- 1Korean Medicine (KM) Science Research Division, Korea Institute of Oriental Medicine, Daejeon, Republic of Korea
- 2Department of Diagnostics, College of Korean Medicine, Wonkwang University, Iksan, Republic of Korea
- 3College of Korean Medicine, Dongguk University, Goyang, Republic of Korea
- 4Kyunghee Dabok Korean Medicine Clinic, Seoul, Republic of Korea
- 5Department of Korean Medicine Rehabilitation, College of Korean Medicine, Semyung University, Jecheon, Republic of Korea
The delayed union of fractures poses considerable challenges in orthopedic treatment, affecting patients’ quality of life and healthcare outcomes. Although various treatment options are available, their efficacy may be limited in patients with prolonged delayed union. This study investigated the therapeutic potential of Jeopgol-tang (JGT), a traditional herbal decoction, for treating cases of delayed union persisting for more than 5 months. Three patients with different fracture sites (pubic ramus, multiple metatarsals, and femoral neck) who exhibited insufficient healing after conventional treatment were administered JGT (100 mL per pack, twice daily) for 2–6 months depending on individual healing progress and fracture complexity. Radiological assessments demonstrated progressive improvement in all cases. Notably, one patient avoided reoperation after exhibiting initial signs of bone healing within 1 month of treatment, whereas all patients achieved complete union and reported improved mobility and reduced pain. These findings suggest that JGT could be an effective complementary treatment option for delayed union, particularly in cases in which conventional treatments have yielded limited success. Nevertheless, larger prospective clinical trials and mechanistic studies are required to validate these results and to explore the therapeutic mechanisms of JGT.
1 Introduction
Bone-fracture healing is a complex biological process involving a series of coordinated molecular and cellular events (1). Although a direct healing pattern can occur when the fracture is reduced and remains nearly completely stable, most cases follow an indirect healing pattern consisting of both endochondral and intramembranous bone healing. This process typically progresses through four distinct phases that include inflammation (hematoma formation), granulation tissue formation, bony callus formation, and bone remodeling (2–4).
When this intricate healing process is disrupted by inadequate immobilization, compromised blood supply, infection, or nutritional deficiency, delayed union or nonunion may occur (4). Delayed union, typically diagnosed when a fracture exhibits no radiological signs of healing between 3- and 6- months post-injury, occurs in 10–15% of surgically managed fracture cases and poses considerable challenges for both patients and healthcare providers (5). Current treatment approaches, including surgical intervention, biophysical stimulation, and local biological enhancement, often result in limited efficacy and may be associated with complications (6–8).
Herbal medicines have been used for fracture healing and treatment of symptoms related to fractures across East Asia for thousands of years (9). Large population cohort studies have revealed a significant association between the use of herbal medicine and a reduced risk of osteoporotic fractures as well as a lower risk of overall mortality, readmission, and reoperation (10, 11). Recent studies have elucidated the mechanisms underlying the effectiveness of these traditional approaches. Herbal medicines can enhance bone formation through multiple mechanisms (12) and pathways, including regulation of osteogenic differentiation (13), modulation of inflammatory responses (14), and promotion of angiogenesis (15, 16).
Jeopgol-tang (JGT), a traditional herbal decoction used for fracture treatment, prepared through non-pressure hot water extraction of various herbs including Angelicae Gigantis Radix, Cnidii Rhizoma, and Achyranthis Radix. This herbal formula has exhibited promising results in the context of bone healing and regeneration. In Sprague–Dawley rats, JGT administration resulted in significantly enhanced callus growth within 2 weeks and increased callus length after 4 weeks compared to that of controls (17). Additionally, safety assessments confirmed that JGT does not induce acute toxicity or adverse effects (18). High-performance liquid chromatography identified nodakenin, ferulic acid, and dipsanoside A as the major compounds in JGT (18). Clinical studies have demonstrated that JGT improves bone density (19) and is effective for delayed union as early as 3 months after the fracture (20).
The present study aimed to investigate the therapeutic potential of JGT in treating cases of delayed union that persisted for more than 5 months. Herein, we present three cases in which conventional treatments failed to achieve adequate healing, focusing on the clinical outcomes and radiological evidence of bone regeneration following JGT administration.
2 Case presentation
2.1 Case 1
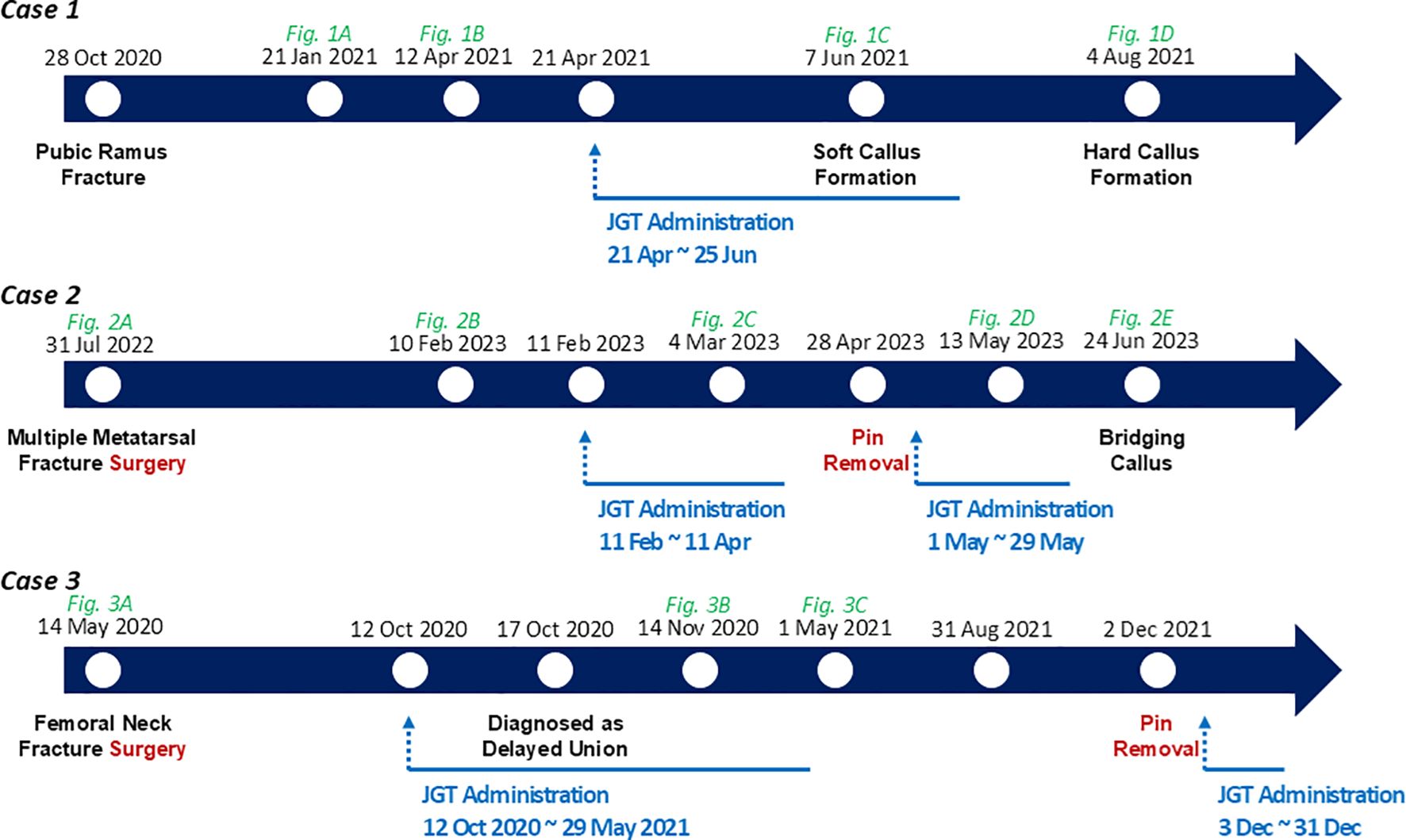
A 65-year-old man was diagnosed with a pubic ramus fracture based on radiographic images after a traffic accident on October 28, 2020. The patient experienced no underlying medical conditions. Owing to the mild displacement of the fracture, conservative treatment was performed at the initial hospital, including hospitalization for three weeks with acupuncture, herbal medicine for blood stasis, anti-inflammatory analgesics, and use of an abdominal binder across the waist and pelvis for stability support. However, callus formation was not complete until 6 months after the fracture. Accordingly, the patient visited our Korean Medicine clinic on April 21, 2021, and underwent JGT treatment for 2 months. On May 21, 2021, the patient received an injection of teriparatide (Forsteo) administered 11 times over 5 months to increase bone density. Radiography revealed callus growth, blurred fracture lines, and clear evidence of continuous callus formation (Figure 1). The improvement in fracture healing was more apparent after JGT treatment (Figures 1C, D) compared with the pretreatment state (Figure 1B). In November 2021, the patient was determined to have achieved complete recovery.
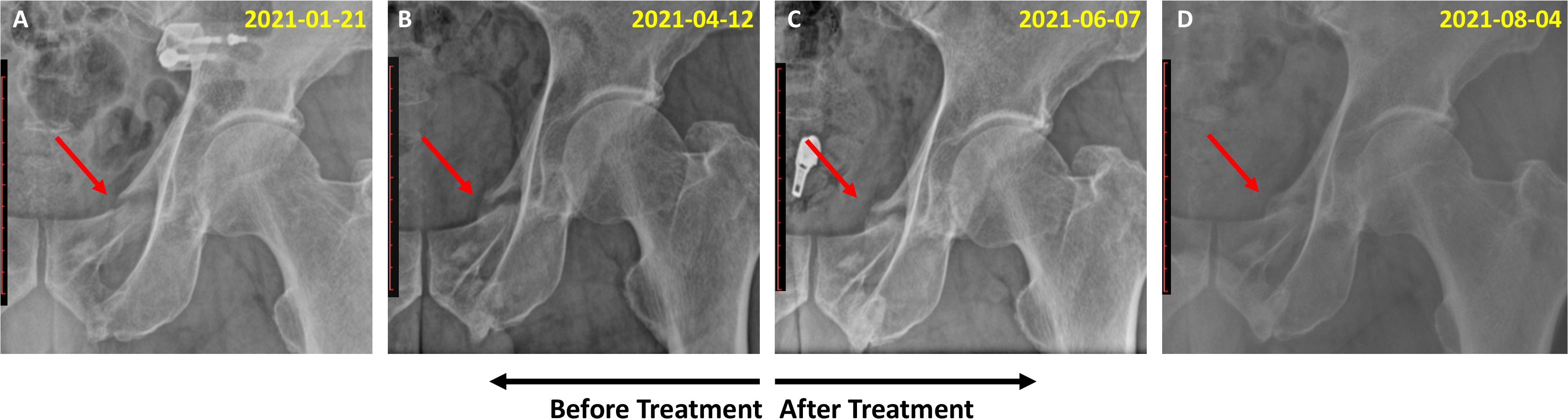
Figure 1. Radiographic images of the pelvis of Case 1, a 65-year-old man with a pubic ramus fracture. (A) Fracture condition of the pubic ramus at 3 months after the traffic accident (January 21, 2021); (B) Callus formation status 6 months after the fracture (April 12, 2021); (C) Soft callus formation 2 months after JGT administration (June 7, 2021); (D) Hard callus formation (August 4, 2021).
2.2 Case 2
On July 30, 2022, a 30-year-old woman was diagnosed with fractures of the left second, third, and fourth metatarsals based on radiographic findings after falling while climbing (Figure 2A). The patient underwent internal fixation surgery the next day, was prescribed conventional medications, and used crutches for four months. However, callus formation was not identified until 6 months after surgery. Owing to incomplete bone union, the patient visited our clinic on February 11, 2023, and began JGT treatment. The patient underwent pin removal surgery on April 28, 2023, as the fracture had united, and underwent JGT for an additional 4 weeks from May 1, 2023. Before starting the herbal treatment, callus formation was insufficient (Figure 2B). Three months after JGT administration, radiographic imaging demonstrated evidence of union, characterized by bridging callus density similar to that of the bony cortex and a blurred fracture line (Figure 2E).
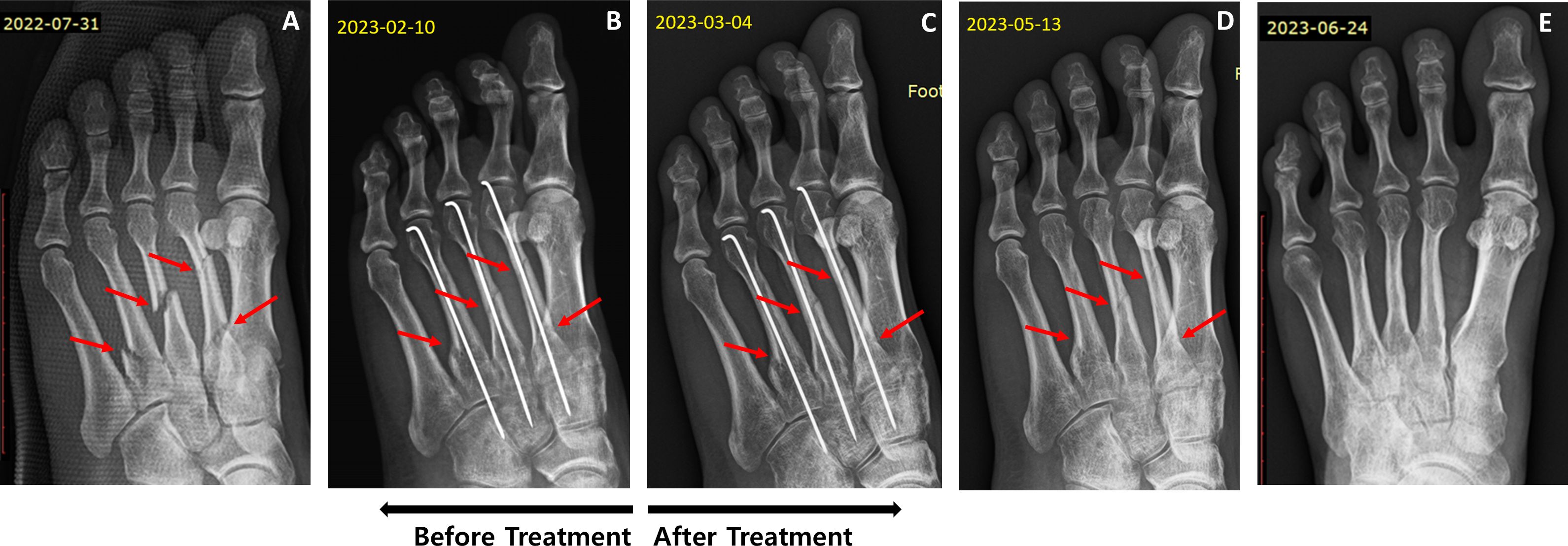
Figure 2. Radiographic images of the left foot of Case 2, a 30-year-old woman with multiple metatarsal fractures in the left foot. (A) Fracture condition before surgery (July 31, 2022); (B) Fracture status 6 months after surgery (February 10, 2023); (C) Fracture condition 1 month after JGT administration (March 4, 2023); (D) Fracture condition 3 months after JGT administration (May 13, 2023); (E) Bridging callus density similar to the bony cortex (June 24, 2023).
2.3 Case 3
In May 2020, a 58-year-old woman was diagnosed with a fracture of the right femoral neck based on radiographic and computed tomography (CT) findings (Figure 3A). The fracture occurred when the patient fell while walking downstairs. The patient underwent internal fixation surgery in May 2020, and crutches were used daily. She also received osteoporosis injections and anti-inflammatory analgesics for 5 months. However, the attending physician diagnosed delayed union, as no callus formation or fracture improvement was observed on radiographic or CT images. The patient visited our clinic on October 12, 2020, for herbal medicine treatment to avoid reoperation and decided to wait another month before reconsidering surgery. On November 14, 2020, after 1 month of JGT administration, CT imaging indicated signs of improvement (Figure 3B), and she continued without reoperation. The patient was able to walk without crutches 4 months after the JGT treatment. On May 1, 2021, seven months after JGT administration, CT imaging revealed substantial fracture healing characterized by bridging callus formation across the fracture gap and restoration of cortical continuity (Figure 3C). She underwent pin removal surgery on December 2, 2021. The timelines for the three cases are presented in Figure 4.
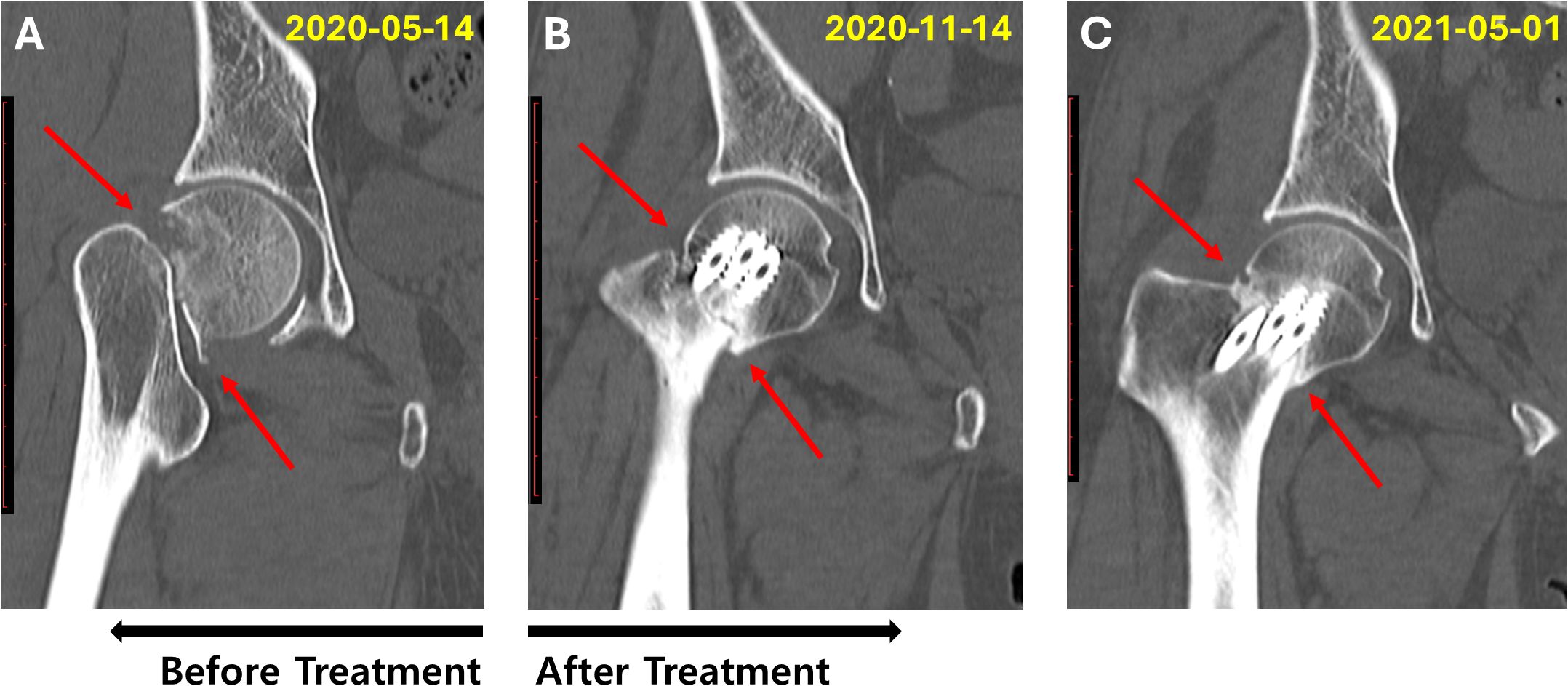
Figure 3. Computed tomography images of the right hip joint of Case 3, a 58-year-old woman with a femoral neck fracture. (A) Frontal planes of the right hip joint, showing the fractured femoral neck immediately after the accident and before surgery (May 14, 2020); (B) Frontal planes of the right hip joint 6 months after the fracture and 1 month after the diagnosis of delayed union (1-month follow-up after JGT administration) (November 14, 2020); (C) Frontal planes showing distinct changes in the right hip joint, demonstrating femoral neck fracture healing (May 1, 2021).
2.4 Diagnostic assessment
The outcome of the fracture healing progression was assessed by a radiologist based on anteroposterior and lateral radiographs or CT images. No specific diagnostic challenges were observed.
2.5 Therapeutic intervention
All patients were administered two packs of the JGT decoction (100 mL per pack) daily. Supplementary Table 1 presents the herbal composition of the JGT prescribed to each patient. In Case 2, Zingiberis Rhizoma and Zizyphi Fructus were added to aid digestion and address cold extremities. In Case 3, the dosage of Citri Unshius Pericarpium was increased from 8 to 16 g in Period 2 due to the patient’s complaints of difficulty sleeping. The same herbal prescription was maintained on December 14, 2020, owing to the improvement in sleep after increasing Citri Unshius Pericarpium. For depression (Case 3), Perillae Folium and Coptidis Rhizoma were included in Period 3. After pin removal (Case 3), herbal medicine was prescribed during Period 4 to address the deficiency. The patient maintained consistent adherence to the prescribed treatment, took JGT as directed, and attended all scheduled follow-up visits for continued prescription. None of the three patients experienced adverse events while taking herbal medicine. No other treatments such as physical therapy, acupuncture, or dietary strategies were provided during the JGT treatment at the clinic.
2.6 Patient perspectives
Case 1: “After I started taking JGT, I felt that the reduction of pain was happening faster. Also, I felt more comfortable walking.”
Case 2: “I did not feel uncomfortable when I started taking JGT. A revision operation was considered because callus formation was not detected six months after surgery. Fortunately, fracture union and pin removal were possible after JGT.”
Case 3: “There was no improvement or callus formation at the fracture site during internal fixation until 5 months after surgery. After 4 weeks of JGT treatment, minimal bone union was observed. I felt that my pain had reduced and walking had improved. Complete fracture healing was achieved without reoperation, and internal fixation was removed.”
3 Discussion
Fracture healing is a challenging and crucial process for both patients and clinicians (4). Fracture nonunion or delayed union directly affects the patients’ quality of life and their physical and mental health (8). As delayed union leads to a higher probability of nonunion, early and aggressive treatment is essential. This case report demonstrates the clinical effectiveness of JGT, a traditional herbal formulation, for treating delayed union lasting more than 5 months.
Experimental studies have been conducted on JGT extract, which consists of eight herbs at specific dosages, to evaluate its efficacy and safety (17, 18). Nodakenin, a marker compound of JGT, promotes osteoblast differentiation through activation of the PI3K/Akt/mTOR signaling pathway while simultaneously inhibiting osteoclastogenesis via suppression of c-Src/TRAF6/NF-κB pathways, demonstrating dual mechanisms crucial for bone remodeling and repair (21). Additionally, nodakenin has been demonstrated to exert anti-osteoporotic effects through comprehensive modulation of the gut-bone axis, including restoration of the Firmicutes/Bacteroidetes ratio, enhancement of beneficial bacterial strains such as Muribaculaceae and Allobaculum, promotion of calcitriol production and subsequent VDR activation, and improvement of intestinal barrier integrity through upregulation of tight junction proteins Occludin and ZO-1 while reducing pro-inflammatory cytokines IL-1β and TNF-α (22).
Ferulic acid, one of the major compounds in JGT, has been demonstrated to enhance vascular endothelial function by increasing nitric oxide bioavailability and promoting angiogenesis through the upregulation of vascular endothelial growth factor, platelet-derived growth factor, and hypoxia-inducible factor-1α expression (23). These vascular effects may contribute to bone healing by improving the blood supply and creating a favorable microenvironment for bone regeneration, particularly in cases of delayed union, where compromised vascularity often impedes the healing process. Furthermore, during fracture healing, key signaling molecules including TGF-β, IL-1, IL-6, TNF-α, and VEGF are released to orchestrate bone repair and vascular proliferation (4). Given that ferulic acid demonstrates pharmacological effects including TGF-β/Smad pathway modulation, regulation of inflammatory cytokines through NF-κB and p38 MAPK pathways, and enhancement of angiogenic factors (23), it may potentially influence bone union processes by optimizing the molecular environment beyond its direct vascular effects.
Thus, JGT may serve as an alternative treatment option for patients who are unsuitable for surgical intervention. In Case 1, a patient with a pubic ramus fracture, for whom the surgical approach was challenging, exhibited soft callus formation and eventually achieved complete union with JGT treatment. Furthermore, in Case 3, where reoperation was considered because of the lack of bone healing despite conventional treatments, including analgesics and osteoporosis injections, signs of fracture recovery were observed after 1 month of JGT administration, allowing the patient to avoid additional surgery. All patients reported high satisfaction with the treatment outcomes, as complete bone union was achieved after JGT treatment in cases where delayed union persisted for > 5 months. These findings suggest that JGT administration after acute fracture management may accelerate healing.
This study had several limitations. First, the results of these three cases cannot be generalized to a broader population. Large-scale prospective observational and comparative studies with comprehensive safety assessment protocols are needed to confirm the effectiveness and safety profile of JGT in treating delayed union. While our cases showed no adverse events and previous studies demonstrated no acute toxicity (18), long-term safety data, potential herb-drug interactions, and dose-dependent effects require systematic evaluation in larger populations. Second, some herbs were added to the basic JGT prescription based on each patient’s condition. This reflects the real-world clinical practice in South Korea, where most herbal medicines prescribed by Korean Medicine doctors are customized individually (24). Future studies should focus on identifying the optimal timing and duration of JGT administration as well as investigating potential synergistic effects when combined with conventional treatments. Further research is required to elucidate the mechanisms of action of JGT, particularly regarding its key bioactive compounds.
The present study provides clinical and scientific evidence for the effectiveness of JGT in fracture healing. These findings suggest that JGT could be a valuable complementary addition to the current treatment options for delayed union, particularly as an adjunctive therapy in cases where conventional treatments alone have been insufficient or when surgical intervention is not feasible.
4 Conclusion
This case report indicates the effectiveness of JGT for delayed union persisting for more than five months. The therapeutic effects of JGT, supported by radiological evidence and patient-reported outcomes, may be attributed to its bioactive compounds that promote bone regeneration through multiple mechanisms, including enhanced vascular function and osteoblast differentiation. These findings suggest that JGT could be considered as a complementary treatment option for delayed union, particularly when conventional treatments have yielded limited success. However, larger clinical studies are warranted to validate these results.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was approved by the Institutional Review Board of Semyung University (IRB No. SMU-2024-12-012-01). The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individuals for the publication of any potentially identifiable images or data included in this article.
Author contributions
EC: Formal analysis, Methodology, Visualization, Writing – original draft. SL: Formal analysis, Methodology, Visualization, Writing – original draft. YC: Conceptualization, Data curation, Writing – review & editing. CY: Funding acquisition, Project administration, Writing – review & editing. HW: Formal analysis, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by the Korea Institute of Oriental Medicine (grant no. KSN2122211).
Acknowledgments
The authors appreciate the consent of patients for this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2025.1595784/full#supplementary-material
References
1. Gómez-Barrena E, Rosset P, Lozano D, Stanovici J, Ermthaller C, and Gerbhard F. Bone fracture healing: Cell therapy in delayed unions and nonunions. Bone. (2015) 70:93–101. doi: 10.1016/j.bone.2014.07.033
2. Marsell R and Einhorn TA. The biology of fracture healing. Injury. (2011) 42:551–5. doi: 10.1016/j.injury.2011.03.031
3. Panteli M, Pountos I, Jones E, and Giannoudis PV. Biological and molecular profile of fracture non-union tissue: Current insights. J Cell Mol Med. (2015) 19:685–713. doi: 10.1111/jcmm.12532
4. Hak DJ, Fitzpatrick D, Bishop JA, Marsh JL, Tilp S, Schnettler R, et al. Delayed union and nonunions: Epidemiology, clinical issues, and financial aspects. Injury. (2014) 45:S3–7. doi: 10.1016/j.injury.2014.04.002
5. Bowers KM and Anderson DE. Delayed union and nonunion: current concepts, prevention, and correction: A review. Bioengineering. (2024) 11:525. doi: 10.3390/bioengineering11060525
6. Einhorn TA and Gerstenfeld LC. Fracture healing: Mechanisms and interventions. Nat Rev Rheumatol. (2015) 11:45–54. doi: 10.1038/nrrheum.2014.164
7. Flierl MA, Smith WR, Mauffrey C, Irgit K, Williams AE, Ross E, et al. Outcomes and complication rates of different bone grafting modalities in long bone fracture nonunions: a retrospective cohort study in 182 patients. J Orthop Surg Res. (2013) 8:33. doi: 10.1186/1749-799X-8-33
8. Yang J, Zhang X, Liang W, Chen G, Ma Y, Zhou Y, et al. Efficacy of adjuvant treatment for fracture nonunion/delayed union: a network meta-analysis of randomized controlled trials. BMC Musculoskelet Disord. (2022) 23:481. doi: 10.1186/s12891-022-05407-5
9. Liao H-H, Yeh C-C, Lin C-C, Chen B-C, Yeh M-H, Chang K-M, et al. Prescription patterns of Chinese herbal products for patients with fractures in Taiwan: A nationwide population-based study. J Ethnopharmacol. (2015) 173:11–9. doi: 10.1016/j.jep.2015.07.014
10. Chen W-J, Livneh H, Hsieh M-H, Yeh C-C, Yeh M-H, Lu M-C, et al. Association of use of Chinese herbal medicines and the risk of fracture in patients with osteoporosis: A population-based cohort study. Osteoporos Int. (2019) 30:807–15. doi: 10.1007/s00198-018-4789-x
11. Cheng C-F, Lin Y-J, Tsai F-J, Li T-M, Lin T-H, Liao C-C, et al. Effects of Chinese herbal medicines on the risk of overall mortality, readmission, and reoperation in hip fracture patients. Front Pharmacol. (2019) 10:629. doi: 10.3389/fphar.2019.00629
12. Tian Z, Hao Y, Wang M, Li Y, Cui K, Hou P, et al. Understanding the mechanism of twenty-five ingredient decoction for setting a fracture in the treatment of fractures based on network pharmacology. Medicine. (2023) 102:e32864. doi: 10.1097/MD.0000000000032864
13. Qian D, Zhang Q, He C-X, Guo J, Huang X-T, Zhao J, et al. Hai-Honghua medicinal liquor is a reliable remedy for fracture by promotion of osteogenic differentiation via activation of PI3K/Akt pathway. J Ethnopharmacol. (2024) 330:118234. doi: 10.1016/j.jep.2024.118234
14. Siu W-S, Ko C-H, Lam K-W, Wat E, Shum W-T, Lau CB-S, et al. Evaluation of a topical herbal agent for the promotion of bone healing. Evid- Based Complement Alternat Med. (2015) 2015:905270. doi: 10.1155/2015/905270
15. Shen J, Li Y-Z, Yao S, Zhu Z-W, Wang X, Sun H-H, et al. Hu’po Anshen Decoction accelerated fracture-healing in a rat model of traumatic brain injury through activation of PI3K/AKT pathway. Front Pharmacol. (2022) 13:952696. doi: 10.3389/fphar.2022.952696
16. Yang Y, Chin A, Zhang L, Lu J, and Wong RWK. The role of traditional Chinese medicines in osteogenesis and angiogenesis. Phytother Res. (2014) 28:1–8. doi: 10.1002/ptr.4959
17. Choi Y, Shim HS, Kim DH, and Park HJ. The effect of Jeopgol-tang 2.0 on recovery of bone fracture in Sprague-Dawley rats. J Physiol Pathol Korean Med. (2024) 38:101–6. doi: 10.15188/kjopp.2024.08.38.4.101
18. Choi Y, Kim H, Kim S-J, Kim J, Jeong J, Leem H, et al. Single oral dose toxicity test of Jeopgoltang extracts in Sprague-Dawley rat. Kor J Herbol. (2024) 39:19–25. doi: 10.6116/kjh.2024.39.2.19
19. Won J, Choi Y, Lee B-C, and Lee H. Improvement of low bone mineral density treated with Jeopgol-tang in a middle-aged man: A case report. J Korean Med. (2021) 42:90–7. doi: 10.13048/jkm.21018
20. Won J, Choi Y, Yoon LS, Lee J-H, Choi K, and Lee H. Individualized herbal prescriptions for delayed union: A case series. Explore (NY). (2023) 19:260–6. doi: 10.1016/j.explore.2022.03.001
21. Liu C, Zhao M, Chen J, Xu L, Wang K, and Li G. Nodakenin alleviates ovariectomy-induced osteoporosis by modulating osteoblastogenesis and osteoclastogenesis. Eur J Pharmacol. (2023) 960:176121. doi: 10.1016/j.ejphar.2023.176121
22. Liu C, Chen J, Wang Z, Li Y, Zhang Y, and Li G. Nodakenin ameliorates ovariectomy-induced bone loss by regulating gut microbiota. Molecules. (2024) 29:1240. doi: 10.3390/molecules29061240
23. Li D, Rui Y, Guo S, Luan F, Liu R, and Zeng N. Ferulic acid: A review of its pharmacology, pharmacokinetics and derivatives. Life Sci. (2021) 284:119921. doi: 10.1016/j.lfs.2021.119921
24. National Institute for Korean Medicine Development. 2023 Herbal Medicine Consumption Survey. Republic of Korea, Seoul: Ministry of Health and Welfare (2024). Available online at: https://nikom.or.kr/koms/board/view.do?menu_idx=19&manage_idx=142&board_idx=564745&group_depth=0&parent_idx=0&group_idx=0&rowCount=10&search_type=title%2Bcontent&search_text=&viewPage=1.
Keywords: fracture, delayed union, herbal medicine, Jeopgol-tang, case report
Citation: Cho E, Lee S, Choi Y, Yang C and Woo H (2025) Case Report: Therapeutic potential of traditional Korean herbal medicine Jeopgol-tang in bone regeneration: a case series of delayed union over 5 months. Front. Endocrinol. 16:1595784. doi: 10.3389/fendo.2025.1595784
Received: 18 March 2025; Accepted: 06 June 2025;
Published: 30 June 2025.
Edited by:
Aixi Yu, Wuhan University, ChinaReviewed by:
Gang Wang, Chinese Academy of Sciences (CAS), ChinaZheng Wang, Wuhan University, China
Shuo Tian, Shandong University of Traditional Chinese Medicine, China
Copyright © 2025 Cho, Lee, Choi, Yang and Woo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hyeonjun Woo, d29vaHllb25qdW5AZ21haWwuY29t
†These authors have contributed equally to this work and share first authorship
 Eunbyul Cho
Eunbyul Cho Seri Lee
Seri Lee Youngjin Choi
Youngjin Choi Changsop Yang
Changsop Yang Hyeonjun Woo
Hyeonjun Woo