- 1School of Public Health, College of Health Science and Medicine, Wolaita Sodo University, Wolaita Sodo, Ethiopia
- 2Department of Ophthalmology and Optometry, Hawassa University College of Medicine and Health Science, Hawassa, Ethiopia
- 3Department of Midwifery, Menelik II Medical and Health Science College, Addis Ababa, Ethiopia
Introduction: Nowadays, diabetes mellitus is a major global health issue with serious social, economic, and developmental impacts. One of its most severe complications is foot problems. Research shows that poor self-care practices in managing diabetic feet are a key factor in ulcer development.
Objective: This study aimed to determine the pooled prevalence of foot self-care practice and associated factors among diabetic patients in Africa.
Methods: We found articles using electronic databases, including PubMed, Cochrane Library, Google Scholar, Web of Science, African Journals Online, and Science Direct. Accordingly, we identified 143 published articles. A total of 31 eligible studies were included in the systematic review. Data extraction used a standardized checklist, and analysis was conducted with STATA 14 statistical software. Various methods were used to assess the presence of publication bias, including funnel plots and the Begg and Egger regression test. A significance level of P ≤0.05 was used to indicate potential publication bias. Heterogeneity between included studies was assessed using the I2 statistics. The random effect model was used to estimate the pooled estimates.
Results: The pooled prevalence of foot self-care practices among diabetic patients in Africa was 46.93% (95%CI (39.44–54.41)). Diabetic foot self-care practices were significantly associated with rural residence (AOR: 2.50, 95% CI (1.65–3.80)), educational level (AOR: 3.00, 95%CI (2.07–4.34)), and knowledge level of diabetes patients (AOR: 3.41, 95%CI (2.22–5.23)).
Conclusions: In conclusion, more than half of diabetic patients had poor diabetes foot self-care practices. Diabetic foot self-care practice was associated with a level of education, rural residence, and the knowledge level of diabetic foot care. Therefore, intervention programs ought to prioritize enhancing the knowledge base of individuals with diabetes to promote better self-care practices for their feet.
1 Introduction
Diabetes mellitus (DM) is complex group of metabolic disorders that primarily manifest through chronic hyperglycemia or elevated blood glucose levels. This condition arises from defects in insulin secretion, insulin action, or both, leading to a variety of physiological complications. The two common forms of diabetes are type one diabetes, which is characterized by an autoimmune destruction of insulin-producing beta cells in the pancreas, and Type 2 diabetes, which typically involves insulin resistance and a relative deficiency in insulin production (1).
In addition to the health implications, foot ulcers also impose a substantial financial burden on both patients and healthcare systems. Costs associated with treating foot-related problems can be considerable, encompassing expenses related to medical consultations, diagnostic tests, wound care supplies, and potential surgical interventions. Furthermore, the need for hospitalization due to complications can lead to additional healthcare costs and lost productivity for patients, who may be unable to work during their recovery (2).
The prevalence of diabetes is escalating worldwide at a concerning pace, with the International Diabetes Federation reporting 537 million individuals diagnosed with the condition in 2021. This figure is anticipated to grow to 643 million by 2030 and reach 783 million by 2045 (3). In Africa, over fifty percent of adults with diabetes are found in some of the continent’s most populous countries, such as South Africa, Nigeria, and Ethiopia (4).
Foot complications are among the most severe and costly consequences of diabetes mellitus (DM), often leading to lower limb amputations due to foot ulcers. They typically arise from peripheral neuropathy, which reduces foot sensation, and peripheral vascular diseases that hinder blood circulation, increasing the risk of infections and gangrene (5).
In developing countries, the rates of foot ulcers and amputations are strikingly high. Contributing factors like poverty, poor sanitation and hygiene, and the common practices of walking barefoot often combine to worsen the impact of diabetic foot injuries (6). If a foot ulcer goes untreated and does not heal, there is a risk of infection, and 5% to 24% of these ulcers could lead to limb amputation within six to eighteen months after the initial evaluation (7).
In many African countries with limited resources, diabetes significantly strains healthcare systems. Research indicates Africa has the world’s second-highest prevalence of diabetic foot ulcers at 7.2% among diabetics (8). A study in Sri Lanka found that over fifty percent of participants understood foot self-care principles, their actual practices were lacking, and only about two-thirds regularly inspected their feet, the only principle consistently followed (9).
A diabetic foot ulcer is the most common complication of diabetes, characterized by lesions in deeper tissues. These ulcers are often associated with neurological impairments and peripheral vascular disease, manifesting as full-thickness wounds below the ankle in individuals with diabetes (7). To mitigate risks, implementing self-care practices for diabetic foot management at home is essential to reduce the likelihood of foot ulcers (10).
Diabetic foot self-care practices include regularly checking footwear, avoiding walking without shoes, not wearing tight socks, maintaining foot hygiene through washing and drying, properly trimming toenails, and using moisturizers to prevent dryness (11). By diligently adhering to these practices, patients can significantly lower their risk of developing gangrenous or ulcerated feet. This proactive approach involves a combination of regular foot inspections, maintaining proper hygiene, and ensuring appropriate footwear, managing underlying health conditions, such as diabetes or circulatory issues, plays a crucial role in foot health (12).
However, a significant obstacle in preventing complications associated with diabetic foot is the insufficient awareness and education concerning the symptoms, risks, and early identification of diabetic foot problems. Many individuals with diabetes may not fully understand the importance of regular foot care or may be unaware of the specific symptoms that can indicate the onset of foot complications, such as numbness, tingling, or changes in skin color and temperature. This lack of knowledge can lead to resulting in more severe complications that could have been prevented with timely intervention (13).
However, there is no representative data on diabetic foot-care practices in Africa. Therefore, this systematic review and meta-analysis aimed to determine the pooled estimate of overall foot self-care practice and associated factors among diabetic patients in Africa. The result of this research serves as a foundational resource for developing national and international strategies, protocols, and guidelines. Ultimately, it will have a significant impact on preventing the risks of DM.
2 Methods
2.1 Search strategy
This systemic review was conducted to assess the pooled prevalence and associated factors of diabetic foot-care practices among diabetic patients in Africa. We thoroughly reviewed existing systematic reviews to avoid redundancy and conducted a detailed search for published studies across several databases, including PubMed, Cochrane Library, Google Scholar, Web of Science, African Journals Online, and Science Direct. A set of predetermined search terms was employed to facilitate a thorough search strategy that encompassed all pertinent studies. All components within the records and Medical Subject Headings were utilized to enhance the search in the advanced PubMed search interface. The search strategy was formulated and refined for various databases, utilizing essential Boolean operators in conjunction with initial keywords (“diabetes mellitus” OR “diabetic foot-care practice” OR “prevalence of diabetes” AND “associated factors” AND “Africa”). The meta-analysis was conducted following the guidelines established by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) (14) (Supplementary Table S1). All searches were limited to papers written in English and the last search in all databases was performed on the 22th July 2024.
2.2 Study selection and eligibility criteria
This research included studies involving diabetic patients and focused on the prevalence of foot-care practices and their associated factors. All studies were conducted in Africa and published in English. However, despite multiple attempts to contact the original authors via email, the current study did not include research publications that were not fully accessible. Since it was impossible to assess the articles’ content without the full texts, this omission was required. Moreover, research from which it was difficult to obtain the required data was not included in study. Furthermore, the systematic review and meta-analysis purposefully left out research from developed countries, editorial letters, reviews, communications, and systematic reviews.
2.3 Outcome measurement
The main outcome of interest was the prevalence of foot self-care practices. The secondary outcome involved the identification of factors associated with these foot-care practices among diabetic patients, which were assessed using odds ratios derived from binary outcomes reported in the primary studies included in the analysis. The key factors included in this review were education level (lower versus higher educational status), knowledge (poor versus good), and, residence (urban versus rural).
2.4 Quality assessment and data extraction
Reference management software aggregates search results from multiple databases and helps eliminate duplicate articles. The Joanna Briggs Institute’s meta-analysis tool was used for critical appraisal (15). Data extraction was performed by YAA and KAG using a standardized checklist in Microsoft Excel. For prevalence, the checklist included the author’s name, publication year, country, sub-region, and study design. For associated factors, data were organized into two-by-two tables to compute the log odds ratio for each factor. Discrepancies were resolved with a third author, BWA, to reach a consensus. YAA supervised the extraction process.
The assessment tool contains eight criteria: It was evaluated using the JBI critical appraisal checklist options of “Yes,” and “No.” The risks for biases were classified as low (total score, 5 to 8) and high (total score, 0 to 4). The study scored 50% or higher on all quality-assessed items, which were considered low-risk and included in this review. Disagreements that arose during the full-text quality assessment were resolved through evidence-based discussion
2.5 Statistical methods and analysis
Using Microsoft Excel 2010, the crucial data was collected and then transferred into Stata-14 for further examination. The I2 statistic, which shows the percentage of total variance due to heterogeneity rather than random variation, was calculated to evaluate the studies’ heterogeneity. Here, zero, twenty-five percent, fifty percent, and seventy-five percent represent no, low, moderate, and high degrees of heterogeneity, respectively.
There was significant heterogeneity among the studies, according to the test statistic (I2 = 98.4%, p < 0.000). Therefore, a random effects model was used to evaluate the overall impact of prevalence of foot-care practices. The DerSimonian-Laird weighting approach was used to generate prevalence rates and odds ratios at a 95% confidence interval. Furthermore, a subgroup analysis based on regional differences was carried out. A sensitivity analysis of the effect of a single study on the pooled prevalence from the meta-analysis was conducted. Using a subjective funnel plot and an objective Egger’s test with a 5% significance level, the publication bias was investigated. Using the odds ratio with a 95% confident interval and a significance level of 5% for the P-value, the association between foot-care practices and variables was estimated. Graphs, tables, text, and a forest plot were used to display the results.
3 Results
3.1 Search and study selection
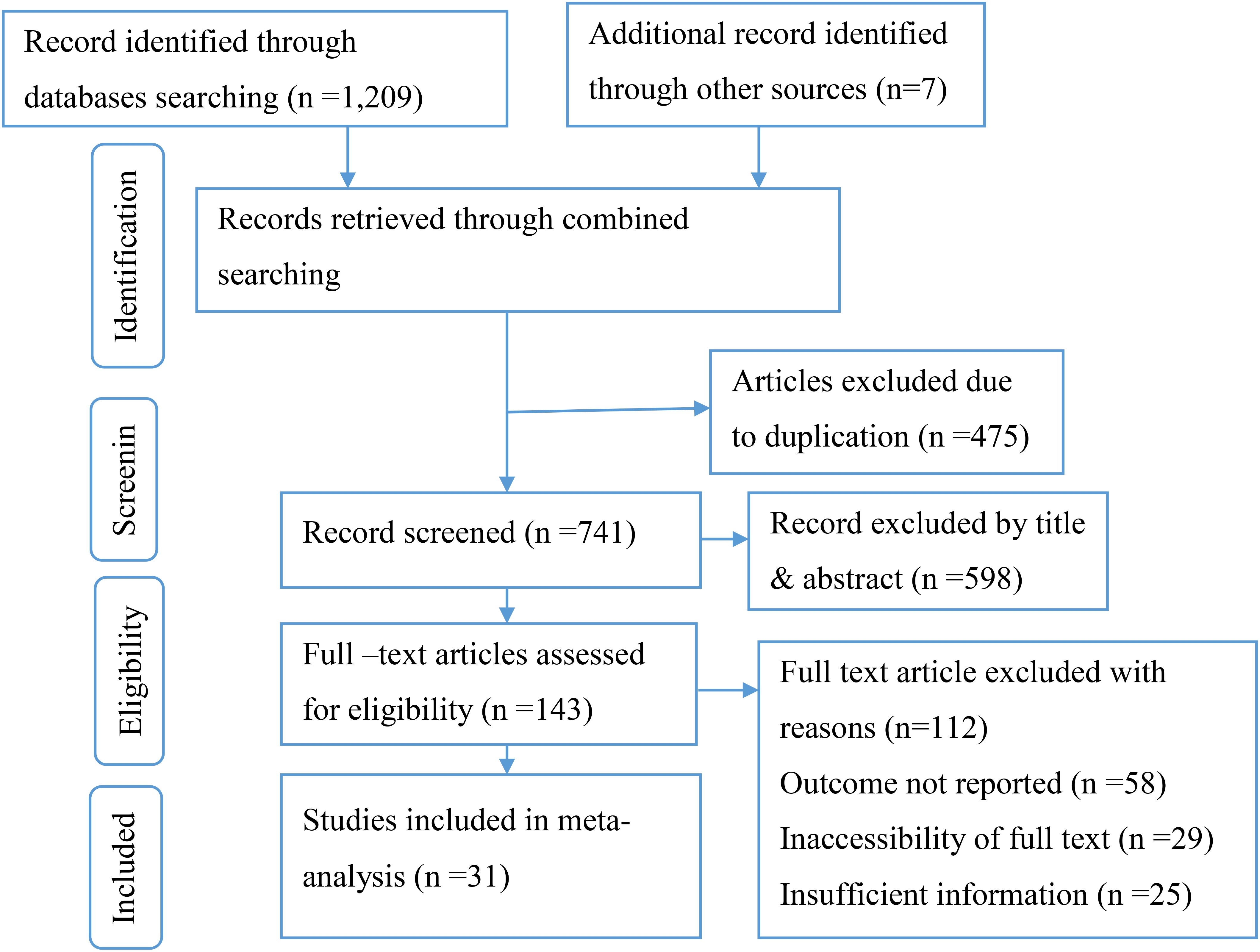
This review included published studies conducted on the prevalence of foot-care practices among diabetic patients in Africa. A total of 1,216 records were retrieved through electronic database searching. From these, 475 duplicated records were excluded, and from 741 articles screened using their titles and abstracts, 598 were excluded. 143, full-text articles were assessed for eligibility. From these, 112 full-text articles were excluded from prior criteria, and finally, 31 full-text primary articles were selected for quantitative analysis (Figure 1).
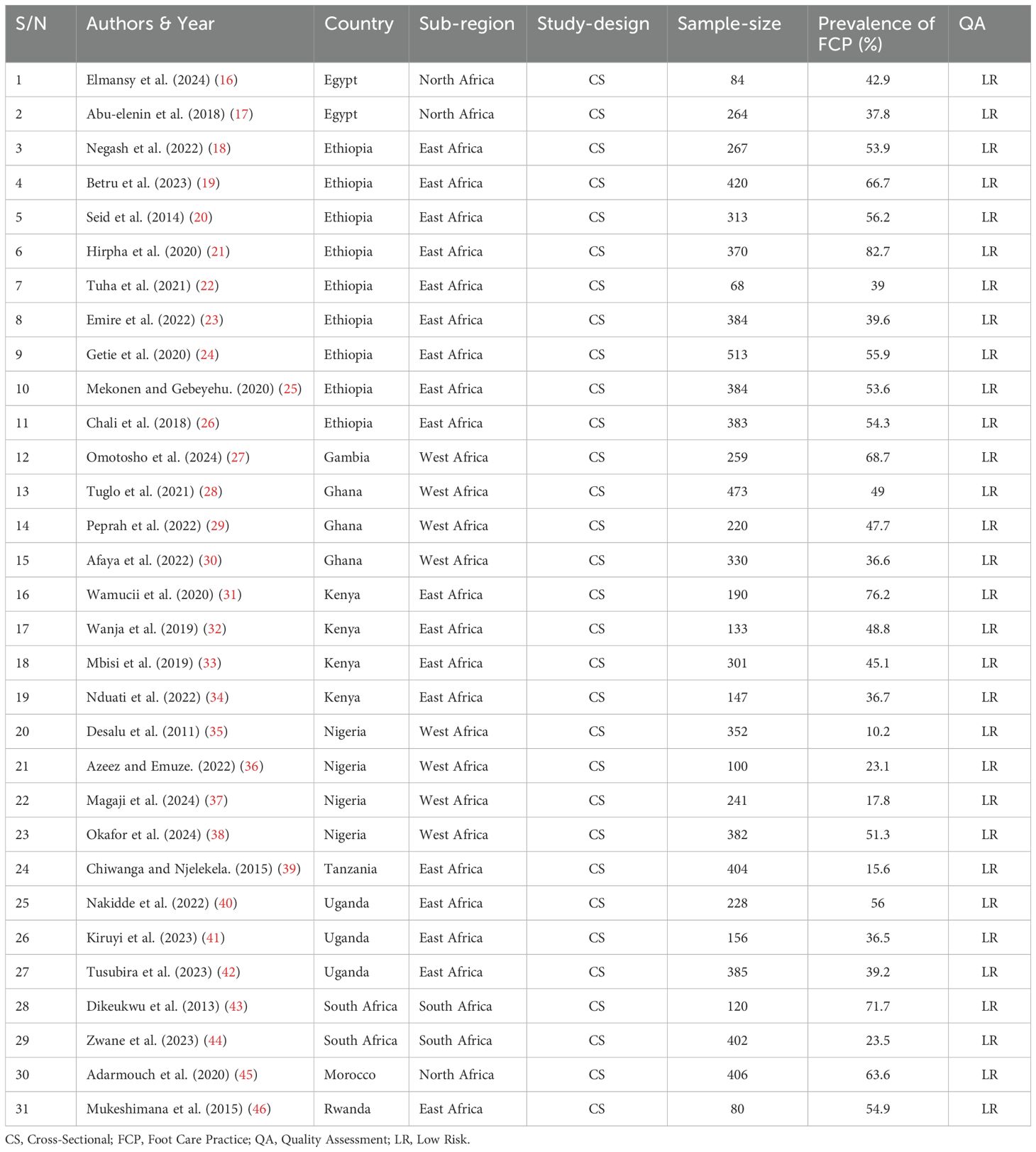
3.2 Characteristics of included studies
Thirty-one (16–46) African countries were represented in this review with a total of 8,759 diabetic patients. From all, eighteen of the studies were from eastern Africa (18–26, 31–34, 39–42, 46), eight were from western African countries (27–30, 35–38), three studies were from northern Africa (16, 17, 45), and two studies from Southern African countries (43, 44). The total sample size ranges from 68 to 513 (22, 24) (Table 1).
3.3 Pooled prevalence of diabetes foot self-care practice in Africa
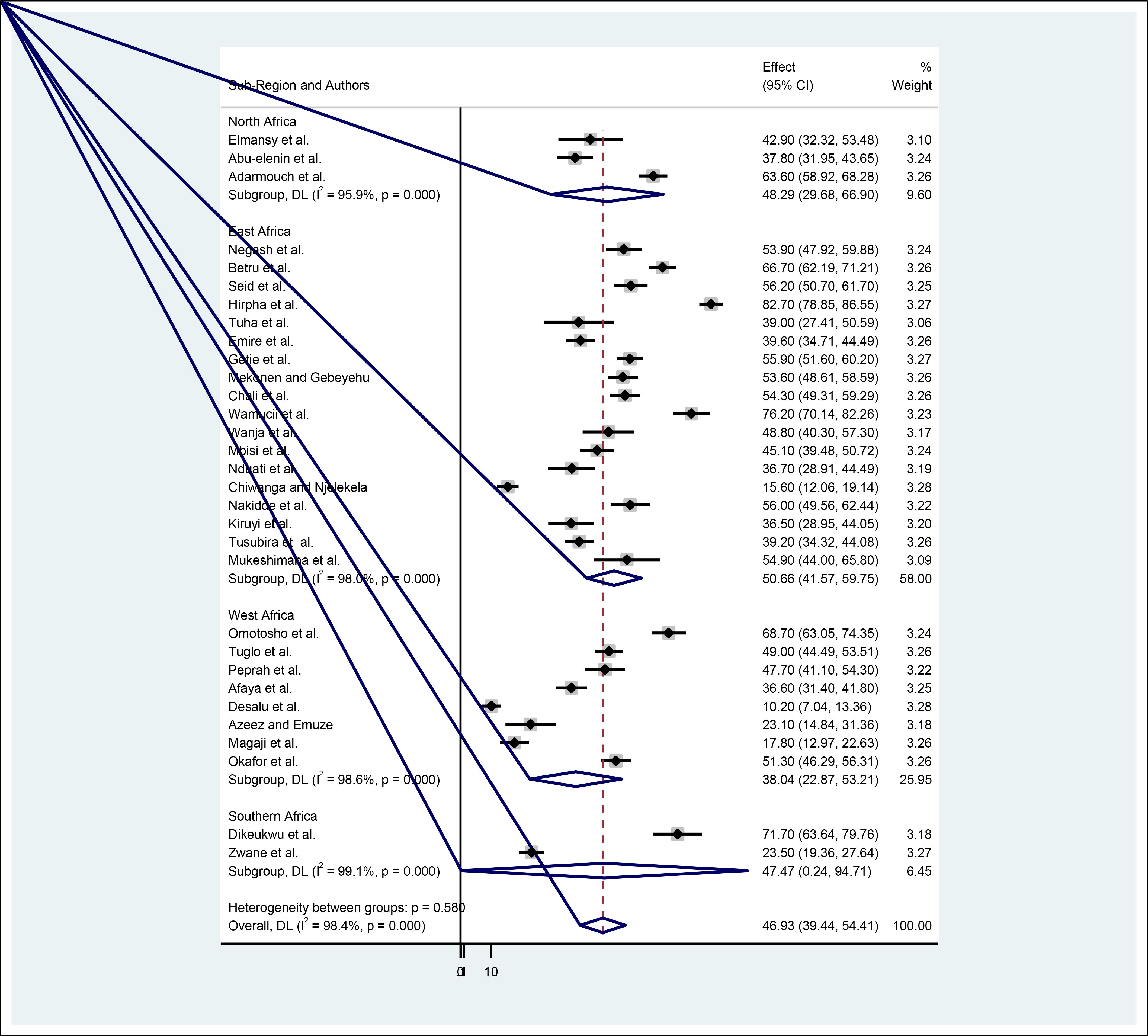
The overall pooled prevalence of diabetes foot self-care practices among diabetic patients was 46.93% (95%CI (39.44–54.41)). This estimate was statistically significant with a P value of less than 0.001. Furthermore, heterogeneity between studies was found to be high with an I2 value of 98.4%, (Figure 2).
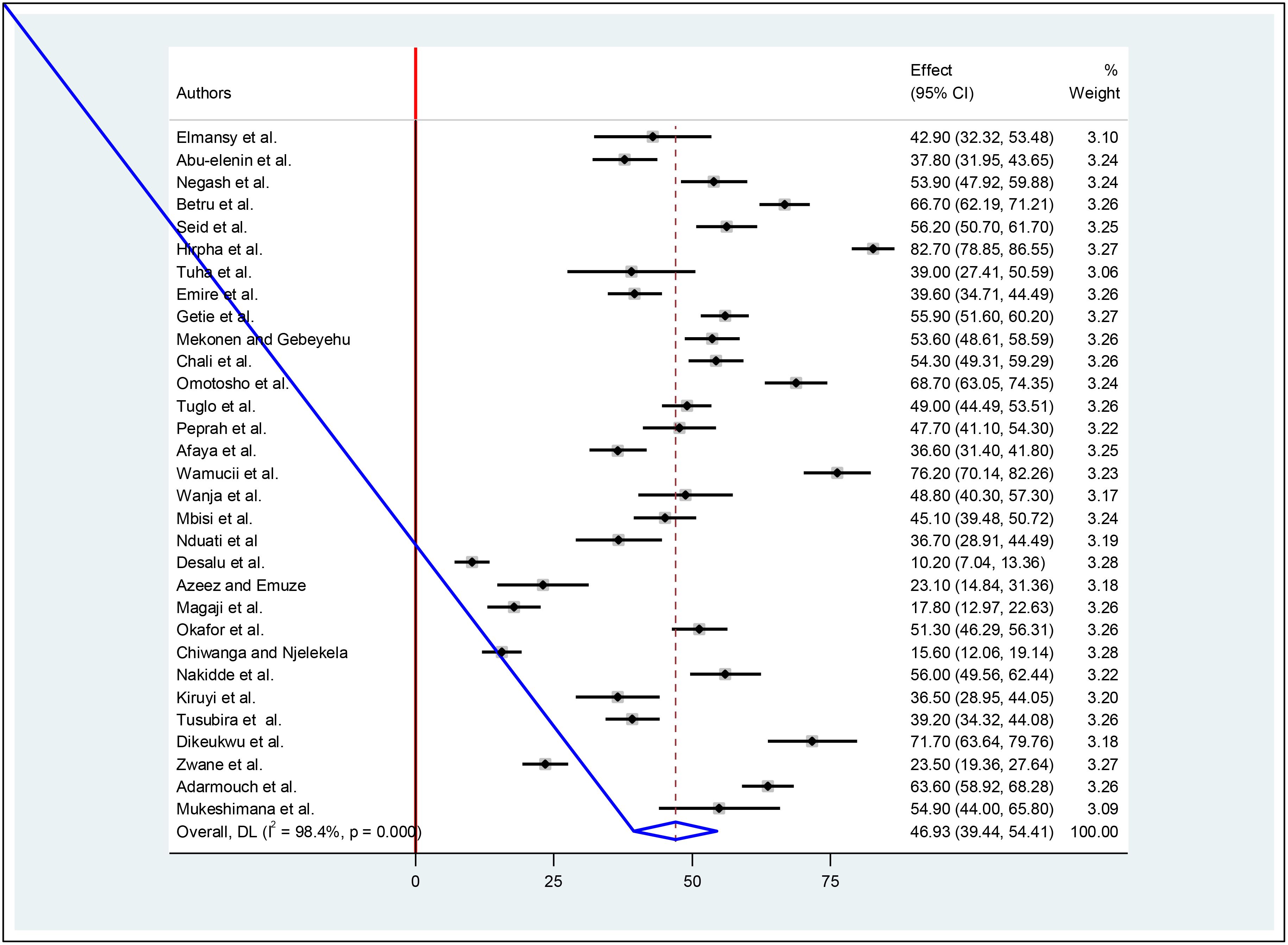
Figure 2. Forest plot of the pooled prevalence of foot self-care practices among diabetic patients in Africa.
3.4 Sub-group meta-analysis
To minimize random variations among the studies, we performed a sub-group analysis based on the regions where the studies were conducted. Based on sub-region, the highest pooled estimate of foot-care practices among diabetic patients was found in East Africa at 50.66% (95% CI: 41.57–59.75), while the lowest was in West Africa at 38.04% (95% CI: 22.87–53.21) (Figure 3).
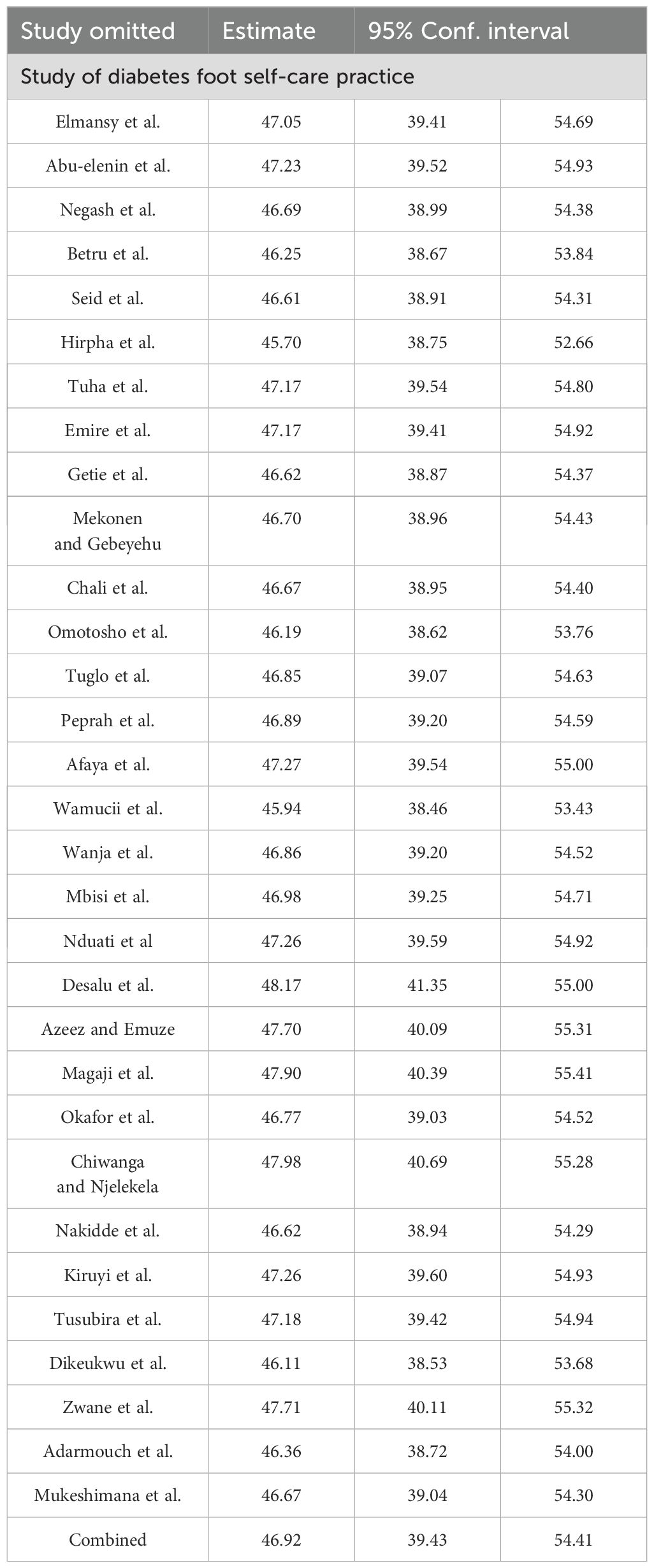
3.5 Sensitivity meta-analysis
A sensitivity analysis using a random-effects model showed that no single study significantly influenced the overall meta-analysis results. The data presented in the table show that the estimates derived from an individual study align more closely with the aggregated estimate hence; there is no significant influence of any single study on the overall findings (Table 2).
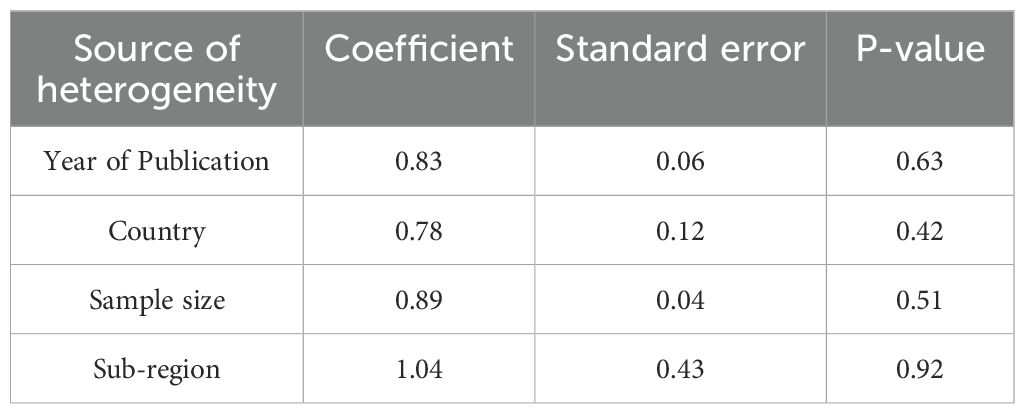
3.6 Meta-regression
A meta-regression analysis was conducted due to significant heterogeneity, with I-square values below 0.05. The aim was to identify sources of this heterogeneity for better result interpretation. However, the analysis found no significant variables related to sample size, publication year, or study sub-regions. Thus, the heterogeneity may stem from unaddressed factors (Table 3).
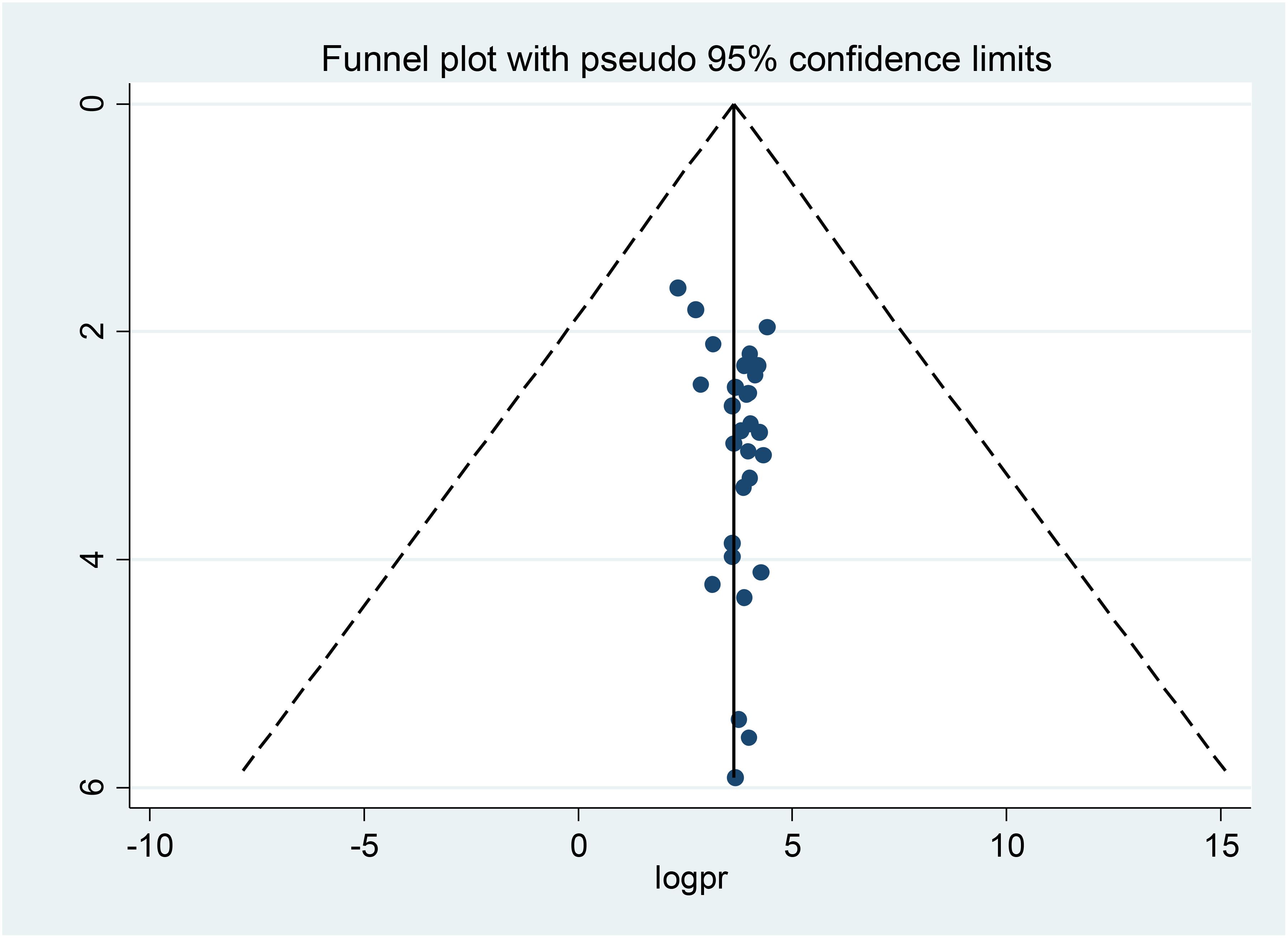
3.7 Publication bias
The distribution of foot self-care practices among diabetic patients was examined for asymmetry through a visual inspection of the forest plot presented as a funnel plot. Furthermore, Egger’s and Begg’s regression test results demonstrated the non-existence of publication bias (p=0.53), and (P=0.34) respectively (Figure 4).
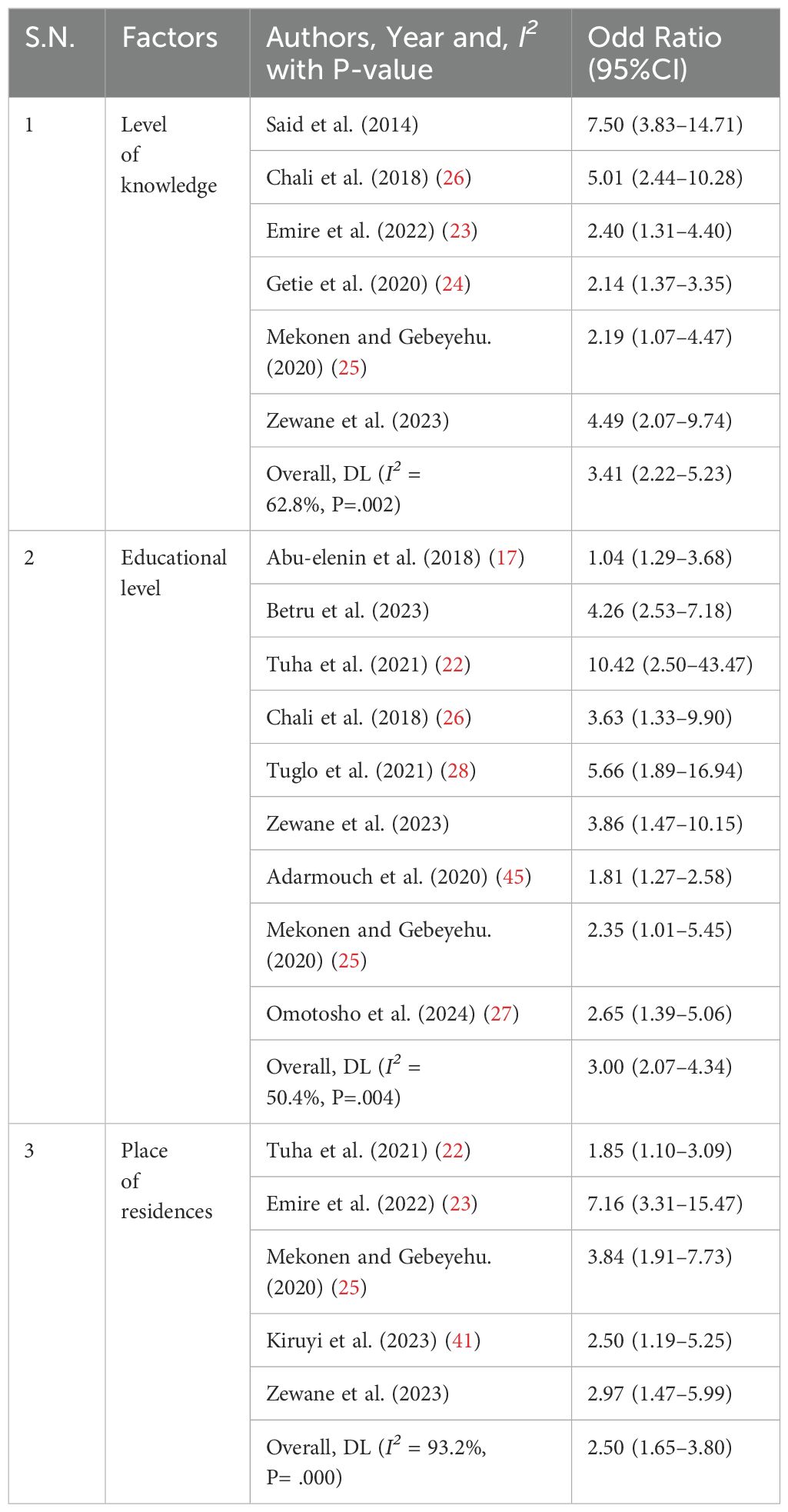
3.8 Factors associated with a diabetic foot self-care practice in Africa
A meta-analysis was conducted to determine the factors associated with foot self-care practices using a random effects model. Consequently, we analyzed the combined effect of three specific factors, knowledge, educational attainment, and place of residence on the outcome variable.
3.8.1 Association between diabetic foot self-care practice and level of knowledge
To examine the association between diabetic foot-care practices and the knowledge of participants, a total of six studies were incorporated into the meta-analysis (20, 23–26, 44). The pooled results of the meta-analysis indicated a significant association between foot self-care practices and the knowledge of participants. Consequently, diabetic patients possessing a strong understanding of foot self-care practices were found to be 3.41 times more likely to be involved in these practices compared to poor knowledge (AOR: 3.41, 95% CI (2.22–5.23)). Moderate heterogeneity was observed across studies (I2 = 62.8%, P=0.002) for this reason, we used a random effects model.
3.8.2 Association between diabetic foot self-care practice and educational level
A total of nine studies were incorporated into the meta-analysis to determine the association between diabetic foot-care practices and the level of education (17, 19, 22, 25–28, 44, 45). The studies included in the analysis indicated that individuals with a college education or higher were 3.00 times more likely to engage in diabetic foot self-care practices than those who were illiterate (AOR: 3.00, 95% CI (2.07–4.34)). Moderate heterogeneity was observed across studies (I2 = 50.4%, P = 0.004) for this reason, we used a random effects model.
3.8.3 Association between diabetic foot self-care practice and residence
To identify the association between diabetic foot-care practice and residence, five studies were included in the meta-analysis (22, 23, 25, 41, 44). Accordingly, the pooled findings of the meta-analysis showed that living in rural was significantly associated with diabetic foot-care practices. As a result, diabetic patients who were living in rural residences were 2.50 times more likely to practices foot self-care as compared to diabetic patients who live in an urban area (AOR:2.50, 95% CI (1.65–3.80)). Higher heterogeneity was observed across studies (I2 = 93.2%, P=0.001), for this reason, we used a random effects model (Table 4).
4 Discussions
This systematic review and meta-analysis was conducted in response to the insufficient evidence regarding the prevalence of good foot-care practices. The primary objective was to estimate the pooled prevalence of foot-care practices and identify the associated factors among diabetic patients in Africa. Effective self-care is crucial for the management of diabetes mellitus, encompassing various components, including foot care (47). practice of self-care is not only important to diabetic patients but also for other medical practices to reduce the direct and indirect costs of medicine (48).
In this meta-analysis, the pooled estimate of overall foot self-care practice among diabetic patients in Africa was 46.93%. The finding was consistent with a previous study conducted in Malaysia (47.8%) (49). However, this finding was much lower than studies conducted in Thailand (87%), and Iran (74%) (50, 51), and higher than the study reported in Spain (30.2%), and Turkey (29.5%) (52, 53). Cultural disparities, economic variations, lifestyle differences, unequal healthcare access, and public education levels may explain the observed differences. Additionally, diverse methodologies for assessing outcomes across countries could contribute to these discrepancies. Furthermore, the varying educational levels and understanding of diabetes foot self-care among patients in different countries likely influence the differences in diabetes foot self-care practices.
This systematic review and meta-analysis also identified factors associated with diabetic foot care practices. Diabetic patients living in rural areas were nearly three times more likely to have poor foot self-care practices than those who live in urban areas. This finding is supported by a study conducted in India (54). The possible reason for those diabetic patients in rural areas often have limited access to health education resources, leading to lower awareness of self-care practices compared to urban patients. In Africa, many rural diabetics are farmers who walk barefoot, increasing their risk of bites and injuries that can lead to foot ulcers. The lack of accessible self-care information further reduces their proactivity in addressing foot issues, heightening the risk of developing foot problems.
In addition, the current research indicates that diabetic patients with limited literacy skills and primary education were three times more likely to exhibit inadequate foot self-care practices compared to their counterparts who had attained college education or higher. Comparable results have been documented in studies carried out in Vietnam and Indonesia (55, 56). As a diabetic patient’s level of education increases, likely, their understanding of foot self-care principles will also enhance. This understanding is crucial for the prevention of diabetes mellitus, which is best managed through consistent practices of foot self-care. Furthermore, individuals with higher educational attainment are generally more inclined to seek out and comprehend information related to their condition, foot care, as well as to recognize the guidance provided by their healthcare providers.
In this study, participants who had good knowledge of foot-care practices were three times more likely to practice foot-care as compared to poorly knowledgeable. The findings of this study are further supported by a similar investigation conducted in India, which also demonstrated an association between knowledge of foot-care practices and the likelihood of engaging in such activities (54). The potential rationale for this is that effective diabetes self-care practices require the active participation of both individuals living with diabetes and healthcare professionals. This collaboration aims to enhance best practices by improving knowledge and comprehension of the condition, as well as anticipating the long-term consequences associated with the disease.
A comprehensive search strategy was used for this systematic review and meta-analysis, including both published and unpublished studies. A random-effects model was used to address the potential variability across studies. However, as a limitation, the results of this study should be interpreted by considering possible limitations, such as the restriction of studies written in English limited the number of studies included in a meta-analysis and the limited number of studies conducted in Africa may hinder the ability to generalize findings to the entire population. This review exhibited significant interestedly heterogeneity, which could not be addressed through subgroup analysis. Additionally, all included studies were cross-sectional, which may have introduced confounding factors that weaken the causal inferences about the relationship between foot self-care practices and associated factors.
5 Conclusions
In conclusion, more than half of diabetic patients had poor diabetes foot self-care practices. Due to having low educational status, living in a rural area, and a level of knowledge among diabetic patients. It is better to give health education to diabetic patients and their caregivers about the basic principles of diabetes foot care, like regular inspection of the feet and appropriate footwear, as well as how to encourage diabetic patients to adhere to foot self-care practices at their regular follow-up time.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
YA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. BA: Data curation, Formal Analysis, Investigation, Software, Validation, Visualization, Writing – original draft. KG: Conceptualization, Methodology, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We would like to express our gratitude to the investigators of primary studies and the database owners.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2025.1527402/full#supplementary-material
References
1. Association AD. Diagnosis and classification of diabetes mellitus. Diabetes Care. (2014) 37:S81–90. doi: 10.2337/dc14-S081
2. Bus SA, Lavery LA, Monteiro-Soares M, Rasmussen A, Raspovic A, Sacco IC, et al. Guidelines on the prevention of foot ulcers in persons with diabetes (IWGDF 2019 update). Diabetes/metabolism Res Rev. (2020) 36:e3269. doi: 10.1002/dmrr.v36.S1
3. Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge A, et al. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Practice. (2018) 138:271–81. doi: 10.1016/j.diabres.2018.02.023
4. Mutyambizi C, Pavlova M, Chola L, Hongoro C, and Groot W. Cost of diabetes mellitus in Africa: a systematic review of existing literature. Globalization Health. (2018) 14:1–13. doi: 10.1186/s12992-017-0318-5
5. Bakker K, Apelqvist J, and Schaper NC. Practical guidelines on the management and prevention of the diabetic foot 2011. Diabetes/metabolism research and reviews. Board IWGotDFE. (2012) 28:225–31.
6. Alexiadou K and Doupis J. Management of diabetic foot ulcers. Diabetes Ther. (2012) 3:1–15. doi: 10.1007/s13300-012-0004-9
7. Armstrong DG, Cohen K, Courric S, Bharara M, and Marston W. Diabetic foot ulcers and vascular insufficiency: our population has changed, but our methods have not. J Diabetes Sci Technol. (2011) 5:1591–5. doi: 10.1177/193229681100500636
8. Zhang P, Lu J, Jing Y, Tang S, Zhu D, and Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis. Ann Med. (2017) 49:106–16. doi: 10.1080/07853890.2016.1231932
9. Jinadasa CVM and Jeewantha M. SP5–14 A study to determine the knowledge and practice of foot care in patients with chronic diabetic ulcers. J Epidemiol Community Health. (2011) 65:A449–A. doi: 10.1136/jech.2011.142976p.50
10. Schaper NC, van Netten JJ, Apelqvist J, Bus SA, Hinchliffe RJ, Lipsky BA, et al. Practical guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update). Diabetes/metabolism Res Rev. (2020) 36:e3266. doi: 10.1002/dmrr.v36.S1
11. Shaki O, Gupta GK, Rai SK, Gupta TP, Kumar RV, Upreti V, et al. Awareness regarding foot self-care practices among diabetic patients in Northeast part of India. Can primary care physician make a difference? A hospital based cross-sectional study. J Family Med Primary Care. (2022) 11:1834–41. doi: 10.4103/jfmpc.jfmpc_1883_21
12. Edmonds M, Manu C, and Vas P. The current burden of diabetic foot disease. J Clin Orthopaed Trauma. (2021) 17:88–93. doi: 10.1016/j.jcot.2021.01.017
13. Muhammad-Lutfi A, Zaraihah M, and Anuar-Ramdhan I. Knowledge and practice of diabetic foot care in an in-patient setting at a tertiary medical center. Malaysian Orthopaedic J. (2014) 8:22. doi: 10.5704/MOJ.1411.005
14. Moher D, Liberati A, Tetzlaff J, and Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Internal Med. (2009) 151:264–9. doi: 10.7326/0003-4819-151-4-200908180-00135
15. Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. Checklist for analytical cross sectional studies. Joanna Briggs Institute Reviewer’s Manual. (2017) 6.
16. El Mansy FM and Elbaqry MG. Self-care knowledge, attitude, and practice among diabetic foot patients: A cross-sectional research. Zagazig Nurs J. (2024) 20:168–83. doi: 10.21608/znj.2024.343681
17. Abu-elenin MM, Elshoura AA, and Alghazaly GM. Knowledge, practice and barriers of foot self-care among diabetic patients at Tanta University Hospitals, Egypt. Egypt J Commun Med. (2018) 36:94–102. doi: 10.21608/ejcm.2018.23001
18. Negash W, Assefa T, Sahiledengle B, Tahir A, Regassa Z, Feleke Z, et al. Prevalences of diabetic foot ulcer and foot self-care practice, and associated factors in adult patients with diabetes in south-east Ethiopia. J Int Med Res. (2022) 50:03000605221129028. doi: 10.1177/03000605221129028
19. Berisso Y, Wondirad M, and Tefera K. Prevalence and factors associated with suboptimal foot self-care practices among adult diabetic patients in governmental hospitals in Hawassa city, Sidama Region, Ethiopia: A cross-sectional study. Ethiopian J Med Health Sci. (2023) 3:264–77.
20. Seid A and Tsige Y. Knowledge, practice, and barriers of foot care among diabetic patients attending Felege Hiwot Referral Hospital, Bahir Dar, Northwest Ethiopia. Adv Nursing. (2015) 2015:934623. doi: 10.1155/2015/934623
21. Hirpha N, Tatiparthi R, and Mulugeta T. Diabetic foot self-care practices among adult diabetic patients: a descriptive cross-sectional study. Diabetes Metab Syndrome Obes. (2020), 4779–86. doi: 10.2147/DMSO.S285929
22. Tuha A, Getie Faris A, Andualem A, and Ahmed Mohammed S. Knowledge and practice on diabetic foot self-care and associated factors among diabetic patients at Dessie referral hospital, northeast Ethiopia: mixed method. Diabetes Metab Syndrome Obes. (2021), 1203–14. doi: 10.2147/DMSO.S300275
23. Emire MS, Zewudie BT, Tarekegn TT, GebreEyesus FA, Amlak BT, Mengist ST, et al. Self-care practice and its associated factors among diabetic patients attending public hospitals in Gurage zone southwest, Ethiopia. PLoS One. (2022) 17:e0271680. doi: 10.1371/journal.pone.0271680
24. Getie A, Geda B, Alemayhu T, Bante A, Aschalew Z, and Wassihun B. Self-care practices and associated factors among adult diabetic patients in public hospitals of Dire Dawa administration, Eastern Ethiopia. BMC Public Health. (2020) 20:1–8. doi: 10.1186/s12889-020-09338-5
25. Mekonen EG and Gebeyehu Demssie T. Preventive foot self-care practice and associated factors among diabetic patients attending the university of Gondar comprehensive specialized referral hospital, Northwest Ethiopia, 2021. BMC Endocr Disord. (2022) 22:124. doi: 10.1186/s12902-022-01044-0
26. Chali SW, Salih MH, and Abate AT. Self-care practice and associated factors among Diabetes Mellitus patients on follow up in Benishangul Gumuz Regional State Public Hospitals, Western Ethiopia: a cross-sectional study. BMC Res notes. (2018) 11:1–8. doi: 10.1186/s13104-018-3939-8
27. Omotosho TOA, Sanyang Y, and Senghore T. Diabetic foot self-care knowledge and practice among patients with diabetes attending diabetic clinic in the Gambia. Int Wound J. (2024) 21:e14963. doi: 10.1111/iwj.14963
28. Tuglo LS, Nyande FK, Agordoh PD, Nartey EB, Pan Z, Logosu L, et al. Knowledge and practice of diabetic foot care and the prevalence of diabetic foot ulcers among diabetic patients of selected hospitals in the Volta Region, Ghana. Int Wound J. (2022) 19:601–14. doi: 10.1111/iwj.13656
29. Peprah MO, Ogbordjor WD, Danquah M, Yeboah HN, Anchirinah BKI, and Adomako EK. Self-Care Practices and Drivers of Anti-Diabetic Type 2 Medication Non-Compliance among Patients Accessing Healthcare at a Health Facility in Ghana. Asian J Med Health. (2022) 20:130–43. doi: 10.9734/ajmah/2022/v20i12776
30. Afaya RA, Bam V, Lomotey AY, and Afaya A. Clinical factors influencing knowledge and self-care practice among adults with type 2 diabetes mellitus. Nurs Open. (2023) 10:2492–500. doi: 10.1002/nop2.v10.4
31. Wamucii EG, Kiage B, and Kyallo F. knowledge and self-care practices among diabetic patients-a case study of thika level 5 hospital, Kenya. J Health Med Nursing. (2020) 5:25–43. doi: 10.47604/jhmn.1180
32. Wanja L, Mwenda C, Mbugua R, and Njau S. Determinants of foot self-care practices among diabetic patients attending diabetic clinic at a referral hospital, Meru County-Kenya. Int J Sci Res Public. (2019) 9:9461. doi: 10.29322/IJSRP.9.10.2019.p9461
33. Mbisi AM, Gitonga LK, and Kiruki S. Foot care practices among type 2 diabetics mellitus patients attending diabetes clinics in Embu County, Kenya. Open J Clin Diagn. (2019) 9:126. doi: 10.4236/ojcd.2019.94009
34. Nduati JN, Gatimu SM, and Kombe Y. Diabetic foot risk assessment among patients with type 2 diabetes in Kenya. East Afr Health Res J. (2022) 6:196. doi: 10.24248/eahrj.v6i2.698
35. Desalu O, Salawu F, Jimoh A, Adekoya A, Busari O, and Olokoba A. Diabetic foot care: self reported knowledge and practice among patients attending three tertiary hospital in Nigeria. Ghana Med J. (2011) 45. doi: 10.4314/gmj.v45i2.68930
36. Azeez TA and Emuze ME. Foot care practices among patients with diabetes mellitus in south-western Nigeria. APIK J Internal Med. (2022) 10:17–21. doi: 10.4103/ajim.ajim_2_21
37. Magaji HY, Olawumi AL, Ogunyele TT, Umar AI, Michael GC, and Grema BA. Influence of family function on self-care practice among type 2 diabetes patients in a primary care clinic in northern Nigeria. Nigerian J Basic Clin Sci. (2024) 21:137–44. doi: 10.4103/njbcs.njbcs_3_24
38. Okafor CN, Okonkwo UP, Ani KU, Onuora EO, Nwokike M, Byabagambi JT, et al. Self-care practices and the associated socio-demographic variables of persons with type 2 diabetes mellitus (T2dm) in southeast, Nigeria. Nutr Metab Insights. (2024) 17:11786388241233534. doi: 10.1177/11786388241233534
39. Chiwanga FS and Njelekela MA. Diabetic foot: prevalence, knowledge, and foot self-care practices among diabetic patients in Dar es Salaam, Tanzania–a cross-sectional study. J foot ankle Res. (2015) 8:1–7. doi: 10.1186/s13047-015-0080-y
40. Nakidde G, Kamoga R, Katushabe E, Luwaga R, and Mwanja MM. Knowledge and Practices of Self-Care among People with Diabetes in South Western Uganda: A Cross-Sectional Study at a Regional Referral Hospital in Mbarara City. Diabetes self-care knowledge Pract Mbarara city. Student’s J Health Res Afr. (2022) 3:14–.
41. Kiruyi S, Kalidi R, Mukooza EK, Walusimbi D, Higenyi E, Ansiima S, et al. Adherence to Self-care Practices among Diabetes Mellitus Patients at a Tertiary Hospital in Eastern Uganda. Hospital. (2023) 27:28. doi: 10.21522/TIJPH.2013.11.02.Art027
42. Tusubira AK, Ssinabulya I, Kalyesubula R, Nalwadda CK, Akiteng AR, Ngaruiya C, et al. Self-care and healthcare seeking practices among patients with hypertension and diabetes in rural Uganda. PloS Global Public Health. (2023) 3:e0001777. doi: 10.1371/journal.pgph.0001777
43. Dikeukwu R and Omole OB. Awareness and practices of foot self-care in patients with diabetes at Dr Yusuf Dadoo district hospital, Johannesburg. J Endocrinol Metab Diab South Africa. (2013) 18:112–8. doi: 10.1080/22201009.2013.10872314
44. Zwane J, Modjadji P, Madiba S, Moropeng L, Mokgalaboni K, Mphekgwana PM, et al. Self-management of diabetes and associated factors among patients seeking chronic care in tshwane, South Africa: A facility-based study. Int J Environ Res Public Health. (2023) 20:5887. doi: 10.3390/ijerph20105887
45. Adarmouch L, Sebbani M, Dahmash L, and Amine M. Self-care activities among patients with type 2 diabetes in Morocco: prevalence and determinants. Open J Epidemiol. (2020) 10:55–65. doi: 10.4236/ojepi.2020.101005
46. Mukeshimana M, Hakizimana G, Mwali C, Umuhoza C, Uwambajimana J, and Asingizwe D. The knowledge and practice of self-care management among patients attending a diabetes clinic in Kigali, Rwanda. Rwanda J. (2015) 2:24–30. doi: 10.4314/rj.v2i1.3F
47. Shrivastava SR, Shrivastava PS, and Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metab Disord. (2013) 12:1–5. doi: 10.1186/2251-6581-12-14
48. Organization WH. Self-care in the context of primary health care. In: WHO regional office for south-east asia. South-East Asia: WHO Regional Office. (2009).
49. Tan MY and Magarey J. Self-care practices of Malaysian adults with diabetes and sub-optimal glycaemic control. Patient Educ counseling. (2008) 72:252–67. doi: 10.1016/j.pec.2008.03.017
50. Kaehaban S, Hongsranagon P, and Havanond P. Factors influencing self-care behaviors of diabetic patients in Diabetes Mellitus Clinic, Changhan Hospital, Roi et Province. Thailand: Chulalongkorn University (2009).
51. Yekta Z, Pourali R, Aghassi MR, Ashragh N, Ravanyar L, and RAHIM PMY. Assessment of self-care practice and its associated factors among diabetic patients in urban area of Urmia, Northwest of Iran. J Res Health Sci. (2011) 1(1):33–8.
52. González-de la Torre H, Quintana-Lorenzo ML, Lorenzo-Navarro A, Suárez-Sanchez JJ, Berenguer-Pérez M, and Verdú-Soriano J. Diabetic foot self-care and concordance of 3 diabetic foot risk stratification systems in a basic health area of Gran Canaria. Enfermería Clínica (English Edition). (2020) 30:72–81. doi: 10.1016/j.enfcle.2019.07.012
53. Karadağ FY, Saltoğlu N, Ak ÖChecktae, Aydın GC, Şenbayrak S, Erol S, et al. Foot self-care in diabetes mellitus: evaluation of patient awareness. Primary Care diabetes. (2019) 13:515–20. doi: 10.1016/j.pcd.2019.06.003
54. Pavithra H, Akshaya KM, Nirgude AS, and Balakrishna A. Factors associated with awareness and practice about foot care among patients admitted with diabetes mellitus: A cross sectional research from a medical college hospital of southern India. Nepal J Epidemiol. (2020) 10:897. doi: 10.3126/nje.v10i3.29213
55. Sen HTN, Visudtibhan PJ, and Siripitayakunkit A. Factors related to foot care behaviors among patients with type 2 diabetes mellitus in Da Nang, Vietnam. Ramathibodi Med J. (2019) 42:57–68. doi: 10.33165/rmj.2019.42.3.162035
Keywords: Africa, associated factors, diabetic patients, foot-care practices, systematic review
Citation: Atalay YA, Alemie BW and Gelaw KA (2025) Prevalence and associated factors of foot self-care practice among diabetic patients in Africa: systematic review and meta-analysis. Front. Endocrinol. 16:1527402. doi: 10.3389/fendo.2025.1527402
Received: 13 November 2024; Accepted: 21 May 2025;
Published: 04 June 2025.
Edited by:
José Luis Lázaro Martínez, Complutense University of Madrid, SpainReviewed by:
Ozden Gokdemir, İzmir University of Economics, TürkiyeAjay Vikram Singh, Federal Institute for Risk Assessment (BfR), Germany
Copyright © 2025 Atalay, Alemie and Gelaw. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yibeltal Assefa Atalay, eWliZWx0YWxhc3NlZmExMkBnbWFpbC5jb20=
†ORCID: Yibeltal Assefa Atalay, orcid.org/0009-0009-3252-8161
 Yibeltal Assefa Atalay
Yibeltal Assefa Atalay Bersufekad Wubie Alemie
Bersufekad Wubie Alemie Kelemu Abebe Gelaw
Kelemu Abebe Gelaw