- National Clinical Research Center for Metabolic Diseases, Key Laboratory of Diabetes Immunology, Ministry of Education, Department of Metabolism and Endocrinology, The Second Xiangya Hospital of Central South University, Changsha, Hunan, China
Objective: This network meta-analysis (NMA) was conducted to compare and rank the effects of training interventions including aerobic exercise (AE), resistance training (RT), combined aerobic and resistance training (CT), and high-intensity interval training (HIIT) on vital metabolic indicators in adults with overweight and obesity.
Methods: PubMed, Cochrane, Embase, and Web of Science were searched from 1990 to February 2023. Articles were included if they described randomized controlled trials (RCTs) examining the effects of exercise training on anthropometry parameters, lipid profiles, glucose metabolism, blood pressure, and cardiorespiratory fitness in adults with overweight and obesity. Weighted mean difference with 95% CI was calculated.
Results: A total of 28 studies with 1,620 patients were included. Results revealed that AE exerts best effects on weight loss (−2.35 [−4.05, −0.64]) and body mass index (−0.9 [−1.38, −0.42]), while HIIT is the most effective in reducing waist circumference (−5.93 [10.71, −1.15]), percentage body fat (−3.93 [−5.73, −2.12]), serum triglycerides (−20.55 [−37.20, −3.91]), and fasting blood glucose (−14.31 [−22.47, −6.16]) and improving VO2 max (7.41 [4.37, 10.45]). However, no significant benefit was observed in terms of total cholesterol and blood pressure.
Conclusions: AE is the optimal exercise type for reducing body weight and BMI, while HIIT exerts the most beneficial effects on improving body composition, cardiorespiratory fitness, and metabolic abnormalities in adults with overweight and obesity.
Systematic review registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023444322, identifier CRD42023444322.
1 Introduction
Obesity is predicted to affect nearly 20% of people around the world and is causing a huge burden as a noncommunicable disease (1). Given the enormous personal and medical costs of overweight and obesity, it is urgent for public health policymakers to identify effective interventions.
Owing to the lack of safe and effective drugs for the treatment of obesity, the main interventions for obesity are still diet control and exercise. The main forms of exercise are aerobic exercise (AE), resistance training (RT), combined aerobic and resistance training (CT), and high-intensity interval training (HIIT) (2). According to the recommendation of guidelines of exercise for people with obesity, moderate-intensity AE for at least 300 min per week (3) was the preferred choice. However, the effects of different exercise modalities on body composition, metabolic health, and cardiovascular health in people with obesity were inconsistent. A meta-analysis reported that AE is beneficial for reducing body weight and fat mass, while RT is effective in reducing fat mass (4). Another meta-analysis showed that HIIT was slightly more effective than AE in improving VO2 max (5). Moreover, a meta-analysis of adolescents with obesity has shown that compared with AE alone, CT resulted in greater reductions in LDL levels (6).
Despite the fact that it is well known that exercise is effective in reducing body weight and fat mass and promoting cardiovascular metabolism, a potential drawback is the large weekly time consumption, which totals approximately 300 to 400 min per week. Thus, in recent years, HIIT is being increasingly recommended as an alternative option mainly because it has high efficiency and is time-saving, as lack of time is the main obstacle that prevents people from exercising (7). There is increasingly strong evidence showing that HIIT has better effects on a series of health indicators in both healthy and chronically ill people than continuous moderate-intensity training (8–10). However, in terms of the effects of exercise training on people with overweight and obesity, most studies are pairwise meta-analyses that cannot rank the effectiveness of different trainings.
Different from a conventional meta-analysis, a network meta-analysis (NMA) is a powerful tool for comparing the effectiveness of different interventions as it can combine direct and indirect evidence and allow for the ranking of treatments (11). However, the current available NMA focused only on the effects among AE, RT, and CT, without considering the HIIT. More importantly, it is unclear which type of exercise is most effective for the different metabolic abnormalities in people with overweight and obesity. Therefore, the aims of this NMA were to comprehensively evaluate and rank the effectiveness of exercise across the vital metabolic indicators including anthropometry, glucose homeostasis, lipid profile, and cardiovascular fitness in adults with overweight and obesity.
2 Materials and methods
This systematic review and NMA follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Network Meta-Analyses (PRISMA-NMA) (12) and is registered in the PROSPERO database (Registration number: CRD42023444322).
2.1 Literature search strategy
Four electronic databases (PubMed, Cochrane, Embase, and Web of Science) were searched from 1900 to February 2023. The search strategy was based on the PICOS tool: (P) Population: individuals with overweight or obesity; (I) Intervention: exercise; (C) Comparator: no exercise or other exercise modality; (O) Outcomes: body composition, lipid metabolism, glucose metabolism, blood pressure, and VO2 max; (S) Study type: randomized controlled trial (RCT). A complete list of the search terms is available in the Supplementary Materials section (Supplementary Table 1).
2.2 Inclusion and exclusion criteria
Studies were considered eligible for inclusion if the following criteria were met: (1) RCT must be published in English. (2) Participants must be adult individuals with overweight or obesity (BMI ≥25 kg/m2). (3) Studies employed an intervention of AE, RT, CT, or HIIT for at least 4 weeks. The definition of exercise interventions is shown in Supplementary Table 2. (4) Outcome of interest included anthropometry (body weight [BW], body mass index [BMI], waist circumference [WC], and percentage body fat [%BF]), lipid metabolism (triglycerides [TG], total cholesterol [TC], high-density lipoprotein [HDL], and low-density lipoprotein [LDL]), glucose metabolism (fasting blood glucose [FBG], fasting blood insulin [FINS], and homeostatic model assessment for insulin resistance [HOMA-IR]), and cardiovascular function (systolic blood pressure [SBP], diastolic blood pressure [DBP], and VO2 max).
The exclusion criteria were as follows: (1) The intervention was combined with diet control. (2) The subjects were reported to be taking medication or had other noncommunicable diseases, such as cancer, hypertension, and diabetes. (3) Articles that did not include the outcome of interest. (4) Conference abstracts, case reports, and dissertations were excluded. (5) Duplications of the searched studies.
Abstracts and full texts were screened by two authors independently, and any uncertainty was discussed among authors.
2.3 Data extraction
Data were extracted by two authors independently. The following characteristics were extracted: (1) first author; (2) publication year; (3) country; (4) sample size; (5) mean age; (6) characteristics of the participants; (7) outcome measures including BW [kg], BMI [kg/m2], WC [cm], %BF [percentage], TG [mg/dL], TC [mg/dL], LDL [mg/dL], HDL [mg/dL], FBG [mg/dL], FINS [μU/mL], HOMA-IR, SBP [mmHg], DBP [mmHg], and VO2 max [mL/kg·min]; and (8) description of the exercise intervention (type, intensity, duration, and frequency).
2.4 Assessment of study quality
We used the Cochrane Risk of Bias Tool (13) to assess the risk of bias (ROB) of the included studies independently. The following domains were considered: (1) randomization process, (2) treatment allocation concealment, (3) blinding of participants and researchers, (4) blinding of outcome assessment, (5) incomplete outcome data, (6) selective reporting, and (7) other bias.
2.5 Statistical analysis
We use weighted mean difference and 95% confidence interval (CI) to report continuous variables. Review Manager 5.3 was used for the traditional pairwise meta-analysis. Statistical heterogeneity was evaluated using the (I2) statistic: I2 > 50% was considered high heterogeneity and random-effects model was employed; otherwise, the fixed-effects model was adopted. For the NMA, Stata16.0. software package “mvmeta” and “network” was used to analyze indirect comparisons between different interventions.
The network diagram was used to present the relationship between exercise interventions. The node-splitting method and loop inconsistency test were performed to test inconsistency. p > 0.05 indicates that there is no significant inconsistency and the consistency model is chosen; otherwise, the inconsistency model is employed (14, 15).
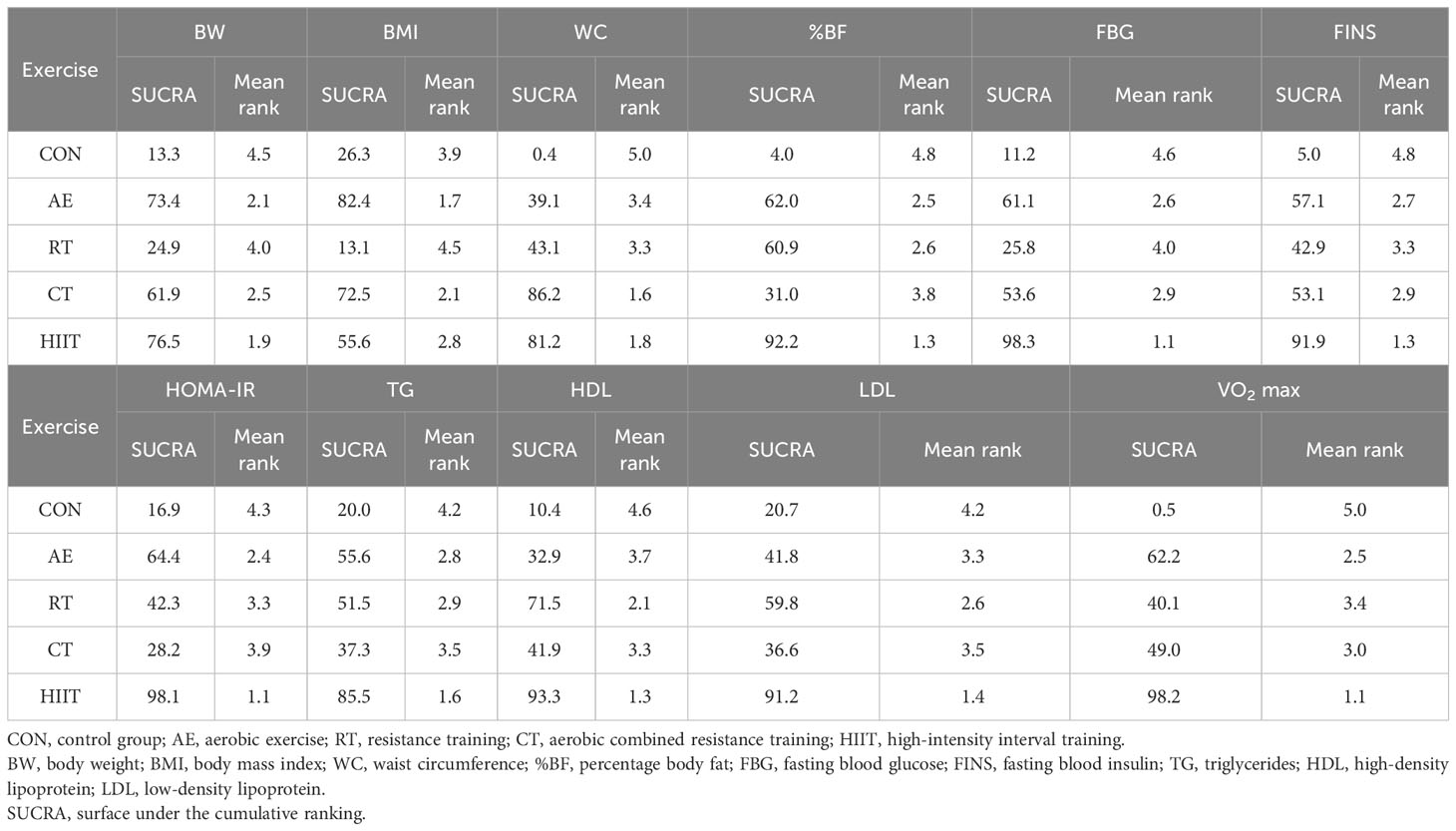
The effectiveness of different interventions was ranked by using the surface under the cumulative ranking probability diagram (SUCRA) (16). The value of SUCRA is higher, and the effects of interventions are better. League tables were used to present the pair-to-pair comparisons between the exercise interventions.
Furthermore, a comparison-adjusted funnel plot was used to assess publication bias. To explore the heterogeneity, subgroup analyses were performed in pairwise meta-analyses, including different duration of exercise (4–8 weeks as short-term duration and >9 weeks as long-term duration) and mean baseline BMI (25–30 kg/m2 as individuals with overweight and ≥30 kg/m2 as individuals with obesity).
3 Results
3.1 Literature selection
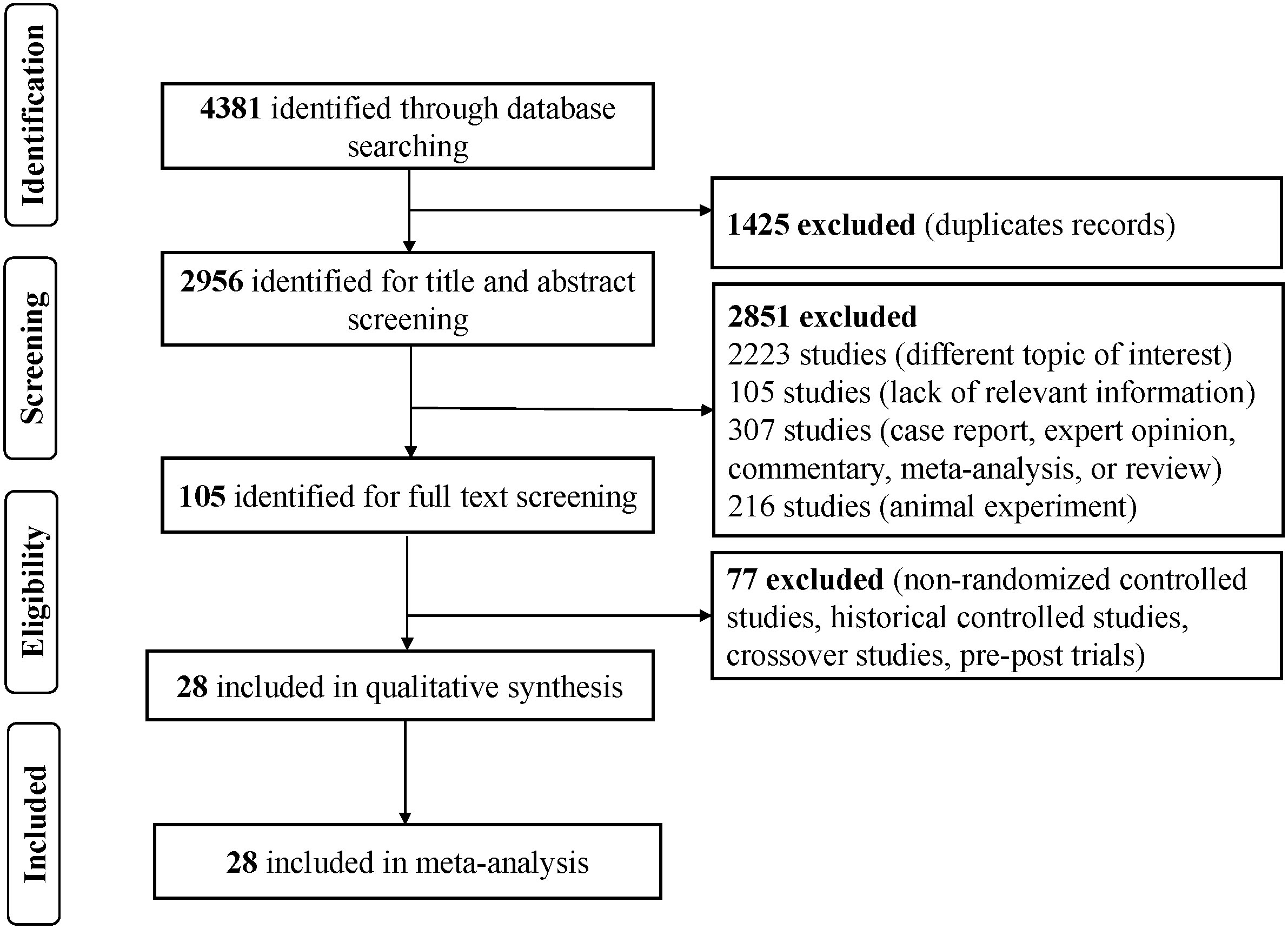
According to the search strategy, 4,381 studies were identified in those four databases. After 1,425 duplicates were removed, 2,956 articles were left to screen the titles and abstracts. After reading the full text of 105 studies, we included 28 RCTs for the NMA. The flowchart of the search and selection process is presented in Figure 1.
3.2 Characteristics of included studies
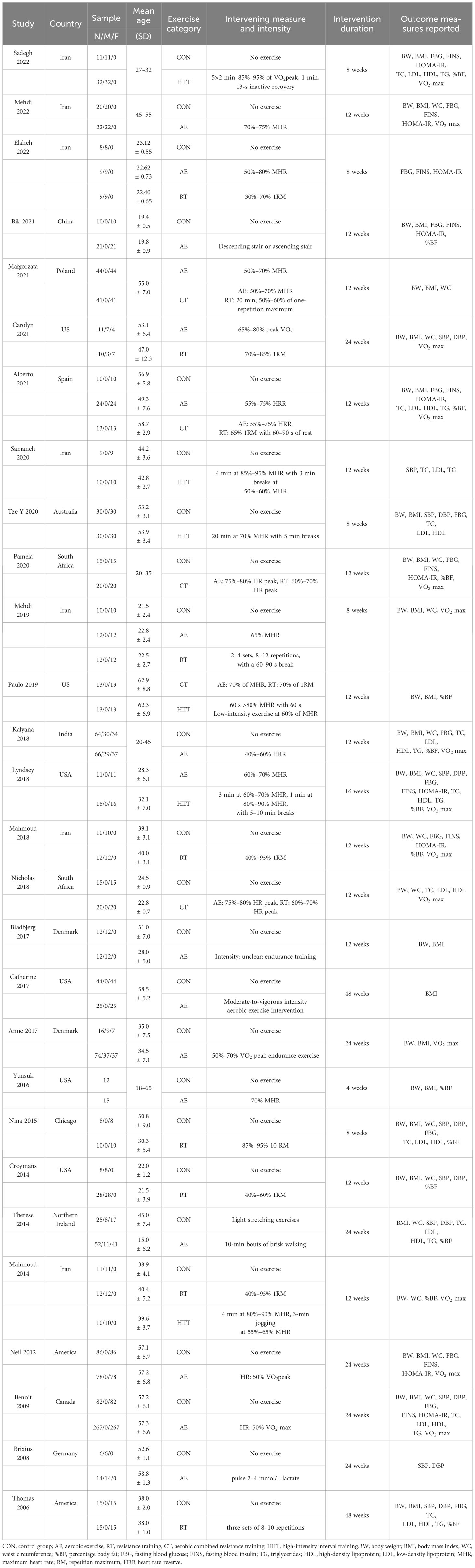
Table 1 shows the clinical and demographic characteristics of the 28 included studies (17–44). A total of 1,620 participants were enrolled in the NMA; sample size ranged from 21 to 349. As for gender, 15 studies recruited women only and 8 studies recruited men only, and 5 studies included both men and women. Of the total, 75% participants were women. With regard to exercise categories, participants were included in the AE (n = 757), RT (n = 108), CT (n = 107), and HIIT (n = 111) groups, respectively. The duration of the training ranged from 4 weeks to 48 weeks (mostly 12 weeks). The number of weekly sessions was mostly three times a week (n = 20).
3.3 Risk of bias and publication bias in the enrolled studies
The summary of the risk of bias assessment is shown in Supplementary Figure 1. In brief, 15 studies showed unclear ROB in random sequence generation, allocation concealment, and blinding of the participants and implementers. All studies showed low ROB in blinding of outcome assessment and selective reporting. Only one study showed risk of other biases. Overall, the quality of the included studies was considered moderate.
3.4 Network meta-analysis and subgroup analyses
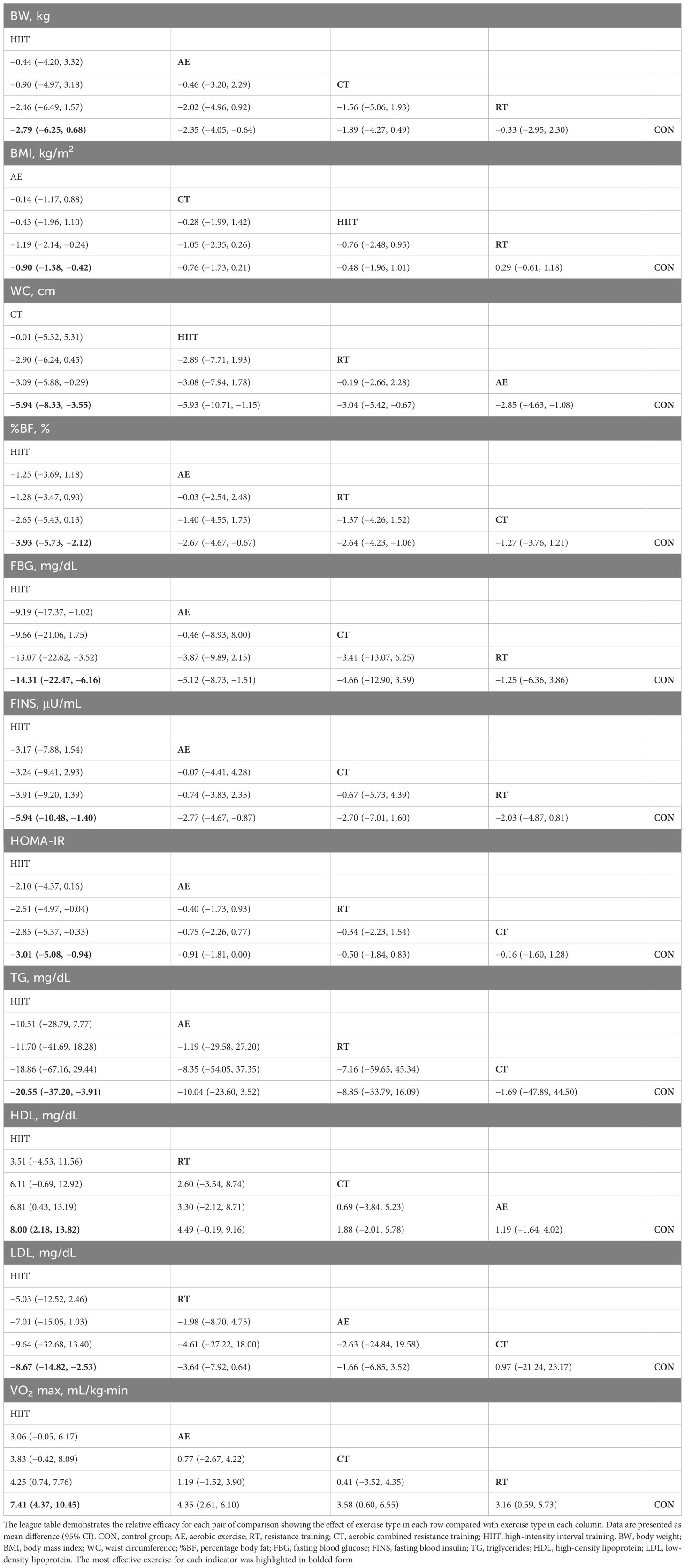
Four measures of anthropometry and body composition (BW, BMI, WC, and %BF), three measures of lipid metabolism (TG, HDL, and LDL), three measures of glucose metabolism (FBG, FINS, and HOMA-IR), and one measure of cardiovascular function (VO2 max) were included in the NMA. Table 2 illustrates the results of pair-to-pair comparisons between the exercise interventions. Figure 2 illustrates NMA maps of studies examining the efficacy of exercise modes on 11 indicators. Table 3 presents the rank of exercise interventions in order of effectiveness. The results of subgroup analyses are shown in Supplementary Table 3. The results of interval plot and cumulative ranking probability plots of NMA can be found in Supplementary Figures 2-23. The results of local inconsistency are displayed in Supplementary Figures 24-34. Funnel plot graphics are illustrated in Supplementary Figures 35-45.
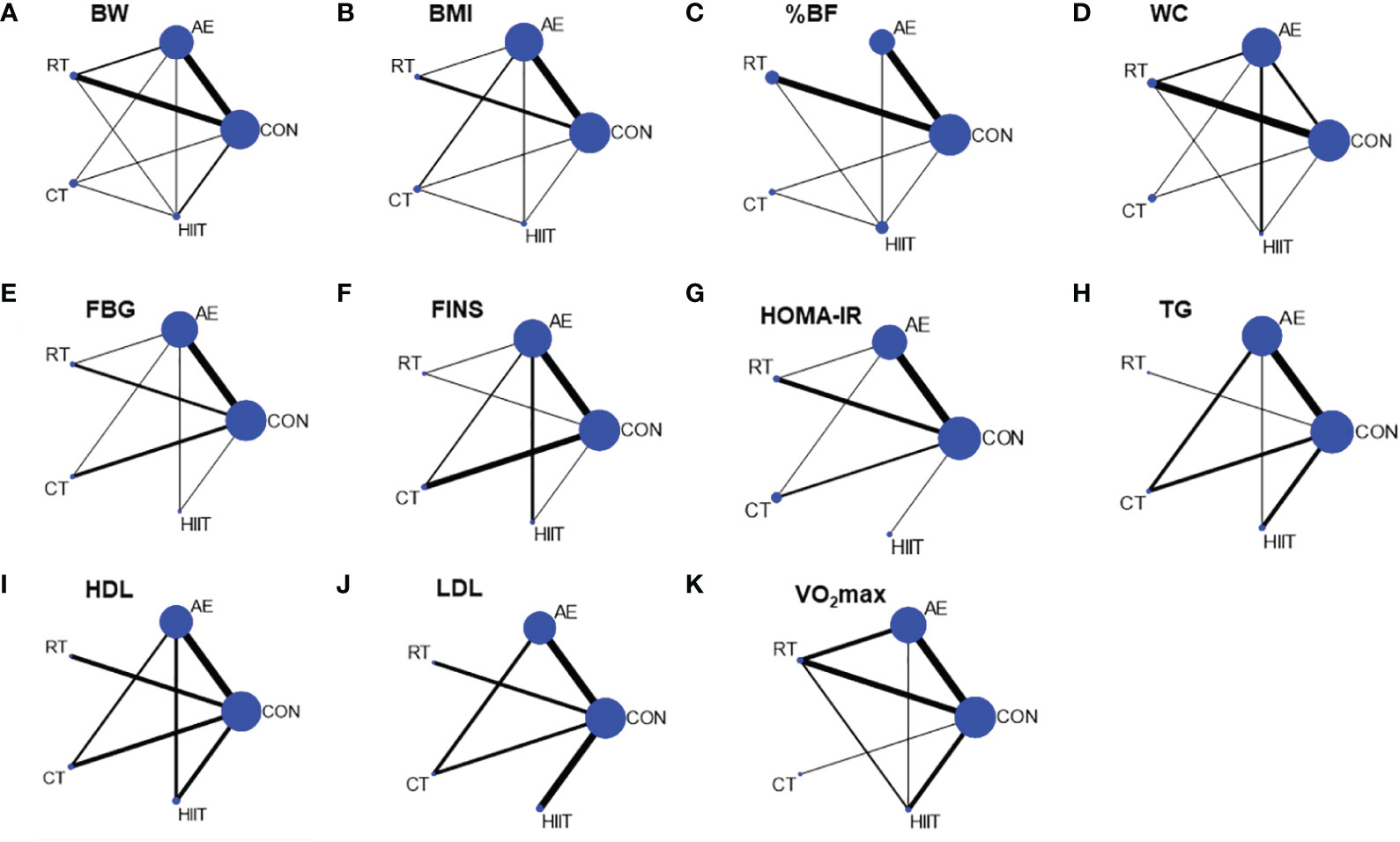
Figure 2 Network diagram of network meta-analysis comparisons. (A) BW, body weight, (B) BMI, body mass index, (C) %BF, percentage body fat, (D) WC, waist circumference, (E) FBG, fasting blood glucose, (F) FINS, fasting blood insulin, (G) HOMA-IR, (H) TG, triglycerides, (I) HDL, high-density lipoprotein, (J) LDL, low-density lipoprotein, (K) VO2 max. CON, control group; AE, aerobic exercise; RT, resistance training; CT, aerobic combined resistance training; HIIT, high-intensity interval training. The size of the nodes represents the number of participants in an intervention, and the thickness of lines between interventions represents the number of studies that compare them.
3.4.1 Anthropometric and body composition
A total of 22 studies assessed BW and 19 studies assessed BMI. The results of NMA showed that only the AE groups had shown a significantly reduced body weight (−2.35 [−4.05, −0.64]) and BMI (−0.9 [−1.38, −0.42]) compared with control. Moreover, 11 studies assessed WC. The CT (−5.94 [−8.33, −3.55]), HIIT (−5.93 [−10.71, −1.15]), RT (−3.04 [−5.42, −0.67]), and AE (−2.85 [−4.63, −1.08]) demonstrated significantly meaningful reductions in WC compared to the control group (Table 2). CT was the best option for WC reduction (SUCRA = 86.2). The %BF was assessed in 12 studies. HIIT (−3.93 [−5.73, −2.12]), AE (−2.67 [−4.67, −0.67]), and RT (−2.64 [−4.23, −1.06]) resulted in greater changes in %BF than control. HIIT was regarded as the best exercise training for reducing %BF (SUCRA = 92.2) (Table 3). Subgroup analysis showed that short-term exercise could only reduce the %BF (−4.59 [−8.42, −0.76]) while long-term duration of exercise could efficiently reduce body weight, BMI, waist circumference, and %BF. In addition, all exercise could improve anthropometric outcomes for individuals with overweight and obesity (Supplementary Table 3).
3.4.2 Glucose metabolism
The FBG, FINS, and HOMA-IR were reported in 15, 15, and 11 studies. AE (−5.12 [−8.73, −1.51]) and HIIT (−14.31 [−22.47, −6.16]) displayed improvements in FBG relative to control. AE (−2.77 [−4.67, −0.87]) and HIIT (−5.94 [−10.48, −1.40]) resulted in greater reductions in FINS relative to control. Regarding HOMA-IR, only the HIIT (−3.01 [−5.08, −0.94]) showed a marked reduction for HOMA-IR compared with control (Table 2). According to the SUCRA score, HIIT is probably the best for reducing fasting glucose levels (SUCRA = 98.3), fasting insulin levels (SUCRA = 91.9), and HOMA-IR (SUCRA = 98.1) compared with other exercise types (Table 3). The subgroup analysis showed that short-term exercise could just reduce insulin levels (−2.19 [−3.12, −1.26]) while long-term exercise could improve insulin resistance by reducing both insulin levels (−2.53 [−4.34, −0.73]) and HOMA-IR (−0.77 [−1.42, −0.12]) (Supplementary Table 3).
3.4.3 Lipid profile
The TC, LDL, HDL, and TG were included in 10, 10, 11, and 8 studies, respectively. Overall, only HIIT elicited meaningful alterations in TC (−16.29 [−30.62, −1.97]), LDL (−8.67 [−14.82, −2.53]), HDL (8.00 [2.18, 13.82]), and TG (−20.55 ([−7.20, −3.91]) and HIIT was the most favorable intervention for improving lipid metabolism (Tables 2, 3). Subgroup analysis showed that short-term exercise had already changed the lipid profiles by reducing TG and LDL levels and increasing HDL levels. The improvement of lipid metabolism was observed in individuals with overweight but not in individuals with obesity (Supplementary Table 3).
3.4.4 Cardiovascular function
SBP, DBP, and VO2 max were reported in 8, 9, and 13 studies. No meaningful reductions in SBP and DBP were observed in the network comparison. Regarding VO2 max, AE (4.35 [2.61, 6.10]), RT (3.16 [0.59, 5.73]), CT (3.58 [0.60, 6.55]), and HIIT (7.41 [4.37, 10.45]) were the exercise modes increasing VO2 max (Table 2). HIIT (SUCRA = 98.2) ranked the highest (Table 3). The results of subgroup analysis showed that short-term exercise has begun to increase VO2 max (7.87 [4.92, 10.82]). Both individuals with overweight (6.25 [4.12, 8.37]) and obesity (3.24 [1.89, 4.59]) could gain benefits in increasing VO2 max. However, we did not observe any difference in blood pressure in subgroup analysis (Supplementary Table 3).
4 Discussion
This NMA comprehensively analyzed the current studies about exercise interventions for people with overweight and obesity. Our main findings indicate that AE is probably the best choice for reducing body weight and BMI, while HIIT may be the optimum strategy to improve glucose homeostasis, lipid metabolism, and cardiorespiratory fitness.
4.1 Anthropometric and body composition
BW and BMI are often the main endpoints in evaluating obesity. BMI could effectively predict overall mortality but limit the alterations in body composition (45, 46). Therefore, %BF may be considered as a more significant indicator for reflecting the changes in body composition (47). Waist circumference represents the level of visceral fat, which is independently related to all-cause mortality and is considered as a better outcome for predicting the conditions of obesity (48, 49). Our study showed that AE is probably the best in controlling BW and BMI, whereas HIIT could be the optimal exercise intervention for reducing WC and %BF in individuals with overweight and obesity. A recent NMA has shown that CT is the best intervention for reducing WC and %BF with a small reduction in weight loss, but this study did not assess the benefits of HIIT in people with obesity (50). A systematic review comparing HIIT with continuous moderate-intensity training on body composition in adults with overweight and obesity has found that HIIT has similar effects on %BF reduction, but requires ~40% less time commitment (51). Another meta-analysis has reported that HIIT provided nearly 30% more reductions in fat mass than continuous moderate-intensity training (52). The subgroup analysis has found that more than 9 weeks of exercise could effectively improve anthropometric outcomes, and individuals with overweight and obesity could obtain benefits from exercise. In general, our results demonstrated that compared with other types of exercise, AE and HIIT were superior in improving body composition.
4.2 Glucose metabolism
Individuals with overweight or obesity are often associated with poor glycemic control, which increase their risk of developing diabetes (53). Our study has shown that HIIT could be the most effective exercise mode in reducing fasting blood glucose, insulin, and HOMA-IR and exercise is more effective in people with obesity (BMI > 30). This may be because overweight participants had relatively healthy glucose metabolism than people with obesity. Additionally, although previous meta-analysis did not consider the effects of duration of exercise on glucose metabolism, our subgroup analysis has found that 4 to 8 weeks of exercise could lower fasting insulin level.
4.3 Lipid profile
Guidelines from the American College of Sports Medicine (ACSM) have recommended that more than 150 min of moderate-intensity exercise per week can effectively reduce blood lipid levels (3). The results of NMA showed that HIIT is the most effective mode in improving TG, LDL, and HDL levels. Previous studies have suggested that exercise could improve the TG and HDL levels, but seldom alter TC levels (54), which is consistent with our results. Additionally, a previous meta-analysis demonstrated that HIIT could improve the blood lipid metabolism for type 2 diabetes mellitus (55). Although patients with overweight and obesity included in our study had no complications of dyslipidemia, the results have shown that HIIT moderately reduced lipid levels within the normal range, which was beneficial for reducing the risk of cardiovascular disease. Subgroup analysis found that TG, LDL, and HDL levels were improved in short-term exercise, indicating that exercise could improve lipid metabolism before obvious body weight reduction. However, the reductions in TG and LDL levels were only observed in individuals with overweight, indicating that exercise alone has a limited effect on improving lipid metabolism in people with obesity.
4.4 Cardiovascular function
Blood pressure is a commonly assessed measure related to cardiovascular health (56). Many studies have shown that exercise can lower diastolic and systolic blood pressure in people with hypertension (57). For patients with overweight and obesity, we did not find significant changes in blood pressure in both pairwise meta-analysis and subgroup analysis. This may because the baseline of blood pressure in included participants is normal.
Cardiorespiratory fitness (CRF) has long been disregarded as an important moderator of the negative association between mortality and obesity (58). Although increasing studies demonstrated that CRF has a greater impact on morbidity and mortality than body fat percentage (59), most meta-analyses have continued to focus on anthropometric measurements more than CRF when evaluating the effects of exercise for patients with obesity, but have not included CRF in their analyses. Our study has found that all types of exercise can significantly improve CRF, of which HIIT has the highest probability of elevating CRF, followed by AE. One previous meta-analysis has reported that compared with moderate-intensity continuous training, HIIT leads to greater improvement in CRF in children (60). Moreover, another meta-analysis demonstrated that HIIT significantly increases CRF more than continuous moderate-intensity training in patients with chronic diseases (10). Our subgroup analysis found that short-term exercise is enough to increase the VO2 max and the benefits existed in both individuals with overweight and obesity. Overall, HIIT may be the preferred option for improving CRF in patients with overweight and obesity.
Previous studies have mainly focused on the effectiveness of HIIT on CRF; beyond that, our research has found that HIIT is also the optimal choice for improving body composition and glucose and lipid metabolism compared with other exercise modalities. Although HIIT has favorable overall improvements, it may not be suitable for people without training foundation. Considering AE is the best for reducing body weight and BMI, it is necessary to take into account the patient’s physical fitness and personal preferences when health professionals advise on exercise training to improve obesity.
5 Strengths and limitations
There are some strengths in this study. First, the included indicators are comprehensive and can represent the systemic metabolic status of patients effectively. Additionally, we used NMA to evaluate and rank the efficacy of interventions by combining direct and indirect evidence obtained from RCTs. Moreover, we performed subgroup analysis using the mean baseline BMI to explore the different efficacy of exercise on people with overweight and obesity and the duration of exercise to explore how long it takes to get metabolic benefits. However, there are several limitations to our study. First, most of the included RCT had high risks in the blinding of participants, which is unlikely to carry out in this kind of intervention, but because the outcomes were all measured objectively, this ROB does not seem to influence the objective outcomes. Second, owing to the limited number of included studies, we did not consider the sequence and intensity of exercise. Third, because of the limited direct comparisons for some interventions, the results should be interpreted cautiously. Fourth, of all patients included, 75% were women. Owing to the limited number of included studies, it is difficult to conduct subgroup analysis of gender, and considering the imbalance of sex ratios, this result may be more suitable for female patients. Fifth, although the majority (46%) of included patients used AE, there was no significant inconsistency in the effects of different exercises, indicating that the difference in number of people did not significantly affect our conclusions.
6 Conclusion
In summary, our study has demonstrated that different types of exercise have varying efficacy for different metabolic abnormalities. AE produces the best results in reducing BW and BMI, whereas HIIT is most likely the best exercise intervention for improving body composition and systemic metabolic status in adults with overweight and obesity. The findings display a deeper insight into the exercise prescription for individuals with overweight and obesity in the real world.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
HW: Data curation, Methodology, Software, Writing – original draft. RC: Data curation, Writing – review & editing. LX: Data curation, Writing – review & editing. FH: Conceptualization, Funding acquisition, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by grants from National Key R&D Program, China (2020YFA0803604; 2022YFA0806102), National Natural Science Foundation of China (91957113; 31871180) to FH.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2023.1294362/full#supplementary-material
References
1. Bodirsky BL, Dietrich JP, Martinelli E, Stenstad A, Pradhan P, Gabrysch S, et al. The ongoing nutrition transition thwarts long-term targets for food security, public health and environmental protection. Sci Rep (2020) 10(1):19778. doi: 10.1038/s41598-020-75213-3
2. Wang S, Zhou H, Zhao C, He H. Effect of exercise training on body composition and inflammatory cytokine levels in overweight and obese individuals: A systematic review and network meta-analysis. Front Immunol (2022) 13:921085. doi: 10.3389/fimmu.2022.921085
3. Liguori G FY, Fountaine C, Roy BA. ACSM's Guidelines for exercise testing and prescription, 11th edition (United States: LWW). (2021).
4. Hsu KJ, Liao CD, Tsai MW, Chen CN. Effects of exercise and nutritional intervention on body composition, metabolic health, and physical performance in adults with sarcopenic obesity: A meta-analysis. Nutrients. (2019) 11(9):2163. doi: 10.3390/nu11092163
5. van Baak MA, Pramono A, Battista F, Beaulieu K, Blundell JE, Busetto L, et al. Effect of different types of regular exercise on physical fitness in adults with overweight or obesity: Systematic review and meta-analyses. Obes Rev (2021) 22 Suppl 4(Suppl 4):e13239. doi: 10.1111/obr.13239
6. Garcia-Hermoso A, Ramirez-Velez R, Ramirez-Campillo R, Peterson MD, Martinez-Vizcaino V. Concurrent aerobic plus resistance exercise versus aerobic exercise alone to improve health outcomes in paediatric obesity: a systematic review and meta-analysis. Br J Sports Med (2018) 52(3):161–6. doi: 10.1136/bjsports-2016-096605
7. Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults' participation in physical activity: review and update. Med Sci Sports Exerc (2002) 34(12):1996–2001. doi: 10.1097/00005768-200212000-00020
8. Milanovic Z, Sporis G, Weston M. Effectiveness of high-intensity interval training (HIT) and continuous endurance training for VO2max improvements: A systematic review and meta-analysis of controlled trials. Sports Med (2015) 45(10):1469–81. doi: 10.1007/s40279-015-0365-0
9. Liou K, Ho S, Fildes J, Ooi SY. High intensity interval versus moderate intensity continuous training in patients with coronary artery disease: A meta-analysis of physiological and clinical parameters. Heart Lung Circ (2016) 25(2):166–74. doi: 10.1016/j.hlc.2015.06.828
10. Weston KS, Wisloff U, Coombes JS. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. Br J Sports Med (2014) 48(16):1227–34. doi: 10.1136/bjsports-2013-092576
11. Rouse B, Chaimani A, Li T. Network meta-analysis: an introduction for clinicians. Intern Emerg Med (2017) 12(1):103–11. doi: 10.1007/s11739-016-1583-7
12. Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med (2015) 162(11):777–84. doi: 10.7326/M14-2385
13. Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ (2011) 343:d5928. doi: 10.1136/bmj.d5928
14. Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G. Graphical tools for network meta-analysis in STATA. PloS One (2013) 8(10):e76654. doi: 10.1371/journal.pone.0076654
15. Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med (2010) 29(7-8):932–44. doi: 10.1002/sim.3767
16. Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol (2011) 64(2):163–71. doi: 10.1016/j.jclinepi.2010.03.016
17. Abbasian S, Ravasi AA, Soori R, Aydin S, Choobineh S, Aydin S. High-intensity interval training ameliorates endothelial dysfunction through adropin, nitric oxide, MR-proADM, and copeptin changes in overweight subjects. Hormones (Athens) (2022) 21(4):707–17. doi: 10.1007/s42000-022-00402-w
18. Akhavan Rasoolzadeh E, Nazarali P, Alizadeh R. Effect of endurance and resistance training on adropin and insulin resistance among overweight men: A randomized clinical trial. Physiol Pharmacol (2021) 26:239–47. doi: 10.52547/phypha.26.3.5
19. Arsenault BJ, Cote M, Cartier A, Lemieux I, Despres JP, Ross R, et al. Effect of exercise training on cardiometabolic risk markers among sedentary, but metabolically healthy overweight or obese post-menopausal women with elevated blood pressure. Atherosclerosis. (2009) 207(2):530–3. doi: 10.1016/j.atherosclerosis.2009.05.009
20. Bairapareddy KC, Maiya AG, Kumar P, Nayak K, Guddattu V, Nayak V. Effect of aerobic exercise on echocardiographic epicardial adipose tissue thickness in overweight individuals. Diabetes Metab Syndr Obes (2018) 11:303–12. doi: 10.2147/DMSO.S145862
21. Bladbjerg EM, Skov J, Nordby P, Stallknecht B. Endurance exercise per se reduces the cardiovascular risk marker t-PA antigen in healthy, younger, overweight men. Thromb Res (2017) 152:69–73. doi: 10.1016/j.thromres.2017.02.022
22. Brixius K, Schoenberger S, Ladage D, Knigge H, Falkowski G, Hellmich M, et al. Long-term endurance exercise decreases antiangiogenic endostatin signalling in overweight men aged 50-60 years. Br J Sports Med (2008) 42(2):126–9;discussion 9. doi: 10.1136/bjsm.2007.035188
23. Chow BC, Li S, Zhu X, Jiao J, Quach B, Baker JS, et al. Effects of descending or ascending stair exercise on body composition, insulin sensitivity, and inflammatory markers in young Chinese women with obesity: A randomized controlled trial. J Sports Sci (2021) 39(5):496–502. doi: 10.1080/02640414.2020.1829362
24. Croymans DM, Krell SL, Oh CS, Katiraie M, Lam CY, Harris RA, et al. Effects of resistance training on central blood pressure in obese young men. J Hum Hypertens (2014) 28(3):157–64. doi: 10.1038/jhh.2013.81
25. Duggan C, Tapsoba JD, Wang CY, Schubert KEF, McTiernan A. Long-term effects of weight loss and exercise on biomarkers associated with angiogenesis. Cancer Epidemiol Biomarkers Prev (2017) 26(12):1788–94. doi: 10.1158/1055-9965.EPI-17-0356
26. Farahati S, Hosseini SRA, Moazzami M, Daloee MH, Daloee SH. The impact of high-intensity interval training versus moderate-intensity continuous training on carotid intima-media thickness and ankle-brachial index in middle-aged women. Int J Prev Med (2020) 11:62. doi: 10.4103/ijpvm.IJPVM_524_18
27. Franklin NC, Robinson AT, Bian JT, Ali MM, Norkeviciute E, McGinty P, et al. Circuit resistance training attenuates acute exertion-induced reductions in arterial function but not inflammation in obese women. Metab Syndr Relat Disord (2015) 13(5):227–34. doi: 10.1089/met.2014.0135
28. Gram AS, Bladbjerg EM, Quist JS, Petersen MB, Rosenkilde M, Stallknecht B. Anti-inflammatory effects of active commuting and leisure time exercise in overweight and obese women and men: A randomized controlled trial. Atherosclerosis. (2017) 265:318–24. doi: 10.1016/j.atherosclerosis.2017.06.923
29. Ho TY, Redmayne GP, Tran A, Liu D, Butlin M, Avolio A, et al. The effect of interval sprinting exercise on vascular function and aerobic fitness of post-menopausal women. Scandinavian J Med Sci Sports (2019) 30(2):312–21. doi: 10.1111/sms.13574
30. Hornbuckle LM, McKenzie MJ, Whitt-Glover MC. Effects of high-intensity interval training on cardiometabolic risk in overweight and obese African-American women: a pilot study. Ethn Health (2018) 23(7):752–66. doi: 10.1080/13557858.2017.1294661
31. Jamka M, Bogdanski P, Krzyzanowska-Jankowska P, Miskiewicz-Chotnicka A, Karolkiewicz J, Dus-Zuchowska M, et al. Endurance training depletes antioxidant system but does not affect endothelial functions in women with abdominal obesity: A randomized trial with a comparison to endurance-strength training. J Clin Med (2021) 10(8):1639. doi: 10.3390/jcm10081639
32. Johannsen NM, Swift DL, Johnson WD, Dixit VD, Earnest CP, Blair SN, et al. Effect of different doses of aerobic exercise on total white blood cell (WBC) and WBC subfraction number in postmenopausal women: results from DREW. PloS One (2012) 7(2):e31319. doi: 10.1371/journal.pone.0031319
33. Kargarfard M, Nobari H, Kamyar K, Zadeh AK, Oliveira R. Effects of 12-week moderate aerobic exercise on ROCK2 activity, hs-CRP and glycemic index in obese patients with impaired glucose tolerance. Physiol Behavior (2022) 257:113976. doi: 10.1016/j.physbeh.2022.113976
34. Kearney TM, Murphy MH, Davison GW, O'Kane MJ, Gallagher AM. Accumulated brisk walking reduces arterial stiffness in overweight adults: evidence from a randomized control trial. J Am Soc Hypertens (2014) 8(2):117–26. doi: 10.1016/j.jash.2013.10.001
35. Koh Y, Park KS. Responses of inflammatory cytokines following moderate intensity walking exercise in overweight or obese individuals. J Exerc Rehabil (2017) 13(4):472–6. doi: 10.12965/jer.1735066.533
36. Lekavich CL, Allen JD, Bensimhon DR, Bateman LA, Slentz CA, Samsa GP, et al. Aerobic versus resistance training effects on ventricular-arterial coupling and vascular function in the STRRIDE-AT/RT trial. Front Cardiovasc Med (2021) 8:638929. doi: 10.3389/fcvm.2021.638929
37. Mogharnasi M, TaheriChadorneshin H, Abbasi-Deloei N. Effect of exercise training type on plasma levels of vaspin, nesfatin-1, and high-sensitivity C-reactive protein in overweight and obese women. Obes Med (2019) 13:34–8. doi: 10.1016/j.obmed.2018.12.006
38. Nikseresht M. Comparison of serum cytokine levels in men who are obese or men who are lean: effects of nonlinear periodized resistance training and obesity. J Strength Cond Res (2018) 32(6):1787–95. doi: 10.1519/JSC.0000000000002039
39. Nikseresht M, Sadeghifard N, Agha-Alinejad H, Ebrahim K. Inflammatory markers and adipocytokine responses to exercise training and detraining in men who are obese. J Strength Cond Res (2014) 28(12):3399–410. doi: 10.1519/JSC.0000000000000553
40. Nono Nankam PA, Mendham AE, De Smidt MF, Keswell D, Olsson T, Bluher M, et al. Changes in systemic and subcutaneous adipose tissue inflammation and oxidative stress in response to exercise training in obese black African women. J Physiol (2020) 598(3):503–15. doi: 10.1113/JP278669
41. Nunes PRP, Martins FM, Souza AP, Carneiro MAS, Orsatti CL, Michelin MA, et al. Effect of high-intensity interval training on body composition and inflammatory markers in obese postmenopausal women: a randomized controlled trial. Menopause. (2019) 26(3):256–64. doi: 10.1097/GME.0000000000001207
42. Olson TP, Dengel DR, Leon AS, Schmitz KH. Moderate resistance training and vascular health in overweight women. Med Sci Sports Exerc (2006) 38(9):1558–64. doi: 10.1249/01.mss.0000227540.58916.0e
43. Perez-Lopez A, Gonzalo-Encabo P, Perez-Kohler B, Garcia-Honduvilla N, Valades D. Circulating myokines IL-6, IL-15 and FGF21 response to training is altered by exercise type but not by menopause in women with obesity. Eur J Sport Sci (2022) 22(9):1426–35. doi: 10.1080/17461391.2021.1939430
44. Woudberg NJ, Mendham AE, Katz AA, Goedecke JH, Lecour S. Exercise intervention alters HDL subclass distribution and function in obese women. Lipids Health Dis (2018) 17(1):232. doi: 10.1186/s12944-018-0879-1
45. Haidar YM, Cosman BC. Obesity epidemiology. Clin Colon Rectal Surg (2011) 24(4):205–10. doi: 10.1055/s-0031-1295684
46. Prospective Studies C, Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. (2009) 373(9669):1083–96. doi: 10.1016/S0140-6736(09)60318-4
47. Millstein RA. Measuring outcomes in adult weight loss studies that include diet and physical activity: a systematic review. J Nutr Metab (2014) 2014:421423. doi: 10.1155/2014/421423
48. Cerhan JR, Moore SC, Jacobs EJ, Kitahara CM, Rosenberg PS, Adami HO, et al. A pooled analysis of waist circumference and mortality in 650,000 adults. Mayo Clin Proc (2014) 89(3):335–45. doi: 10.1016/j.mayocp.2013.11.011
49. Staiano AE, Reeder BA, Elliott S, Joffres MR, Pahwa P, Kirkland SA, et al. Body mass index versus waist circumference as predictors of mortality in Canadian adults. Int J Obes (Lond) (2012) 36(11):1450–4. doi: 10.1038/ijo.2011.268
50. O'Donoghue G, Blake C, Cunningham C, Lennon O, Perrotta C. What exercise prescription is optimal to improve body composition and cardiorespiratory fitness in adults living with obesity? A network meta-analysis. Obes Rev (2021) 22(2):e13137. doi: 10.1111/obr.13137
51. Wewege M, van den Berg R, Ward RE, Keech A. The effects of high-intensity interval training vs. moderate-intensity continuous training on body composition in overweight and obese adults: a systematic review and meta-analysis. Obes Rev (2017) 18(6):635–46. doi: 10.1111/obr.12532
52. Viana RB, Naves JPA, Coswig VS, de Lira CAB, Steele J, Fisher JP, et al. Is interval training the magic bullet for fat loss? A systematic review and meta-analysis comparing moderate-intensity continuous training with high-intensity interval training (HIIT). Br J Sports Med (2019) 53(10):655–64. doi: 10.1136/bjsports-2018-099928
53. Bays HE, Gonzalez-Campoy JM, Bray GA, Kitabchi AE, Bergman DA, Schorr AB, et al. Pathogenic potential of adipose tissue and metabolic consequences of adipocyte hypertrophy and increased visceral adiposity. Expert Rev Cardiovasc Ther (2008) 6(3):343–68. doi: 10.1586/14779072.6.3.343
54. Durstine JL, Grandjean PW, Davis PG, Ferguson MA, Alderson NL, DuBose KD. Blood lipid and lipoprotein adaptations to exercise: a quantitative analysis. Sports Med (2001) 31(15):1033–62. doi: 10.2165/00007256-200131150-00002
55. Peng Y, Ou Y, Wang K, Wang Z, Zheng X. The effect of low volume high-intensity interval training on metabolic and cardiorespiratory outcomes in patients with type 2 diabetes mellitus: A systematic review and meta-analysis. Front Endocrinol (Lausanne) (2022) 13:1098325. doi: 10.3389/fendo.2022.1098325
56. Kikuya M, Ohkubo T, Asayama K, Metoki H, Obara T, Saito S, et al. Ambulatory blood pressure and 10-year risk of cardiovascular and noncardiovascular mortality: the Ohasama study. Hypertension. (2005) 45(2):240–5. doi: 10.1161/01.HYP.0000152079.04553.2c
57. Saco-Ledo G, Valenzuela PL, Ruiz-Hurtado G, Ruilope LM, Lucia A. Exercise reduces ambulatory blood pressure in patients with hypertension: A systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc (2020) 9(24):e018487. doi: 10.1161/JAHA.120.018487
58. Carbone S, Del Buono MG, Ozemek C, Lavie CJ. Obesity, risk of diabetes and role of physical activity, exercise training and cardiorespiratory fitness. Prog Cardiovasc Dis (2019) 62(4):327–33. doi: 10.1016/j.pcad.2019.08.004
59. McAuley PA, Blaha MJ, Keteyian SJ, Brawner CA, Al Rifai M, Dardari ZA, et al. Fitness, fatness, and mortality: the FIT (Henry ford exercise testing) project. Am J Med (2016) 129(9):960–5 e1. doi: 10.1016/j.amjmed.2016.04.007
Keywords: exercise training, obesity, metabolism, network meta-analysis, HIIT
Citation: Wang H, Cheng R, Xie L and Hu F (2024) Comparative efficacy of exercise training modes on systemic metabolic health in adults with overweight and obesity: a network meta-analysis of randomized controlled trials. Front. Endocrinol. 14:1294362. doi: 10.3389/fendo.2023.1294362
Received: 14 September 2023; Accepted: 20 December 2023;
Published: 16 January 2024.
Edited by:
Liwei Xie, Guangdong Academy of Science, ChinaReviewed by:
Fang Zhang, Shanghai General Hospital, ChinaYingjie Wu, Shandong Provincial Hospital, China
Copyright © 2024 Wang, Cheng, Xie and Hu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fang Hu, aHVfZmFuZzk4QGNzdS5lZHUuY24=
 Huiying Wang
Huiying Wang Fang Hu
Fang Hu