- 1Institute for Maternal and Child Health, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) Burlo Garofolo, Trieste, Italy
- 2Faculty of Medicine, University of Ljubljana, Ljubljana, Slovenia
- 3Department of Endocrinology, Diabetes and Metabolism, University Children’s Hospital, University Medical Centre Ljubljana, Ljubljana, Slovenia
- 4Center for Pediatric Diabetology, Azienda Ospedaliero-Universitaria (AOU) Città Della Salute e Della Scienza, Torino, Italy
- 5Diabetes Research Institute, Department of Pediatrics, IRCCS San Raffaele Hospital, Milano, Italy
- 6Division of Pediatrics, S. Chiara General Hospital, Trento, Italy
- 7Division of Pediatrics, Department of Health Sciences, Università Del Piemonte Orientale, Novara, Italy
Introduction: The purpose of this study was to evaluate lipid profile and kidney function in children and adolescents with Type 1 Diabetes.
Methods: This was a retrospective study including 324 children and adolescents with Type 1 Diabetes (48% females, mean age 13.1 ± 3.2 years). For all participants, demographic and clinical information were collected. The prevalence of dyslipidemia and kidney function markers were analyzed according to age. Multivariate linear regression analyses were performed to test the association of lipids or markers of renal function with demographic and clinical information (sex, age, disease duration, BMI SDS, HbA1c).
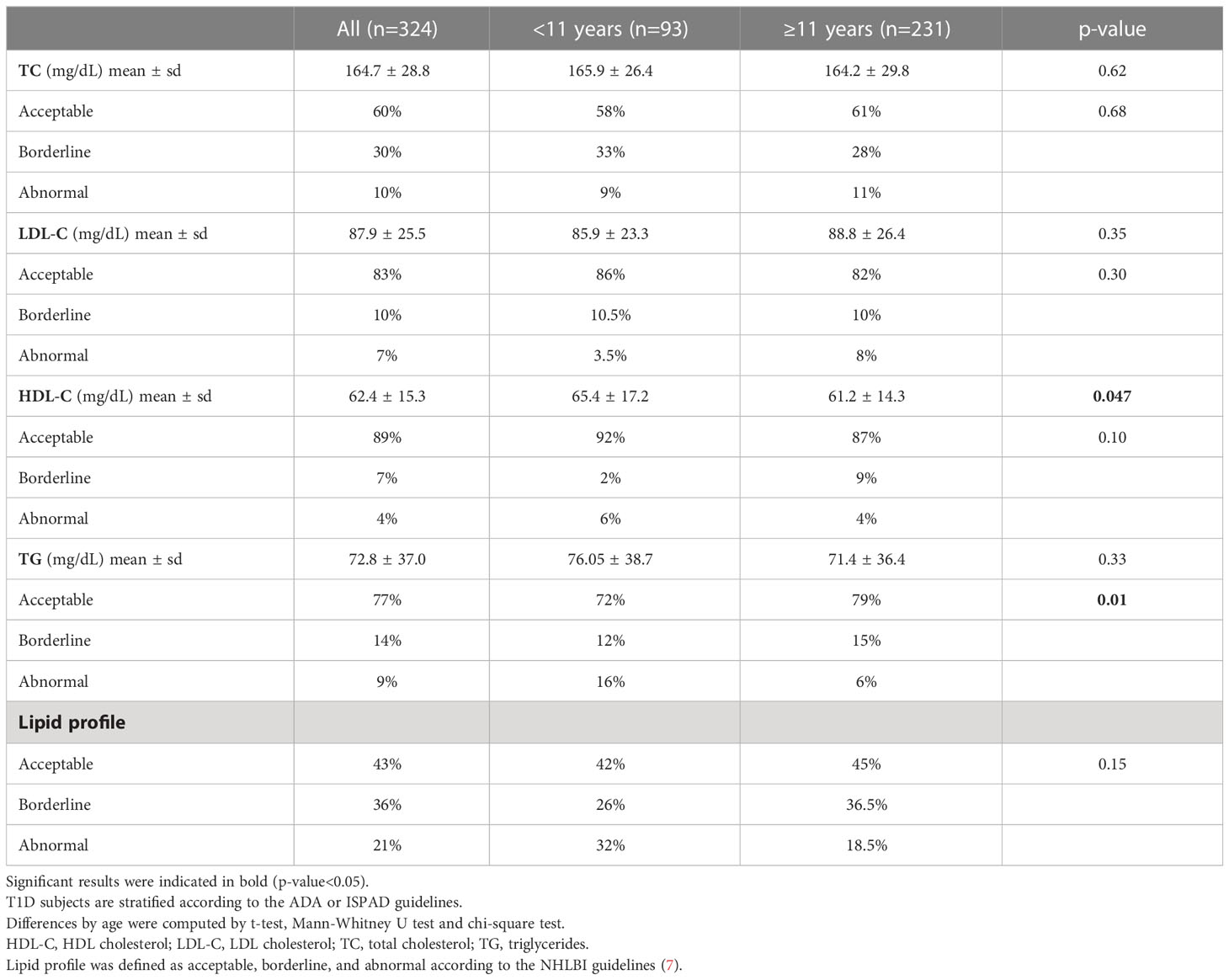
Results: In our study the rate of dyslipidemia reached 32% in children <11 years and 18.5% in those ≥11 years. Children <11 years presented significantly higher triglyceride values. While the albumin-to-creatinine ratio was normal in all individuals, 17% had mildly reduced estimated glomerular filtration rate. Median of HbA1c was the most important determinant of lipids and kidney function, being associated with Total Cholesterol (p-value<0.001); LDL Cholesterol (p-value=0.009), HDL Cholesterol (p-value=0.045) and eGFR (p-value=0.001).
Conclusion: Dyslipidemia could be present both in children and adolescents, suggesting that screening for markers of diabetic complications should be performed regardless of age, pubertal stage, or disease duration, to optimize glycemia and medical nutrition therapy and/or to start a specific medical treatment.
1 Introduction
The development of micro and macrovascular complications is rare in children and adolescents with Type 1 Diabetes (T1D) meeting recommended HbA1c value: a declining incidence of vascular complications has been reported in the developed world (1, 2), while it is still an issue in developing countries (3).
The 2023 ADA Standards of Medical Care and the 2022 ISPAD Clinical Practice in children and adolescents with T1D (4, 5) still suggest an age limit to perform screening for risk factors for diabetes-related complications, such as dyslipidemia and albuminuria. Nevertheless, several studies demonstrated that the atherosclerotic process begins in childhood and that the first subclinical indications of cardiovascular risk may occur before puberty (6). Lipids above the recommended values were previously reported in subjects with T1D from 2 years of age, confirming that risk factors for cardiovascular complications start early after diabetes diagnosis (7, 8). Similarly, decreased estimated glomerular filtration rates were reported in children with T1D between 2 and 18 years of age (9).
However, overall, these past studies did not perform a comparison of the prevalence of lipid and renal abnormalities among T1D subjects belonging to different age groups.
Therefore, in this study, we analyzed lipid profile and kidney function in children and adolescents with T1D stratified for cut-off established by ADA and ISPAD guidelines for start to screening, hypothesizing that their screening is of fundamental importance, regardless of age, pubertal status and disease duration. Moreover, we also analyzed demographic and clinical factors associated with lipids and renal markers.
2 Methods
2.1 Study participants
Three hundred twenty-four subjects with T1D and age <21 years, with at least one year of disease duration, were recruited at Diabetes Units of IRCCS Burlo Garofolo (Trieste, Italy) (n=90), Regina Margherita Children’s hospital (Torino, Italy) (n=90), Santa Chiara hospital (Trento, Italy), (n=14), University Medical Center (Ljubljana, Slovenia) (n=80) and IRCCS San Raffaele (Milano, Italy) (n=50) between 2018 and 2021.
2.2 Study procedures
We retrospectively collected demographic and anthropometric information, such as age, sex, height, weight, and pubertal status. Puberty is defined as the presence of breast budding in girls and a testicular volume of 4 ml in boys. Standard deviation scores of body mass index (BMI SDS) were calculated according to WHO reference charts using the Growth Calculator 4 software (http://www.weboriented.it/gh4/).
Clinical information included age at diagnosis, disease duration, and HbA1c at the regular visits in the previous year. Based on the cut-off of HbA1c of 7% (53mmol/mol), T1D subjects were categorized in two groups (4, 5).
Laboratory data were collected from the latest performed screening.
Fasting lipids were collected, and the lipids profile was defined as acceptable, borderline, and abnormal according to the NHLBI guidelines (10). The following cut-off points for dyslipidemia definition were considered: total cholesterol (TC) ≥200 mg/dL; LDL cholesterol (LDL-C) ≥130 mg/dL; HDL cholesterol (HDL-C) <40 mg/dL; triglycerides (TG) ≥100 mg/dL up to 9 years and triglycerides ≥130 mg/dL over 9 years. Subjects with single or combined lipids alterations were considered “abnormal lipid profile.”
Evaluation of albuminuria was determined as albumin to creatinine ratio (ACR), by first monitoring urine sample, and ACR value >30 mg/g were considered abnormal (11).
The estimated glomerular filtration rate (eGFR) was calculated using Schwartz’s equation: 0.413 x height (cm)/serum creatinine mg/dL (12). eGFR values <90 mL/min/1.73 m2 were considered abnormal (11).
2.3 Statistical analysis
Descriptive statistics represent percentages, means, standard deviations (SD). T1D subjects were stratified for pubertal status (pre-pubertal vs. pubertal), disease duration (<5 vs. ≥5 years) following ADA or ISPAD guidelines. Moreover, for age ISPAD guidelines (<11 vs. ≥11) were applied for lipids analysis, while ADA guidelines (≤10 vs. >10 years) for kidney function analysis.
The skewness and kurtosis were calculated for testing the normality. Differences between T1D individuals stratified for age, pubertal status or disease duration were analyzed by chi-squared tests to compare categorical data. While t-tests or Mann-Whitney test used to compare the means when the variable is normally or not-normally distributed, respectively.
Multivariate linear regression analyses were performed to test the association of lipids or markers of renal function with sex, age, disease duration, BMI SDS and median HbA1c as explanatory variables.
Statistical analyses were performed with R stats package, v 4.2.2 (www.r-project.org).
3 Results
Among the 324 T1D individuals included in this study, 156 (48%) were females. The mean age at enrollment was 13.1 ± 3.2 years, and 77% were pubertal, with a mean BMI SDS of 0.13 ± 1.1. The mean disease duration was 5.4 ± 3.6 years. Median HbA1c over the previous year was 7.69 ± 1.01% (60 mmol/mol). T1D characteristics were summarized in Table 1.
Lipid profiles and renal function markers are reported in Table 2 and Table 3, respectively.
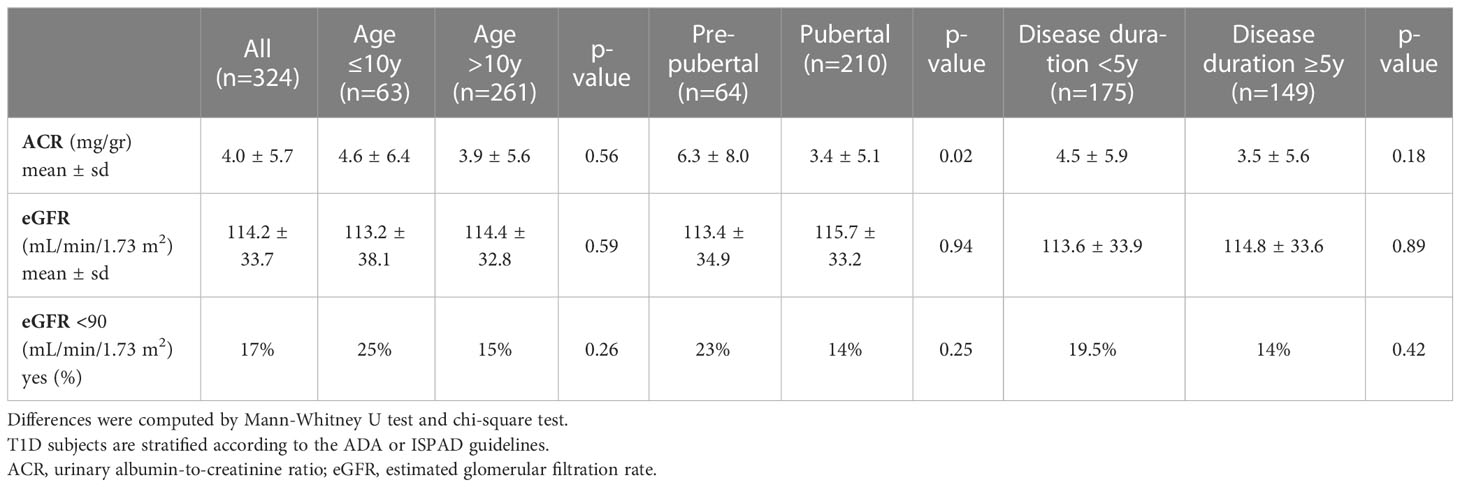
Table 3 Kidney function markers in T1D subjects stratified by age, pubertal status and disease duration.
Overall, 21% (n=65) of the participants had abnormal plasma lipid values; the percentage of dyslipidemia reached 32% (n=25) in children <11 and 18.5% (n=40) in those ≥11 years. Moreover, TG values were higher in individuals <11 (n=14) than in those ≥11 years (n=12) (16% vs. 6%, p-value=0.01) (Table 2). No other significant differences in lipid levels emerged, except for HDL-C values, which were slightly higher in children <11 than in children ≥11 years (p-value=0.047).
No significant differences emerged for eGFR. ACR levels are statistically different between non-pubertal and pubertal T1D subjects (p value=0.02), although the ACR values are in the normal range in both groups. Furthermore, around 17% of T1D subjects presented an eGFR <90 mL/min/1.73 m2, and this percentage reached 25% in children aged ≤10 years (Table 3).
At multivariate analysis, higher TC levels were associated with female sex (p-value=0.001) and high median HbA1c over the previous year (p-value<0.001); higher LDL-C levels were associated with increasing age (p-value=0.007), female sex (p-value=0.009), high median HbA1c (p-value=0.009) and slightly with increased BMI SDS (p-value=0.046); higher HDL-C value was associated with younger age (p-value=0.001) and high median HbA1c (p-value=0.045); finally, higher TG levels were directly associated with increased median HbA1c (p-value=0.033) (Table 4).
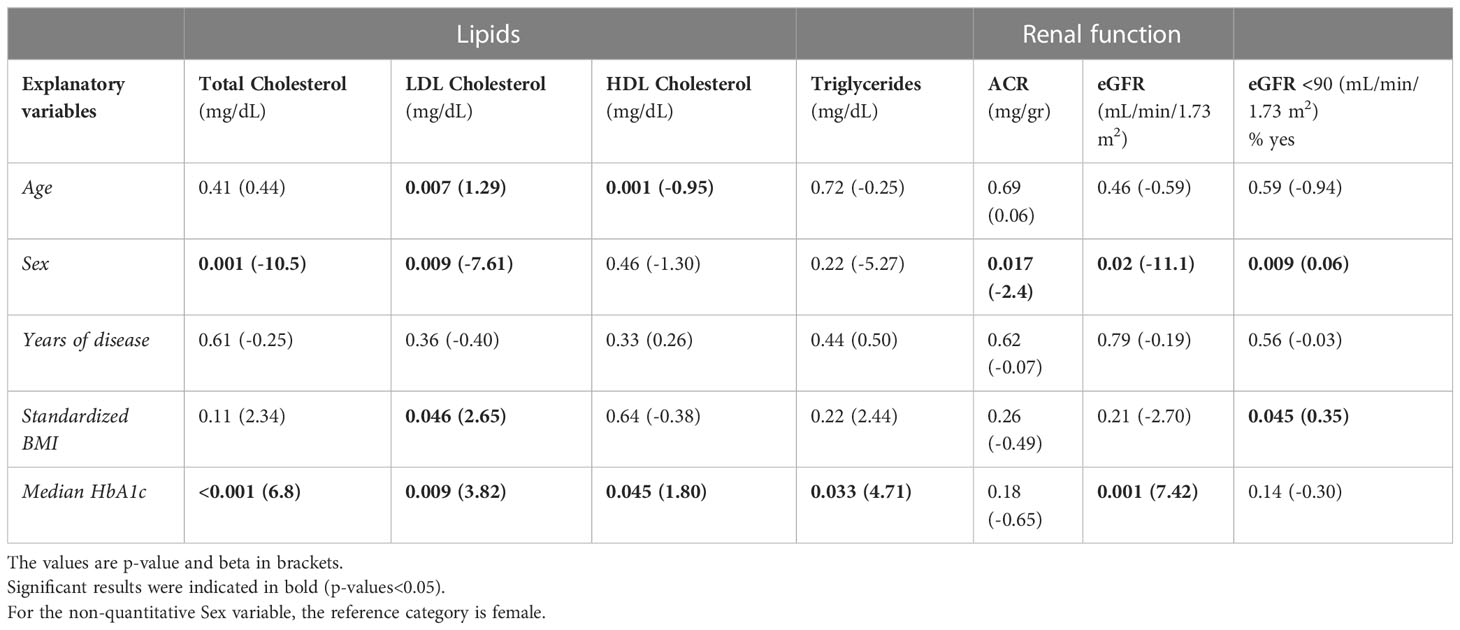
Table 4 Factors associated with lipids and renal function as assessed by multivariate regression models.
Moreover, greater ACR levels were associated with female sex (p-value=0.01), whereas higher eGFR levels were associated with female sex (p-value=0.02) and higher HbA1c value (p-value=0.001) (Table 4). Finally, eGFR<90 was associated with male sex (p-value=0.009) and with slightly increased BMI (p-value=0.045).
4 Discussion
Despite improvements in management, kidney and cardiovascular diseases are still significant causes of mortality among people with T1D (13, 14). Although they rarely occur during childhood, changes in cardiac function and lipid levels may indicate a disease process that begins early in the course of the disease (15, 16); moreover, disease onset before the age of 15 has been associated with early onset albuminuria with a more rapid decrease in eGFR (17). Intensive education and treatment at a young age may prevent or delay the onset and progression of complications (18), with a positive ‘legacy effect’ even after 30 years (19). To prevent the development of such complications, diabetes management requires multi-level risk reduction strategies that include also screening for risk factors (20).
Concerning dyslipidemia screening, ADA recommended that “if initial LDL-C is <100 mg/dL, subsequent testing should be performed at 9–11 years of age” (4). Similarly, ISPAD recommends that “screening for dyslipidemia is recommended soon after diagnosis (when glycemia is stabilized) in all young people with T1D from age 11 years”, in the absence of a family history of hypercholesterolemia or early cardiovascular death (5).
In the present study, we showed that not only there are no significant differences in lipids profile in children below and over 11 years, but also that rate of dyslipidemia (defined as single or combined lipids alterations) reached 32% in children <11 years compared to 18.5% in those ≥11 years.
We also found that elevated lipid levels were associated with higher HbA1c, confirming HbA1c over the previous year as one of the most important determinants of lipid profile. Moreover, LDL-C and HDL-C levels were associated with age, with a direct and inverse relationship, respectively. With regards to HDL-C (known as the “good” cholesterol for the well-documented inverse relationship with adverse cardiovascular outcomes), it has been shown that, in the presence of chronic inflammation or renal dysfunction, it might reverse its effect and become detrimental to endothelial function (21). Interestingly, children <11 years presented higher triglyceride values than adolescents (p-value=0.01), although this age group had fewer non-modifiable risk factors for diabetes mismanagement, such as puberty and long disease duration.
With regards to nephropathy screening, ADA recommended that “annual screening for albuminuria with a random spot urine sample for ACR should be considered at puberty or at age >10 years, whichever is earlier, once the child has had diabetes for five years” and that “eGFR should be considered at baseline and repeated as indicated based on clinical status, age, diabetes duration, and therapies” (4). Similar recommendations are given in the ISPAD guidelines that recommend starting screening for ACR and eGFR at puberty or age 11 years with 2-5 years of diabetes duration (5). In our sample, ACR was normal in all individuals. However, it has been proposed that non-albuminuric patients with diabetes may progress in any case toward chronic kidney disease; as a matter of fact, in a previous study also pediatric individuals with normal albuminuria but mildly reduced eGFR (60-89 mL/min/1.73 m2) showed a worst cardiometabolic risk profile with higher levels of insulin requirement, TG/HDL-C ratio, neutrophil/lymphocytes ratio, blood pressure, uric acid, and low HDL-C levels (22). The rate of subjects with an eGFR value below 90 mL/min/1.73 m2 in the present study was 17%, and this figure reached 25% in children under the age of 10 and 23% in the prepubertal stage, although there were no statistically significant differences between age, pubertal status, or disease duration. On the contrary, higher eGFR was associated with higher HbA1c, that directly correlates with hyperfiltration, also in individuals with short duration of T1D (23).
5 Limitations of the study
A potential limitation of this study is the lack of information on LDL-C levels at onset and family history. In addition, we have no information on other markers for the screening of renal function, such as Cystatin C. Lastly, the recruitment of only European samples, makes our findings not generalizable to other ethnic groups. Despite these limitations, the accuracy of collected clinical and demographic information is the key strength of the present study.
6 Conclusions
The findings of our study show that diabetes-associated risk factors, such as abnormal lipid profiles and mildly reduced eGFR, are already present in childhood, suggesting that screening for markers of diabetic complications should be performed regardless of age, pubertal stage, or disease duration, to optimize glycemia and medical nutrition therapy and/or to start a specific medical treatment. This should be considered in clinical management and the following standards of medical care.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The ethics committee approved the study [CEUR-2018-Em-323-Burlo (Italy) and KME-0120-65/2019/4]. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
EC, AR, and GTo designed and performed the research. EC, KD, DT, GTa, RB, RF acquired data. EC and AR analyzed and interpreted data. EC, AR, and GTo drafted the manuscript. EC, AR, KD, DT, GTa, RB, RF, IR, TB, and GTo revised the manuscript. GTo is the guarantor of this work and, as such, has full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Ministry of Health, Roma – Italy, in collaboration with the Institute for Maternal and Child Health IRCCS Burlo Garofolo, Trieste – Italy (GR-2019-12369573 to AR, RC 26/22 to AR).
Acknowledgments
We thank all the participants and the staff of the involved institutes for their support in conducting this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bojestig M, Arnqvist HJ, Hermansson G, Karlberg BE, Ludvigsson J. Declining incidence of nephropathy in insulin-dependent diabetes mellitus. N Engl J Med (1994) 330(1):15–8. doi: 10.1056/nejm199401063300103
2. Downie E, Craig ME, Hing S, Cusumano J, Chan AK, Donaghue KC. Continued reduction in the prevalence of retinopathy in adolescents with type 1 diabetes: role of insulin therapy and glycemic control. Diabetes Care (2011) 34(11):2368–73. doi: 10.2337/dc11-0102
3. Majaliwa ES, Munubhi E, Ramaiya K, Mpembeni R, Sanyiwa A, Mohn A, et al. Survey on acute and chronic complications in children and adolescents with type 1 diabetes at muhimbili national hospital in dar es salaam, Tanzania. Diabetes Care (2007) 30(9):2187–92. doi: 10.2337/dc07-0594
4. ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 14. children and adolescent: standard of care in diabetes-2023. Diabetes Care (2023) 146(Suppl 1):S230–53. doi: 10.2337/dc23-S014
5. Bjornstad P, Dart A, Donaghue KC, Dost A, Feldman EL, Tan GS, et al. ISPAD clinical practice consensus guidelines 2022: microvascular and macrovascular complications in children and adolescents with diabetes. Pediatr Diabetes (2022) 23(8):1432–50. doi: 10.1111/pedi.13444
6. Haller MJ, Stein J, Shuster J, Theriaque D, Silverstein J, Schatz DA, et al. Peripheral artery tonometry demonstrates altered endothelial function in children with type 1 diabetes. Pediatr Diabetes (2007) 8(4):193–8. doi: 10.1111/j.1399-5448.2007.00246.x
7. Fornari E, Piona C, Rabbone I, Cardella F, Mozzillo E, Predieri B, et al. Cardiovascular risk factors in children and adolescents with type 1 diabetes in Italy: a multicentric observational study. Pediatr Diabetes (2020) 21(8):1546–55. doi: 10.1111/pedi.13123
8. Schwab KO, Doerfer J, Hecker W, Grulich-Henn J, Wiemann D, Kordonouri O, et al. Spectrum and prevalence of atherogenic risk factors in 27,358 children, adolescents, and young adults with type 1 diabetes: cross-sectional data from the German diabetes documentation and quality management system (DPV). Diabetes Care (2006) 29(2):218–25. doi: 10.2337/diacare.29.02.06.dc05-0724
9. Favel K, Irvine M, Ronsley R, Panagiotopoulos C, Mammen C. Glomerular filtration rate abnormalities in children with type 1 diabetes. Can J Diabetes (2022) 46(5):457–63.e1. doi: 10.1016/j.jcjd.2022.01.007
10. Expert Panel of Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescent; National Heart, Lung and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics (2011) 128(5):S213–56. doi: 10.1542/peds.2009-2107C
11. Levey AS, Eckardt K-U, Dorman NM, Christiansen SL, Hoorn EJ, Ingelfinger JR, et al. Nomenclature for kidney function and disease: report of a kidney disease: improving global outcomes (KDIGO) consensus conference. Kidney Int (2020) 97(6):1117–29. doi: 10.1016/j.kint.2020.02.010
12. Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, et al. New equations to estimate GFR in children with CKD. J Am Soc Nephrol (2009) 20(3):629–37. doi: 10.1681/ASN.2008030287
13. Groop PH, Thomas MC, Moran JL, Wadèn J, Thorn LM, Mäkinen VP, et al. The presence and severity of chronic kidney disease predicts all-cause mortality in type 1 diabetes. Diabetes (2009) 58(7):1651–8. doi: 10.2337/db08-1543
14. Sharma H, Lencioni M, Narendran P. Cardiovascular disease in type 1 diabetes. Cardiovasc Endocrinol Metab (2019) 8(1):28–34. doi: 10.1097/XCE.0000000000000167
15. Hensel KO, Grimmer F, Roskopf M, Jenke AC, Wirth S, Heusch A. Subclinical alterations of cardiac mechanics present early in the course of pediatric type 1 diabetes mellitus: a prospective blinded speckle tracking stress echocardiography study. J Diabetes Res (2016) 2016:2583747. doi: 10.1155/2016/2583747
16. Maahs DM, Dabelea D, D’Agostino RB Jr, Andrews JS, Shah AS, Crimmins N, et al. Glucose control predicts 2-year change in lipid profile in youth with type 1 diabetes. J Pediatr (2013) 162(1):101–7.e1. doi: 10.1016/j.jpeds.2012.06.006
17. Edqvist J, Rawshani A, Rawshani A, Adiels M, Franzén S, Bjorck L, et al. Trajectories in HbA1c and other risk factors among adults with type 1 diabetes by age at onset. BMJ Open Diabetes Res Care (2021) 9(1):e002187. doi: 10.1136/bmjdrc-2021-002187
18. Diabetes Control and Complications Trial Research Group. Effect of intensive diabetes treatment on developing and progressing long-term complications in adolescents with insulin-dependent diabetes mellitus: diabetes control and complications trial. J Pediatr (1994) 125(2):177–88. doi: 10.1016/s0022-3476(94)70190-3
19. Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) Study Research Group. Intensive diabetes treatment and cardiovascular outcomes in type 1 diabetes: the DCCT/EDIC study 30-year follow-up. Diabetes Care (2016) 39(5):686–93. doi: 10.2337/dc15-1990
20. Lithovius R, Harjutsalo V, Forsblom C, Saraheimo M, Groop PH. The consequences of failure to achieve targets of guidelines for prevention and treatment of diabetic complications in patients with type 1 diabetes. Acta Diabetol (2015) 52(1):31–8. doi: 10.1007/s00592-014-0595-x
21. Chiesa ST, Charakida M, McLoughlin E, Nguyen HC, Georgiopoulos G, Motran L, et al. Elevated high-density lipoprotein in adolescents with type 1 diabetes is associated with endothelial dysfunction in the presence of systemic inflammation. Eur Heart J (2019) 40(43):3559–66. doi: 10.1093/eurheartj/ehz114
22. Di Bonito P, Mozzillo E, Rosanio FM, Maltoni G, Piona CA, Franceschi R, et al. Albuminuric and non-albuminuric reduced eGFR phenotypes in youth with type 1 diabetes: factors associated with cardiometabolic risk. Nutr Metab Cardiovasc Dis (2021) 31(7):2033–41. doi: 10.1016/j.numecd.2021.03.019
Keywords: type 1 diabetes, lipids profile, kidney function, age, guidelines
Citation: Catamo E, Robino A, Dovc K, Tinti D, Tamaro G, Bonfanti R, Franceschi R, Rabbone I, Battelino T and Tornese G (2023) Screening of lipids and kidney function in children and adolescents with Type 1 Diabetes: does age matter? Front. Endocrinol. 14:1186913. doi: 10.3389/fendo.2023.1186913
Received: 15 March 2023; Accepted: 23 May 2023;
Published: 02 June 2023.
Edited by:
Stefano Zucchini, Sant’Orsola-Malpighi Polyclinic, ItalyReviewed by:
Daniel Turudic, University Hospital Center Zagreb, CroatiaTetyana Chaychenko, Kharkiv National Medical University, Ukraine
Copyright © 2023 Catamo, Robino, Dovc, Tinti, Tamaro, Bonfanti, Franceschi, Rabbone, Battelino and Tornese. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eulalia Catamo, ZXVsYWxpYS5jYXRhbW9AYnVybG8udHJpZXN0ZS5pdA==
†These authors have contributed equally to this work
 Eulalia Catamo
Eulalia Catamo Antonietta Robino
Antonietta Robino Klemen Dovc
Klemen Dovc Davide Tinti
Davide Tinti Gianluca Tamaro1
Gianluca Tamaro1 Riccardo Bonfanti
Riccardo Bonfanti Roberto Franceschi
Roberto Franceschi Ivana Rabbone
Ivana Rabbone Tadej Battelino
Tadej Battelino Gianluca Tornese
Gianluca Tornese