- 1University of Trieste, Trieste, Italy
- 2Institute for Maternal and Child Health IRCCS “Burlo Garofolo”, Trieste, Italy
Introduction: The COVID-19 pandemic disrupted healthcare systems, affecting consultations and diagnostics. In pediatric endocrinology, referral patterns shifted, with increased central precocious puberty (CPP) diagnoses and decreased growth hormone deficiency (GHD) evaluations. This study examines trends in stimulation tests, referrals, and diagnoses from 2019 to 2023 to assess the pandemic’s impact on pediatric endocrinology.
Methods: This retrospective study analyzed stimulation tests performed at the Institute for Maternal and Child Health IRCCS “Burlo Garofolo,” Trieste, Italy, from 2019 to 2023, divided into pre-pandemic (2019–March 2020), pandemic (March 2020–January 2022), and post-pandemic (February 2022–December 2023) phases.
Results: A total of 1,526 tests were conducted on 1,042 patients. Tests per day remained stable (pre-pandemic: 0.84; pandemic: 0.82; post-pandemic: 0.85). The Arginine Stimulation Test (ATT), the most frequent test pre-pandemic (31%), decreased during the pandemic (20%, p<0.001), while the LHRH Test (LHRHT) increased from 22% to 28% (p<0.001), becoming the most requested test. Diagnosis rates for GHD and CPP remained stable, but the proportion of females diagnosed with CPP increased significantly during the pandemic (91% vs. 69%, p=0.022). CPP testing declined (p=0.018) post-pandemic, while GHD testing returned to pre-pandemic levels.
Conclusion: The pandemic altered diagnostic patterns, with reduced GHD evaluations reflecting limited healthcare access. Post-pandemic recovery suggests a resolution of diagnostic delays. The temporary surge in CPP cases, likely influenced by pandemic-related lifestyle changes, subsided post-pandemic, aligning with pre-pandemic trends. To date, no other studies have reported similar variations in GHD incidence during the pandemic.
Introduction
The COVID-19 pandemic significantly impacted healthcare systems, leading to a substantial reduction in medical consultations, both in emergency rooms and outpatient clinics (1, 2). In pediatrics, this was largely due to parental fears of viral exposure (3, 4).
In pediatric endocrinology, approximately half of initial referrals are typically related to the evaluation of short stature or early puberty (5). During the pandemic, changes in referral patterns and diagnoses have been described. In particular, many centers have noticed an important increase in referrals and diagnoses of central precocious puberty (CPP) in girls since the early months of 2020 (6); since puberty onset is regulated by both genetic and environmental factors, several potential triggers—such as stress and sudden lifestyle changes (e.g., increased screen time, dietary variations, altered sleep habits)—have been hypothesized to contribute to this trend (7–12). Parents also may have observed pubertal signs more readily while spending more time at home. In contrast, referrals for short stature and diagnoses of growth hormone deficiency (GHD) decreased, likely due to postponed pediatric visits (13).
In the following years, the improvement of containment measures and the development of the anti-SARS-CoV-2 vaccination campaign enabled the gradual resumption of routine hospital activities (14), eventually returning to pre-pandemic levels. However, it remained unclear whether diagnostic patterns previously reported in pediatric endocrinology returned to pre-pandemic trends or persisted, potentially exhibiting a “dragging” effect.
This study aimed to assess the evolution of stimulation tests and endocrine diagnoses from 2019 to 2023, focusing on the persistence or reversal of pandemic-related changes, especially in CPP and GHD.
Materials and methods
We conducted a retrospective study at the Institute for Maternal and Child Health IRCCS “Burlo Garofolo” in Trieste, Italy, a tertiary hospital and research institute that serves as a pediatric referral center for the province of Trieste and as a national reference hospital.
All records of children and adolescents who underwent a stimulation test from January 1, 2019, to December 31, 2023, were reviewed. To better understand how the pandemic impacted the frequency and distribution of tests and diagnoses, we categorized the analyzed five-year period (2019–2023) into three distinct time intervals:
- the pre-pandemic period: January 1, 2019, to March 7, 2020 (the day before the nationwide lockdown in Italy) (15);
- the pandemic period: March 8, 2020, to January 31, 2022, during which hospital access was restored (16), allowing the return to daily activities even for individuals without a “Green Pass”;
- the post-pandemic period: February 1, 2022, to December 31, 2023.
Since these three periods differ in duration, corrections were applied based on the number of days in each period to ensure a standardized comparison of test frequencies and diagnoses.
To access all patients’ data, we used the “G2 Clinico” platform (a management system for specialist activities). We collected information on age at presentation, sex, height Standard Deviation Score (SDS), BMI SDS, reasons for referral, type and number of tests performed, test results, and final diagnosis, as previously described (17).
Ethical Committee approval was not required, as the General Authorization to Process Personal Data for Scientific Research Purposes (Authorization no. 9/2014) states that retrospective archive studies using ID codes, which prevent data from being traced back directly to the subject, do not need ethics approval (18).
Parents provided informed consent at the first visit, agreeing that “clinical data may be used for clinical research purposes, epidemiology, the study of pathologies, and training, to improve knowledge, care, and prevention.”
The statistical analyses were primarily descriptive. Data were presented as absolute and percentage frequencies and were described using means or medians and interquartile ranges (IQRs), depending on their distribution. The two-proportions Z-test was used to evaluate associations between two proportions, while Mood’s median test was applied to assess differences in the medians of two groups for continuous variables. All tests were two-tailed, and a p-value <0.05 was considered statistically significant. Analyses were performed using R 4.4.2 (2024, R Core Team, Vienna, Austria).
Results
Over the five-year study period, a total of 1,526 stimulation tests were performed on 1,042 individuals, 55% of whom were female. Among these, 270 individuals (26%) underwent more than one test. The year with the lowest number of tests was 2020, with 266 tests, while the highest numbers were recorded in 2021 and 2023, with 328 tests each. Overall, 474 tests (31%) yielded pathological results.
The most frequently performed test overall was the Arginine Tolerance Test (ATT), accounting for 367 tests (24%), followed by the Luteinizing Hormone-Releasing Hormone Test (LHRHT) (n = 346, 23%), the Standard Dose Synacthen Test (SDST) (n = 309, 20%), and the Insulin Tolerance Test (ITT) (n = 290, 19%).
The primary reasons for performing stimulation tests included short stature (370 tests, 24%, as the first stimulation test; 163 tests, 11%, as a second stimulation test), precocious pubarche (n = 309, 20%), and precocious puberty (n = 252, 16%).
Trends in stimulation tests over time
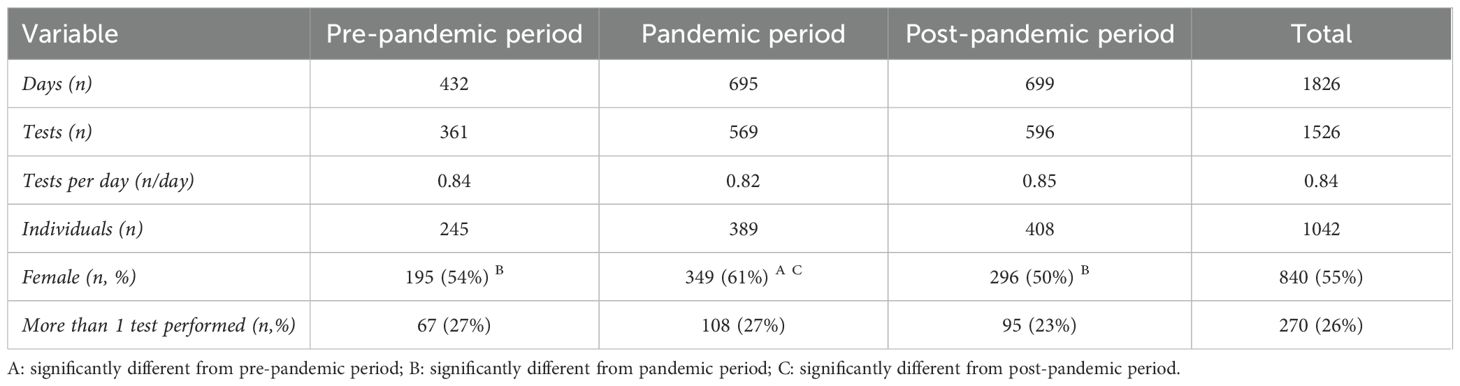
Analyzing the three time periods described above, we observed a stable trend in the number of tests performed (Table 1):
- in the pre-pandemic period, a total of 361 tests were conducted over 432 days, corresponding to an average of 0.84 tests per day.
- during the pandemic period, 569 tests were performed across 695 days, resulting in an average of 0.82 tests per day.
- in the post-pandemic period, 596 tests were conducted over 699 days, with an average of 0.85 tests per day.
Given the differences in duration among the three periods, corrections were applied based on the number of days in each period to ensure a standardized comparison of test frequencies and diagnoses.
Period-to-period comparisons of the average number of tests per day showed no significant differences, indicating that despite the restrictions, our service continued to provide consistent clinical care. The distribution of stimulation tests and pathological responses is reported in Table 2.
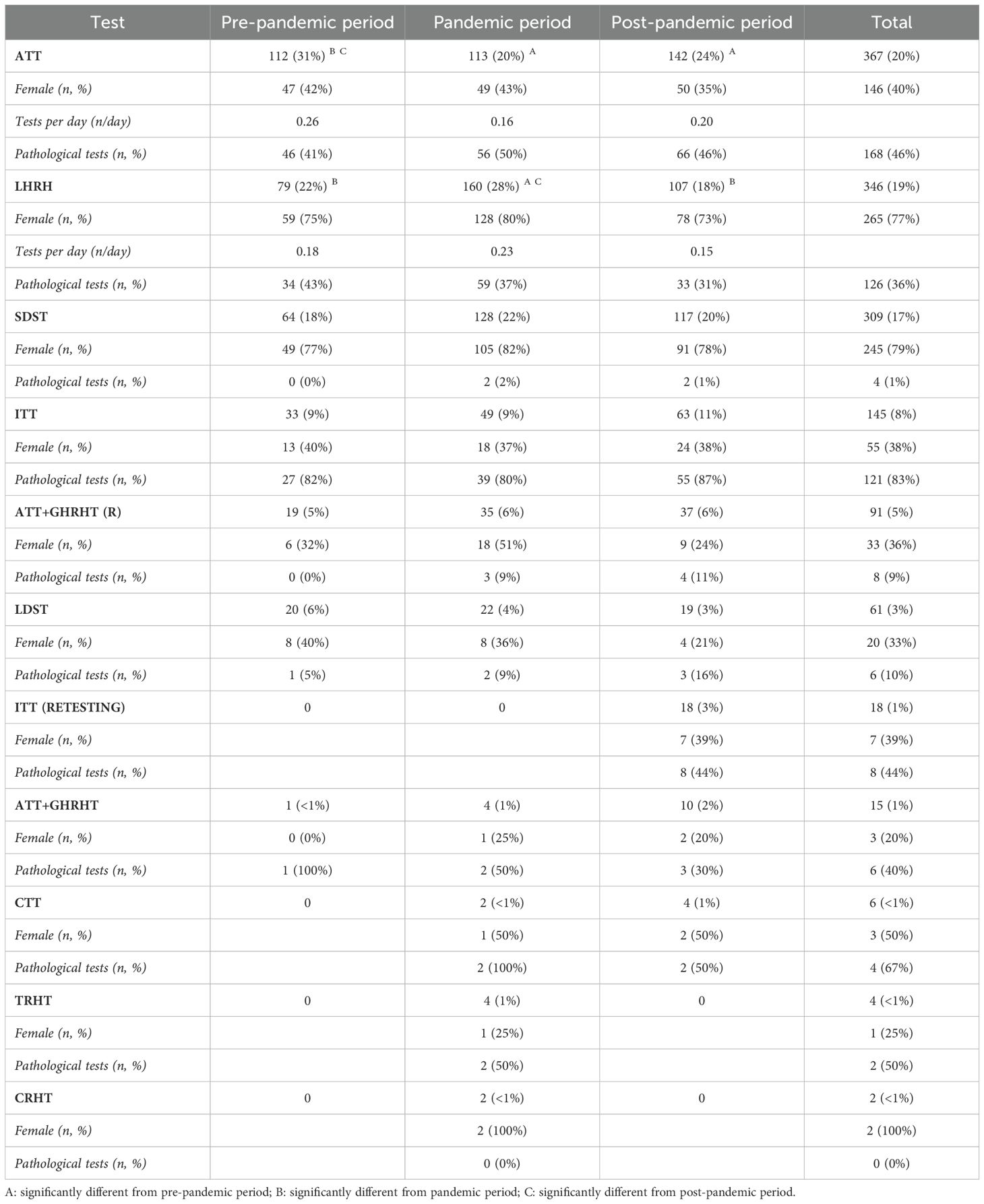
Table 2. Distribution of stimulation test conducted from 2019 to 2023 and rate of pathological response.
Changes in test distribution
- In the pre-pandemic period, the most frequently conducted test was the ATT (n = 112, 31%), followed by the LHRHT (n = 79, 22%) and the SDST (n = 64, 18%).
- During the pandemic period, we observed a shift in this trend: the most commonly performed test was the LHRHT (n = 160, 28%), followed by the SDST (n = 128, 22%) and the ATT (n = 113, 20%).
- In the post-pandemic period, the ATT returned as the most frequently conducted test (n = 142, 24%), followed by the SDST (n = 117, 20%) and the LHRHT (n = 107, 18%).
The proportion of ATT tests relative to the total number of tests significantly decreased during the pandemic compared to the pre-pandemic period (from 31% to 20%, p < 0.001) and remained significantly lower in the post-pandemic period compared to pre-pandemic levels (31% to 24%, p = 0.018).
Conversely, the proportion of LHRHT tests increased significantly during the pandemic compared to the pre-pandemic period (22% to 28%, p = 0.041) and remained significantly higher in the pandemic period compared to the post-pandemic period (18%, p < 0.001), while there was no significant difference between the pre-pandemic and post-pandemic periods (22% to 18%, p = 0.160) (Figure 1).
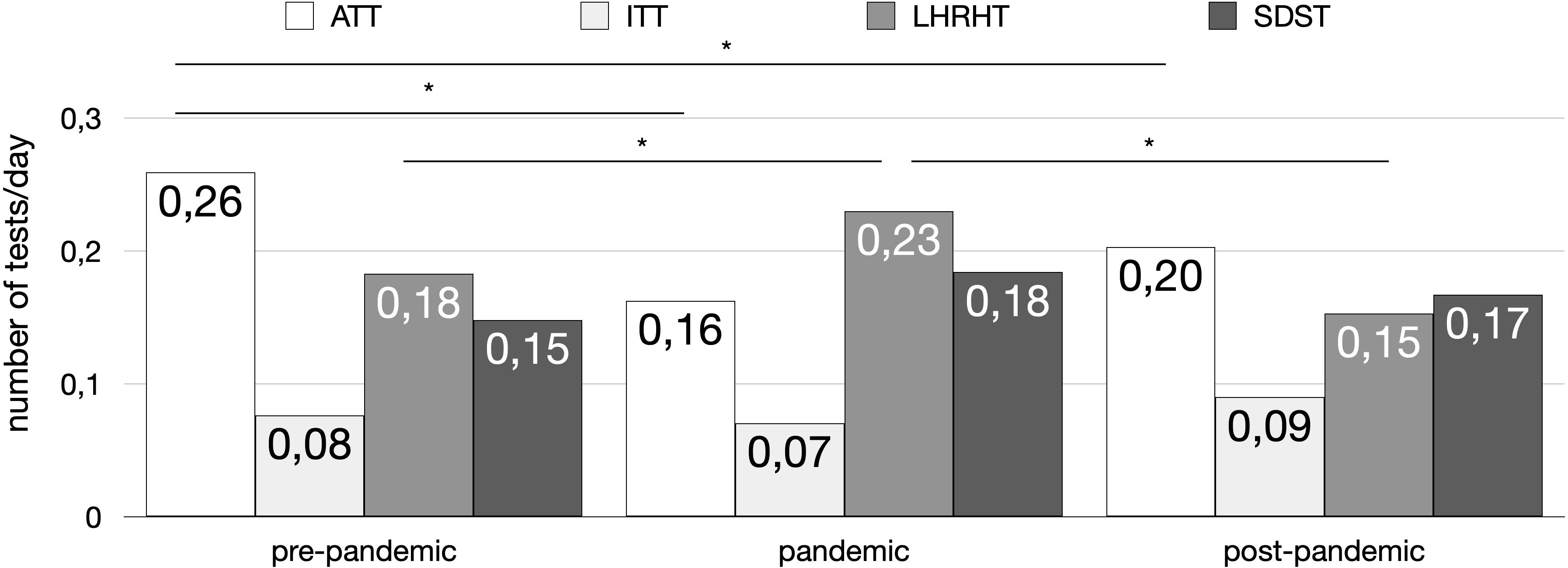
Figure 1. Distribution of the principal stimulation tests (number of tests per day) across the three time periods (pre-pandemic, pandemic, and post-pandemic). The tests included: Arginine Tolerance Test (ATT) (white bars), Insulin Tolerance Test (ITT) (light gray bars), Luteinizing Hormone-Releasing Hormone Test (LHRHT) (medium gray bars), and Standard Dose Synacthen Test (SDST) (dark gray bars). Asterisks (*) indicate statistically significant differences (p < 0.05) between groups.
No significant differences were observed for the remaining tests, likely due to their lower frequency of execution.
Sex distribution of tested patients
Females were more frequently tested than males in all three time periods. Additionally, a significant increase in the proportion of females undergoing testing was observed during the pandemic period, compared to both the pre-pandemic period (61.3% vs. 54%, p = 0.027) and the post-pandemic period (61.3% vs. 49.7%, p < 0.001).
However, the proportion of females tested in the pre- and post-pandemic periods was similar (49.7% vs. 54%, p = 0.205). This increase was likely attributable to the higher number of LHRHT tests performed in females during the pandemic period.
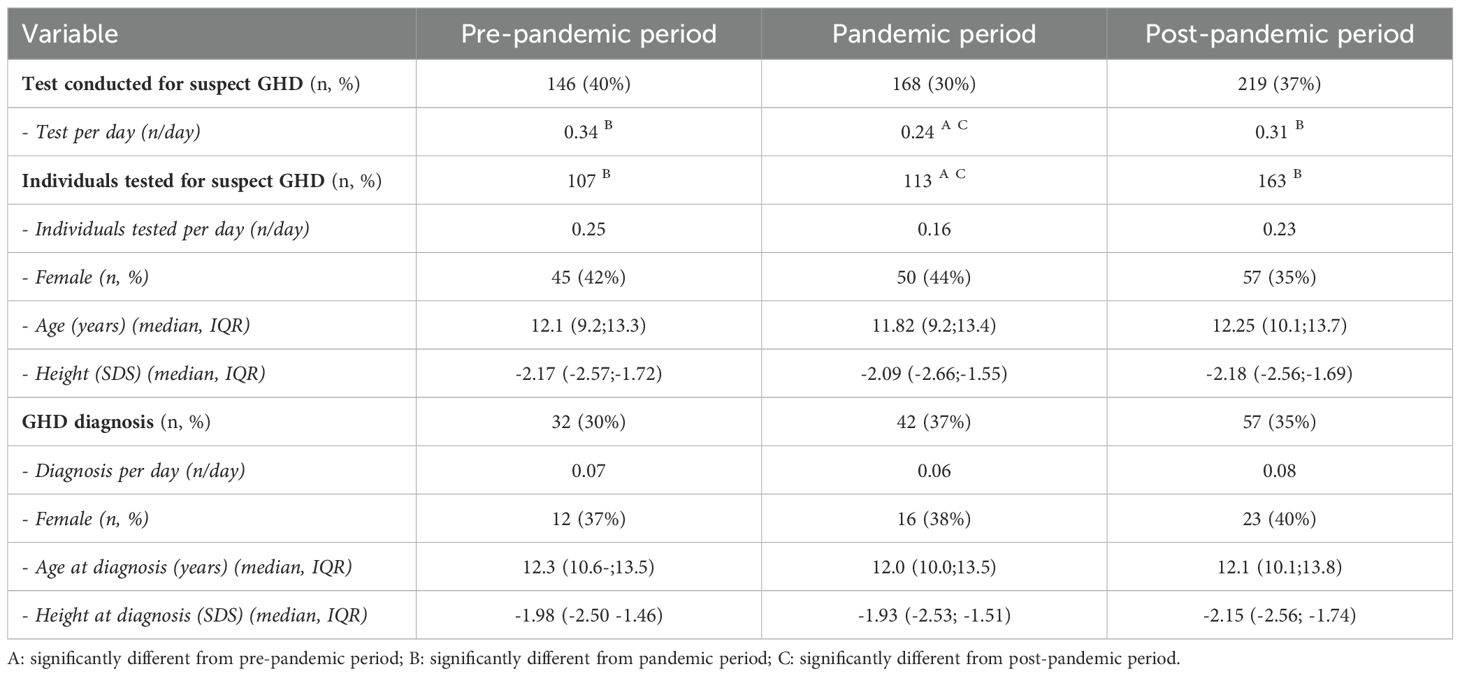
Evaluation and diagnosis of growth hormone deficiency
- During the pre-pandemic period, 146 tests for suspected GHD were conducted on 107 individuals, with an average of 0.25 individuals tested per day. Tests for suspected GHD accounted for 40% of the total tests performed.
- In the pandemic period, the number of tests and individuals tested per day significantly decreased, with 168 tests performed on 113 individuals over 695 days, corresponding to an average of 0.16 individuals tested per day. These tests represented 30% of the total tests performed.
- In the post-pandemic period, 219 tests were conducted on 163 individuals, representing 37% of the total tests performed, with an average of 0.23 individuals tested per day.
A significant difference in the proportion of individuals tested for suspected GHD was observed between the pre-pandemic and pandemic periods (p < 0.001) and between the post-pandemic and pandemic periods (p = 0.002) (Figure 2). In contrast, the number of individuals tested for suspected GHD was similar between the pre-pandemic and post-pandemic periods (p = 0.394), indicating that significantly fewer individuals were tested for suspected GHD during the pandemic period.
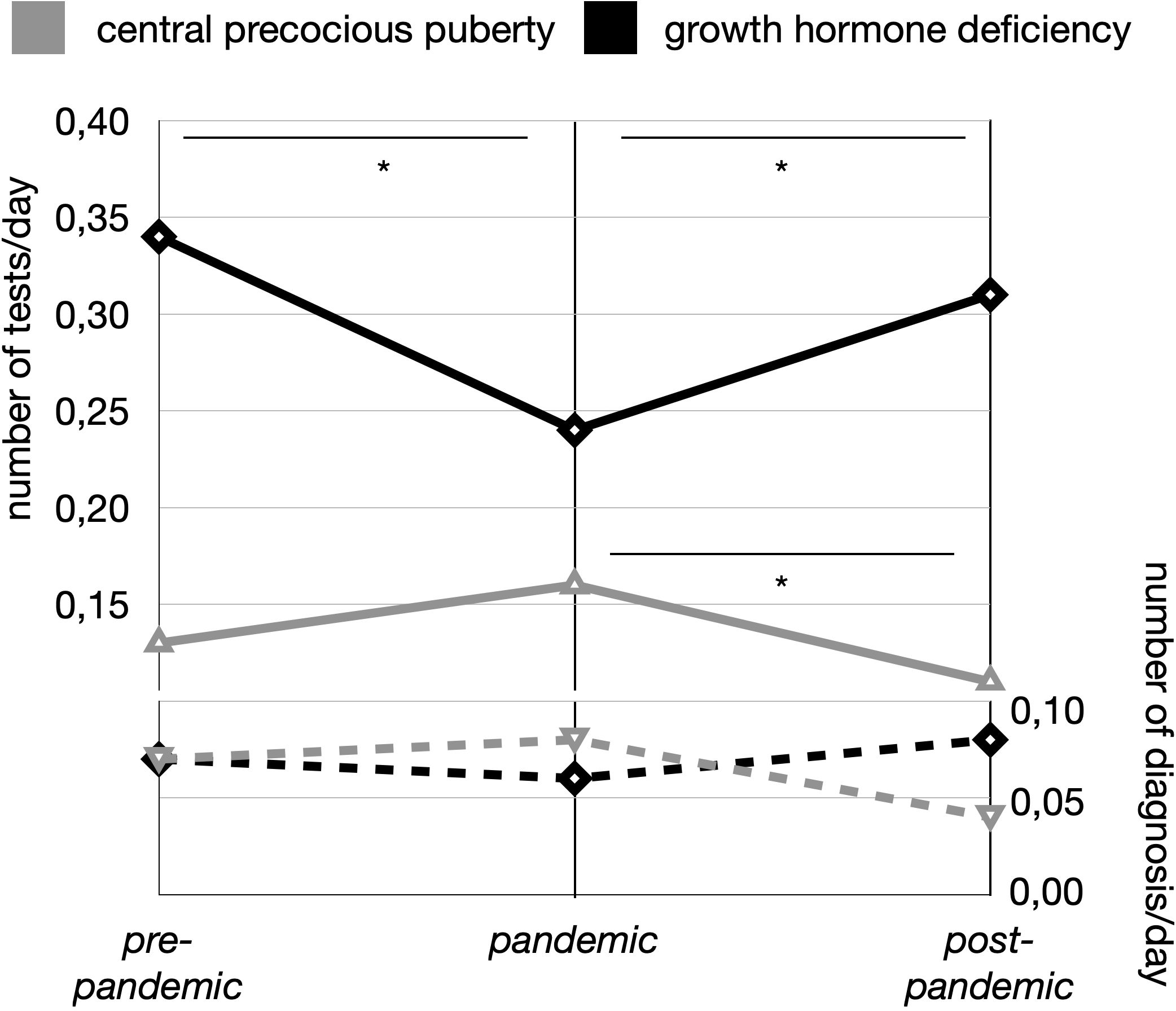
Figure 2. Trends in stimulation tests and diagnoses for central precocious puberty (CPP) and growth hormone deficiency (GHD) across the three study periods (pre-pandemic, pandemic, and post-pandemic). Solid lines represent the number of stimulation tests per day, with gray indicating CPP and black indicating GHD. Dashed lines represent the number of diagnoses per day, with gray for CPP and black for GHD. Asterisks (*) indicate statistically significant differences (p < 0.05) between time periods.
Similar results were observed when considering the number of tests for suspected GHD performed per day (p < 0.001 between pre-pandemic and pandemic periods, p = 0.003 between pandemic and post-pandemic periods, p = 0.426 between pre-pandemic and post-pandemic periods).
Despite these differences, no significant variations were observed in the proportion of GHD diagnoses across the three periods:
- 32 individuals were diagnosed with GHD pre-pandemic (30%),
- 42 during the pandemic (37%), and
- 57 post-pandemic (35%).
Likewise, the number of diagnoses per day did not differ significantly across the three periods (0.07/day pre-pandemic, 0.06/day pandemic, 0.08/day post-pandemic) (Figure 2).
No significant differences were found in sex distribution or age at presentation among the tested children across the three periods. Similarly, there were no significant differences in the median height of tested children, although the post-pandemic period had the lowest median height at diagnosis (-2.15 SDS).
Details regarding GHD tests are reported in Table 3.
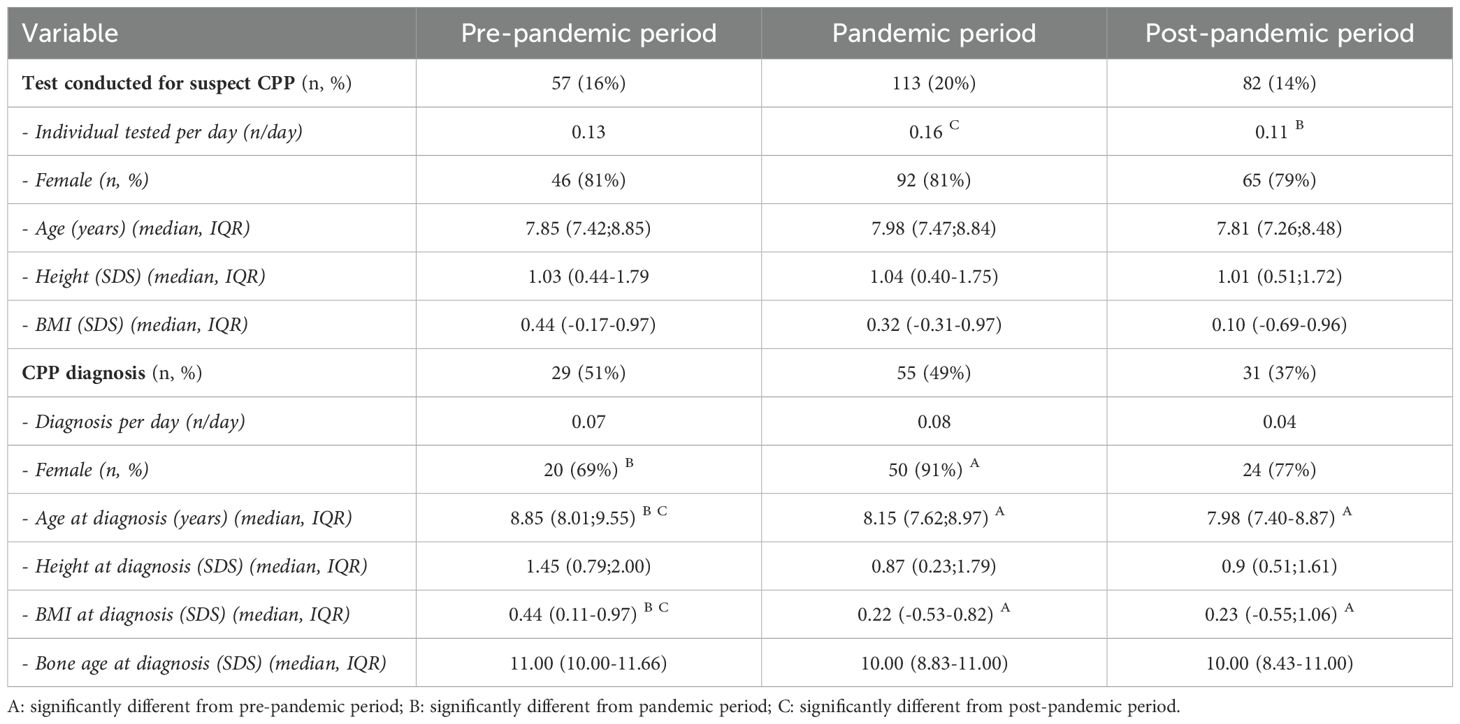
Evaluation and diagnosis of central precocious puberty
Among individuals tested for suspected CPP, the highest proportion was observed during the pandemic period. Specifically:
- in the pre-pandemic period, 57 tests for suspected CPP were performed, accounting for 16% of the total tests, with an average of 0.13 tests per day.
- during the pandemic period, the number of tests increased to 113, representing 20% of the total tests, with an average of 0.16 tests per day.
- in the post-pandemic period, the number of tests decreased to 82, accounting for 14% of the total tests, with an average of 0.11 tests per day.
A significant difference was observed in the proportion of individuals tested for suspected CPP between the pandemic and post-pandemic periods (p = 0.0043), indicating that significantly more individuals were tested for suspected CPP during the pandemic compared to the post-pandemic period (Figure 2).
Regarding individuals diagnosed with CPP:
- 29 diagnoses were made pre-pandemic (51%).
- 55 diagnoses were made during the pandemic (49%).
- 31 diagnoses were made post-pandemic (47%).
No significant differences were observed in the proportion of CPP diagnoses across the three periods, nor in the number of diagnoses per day (Figure 2). Further details regarding CPP testing are provided in Table 4.
No significant differences were found among tested patients in terms of age at presentation or median height at presentation. However, BMI at presentation in patients tested for CPP was significantly higher in the pre-pandemic period compared to both the pandemic and post-pandemic periods.
Among patients diagnosed with CPP, an overall decrease in the median age at diagnosis was observed:
- a significant difference was found between the pre-pandemic period (8.85 years; 8.01–9.55) and the pandemic period (8.15 years; 7.62–8.97) (p = 0.022).
- a further significant difference was observed between the pre-pandemic period and the post-pandemic period, where the lowest median age at diagnosis was recorded (7.98 years; 7.40–8.87) (p = 0.010).
- in contrast, the median age at diagnosis was similar between the pandemic and post-pandemic periods.
The highest median bone age at diagnosis of CPP was reported during the pre-pandemic period (11.00 years; 10.00–11.66), which was significantly higher than during the pandemic period (10.00 years; 8.83–11.00) (p = 0.012). However, no significant difference in median bone age at diagnosis was found between the pandemic and post-pandemic periods (10.00 years; 8.43–11.00).
Throughout the entire study period, females were tested for CPP more frequently than males. A total of 252 tests for CPP were conducted, of which 203 were in females (80.5%). The total number of CPP diagnoses during the study period was 115, with 94 of these cases occurring in females (82%).
- Pre-pandemic period: 46 females were tested (81% of total CPP tests), and 20 diagnoses were made (69% of CPP diagnoses).
- Pandemic period: 92 females were tested (81%), and 50 received the diagnosis (91% of CPP diagnoses).
- Post-pandemic period: 65 females were tested (79%), and 24 diagnoses were made (77% of CPP diagnoses).
While the proportion of females tested remained consistent across the three periods, the prevalence of females diagnosed with CPP was highest during the pandemic period (91%), which was significantly higher than in the pre-pandemic period (69%, p = 0.0239). No significant difference was found in the prevalence of females diagnosed between the pandemic and post-pandemic periods, although the prevalence decreased post-pandemic (from 91% to 77%, p = 0.158). Likewise, no significant difference was observed between the pre-pandemic and post-pandemic periods (from 69% to 77%, p = 0.654).
Discussion
In this retrospective study, we analyzed endocrinological stimulation tests conducted at a tertiary pediatric center over a five-year period (2019–2023), focusing on the impact of the COVID-19 pandemic on diagnostic patterns. Our findings provide novel insights into how healthcare disruptions affected diagnostic activities and how these patterns evolved in the post-pandemic period.
Across the full study period, the number of tests performed per day remained stable, indicating that despite pandemic-related restrictions, our service continued to provide uninterrupted care. However, the pandemic led to notable shifts in referral patterns. Previously published data from our center had shown a significant reduction in testing for GHD during the pandemic and an increase in CPP-related referrals, particularly among females (13). Our expanded dataset confirms these trends and shows a clear return to pre-pandemic diagnostic patterns (“back to normal”) in the subsequent years.
GHD: a silent diagnostic drop
We observed a significant decline in the number of GHD evaluations during the COVID-19 pandemic, followed by a return to pre-pandemic levels. Specifically, our data show that the daily number of individuals tested for GHD was comparable before (0.25/day) and after the pandemic (0.23/day), but significantly lower during the pandemic period (0.16/day, p < 0.005). This reduction—also reported in our previous study, where a 35% drop in GHD-related tests and a 30% reduction in confirmed diagnoses in 2020 compared to 2019 were observed (13)—is likely attributable to the suspension of routine well-child visits, parental reluctance to seek non-urgent medical care, and reduced opportunities for caregivers to monitor and compare children’s growth trajectories with their peers. The widespread implementation of remote schooling and the near-total suspension of extracurricular activities further limited social interactions, potentially delaying the recognition of growth delays.
Although this temporary decline raised concerns about missed opportunities for timely diagnosis, the daily number of confirmed GHD diagnoses remained stable across the three periods (0.07/day pre-pandemic, 0.06/day during the pandemic, and 0.08/day post-pandemic). In the present analysis, the pandemic period spanned from March 8, 2020, to January 31, 2022, (from the nationwide lockdown in Italy to the full restoration of free access to daily activity, including hospital access). Compared to our previous study, which focused primarily on the peak pandemic phase of 2020, the extended observation window likely captured a partial recovery of diagnostic activities. Indeed, although the number of evaluations remained lower, the percentage of confirmed diagnoses among those tested was higher during the pandemic (37%) and post-pandemic periods (35%) compared to the pre-pandemic period (30%), albeit without reaching statistical significance. This suggests that despite reduced screening, children referred during the pandemic may have presented with more overt clinical signs, leading to a higher diagnostic yield and possibly mitigating the risk of missed diagnoses.
While the impact of the pandemic on CPP diagnosis has been widely investigated, its effect on GHD evaluation remains underexplored. Our findings therefore provide a novel contribution to addressing this gap in the current literature. Notably, disparities in GHD evaluation and treatment are deeply influenced by structural and socio-demographic factors, including caregiver perceptions and provider biases. The pandemic may have exacerbated these disparities by disproportionately limiting healthcare access and delaying referrals—especially among populations already underserved. Our data reinforce the need to ensure equitable and timely access to growth monitoring and endocrine evaluations, particularly in times of healthcare system disruption (19).
CPP: a confirmed international spike
In our study, we observed a clear increase in CPP-related diagnostic activity during the COVID-19 pandemic, both in terms of testing frequency and confirmed diagnoses. Specifically, the proportion of stimulation tests performed for suspected CPP increased from 14–16% in the pre- and post-pandemic periods to 20% during the pandemic. The number of daily CPP tests also rose significantly during the pandemic (from 0.13/day pre-pandemic to 0.16/day), with a predominant increase among girls.
This trend is supported by a robust body of international literature documenting similar increases in CPP diagnoses across diverse populations and healthcare settings. Reports from Italy (6, 13, 20–28), Germany (29), Portugal (30), Spain (31) Turkey (32–35), Lebanon (36), Japan (37), South Korea (38), Thailand (39), Singapore (40), China (41, 42), India (43), the United States (44–46), Argentina (47, 48) and Brazil (49) consistently describe this phenomenon. In some of these studies, the number of CPP diagnoses more than doubled compared to previous years—for example, a 5.01-fold increase reported by Fu et al. (42) and a 2.3-fold increase by Geniuk et al. (48)—underscoring the global nature of this shift.
Interestingly, in our cohort, the proportion of confirmed CPP diagnoses among those tested remained stable across all periods (0.07/day pre-pandemic, 0.08/day during the pandemic, 0.04/day post-pandemic), suggesting that the rise in diagnoses was not attributable to overtesting or relaxed diagnostic thresholds. Rather, the data point toward a genuine increase in incidence—particularly among females. Indeed, the proportion of females diagnosed with CPP rose significantly during the pandemic (from 69% pre-pandemic to 91%, p = 0.0043), before decreasing to 77% in the post-pandemic period. Notably, this increase was observed exclusively among females, with no significant change in diagnoses among males, aligning with previous reports (48, 50). This finding reinforces the idea that male CPP may be less influenced by environmental factors and is more often associated with organic or genetic causes (51, 52).
Unlike our study, which showed stable BMI trends across the observed periods, several reports noted increased BMI among children diagnosed with CPP during the pandemic (6, 23, 36, 39, 40). However, other studies (21, 43, 46, 48) found no significant differences in BMI, suggesting that lifestyle factors—beyond weight gain alone—may be at play.
Importantly, our data extend beyond the acute phase of the pandemic, capturing a return to pre-pandemic referral and diagnosis patterns by 2022–2023. To date, only two published studies have included longitudinal post-pandemic data, making our study one of the few to explore trends in the normalization of CPP care. Vargas Trujillo et al. reported a doubling of CPP cases requiring puberty suppression during the pandemic, followed by a gradual decline in the post-pandemic period (46). Similarly, Chioma et al. observed an increase in progressive CPP diagnoses in 2020, which decreased in 2021 and returned to pre-pandemic levels by 2022 (22). Notably, Chioma et al. also documented a significant increase in screen time and a reduction in physical activity in 2020 compared to both 2019 and 2022. As pandemic restrictions eased, these environmental stressors diminished, and the surge in CPP cases subsided. These findings support the hypothesis that environmental factors—such as reduced physical activity, increased screen exposure, sleep disruption, and psychosocial stress—may have acted as triggers for earlier pubertal onset, particularly among girls (11). This also reinforces the notion that female puberty may be more sensitive to environmental influences.
Contrasting with the findings of Vargas Trujillo et al., who reported an increasing trend in both median age at diagnosis (from 7.1 years pre-pandemic, to 7.35 during the pandemic, and 8.01 post-pandemic) and bone age (from 9.5 to 10.4 years) (46), our data reveal a progressive decrease in median age at CPP diagnosis across the three periods (from 8.85 years pre-pandemic, to 8.15 during the pandemic, and 7.98 post-pandemic). One possible explanation for this discrepancy may lie in differences in referral timing: while Vargas Trujillo et al. interpreted the older age at diagnosis as the result of delayed access to care, our center may have succeeded in maintaining more timely evaluations despite external constraints. Alternatively, our findings might reflect broader secular trends toward earlier pubertal onset, which have been observed globally since the 1990s (53, 54). Notably, Chioma et al. did not report significant changes in age at diagnosis across study years, further underscoring the variability of pandemic-related effects across populations and healthcare systems.
This study has several strengths. First, it presents a comprehensive five-year analysis from a single tertiary pediatric center, covering the pre-pandemic, pandemic, and post-pandemic phases. By standardizing test frequency according to observation time, we minimized potential biases due to differences in period length. Additionally, by including both GHD and CPP, we provide a broader and more nuanced picture of how different endocrine conditions were impacted by healthcare disruptions and subsequently recovered.
While the increase in CPP diagnoses during the pandemic has been widely documented, few studies have explored the normalization phase in the post-pandemic period, and even fewer have assessed the temporary decline and subsequent recovery of GHD diagnostics. Our findings therefore contribute uniquely to both areas. From a clinical perspective, these results underscore the resilience and adaptability of pediatric endocrinology services, while also highlighting the need for targeted strategies to ensure timely referrals during healthcare crises.
Nonetheless, some limitations must be acknowledged. The retrospective design and single-center scope may limit the generalizability of our findings. Although we adjusted for differences in observation time, unmeasured confounding factors—such as seasonal variation in referrals or shifts in local healthcare policies—may have influenced the observed trends. Furthermore, while we hypothesize that environmental and behavioral changes contributed to the increased CPP referrals, we did not collect direct data on lifestyle factors such as screen time, dietary habits, physical activity, or psychosocial stress. This limits the strength of causal inferences. Prospective studies incorporating behavioral, metabolic, and hormonal assessments are needed to better elucidate these associations.
Finally, although our time-stratified analysis helps to distinguish pandemic-related trends from longer-term changes, it remains possible that broader secular shifts—both genetic and environmental—may also influence pubertal timing and growth. Future multicenter studies involving diverse populations, larger sample sizes, and long-term outcome data will be essential to validate and expand on our findings.
Conclusion
The findings of this study highlight the significant, albeit temporary, impact of the COVID-19 pandemic on pediatric endocrinology diagnostic patterns, particularly for GHD and CPP. During the pandemic period, notable deviations in testing and diagnosis trends were observed. The post-pandemic recovery demonstrates the resilience and adaptability of healthcare systems in restoring routine activities. Although the critical phase of the pandemic is behind us, it remains highly relevant to reflect on how such a global event significantly altered daily habits and access to healthcare; examining its impact on diagnostic trends continues to offer valuable insights into system resilience and evolving patient priorities. The observed shifts in diagnostic patterns underscore the potential influence of environmental and lifestyle factors on endocrine conditions, warranting further investigation. These insights not only deepen our understanding of the pandemic’s repercussions on pediatric health but also emphasize the importance of maintaining accessible and proactive healthcare services during times of crisis to mitigate diagnostic delays and ensure timely interventions.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
MP: Conceptualization, Data curation, Writing – original draft, Writing – review & editing. SP: Data curation, Writing – original draft, Writing – review & editing. PD: Data curation, Formal Analysis, Validation, Writing – original draft, Writing – review & editing. GTa: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. VV: Investigation, Writing – original draft, Writing – review & editing. GV: Investigation, Writing – original draft, Writing – review & editing. DS: Investigation, Writing – original draft, Writing – review & editing. EF: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. EB: Supervision, Writing – original draft, Writing – review & editing. GTo: Funding acquisition, Methodology, Supervision, Validation, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Italian Ministry of Health, through the contribution given to the Institute for Maternal and Child Health IRCCS Burlo Garofolo, Trieste, Italy (RC 16/24).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that Generative AI was used in the creation of this manuscript. During the preparation of this work the authors used ChatGPT in order to revise the language. After using this tool, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Indolfi G, Stivala M, Lenge M, Diaz Naderi R, McIntosh J, Llandrich RC, et al. Impact of SARS-CoV-2 pandemic and strategies for resumption of activities during the second wave of the pandemic: A report from eight paediatric hospitals from the ECHO network. Front Public Health. (2021) 9:630168. doi: 10.3389/fpubh.2021.630168
2. Cozzi G, Molina Ruiz I, Giudici F, Romano S, Grigoletto V, Barbi E, et al. Pediatric emergency cases in the first year of the COVID-19 pandemic in a tertiary-level emergency setting. Front Pediatr. (2022) 10:918286. doi: 10.3389/fped.2022.918286
3. Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. (2020) 4:e10–1. doi: 10.1016/S2352-4642(20)30108-5
4. Barten DG, Latten GHP, Van Osch FHM. Reduced emergency department utilization during the early phase of the COVID-19 pandemic: viral fear or lockdown effect? Disaster Med Public Health Prep. (2022) 16:36–9. doi: 10.1017/dmp.2020.303
5. Bellotto E, Monasta L, Pellegrin MC, Bossini B, Tamaro G, Conte MS, et al. Pattern and features of pediatric endocrinology referrals: A retrospective study in a single tertiary center in Italy. Front Pediatr. (2020) 8:580588. doi: 10.3389/fped.2020.580588
6. Stagi S, De Masi S, Bencini E, Losi S, Paci S, Parpagnoli M, et al. Increased incidence of precocious and accelerated puberty in females during and after the Italian lockdown for the coronavirus 2019 (COVID-19) pandemic. Ital J Pediatr. (2020) 46:165. doi: 10.1186/s13052-020-00931-3
7. Alonso GF. Precocious puberty, pandemic and beyond. Pituitary. (2024) 27:916–24. doi: 10.1007/s11102-024-01434-8
8. Fanaki M, Michala L, Nazari E, Daskalakis G. Central precocious puberty during the COVID-19 pandemic period: A systematic review of literature. Cureus. (2024) 16:e71002. doi: 10.7759/cureus.71002
9. Hoskyns RB, Howard SR. Effects of the COVID-19 pandemic on the incidence of central precocious puberty; a narrative review. J Pediatr Endocrinol Metab. (2024) 37:102–9. doi: 10.1515/jpem-2023-0507
10. Prosperi S, Chiarelli F. Early and precocious puberty during the COVID-19 pandemic. Front Endocrinol (Lausanne). (2023) 13:1107911. doi: 10.3389/fendo.2022.1107911
11. Street ME, Sartori C, Catellani C, Righi B. Precocious puberty and covid-19 into perspective: potential increased frequency, possible causes, and a potential emergency to be addressed. Front Pediatr. (2021) 9:734899. doi: 10.3389/fped.2021.734899
12. Zhang J, Xu J, Tang X, Wu R. Comparison of central precocious puberty frequency before and during COVID-19: a systematic review and meta-analysis. BMC Endocr Disord. (2024) 24:219. doi: 10.1186/s12902-024-01749-4
13. Peinkhofer M, Bossini B, Penco A, Giangreco M, Pellegrin MC, Vidonis V, et al. Reduction in pediatric growth hormone deficiency and increase in central precocious puberty diagnoses during COVID-19 pandemics. Ital J Pediatr. (2022) 48:49. doi: 10.1186/s13052-022-01238-1
14. Radhakrishnan L, Carey K, Hartnett KP, Kite-Powell A, Zwald M, Anderson KN, et al. Pediatric emergency department visits before and during the COVID-19 pandemic — United States, January 2019–January 2022. MMWR Morb Mortal Wkly Rep. (2022) 71:313–8. doi: 10.15585/mmwr.mm7108e1
15. Decree Law no.14 of the Italian Prime Minister. Further measures for the containment and contrast of the spread of the Covid-19 virus throughout the entire national territory (2020). Available online at: https://www.gazzettaufficiale.it/eli/id/2020/03/09/20G00030/sg (Accessed February 3, 2025).
16. Decree of the President of the Council of Ministers. Identification of essential and primary needs for which the possession of one of the COVID-19 Green Certifications is not required (2022). Official Gazette General Series. Available online at: https://www.gazzettaufficiale.it/eli/id/2022/01/24/22A00555/SG (Accessed February 3, 2025).
17. Penco A, Bossini B, Giangreco M, Vidonis V, Vittori G, Grassi N, et al. Should pediatric endocrinologists consider more carefully when to perform a stimulation test? Front Endocrinol. (2021) 12:660692. doi: 10.3389/fendo.2021.660692
18. The Italian Data Protection Authorithy. Authorisation no. 9/2014 - General Authorisation to Process Personal Data for Scientific Research Purposes (2014). Available online at: https://www.garanteprivacy.it/web/guest/home/docweb/-/docweb-display/docweb/3786078 (Accessed February 3, 2025).
19. Beliard K, Wu V, Samuels J, Lipman TH, Rapaport R. Identifying and addressing disparities in the evaluation and treatment of children with growth hormone deficiency. Front Endocrinol (Lausanne). (2022) 13:989404. doi: 10.3389/fendo.2022.989404
20. Barberi C, Di Natale V, Assirelli V, Bernardini L, Candela E, Cassio A. Implicating factors in the increase in cases of central precocious puberty (CPP) during the COVID-19 pandemic: Experience of a tertiary centre of pediatric endocrinology and review of the literature. Front Endocrinol. (2022) 13:1032914. doi: 10.3389/fendo.2022.1032914
21. Chioma L, Bizzarri C, Verzani M, Fava D, Salerno M, Capalbo D, et al. Sedentary lifestyle and precocious puberty in girls during the COVID-19 pandemic: an Italian experience. Endocr Connect. (2022) 11:e210650. doi: 10.1530/EC-21-0650
22. Chioma L, Chiarito M, Bottaro G, Paone L, Todisco T, Bizzarri C, et al. COVID-19 pandemic phases and female precocious puberty: The experience of the past 4 years (2019 through 2022) in an Italian tertiary center. Front Endocrinol. (2023) 14:1132769. doi: 10.3389/fendo.2023.1132769
23. Fava D, Pepino C, Tosto V, Gastaldi R, Pepe A, Paoloni D, et al. Precocious puberty diagnoses spike, COVID-19 pandemic, and body mass index: findings from a 4-year study. J Endocr Soc. (2023) 7:bvad094. doi: 10.1210/jendso/bvad094
24. Goffredo M, Pilotta A, Parissenti I, Forino C, Tomasi C, Goffredo P, et al. Early onset of puberty during COVID-19 pandemic lockdown: experience from two Pediatric Endocrinology Italian Centers. J Pediatr Endocrinol Metab. (2023) 36:290–8. doi: 10.1515/jpem-2022-0492
25. Goggi G, Moro M, Chilà A, Fatti L, Cangiano B, Federici S, et al. COVID-19 lockdown and the rate of central precocious puberty. J Endocrinol Invest. (2024) 47:315–23. doi: 10.1007/s40618-023-02146-9
26. Turriziani Colonna A, Curatola A, Sodero G, Lazzareschi I, Cammisa I, Cipolla C. Central precocious puberty in children after COVID-19 outbreak: a single-center retrospective study. Minerva Pediatr (Torino) (2022). doi: 10.23736/S2724-5276.22.06827-6
27. Umano GR, Maddaluno I, Riccio S, Lanzaro F, Antignani R, Giuliano M, et al. Central precocious puberty during COVID-19 pandemic and sleep disturbance: an exploratory study. Ital J Pediatr. (2022) 48:60. doi: 10.1186/s13052-022-01256-z
28. Verzani M, Bizzarri C, Chioma L, Bottaro G, Pedicelli S, Cappa M. Impact of COVID-19 pandemic lockdown on early onset of puberty: experience of an Italian tertiary center. Ital J Pediatr. (2021) 47:52. doi: 10.1186/s13052-021-01015-6
29. Baehr S, Schnabel D, Woelfle J, Schreiner F, Gohlke B. National survey of referrals for precocious puberty in Germany. BMJ Paediatr Open. (2023) 7:e001987. doi: 10.1136/bmjpo-2023-001987
30. Resende MM, Gomes Pereira P, Mendes C, Oliveira MJ, Borges T, Freitas J. Emerging trend of central precocious puberty: A retrospective study of cases diagnosed before and during the COVID-19 pandemic in a Portuguese tertiary-level hospital. Cureus. (2024) 16:e76504. doi: 10.7759/cureus.76504
31. Ariza Jimenez AB, Aguilar Gomez-Cardenas FJ, de la Camara Moraño C. Likely impact of COVID-19 on referrals to pediatric endocrinology: Increased incidence of precocious puberty in a third-level hospital. Endocrinol Diabetes Nutr (Engl Ed). (2022) 69:542–4. doi: 10.1016/j.endien.2022.07.002
32. Acar S, Özkan B. Increased frequency of idiopathic central precocious puberty in girls during the COVID-19 pandemic: preliminary results of a tertiary center study. J Pediatr Endocrinol Metab. (2021) 35:249–51. doi: 10.1515/jpem-2021-0565
33. Acinikli KY, Erbaş İC, Besci Ö, Demir K, Abacı A, Böber E. Has the frequency of precocious puberty and rapidly progressive early puberty increased in girls during the COVID-19 pandemic? J Clin Res Pediatr Endocrinol. (2022) 14:302–7. doi: 10.4274/jcrpe.galenos.2022.2022-12-11
34. Yesiltepe Mutlu G, Eviz E, Haliloglu B, Kirmizibekmez H, Dursun F, Ozalkak S, et al. The effects of the covid-19 pandemic on puberty: a cross-sectional, multicenter study from Turkey. Ital J Pediatr. (2022) 48:144. doi: 10.1186/s13052-022-01337-z
35. Orman B, Esen S, Keskin M, Muratoğlu Şahin N, Savaş Erdeve Ş, Çetinkaya S. Status of central precocious puberty cases at the onset of coronavirus disease 2019 pandemic: A single-center experience. Turk Arch Pediatr. (2022) 57:349–53. doi: 10.5152/TurkArchPediatr.2022.2101313
36. Itani A, Abou Hamdan A, Zgheib H, Ghandour Z, Costanian C, Azar A. Increased incidence of precocious puberty in girls during COVID-19 pandemic: early indicator of the upcoming childhood metabolic syndrome pandemic? Glob Pediatr Health. (2022) 9:2333794X221134565. doi: 10.1177/2333794X221134565
37. Matsubara K, Higuchi S, Watanabe Y, Kitayama K, Yamada Y, Yorifuji T. Increased frequency of central precocious puberty during the coronavirus disease (COVID-19) pandemic at a single center in the Osaka Metropolitan Area of Japan. Clin Pediatr Endocrinol. (2023) 32:58–64. doi: 10.1297/cpe.2022-0008
38. Choi KH, Park SC. An increasing tendency of precocious puberty among Korean children from the perspective of COVID-19 pandemic effect. Front Pediatr. (2022) 10:968511. doi: 10.3389/fped.2022.968511
39. Yaisilp P, Numsriskulrat N, Sahakitrungruang T. Clinical and epidemiological insights into early puberty in Thai girls: a 5-year study. Ann Pediatr Endocrinol Metab. (2025) 30:17–24. doi: 10.6065/apem.2448112.056
40. Leong A, Vasanwala RF. Early puberty trend during the COVID-19 pandemic in Singapore: A retrospective review in a single tertiary centre. J ASEAN Fed Endocr Soc. (2024) 39:6–11. doi: 10.15605/jafes.039.01.12
41. Chen Y, Chen J, Tang Y, Zhang Q, Wang Y, Li Q, et al. Difference of precocious puberty between before and during the COVID-19 pandemic: A cross-sectional study among Shanghai school-aged girls. Front Endocrinol (Lausanne). (2022) 13:839895. doi: 10.3389/fendo.2022.839895
42. Fu D, Li T, Zhang Y, Wang H, Wu X, Chen Y, et al. Analysis of the incidence and risk factors of precocious puberty in girls during the COVID-19 pandemic. Int J Endocrinol. (2022) 2022:9229153. doi: 10.1155/2022/9229153
43. Mondkar SA, Oza C, Khadilkar V, Shah N, Gondhalekar K, Kajale N, et al. Impact of COVID-19 lockdown on idiopathic central precocious puberty - experience from an Indian centre. J Pediatr Endocrinol Metab. (2022) 35:895–900. doi: 10.1515/jpem-2022-0157
44. Baby M, Ilkowitz J, Cheema Brar P. Impacts of the COVID-19 pandemic on the diagnosis of idiopathic central precocious puberty in pediatric females in New York City. J Pediatr Endocrinol Metab. (2023) 36:517–22. doi: 10.1515/jpem-2022-0628
45. Vargas Trujillo M, Rungvivatjarus T, Klein KO. Incidence of central precocious puberty more than doubled during COVID-19 pandemic: Single-center retrospective review in the United States. Front Pediatr. (2022) 10:1007730. doi: 10.3389/fped.2022.1007730
46. Vargas Trujillo M, Rungvivatjarus T, Klein KO. Incidence of central precocious puberty declines to pre-pandemic levels post COVID-19 pandemic increase: single-center retrospective review in the United States. Front Pediatr. (2024) 12:1352295. doi: 10.3389/fped.2024.1352295
47. Benedetto M, Riveros V, Eymann A, Terrasa S, Alonso G. Analysis of the incidence of central precocious puberty treated with gonadotropin-releasing hormone analogs. Impact of the COVID-19 pandemic. Arch Argent Pediatr. (2023) 121:e202202849. doi: 10.5546/aap.2022-02849.eng
48. Geniuk N, de Jesús Suárez Mozo M, Pose MN, Vidaurreta S. Rapidly progressive precocious puberty during the COVID-19 lockdown. Arch Argent Pediatr. (2023) 121:e202202840. doi: 10.5546/aap.2022-02840.eng
49. Oliveira Neto CP, Azulay RSS, Almeida AGFP, Tavares MDGR, Vaz LHG, Leal IRL, et al. Differences in Puberty of Girls before and during the COVID-19 Pandemic. Int J Environ Res Public Health. (2022) 19:4733. doi: 10.3390/ijerph19084733
50. Tsinopoulou VR, Stamati A, Sotiriou G, Sakellari EI, Dimitriadou M, Galli-Tsinopoulou A, et al. Puberty in boys with type 1 diabetes mellitus: What has changed? Diabetes Res Clin Pract. (2023) 203:110837. doi: 10.1016/j.diabres.2023.110837
51. Bräuner EV, Busch AS, Eckert-Lind C, Koch T, Hickey M, Juul A. Trends in the incidence of central precocious puberty and normal variant puberty among children in Denmark, 1998 to 2017. JAMA Netw Open. (2020) 3:e2015665. doi: 10.1001/jamanetworkopen.2020.15665
52. Moise-Silverman J, Silverman LA. A review of the genetics and epigenetics of central precocious puberty. Front Endocrinol. (2022) 13:1029137. doi: 10.3389/fendo.2022.1029137
53. Herman-Giddens ME, Slora EJ, Wasserman RC, Bourdony CJ, Bhapkar MV, Koch GG, et al. Secondary sexual characteristics and menses in young girls seen in office practice: A study from the pediatric research in office settings network. Pediatrics. (1997) 99:505–12. doi: 10.1542/peds.99.4.505
Keywords: precocious puberty, growth hormone deficiency, stimulation tests, COVID-19, central precocious puberty (CPP)
Citation: Peinkhofer M, Passarella S, Dalena P, Tamaro G, Vidonis V, Vittori G, Slama D, Faleschini E, Barbi E and Tornese G (2025) Back to normal? A retrospective study on stimulation test and endocrinological diagnosis before, during and after COVID-19 pandemics. Front. Endocrinol. 16:1571685. doi: 10.3389/fendo.2025.1571685
Received: 05 February 2025; Accepted: 14 April 2025;
Published: 05 May 2025.
Edited by:
Semra Çaglar Çetinkaya, University of Health Sciences, TürkiyeReviewed by:
Clariano Pires De Oliveira Neto, Federal University of Maranhão, BrazilJessica Munarin, University of Turin, Italy
Copyright © 2025 Peinkhofer, Passarella, Dalena, Tamaro, Vidonis, Vittori, Slama, Faleschini, Barbi and Tornese. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gianluca Tornese, Z2lhbmx1Y2EudG9ybmVzZUBidXJsby50cmllc3RlLml0
†These authors have contributed equally to this work and share first authorship
‡ORCID: Paolo Dalena, orcid.org/0000-0003-2920-9572
Gianluca Tamaro, orcid.org/0000-0003-1635-9141
Elena Faleschini, orcid.org/0000-0002-7045-5524
Egidio Barbi, orcid.org/0000-0002-6343-846X
Gianluca Tornese, orcid.org/0000-0002-4395-3915
 Martina Peinkhofer
Martina Peinkhofer Sofia Passarella1†
Sofia Passarella1† Paolo Dalena
Paolo Dalena Gianluca Tamaro
Gianluca Tamaro Egidio Barbi
Egidio Barbi Gianluca Tornese
Gianluca Tornese