adolescence. Semin Reprod Med (2014) 32(3):194. doi: 10.1055/s-0034-1371091
11. Hillman SC, Bryce C, Caleyachetty R, Dale J. Women’s experiences of diagnosis and management of polycystic ovary syndrome: a mixed-methods study in general practice. Br J Gen Pract (2020) 70(694):e322–9. doi: 10.3399/bjgp20X708881
12. Gibson-Helm M, Teede H, et al. Delayed diagnosis and a lack of information associated with dissatisfaction in women with polycystic ovary syndrome. J Clin Endocrinol Metab (2017) 102(2):604–12. doi: 10.1210/jc.2016-2963
13. Ismayilova M, Yaya S. “I felt like she didn’t take me seriously”: a multi-methods study examining patient satisfaction and experiences with polycystic ovary syndrome (PCOS) in Canada. BMC Womens Health (2022) 22(1):47. doi: 10.1186/s12905-022-01630-3
14. Hoyos LR, Putra M, Armstrong AA, Cheng CY, Riestenberg CK, Schooler TA, et al. Measures of patient dissatisfaction with health care in polycystic ovary syndrome: retrospective analysis. J Med Internet Res (2020) 22(4):e16541. doi: 10.2196/16541
15. Avery JC, Braunack-Mayer AJ. The information needs of women diagnosed with Polycystic Ovarian Syndrome–implications for treatment and health outcomes. BMC Womens Health (2007) 7. doi: 10.1186/1472-6874-7-9
16. Lau GM, Elghobashy M, Thanki M, Ibegbulam S, Latthe P, Gillett CDT, et al. A systematic review of lived experiences of people with polycystic ovary syndrome highlights the need for holistic care and co-creation of educational resources. Front Endocrinol (Lausanne) (2022) 13:2958. doi: 10.3389/fendo.2022.1064937
17. Barbara Downe-Wamboldt RNP. Content analysis: Method, applications, and issues. Health Care Women Int (2009) 13(3):313–21. doi: 10.1080/07399339209516006
18. Bengtsson M. How to plan and perform a qualitative study using content analysis. NursingPlus Open (2016) 2:8–14. doi: 10.1016/j.npls.2016.01.001
19. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol (2006) 3(2):77–101. doi: 10.1191/1478088706qp063oa
20. Solomon P. Peer support/peer provided services underlying processes, benefits, and critical ingredients. Psychiatr Rehabil J (2004) 27(4):392–401. doi: 10.2975/27.2004.392.401
21. Percy CA, Gibbs T, Potter L, Boardman S. Nurse-led peer support group: experiences of women with polycystic ovary syndrome. J Adv Nurs (2009) 65(10):2046–55. doi: 10.1111/j.1365-2648.2009.05061.x
22. Holbrey S, Coulson NS. A qualitative investigation of the impact of peer to peer online support for women living with Polycystic Ovary Syndrome. BMC Women’s Health (2013) 13(1):1–9. doi: 10.1186/1472-6874-13-51
23. Sharma S, Mishra AJ. Tabooed disease in alienated bodies: A study of women suffering from Polycystic Ovary Syndrome (PCOS). Clin Epidemiol Glob Health (2018) 6(3):130–6. doi: 10.1016/j.cegh.2017.09.001
24. Carron R, Kooienga S, Gilman-Kehrer E, Alvero R. Cultural experiences, patterns, and practices of American Indian women with Polycystic Ovary Syndrome: an Ethnonursing study. J Transcult Nurs (2020) 31(2):162–70. doi: 10.1177/1043659619856670
25. Elhariry M, Malhotra K, Solomon M, Goyal K, Kempegowda P. Top 100 #PCOS influencers: Understanding who, why and how online content for PCOS is influenced. Front Endocrinol (Lausanne) (2022) 13:3213. doi: 10.3389/fendo.2022.1084047
26. Malhotra K, Pan CSC, Davitadze M, SEva TP, Kempegowda P, Chu JJ, et al. Identifying the challenges and opportunities of PCOS awareness month by analysing its global digital impact. Front Endocrinol (Lausanne) (2023) 14:1109141/full. doi: 10.3389/fendo.2023.1109141/full
27. Copp T, Hersch J, Muscat DM, McCaffery KJ, Doust J, Dokras A, et al. The benefits and harms of receiving a polycystic ovary syndrome diagnosis: a qualitative study of women’s experiences. Hum Reprod Open (2019) 2019(4):hoz026. doi: 10.1093/hropen/hoz026
28. Tomlinson J, Pinkney J, Adams L, Stenhouse E, Bendall A, Corrigan O, et al. The diagnosis and lived experience of polycystic ovary syndrome: A qualitative study. J Adv Nurs (2017) 73(10):2318–26. doi: 10.1111/jan.13300
29. Armanini D, Boscaro M, Bordin L, Sabbadin C. Controversies in the pathogenesis, diagnosis and treatment of PCOS: focus on insulin resistance, inflammation, and hyperandrogenism. Int J Mol Sci (2022) 23(8):4110. doi: 10.3390/ijms23084110
30. Gibson-Helm ME, Lucas IM, Boyle JA, Teede HJ. Women’s experiences of polycystic ovary syndrome diagnosis. Fam Pract (2014) 31(5):545–9. doi: 10.1093/fampra/cmu028
Keywords: polycystic ovary syndrome, qualitative research, education, perceptions, polycystic ovarian syndrome, age, ethnicity
Citation: Elghobashy M, Lau GM, Davitadze M, Gillett CDT, O’Reilly MW, Arlt W, PCOS SEva Working Group, Lindenmeyer A and Kempegowda P (2023) Concerns and expectations in women with polycystic ovary syndrome vary across age and ethnicity: findings from PCOS Pearls Study. Front. Endocrinol. 14:1175548. doi: 10.3389/fendo.2023.1175548
Received: 27 February 2023; Accepted: 11 July 2023;
Published: 09 August 2023.
Edited by:
Albert Salas-Huetos, University of Rovira I Virgili, SpainReviewed by:
Chiara Sabbadin, University of Padua, ItalyHamid Mani, Isle of Wight NHS Trust, United Kingdom
Copyright © 2023 Elghobashy, Lau, Davitadze, Gillett, O’Reilly, Arlt, PCOS SEva Working Group, Lindenmeyer and Kempegowda. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Punith Kempegowda, cC5rZW1wZWdvd2RhQGJoYW0uYWMudWs=
†These authors share first authorship
‡These authors share senior authorship
 Mirna Elghobashy1†
Mirna Elghobashy1† Gar Mun Lau
Gar Mun Lau Meri Davitadze
Meri Davitadze Antje Lindenmeyer
Antje Lindenmeyer Punith Kempegowda
Punith Kempegowda