- 1Department of Pharmacology, Faculty of Medicine, Sanaa University, Sanaa, Yemen
- 2Department of Pharmacy, Jiblah University for Medical and Health Science, Ibb, Yemen
- 3Department of Laboratory, Faculty of Medicine and Health Sciences, AL Nasser University, Sanaa, Yemen
- 4College of Medical Sciences, Azal University for Human Development, Sanaa, Yemen
Background: Diabetes mellitus is a major global health concern associated with serious complications. Effective management of blood glucose levels is crucial in reducing these complications.
Objectives: This study aimed to evaluate blood glucose management strategies among diabetic patients in general hospitals in Sana’a city, Yemen.
Methods: A cross-sectional study was conducted involving 50 diabetic patients. Data on demographics, risk factors, treatment adherence, lifestyle habits, and biochemical markers were collected through questionnaires and laboratory tests. Statistical analysis was performed using SPSS.
Results: The study found a higher prevalence of diabetes among males, individuals aged 41–60 years, married persons, and those who were illiterate. “Type 2 Diabetes Mellitus was more common than insulin-dependent diabetes mellitus (IDDM) (80% vs. 20%). Laboratory monitoring was the most commonly used management strategy, while adherence to treatment, exercise, and nutrition was lower. Patients adhering to treatment, exercise, and nutrition therapy showed significantly better clinical and biochemical profiles, including lower LDL, triglycerides, total cholesterol, HbA1c, fasting blood sugar, BMI, and blood pressure levels. The prevalence of diabetes complications was lower among patients who followed management protocols.
Conclusions: Regular treatment adherence, exercise, nutrition therapy, and laboratory monitoring contribute to improved blood glucose control and reduce diabetes-related complications. Enhancing patient education and adherence to management strategies is essential for better clinical outcomes.
Introduction
Diabetes mellitus (DM) is a very common metabolic disease characterized by high glucose levels in the blood due to dysfunction in the pancreas to produce sufficient amounts of insulin hormone. Diabetes Mellitus (DM) is likely one of the oldest diseases recognized by humanity. The earliest documentation of this condition can be traced back to an Egyptian manuscript dating approximately 3,000 years ago (1) Treatment of almost all types of DM became available when insulin was discovered and produced in 1921 (2). Management of type 2 diabetes mellitus can be achieved through lifestyle modifications, dietary changes, and the implementation of available pharmacological treatments (3). Diabetes mellitus significantly contributes to morbidity, ranking as one of the leading causes of renal failure, blindness, and limb amputation in adults. Additionally, it plays an often-underestimated role in overall mortality (4). The origin and etiology of diabetes mellitus can vary significantly, but they consistently involve defects in either insulin secretion or insulin resistance at some stage of disease progression. Patients with diabetes mellitus typically present with either type 1 diabetes immune mediated or idiopathic or type 2 diabetes mellitus, previously referred to as non-insulin-dependent diabetes mellitus. Type 2 diabetes is the most prevalent form of the condition, characterized by hyperglycaemia, insulin resistance, and relative insulin deficiency (ADA) (3) Research indicates that rigorous metabolic management may postpone or prevent the development of complications associated with diabetes (5). The results of large randomized trials involving individuals with type 1 diabetes or newly diagnosed or established type 2 diabetes demonstrate that effective glycaemic control can delay the onset and slow the progression of microvascular complications, such as nephropathy, retinopathy, and neuropathy (6). The needs of diabetic patients extend beyond achieving adequate glycaemic control. Effective management also includes preventing complications, limiting disability, and facilitating rehabilitation. Maintaining blood glucose levels within the target range is a primary goal in the treatment of diabetes mellitus. Data from the Diabetes Control and Complications Trial (DCCT Research Group) show that in individuals with type 1 diabetes, a 10% reduction in glycated hemoglobin (GHb) levels was associated with a 43% decrease in the risk of retinopathy progression (7). Findings from the Gallichan study, further indicated that morbidity associated with diabetes mellitus—as well as the use of healthcare resources for managing diabetic complications—could potentially be reduced by significantly improving blood glucose control (8). Although various methods exist for blood glucose monitoring, the associated costs can be substantial. Gallichan estimated that the annual cost of self-monitoring by diabetes mellitus patients within the National Health Service (NHS) was approximately £42 million (8) Factors to consider when establishing glycaemic goals include psychosocial limitations (9). In patients with hypoglycaemia unawareness, glycaemic targets should be adjusted to less stringent levels over extended periods, with the aim of potentially reversing the condition (10). For patients with severe comorbidities that may hinder management strategies, the objective shifts to preventing clinically significant glycosuria, fluid and electrolyte loss, infections, and the onset of non-ketotic hyperosmolar coma. Insulin is prescribed for individuals with type 1 diabetes and for those with type 2 diabetes who exhibit insulinopenia and do not respond adequately to dietary therapy or oral hypoglycaemic agents (11). In such cases, insulin therapy may be the most effective method for reducing blood glucose levels (12). A significant proportion of patients with type 2 diabetes will ultimately require insulin therapy. Due to insulin resistance, these patients may need doses exceeding 1 unit per kilogram of body weight per day (13). Recent studies suggest that hyperglycaemia in hospital settings is not a benign condition. Intensive treatment of diabetes and hyperglycaemia has been associated with reduced morbidity and mortality. Evaluations of inpatient hyperglycaemia management have emphasized the importance of glycaemic control in improving hospital outcomes (14) The overarching goal of diabetes management is to maintain blood glucose levels near normal while avoiding hypoglycaemia, with an HbA1c target typically between 7% and 8% (15). This is generally achieved through a combination of dietary modification, physical activity, weight loss, and appropriate use of medications, including insulin and oral agents. Complications occur less frequently and are less severe in individuals who maintain good glycaemic control. Type 1 diabetes must be managed with insulin injections. In contrast, the prevention and treatment of type 2 diabetes involve following a healthy diet, regular physical activity, maintaining a normal body weight, and avoiding tobacco use. Pharmacological treatment may include insulin sensitizers, with or without insulin (16). Additionally, managing blood pressure and ensuring proper foot and eye care are critical components of diabetes management (17).
Methodology
Study design
The investigation utilized a cross-sectional study design. Conducted in several general hospitals, including Al-Kuwait, Alsabeen, Republic, and 48, other hospitals located in Sana’a city, Yemen. The study population comprised all individuals diagnosed with diabetes mellitus at the participating hospitals, with a total of 50 diabetic patients prospectively enrolled, ranging in age from 21 to 90 years.
Inclusion criteria
This study included all patients with diabetes mellitus who consented to participate, met the inclusion criteria, and were hospitalized on the days of the student researchers’ visits.
Exclusion criteria
The study excluded patients who refused to withdraw their samples or complete questionnaires, as well as those with hyperthyroidism, pancreatitis, Cushing’s syndrome, glucagonoma, heart attack, or who were taking glucose-raising medications such as estrogen, glucagon, prednisone, or oral contraceptives.
Data collection
The survey included a self-interview and an administered questionnaire with the diabetic patients. The questionnaire was designed to include personal information like name, age, sex, occupation, address, and level of education, as well as information about daily habits and diets, clinical information like weight, height, and blood pressure, medical histories of other diseases, and risk factors and complications related to DM.
Limitation
This study has several limitations that should be considered when interpreting the findings. First, the relatively small sample size of 50 diabetic patients limits the statistical power of the analysis and reduces the generalizability of the results to the wider diabetic population in Sana’a city and Yemen. Secondly, the recruitment was limited to hospitalized patients present during the researchers’ visits, which may introduce selection bias by overrepresenting patients with more severe disease or complications. This sampling method limits the applicability of findings to community-dwelling or outpatient diabetic populations who might have different management experiences and outcomes.
Additionally, the cross-sectional design provides only a snapshot of diabetes management and does not allow for assessment of causal relationships or changes over time. Self-reported data on treatment adherence, exercise, and nutrition may be subject to recall bias or social desirability bias, potentially affecting the accuracy of reported behaviors.
Finally, some biochemical and clinical parameters were measured only once, which may not fully capture fluctuations in blood glucose control or other metabolic variables.
Future studies should address these limitations by including larger, randomized, and more diverse patient populations, employing longitudinal designs, and incorporating objective measures of adherence and glycemic control.
Statistical analysis
The data were analyzed using SPSS Version 20 (Statistical Package for the Social Sciences), checked for normal distribution, and expressed as percentages, mean ± SD. Independent sample T tests and Chi-square tests were employed to assess differences in variables, while risk factors were estimated using odds ratios (OR) through binary logistic regression. ANOVA was used to look at the important connections between the parameters. Differences were considered significant when the P-value was less than 0.05.
Results
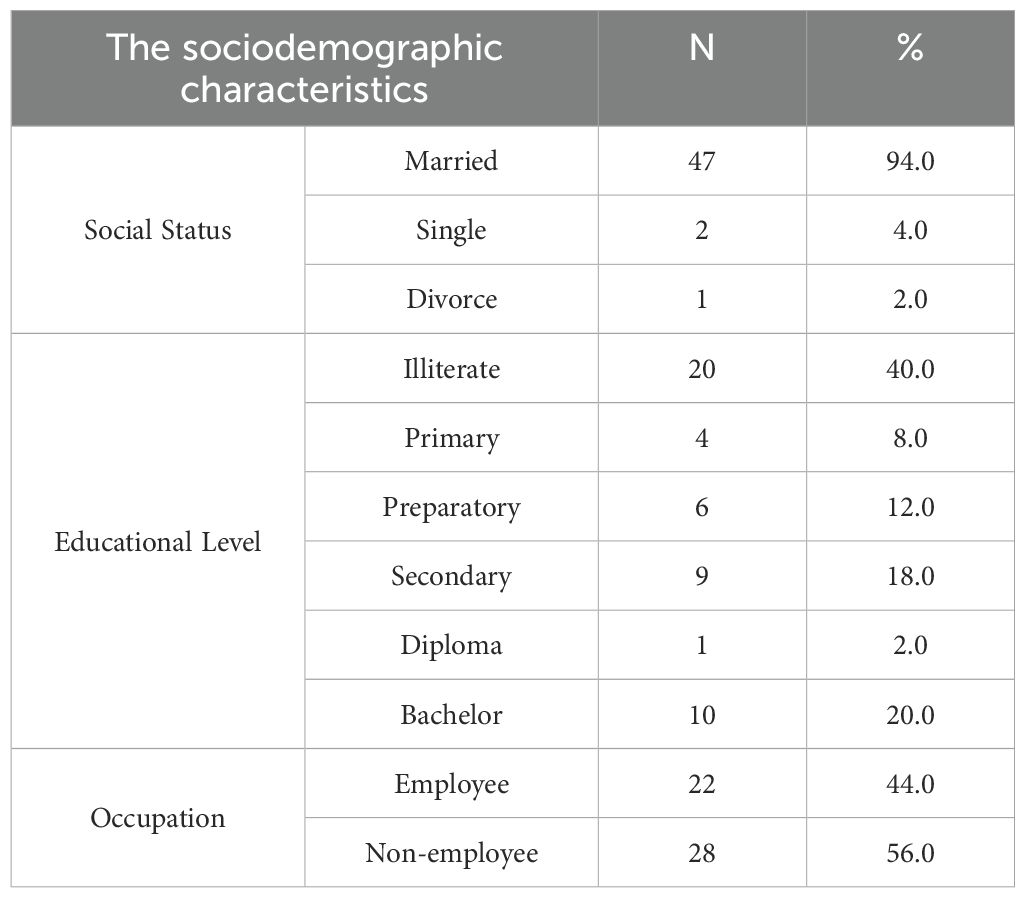
Table 1 indicates that a significant proportion of patients were married (94%), unemployed (56%), and illiterate (40%). The age group most affected was 41–60 years, comprising 52% of cases, with a slight predominance observed among males at 52%. These factors indicate a possible association between socioeconomic vulnerability and diabetes prevalence.
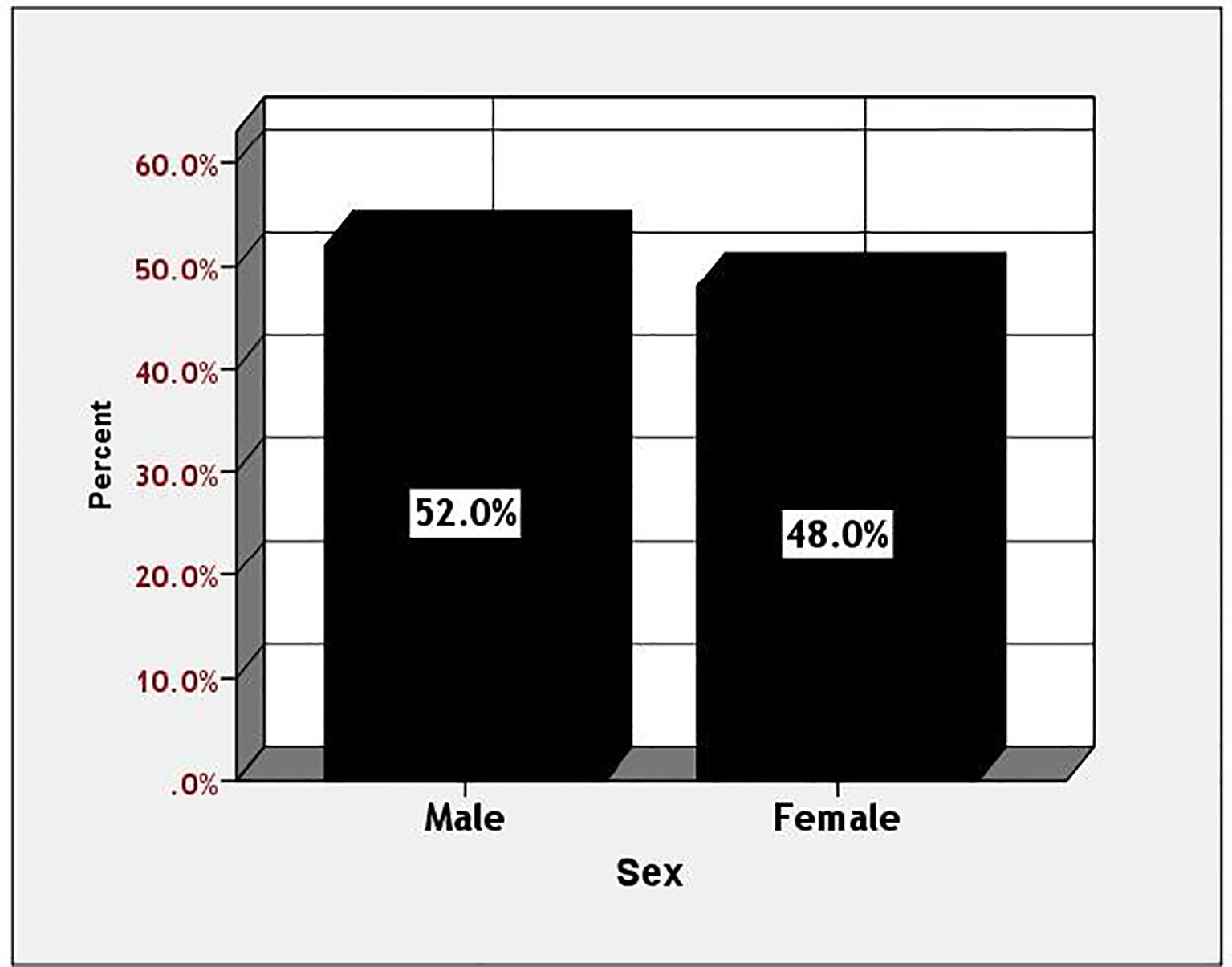
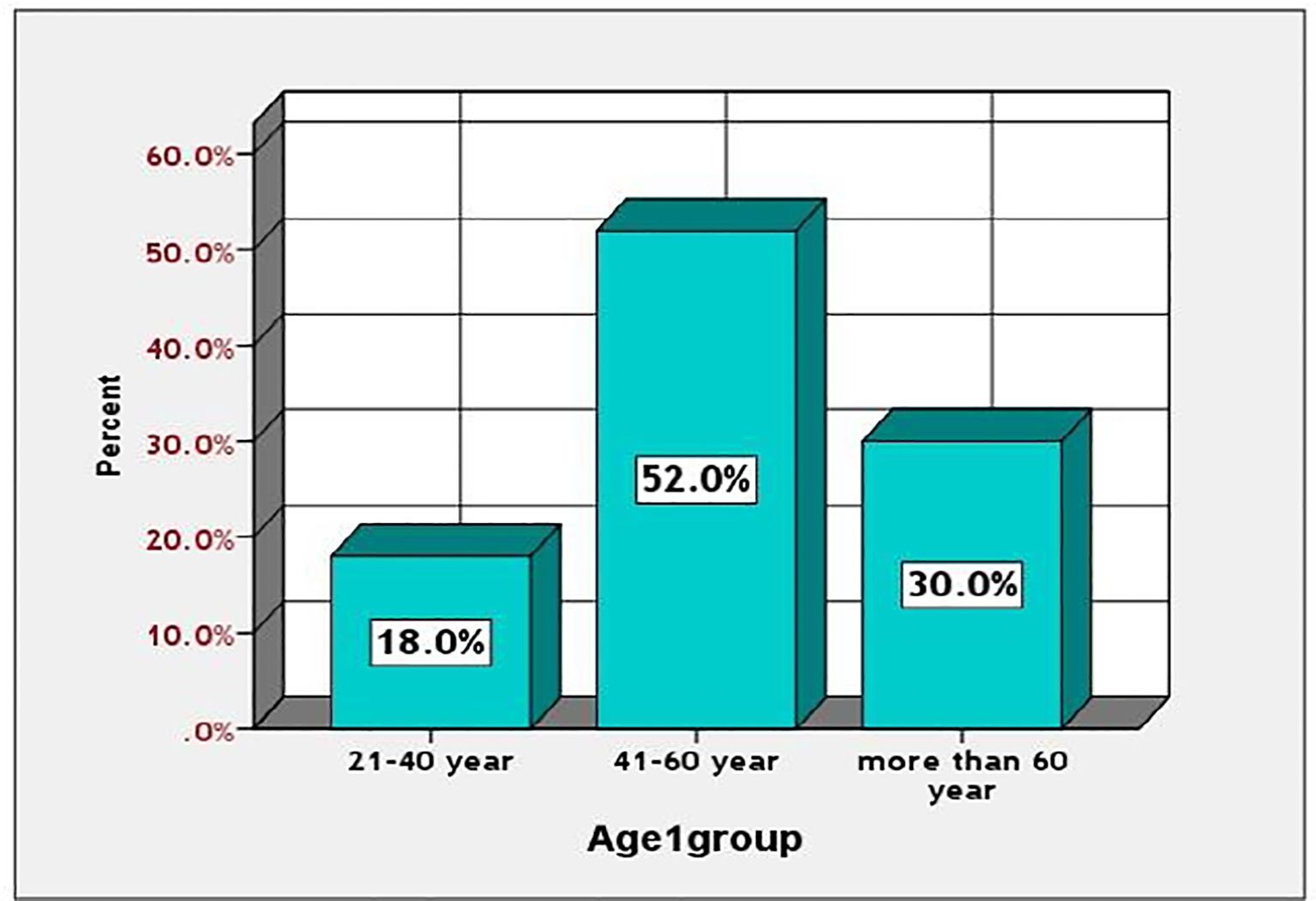
Among diabetic patients, those aged 41 to 60 exhibited a significantly higher prevalence of diabetes mellitus (52%), compared to 18% in the 21 to 40 age group and 30% in individuals over 60. The prevalence was greater in men compared to women (52% versus 48%). This information is illustrated in Figures 1, 2.
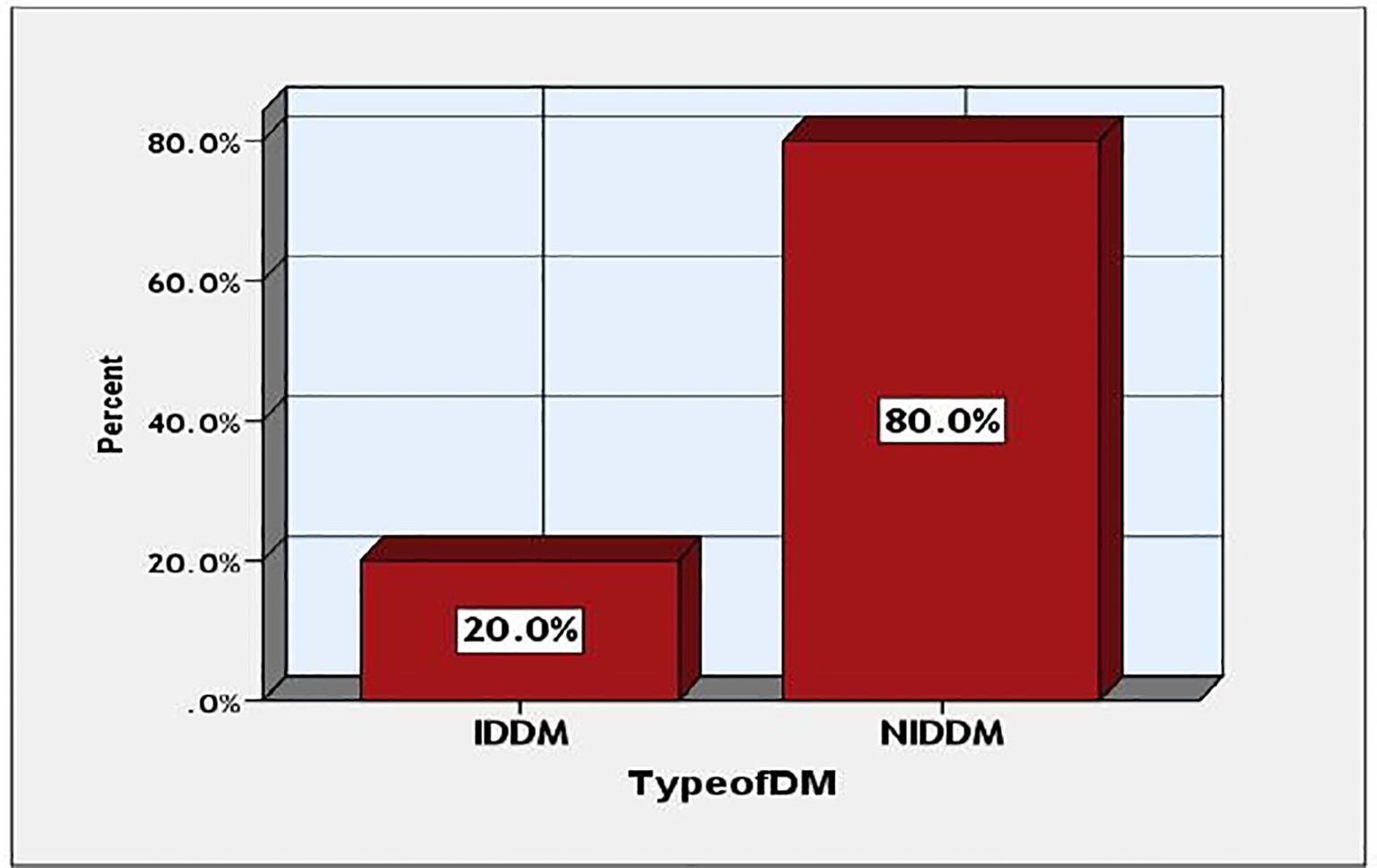
This study examines the prevalence of various forms of diabetes among the participants. The data indicates that type 2 diabetes mellitus was significantly more prevalent than IDDM, with occurrences of 40 (80%) against 10 (20%), as illustrated in Figure 3.
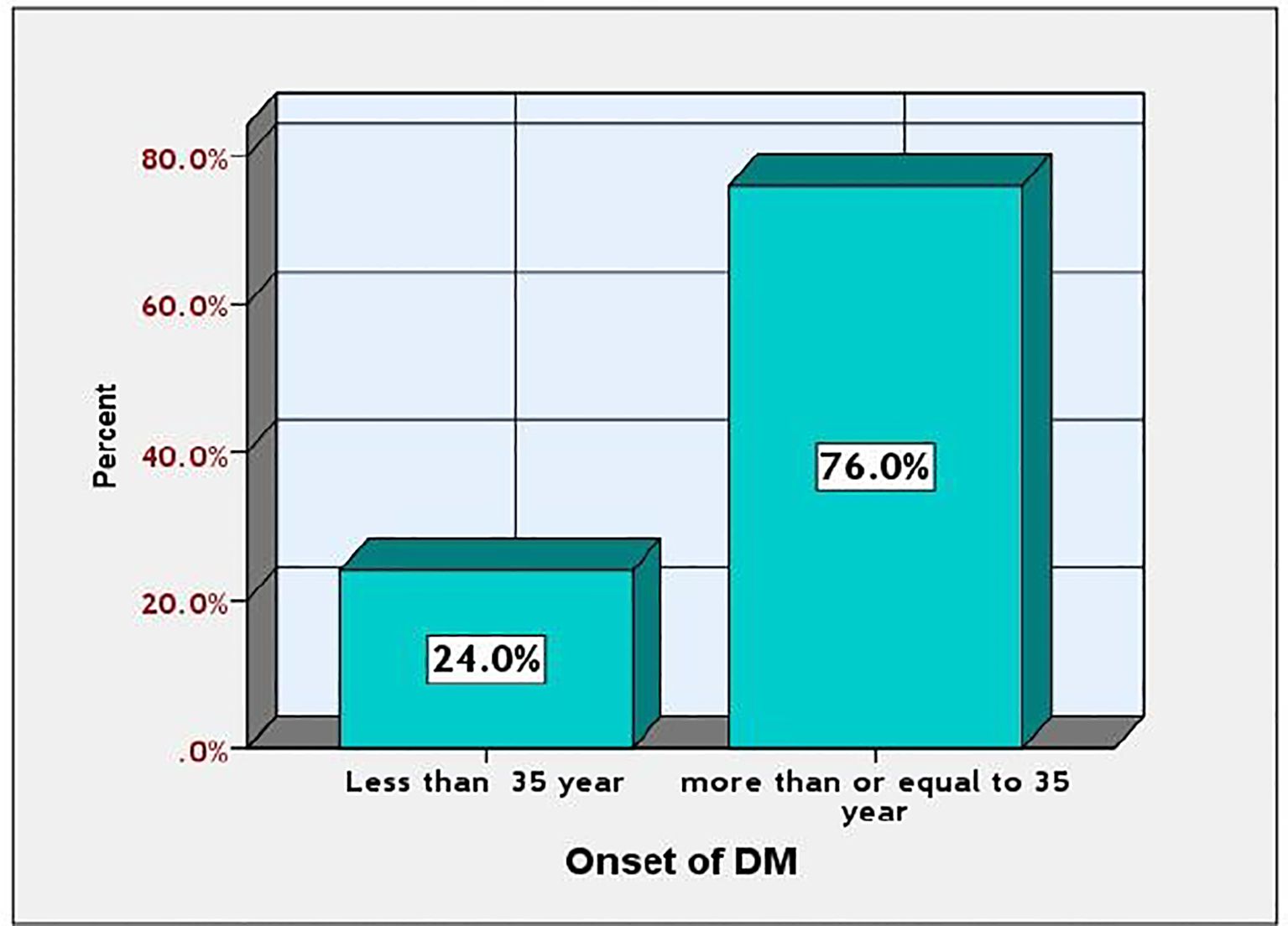
Figure 4 illustrates the onset rate of diabetes mellitus (DM) among the studied diabetic patients. Diabetes mellitus (DM) prevalence was higher in individuals aged 35 and older compared to those younger than 35, with rates of 38.76% and 12.24%, respectively.
Table 2 indicates that oral antidiabetic drugs were the most frequently utilized, accounting for 44%, followed by antihypertensives at 22%, insulin at 20%, and combination therapies at 14%. This corresponds with the elevated prevalence of type 2 diabetes mellitus and indicates a preference for pharmacological treatment rather than lifestyle modifications.
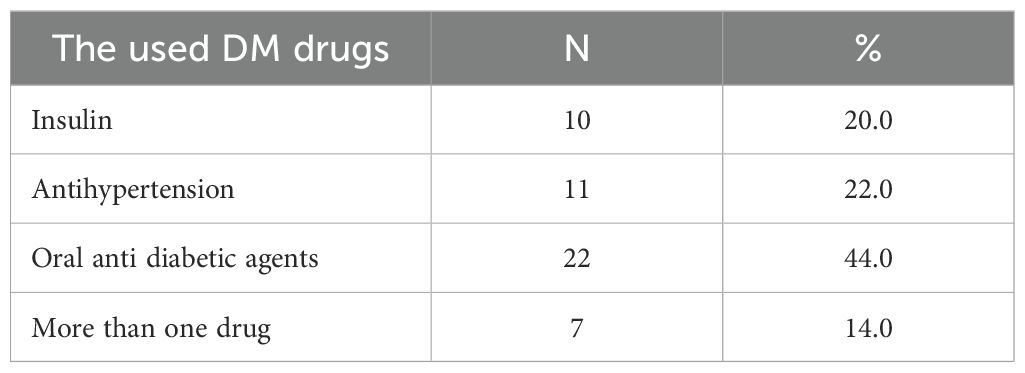
Table 2. Identify different type of the used DM drugs and their prevalence among the studied diabetic patients.
Table 3 indicates that lab monitoring was significantly more prevalent in males (88.4%) compared to females (62.5%, p = 0.040). Other strategies, including exercise, treatment regulation, and nutrition therapy, exhibited no significant gender differences, suggesting possible disparities in access to diagnostic services.
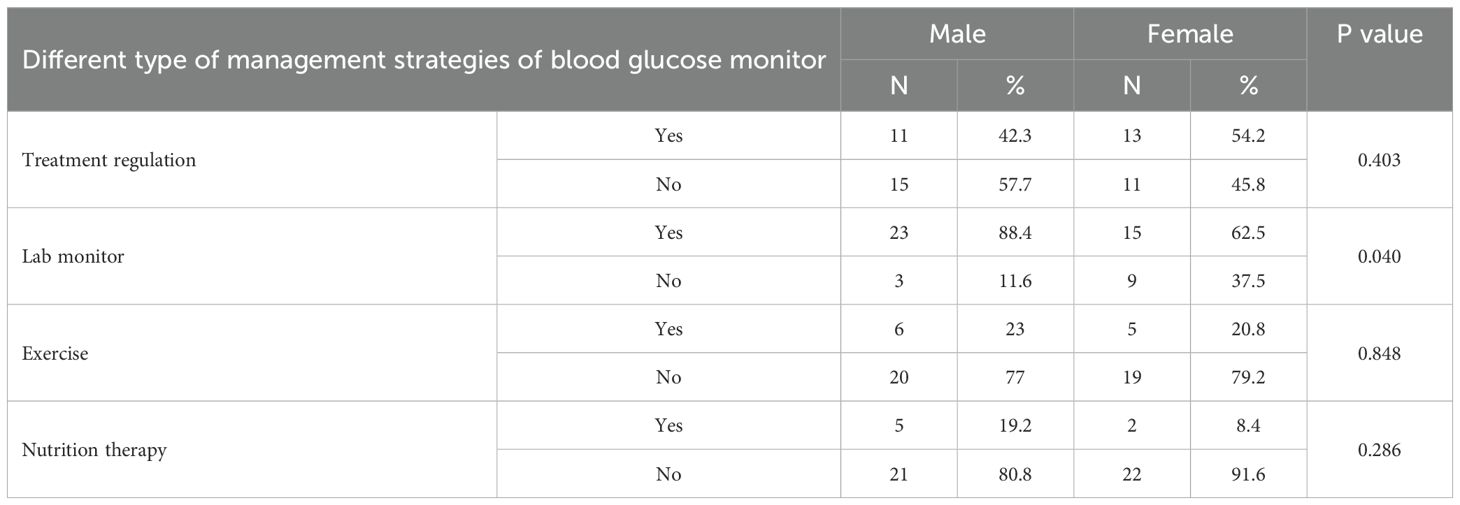
Table 3. Distribution different type of management strategies of blood glucose level control among the studied diabetic patients according to the sex.
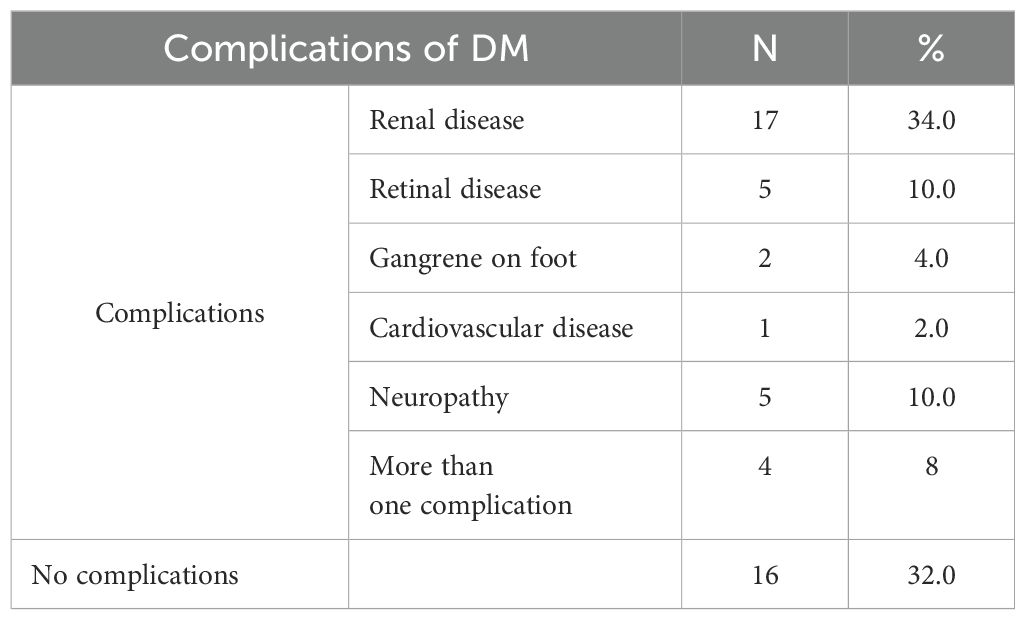
Table 4 indicates a significant complication rate of 68%, with renal disease at 34% as the most prevalent, followed by retinopathy and neuropathy, each at 10%. This tables underscores the necessity for enhanced glycaemic regulation and prompt identification of complications.
Table 5 indicates that BMI was significantly elevated in type 2 diabetic patients (28.2 vs. 20.0, p = <0.001). Other markers, including LDL, HDL, HbA1c, and FBS, were elevated in both groups; however, no statistically significant differences were observed. The findings underscore the significance of obesity in the context of type 2 diabetes.
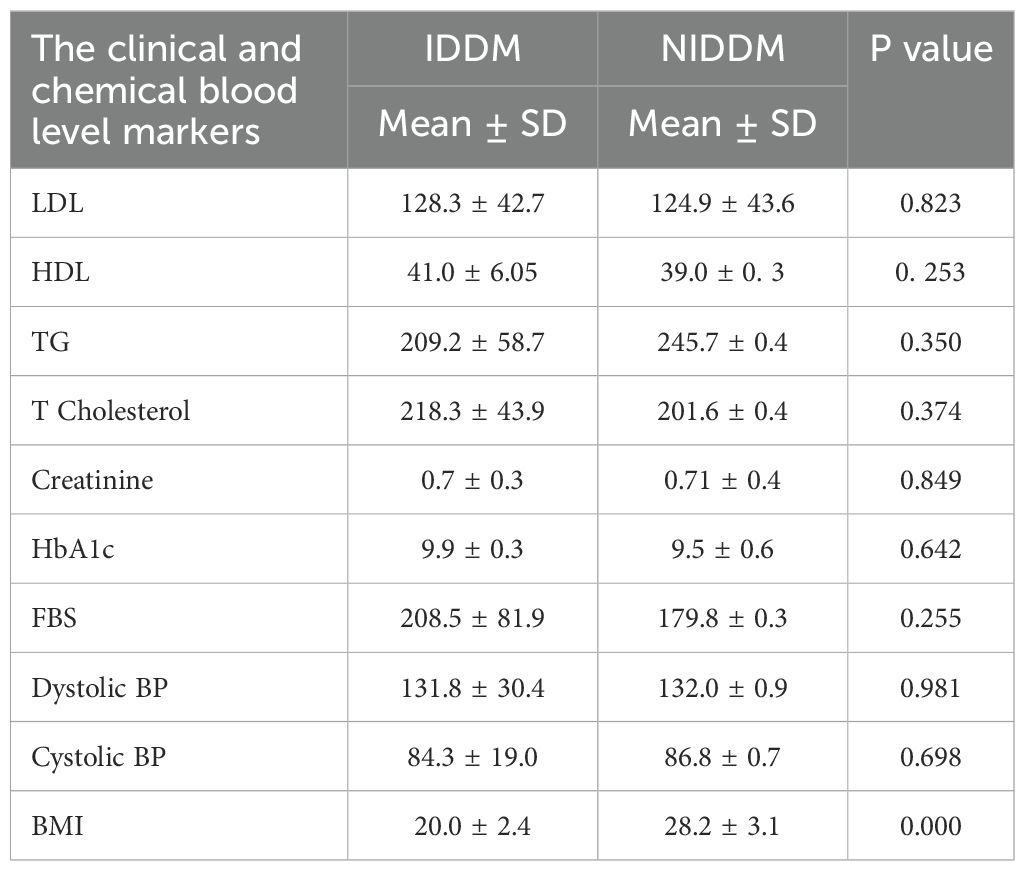
Table 5. Mean of The clinical and biochemical blood level markers among the studied diabetic patients. .
Table 6 indicated that the prevalence of positive urine ketone bodies was significantly higher in IDDM patients (30% compared to 2.5%, p = <0.001, OR = 16.714), thereby identifying IDDM as a risk factor for ketosis. Additional markers such as proteinuria and glycosuria were more common in type 2 diabetes mellitus; however, they did not reach statistical significance.
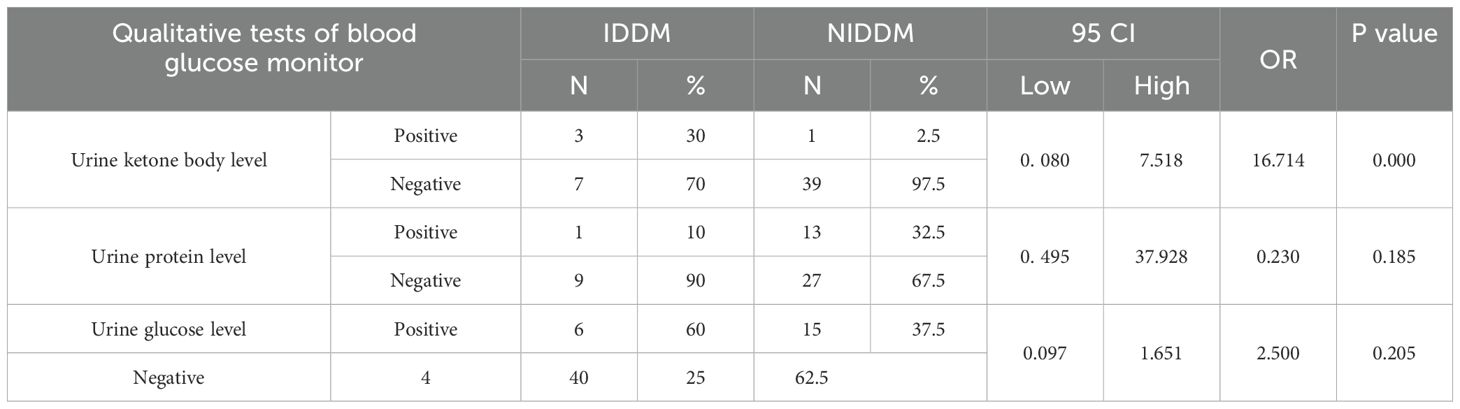
Table 6. Results of qualitative tests of blood glucose level control among the studied diabetic patients.
Table 7 indicates that patients adhering to treatment exhibited significantly lower systolic blood pressure (83.2 vs. 89.0 mmHg, p = 0.022) and diastolic blood pressure (129.9 vs. 133.8 mmHg, p = 0.032).
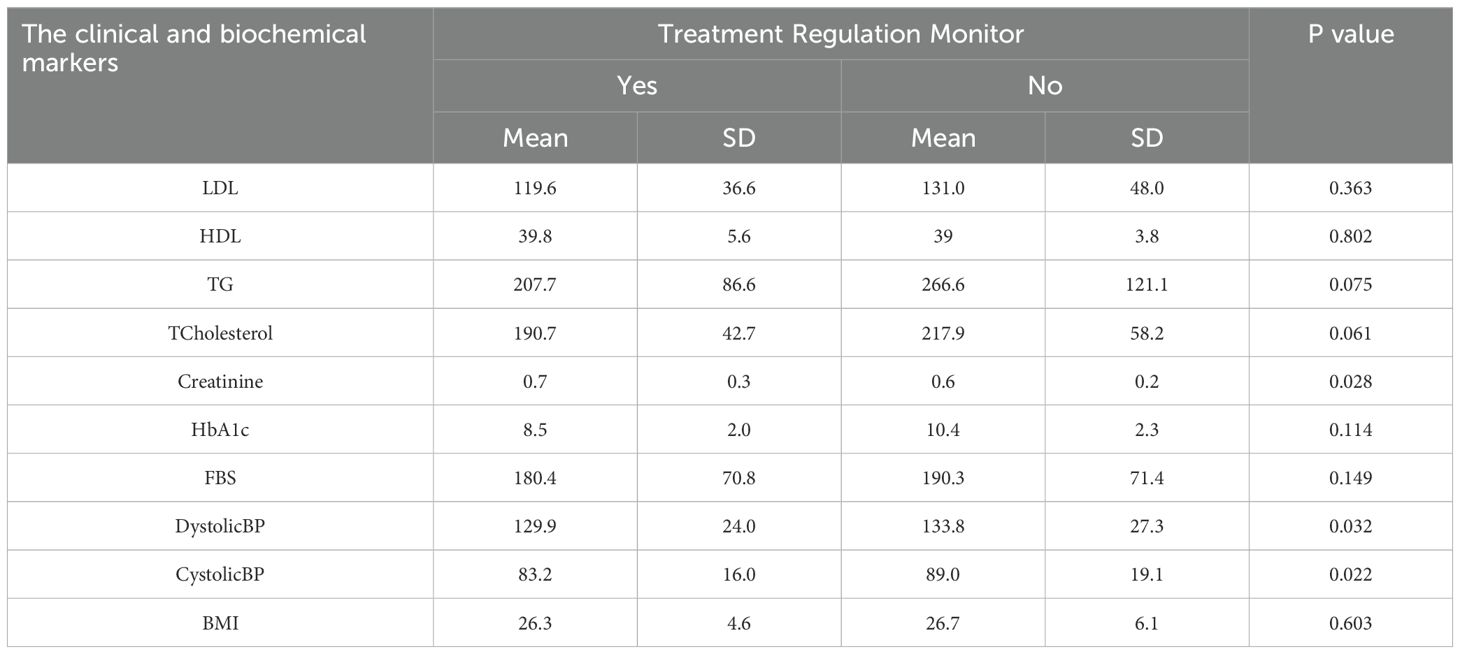
Table 7. Effect of treatment regulation on the clinical and biochemical blood level markers among the studied diabetic patients.
Table 8 presents lab monitoring results associated with lower triglyceride levels (220.9 vs. 293.5, p = 0.050) and HbA1c (9.2 vs. 10.4%, p = 0.002), indicating improved glycaemic control.
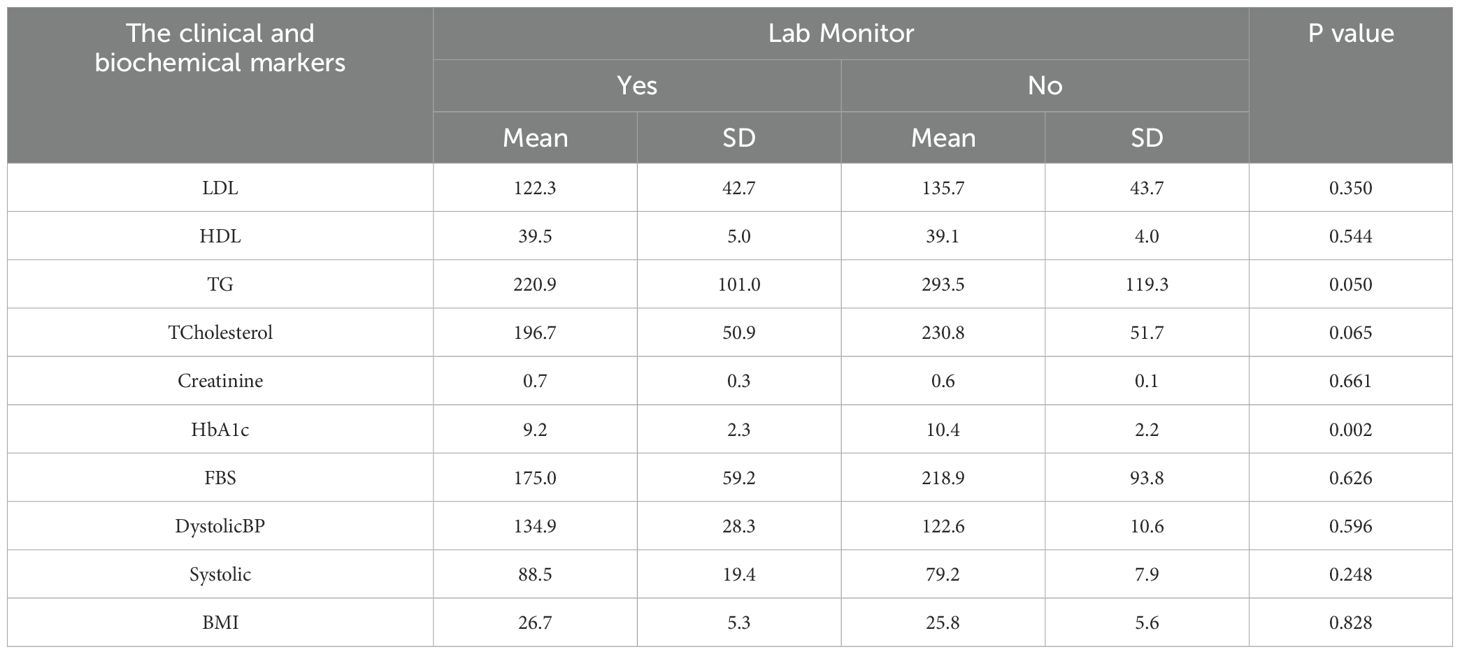
Table 8. Effect of lab monitor on the clinical and biochemical blood level markers among the studied diabetic patients.
Table 9 presents nutrition therapy. The intervention led to a significant reduction in triglycerides (164 vs. 250.4, p = 0.001), cholesterol levels (176.1 vs. 209.5, p = 0.023), and fasting blood sugar (121.1 vs. 196.0, p = <0.001).
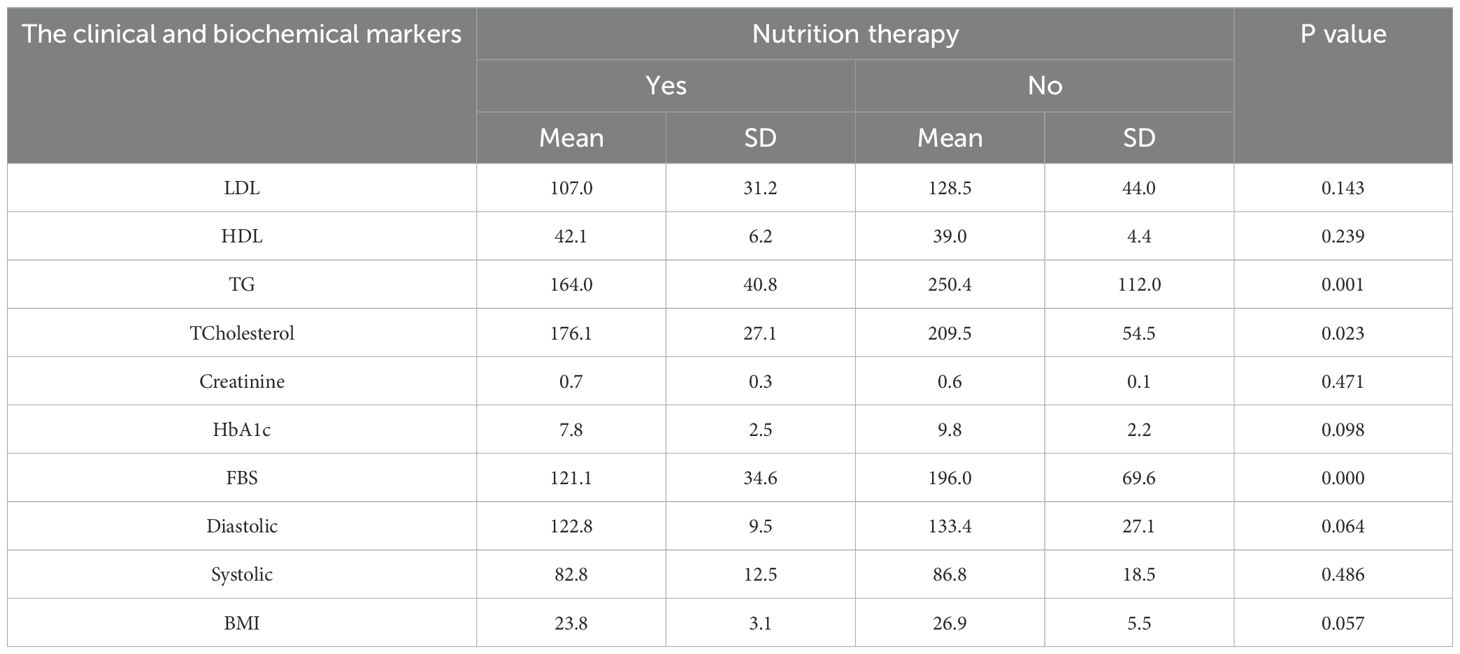
Table 9. Effect of nutrition therapy on the clinical and biochemical blood level markers among the studied diabetic patients. .
Table 10 indicates that educated patients exhibited a significantly lower BMI (25.1 vs. 28.7, p = 0.025) and generally superior biochemical profiles, although the majority of other differences did not reach statistical significance. This demonstrates the beneficial impact of health literacy on diabetes management.
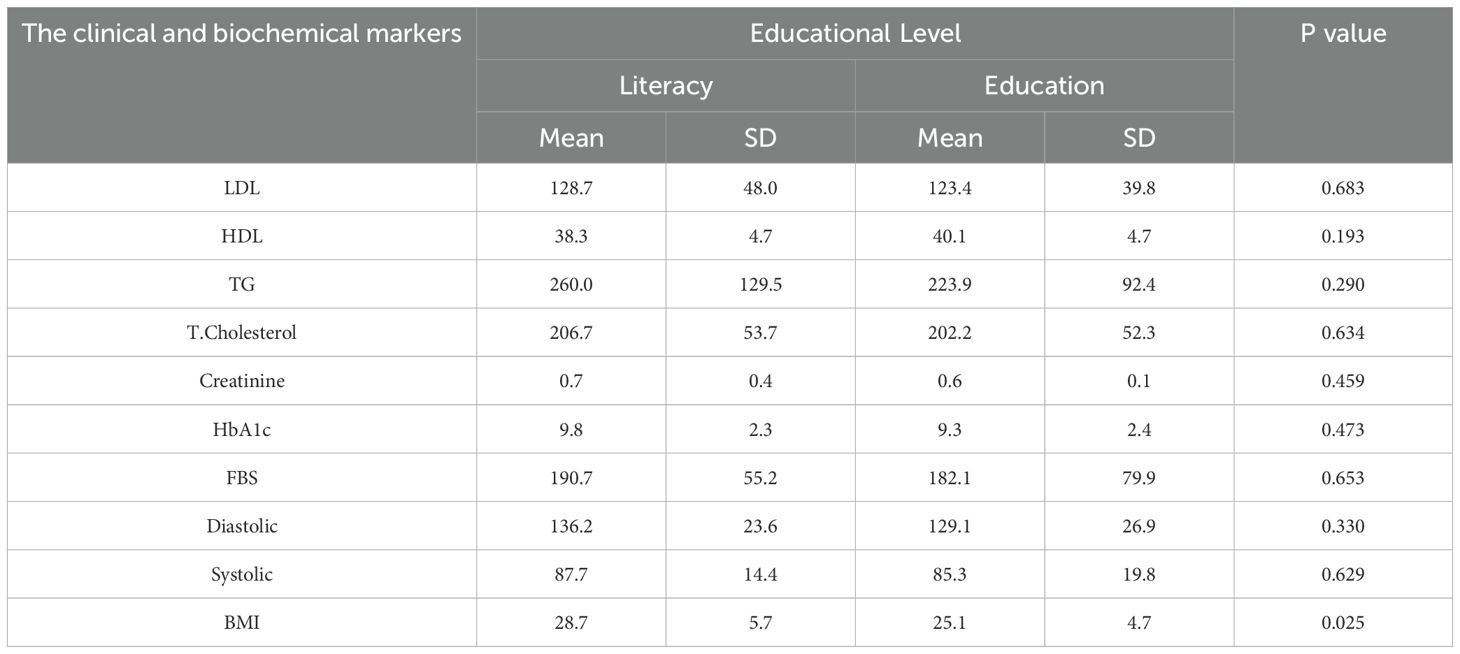
Table 10. The association between the clinical and biochemical blood level markers and educational level among the studied diabetic patients.
Table 11 indicates that females exhibited a higher BMI (28.0 vs. 25.1, p = 0.058) and elevated levels of most biomarkers, although these differences did not reach statistical significance. These trends may suggest distinct risk patterns or variations in care based on gender.
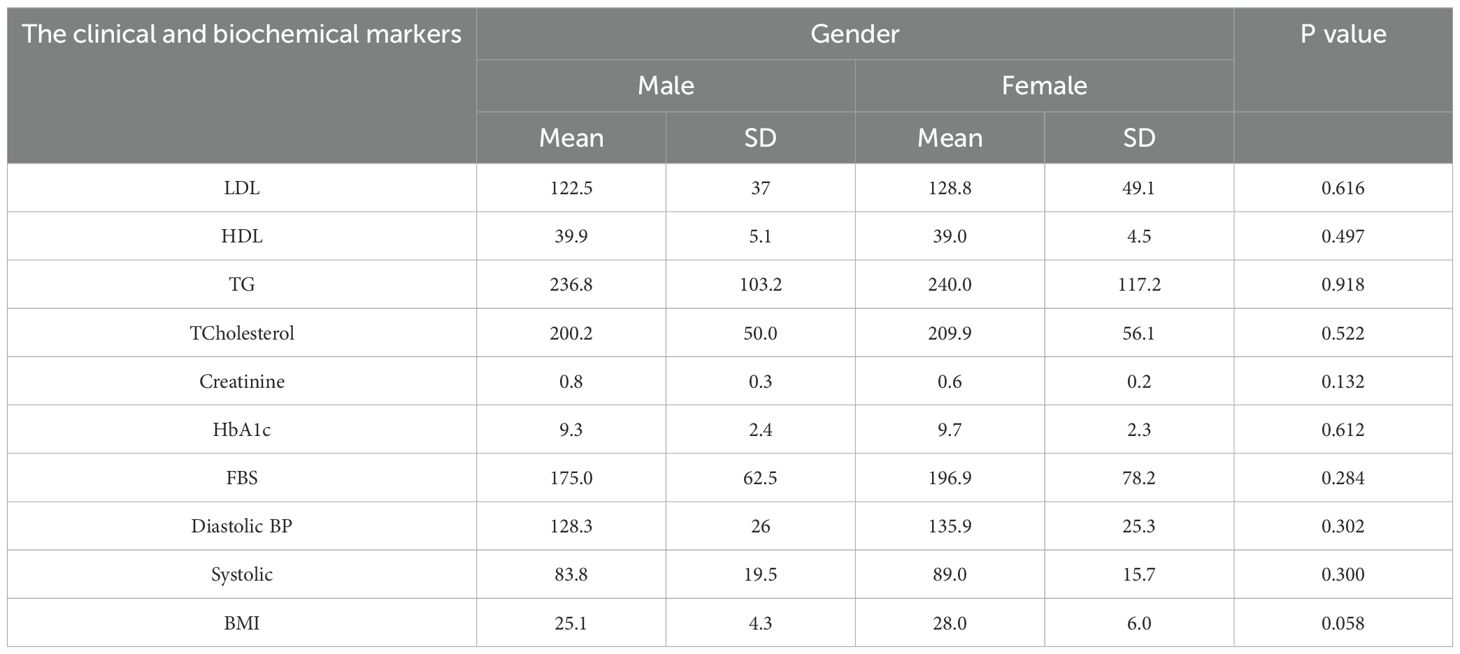
Table 11. The association between the clinical, biochemical blood level markers and the gender among the studied diabetic patients.
Table 12 showed that non-adherence to management methods (treatment, exercise, and diet) was related to a higher incidence of problems; however, this was not statistically significant. Exercise and nutrition had odds ratios of 1.333 and 1.207, respectively, indicating a potential risk of problems in the absence of these interventions.
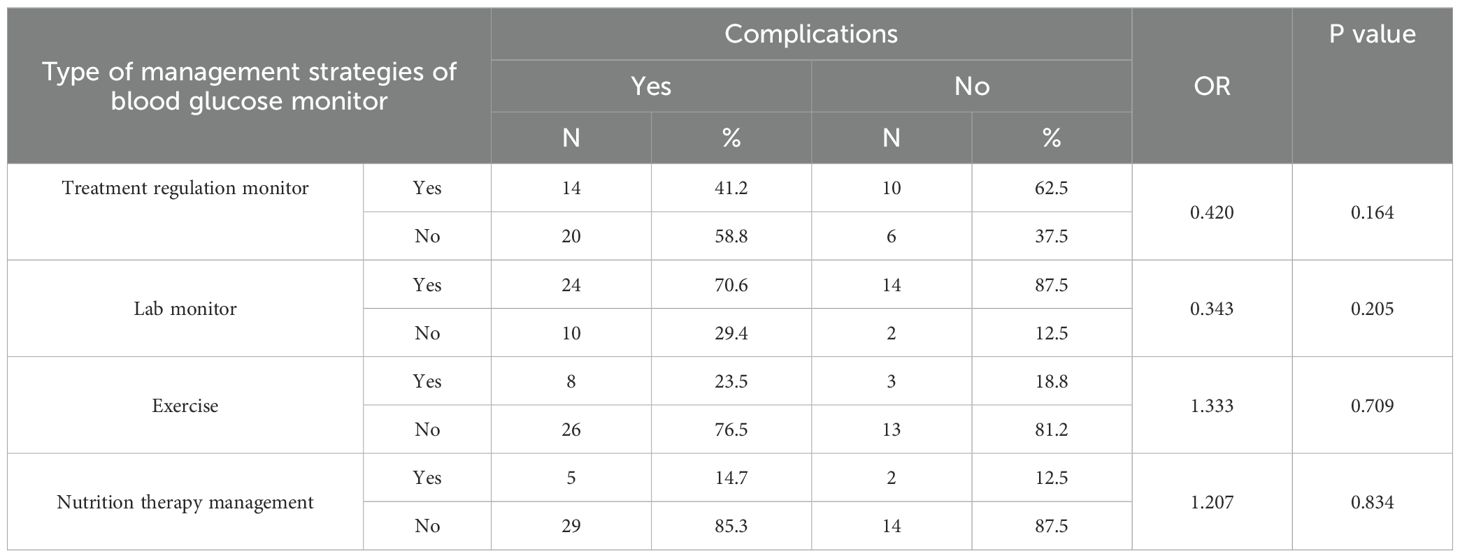
Table 12. The association between different type of management strategies of blood glucose level control and complications of DM among the studied diabetic patients.
Discussions
The investigation revealed that kidney disorders were the most common complication in individuals with diabetes, followed by eye disorders, nerve damage, foot gangrene, and heart-related conditions. This is consistent with the findings of Mazin Yousif Elhendi (18), who similarly identified these as prevalent complications among diabetic patients. Changes in metabolism and blood flow associated with diabetes lead to glomerular sclerosis and fibrosis, which exacerbate diabetic nephropathy.
The study indicated that non-treatment regulation (52%) and lack of nutritional therapy (86%) were more common than their respective alternatives. Laboratory monitoring was the predominant strategy, utilized by 76% of participants. These findings align with those of Ahmed Ismail Albarrak (19), who observed a low compliance rate with ADA standards of care at 36.3%. However, documentation of elements such as medical history, meal planning, and glucose monitoring occurred more frequently. Mazin Yousif Elhendi (18) reported comparable trends, indicating treatment regulation at 92.7%, laboratory monitoring at 74%, and dietary management at 26.8%.
Patients adhering to treatment regulations exhibited reduced levels of LDL, triglycerides (TG), total cholesterol, HbA1c, fasting blood sugar (FBS), and BMI, alongside significantly lower blood pressure. Interestingly, these patients showed elevated creatinine levels, possibly due to the administration of newer medications like GLP-1 receptor agonists, which enhance insulin secretion and reduce postprandial glucose fluctuations. These findings are supported by both Mazin Yousif Elhendi (18) and Diabetes UK (2010) (20), emphasizing the importance of effective therapy in mitigating diabetes-related complications.
Individuals adhering to a dietary regimen exhibited reduced levels of LDL, HbA1c, blood pressure, and BMI, along with significantly decreased TG, total cholesterol, and FBS. These results are consistent with recommendations from the American Diabetes Association (ADA) (21) which has highlighted the effectiveness of nutrition therapy in lowering blood glucose, lipid levels, body weight, and blood pressure. Additionally, Hawthorne (22) emphasized the role of dietary guidance in managing weight, hypertension, and glycaemic control among diabetic patients.
Patients who engaged in regular physical activity showed significantly decreased levels of LDL, BMI, TG, total cholesterol, creatinine, HbA1c, and FBS. These findings are in line with those of the DCCT Research Group (23) which stressed the importance of exercise in maintaining normoglycemia and preventing long-term diabetes complications.
Diabetic patients who received education exhibited reduced levels of LDL, TG, total cholesterol, creatinine, HbA1c, FBS, and blood pressure, along with significantly lower BMI. Diabetes self-management education (DSME) plays a critical role in preventing or delaying complications associated with diabetes. Studies by (24, 25) demonstrated that DSME improves glycaemic control. Further support comes from Marden (26) and Chaudhary (27), who emphasized the importance of literacy and education in enhancing outcomes and reducing complications.
Non-adherence to treatment, exercise, or nutrition therapy was associated with an increased prevalence of complications among patients. In contrast, individuals who underwent regular laboratory monitoring experienced a reduced incidence of complications. These results are supported by the American Diabetes Association (2002) (21), Diabetes UK (2010) (20), and the DCCT Research Group (1995) (23) all of whom emphasize the importance of strict metabolic control in preventing diabetes complications.
Study limitations
This study has several limitations. Firstly, the relatively small sample size of 50 diabetic patients limits the statistical power of the analysis and reduces the generalizability of the results to the wider diabetic population in Sana’a city and Yemen. Secondly, the recruitment was limited to hospitalized patients present during the researchers’ visits, which may introduce selection bias by overrepresenting patients with more severe disease or complications. This sampling method limits the applicability of findings to community-dwelling or outpatient diabetic populations, who may have different management experiences and outcomes. Additionally, the cross-sectional design provides only a snapshot of diabetes management and does not allow for assessment of causal relationships or changes over time. Self-reported data on treatment adherence, exercise, and nutrition may be subject to recall or social desirability bias, potentially affecting the accuracy of reported behaviors. Finally, some biochemical and clinical parameters were measured only once, which may not fully capture fluctuations in blood glucose control or other metabolic variables.
Our study suggests several recommendations to improve diabetes management in hospitals across Sana’a:
Enhance patient education, especially for those with low literacy levels, strengthen adherence support for treatment, nutrition, and exercise, increase regular laboratory monitoring, particularly for women, establish multidisciplinary care teams, expand outpatient and community-based follow-up, Improve healthcare resources and infrastructure. these measures could significantly improve patient outcomes and reduce the incidence of diabetes-related complications.
Conclusions
This study highlights that diabetes mellitus in Sana’a city predominantly affects middle-aged, married, and unemployed individuals with low educational levels. Non-insulin-dependent diabetes mellitus is the most common form, and renal complications are prevalent among patients. Laboratory monitoring is the most commonly employed management strategy, while adherence to treatment, exercise, and nutrition remains suboptimal, especially among females. Patients who adhered to treatment, nutritional guidance, and laboratory monitoring exhibited better biochemical profiles and reduced complication rates, underscoring the importance of comprehensive diabetes management. Education and gender differences influence disease control and outcomes, suggesting the need for targeted interventions.
Given the study’s limitations, including a small, hospital-based sample, further research with larger and more representative populations is necessary. Strengthening patient education, improving lifestyle adherence, and enhancing access to regular monitoring are critical steps to reduce the burden of diabetes complications in this population.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
This study approved by the Intuitional Review Board in the Ethics Committee of the Faculty of Medicine and Health Science, Sanaa University, Yemen (Research code: REC-72-2020). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
ASA-S: Data curation, Investigation, Resources, Validation, Writing – original draft, Writing – review & editing. MA: Writing – original draft. AA: Writing – original draft, Methodology. YA-W: Writing – review & editing, Validation, Supervision. ZAT: Writing – review & editing, Methodology, Formal analysis.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
Our gratitude goes out to every one of the study participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Al-Shami AS, Jha DK, Babukutty BE, Haque M, and Khadka J. Evaluation of protective effect of aegle marmelos fruits extracts against streptozotocin-induced type 1 diabetes mellitus in rat’s model. Asian J Pharm Clin Res. (2022) 15:1–6. doi: 10.22159/ajpcr.2022.v15i12.45840
3. American Diabetes Association. 2. Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes—2024. Diabetes Care. (2024) 47:S20–38.
5. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes. Lancet. (1998) 352:837–53. doi: 10.1016/S0140-6736(98)07019-6
6. Diabetes Control and Complications Trial (DCCT) Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. (1993) 329:977–86. doi: 10.1056/NEJM199309303291401
7. DCCT Research Group. The relationship of glycemic exposure (HbA1c) to the risk of development and progression of retinopathy in the Diabetes Control and Complications Trial. Diabetes. (1995) 44:968–83. doi: 10.2337/diab.44.8.968
8. Gallichan M. Self-monitoring of blood glucose: has the emperor got clothes? Pract Diabetes Int. (1997) 14:49–52.
9. American Diabetes Association. 6. Glycemic targets: standards of medical care in diabetes—2024. Diabetes Care. (2024) 47:S98–110.
10. American Diabetes Association. 15. Diabetes care in older adults: standards of medical care in diabetes—2024. Diabetes Care. (2024) 47:S234–42.
11. Joslin Diabetes Center. Clinical Guidelines for Insulin Use in Diabetes. Boston, MA: Joslin Diabetes Center (2022).
12. Moghissi ES, Korytkowski MT, DiNardo M, Einhorn D, Hellman R, Hirsch IB, et al. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Diabetes Care. (2009) 32:1119–31. doi: 10.2337/dc09-9029
13. American Association of Clinical Endocrinology (AACE). AACE clinical practice guidelines for developing a diabetes mellitus comprehensive care plan – 2023 update. Endocr Pract. (2023) 29:157–81.
14. Van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med. (2001) 345:1359–67. doi: 10.1056/NEJMoa011300
15. American Diabetes Association. 5. Facilitating behavior change and well-being to improve health outcomes: standards of medical care in diabetes—2024. Diabetes Care. (2024) 47:S76–85.
16. World Health Organization. Prevention and Control of Noncommunicable Diseases: Guidelines for Primary Health Care in Low-Resource Settings. Geneva: WHO Press (2012).
17. World Health Organization. Package of Essential Noncommunicable (PEN) Disease Interventions for Primary Health Care in Low-Resource Settings. Geneva: WHO Press (2020).
18. Elhendi MY. Complications and management of diabetes mellitus in diabetic patients attending the Military Hospital, Sudan. Sudan J Med Sci. (2014) 9:15–22.
19. Albarrak AI, Mohammed R, Al Elq A, AlQahtani S, Balaha M, and Al Shahrani A. Assessment of physician’s adherence to the American Diabetes Association guidelines at a tertiary care hospital in Riyadh. Saudi J Health Sci. (2012) 1:60–5.
20. Diabetes UK. Evidence-based nutrition guidelines for the prevention and management of diabetes. London: Diabetes UK (2010).
21. American Diabetes Association. Standards of medical care in diabetes—2002. Diabetes Care. (2002) 25:S33–49.
22. Hawthorne K, Robles Y, Cannings-John R, and Edwards AGK. Culturally appropriate health education for type 2 diabetes mellitus in ethnic minority groups. Cochrane Database Syst Rev. (2008) 3:CD006424.
23. The Diabetes Control and Complications Trial Research Group. The effect of intensive diabetes treatment on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. (1993) 329:977–86. doi: 10.1056/NEJM199309303291401
24. Deakin T, McShane CE, Cade JE, and Williams RD. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev. (2005) 2:CD003417.
25. Norris SL, Lau J, Smith SJ, Schmid CH, and Engelgau MM. Self-management education for adults with type 2 diabetes: A meta-analysis of the effect on glycemic control. Diabetes Care. (2002) 25:1159–71. doi: 10.2337/diacare.25.7.1159
26. Marden S, Thomas PW, Sheppard ZA, Knott J, Lueddeke J, and Kerr D. Poor numeracy skills are associated with glycaemic control in type 1 diabetes. Diabetes Med. (2012) 29:662–9. doi: 10.1111/j.1464-5491.2011.03466.x
Keywords: diabetes mellitus, blood glucose control, management strategies, laboratory monitoring, Yemenis patients, blood bio-markers
Citation: Salman Al-Shami A, Alzumor M, Aladhal A, Al-Worafi Y and Thawaba ZA (2025) “Assessment of diabetes management strategies for blood glucose control in Sana’a City General Hospitals”. Front. Endocrinol. 16:1587901. doi: 10.3389/fendo.2025.1587901
Received: 05 March 2025; Accepted: 30 June 2025;
Published: 17 July 2025.
Edited by:
Yun Shen, Pennington Biomedical Research Center, United StatesReviewed by:
Pranay Punj Pankaj, Nagaland University, IndiaPriscilla Oluwadamilare, Obafemi Awolowo University Teaching Hospitals Complex, Nigeria
Copyright © 2025 Salman Al-Shami, Alzumor, Aladhal, Al-Worafi and Thawaba. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ali Salman Al-Shami, YWxzaGFtaWFsaTUxM0BnbWFpbC5jb20=
 Ali Salman Al-Shami
Ali Salman Al-Shami Mokhtar Alzumor3
Mokhtar Alzumor3