- 1Wuxi Medical College of Jiangnan University, Wuxi, China
- 2Department of Nursing, Wuxi Maternity and Child Health Care Hospital, Wuxi, China
- 3Department of Microsurgery, University of South China, Hengyang, China
Background: Obesity and psychological factors were identified as risk factors for female infertility. The study investigated the correlation between WWI, depression, and secondary infertility, focusing on the potential mediating role of depression.
Methods: According to the data from NHANES, this cross-sectional study used multiple regression analysis, subgroup analysis, and smooth curve fitting to explore the relationship between WWI, depression, and secondary infertility. The diagnostic ability of WWI was evaluated and compared to other obesity indicators using the ROC curve. The mediating effect test adopted the distribution of the product.
Results: This study involved 2778 participants, including 381 (13.7%) women with secondary infertility. Results showed that higher WWI (OR = 1.31; 95% CI, 1.11-1.56) and depression scores (OR = 1.03; 95% CI, 1.01-1.06) were associated with secondary infertility. There was a positive correlation between WWI and secondary infertility (nonlinear p = 0.8272) and this association was still consistent in subgroups (all P for interaction> 0.05). Compared with other obesity indicators, WWI (AUC = 0.588) also shows good predictive performance for secondary infertility. Mediation analysis showed that depression mediated the relationship between 3.94% of WWI and secondary infertility, with a confidence interval of Za * Zb excluding 0.
Conclusion: WWI exhibited a relatively good correlation in predicting secondary infertility than other obesity indicators, and depression may be a mediator between WWI and secondary infertility. Focusing on the potential mediating role of depression, the risk of secondary infertility due to obesity may be beneficially reduced in women.
Introduction
Secondary infertility refers to a woman who has previously been pregnant and has had regular sexual activity without contraception, but has not been pregnant for 12 consecutive months (1). Infertility troubles thousands of women of childbearing age, and according to statistics, the incidence of infertility ranges from 3% to 30% (2, 3). A multicenter study in China shows that 24.58% of women have infertility, and the incidence of secondary infertility is 18.04% (4). The factors that cause female infertility include reproductive system-related diseases, abnormal immune function, and social and physiological psychological factors (5, 6). More and more evidence also emphasizes the impact of lifestyle on infertility (7). A comprehensive understanding of easily modifiable risk factors, such as obesity and depression, is crucial for preventing and controlling secondary infertility in women.
Obese women exhibit a significantly increased risk of anovulatory infertility (8). Especially central obesity and visceral fat can lead to “hyperinsulinemia”. “Insulin resistance” directly affects the ovaries, reducing the production of liver sex hormone binding globulin, leading to hyperandrogenism (9, 10). These changes all disrupt the hypothalamic-pituitary gonadal axis, decreasing fertility (11). Currently, most studies use body mass index (BMI) and a body shape index (ABSI) to evaluate overall and abdominal fat content (12, 13). In contrast, the weight-adjusted-waist index (WWI) is more sensitive in assessing central obesity and predicting female infertility (14). The WWI is an anthropometric measure of central obesity, defined as WC divided by the square of body weight. It can reflect the composition of fat and muscle mass, even in different BMI categories (15). Studies have shown that WWI levels were positively linked to an increased risk of infertility in American females and showed a stronger association than other markers of obesity (14). Although WWI as a central obesity indicator can effectively predict infertility (16), the relationship between WWI and secondary infertility in women has not been studied before.
At present, studies have also shown a positive correlation between WWI and depressive symptoms, and this association is stronger than BMI and waist circumference (17). Depression plays an crucial mediating role in many diseases, including inflammatory bowel disease and breast cancer (18, 19). However, there are few reports on the psychological mechanisms between WWI and secondary infertility. There is a bidirectional connection between depression and infertility; that is, depression is a risk factor for infertility and a common psychological symptom in infertile women (20, 21). Compared to women with primary infertility, women with secondary infertility have a higher probability of psychological distress (22). Women with depression are less likely to use healthcare to treat infertility (23). Over time, changes in endocrine hormones and emotional disorders may affect the growth of the endometrium making it difficult to effectively address secondary infertility (24, 25). Given the relationship between WWI, depression, and infertility, depression may play a role in the association between WWI and secondary infertility.
Therefore, the study investigates the relationship between WWI and depression in women aged 18-45 in the United States and secondary infertility. To our knowledge, this is the first study to evaluate the relationship between WWI and secondary infertility. In addition, this study hypothesizes that depression plays a mediating role in the relationship between WWI and secondary infertility. On the basis of exploring the relationship between WWI, depression, and secondary infertility, analyze the role of depression in the relationship between WWI and secondary infertility.
Materials and methods
Survey description
The cross-sectional data was from NHANES, a national study conducted by the National Center for Health Statistics (NCHS) to evaluate the nutritional and health status of the United States. The Research Ethics Review Committee of NCHS approved all NHANES research protocols and obtained written informed consent from all survey participants. Participants provided demographic, dietary, examination, laboratory and questionnaire data. All detailed NHANES research designs and data are publicly available at www.cdc.gov/nchs/NHANEs/. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines for cross-sectional studies.
Study population
The NHANES datasets were utilized for this investigation from 1999-2020. Participants with complete data on WWI, depression and secondary infertility participated in our analysis. Initially, a total of 107,621 participants were recruited. They were excluding those with missing secondary infertility diagnostic (n=101067), age not between 18 and 45 years old (n=2151), never been pregnant before (n=1523), missing data about depression (n=3), and WWI (n=99). The missing covariate values were represented by means or other. Our final analysis included 2778 eligible participants (Figure 1).
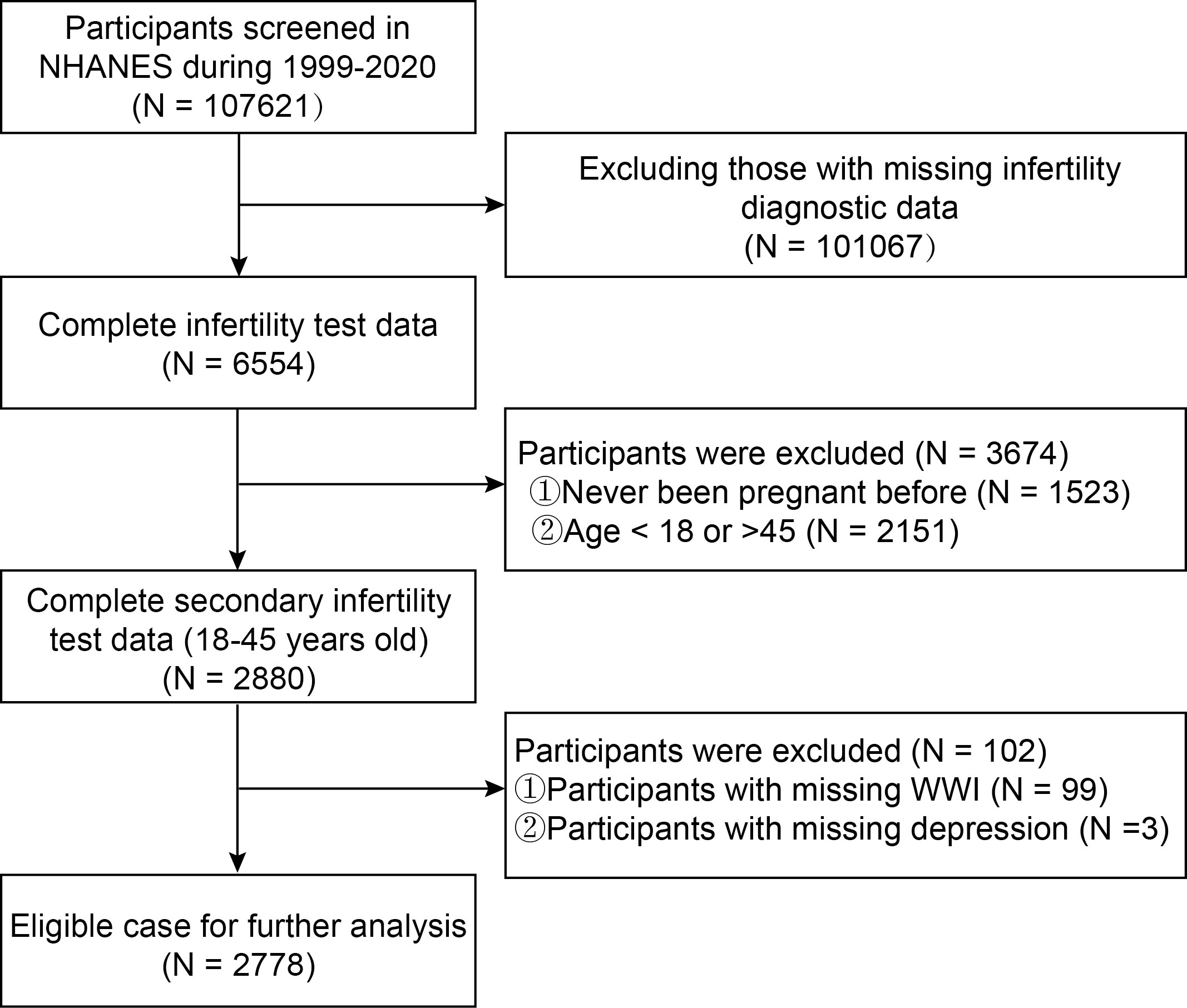
Figure 1 Flowchart of study population inclusion in 1999–2020 NHANES. NHANES, National Health and Nutrition Examination Survey; WWI, weight-adjusted-waist index.
Assessment of secondary infertility
Secondary infertility was determined based on the Reproductive Health Questionnaire (RHQ) questions RHQ074: “Tried for a year to become pregnant?” and RHQ131”Ever been pregnant?”. Participants who answered “yes” to the two questions were considered as having secondary infertility.
Assessment of weight-adjusted-waist index
WWI samples of NHANES participants were obtained in examination data. The WWI calculation was based on the participant’s waist circumference divided by the square root of their weight (26). The unit of waist circumference is centimeters, and the unit of weight is kilograms. The WWI score is positively correlated with central obesity (27) (Equation 8). WWI was treated as a continuous variable and designed as an exposed variable in our study.
Assessment of other obesity indicators
Typical obesity indicators include waist circumference (WC), body mass index (BMI) (Equation 1), waist-BMI ratio (wBMI) (Equation 4), waist-to-height ratio (WHtR) (Equation 2), waist-to-hip ratio (WHR) (Equation 3), conicity index (CI) (Equation 5), body roundness index (BRI) (Equation 7), and a body shape index (ABSI) (Equation 6). These obesity indicators were determined based on the Body Measures Examination (BMX) items. The calculation formula for these indicators is as follows (13, 14):
Assessment of depression
Depression samples of NHANES participants were obtained in questionnaire data. The Patient Health Questionnaire-9 (PHQ-9) has 9 items and is a simple and effective self-assessment scale for depression disorders, with good reliability and validity, as demonstrated by a reported Cronbach’ s α 0.89 (28, 29). A score of 0-4 indicates no depression, a score of 5-9 indicates mild depression, a score of 10-14 indicates moderate depression, and a score of ≥ 15 indicates severe depression (29).
Assessment of covariates of interest
Demographic and dietary covariates in our study included age, race, education level, marital status, family income to poverty ratio, and dietary fiber (gm). Body measure covariates included BMI. The questionnaire variates composed of alcohol use, diabetes, sleep disorders, minutes of sedentary activity, age when first menstrual period occurred, had regular periods in past 12 months, ever treated for a pelvic infection/PID and ever taken birth control pills were also included. All detailed measurement processes of these variables are publicly available at www.cdc.gov/nchs/nhanes/.
Statistical analysis
Data description and statistical analysis were based on complex weighting in descriptive analysis. Continuous variables were summarized as the means with standard error (SE), and categorical parameters were presented as proportions. Using logistic regression analysis to analyze the risk relationship between WWI and secondary infertility, this study constructed three logistic regression models that adjusted for different confounding factors. Among them, Model 1: did not adjust for any confounding factors; Model 2: adjusted for age, and race; Model 3: further adjustments were made to age, ethnicity/race, education level, marital status, family income, BMI, alcohol use, diabetes, dietary fiber (gm), minutes sedentary activity, sleep disorder, age when first menstrual period occurred, had regular periods in past 12 months, ever treated for a pelvic infection/PID and ever taken birth control pills based on Model 2. In sensitivity analysis, linear trend tests were conducted with WWI quartile groups as independent variables to evaluate its robustness (30). Subgroup analysis was performed using a stratified multivariable logistic regression model, and stratified factors included age, ethnicity/race, education level, marital status, BMI, diabetes, PHQ-9 score, had regular periods in past 12 months, ever treated for a pelvic infection/PID, and ever taken birth control pills. This study used smooth curve fitting to observe whether the relationship between WWI and secondary infertility is linear. If non-linear, threshold effect analysis was used to provide each interval and calculate the threshold. We also analyzed the ability of WWI and other obesity indicators to predict secondary infertility through the receiver operating characteristic (ROC) curve and the area under the comparison curve (AUC) value. Finally, the product distribution method was used to test the mediating effect of depression between WWI and secondary infertility (31, 32). Other representations were used for missing values in classification variables based on existing data, while for missing values in continuous variables, mean interpolation was used. PackageR (http://www.r-project.org) and EmpowerStats (http://www.empowerstats.com) were used for all analyses. Statistical significance was assessed at a two-sided value of P<0.05.
Results
Baseline characteristics of participants
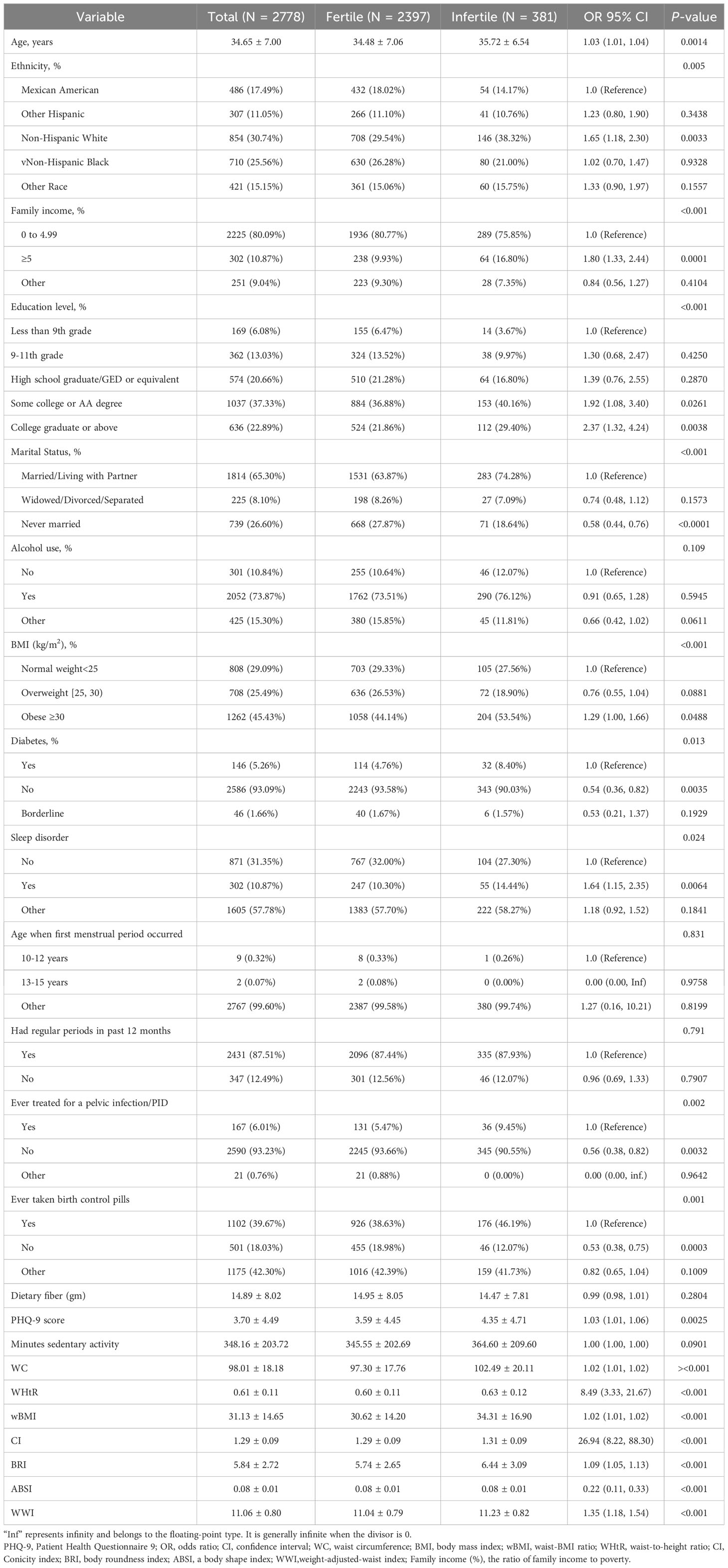
A total of 2778 secondary infertility participants were selected, all of whom were women aged 18-45. Table 1 presents the characteristics of the NHANES participants by secondary infertility status. Among these, 381 females were diagnosed with secondary infertility, accounting for 13.71% of participants. Females with secondary infertility were older (35.72 ± 6.54 years old), had higher BMI, and family income and education level, and had a higher proportion of diabetes and sleep disorders than those without secondary infertility. The secondary infertility group tended to be non-Hispanic white race/ethnicity and never married more than the healthy controls. What’s more, secondary infertility females demonstrated higher PHQ-9 scores and WWI.
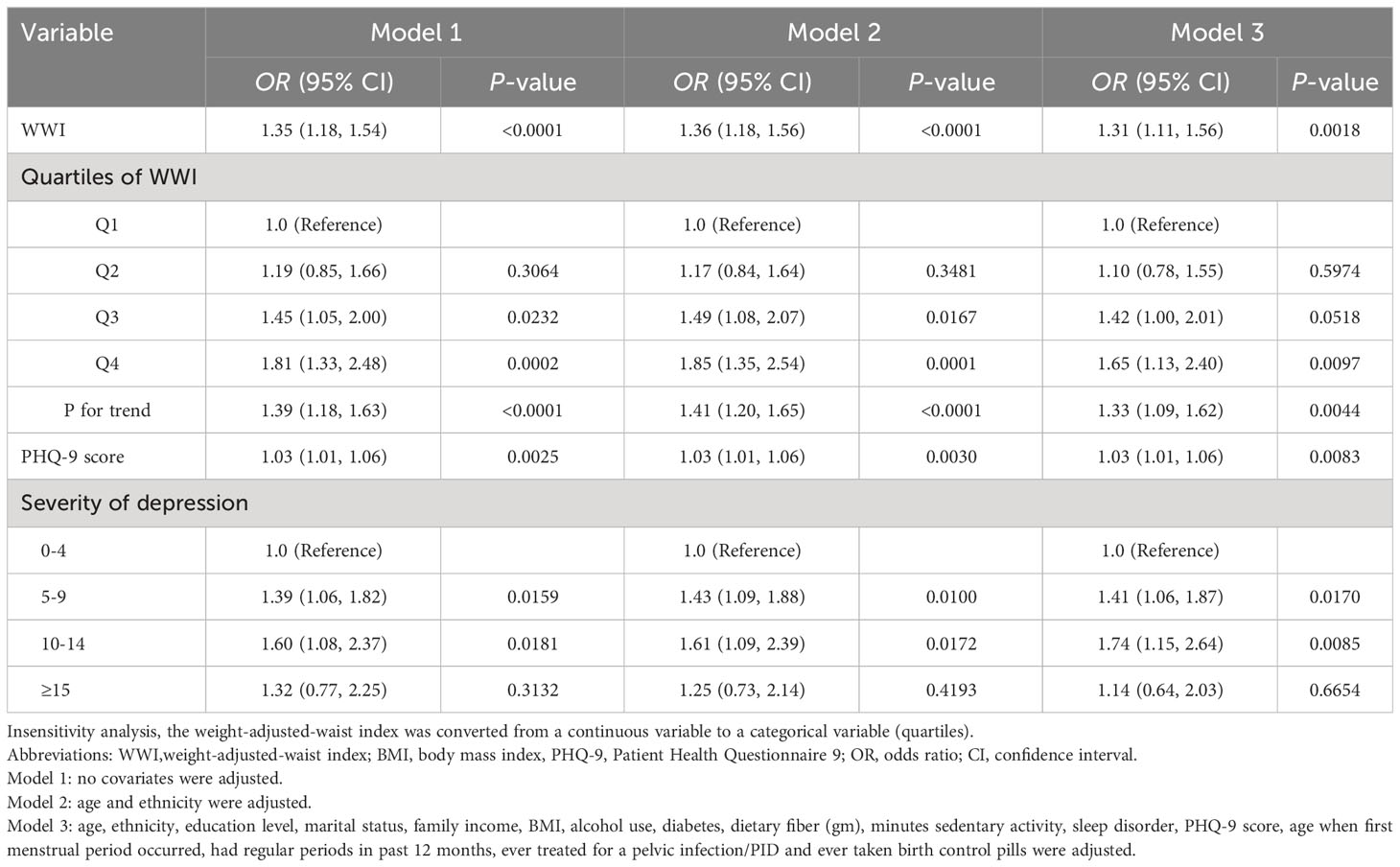
The associations of weight-adjusted-waist index and depression with secondary infertility
Logistic regression analysis showed that after adjusting for all confounding factors, the correlation between WWI, depression, and secondary infertility remained significant. As shown in Table 2, an increase of one unit in WWI is associated with a 31% increase in the prevalence of secondary infertility, while an increase of one point in the PHQ-9 score is associated with a 3% increase in the prevalence of secondary infertility. Sensitivity analysis using WWI as a categorical variable (quartile) still showed significant statistical significance (OR=1.33, 95% CI: 1.09-1.62; P = 0.0044). Subgroup analysis for the association between WWI and infertility (Table 3). None of the stratifications including age, ethnicity, education lever, marital status, PHQ-9 score, BMI, diabetes, had regular periods in past 12 months, ever treated for a pelvic infection/PID and ever taken birth control pills affected the positive association of WWI and infertility
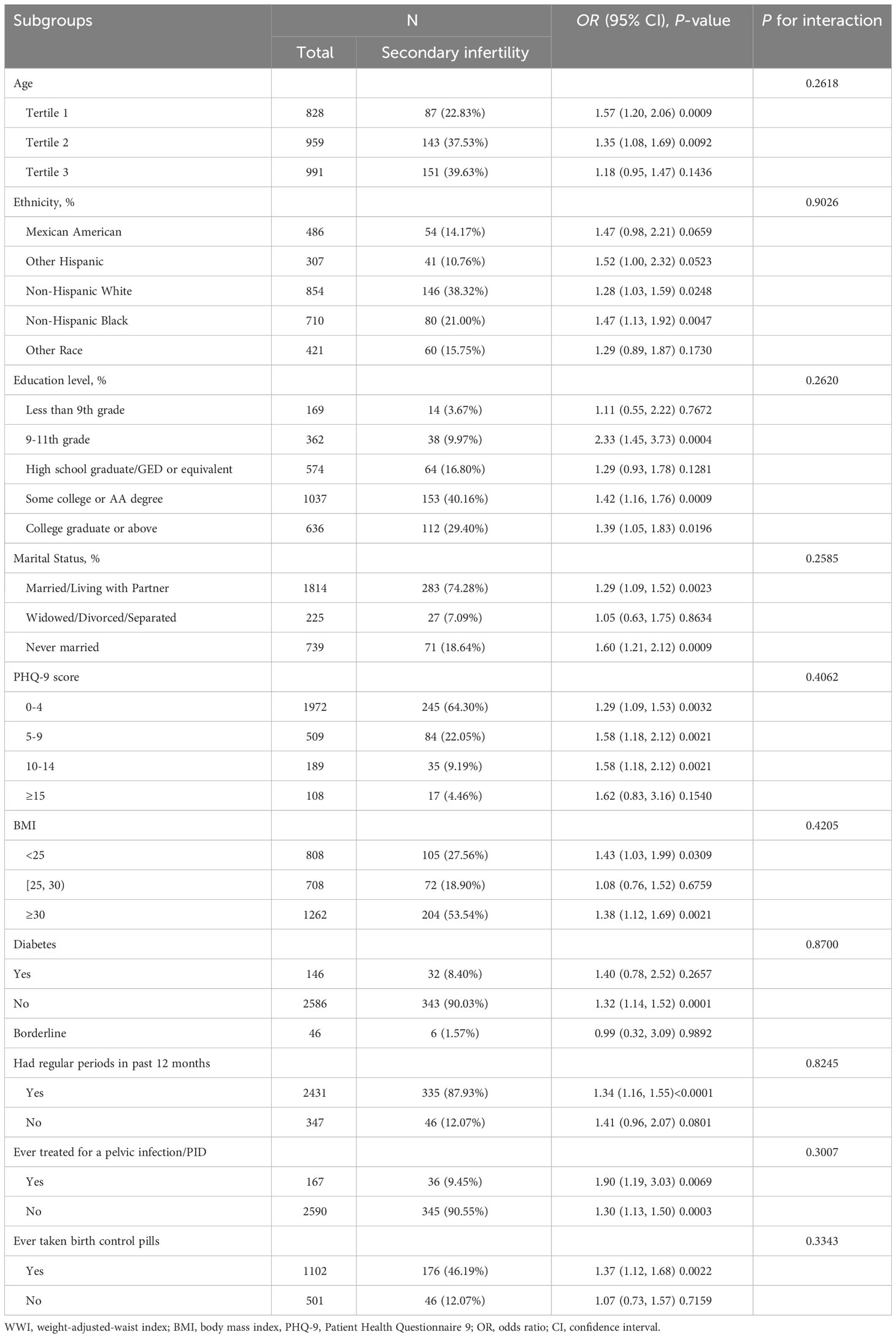
WWI showed a good correlation than other markers of obesity including WC, BMI, WHtR, WHR, wBMI, BRI and ABSI for secondary infertility
Smooth curve fitting exhibited a positive relationship between WWI and secondary infertility (Figure 2A). Then, we calculated the AUC values to compare the predictive accuracy of WWI with other obesity indicators (WC, BMI, WHtR, WHR, wBMI, CI, BRI and ABSI) for secondary infertility (Figures 2B, C). We found that the AUC values of WWI and CI were higher than the other obesity indicators in predicting secondary infertility. Moreover, the difference in AUC values between WWI and other obesity indicators was statistically significant (all P< 0.05), suggesting that WWI maybe have a good advantage in evaluating secondary infertility (Table 4).
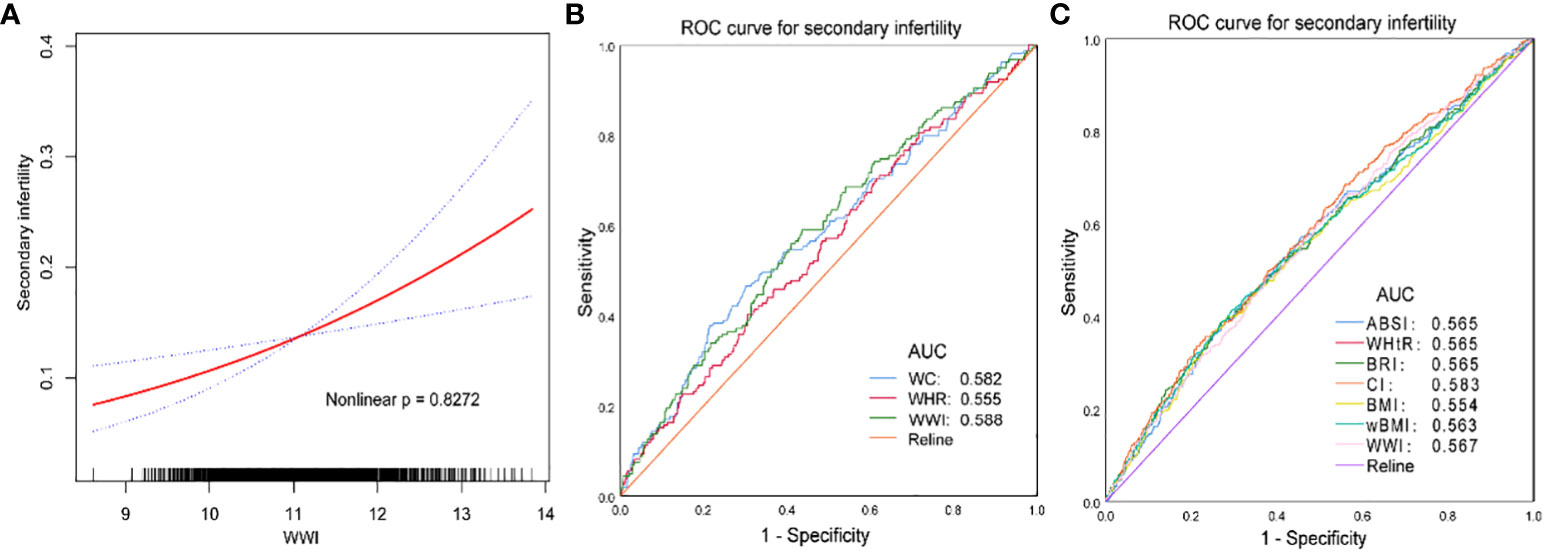
Figure 2 (A, C) the NHANES datasets were utilized for this investigation from 1999-2020. (B) the NHANES datasets were utilized for this investigation from 2017-2020. WC, waist circumference; BMI, body mass index; wBMI, waist-BMI ratio; WHtR, waist-to-height ratio; WHR, waist-to-hip ratio; CI, Conicity index; BRI, body roundness index; ABSI, a body shape index; WWI,weight-adjusted-waist index. Age, ethnicity, education level, marital status, family income, BMI, alcohol use, diabetes, dietary fiber (gm), minutes sedentary activity, sleep disorder, PHQ-9 score, age when first menstrual period occurred, had regular periods in past 12 months, ever treated for a pelvic infection/PID and ever taken birth control pills were adjusted.
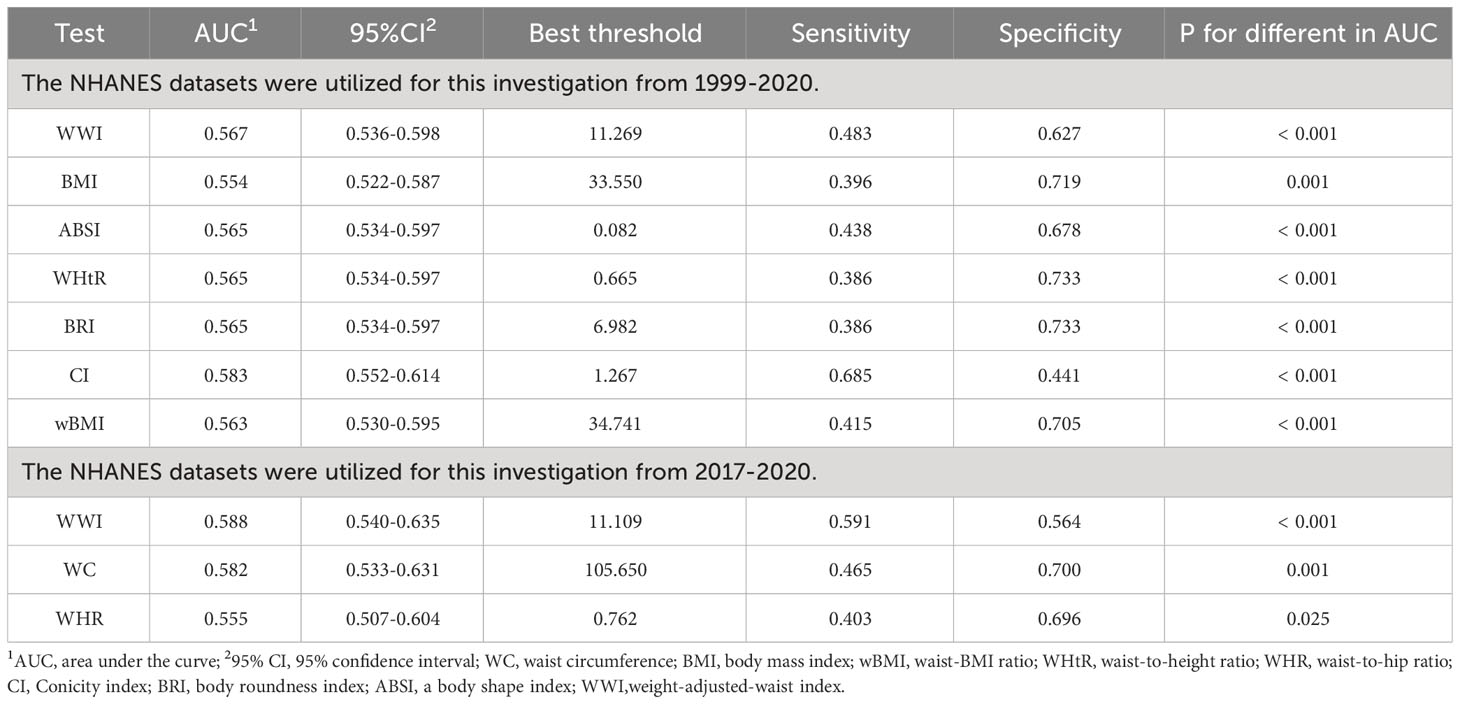
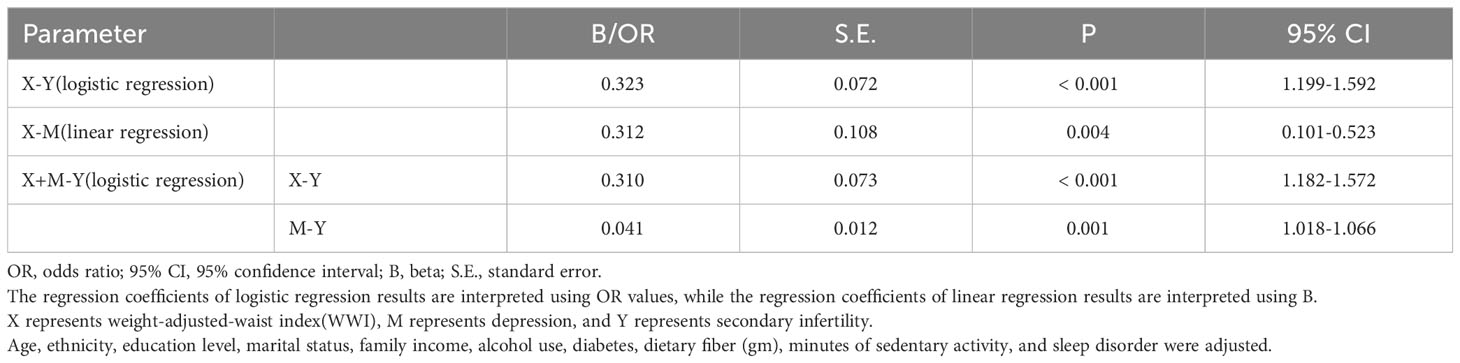
Mediation analyses
The first step is to perform a logistic regression analysis of WWI(X) for secondary infertility(Y), and obtain c=0.323, SE(c)=0.072; Perform linear regression analysis of WWI(X) for depression(M), and obtain coefficients a=0.312 and SE(a)=0.108; Finally, a logistic regression analysis was conducted between WWI(X) and depression(M) for secondary infertility(Y), and the coefficients b=0.041, c ‘=0.310, SE(b)=0.012, and SE(c’) =0.073 were obtained (Table 5).
The second step is that the total effect (p<0.001) and direct effect(p<0.001) of WWI on secondary infertility are statistically significant. The 95% confidence interval for mediating effects obtained from the R Mediation software package of R software using the product distribution method is [2.390833, 21.252207], excluding 0. Therefore, the mediating effect of depression between WWI and secondary infertility is significant.
Step 3, calculated by SPSS software, SD(X)=0.798, SD(M)=4.491, Var(X)=0.638, Var(M)=20.171, and Cov(X, M)=0.265. According to the formula, Var(Y’)=3.356, Var(Y’’)=3.392, then SD(Y’)=1.832, SD(Y ‘‘)=1.842. Calculate using the formula to obtain aSTD=0.0554, bSTD=0.09996, c’STD=0.13430, cSTD=0.14070. Specific formula: aSTD=aSD(X)/SD(M), bSTD=bSD(M)/SD(Y’’), cSTD =cSD(X)/SD(Y’), c’STD=c’SD(X)/SD(Y’’), Var(Y’)=c2Var(X)+π2/3, Var(Y’’)=c’2Var(X)+b2Var(M)+ 2bc’Cov(X,M)+π2/3. In the above formula, there is a subscript STD on the left, which represents the standardized coefficient converted from the coefficient in Logistic units. Where π2/3 is the variance of the standard logistic distribution. The mediating effect of depression accounts for 3.94% of the total effect [(aSTD × bSTD/(aSTD × bSTD+c’STD). The analysis of the mediating effect pathway is shown in Figure 3.
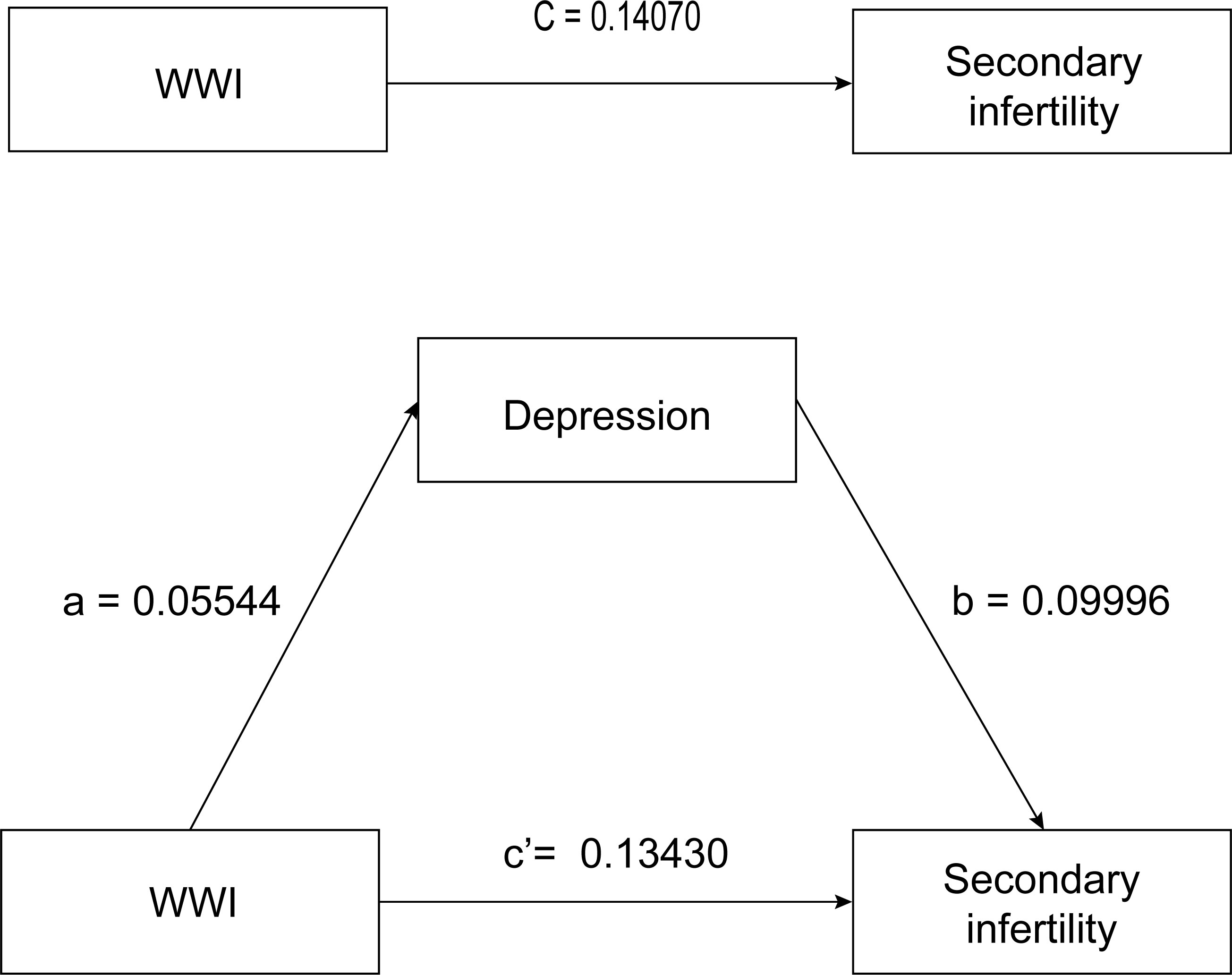
Figure 3 WWI, weight-adjusted-waist index. Age, ethnicity, education level, marital status, family income, alcohol use, diabetes, dietary fiber (gm), minutes sedentary activity, and sleep disorder were adjusted. Total effect 0.14070; Direct effect 0.13430; Indirect effect 0.00554.
Discussion
Secondary infertility accounts for a relatively high proportion of women among all infertility patients (2). This study investigated the relationship between WWI and depression in women aged 18-45 in the United States and secondary infertility. To our knowledge, this is the first study to evaluate the relationship between WWI and secondary infertility. We found a positive correlation between WWI and secondary infertility in rough and adjusted models. Sensitivity analysis using WWI as a quartile also revealed a correlation between WWI (OR=1.33; 95% CI, 1.09-1.62, P =0.0044)and secondary infertility. Subgroup analysis showed that this association between WWI and secondary infertility was stable across various demographic situations. The results of this study are similar to other studies, Wen et al. also found that WWI (OR=1.42, 95% CI: 1.22-1.65) hurts a person’s fertility (14). Legese et al. found that the incidence of secondary infertility is significantly higher in obese women (33). More and more evidence suggests that obesity can lead to anovulation, menstrual irregularities, reduced conception rates, and reduced response to fertility treatment (34, 35). However, the underlying causes of this unfavorable relationship between females’ secondary infertility and WWI are uncertain. It may be that adipose tissue affects the ovarian and endometrial function of obese women by producing leptin, free fatty acids, and cytokines (36).
We further found that compared to other obesity markers, the correlation between WWI, CI and secondary infertility is stronger, indicating that WWI may be more accurate in predicting secondary infertility than other obesity-related indicators. WWI is a newly developed obesity indicator that can more accurately predict total body fat percentage and has been explored in various fields (37, 38). Park et al. research shows that WWI is closely related to the incidence rate of cardiac metabolism and cardiovascular death, which is not apparent in BMI (39). Qin et al. observed that the prevalence of proteinuria is significantly related to WWI, and WWI (OR=1.28; BMI: OR=1.02; WC: OR=1.01) may be more accurate than other obesity indicators in predicting the incidence rate of proteinuria (40). Wen et al. also validated the predictive efficacy of WWI (WWI: OR=1.33; BMI: OR=1.30; WC: OR=1.28; ABSI: OR=1.21) in infertile populations (14). More importantly, we verified that the correlation between WWI (AUCWWI=0.588) and secondary infertility is higher than other typical obesity indicators(WC, BMI, WHtR, WHR, wBMI, BRI and ABSI). In summary, it is widely believed that WWI may be used as a predictive factor for obesity-related diseases, and our research supports this statement.
The relationship between WWI and infertility has been established in recent years, but the mechanism behind this is still unclear, especially in women with secondary infertility. Previous systematic evaluations have shown that obese women have a higher risk of developing depressive symptoms (21), and obesity may lead to changes in the gut microbiota, thereby affecting the host’s emotions and behavior (41). Psychological barriers are becoming increasingly common in modern society. Preexisting emotional disorders, such as anxiety and depression, may hurt the outcome of infertility treatment (42), which may be due to emotional disorders affecting hormone secretion and endometrial growth (20). In the same way, the incidence of psychological depression will significantly increase with the prolongation of infertility, and women with infertility are twice as likely to be affected by emotional disorders as other women (43, 44). Previous studies have shown that depression plays a mediating role in treating and caring for various diseases (45, 46). Based on the large population of NHANES, Pan et al. study showed that the PHQ-9 score was estimated to mediate a 0.2% (P=0.03) association between ABSI and infertility (17). We also found that in secondary infertility women, 3.94% of the relationship between WWI and secondary infertility seems to be mediated by depressive symptoms. These results indicate that improving depression symptoms in patients may reduce the likelihood of secondary infertility caused by WWI.
More and more research is focuses on potential mediators and interventions for reversing infertility, manifested in weight loss, physical activity, dietary factors, and weight loss surgery (47). However, the results of these interventions are not satisfactory. A systematic review shows that cognitive-behavioral treatment(CBT), mind-body interventions(MBI), and stress management skills(SMS) are the most common psychological interventions for infertile women, and are beneficial for improving their mental health status (48). Psychological intervention is equally necessary as medication for infertility (49), and our study suggests the mediating effect of depression between WWI and secondary infertility. Management strategies determined based on female depression scores and WWI may help reduce women’s secondary infertility risk.
Our research has several advantages. Our research is based on national data, and the results are widely applicable to the general population in the United States. Regression analysis was adjusted for covariates, and the large sample size allowed us to conduct sensitivity analysis and subgroup analysis to confirm the robustness of the results. Finally, the mediating role of depression between WWI and secondary infertility was verified. However, there are still some restrictions that need to be declared. Although we have adjusted for some potential covariates, many factors still affect secondary infertility, and we cannot completely rule out the effects of other potential confounding factors, such as other social, environmental and antidepressants use variables. Our research findings are based on one country and race, so it remains to be investigated whether these findings apply to other races or countries. This survey was a cross-sectional study that can only explore the relationship between WWI, depression, and secondary infertility, providing clues for etiological research. It cannot verify the causal relationship between disease and etiology. In addition, in the mediation analysis, depression mediate partly the association between WWI and secondary infertility, but its effect is relatively weak. Therefore, further cohort studies are needed to verify its causal relationship, in order to ensure that readers have a clearer and more accurate understanding of the relationship between depression and secondary infertility in WWI.
Conclusion
This study shows that WWI and depression are associated with secondary infertility, and WWI’s predictive power for secondary infertility is better than other obesity indicators. In addition, depressive symptoms may play a mediating role in the relationship between WWI and secondary infertility. This suggests that clinical healthcare workers should pay more attention to the mental health of obese women in the future, which may protect them from infertility.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: www.cdc.gov/nchs/nhanes/.
Ethics statement
The studies involving humans were approved by The Research Ethics Review Board of the NCHS. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
FS: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. ML: Conceptualization, Data curation, Formal analysis, Funding acquisition, Supervision, Writing – review & editing. SH: Conceptualization, Data curation, Formal analysis, Funding acquisition, Supervision, Writing – review & editing. RX: Data curation, Formal analysis, Methodology, Software, Supervision, Writing – review & editing. HC: Conceptualization, Formal analysis, Supervision, Writing – review & editing. ZS: Conceptualization, Formal analysis, Supervision, Writing – review & editing. HB: Conceptualization, Formal analysis, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Wuxi Research project of Wuxi Municipal Health Commission (FYKY202201), Wuxi Science and Technology Development Fund Project (Y20212036) and Wuxi Municipal Health Commission Maternal and Child Health Research Project (FYKY202105).
Acknowledgments
We thank the assistance of all authors in the manuscript preparation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2024.1330206/full#supplementary-material
References
1. Vander Borght M, Wyns C. Fertility and infertility: Definition and epidemiology. Clin Biochem. (2018) 62:2–10. doi: 10.1016/j.clinbiochem.2018.03.012
2. Polis CB, Cox CM, Tunçalp Ö, McLain AC, Thoma ME. Estimating infertility prevalence in low-to-middle-income countries: an application of a current duration approach to Demographic and Health Survey data. Hum Reprod. (2017) 32:1064–74. doi: 10.1093/humrep/dex025
3. Infertility workup for the women's health specialist: ACOG committee opinion, number 781. Obstet Gynecol. (2019) 133:e377–e84. doi: 10.1097/AOG.0000000000003271
4. Liang S, Chen Y, Wang Q, Chen H, Cui C, Xu X, et al. Prevalence and associated factors of infertility among 20-49 year old women in Henan Province, China. Reprod Health. (2021) 18:254. doi: 10.1186/s12978-021-01298-2
5. Garolla A, Pizzol D, Carosso AR, Borini A, Ubaldi FM, Calogero AE, et al. Practical clinical and diagnostic pathway for the investigation of the infertile couple. Front Endocrinol (Lausanne). (2020) 11:591837. doi: 10.3389/fendo.2020.591837
6. Carson SA, Kallen AN. Diagnosis and management of infertility: A review. Jama. (2021) 326:65–76. doi: 10.1001/jama.2021.4788
7. Bala R, Singh V, Rajender S, Singh K. Environment, lifestyle, and female infertility. Reprod Sci. (2021) 28:617–38. doi: 10.1007/s43032-020-00279-3
8. Giviziez CR, Sanchez EG, Approbato MS, Maia MC, Fleury EA, Sasaki RS. Obesity and anovulatory infertility: A review. JBRA assisted Reprod. (2016) 20:240–5. doi: 10.5935/1518-0557.20160046
9. Zeng X, Xie YJ, Liu YT, Long SL, Mo ZC. Polycystic ovarian syndrome: Correlation between hyperandrogenism, insulin resistance and obesity. Clinica chimica acta; Int J Clin Chem. (2020) 502:214–21. doi: 10.1016/j.cca.2019.11.003
10. Wei W, Zhang X, Zhou B, Ge B, Tian J, Chen J. Effects of female obesity on conception, pregnancy and the health of offspring. Front Endocrinol (Lausanne). (2022) 13:949228. doi: 10.3389/fendo.2022.949228
11. Sciarra F, Franceschini E, Campolo F, Gianfrilli D, Pallotti F, Paoli D, et al. Disruption of circadian rhythms: A crucial factor in the etiology of infertility. Int J Mol Sci. (2020) 21:3943. doi: 10.3390/ijms21113943
12. Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PloS One. (2012) 7:e39504. doi: 10.1371/journal.pone.0039504
13. Głuszek S, Ciesla E, Głuszek-Osuch M, Kozieł D, Kiebzak W, Wypchło Ł, et al. Anthropometric indices and cut-off points in the diagnosis of metabolic disorders. PloS One. (2020) 15:e0235121. doi: 10.1371/journal.pone.0235121
14. Wen Z, Li X. Association between weight-adjusted-waist index and female infertility: a population-based study. Front Endocrinol (Lausanne). (2023) 14:1175394. doi: 10.3389/fendo.2023.1175394
15. Kim NH, Park Y, Kim NH, Kim SG. Weight-adjusted waist index reflects fat and muscle mass in the opposite direction in older adults. Age Ageing. (2021) 50:780–6. doi: 10.1093/ageing/afaa208
16. He Q, Chen C, Bai S. The association between weight-adjusted-waist index and self-reported infertility among women of reproductive age in the United States. J obstetrics gynaecology Res. (2023) 49:2929–37. doi: 10.1111/jog.15782
17. Liu H, Zhi J, Zhang C, Huang S, Ma Y, Luo D, et al. Association between Weight-Adjusted Waist Index and depressive symptoms: A nationally representative cross-sectional study from NHANES 2005 to 2018. J Affect Disord. (2024) 350:49–57. doi: 10.1016/j.jad.2024.01.104
18. Ruan X, Chen J, Sun Y, Zhang Y, Zhao J, Wang X, et al. Depression and 24 gastrointestinal diseases: a Mendelian randomization study. Trans Psychiatry. (2023) 13:146. doi: 10.1038/s41398-023-02459-6
19. Wang X, Wang N, Zhong LLD, Su K, Wang S, Zheng Y, et al. Development and validation of a risk prediction model for breast cancer prognosis based on depression-related genes. Front Oncol. (2022) 12:879563. doi: 10.3389/fonc.2022.879563
20. Wdowiak A, Makara-Studzińska M, Raczkiewicz D, Cyranka K. Reproductive problems and intensity of anxiety and depression in women treated for infertility. Psychiatria polska. (2022) 56:153–70. doi: 10.12740/PP/125885
21. Wang Y, Ni Z, Li K. The prevalence of anxiety and depression of different severity in women with polycystic ovary syndrome: a meta-analysis. Gynecological endocrinology: Off J Int Soc Gynecological Endocrinol. (2021) 37:1072–8. doi: 10.1080/09513590.2021.1942452
22. Yoldemir T, Yassa M, Atasayan K. Comparison of depression between primary and secondary infertile couples. Gynecological endocrinology: Off J Int Soc Gynecological Endocrinol. (2020) 36:1131–5. doi: 10.1080/09513590.2020.1807503
23. Herbert DL, Lucke JC, Dobson AJ. Depression: an emotional obstacle to seeking medical advice for infertility. Fertil Steril. (2010) 94:1817–21. doi: 10.1016/j.fertnstert.2009.10.062
24. Pathare ADS, Loid M, Saare M, Gidlöf SB, Zamani Esteki M, Acharya G, et al. Endometrial receptivity in women of advanced age: an underrated factor in infertility. Hum Reprod Update. (2023) 29:773–93. doi: 10.1093/humupd/dmad019
25. Li X, Peng Y, Mao Y, Li Y, Gong F, Ouyang Y. Endometrial receptivity change: ultrasound evaluation on ovulation day and transplantation day during the natural frozen embryo transfer cycle. Front Endocrinol (Lausanne). (2023) 14:1118044. doi: 10.3389/fendo.2023.1118044
26. Kim JY, Choi J, Vella CA, Criqui MH, Allison MA, Kim NH. Associations between weight-adjusted waist index and abdominal fat and muscle mass: multi-ethnic study of atherosclerosis. Diabetes Metab J. (2022) 46:747–55. doi: 10.4093/dmj.2021.0294
27. Kim KJ, Son S, Kim KJ, Kim SG, Kim NH. Weight-adjusted waist as an integrated index for fat, muscle and bone health in adults. J cachexia sarcopenia Muscle. (2023) 14:2196–203. doi: 10.1002/jcsm.13302
28. Patel JS, Oh Y, Rand KL, Wu W, Cyders MA, Kroenke K, et al. Measurement invariance of the patient health questionnaire-9 (PHQ-9) depression screener in U.S. adults across sex, race/ethnicity, and education level: NHANES 2005-2016. Depression Anxiety. (2019) 36:813–23. doi: 10.1002/da.22940
29. Negeri ZF, Levis B, Sun Y, He C, Krishnan A, Wu Y, et al. Accuracy of the Patient Health Questionnaire-9 for screening to detect major depression: updated systematic review and individual participant data meta-analysis. Bmj. (2021) 375:n2183. doi: 10.1136/bmj.n2183
30. VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. (2017) 167:268–74. doi: 10.7326/M16-2607
31. Tofighi D, MacKinnon DP. RMediation: an R package for mediation analysis confidence intervals. Behav Res Methods. (2011) 43:692–700. doi: 10.3758/s13428-011-0076-x
32. MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Eval Rev. (1993) 17:144–58. doi: 10.1177/0193841X9301700202
33. Legese N, Tura AK, Roba KT, Demeke H. The prevalence of infertility and factors associated with infertility in Ethiopia: Analysis of Ethiopian Demographic and Health Survey (EDHS). PloS One. (2023) 18:e0291912. doi: 10.1371/journal.pone.0291912
34. Al-Lami RA, Taha SA, Jalloul RJ, Salih SM. Obesity in infertile women, a cross-sectional study of the United States using NSFG 2011-2019. Reprod Sci. (2022) 29:1449–56. doi: 10.1007/s43032-021-00777-y
35. Boedt T, Vanhove AC, Vercoe MA, Matthys C, Dancet E, Lie Fong S. Preconception lifestyle advice for people with infertility. Cochrane Database systematic Rev. (2021) 4:Cd008189. doi: 10.1002/14651858.CD008189.pub3
36. Gambineri A, Laudisio D, Marocco C, Radellini S, Colao A, Savastano S. Female infertility: which role for obesity? Int J Obes Suppl. (2019) 9:65–72. doi: 10.1038/s41367-019-0009-1
37. Ding C, Shi Y, Li J, Li M, Hu L, Rao J, et al. Association of weight-adjusted-waist index with all-cause and cardiovascular mortality in China: A prospective cohort study. Nutrition metabolism Cardiovasc Dis NMCD. (2022) 32:1210–7 doi: 10.1016/j.numecd.2022.01.033
38. Ye J, Hu Y, Chen X, Yin Z, Yuan X, Huang L, et al. Association between the weight-adjusted waist index and stroke: a cross-sectional study. BMC Public Health. (2023) 23:1689. doi: 10.1186/s12889-023-16621-8
39. Park Y, Kim NH, Kwon TY, Kim SG. A novel adiposity index as an integrated predictor of cardiometabolic disease morbidity and mortality. Sci Rep. (2018) 8:16753. doi: 10.1038/s41598-018-35073-4
40. Qin Z, Chang K, Yang Q, Yu Q, Liao R, Su B. The association between weight-adjusted-waist index and increased urinary albumin excretion in adults: A population-based study. Front Nutr. (2022) 9:941926. doi: 10.3389/fnut.2022.941926
41. Schachter J, Martel J, Lin CS, Chang CJ, Wu TR, Lu CC, et al. Effects of obesity on depression: A role for inflammation and the gut microbiota. Brain behavior Immun. (2018) 69:1–8. doi: 10.1016/j.bbi.2017.08.026
42. Schaller MA, Griesinger G, Banz-Jansen C. Women show a higher level of anxiety during IVF treatment than men and hold different concerns: a cohort study. Arch gynecology obstetrics. (2016) 293:1137–45. doi: 10.1007/s00404-016-4033-x
43. Dong M, Xu X, Li Y, Wang Y, Jin Z, Tan J. Impact of infertility duration on female sexual health. Reprod Biol Endocrinol RB&E. (2021) 19:157. doi: 10.1186/s12958-021-00837-7
44. Merrell J, Lavery M, Ashton K, Heinberg L. Depression and infertility in women seeking bariatric surgery. Surg Obes related Dis Off J Am Soc Bariatric Surg. (2014) 10:132–7. doi: 10.1016/j.soard.2013.10.019
45. Peng X, Lu Y, Chen PY, Wong CH. The mediating effect of depression on the relationship between osteoarthritis and cardiovascular disease mortality: A cohort study. J Affect Disord. (2023) 341:329–34. doi: 10.1016/j.jad.2023.08.108
46. Zhou W, Sun L, Zeng L, Wan L. Mediation of the association between sleep disorders and cardiovascular disease by depressive symptoms: An analysis of the National health and Nutrition Examination Survey (NHANES) 2017-2020. Prev Med Rep. (2023) 33:102183. doi: 10.1016/j.pmedr.2023.102183
47. Boyle BR, Ablett AD, Ochi C, Hudson J, Watson L, Rauh D, et al. The effect of weight loss interventions for obesity on fertility and pregnancy outcomes: A systematic review and meta-analysis. Int J gynaecology obstetrics: Off Organ Int Fed Gynaecology Obstetrics. (2023) 161:335–42. doi: 10.1002/ijgo.14597
48. Koochaksaraei FY, Simbar M, Khoshnoodifar M, Faramarzi M, Nasiri M. Interventions promoting mental health dimensions in infertile women: a systematic review. BMC Psychol. (2023) 11:254. doi: 10.1186/s40359-023-01285-1
Keywords: secondary infertility, weight-adjusted-waist index (WWI), depression, NHANES, ROC, mediating effect
Citation: Sun F, Liu M, Hu S, Xie R, Chen H, Sun Z and Bi H (2024) Associations of weight-adjusted-waist index and depression with secondary infertility. Front. Endocrinol. 15:1330206. doi: 10.3389/fendo.2024.1330206
Received: 30 October 2023; Accepted: 19 February 2024;
Published: 07 March 2024.
Edited by:
Kulvinder Kochar Kaur, Kulvinder Kaur Centre For Human Reproduction, IndiaReviewed by:
Daiji Nagayama, Toho University, JapanWeijian Li, Shenzhen Luohu People’s Hospital, China
Amani Alrasheedi, King Abdulaziz University, Saudi Arabia
Copyright © 2024 Sun, Liu, Hu, Xie, Chen, Sun and Bi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Min Liu, bGl1bWluXzc2QDE2My5jb20=
 Fei Sun
Fei Sun Min Liu
Min Liu Shanshan Hu2
Shanshan Hu2 Ruijie Xie
Ruijie Xie