- 1Department of Orthopaedics, Lanzhou University Second Hospital, Lanzhou, Gansu, China
- 2Orthopaedics Key Laboratory of Gansu Province, Lanzhou, Gansu, China
- 3Department of Orthopaedics, Qinghai Provincial People’s Hospital, Xining, Qinghai, China
Background: Modic changes refer to bone marrow alterations beneath vertebral endplates and are potentially linked to infection, trauma, disc degeneration, scoliosis, and other pathological conditions. Systematic evaluations of their incidence and associated risk factors in the lumbar spine are lacking. This study aimed to analyze and evaluate the incidence and risk factors of Modic changes in lumbar spine disorders.
Methods: A comprehensive systematic review was conducted using Web of Science, PubMed, Cochrane Library, and Embase databases. Eligible studies reported the incidence and associated risk factors of Modic changes in the lumbar spine. Data were extracted and systematically analyzed from the selected studies, and meta-analyses were conducted employing random or fixed effects models.
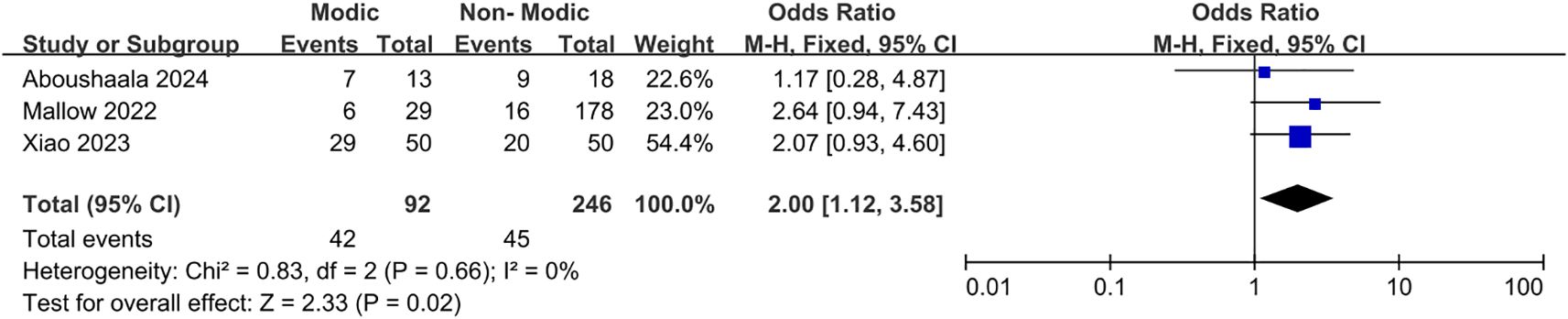
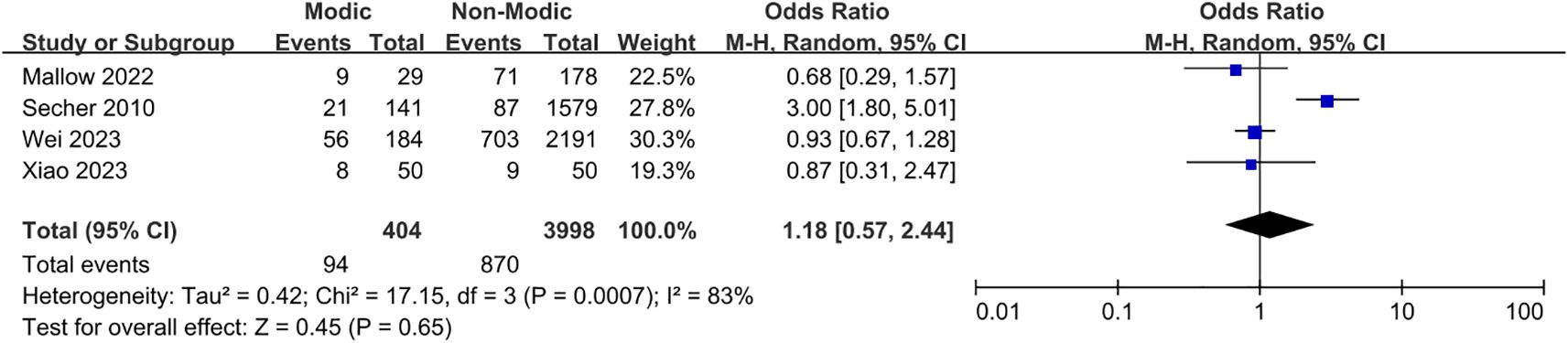
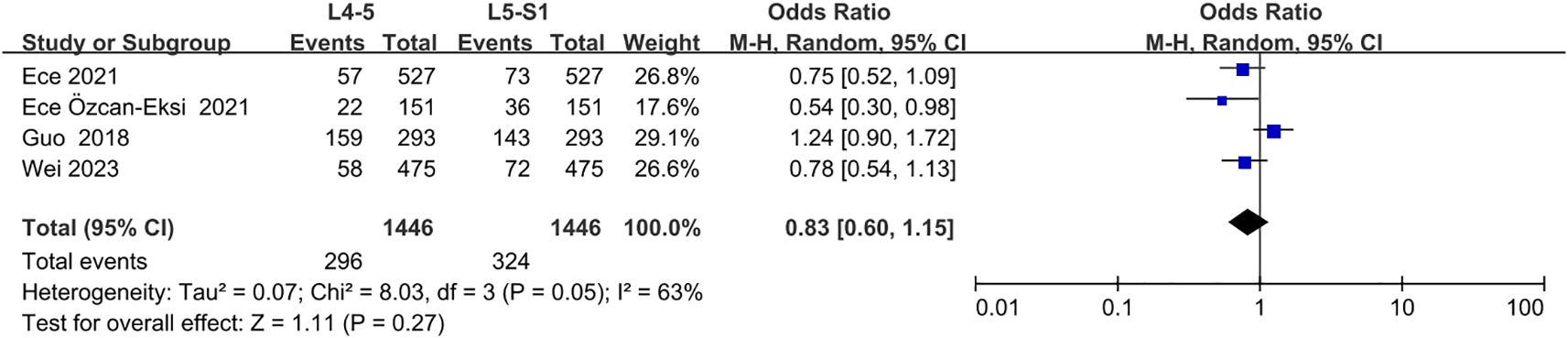
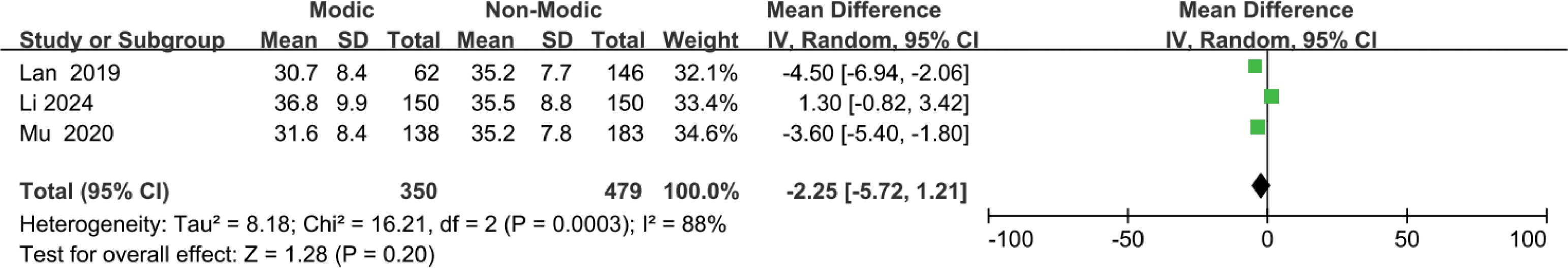
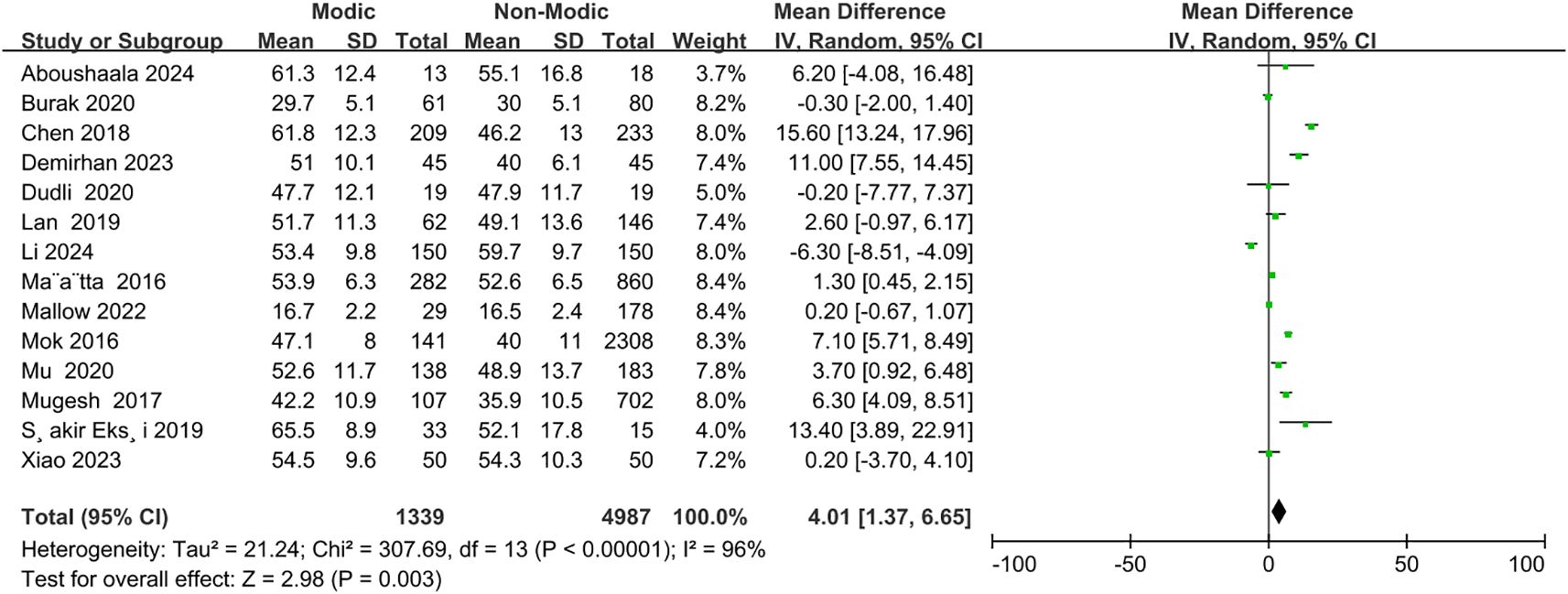
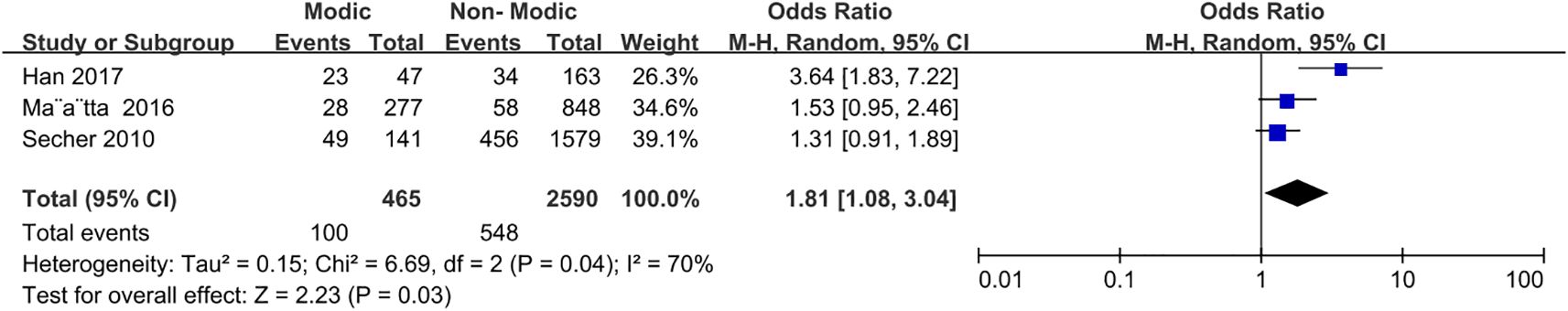
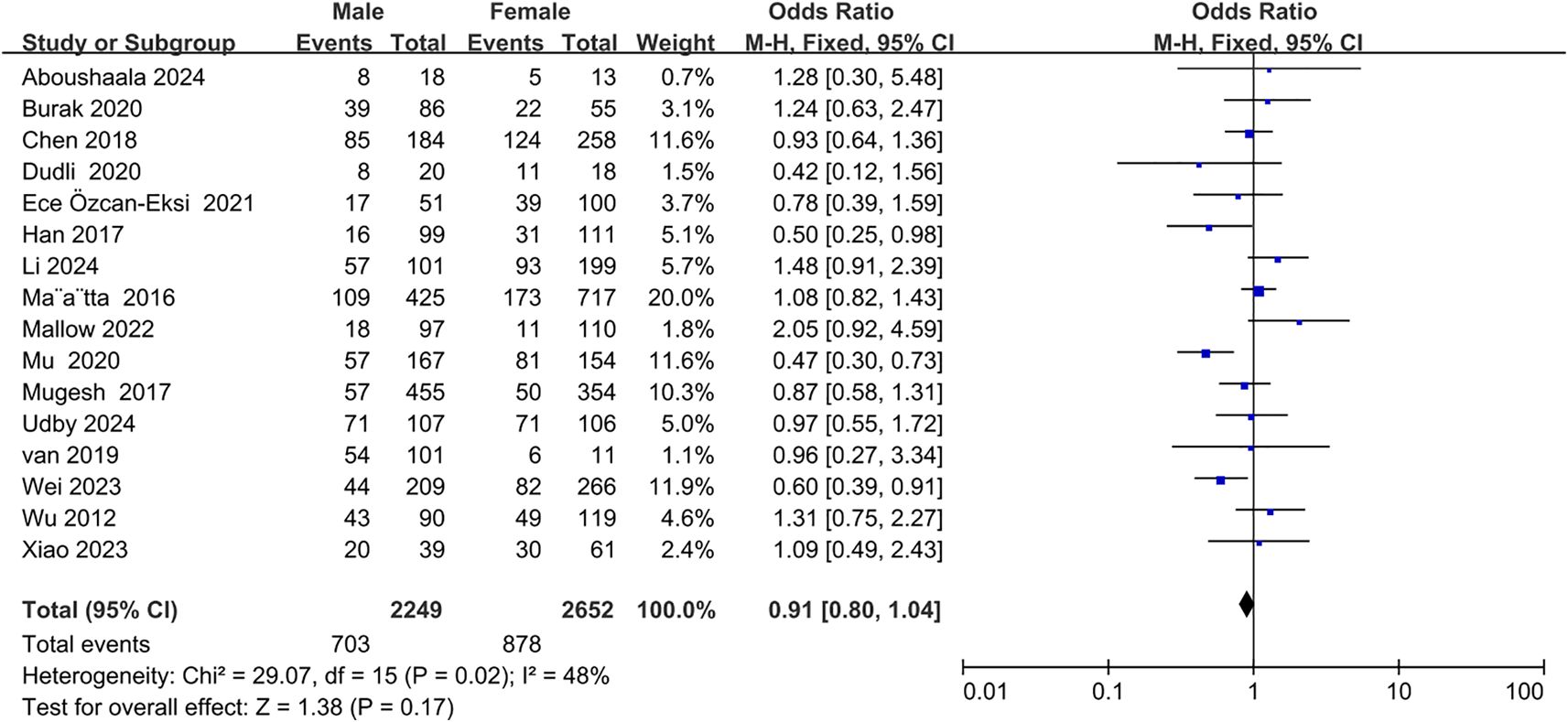
Results: Twenty-five studies were included in the meta-analysis. The overall incidence of Modic changes was 35%. Six risk factors were identified and quantitatively assessed. Strong evidence supported the association of endplate changes (OR=3.56; 95% CI=2.00 to 6.32; p<0.0001); moderate evidence supported the association of age (OR=4.01; 95% CI=1.37 to 6.65; p=0.003), disc degeneration (OR=8.54; 95% CI=1.98 to 36.73; p=0.004), and lumbar lordosis angle (OR=-4.14; 95% CI=-6.79 to -1.49; p=0.002); minor evidence supported the association of spondylolisthesis (OR=2.00; 95% CI=1.12 to 3.58; p=0.02) and physical labor (OR=1.81; 95% CI=1.08 to 3.04; p=0.03) with the occurrence of Modic changes in the lumbar spine. No significant associations were found to support body mass index, sex, disc herniation, smoking, distributional segmentation, or sacral slope angle as risk factors for Modic changes in the lumbar spine.
Conclusion: Modic changes occur in 35% of lumbar spine cases, with advanced age, disc degeneration, endplate changes, spondylolisthesis, reduced anterior lumbar lordosis angles, and participation in physical labor identified as associated risk factors.
1 Introduction
Lower back pain is a prevalent symptom of spinal disorders, often caused by various underlying conditions and associated with a certain disability rate. Severe disabling pain significantly impairs the long-term quality of life for patients and imposes a substantial burden on global economic development (1–4). The etiology of lower back pain is highly complex, involving factors such as lumbar disc degeneration, lumbar disc herniation, lumbar muscle strain, and lumbar spondylolisthesis (2, 5–8). Furthermore, Modic changes are thought to be strongly associated with lower back pain (9–11).
In 1987, De Roos reported Modic-like changes using nuclear magnetic resonance (NMR) imaging of the lumbar spine (12). Modic changes refer to alterations in the bony tissue beneath the vertebral endplates, which can be differentiated and confirmed via magnetic resonance imaging (MRI) (13). Modic changes are classified into three distinct types based on NMR manifestations: Type I is characterized by edema and inflammatory changes in the bone beneath the endplate; Type II is marked by fatty infiltration and degenerative changes; Type III is distinguished by sclerotic alterations in the local bone beneath the endplate (14–17). Modic changes are significantly associated with severe disc herniation, disc degeneration, and chronic lower back pain (12, 17–19). Nevertheless, their pathogenesis remains complex, and their etiology is yet to be fully elucidated. This may be related to compromised defensive properties, such as the structural integrity of the vertebral endplates, along with other contributing factors (20).
Numerous studies have investigated risk factors associated with Modic changes. Li et al. (21) demonstrated that factors such as disc degeneration, spondylolisthesis, and disc height may be linked to Modic changes. Some studies have suggested that obesity and elevated body mass index (BMI) may be associated with Modic changes (22), while others have found no such relationship (23). Furthermore, whether smoking, lumbar disc herniation, and lumbar segmental distribution are associated with the occurrence and progression of Modic remains controversial. To date, no meta-analysis has been conducted on the incidence and associated risk factors of Modic changes in the lumbar spine. Comprehensive analyses are crucial for confirming these factors, as they are essential for the early diagnosis and management of degenerative spinal conditions. Therefore, this systematic review and meta-analysis aimed to determine the incidence and risk factors of Modic changes in patients with lumbar spinal disorders.
2 Methods
This systematic review and meta-analysis adhered to the guidelines outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (24) and AMSTAR (Assessing the Methodological Quality of Systematic Reviews) Guidelines (25).
2.1 Literature search strategies
A comprehensive search of all relevant English-language publications available as of May 10, 2024, was conducted across the PubMed, Embase, Web of Science, and Cochrane Library databases, in consultation with independent information technology experts. The search strategy (Table 1) utilized the following search terms: disc degeneration, lumbar spine, lower back pain, Modic changes, incidence, and risk factors. Titles and abstracts were screened to identify potentially relevant articles, and full-text publications and reference lists were obtained for further in-depth analysis based on the inclusion criteria.
2.2 Inclusion and exclusion criteria
Studies that met the following inclusion criteria were included for review: (1) Patients of all ages suffering from low back pain due to degenerative lumbar spine conditions (including lumbar disc herniation, lumbar spondylolisthesis, and degenerative lumbar lateral herniation, among other degenerative lumbar spine conditions), treated surgically or non-surgically; (2) Healthy participants; (3) Modic changes beneath the vertebral endplates confirmed by MRI; and (4) Publications in English language. Studies were excluded based on the following: (1) Pregnancy, traumatic fracture, spinal infection or tuberculosis, spinal deformity, malignancy, radiotherapy, recent use of antibiotics or corticosteroids, and psychological or psychiatric disorders; (2) Meta-analyses, case reports, reviews, technical notes, or abstracts only; and (3) Missing clinical data.
2.3 Quality assessment
Two independent reviewers used the Newcastle-Ottawa Scale (NOS) as a tool to assess the quality of the included studies, which were evaluated based on patient selection, group comparability, and the identification of outcomes of interest. Study quality was rated on a scale of 0 to 9, with low (1–3), medium (4–6), and high (7–9) ratings. Any discrepancy between the reviewers was resolved through consensus following discussion.
2.4 Data extraction
Two independent reviewers screened all titles and abstracts, selecting relevant articles for full-text review. Data were extracted from all eligible studies that met the inclusion criteria, including information on authorship, publication date, country of origin, patient type, sample size per factor, incidence of Modic changes, study design, and level of evidence. In cases where data were missing or unavailable, the corresponding authors were contacted. If the authors were unable to provide the necessary data, the study was excluded from the analysis.
2.5 Statistical analysis
Meta-analysis was performed on studies investigating the incidence of Modic changes in the lumbar spine and the associated risk factors. Statistical analyses and graphical representations were generated using Review Manager software (RevMan) version 5.4. Studies reporting odds ratios (ORs) were included in the meta-analysis. Heterogeneity was assessed using the I² statistic, with slight statistical heterogeneity defined as I² < 50%. Data were analyzed using a fixed-effects model, or a random-effects model if I² ≥ 50%. The estimated incidence was calculated as a combined proportion with a 95% confidence interval (CI).
3 Results
3.1 Search results
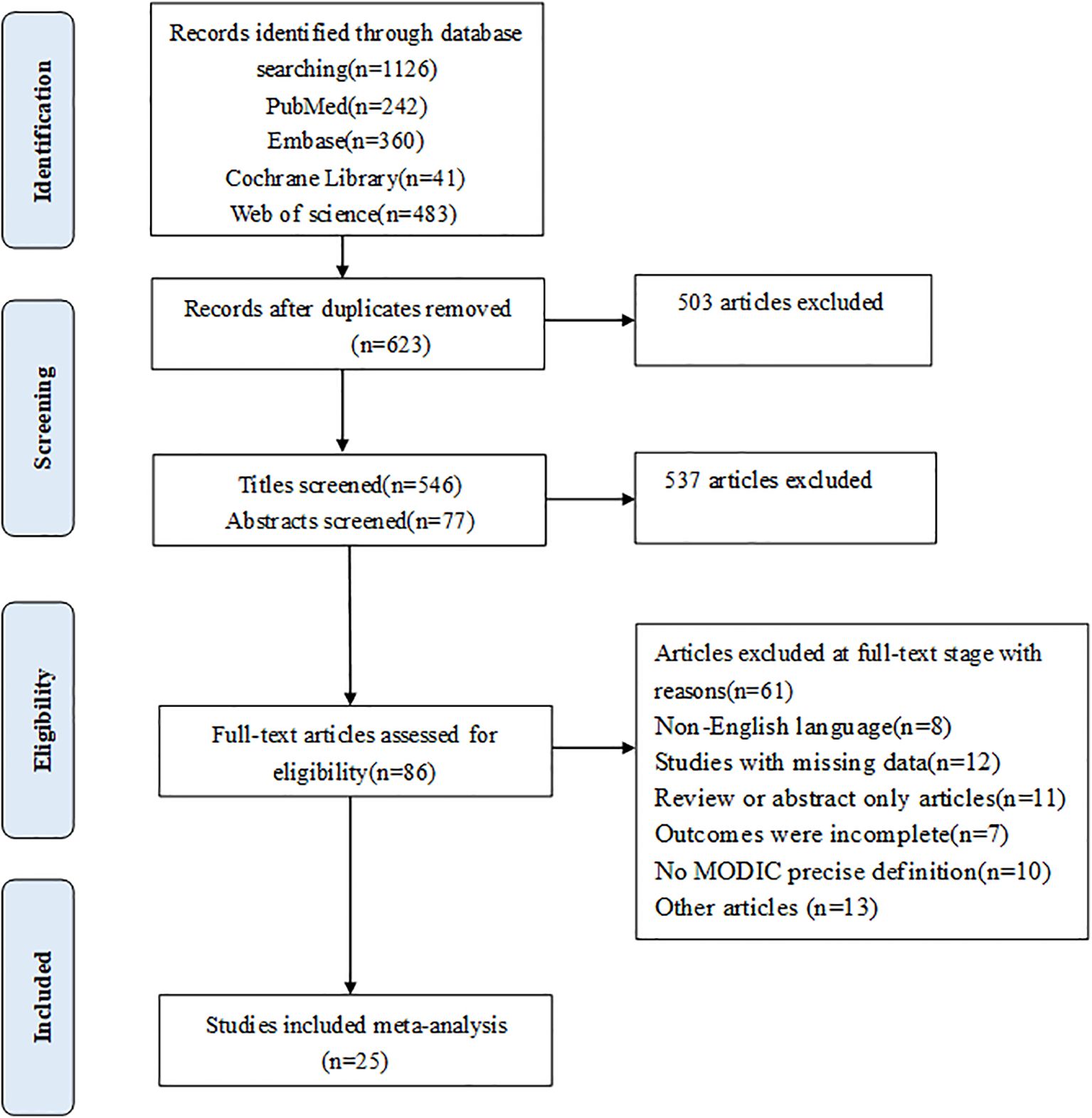
The study initially retrieved a total of 1,126 articles for review. Most of the articles were excluded based on the predefined inclusion criteria. Titles and abstracts were screened, and 86 potentially relevant papers were selected for further assessment (Figure 1). Ultimately, 25 studies met the inclusion criteria.
3.2 Characteristics of included studies
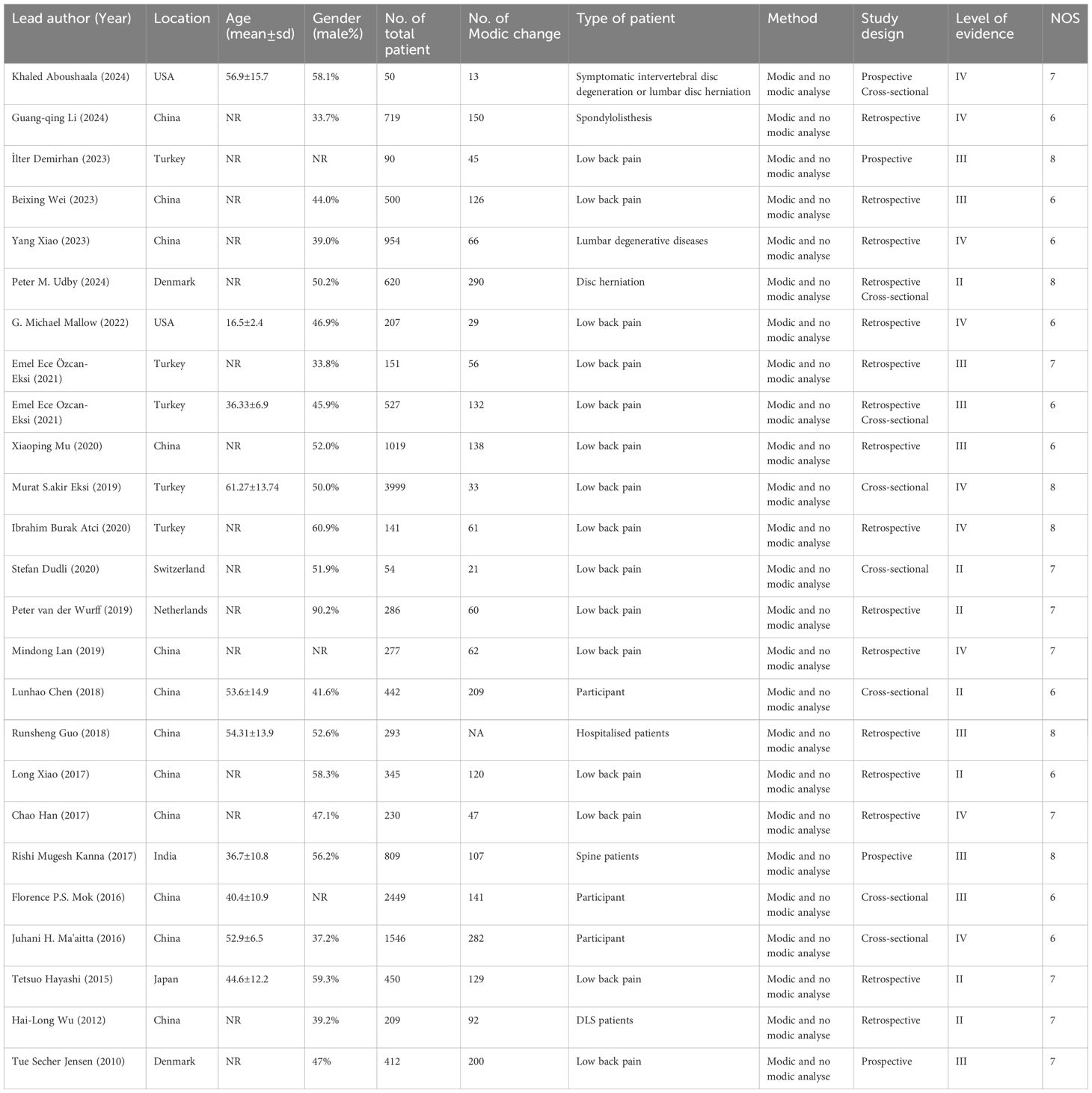
The 25 studies that met the inclusion criteria encompassed 10,440 individuals, including patients with low back pain and healthy participants aged 10–89 years. Of these studies, 4 were prospective, 16 were retrospective, and 8 were cross-sectional in design. Nineteen studies were conducted in Asia (twelve in China (9, 20, 21, 23, 26–33), five in Turkey (22, 34–37), one in India (38), one in Japan (39)), four in Europe (two in Denmark (40, 41), one in Switzerland (42), one in the Netherlands (43)), and two in the Americas (all in the U.S.A (44, 45).). The mean quality score obtained from the included studies based on the NOS criteria was 6.84 ± 0.80. According to the level of evidence ratings, seven studies were classified as level II, nine as level III, and nine as level IV (Table 2). According to the GRADE criteria, seven risk factors received high-level recommendations, whereas five were classified as moderate. The overall incidence of Modic changes in the lumbar spine across the studies was 35%, with 12 identified and quantified risk factors. The characteristics of the studies and patient demographics are presented in Table 2.
3.3 Incidence of modic changes
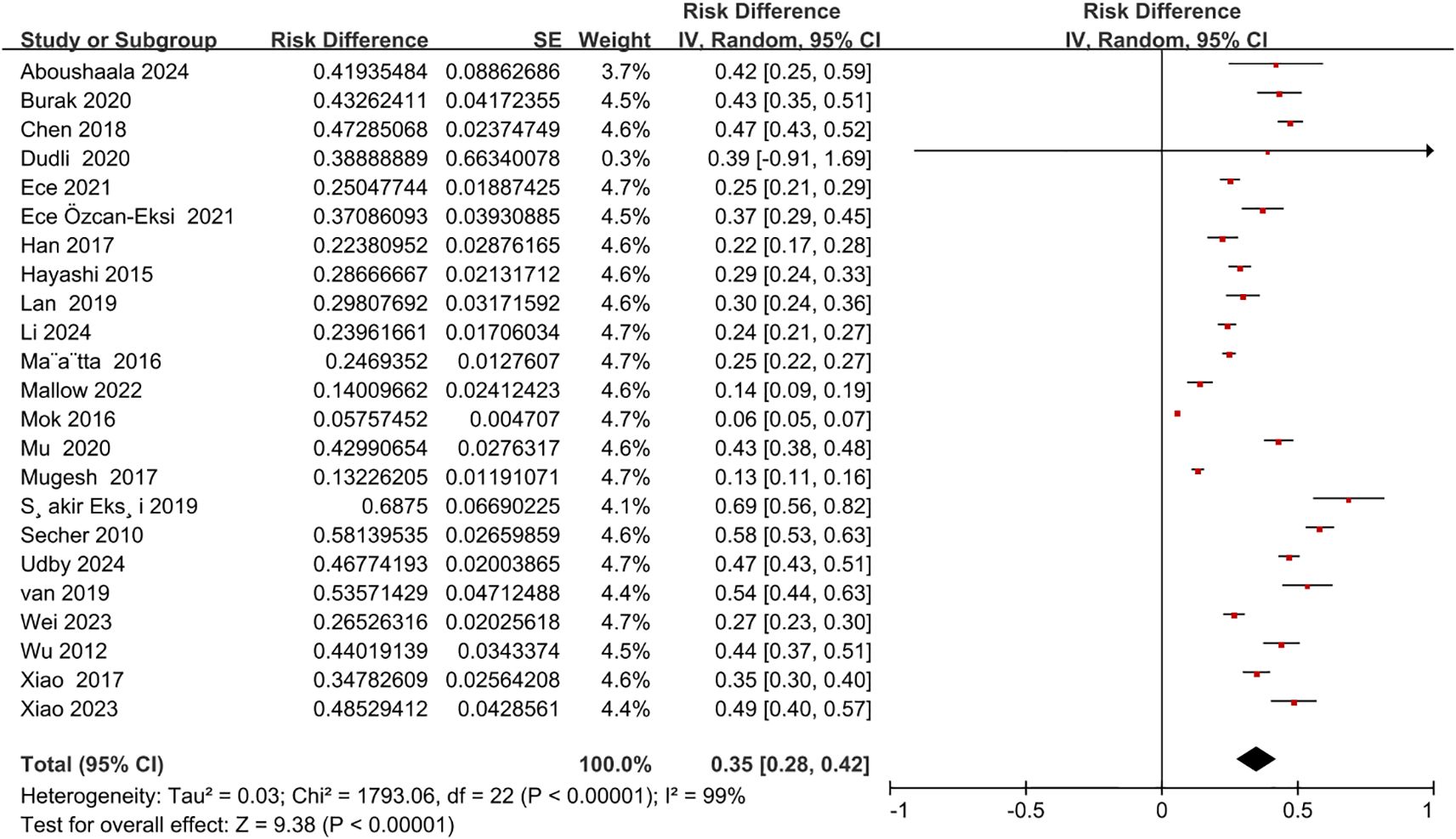
This meta-analysis pooled data from 25 studies, encompassing a total of 10,440 patients and healthy participants. The overall incidence of Modic changes in the lumbar spine was 35% (95% CI = 0.28 to 0.42; Z = 9.38; p < 0.00001; I² = 99%) (Figure 2).
3.4 Risk factors
Seventeen risk factors were identified, of which 12 were quantitatively analyzed based on the 25 studies included in the review. The risk factors identified in more than three studies included sex, age, smoking, BMI, disc degeneration, lumbar disc herniation, endplate changes, anterior lumbar lordosis angle, sacral angle, spondylolisthesis, segmental distribution, and physical labor.
3.5 Patient-related factors
3.5.1 Age
A total of 14 studies (9, 21, 23, 26, 29, 30, 33, 34, 36–38, 42, 44, 45) reported an association between age and the occurrence of Modic changes (Figure 3). The meta-analysis demonstrated that older patients were more likely to develop Modic changes than younger patients (OR = 4.01; 95% CI: 1.37 to 6.65; Z = 2.98; p = 0.003; I² = 96%; Figure 3). Based on the reviewed studies, we found moderate evidence suggesting older age as an important risk factor for Modic changes in the lumbar spine.
3.5.2 Physical labor
Three studies (32, 33, 41) reported correlations between physical labor and the occurrence of Modic changes (Figure 4). Analysis of the pooled data indicated that patients who engaged in physical labor were more likely to develop Modic changes. The meta-analysis revealed that Modic changes occurred in 15.43% of patients who engaged in physical labor and in 15.16% of patients who did not (OR = 1.81; 95% CI: 1.08 to 3.04; Z = 2.23; p = 0.03; I² = 70%; Figure 4). Therefore, we found minor evidence suggesting that engagement in physical labor is a risk factor for the development of Modic changes.
3.5.3 Sex, BMI, and smoking
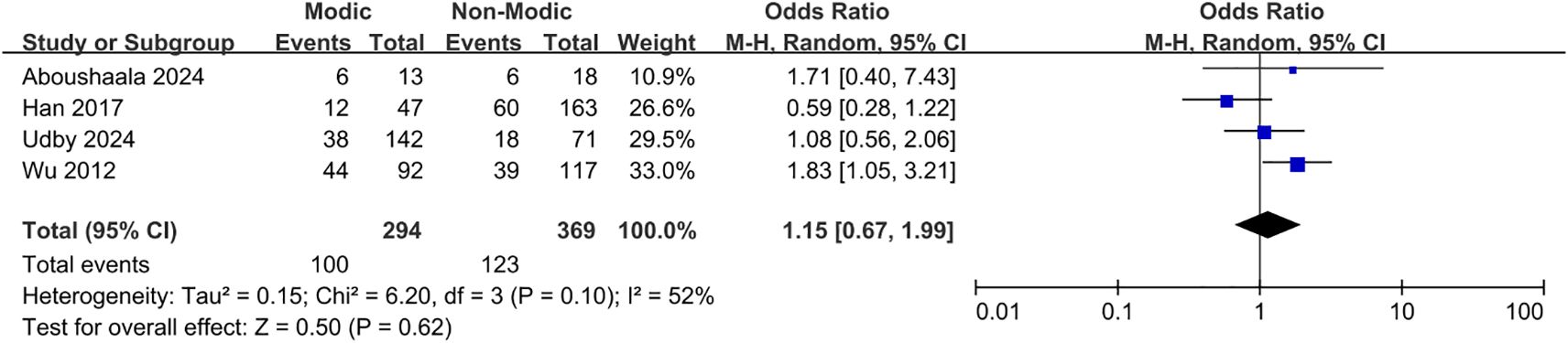
Sixteen studies (20–23, 26, 27, 30, 32, 33, 37, 38, 40, 42–45) demonstrated a correlation between sex and Modic changes, indicating that sex was not significantly associated with the occurrence of Modic changes (OR = 0.91; 95% CI = 0.80 to 1.04; Z = 1.38; p = 0.17; I² = 48%; Figure 5). Additionally, nine studies (9, 21, 23, 30, 34, 36, 42, 44, 45) investigated the relationship between BMI and Modic changes, and no significant correlation was found (OR = 1.07; 95% CI = -0.38 to 2.51; Z = 1.45; p = 0.15; I² = 95%; Figure 6). Four studies (27, 32, 40, 44) confirmed no significant correlation between smoking and the presence of Modic changes (OR = 1.15; 95% CI = 0.67 to 1.99; Z = 0.50; p = 0.62; I² = 52%; Figure 7). Consequently, this meta-analysis confirmed that sex, body mass index, and smoking were not significant risk factors for Modic changes in the lumbar spine.
3.6 Imaging-related factors
3.6.1 Degenerative discs
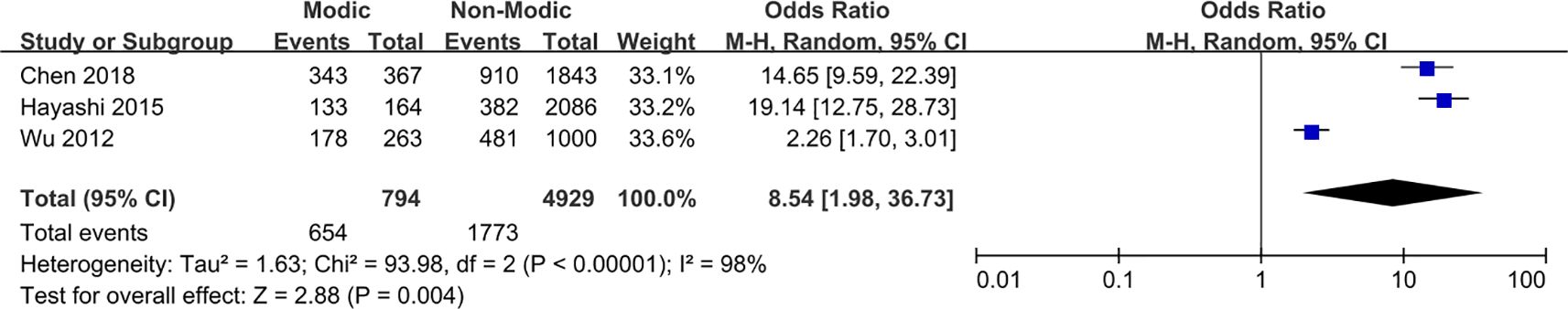
Three studies (27, 30, 39) reported an association between disc degeneration and Modic changes (Figure 8). The pooled data analysis indicated a correlation between the presence of disc degeneration and the occurrence of Modic changes in patients. The meta-analysis revealed that Modic changes occurred in 26.95% of patients with disc degeneration and 4.25% of patients without disc degeneration (OR = 8.54; 95% CI: 1.98 to 36.73; Z = 2.88; p = 0.004; I² = 98%; Figure 8). Consequently, this analysis provides moderate evidence that disc degeneration is an important risk factor for Modic changes in the lumbar spine.
3.6.2 Endplate changes
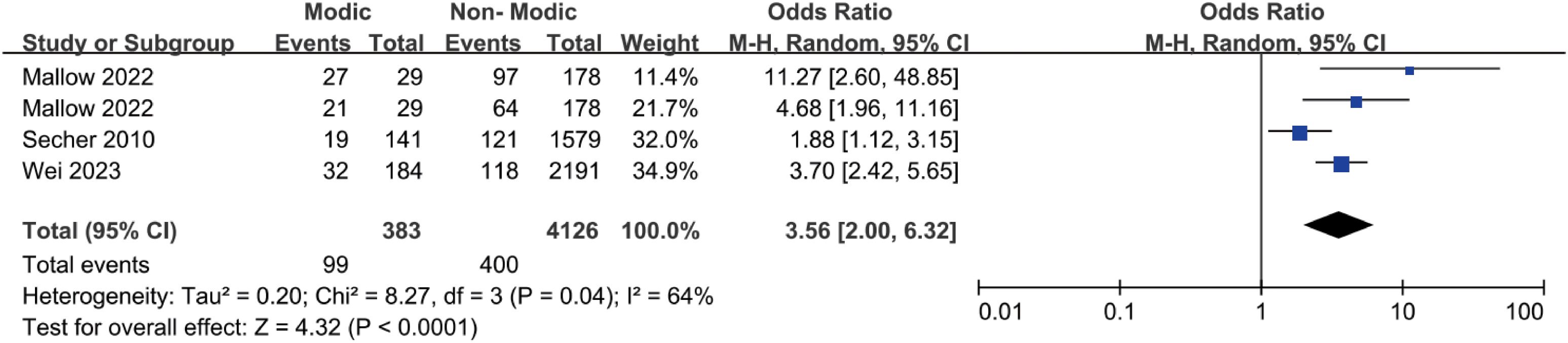
Three studies (20, 41, 45) reported an association between endplate changes and Modic changes (Figure 9). The pooled data analysis indicated a correlation between endplate changes and the occurrence of Modic changes in patients. The meta-analysis revealed that 19.84% of patients with endplate alterations developed Modic changes, compared to 7.08% of those without endplate alterations (OR = 3.56; 95% CI = 2.00 to 6.32; Z = 4.32; p < 0.0001; I² = 64%; Figure 9). Consequently, this analysis provides compelling evidence that endplate changes represent a key risk factor for Modic changes in the lumbar spine.
3.6.3 Lumbar lordosis angle
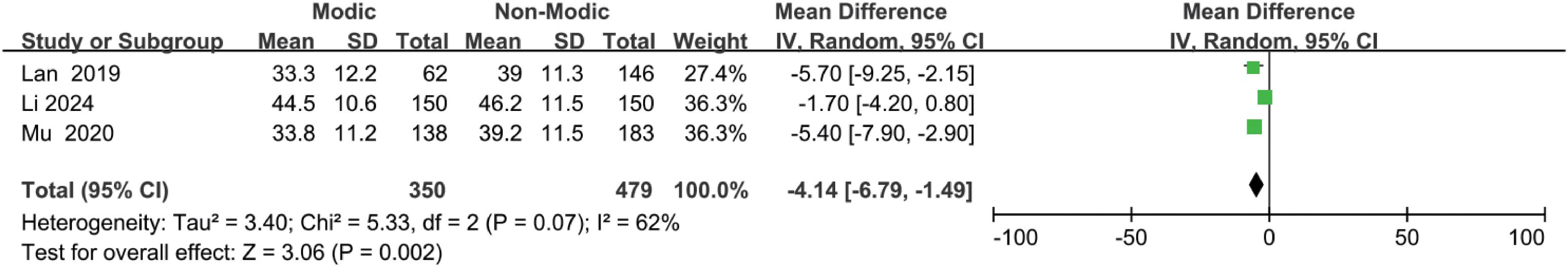
Three studies (21, 23, 29) reported an association between lumbar lordosis and Modic changes (Figure 10). The pooled data analysis indicated that patients with smaller anterior lumbar lordosis angles were more likely to exhibit Modic changes. The meta-analysis revealed that patients with smaller anterior lumbar lordosis angles were more likely to develop Modic changes, while those with larger anterior lumbar lordosis angles were less likely to do so (OR = -4.14; 95% CI = -6.79 to -1.49; Z = 3.06; p = 0.002; I² = 62%; Figure 10). Based on these results, we found moderate evidence suggesting that a reduced anterior lumbar lordosis angle appears to be an important risk factor for Modic changes in the lumbar spine.
3.6.4 Spondylolisthesis
Three studies (26, 44, 45) reported an association between spondylolisthesis and Modic changes (Figure 11). Pooled data analysis indicated that patients with spondylolisthesis were more likely to develop Modic changes, while the meta-analysis revealed that Modic changes occurred in 48.28% of patients with spondylolisthesis and 19.92% of those without spondylolisthesis (OR = 2.00; 95% CI = 1.12 to 3.58; Z = 2.33; p = 0.02; I² = 0%; Figure 11). Therefore, we found minor evidence suggesting that spondylolisthesis is a risk factor for Modic changes in the lumbar spine.
3.6.5 Lumbar disc herniation, segmental distribution, and sacral slope angle
Four studies (20, 26, 41, 45) investigated the correlation between lumbar disc herniation and Modic changes, indicating that lumbar disc herniation was not significantly associated with the presence of Modic changes (OR = 1.18; 95% CI = 0.57 to 2.44; Z = 0.45; p = 0.65; I² = 83%; Figure 12). Additionally, four studies (20, 22, 31, 35) reported no significant associations between segmental distribution and Modic alterations (OR = 0.83; 95% CI = 0.60 to 1.15; Z = 1.11; p = 0.27; I² = 63%; Figure 13). Furthermore, three studies (21, 23, 29) confirmed that the size of the sacral slope angle was not significantly associated with the presence of Modic alterations (OR = -2.25; 95% CI = -5.72 to 1.21; Z = 1.28; p = 0.20; I² = 88%; Figure 14). Therefore, this meta-analysis found no substantial evidence to confirm that lumbar disc herniation, segmental distribution, or sacral slope angle are significant risk factors for the development of Modic changes in the lumbar spine.
4 Discussion
This systematic review and meta-analysis yielded three key findings. First, the analysis determined a 35% incidence of Modic changes in the lumbar spine based on data from X studies. Second, strong evidence suggests that the risk factors associated with the development of Modic changes in the lumbar spine include advanced age, lumbar disc degeneration, endplate changes, spondylolisthesis, reduced anterior lumbar lordosis angles, and participation in physical labor. Third, no evidence was found linking sex, BMI, smoking, lumbar disc herniation, segmental distribution, or sacral angle to Modic changes in the lumbar spine.
Lower back pain associated with Modic changes, characterized by abnormal alterations in the vertebral endplates and sub-endplates, has garnered significant research attention. These changes appear as abnormal signals in the endplates on MRI. Modic changes can induce disabling lower back pain (46, 47). The present study demonstrated an incidence rate of 35% for Modic changes, higher than that in the general population, possibly due to the broader population range included in this study. However, since De Roos et al.’s initial study (12), research on its pathogenesis and risk factors has remained controversial. This meta-analysis provides robust evidence demonstrating an association between Modic changes and various factors, including age, disc degeneration, endplate changes, spondylolisthesis, the anterior lumbar lordosis angle, and physical labor.
The 14 studies included in this meta-analysis indicated that patients with Modic changes were generally older, consistent with most previous findings (9, 23, 30, 33, 36). However, Li et al. (21) reported that in patients with lumbar spondylolisthesis, Modic changes were more prevalent in younger individuals (mean age, 53.44 ± 9.80 years; n = 150) than in older individuals (mean age, 59.68 ± 9.66 years; n = 150). Mallow et al. (45) reported that Modic changes were present in a subset of adolescents (Modic group: 16.7 ± 2.2 years, n = 29; non-Modic group: 16.5 ± 2.4 years, n = 178). A focus on Modic changes in younger patients may hold significant potential for advancing our understanding of its pathogenesis and providing treatment strategies. Additionally, some researchers have reported no significant relationship between age and the development of Modic changes (26, 29, 42, 44). Definitive evidence from this meta-analysis suggests that older patients are more prone to Modic changes, which may be linked to the development of disc degeneration, spondylolisthesis, reduced vertebral stability, spinal stenosis, and osteoporosis; however, the specific causes and mechanisms underlying these associations remain unclear.
Studies consistently report that disc degeneration has the potential to trigger Modic changes. Eksi et al. (35) investigated the relationship between severe disc degeneration and Modic changes, concluding that this association is particularly strong in the lower lumbar region, with Modic changes detected in 88–90% of cases involving disc degeneration in this area. Wu et al. (27) identified disc degeneration as a risk factor for Modic changes, suggesting that patients with disc degeneration (27.0% [178/659]) are more likely to develop Modic changes than those without disc degeneration (14.1% [85/604]). Jensen et al. (41) found a strong correlation between disc degeneration and new-onset Modic changes, suggesting that disc degeneration may be a potential predictor for Modic alterations. The current meta-analysis of three studies found strong evidence of a significant correlation between disc degeneration and Modic changes, with a higher incidence of Modic changes in patients with disc degeneration (26.95% [654/2427]) than in those without (4.25% [140/3296]). This may be related to changes in angular motion, translational motion, and disc height in degenerated discs. However, the exact mechanism remains unclear, warranting further research to confirm this association.
Endplate changes included Schmorl’s nodes and endplate damage. The current meta-analysis, comprising three studies, demonstrated a higher incidence of Modic changes in patients with endplate changes (19.84% [99/499]) than in those without (7.08% [284/4010]). Jensen et al. (41) concluded that endplate changes were strongly associated with Modic changes, as indicated by a higher incidence of Modic changes in patients with endplate changes (13.57% [19/140]) than in those without (7.72% [122/1580]), suggesting that endplate changes could serve as a potential predictor. Similar findings were reported by Wei et al. (20), in which the incidence of Modic changes was higher in patients with endplate changes (21.33% [32/150]) than in those without endplate changes (6.83% [152/2225]). Mallow et al. (45) found a strong correlation between endplate changes and the presence of Modic changes, with the incidence of Modic changes being higher in patients with endplate changes (endplate damage, 21.8% [27/124]; Schmorl’s nodes, 24.71% [21/85]) than in those without endplate changes (endplate damage, 2.4% [2/83]; Schmorl’s nodes, 6.56% [8/122]). These studies suggest that the association between endplate changes and Modic changes is becoming increasingly evident. This association may be due to endplate changes that cause microstructural alterations in the disc and microfractures in the endplate, potentially leading to bacterial invasion. However, the specific mechanisms through which endplate changes influence Modic changes remain unclear and require further investigation.
Spondylolisthesis, physical labor, and anterior lumbar lordosis angles warrant attention. Wei et al. (20) found a strong correlation between lumbar spondylolisthesis and the occurrence of Modic changes, with a higher incidence in patients with spondylolisthesis (32.7% [32/98]) than in those without (6.7% [152/2277]); most Modic changes were characterized as Modic type II. Hayashi et al. (39) demonstrated that the incidence of Modic changes in patients with a spondylolisthesis degree greater than 0.8 mm (10.9% [119/1082]) was higher than in those with a spondylolisthesis degree less than or equal to 0.8 mm (3.85% [45/1168]), providing strong evidence of the correlation between spondylolisthesis severity and Modic changes. In study, Modic type II was identified as the most prevalent form of Modic change, and Modic change was more common in patients with spondylolisthesis (45). This is hypothesized to be associated with bone marrow changes and the disease’s developmental stage (48). Han et al. (32) concluded that the incidence of Modic changes was higher in patients who engaged in heavier physical labor (40.4% [23/57]) than in those who engaged in lighter physical labor (15.7% [24/153]). Additionally, Modic type III changes were more prevalent in patients who performed more rigorous physical labor, suggesting that physical labor can be considered a risk factor (32). This may be related to microinjuries of the vertebral endplates and fatigue degeneration caused by heavy physical labor, consistent with the findings of previous studies (49, 50). The anterior lumbar lordosis angle is a distinctive angle that has evolved in humans to maintain an upright posture (51). Xia et al. (52) concluded that the frequency of Modic changes was negatively correlated with the anterior lumbar lordosis angle, potentially owing to axial decompression of the vertebral body and alterations in endplate shear. However, Li et al. (21) found no significant correlation between Modic changes and the anterior lumbar lordosis angle. This meta-analysis demonstrated that spondylolisthesis, physical labor, and the anterior lumbar lordosis angle are strongly associated with Modic changes. Patients with spondylolisthesis exhibited a higher incidence of Modic changes (48.28% [42/87]) than those without spondylolisthesis (19.92% [50/251]). Similarly, individuals who engaged in physical labor had a higher incidence of Modic alterations (15.43% [100/648]) than those who did not engage in physical labor (15.16% [365/2407]). Additionally, patients with smaller anterior lumbar lordosis angles were more likely to exhibit Modic changes. These factors can be considered risk factors for Modic changes.
This review and meta-analysis had some limitations. Although 25 studies were included, their overall methodological quality was moderate, and the inclusion of lower-quality studies may have influenced the results. Subtype-specific analyses of Modic changes (Types I–III) were not conducted due to the insufficient data available from the included studies. Furthermore, significant heterogeneity was observed, indicating considerable inter-study variability. Future research should prioritize high-quality studies and employ more advanced methodologies.
5 Conclusion
The objective of this systematic review and meta-analysis was to determine the incidence and associated risk factors of Modic changes in the lumbar spine. The findings suggest an approximate incidence of 35%, with risk factors including advanced age, disc degeneration, endplate changes, spondylolisthesis, reduced anterior lumbar lordosis angles, and participation in physical labor.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
ZC: Formal Analysis, Software, Writing – original draft, Writing – review & editing. MZ: Writing – review & editing. JJ: Data curation, Formal Analysis, Writing – review & editing. GZ: Methodology, Software, Writing – review & editing. LL: Project administration, Supervision, Writing – review & editing. ZY: Software, Formal Analysis, Writing – review & editing. FZ: Conceptualization, Visualization, Writing – review & editing. XK: Conceptualization, Investigation, Visualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the National Natural Science Foundation of China (Grant No. 82272536), the Natural Science Foundation of Gansu province (Grant No. 24JRRA380), and the Qinghai Province “Kunlun Talents -High-end Innovation and Entrepreneurship Talents” Project in 2022 (QHKLYC-GDCXCY-2022-058).
Acknowledgments
We would like to thank Editage (www.editage.cn) for English language editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CI, confidence interval; OR, odds ratio; MRI, magnetic resonance imaging.
References
1. Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What low back pain is and why we need to pay attention. Lancet. (2018) 391:2356–67. doi: 10.1016/S0140-6736(18)30480-X
2. Knezevic NN, Candido KD, Vlaeyen JWS, Van Zundert J, and Cohen SP. Low back pain. Lancet. (2021) 398:78–92. doi: 10.1016/S0140-6736(21)00733-9
3. Massaad E, Mitchell TS, Duerr E, Kiapour A, Cha TD, Coumans JC, et al. Disparities in surgical intervention and health-related quality of life among racial/ethnic groups with degenerative lumbar spondylolisthesis. Neurosurgery. (2024) 95:576–83. doi: 10.1227/neu.0000000000002925
4. Rahyussalim AJ, Zufar MLL, and Kurniawati T. Significance of the association between disc degeneration changes on imaging and low back pain: A review article. Asian Spine J. (2020) 14:245–57. doi: 10.31616/asj.2019.0046
5. Wang Y, Zhang C, Cheng J, Yan T, He Q, Huang D, et al. Cutting-edge biomaterials in intervertebral disc degeneration tissue engineering. Pharmaceutics. (2024) 16(8):979. doi: 10.3390/pharmaceutics16080979
6. Liu Z, Qiao F, Liu D, Kong X, Liu K, Gu H, et al. Periplocin targets LRP4 to regulate metabolic homeostasis and anti-inflammation for the treatment of IVDD. Phytomedicine. (2025) 143:156885. doi: 10.1016/j.phymed.2025.156885
7. Lu Z and Zheng Z. Integrated analysis of single-cell and bulk RNA sequencing data identifies the characteristics of ferroptosis in lumbar disc herniation. Funct Integr Genomics. (2023) 23:289. doi: 10.1007/s10142-023-01216-8
8. Cholewicki J, Lee AS, Popovich JM Jr, Mysliwiec LW, Winkelpleck MD, Flood JN, et al. Degenerative spondylolisthesis is related to multiparity and hysterectomies in older women. Spine (Phila Pa 1976). (2017) 42:1643–7. doi: 10.1097/BRS.0000000000002178
9. Mok FP, Samartzis D, Karppinen J, Fong DY, Luk KD, and Cheung KM. Modic changes of the lumbar spine: prevalence, risk factors, and association with disc degeneration and low back pain in a large-scale population-based cohort. Spine J. (2016) 16:32–41. doi: 10.1016/j.spinee.2015.09.060
10. Kawabata S, Nagai S, Ito K, Takeda H, Ikeda D, Kawano Y, et al. Intradiscal administration of autologous platelet-rich plasma in patients with Modic type 1 associated low back pain: A prospective pilot study. JOR Spine. (2024) 7:e1320. doi: 10.1002/jsp2.1320
11. Crump KB, Alminnawi A, Bermudez-Lekerika P, Compte R, Gualdi F, McSweeney T, et al. Cartilaginous endplates: A comprehensive review on a neglected structure in intervertebral disc research. JOR Spine. (2023) 6:e1294. doi: 10.1002/jsp2.1294
12. de Roos A, Kressel H, Spritzer C, and Dalinka M. MR imaging of marrow changes adjacent to end plates in degenerative lumbar disk disease. AJR Am J Roentgenol. (1987) 149:531–4. doi: 10.2214/ajr.149.3.531
13. Modic MT, Steinberg PM, Ross JS, Masaryk TJ, and Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. (1988) 166:193–9. doi: 10.1148/radiology.166.1.3336678
14. Samartzis D, Mok FPS, Karppinen J, Fong DYT, Luk KDK, and Cheung KMC. Classification of Schmorl’s nodes of the lumbar spine and association with disc degeneration: a large-scale population-based MRI study. Osteoarthritis Cartilage. (2016) 24:1753–60. doi: 10.1016/j.joca.2016.04.020
15. Dudli S, Fields AJ, Samartzis D, Karppinen J, and Lotz JC. Pathobiology of modic changes. Eur Spine J. (2016) 25:3723–34. doi: 10.1007/s00586-016-4459-7
16. Modic MT, Masaryk TJ, Ross JS, and Carter JR. Imaging of degenerative disk disease. Radiology. (1988) 168:177–86. doi: 10.1148/radiology.168.1.3289089
17. Kuisma M, Karppinen J, Niinimäki J, Ojala R, Haapea M, Heliövaara M, et al. Modic changes in endplates of lumbar vertebral bodies: prevalence and association with low back and sciatic pain among middle-aged male workers. Spine (Phila Pa 1976). (2007) 32:1116–22. doi: 10.1097/01.brs.0000261561.12944.ff
PubMed Abstract | PubMed Abstract | Crossref Full Text | Google Scholar
18. Rajasekaran S, Ramachandran K, K SS, Kanna RM, and Shetty AP. From modic to disc endplate bone marrow complex - the natural course and clinical implication of vertebral endplate changes. Global Spine J. (2025) 15:196–209. doi: 10.1177/21925682241271440
19. Chen Y, Bao J, Yan Q, Wu C, Yang H, and Zou J. Distribution of Modic changes in patients with low back pain and its related factors. Eur J Med Res. (2019) 24:34. doi: 10.1186/s40001-019-0393-6
PubMed Abstract | PubMed Abstract | Crossref Full Text | Google Scholar
20. Wei B and Wu H. Study of the distribution of lumbar modic changes in patients with low back pain and correlation with lumbar degeneration diseases. J Pain Res. (2023) 16:3725–33. doi: 10.2147/JPR.S430792
21. Li GQ, Kang X, Li W, and Pei SS. Study and analysis of the correlation between lumbar spondylolisthesis and Modic changes. Front Surg. (2024) 11:1296275. doi: 10.3389/fsurg.2024.1296275
22. Özcan-Ekşi EE, Turgut VU, Küçüksüleymanoǧlu D, and Ekşi M. Obesity could be associated with poor paraspinal muscle quality at upper lumbar levels and degenerated spine at lower lumbar levels: Is this a domino effect? J Clin Neurosci. (2021) 94:120–7. doi: 10.1016/j.jocn.2021.10.005
23. Mu X, Peng W, Yu C, Xiong J, Wei J, Ou Y, et al. Modic changes of the lumbar spine-their association with the lumbar sagittal parameters: A retrospective imaging study. J Orthop Surg Res. (2020) 15:220. doi: 10.1186/s13018-020-01745-z
24. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int J Surg. (2021) 88:105906. doi: 10.1016/j.ijsu.2021.105906
25. Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. Bmj. (2017) 358:j4008. doi: 10.1136/bmj.j4008
26. Xiao Y, Xiu P, Yang X, Wang L, Li T, Gong Q, et al. Does preoperative modic changes influence the short-term fusion rate of single level transforaminal lumbar interbody fusion?-a matched-pair case control study. Orthop Surg. (2023) 15:2309–17. doi: 10.1111/os.13795
PubMed Abstract | PubMed Abstract | Crossref Full Text | Google Scholar
27. Wu HL, Ding WY, Shen Y, Zhang YZ, Guo JK, Sun YP, et al. Prevalence of vertebral endplate modic changes in degenerative lumbar scoliosis and its associated factors analysis. Spine (Phila Pa 1976). (2012) 37:1958–64. doi: 10.1097/BRS.0b013e31825bfb85
PubMed Abstract | PubMed Abstract | Crossref Full Text | Google Scholar
28. Xiao L, Ni C, Shi J, Wang Z, Wang S, Zhang J, et al. Analysis of correlation between vertebral endplate change and lumbar disc degeneration. Med Sci Monit. (2017) 23:4932–8. doi: 10.12659/MSM.904315
29. Lan M, Ou Y, Wang C, Wei W, Lu X, Wei J, et al. Patients with Modic type 2 change have a severe radiographic representation in the process of lumbar degeneration: a retrospective imaging study. J Orthop Surg Res. (2019) 14:298. doi: 10.1186/s13018-019-1355-y
PubMed Abstract | PubMed Abstract | Crossref Full Text | Google Scholar
30. Chen L, Hu X, Zhang J, Battié MC, Lin X, and Wang Y. Modic changes in the lumbar spine are common aging-related degenerative findings that parallel with disk degeneration. Clin Spine Surg. (2018) 31:312–7. doi: 10.1097/BSD.0000000000000662
31. Guo R, Yang X, Zhong Y, Lai Q, Gao T, Lai F, et al. Correlations between Modic change and degeneration in 3-joint complex of the lower lumbar spine: A retrospective study. Med (Baltimore). (2018) 97:e12496. doi: 10.1097/MD.0000000000012496
32. Han C, Kuang MJ, Ma JX, and Ma XL. Prevalence of Modic changes in the lumbar vertebrae and their associations with workload, smoking and weight in northern China. Sci Rep. (2017) 7:46341. doi: 10.1038/srep46341
33. Määttä JH, Karppinen J, Paananen M, Bow C, Luk KDK, Cheung KMC, et al. Refined phenotyping of modic changes: imaging biomarkers of prolonged severe low back pain and disability. Med (Baltimore). (2016) 95:e3495. doi: 10.1097/MD.0000000000003495
34. Demirhan İ, Oner E, Yuksel Z, Yuksel M, Belge Kurutas E, et al. Raftlin and 8-iso-prostaglandin F2α levels and gene network analysis in patients with Modic changes. Eur Spine J. (2023) 32:2368–76. doi: 10.1007/s00586-023-07757-7
PubMed Abstract | PubMed Abstract | Crossref Full Text | Google Scholar
35. Özcan-Ekşi EE, Yayla A, Orhun Ö, Turgut VU, Arslan HN, Ekşi M, et al. Is the distribution pattern of modic changes in vertebral end-plates associated with the severity of intervertebral disc degeneration?: A cross-sectional analysis of 527 caucasians. World Neurosurg. (2021) 150:e298–304. doi: 10.1016/j.wneu.2021.02.128
36. Ekşi M, Kara M, Özcan-Ekşi EE, Aytar MH, Güngör A, Özgen S, et al. Is diabetes mellitus a risk factor for modic changes?: A novel model to understand the association between intervertebral disc degeneration and end-plate changes. J Orthop Sci. (2020) 25:571–5. doi: 10.1016/j.jos.2019.09.005
37. Atci IB, Yilmaz H, Samanci MY, Atci AG, Karagoz Y, et al. The prevalence of lumbar paraspinal muscle fatty degeneration in patients with modic type I and I/II end plate changes. Asian Spine J. (2020) 14:185–91. doi: 10.31616/asj.2018.0333
38. Kanna RM, Shanmuganathan R, Rajagopalan VR, Natesan S, Muthuraja R, Cheung KMC, et al. Prevalence, patterns, and genetic association analysis of modic vertebral endplate changes. Asian Spine J. (2017) 11:594–600. doi: 10.4184/asj.2017.11.4.594
39. Hayashi T, Daubs MD, Suzuki A, Scott TP, Phan KH, Ruangchainikom M, et al. Motion characteristics and related factors of Modic changes in the lumbar spine. J Neurosurg Spine. (2015) 22:511–7. doi: 10.3171/2014.10.SPINE14496
PubMed Abstract | PubMed Abstract | Crossref Full Text | Google Scholar
40. Udby PM, Modic M, Elmose S, Carreon LY, Andersen M, Karppinen J, et al. The clinical significance of the modic changes grading score. Global Spine J. (2024) 14:796–803. doi: 10.1177/21925682221123012
41. Jensen TS, Kjaer P, Korsholm L, Bendix T, Sorensen JS, Manniche C, et al. Predictors of new vertebral endplate signal (Modic) changes in the general population. Eur Spine J. (2010) 19:129–35. doi: 10.1007/s00586-009-1184-5
42. Dudli S, Ballatori A, Bay-Jensen AC, McCormick ZL, O'Neill CW, Demir-Deviren S, et al. Serum biomarkers for connective tissue and basement membrane remodeling are associated with vertebral endplate bone marrow lesions as seen on MRI (Modic changes). Int J Mol Sci. (2020) 21. doi: 10.3390/ijms21113791
43. van der Wurff P, Vredeveld T, van de Graaf C, Jensen RK, and Jensen TS. Exploratory study for clinical signs of MODIC changes in patients with low-back pain in the Netherlands armed forces. Chiropr Man Therap. (2019) 27:5. doi: 10.1186/s12998-018-0229-4
44. Aboushaala K, Chee AV, Toro SJ, Vucicevic R, Yuh C, Dourdourekas J, et al. Discovery of circulating blood biomarkers in patients with and without Modic changes of the lumbar spine: a preliminary analysis. Eur Spine J. (2024) 33:1398–406. doi: 10.1007/s00586-024-08192-y
45. Mallow GM, Zepeda D, Kuzel TG, Barajas JN, Aboushaala K, Nolte MT, et al. ISSLS PRIZE in Clinical Science 2022: Epidemiology, risk factors and clinical impact of juvenile Modic changes in paediatric patients with low back pain. Eur Spine J. (2022) 31:1069–79. doi: 10.1007/s00586-022-07125-x
46. Munir S, Freidin MB, Rade M, Määttä J, Livshits G, and Williams FMK. Endplate defect is heritable, associated with low back pain and triggers intervertebral disc degeneration: A longitudinal study from twinsUK. Spine (Phila Pa 1976). (2018) 43:1496–501. doi: 10.1097/BRS.0000000000002721
PubMed Abstract | PubMed Abstract | Crossref Full Text | Google Scholar
47. Määttä JH, Wadge S, MacGregor A, Karppinen J, and Williams FM. ISSLS prize winner: vertebral endplate (Modic) change is an independent risk factor for episodes of severe and disabling low back pain. Spine (Phila Pa 1976). (2015) 40:1187–93. doi: 10.1097/BRS.0000000000000937
48. Ohtori S, Yamashita M, Yamauchi K, Inoue G, Koshi T, Suzuki M, et al. Change in Modic type 1 and 2 signals after posterolateral fusion surgery. Spine (Phila Pa 1976). (2010) 35:1231–5. doi: 10.1097/BRS.0b013e3181bde562
49. Leboeuf-Yde C, Kjaer P, Bendix T, and Manniche C. Self-reported hard physical work combined with heavy smoking or overweight may result in so-called Modic changes. BMC Musculoskelet Disord. (2008) 9:5. doi: 10.1186/1471-2474-9-5
50. Albert HB, Kjaer P, Jensen TS, Sorensen JS, Bendix T, and Manniche C. Modic changes, possible causes and relation to low back pain. Med Hypotheses. (2008) 70:361–8. doi: 10.1016/j.mehy.2007.05.014
51. Lee CH, Chung CK, Jang JS, Kim SM, Chin DK, and Lee JK. ‘Lumbar degenerative kyphosis’ Is not byword for degenerative sagittal imbalance: time to replace a misconception. J Korean Neurosurg Soc. (2017) 60:125–9. doi: 10.3340/jkns.2016.0607.001
Keywords: modic change, lumbar spine, lower back pain, meta-analysis, incidence, risk factor
Citation: Cao Z, Zhang M, Jia J, Zhang G, Li L, Yang Z, Zheng F and Kang X (2025) Incidence and risk factors for modic changes in the lumbar spine: a systematic review and meta-analysis. Front. Endocrinol. 16:1585552. doi: 10.3389/fendo.2025.1585552
Received: 28 February 2025; Accepted: 10 July 2025;
Published: 30 July 2025.
Edited by:
Federico Baronio, Dpt Hospital of Woman and Child, ItalyReviewed by:
Fulvio Tartara, University Hospital of Parma, ItalyMustafa Hızal, Abant Izzet Baysal University, Türkiye
Copyright © 2025 Cao, Zhang, Jia, Zhang, Li, Yang, Zheng and Kang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Feng Zheng, aHlkZ2syMDExQDE2My5jb20=; Xuewen Kang, ZXJ5X2thbmd4d0BsenUuZWR1LmNu
†These authors have contributed equally to this work
 Zhenyu Cao1,2,3†
Zhenyu Cao1,2,3† Guangzhi Zhang
Guangzhi Zhang Lei Li
Lei Li Xuewen Kang
Xuewen Kang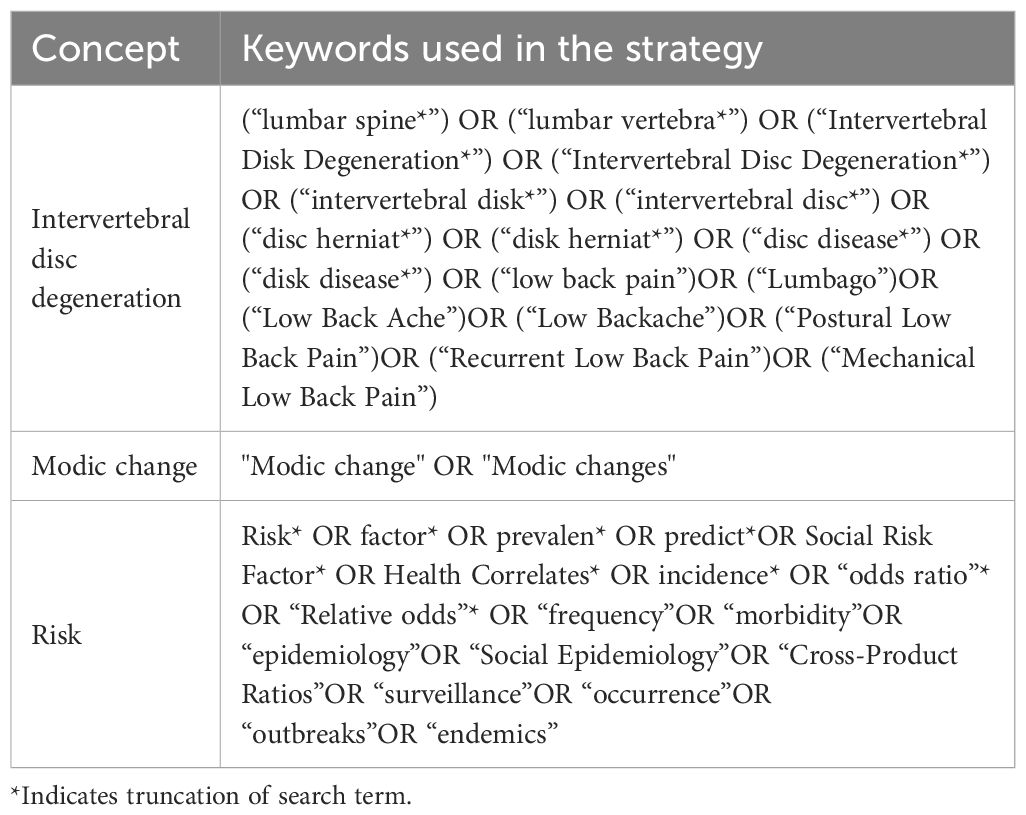
![Forest plot showing the mean differences between Modic and non-Modic groups across multiple studies. Each study's point estimate and confidence interval are depicted, with overall mean difference calculated at 1.07 [95% CI: -0.38, 2.51]. The heterogeneity statistics are Tau² = 3.99, Chi² = 155.67, df = 8, I² = 95%, with a p-value less than 0.00001.](https://www.frontiersin.org/files/Articles/1585552/fendo-16-1585552-HTML/image_m/fendo-16-1585552-g006.jpg)