- 1College of Acupuncture and Tuina, Changchun University of Chinese Medicine, Changchun, Jilin, China
- 2Department of Acupuncture and Tuina, Affiliated Hospital of Changchun University of Traditional Chinese Medicine, Changchun, Jilin, China
- 3School of Medical Information, Changchun University of Chinese Medicine, Changchun, Jilin, China
Background: Diabetic peripheral neuropathy (DPN) is a common complication of diabetes mellitus, characterized by high morbidity and significant disability. Traditional Chinese medicine (TCM) has shown potential in relieving symptoms and improving neurological function through multi-targeted mechanisms; however, the efficacy and safety of different TCM therapies have yet to be systematically evaluated.
Objective: This study aims to provide evidence-based medicine for treating DPN with TCM therapy by network meta-analysis (NMA).
Methods: This study comprehensively searched nine databases constructed up to November 2024. The quality and evidence of the included RCTs were assessed using the risk of bias assessment tool and GRADE pro, and pairwise meta-analysis and NMA were performed using RevMan, Stata, and R Studio. The results showed that 95 RCTs involving 8194 patients were included, containing 9 TCM therapies.
Results: TCM Decoration + Acupuncture ranked highest in improving the motor conduction velocity of the common peroneal nerve (SUCRA = 0.81), followed by TCM Decoction + Chinese Herbal Footbath (SUCRA = 0.80), electroacupuncture (SUCRA = 0.75). Regarding the sensory conduction velocity of the common peroneal nerve, TCM Decoration + Chinese Herbal Foot (SUCRA=0.87) ranked first, followed by TCM Decoction + Acupuncture (SUCRA = 0.83), and TCM Decoction (SUCRA = 0.51). Electroacupuncture (SUCRA = 0.83) ranks first in improving median nerve motor conduction velocity, followed by TCM Decoction + Acupuncture (SCURA = 0.98), TCM Decoction (SUCRA = 0.55). TCM Decoration + Acupuncture (SUCRA=0.98) ranks first in improving the sensory conduction velocity of the median nerve, followed by electroacupuncture (SUCRA = 0.51), and Chinese Patent Medicine (SUCRA = 0.51). TCM Decoration + Chinese Herbal Footbath (SUCRA = 0.85) ranked first in improving overall clinical symptoms of DPN.
Conclusion: The effectiveness and safety of traditional Chinese medicine therapy in treating DPN have been preliminarily verified. In clinical practice, conservative clinical stratification selection can be made based on the results of this study and the actual situation. In addition, due to the limited quality of the included studies, larger sample sizes and high-quality research are still needed.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/, identifier (CRD42024589159).
Introduction
About 5.37 million people worldwide have diabetes, and in 2045, it is expected to reach 783 million (1). Diabetic peripheral neuropathy (DPN) is one of the common complications of type 1 and type 2 diabetes mellitus. DPN is characterized by peripheral nerve involvement in the lower limbs, with symmetrical numbness, discomfort, and pain in the lower limbs, which often starts from the feet, spreads upward to the calves, and later spreads to the upper limbs. Clinical signs include profound sensory deficits, such as decreased or absent Achilles tendon reflex, knee tendon reflex, and positional and vibration senses, which often lead to gait and balance dysfunction (2). A meta-analysis including 29 randomized controlled trials with a total of 50,112 patients showed that the prevalence of DPN was strongly associated with age, duration of disease, and body weight of diabetic patients, with an overall prevalence of approximately 30%, and that the prevalence of DPN was higher in type 2 diabetes mellitus (31.5%) than in type 1 diabetes mellitus (17.5%) (3). DPN has become one of the key factors triggering diabetic foot ulcers, which in severe cases will lead to lower limb amputation or death. According to statistics, the total cost of lower extremity foot ulcers and amputations due to diabetes mellitus in the United States is as high as 460 million - 1.37 billion dollars, and surveys in some European countries have found that the personal cost of amputations due to DPN amounts to 83728 dollars (4, 5). Research indicates that patients with diabetes who undergo amputation face a 68% mortality rate within five years (6). This high mortality rate highlights how DPN not only diminishes patients’ quality of life but also imposes significant financial burdens on families and society. As a result, considerable focus has been on finding effective treatments for DPN. The pathogenesis of DPN is complex. It is believed that metabolic disorders due to blood glucose and dyslipidemia can lead to the development of DPN by increasing oxidative stress, inflammation and insulin resistance, and through specific signaling pathways that can lead to demyelination or neuronal damage (7). There is currently no effective treatment for DPN, and the primary goal is to improve clinical symptoms. While controlling blood glucose levels can significantly enhance DPN that arises from type 1 diabetes, it appears to have minimal impact on DPN resulting from type 2 diabetes (8, 9). Pregabalin is considered a level-A treatment for DPN and is commonly prescribed for managing the neuropathic pain associated with this condition (8). However, several adverse effects should not be overlooked. A systematic review involving 38 randomized controlled trials found that the side effects of pregabalin include dizziness, blurred vision, drowsiness, cognitive impairment, and decreased coordination. These adverse effects are related to the dosage selected. Additionally, the economic cost of the medication is a significant factor limiting its use (10). Gabapentin, another recommended medication, is limited in its use in elderly patients due to the higher doses used to achieve therapeutic effects (11). Moreover, adverse reactions still occur (12). Tricyclic antidepressants have demonstrated some efficacy for neuropathic pain in a few small randomized controlled trials. However, the evidence remains insufficient, and side effects significantly limit their use (13, 14). The evidence regarding the long-term effectiveness of opioids, despite their strong short-term pain-relieving effects, is limited. Similar to tricyclic antidepressants, the potential for addiction and the side effects of long-term opioid use are concerns for many patients. Overall, these medications have minimal difference, with only one-third of patients experiencing symptomatic improvement. Additionally, there are numerous contraindications associated with their use (15). It is crucial to intervene early in DPN to slow the progression of the disease and prevent further nerve cell damage. As a result, there is an urgent need to find a safe and effective treatment to address the challenges faced by DPN patients.
TCM therapies have made some progress in treating DPN. TCM provides a range of internal and external treatments and focuses on assessing their effectiveness through various factors, including neurophysiology, blood rheology, levels of inflammatory markers, and glycolipid metabolism (16, 17). The advantage of TCM therapies is that they can target multiple targets and play a positive role in developing and treating DPN through multiple pathways. These therapies may work through various mechanisms, including reducing inflammation, oxidative stress, and apoptosis and alleviating endoplasmic reticulum stress; additionally, TCM can improve mitochondrial function and help regulate gut microbiota (18–20). In recent years, interventions in TCM for treating DPN have been classified into three main categories: single-drug extracts, herbal decoctions, and Chinese patent medicines. External therapies include acupuncture, Chinese herbal footbath, acupoint injections, and combinations of these methods. Although these therapies show promise in treating DPN, it remains unclear whether there are significant differences among the various therapeutic approaches and which intervention may be the most effective (19, 21). To evaluate the efficacy and safety of TCM therapies for DPN and identify the optimal treatment regimen, we will conduct direct and indirect comparisons of TCM protocols utilized for DPN thus far. We aim to provide evidence-based medical information to support the use of TCM therapies in treating DPN.
Methods
This systematic review and meta-analysis will adhere to the latest 2020 guidelines for systematic reviews and the PRISMA checklist (Supplementary Table S1). Before commencing this study, only a preliminary search was conducted to evaluate the feasibility and scope of potential studies. This initial search did not involve the formal screening process, data extraction, or analysis procedures. The protocol for this systematic review was registered on PROSPERO (registration number CRD42024589159) on September 10, 2024.
Eligibility criteria
We only analyzed randomized controlled trials of TCM therapies for treating DPN. RCTs were required to have the following inclusion criteria: (1) the diagnosis of patients with DPN should be precise (no restriction on age, gender, and duration of the disease); (2) the interventions in the treatment group were TCM therapies, including internal treatments of TCM (TCM Decoction, Chinese Patent Medicine, single herbs, etc.), external treatments of TCM (Chinese Herbal Footbath, acupuncture, electroacupuncture, etc.), or their combination; (3) The control group’s interventions were Western medicines only.
We will exclude the following studies: (1) duplicate studies, (2) reviews, animal experiments, protocols, conference papers, dissertations, and case reports; (3) studies that were not formally published; and (4) studies with incomplete data.
Information sources
We searched the following databases for RCTs of TCM therapies for the treatment of DPN (searches were performed until November 2024): PubMed, Cochrane Library, Embase, Web of Science, Medline, China National Knowledge Infrastructure (CNKI), Wanfang Data Knowledge Service Platform (Wanfang), VIP Database (VIP), and China Biology Medicine disc, (CBM disc). A detailed search strategy was completed on November 20, 2024, and some of the search strategies are documented in Supplementary Table S2.
Selection of studies and data collection
Three reviewers completed this process. Two reviewers (Yubo Gong and Xiaogang Hao) first excluded the duplicate studies used and then skimmed the titles and abstracts of the remaining studies. After excluding some studies that did not fit the topic, the full text of the remaining studies was carefully read to ensure data availability. Disagreements during the process will be addressed through discussion to reach a consensus. If these disagreements cannot be resolved, the third reviewer (Xuefeng Li) will make a decision after conducting an independent review. For the studies that met the inclusion criteria, we will extract the first author, year of publication, disease duration, age, sample size, intervention, and outcome indicators. We will use electromyography (EMG) results as the primary outcome indicator, and secondary outcome indicators may also include the Toronto Clinical Scoring System (TCSS), blood glucose, glycosylated hemoglobin (HbA1c), and total effective rate.
Risk of bias assessment
We used the risk of bias assessment tool recommended by the Cochrane Handbook to evaluate the risk of bias in the final included studies. The tool evaluated seven aspects of random generation: Random sequence generation, allocation concealment, blinding of patients and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases in the studies. The assessment of risk of bias will be reported as low risk, high risk, and unclear (Supplementary Table S3). Two reviewers (Ting Pan and Xue Zhou) will complete the assessment and discuss disagreements. If it is not resolved, a third reviewer (Siyi Wang) will assess and finalize it.
Synthesis methods
First, pairwise meta-analysis was performed using Review Manager 5.4 software. The OR (odds ratio) and MD (mean difference) values were used to analyze dichotomous and continuous variables. Cochran’s I-square (I2) was used to determine the heterogeneity. If I2 < 50%, it indicates no significant statistical heterogeneity among the studies, and a fixed-effect model should be adopted. Otherwise, a random-effects model will be applied.
For network meta-analysis (NMA), we used Stata 15.0 and RStudio software. Stata 15.0 was used to generate network evidence plots and funnel plots and conduct a sensitivity analysis. The “mvmeta” package in Stata was utilized to create network evidence plots, visually illustrating the relationships between different interventions. In these plots, each point represents an intervention, and the size of the node indicates the sample size. A line connecting two nodes signifies a direct comparison between the two interventions. In contrast, the thickness of the line reflects the sample size for those interventions that have a direct comparison. When there is a closed loop, the node-splitting method is required to assess whether the results are inconsistent. Funnel plots were used for publication bias, while Egger’s test was used for validation to prove the absence of publication bias when P > 0.05. The data were analyzed using the “gemtc” and “JAGs-4.3.1” packages in RStudio, and the consistency model was fitted based on the Markov chain Monte Carlo method (MCMC) framework to fit the consistency model. The consistency model was used for testing when P > 0.05, and vice versa, using the inconsistency model. The consistency model was used for testing when P > 0.05, and vice versa, using the inconsistency model. Binary variables were analyzed using OR values as effect sizes, continuous variables were analyzed using MD, and the 95% CI (Confidence interval) value of the effect sizes was calculated, with a 95% CI that did not contain one considered statistically significant. The potential scale reduction factor (PSRF) was used to assess the convergence effect of the results of the reticulated meta-analysis. When the PSRF value is closer to 1, it indicates a better convergence result and more reliable results. A table of two-by-two comparisons will be generated for the final results, and the surface under the cumulative ranking curve (SUCRA) values will be used to rank the interventions. SUCRA values reflect the relative rank order between interventions and do not directly indicate the magnitude of effect sizes or the clinical importance of differences. The fact that an intervention has a higher SUCRA value means that it has a higher likelihood of being relatively superior among the interventions compared, but whether that superiority reaches a clinically meaningful threshold needs to be judged in conjunction with the effect size estimates (e.g., risk ratios, mean differences, etc.) and their 95% confidence intervals.
Certainty of the evidence assessment
We utilized the GRADE system, as recommended by the BMJ (22), to evaluate the quality of evidence. The quality of evidence may be compromised in five ways: study limitations, inconsistency, indirectness, imprecision, and risk of bias. We used GRADE Pro version 3.6.1 to create a table outlining the levels of evidence.
Results
Study selection and characteristics of included trials
A total of 3279 studies were retrieved through the predefined search strategies, of which 1945 were duplicates. After the duplicates were eliminated, the remaining 1334 studies were browsed for titles and abstracts, and 770 were excluded in this step. Finally, the remaining 564 studies were scrutinized in full text, and 469 studies that did not meet the inclusion criteria were excluded. After the screening process, 95 RCTs were finally included; the complete screening process is shown in Figure 1.
The 95 RCTs incorporated within this study were all characterized by a two-arm trial design, encompassing 8,194 participants. The interventions encompassed TCM Decoction, Chinese Patent Medicine, acupuncture, electroacupuncture, TCM Decoction combined with acupuncture, TCM Decoction combined with Chinese Herbal Footbath, TCM Decoction combined with Chinese Medicine Fumigation, acupoint injections combined with Chinese Medicine Fumigation, and Western medicines, either oral or injectable. Of these RCTs, 87 (7833 participants) evaluated the total effective rate; 8 (550 participants) reported the adverse events; 87 (2461 participants) measured the motor conduction velocity of the common peroneal nerve, 23 (1893 participants) determined the sensory conduction velocity of the common peroneal nerve, 23 (2038 participants) evaluated the motor conduction velocity of the median nerve, 24 (2116 participants) assessed the sensory conduction velocity of the median nerve, 9 (817 participants) gauged the TCSS, 12 (1056 participants) scrutinized fasting blood glucose (FBG) levels, and 11 (992 participants) evaluated two-hour post-load plasma glucose (2hPG). Detailed information on the included studies is recorded in Table 1.
Risk of bias in studies
Overall, the risk of bias of the RCTs included in this study ranged from low-risk to high. Regarding randomization, about 17.89% (n = 17) of the RCTs were assessed as low risk using a randomized table of numbers. In contrast, the other studies were assessed as an unclear risk for only mentioning randomization without specifying the exact method. 89.47% (n = 85) of the RCTs were assessed as low risk for adequately reporting on the concealment of the allocation scheme; in terms of blinding, 98.95% of the studies were assessed as high risk due to specificity of treatment programs; for blinding of outcome assessment, 74.73% (n = 71) were assessed as low risk; 2.11% (n = 2) selectively reported on the outcome indicators mentioned in the text (but with justification), and were therefore assessed as unclear risk; all RCTs included in the present study were not found to be at risk of cause other biases in risk (Figure 2).
Pairwise meta-analysis
Motor conduction velocity of common peroneal nerve
In terms of improving the motor conduction velocity of the common peroneal nerve, TCM Decoction (MD = 3.36, 95%CI 2.97 to 3.75, I2 = 79%, P < 0.00001), Chinese Patent Medicine (MD = 2.96, 95%CI 1.74 to 4.19, I2 = 35%, P < 0.00001), acupuncture (MD = 2.47, 95%CI 1.41 to 3.53, I2 = 65%, P < 0.00001), electroacupuncture (MD = 5.13, 95%CI 3.82 to 6.44, I2 = 84%, P < 0.00001), TCM Decoction+ Acupuncture (MD = 5.31, 95%CI 4.30 to 6.32, I2 = 0%, P < 0.00001), TCM Decoction+ Chinese Herbal Footbath (MD = 3.27, 95%CI 2.35 to 4.19, I2 = 98%, P < 0.00001) all showed an advantage over Western medicines (Table 2). The forest plots are recorded in Supplementary Figure S1.
Sensory conduction velocity of common peroneal nerve
About the sensory conduction velocity of the common peroneal nerve, TCM Decoction (MD = 3.42, 95%CI 3.08 to 3.76, I2 = 94%, P < 0.00001), Chinese Patent Medicine (MD = 2.60, 95%CI 1.61 to 3.60, I2 = 90%, P < 0.00001), acupuncture (MD = 3.39, 95%CI 2.24 to 4.54, I2 = 0%, P < 0.00001), TCM Decoction+ Acupuncture (MD = 6.23, 95%CI 5.00 to 7.46, I2 = 90%, P < 0.00001), TCM Decoction+ Chinese Herbal Footbath (MD = 10.56, 95%CI 9.61 to 11.51, I2 = 99%, P < 0.00001) had a positive effect, the detailed results are recorded in Table 3, and the forest plots are recorded in Supplementary Figure S2.
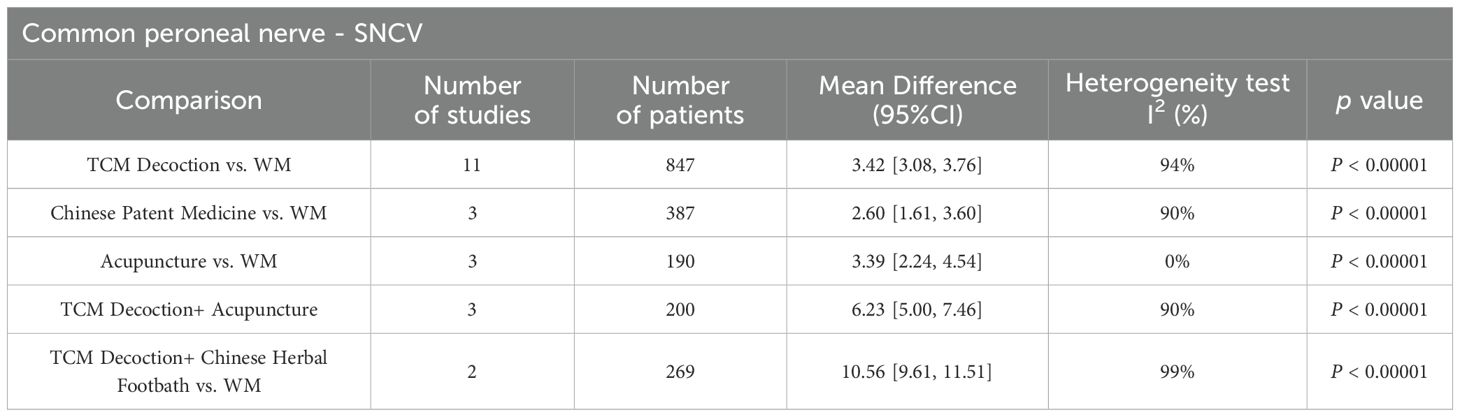
Table 3. Pairwise meta-analysis results of sensory conduction velocity of the common peroneal nerve.
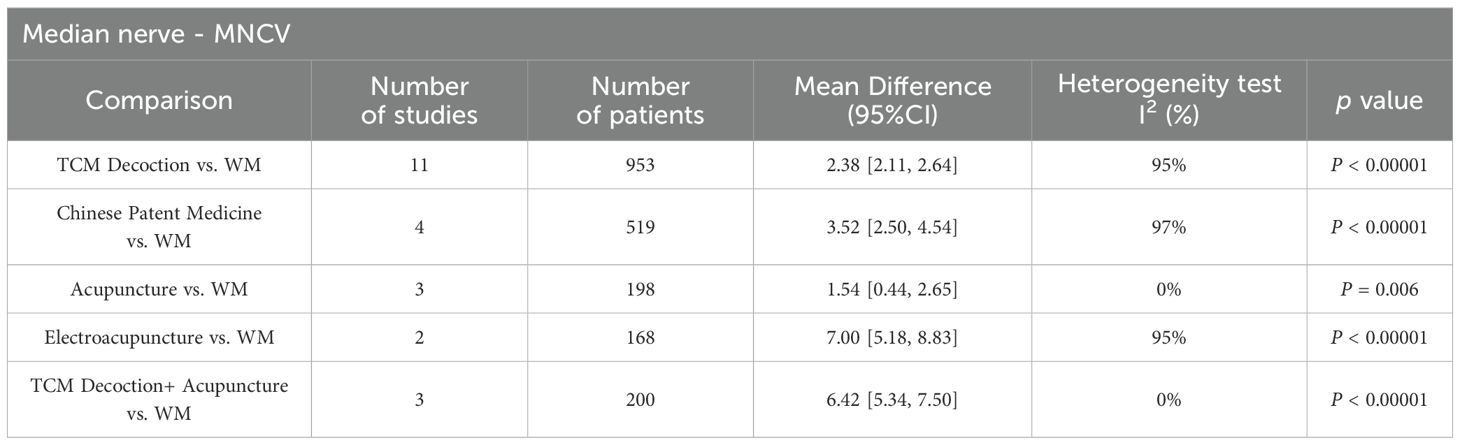
Motor conduction velocity of median nerve
In the realm of enhancing motor conduction velocity of median nerve, the efficacy of TCM Decoction (MD = 3.91, 95%CI 3.51 to 4.30, I2 = 95%, P < 0.00001), Chinese Patent Medicine (MD = 3.52, 95%CI 2.50 to 4.54, I2 = 97%, P < 0.00001), electroacupuncture (MD = 7.00, 95%CI 5.18 to 8.83, I2 = 95%, P < 0.00001), and TCM Decoction+ Acupuncture (MD = 6.42, 95%CI 5.34 to 7.50, I2 = 0%, P < 0.00001) has demonstrated superiority when contrasted with conventional Western medicine. Conversely, the therapeutic outcomes of acupuncture alone (MD = 1.54, 95%CI 0.44 to 2.65, I2 = 95%, P < 0.00001) seem to align closely in efficacy with those of Western medicine. Results are illustrated in Table 4, with the forest plots in Supplementary Figure S3.
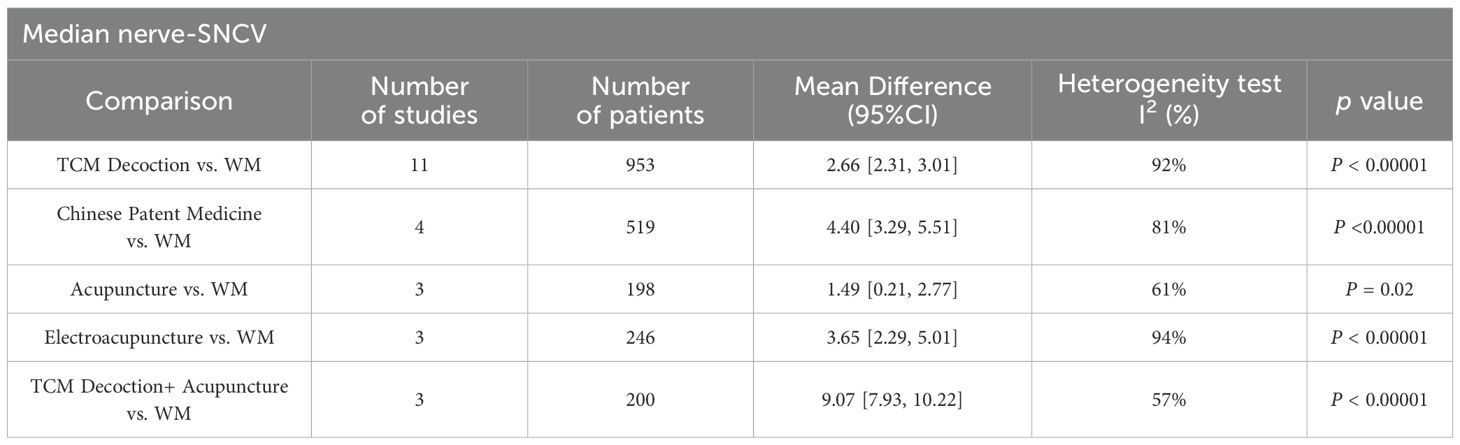
Sensory conduction velocity of median nerve
In terms of increasing sensory conduction velocity of the median nerve, TCM Decoction (MD = 2.66, 95%CI 2.31 to 3.01, I2 = 92%, P < 0.00001), Chinese Patent Medicine (MD = 4.40, 95%CI 2.29 to 5.51, I2 = 81%, P < 0.00001), electroacupuncture (MD = 3.65, 95%CI 2.11 to 2.64, I2 = 97%, P < 0.00001), TCM Decoction+ Acupuncture (MD = 9.07, 95%CI 7.93 to 10.22, I2 = 57%, P < 0.00001) showed remarkable efficacy compared to Western medicine, however, acupuncture (MD = 1.49, 95%CI 0.21 to 2.77, I2 = 61%, P = 0.02) did not show an advantage over Western medicine (Table 5). The forest plots are shown in Supplementary Figure S4.
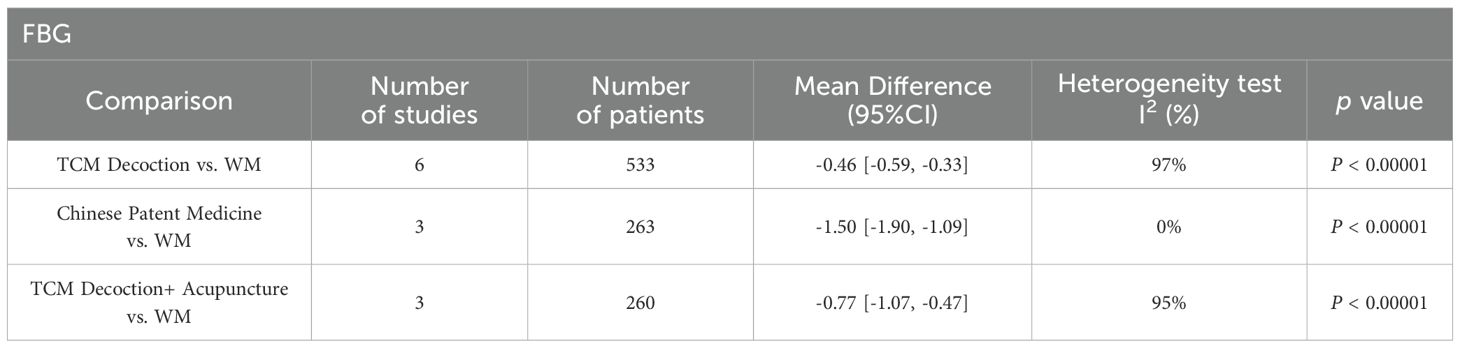
FBG
Regarding fasting glucose, TCM Decoction (MD = -0.46, 95%CI -0.59 to -0.33, I2 = 97%, P < 0.00001), Chinese Patent Medicine (MD = -1.50, 95%CI -1.90 to -1.09, I2 = 0%, P < 0.00001), TCM Decoction+ Acupuncture (MD = -0.77, 95%CI -0.17 to -0.47, I2 = 95%, P < 0.00001) had better efficacy than Western medicine (Table 6). Forest plots are recorded in Supplementary Figure S5.
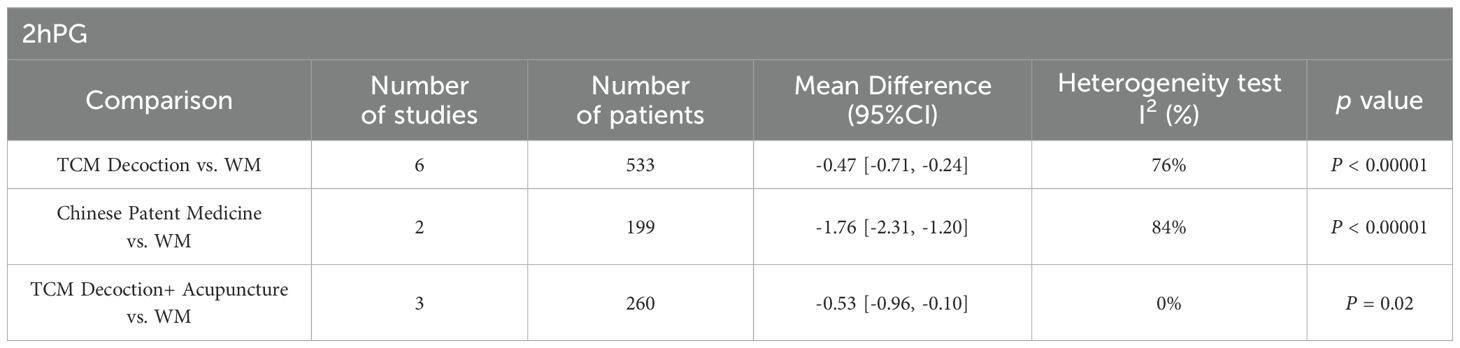
2hPG
The results of pairwise meta-analysis for 2hFG indicated that compared with Western medicine, TCM Decoction (MD = -0.47, 95%CI -0.71 to -0.24, I2 = 76%, P < 0.00001), Chinese Patent Medicine (MD = -1.76, 95%CI -2.31 to -1.20, I2 = 84%, P < 0.00001), and TCM Decoction+ Acupuncture (MD = -0.53, 95%CI -0.96 to -0.10, I2 = 0%, P = 0.02) had better clinical efficacy (Table 7). Forest plots are summarized in Supplementary Figure S6.
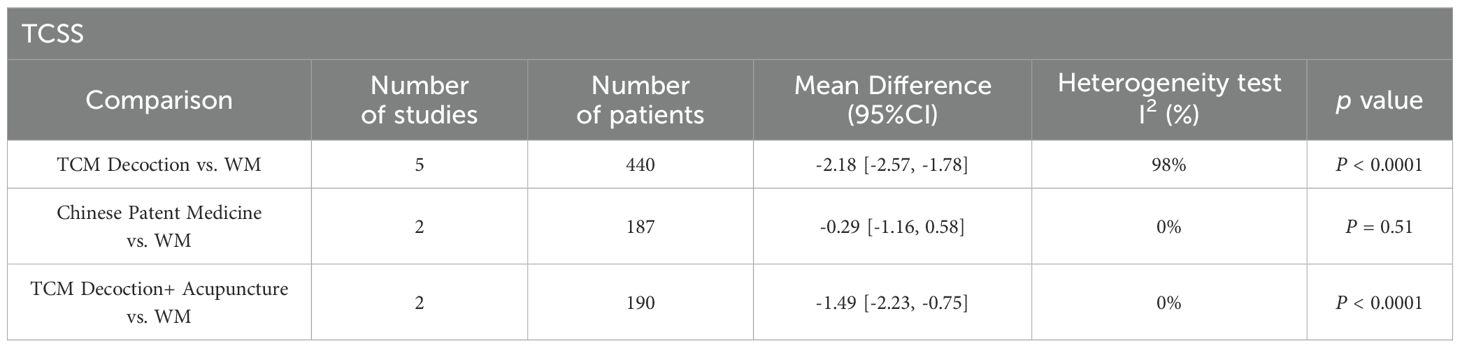
TCSS
The results of pairwise meta-analysis of TCSS showed that the efficacy of TCM Decoction (MD = -2.18, 95%CI -2.57 to -1.78, I2 = 98%, P < 0.0001), TCM Decoction+ Acupuncture (MD = -1.49, 95%CI - -2.23 to -0.75, I2 = 0%, P < 0.0001), showed clinical superiority over that of Western medicine. In contrast, Chinese Patent Medicine (MD = -0.29, 95%CI -1.16 to 0.58, I2 = 61%, P = 0.51) did not have this advantage. Detailed information is recorded in Table 8, and the forest plots are shown in Supplementary Figure S7.
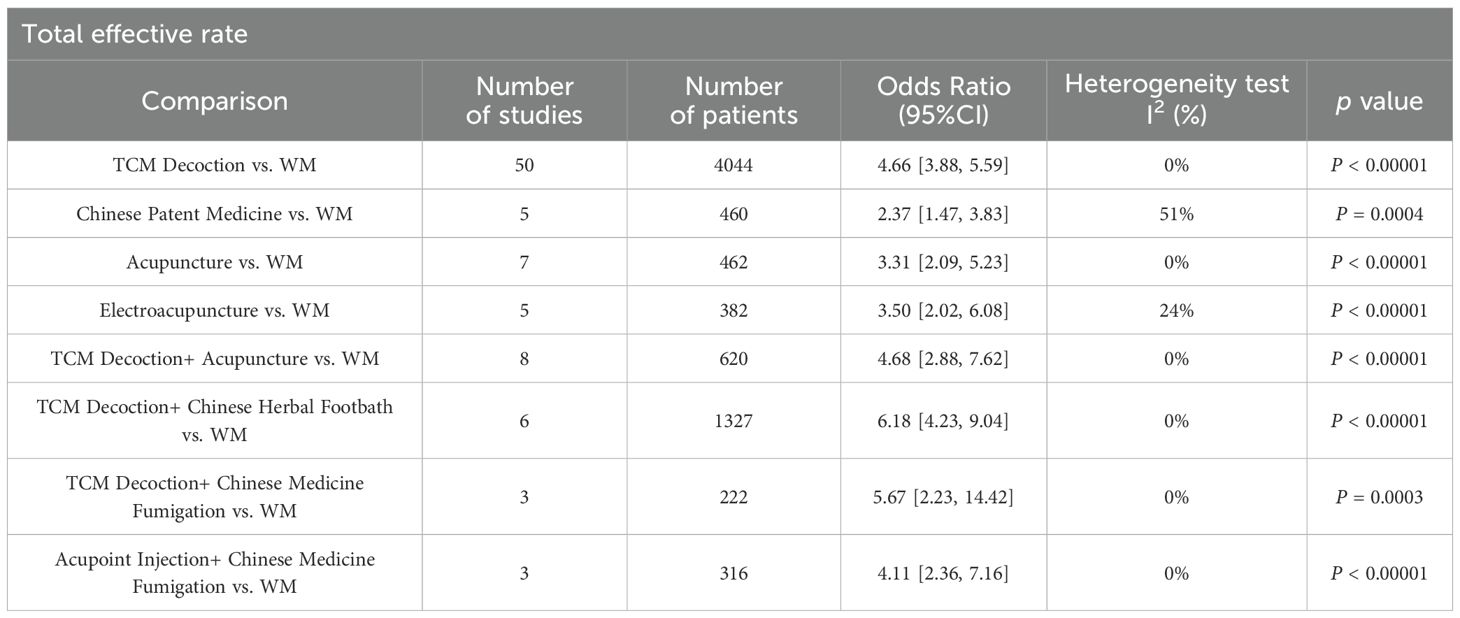
Total effective rate
The meta-analysis of total clinical effectiveness showed that TCM Decoction (MD = 4.66, 95%CI 3.88 to 5.59, I2 = 0%, P < 0.00001), Chinese Patent Medicine (MD = 2.37, 95%CI 1.47 to 3.83, I2 = 51%, P = 0.0004), acupuncture (MD = 3.31, 95%CI 2.09 to 5.23, I2 = 0%, P < 0.00001), electroacupuncture (MD = 3.50, 95%CI 2.02 to 6.08, I2 = 24%, P < 0.00001), TCM Decoction+ Acupuncture (MD = 4.68, 95%CI 2.88 to 7.62, I2 = 0%, P < 0.00001), TCM Decoction+ Chinese Herbal Footbath (MD = 6.18, 95%CI 4.23 to 9.04, I2 = 0%), TCM Decoction+ Chinese Medicine Fumigation (MD = 5.67, 95%CI 2.23 to 14.42, I2 = 0%, P = 0.0003), Acupoint Injection+ Chinese Medicine Fumigation (MD = 4.11, 95%CI 2.36 to 7.16, I2 = 0%, P < 0.00001) were superior to Western medicine (Table 9). Forest plots are given in Supplementary Figure S8.
Network meta-analysis
Network evidence plot
28 RCTs reported motor conduction velocity of common peroneal nerve and included a total of 7 therapies, and according to the network evidence plot (Figure 3A), it can be seen that TCM Decoction, Chinese Patent Medicine, acupuncture, electroacupuncture, TCM Decoction+ Acupuncture, TCM Decoction+ Chinese Herbal Footbath and Western medicine, with the highest frequency of comparisons between TCM Decoction and Western medicine; 22 RCTs reported sensory conduction velocity of common peroneal nerve (Figure 3B), with a total of 6 therapies, including TCM Decoction, Chinese Patent Medicine, acupuncture, TCM Decoction+ Acupuncture, TCM Decoction+ Chinese Herbal Footbath, and Western medicine; regarding the median nerve, the therapies involved included TCM Decoction, Chinese Patent Medicine, acupuncture, electroacupuncture, TCM Decoction+ Acupuncture, and Western medicine, of which 23 RCTs reported motor conduction velocity of median nerve and 24 RCTs reported sensory conduction velocity of median nerve, and the network evidence plots are shown in Figures 3C, D. 9 RCTs reported TCSS, involving 4 therapies, TCM Decoction, Chinese Patent Medicine, TCM Decoction+ Acupuncture, and Western medicine (Figure 3E); 12 RCTs reported FBG, 11 RCTs reported 2hPG, involving a total of 4 therapies, TCM Decoction, Chinese Patent Medicine, TCM Decoction+ Acupuncture, and Western medicine (Figures 3F, G); 87 RCTs reported total effective rate, involving 9 therapies, including TCM Decoction, Chinese Patent Medicine, acupuncture, electroacupuncture, TCM Decoction + Acupuncture, TCM Decoction + Chinese Herbal Footbath, TCM Decoction + Chinese Medicine Fumigation, Acupoint Injection + Chinese Medicine Fumigation, and Western Medicine (Figure 3H).
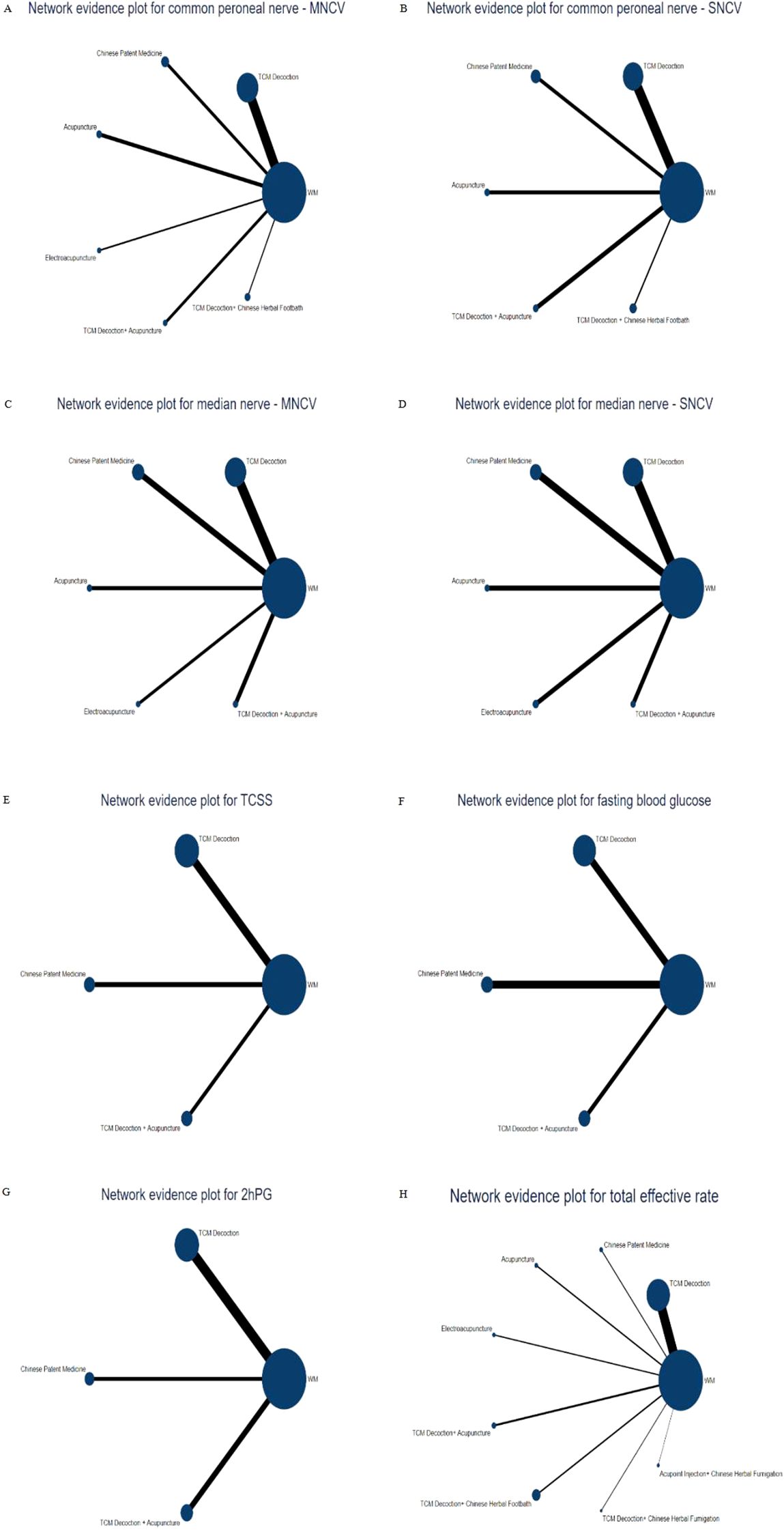
Figure 3. Network evidence plot. (A) Network evidence plot for motor conduction velocity of common peroneal nerve; (B) Network evidence plot for sensory conduction velocity of common peroneal nerve; (C) Network evidence plot for motor conduction velocity of median nerve; (D) Network evidence plot for sensory conduction velocity of median nerve; (E) Network evidence plot for TCSS; (F) Network evidence plot for FBG; (G) Network evidence plot for 2hPG; (H) Network evidence plot for total effective rate.
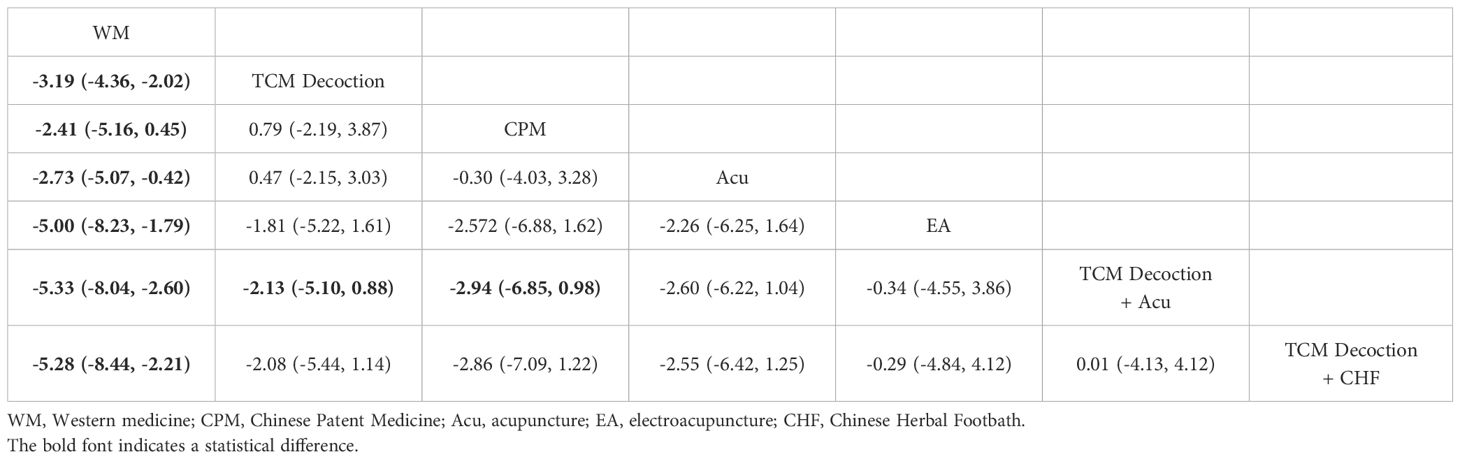
Motor conduction velocity of common peroneal nerve
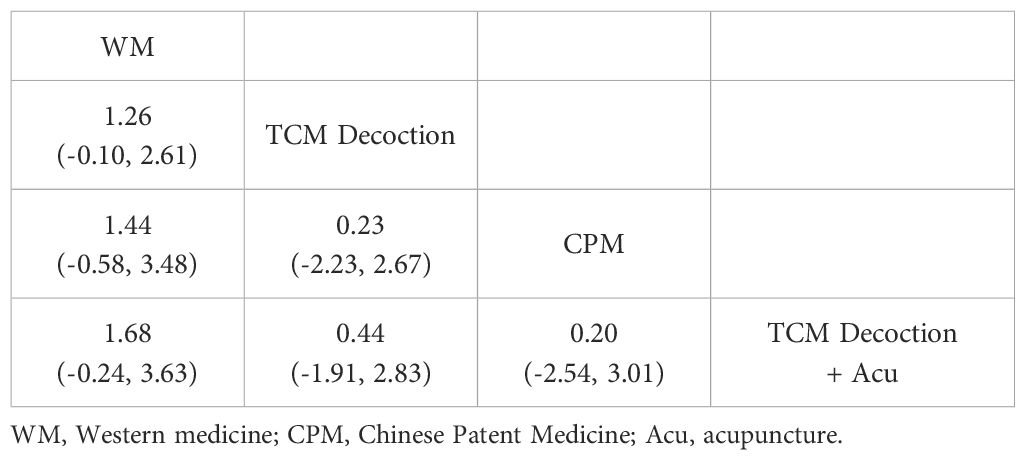
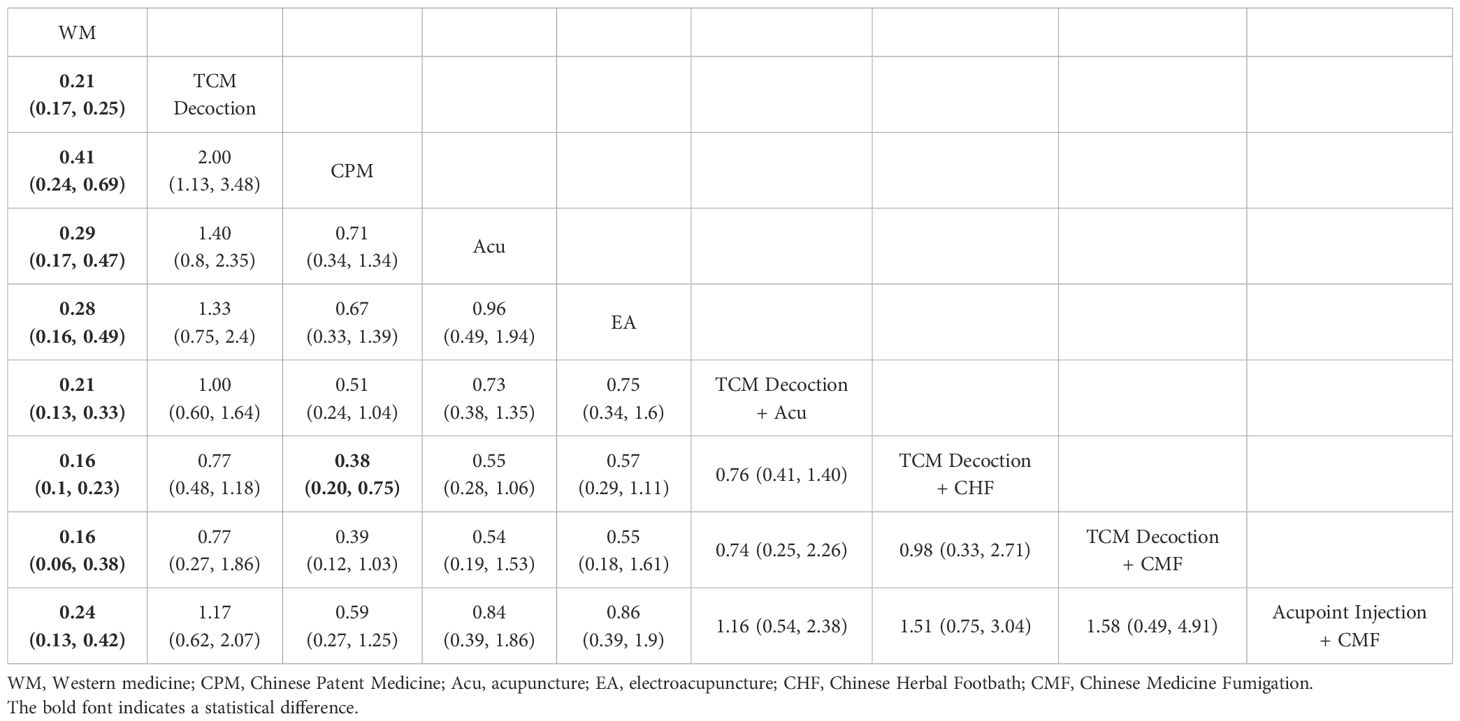
NMA results for motor conduction velocity of the common peroneal nerve showed that TCM Decoction (MD = -3.19, 95%CI -4.36 to -2.02), Chinese Patent Medicine (MD = -2.41, 95%CI -5.16 to 0.45), Acupuncture (MD = -2.729, 95%CI -5.07 to -0.42), Electroacupuncture (MD = -5.00, 95%CI -8.23 to -1.79), TCM Decoction+ Acupuncture (MD = -5.33, 95%CI -8.05 to -2.60), TCM Decoction+ Chinese Herbal Footbath (MD = -5.28, 95%CI -8.44 to -2.21) were all superior to Western medicine. TCM decoction combined + Acupuncture outperformed TCM decoction alone (MD = -2.13, 95% CI -5.10 to 0.88) and Chinese Patent Medicine (MD = -2.94, 95% CI -6.85 to 0.98). Comparisons between other therapies showed no statistically significant differences (Table 10).
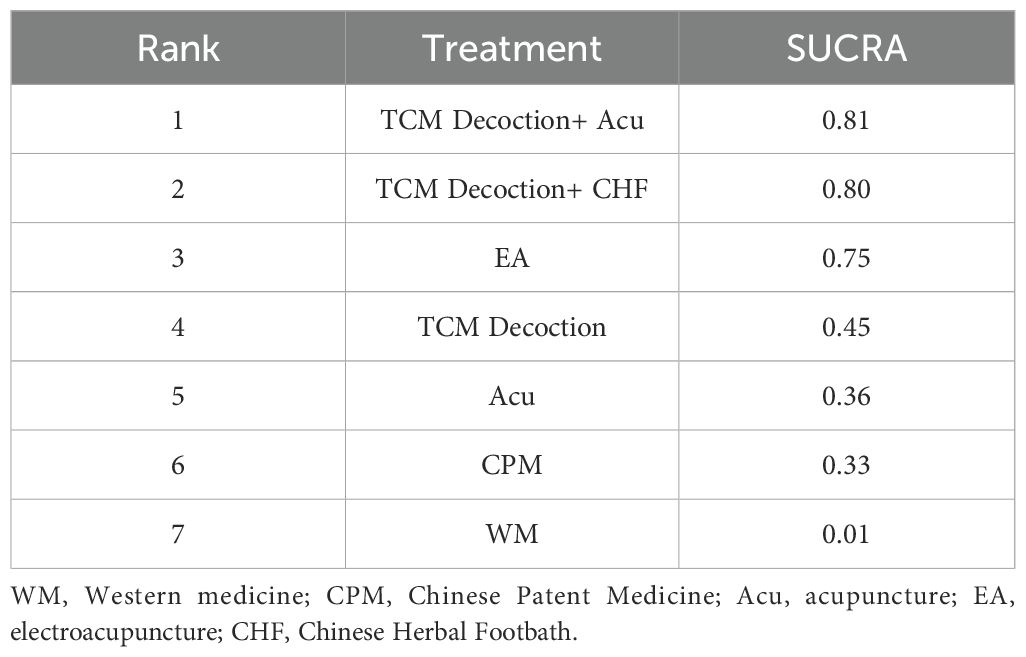
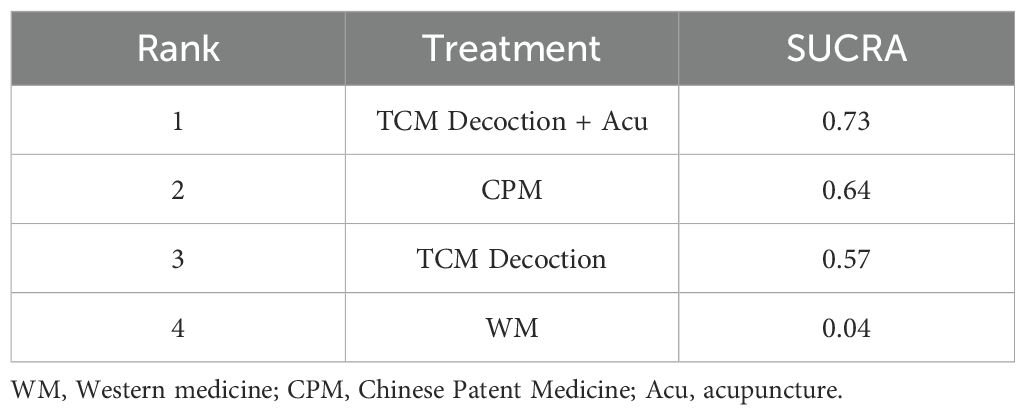
The SUCRA values and probability rank results of relevant TCM therapies to improve the motor conduction velocity of the common peroneal nerve in DPN patients were TCM Decoction + Acupuncture (SUCRA = 0.81), TCM Decoction + Chinese Herbal Footbath (SUCRA = 0.80), electroacupuncture (SUCRA = 0.75), TCM Decoction (SUCRA = 0.45), acupuncture (SUCRA = 0.36), Chinese Patent Medicine (SUCRA = 0.33), WM (SUCRA = 0.01) (Table 11).
Sensory conduction velocity of common peroneal nerve
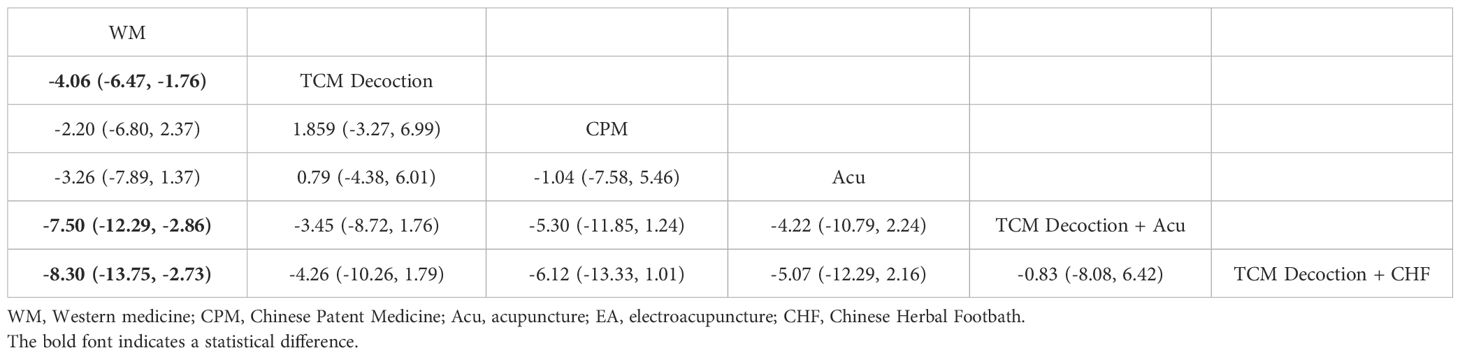
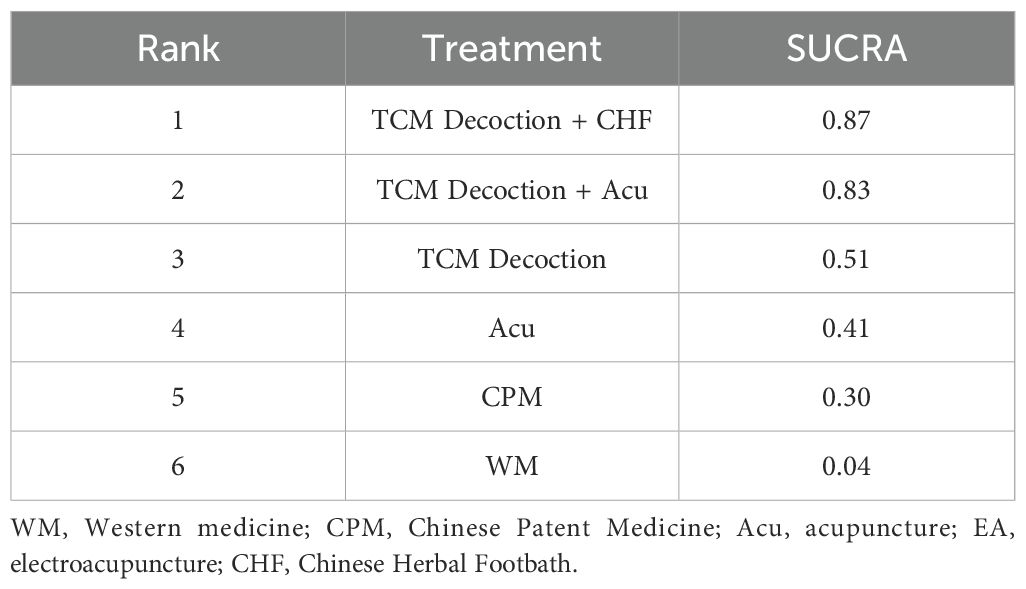
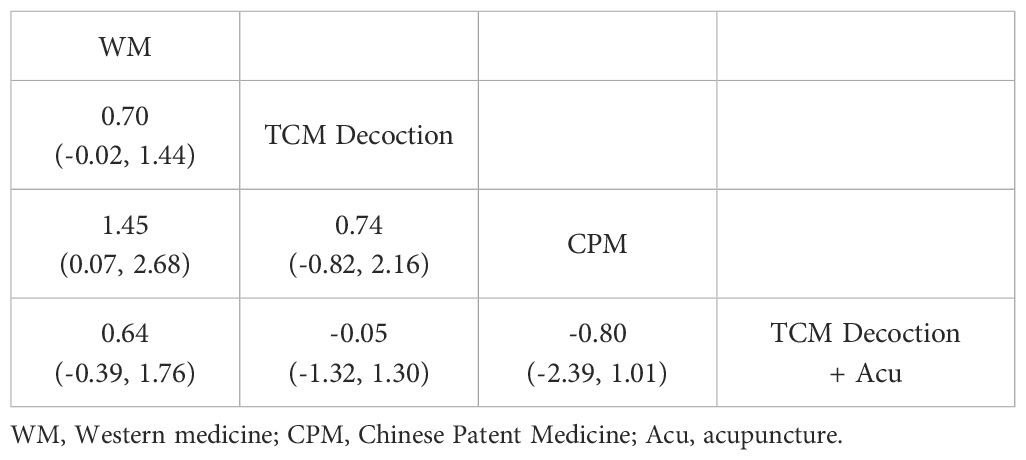
The results of NMA for sensory conduction velocity of common peroneal nerve showed that compared with Western medicine, TCM Decoction (MD = -4.06, 95%CI -6.47 to -1.76), TCM Decoction + Acupuncture (MD = -7.50, 95%CI -12.29 to -2.86, TCM Decoction + Chinese Herbal Footbath (MD = -8.30, 95%CI -13.75 to -2.73) were found to be superior, while the remaining therapies were not statistically significant when compared to each other (Table 12).
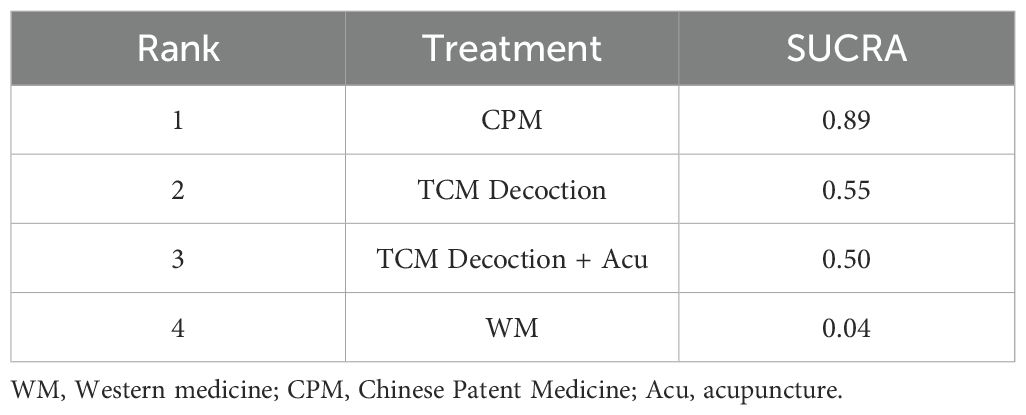
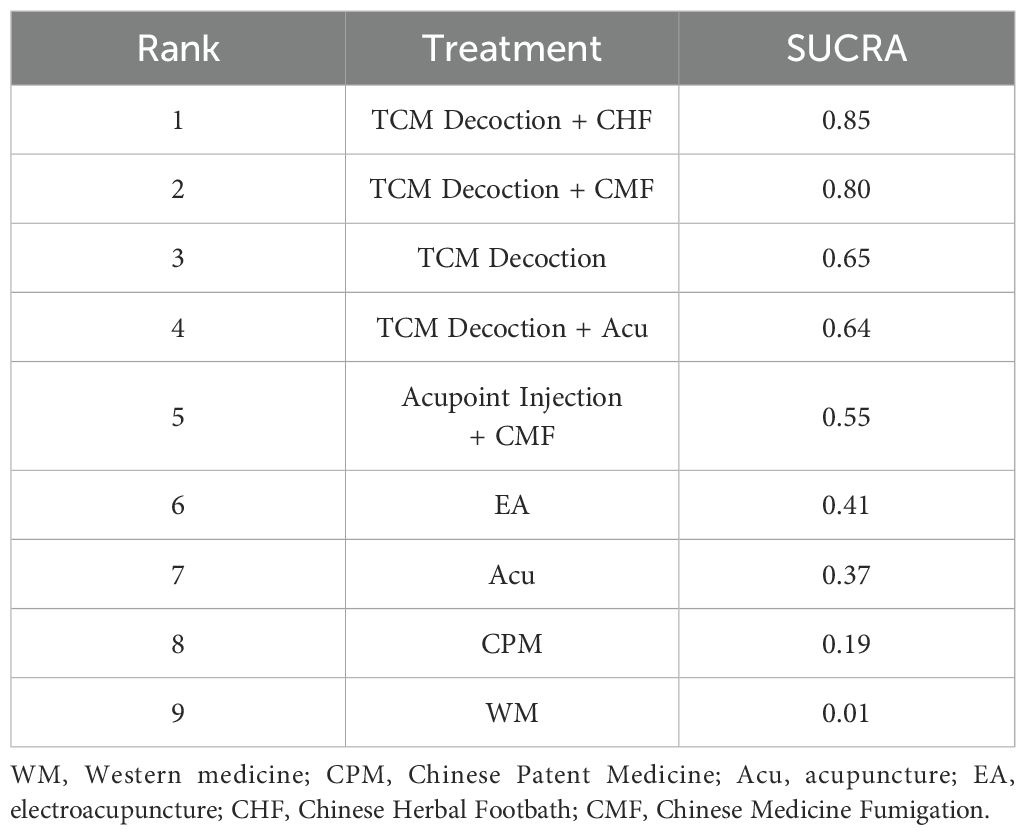
The SUCRA values and rank of TCM therapies to improve the sensory conduction velocity of the common peroneal nerve in patients with DPN were as follows: TCM Decoction + Chinese Herbal Footbath (SUCRA = 0.87), TCM Decoction + Acupuncture (SUCRA = 0.83), TCM Decoction (SUCRA = 0.51), acupuncture (SUCRA = 0.41), Chinese Patent Medicine (SUCRA = 0.30), and WM ((SUCRA = 0.04) (Table 13).
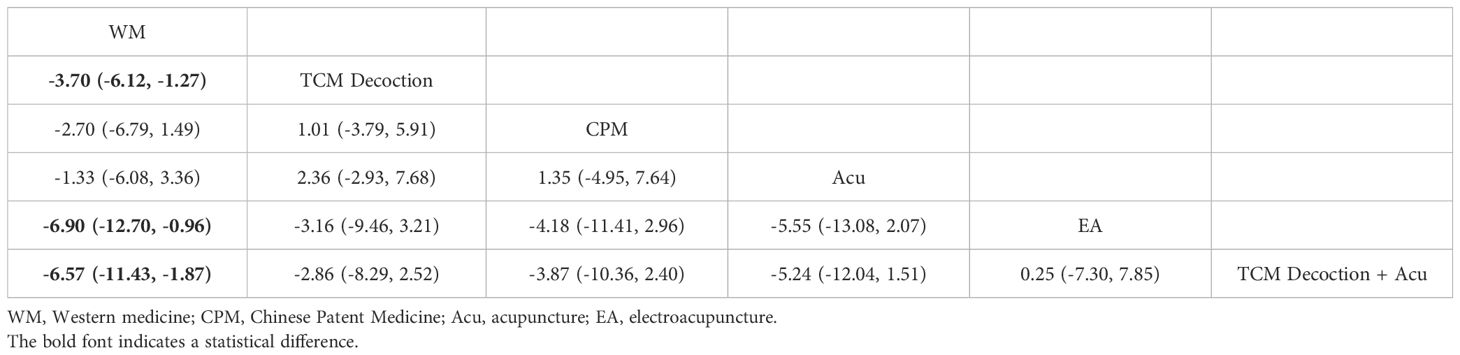
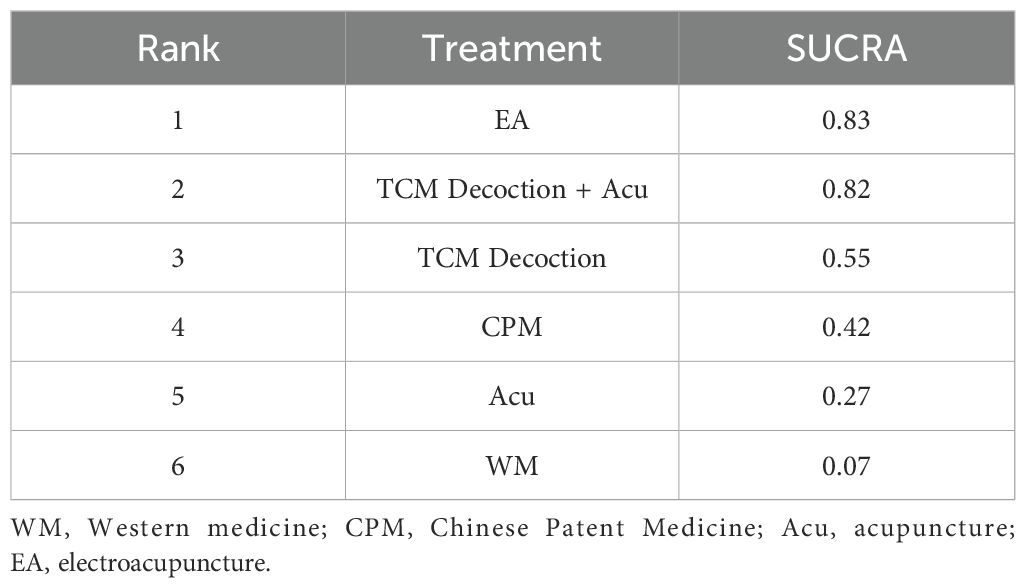
Motor conduction velocity of median nerve
The NMA results for motor conduction velocity of median nerve demonstrated that TCM Decoction (MD = -3.70, 95%CI -6.12 to -1.27), Electroacupuncture (MD = -6.90, 95%CI -12.70 to -1.08), TCM Decoction+ Acupuncture (MD = -6.57, 95%CI -11.29 to -1.87) were more effective than Western medicine. The comparison between the remaining therapies was not statistically significant (Table 14).
The SUCRA values and rank of TCM therapies to improve the motor conduction velocity of the median nerve were as follows: electroacupuncture (SUCRA = 0.83), TCM Decoction + Acupuncture (SUCRA = 0.83), TCM Decoction (SUCRA = 0.55), Chinese Patent Medicine (SUCRA = 0.42), acupuncture (SUCRA = 0.27), and Western medicine (SUCRA = 0.07) (Table 15).
Sensory conduction velocity of median nerve
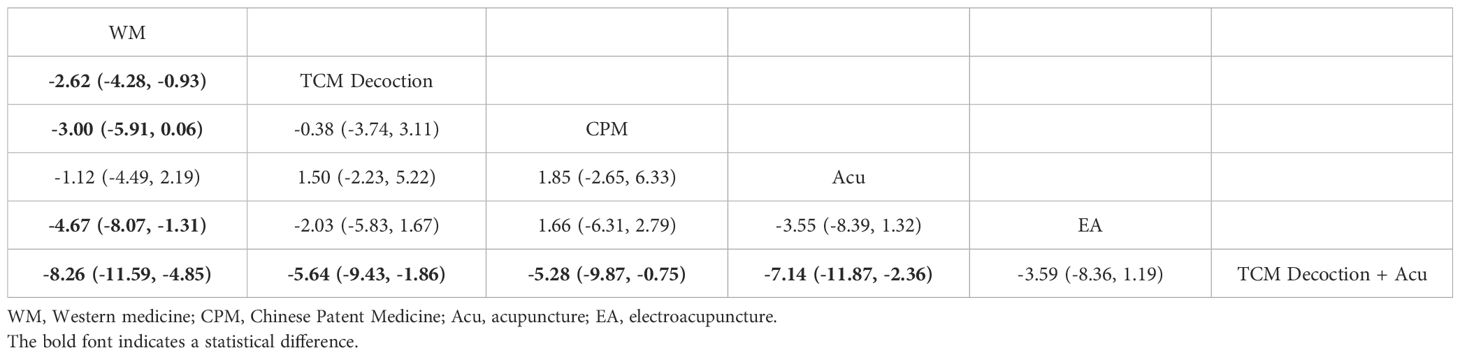
For sensory conduction velocity of median nerve, TCM Decoction (MD = -2.62, 95%CI -4.28 to -0.93), Chinese Patent Medicine (MD = -3.00, 95%CI -5.91 to -0.66), electroacupuncture (MD = - 4.67, 95%CI -8.07 to -1.31), and TCM Decoction + Acupuncture (MD = -8.26, 95%CI -11.59 to -0. 4.8) were more effective than Western medicine. In addition, TCM Decoction + Acupuncture was more effective than TCM Decoction (MD = -5.64, 95%CI -9.43 to -1.86), Chinese Patent Medicine (MD = -5.28, 95%CI -9.87 to -0.75), and acupuncture (MD = -7.14, 95%CI -11.87 to -2.3) (Table 16).
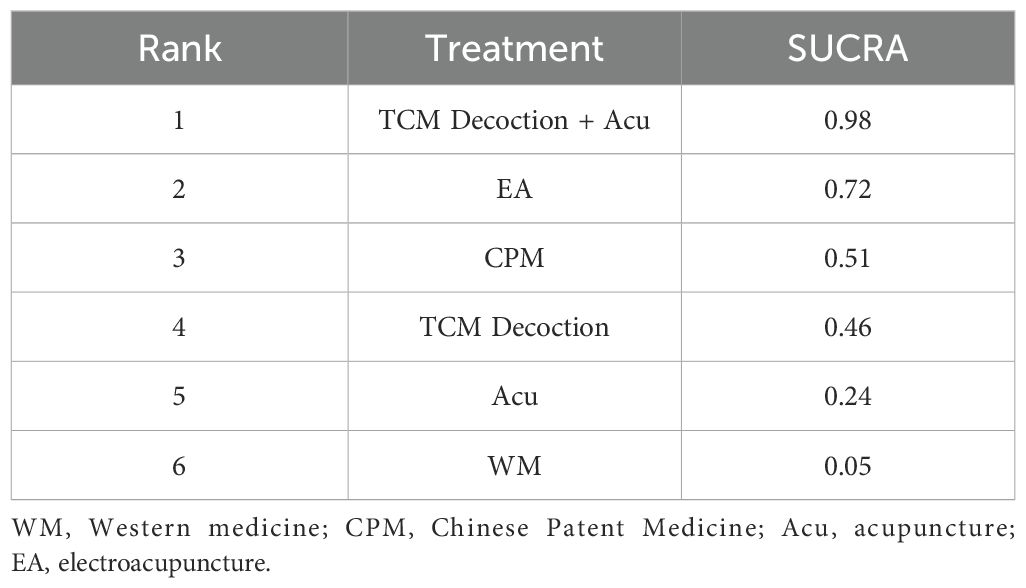
In terms of improving the median nerve’s sensory conduction velocity, TCM Decoction + Acupuncture (SUCRA = 0.98) became the best therapy, followed by electroacupuncture (SUCRA = 0.72), Chinese Patent Medicine (SUCRA = 0.51), TCM Decoction (SUCRA = 0.46), acupuncture (SUCRA = 0.24), and Western medicine (Table 17).
TCSS
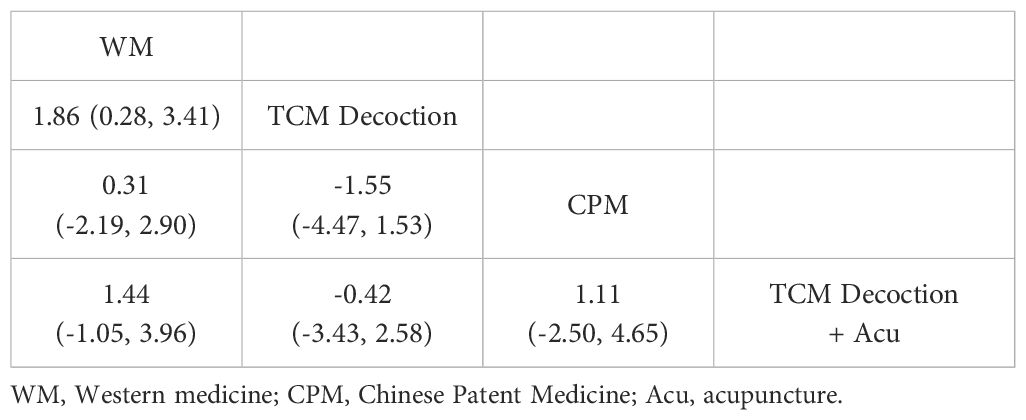
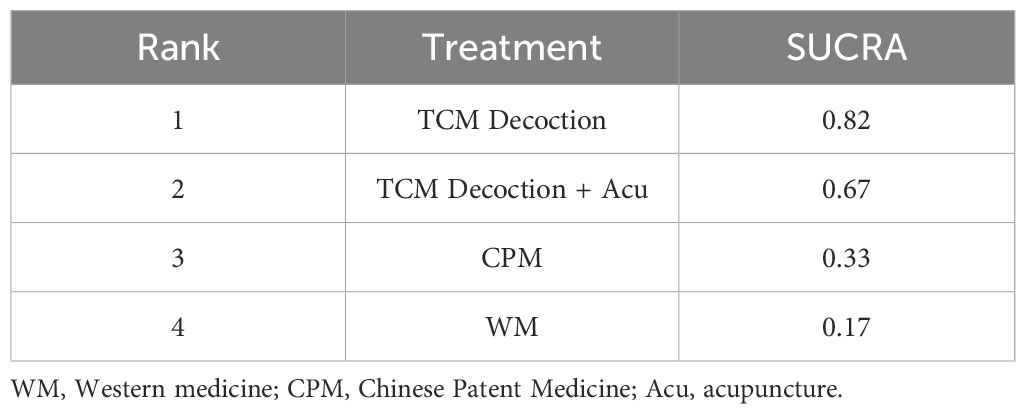
The NMA results from the TCSS showed no statistically significant differences in the comparisons between the 5 therapies (Table 18). Possible rank results are shown in Table 19.
FBG
The NMA results for fasting glucose showed that comparisons between treatments were not statistically significant (Table 20). The rank results are shown in Table 21.
2hPG
Regarding 2hPG, there are no statistically significant differences in the comparisons between the various TCM therapies (Table 22), and the possible rank results are shown in the Table 23.
Total effective rate
The NMA results of the total effective rate of TCM therapies to improve DPN showed that compared to Western medicine, TCM Decoction (OR = 0.21, 95%CI 0.17 to 0.25), Chinese Patent Medicine (OR = 0.41, 95%CI 0.24 to 0.69), acupuncture (OR = 0.29, 95%CI 0.17 to 0.47), electroacupuncture (OR = 0.28, 95%CI 0.16 to 0.49), TCM Decoction + Acupuncture (OR = 0.21, 95%CI 0.13 to 0.33), TCM Decoction + Chinese Herbal Footbath (OR = 0.16, 95%CI 0.10 to 0.23), TCM Decoction + Chinese Medicine Fumigation (OR = 0.16, 95%CI 0.06 to 0.38), Acupoint Injection + Chinese Medicine Fumigation (OR = 0.24, 95%CI 0.13 to 0.42) all achieved better clinical efficacy, in addition, TCM Decoction + Chinese Herbal Footbath was more effective than Chinese Patent Medicine (OR = 0.38, 95%CI 0.20 to 0.75) for overall symptom improvement in DPN patients. Other therapies were not statistically significant in a two-by-two comparison (Table 24). TCM Decoction + Chinese Herbal Football (SUCRA = 0.85) became the best therapy among TCM therapies; the rank of the TCM therapies is shown in Table 25.
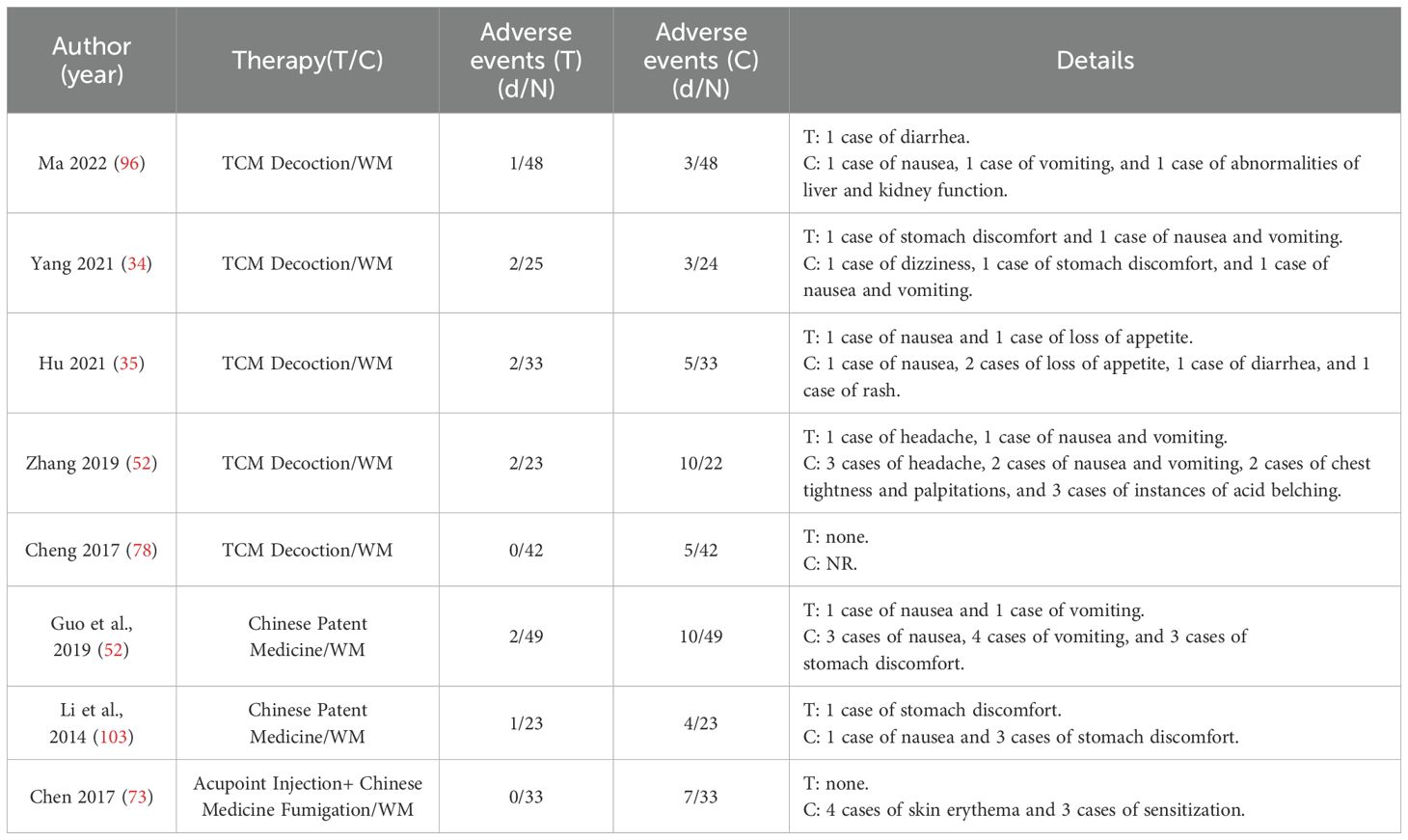
Adverse events
8 studies reported adverse events, as shown in Table 26. Adverse events that occurred in the treatment group included stomach discomfort, such as nausea and vomiting. In addition to the above, two slightly more serious adverse events were reported in the Western medicine group, which were impaired liver and kidney function. In addition, the acupoint injection combined with the Chinese Medicine Fumigation group reported 4 cases of skin erythema and 3 of sensitization. Overall, the number of adverse events in the treatment group was lower than in the control group, and no serious adverse events occurred.
Subgroup analysis
Due to the significant heterogeneity in some results, we conducted subgroup analyses (Supplementary Figure S9). The findings from subgroup analyses indicated that various TCM decoction prescriptions did not significantly impact the conduction velocity of the common peroneal nerve and median nerve (P > 0.05). Additionally, for the conduction velocity of the common peroneal nerve, varying durations of acupuncture treatment did not reveal any significant differences in effect size (P > 0.05).
Sensitivity analysis
We performed a sensitivity analysis of the indicators related to electromyography, including the motor conduction velocity of the common peroneal nerve, the sensory conduction velocity of the common peroneal nerve, the motor conduction velocity of the median nerve, and the sensory conduction velocity of the median nerve, and confirmed the stability of the results. The results of the sensitivity analysis are shown in Figure 4.
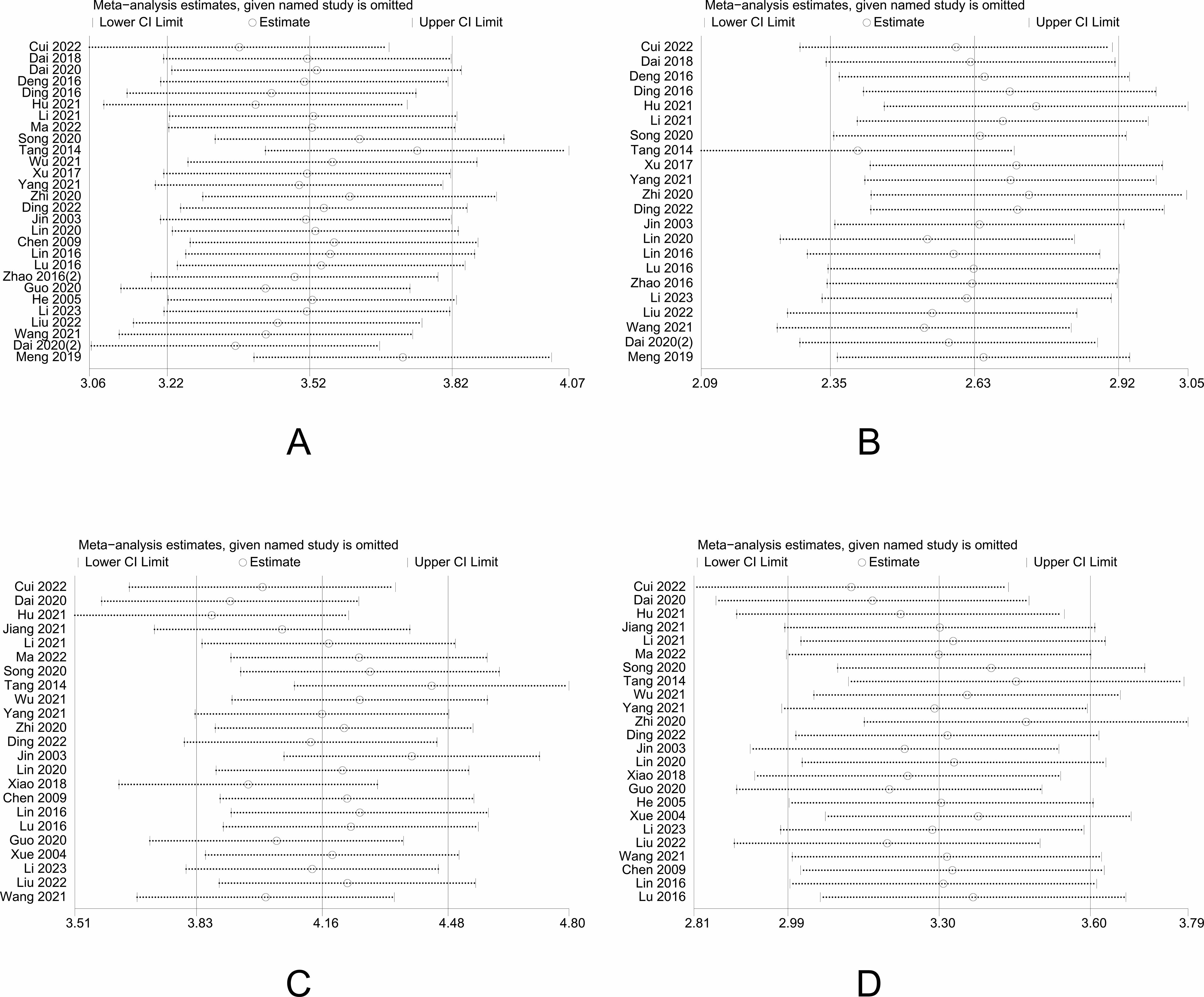
Figure 4. Results of sensitivity analysis. (A) sensitivity analysis result for motor conduction velocity of common peroneal nerve; (B) sensitivity analysis result for sensory conduction velocity of common peroneal nerve; (C) sensitivity analysis result for motor conduction velocity of median nerve; (D) sensitivity analysis result for sensory conduction velocity of median nerve.
Publication bias
Stata 17.0 generated a comparison-corrected funnel plot (Figure 5). The funnel plot indicated the possibility of a small sample effect, so an Egger test was also conducted to further verify the existence of publication bias. The results of the Egger test are shown in the Supplementary Figure S10. The Egger test showed that P > 0.05, indicating that there was no publication bias.
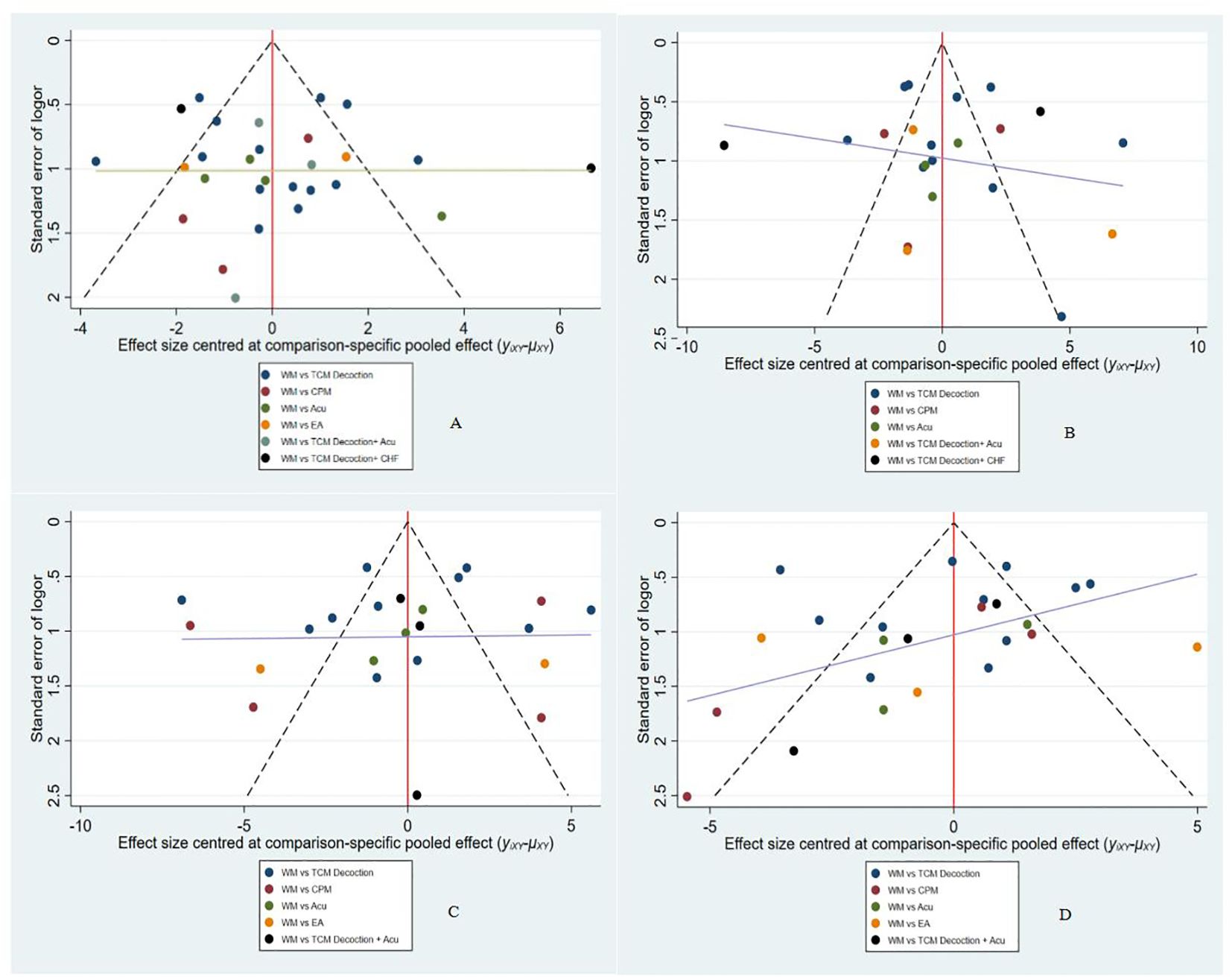
Figure 5. Publication bias. (A) funnel plot for motor conduction velocity of common peroneal nerve; (B) funnel plot for sensory conduction velocity of common peroneal nerve; (C) funnel plot for motor conduction velocity of median nerve; (D) funnel plot for sensory conduction velocity of median nerve.
Quality of evidence
The quality of the evidence was evaluated using the GRADE profiler, which showed that most of the evidence was downgraded due to the presence of risk of bias and inconsistency, with the quality of the evidence graded from very low to high (Supplementary Figure S11).
Discussion
In addition to blood glucose, many metabolic factors also play an important role in the development of DPN, so the focus of the treatment of DPN needs to be changed from simple glycemic control to multi-targeted therapy (118). According to previous investigations, glycemic control can only intervene in the development of DPN in T1DM but is ineffective in treating DPN caused by T2DM. As the research on TCM in treating DPN becomes more and more extensive, it has been found that TCM has the advantages of being multi-targeted, having good efficacy, and having mild side effects. The treatment of DPN with TCM is not limited to oral medications but also employs several external therapies or a combination of them, which has achieved significant clinical efficacy (21). Previous studies have explored the effectiveness of TCM external therapies on DPN but have not comprehensively investigated TCM therapies (119). Based on the above, we conducted a comprehensive search of RCTs of all therapies related to TCM for the treatment of DPN. We attempted to find the optimal therapeutic regimen of TCM for treating DPN through the NMA approach.
In this study, we retrieved 3279 TCM RCTs for the treatment of DPN and finally included 95. The 95 RCTs involved 9 therapies, including TCM Decoction, Chinese Patent Medicine, acupuncture, electroacupuncture, TCM Decoction+ Acupuncture, TCM Decoction+ Chinese Herbal Footbath, TCM Decoction+ Chinese Medicine Fumigation, Acupoint Injection+ Chinese Medicine Fumigation, and Western medicine. We evaluated electromyography (common peroneal nerve and median nerve), FBG, 2hPG, TCSS, and total effective rate. Furthermore, our findings indicate that therapies related to TCM can enhance patients’ blood glucose profiles by reducing FBG and 2hPG. It is widely recognized that effective management of blood glucose can alleviate clinical symptoms and halt the progression of the disease in patients with DPN. We evaluated neurophysiological indicators, motor and sensory conduction velocities of the common peroneal and median nerves (reflecting the recovery of nerve fiber function); glycemic indicators, including FBG and 2hPG (reflecting the control of blood glucose); TCSS and the total effective rate (evaluating the improvement of clinical symptoms). The pairwise meta-analysis and NMA results consistently showed that the TCM-related therapies demonstrated more significant clinical advantages in improving nerve conduction velocity than Western medicine. TCM-related therapies effectively improve clinical symptoms in DPN patients. Specifically, in pairwise meta-analysis, TCM therapies significantly improved nerve conduction velocity in DPN patients; however, it is worth noting that the current study did not find any advantage of acupuncture over Western medicine in improving the conduction velocity of the median nerve. Furthermore, our findings indicate that therapies related to TCM can enhance patients’ blood glucose profiles by reducing FBG and 2hPG. It is widely recognized that effective management of blood glucose can alleviate clinical symptoms and halt the progression of the disease in patients with DPN.
We conducted an NMA comparing the nine therapies pairwise for further analysis. The SUCRA values establish the final ranking of the interventions. It is crucial to clarify that while SUCRA values indicate the relative rank order among the treatments, they do not directly convey the magnitude of the effect sizes or the clinical significance of the differences observed. Electromyography (EMG) is one of the objective diagnostic tools for DPN and aids in its early diagnosis. The results of this study showed that for improving motor conduction velocity of common peroneal nerve, the top-ranked therapies compared to WM were: TCM Decoction + Acupuncture (SUCRA = 0.81), TCM Decoction + Chinese Herbal Footbath (SUCRA = 0.80), and Electroacupuncture (SUCRA = 0.75); for sensory conduction velocity of common peroneal nerve, the therapies with the highest probability of ranking top were: TCM Decoction + Chinese Herbal Footbath (SUCRA = 0.87), TCM Decoction + Acupuncture (SUCRA = 0.83), and TCM Decoction (SUCRA = 0.51); The NMA results for motor conduction velocity of median nerve indicated that electroacupuncture (SUCRA = 0.83), TCM Decoction + Acupuncture (SUCRA = 0.82), and TCM Decoction (SUCRA = 0.55) were the top three interventions; for improving sensory conduction velocity of median nerve, the top-ranked therapies were: TCM Decoction + Acupuncture (SUCRA = 0.98), electroacupuncture (SUCRA = 0.72), and Chinese Patent Medicine (SUCRA = 0.51); TCM Decoction + Chinese Herbal Footbath (SUCRA = 0.85) ranked first in improving the overall symptoms of DPN. However, it is important to note that the comparisons between these therapies showed no statistically significant differences. These findings indicate that, compared to WM, combination therapies based on TCM Decoction significantly affect the DPN indicators evaluated. Therefore, we conclude that TCM Decoction combination therapies (specifically Decoction + Acupuncture and TCM Decoction + Chinese Herbal Footbath) demonstrate the most pronounced therapeutic efficacy for DPN, outperforming either WM or single-modality TCM therapies (such as TCM Decoction alone or Acupuncture alone). Furthermore, while Chinese Patent Medicine may show some effect compared to WM (Tables 10, 16), its effect sizes were generally smaller than those of the higher-ranked interventions, suggesting its efficacy might be relatively weaker or associated with greater uncertainty. Consequently, in routine clinical practice, we do not recommend Chinese Patent Medicine as a first-line treatment for DPN. It may be considered as an alternative option for specific patient populations, such as those who cannot tolerate conventional medications or are seeking adjunctive therapy, especially when higher-ranked interventions are unavailable. Patients must be fully informed about the limitations of the evidence regarding the relative efficacy of Chinese Patent Medicine. Although the results of this study showed that TCM therapies showed effectiveness in improving TCSS, FBG, and 2hPG in comparison to Western medicine in pairwise meta-analysis, no statistical difference was found in the two-by-two comparison when performing NMA, so this study did not conclude the optimal intervention for TCM therapies to improve TCSS, FBG, and 2hPG. This study summarized the adverse events reported by 8 RCTs (Table 26), including dizziness, gastrointestinal discomfort, skin erythema, etc. The adverse events were mild, and the number of events was very low, so they can be considered safe. The present study yields findings worthy of further investigation. While the pairwise meta-analysis indicated that TCM therapies were effective in improving TCSS, FBG, and 2hPG when compared to Western medicines, the two-by-two direct comparisons within the framework of the current NMA did not reveal statistically significant differences between these therapies or when compared to Western medications. This limitation hinders our ability to draw definitive conclusions regarding the most effective interventions for enhancing TCSS, FBG, and 2hPG. Future research may require larger sample sizes or more refined designs for validation. Regarding safety assessment (Table 26), adverse events reported in the eight RCTs included in this study primarily involved mild occurrences such as dizziness, gastrointestinal discomfort, and skin erythema. The frequency of these events was low, and all were mild and self-limiting. Considering the available evidence, the various interventions explored, particularly the top-ranked TCM combination treatment, demonstrate a relatively favorable safety profile for patients with DPN.
Regarding the pathogenesis of DPN, a recent study demonstrated an association with metabolic abnormalities, oxidative stress, endoplasmic reticulum stress, mitochondrial dysfunction, microvascular dysfunction, and inflammation (120). Regarding the pathogenesis of DPN, a recent study demonstrated an association with metabolic abnormalities, oxidative stress, endoplasmic reticulum stress, mitochondrial dysfunction, microvascular dysfunction, and inflammation. In recent years, with in-depth research on the mechanisms of DPN in TCM, many innovative therapeutic options have been provided for clinical management and treatment. Oral medications used in TCM to treat DPN include herbal extracts, Chinese herbal compounds, and Chinese Patent Medicine. Included in this study were Chinese medicine compounds (referred to as TCM Decoction in this study) and Chinese Patent Medicine. The efficacy of TCM Decoction and Chinese Patent Medicine in treating DPN has been recognized in many clinical and mechanism studies. Many clinical and mechanism studies have recognized the efficacy of Chinese herbal compounds and Chinese Patent Medicine in treating DPN. A study in 2023 used metabolomics and microbiome to validate the mechanism of Huangqi Guizhi Wuwu Decoction for treating DPN. It was concluded that Huangqi Guizhi Wuwu Decoction could reduce inflammation and oxidative stress by regulating sphingolipid metabolism, biosynthesis of unsaturated fatty acids, arachidonic acid metabolism, and lactobacilli, thus improving the structure of peripheral nerves and enhancing the sciatic nerve conduction velocity in DPN mice (121). Another study verified that Jiaweibugan decoction regulates glutathione, nuclear factor kappa B p 65, and p38 mitogen-activated protein kinase expression through the anti-oxidative stress pathway, thereby repairing damaged peripheral nerves (122). In Chinese Patent Medicine, a study found that Compound Qiying Granules could improve peripheral nerve fiber myelination lesions through endoplasmic reticulum stress and apoptosis (123). As Chinese medicine research continues to deepen, herbal extracts are created. Herbal extracts are extracted, separated, and processed from herbs using modernized techniques. Studies of their pharmacological mechanisms have provided strong evidence for using TCM in treating DPN. Based on their chemical structures, herbal extracts used in treating DPN can be categorized into glycosides, phenols, alkaloids, flavonoids, etc. Specifically, it includes Notoginsenoside R1 extracted from Panax notoginseng, Astragaloside IV extracted from Astragali radix, Saikosaponin d extracted from Radix Bupleuri, and Puerarin extracted from Radix puerariae, etc. The above herbal extracts have been verified to improve DPN through anti-inflammatory, antioxidative, and endoplasmic reticulum stress regulation (124–126). Chinese Herbal Footbath is one of the external treatments of TCM, which enables the pharmacological effects of the above-mentioned herbs to be absorbed directly through the skin of the feet, acupoints, reflex zones, etc., and reach the lesions directly. Acupuncture is another standard external treatment method in TCM. In recent years, acupuncture has been widely researched to treat clinical diseases in various disciplines, and the related mechanism research has gradually improved. Studies have shown that acupuncture can treat DPN by regulating oxidative stress, improving inflammation, and regulating nerve growth factors (127–130). The above provides a reliable basis for our findings. It is well known that DPN patients first present with sensory deficits in the lower extremities, followed by sensory deficits in the upper extremities, and with the progression of the disease, some may present with motor deficits. For most DPN patients, sensory impairment is the main symptom of DPN patients, and this may be a long-term process. For sensory deficits in DPN, our results suggest that the combination therapy of TCM Decoction becomes the best treatment option to improve the sensory conduction velocity of the common peroneal and median nerve; in addition, this study also found that the most effective treatment to improve the overall symptoms of patients with DPN is TCM Decoction + Chinese Herbal Footbath. TCM Decoction has the advantage of multi-target regulation, which can not only directly improve the symptoms of DPN through its pharmacological action but also achieve the purpose of blood glucose regulation through compatibility and slow down the development of DPN (131, 132). Therefore, TCM Decoction combined with Chinese Herbal Footbath or acupuncture is a comprehensive treatment program that combines internal and external treatments to enhance the effect of directly reaching the lesion and effectively targeting the sensory disorders of DPN patients. As for motor dysfunction, although they are less common than sensory impairment, they can still be detected in electromyography. Our results showed that TCM Decoction + Acupuncture emerged as the best intervention to improve the motor conduction velocity of the common peroneal nerve (SUCRA = 0.81), and electroacupuncture emerged as the best intervention to improve the motor conduction velocity of the median nerve (SUCRA = 0.83). Numerous studies have found that patients with DPN have extensive cerebral cortex thinning or reduced grey matter volume in the central nervous system (especially the brain, not just the peripheral nervous system) and that extensive structural damage to the brain may be the underlying cause of the motor dysfunction that occur in patients (133–135). As for motor dysfunction, although they are less common than sensory impairment, they can still be detected in electromyography. Our results showed that TCM Decoction + Acupuncture emerged as the best intervention to improve the motor conduction velocity of the common peroneal nerve (SUCRA = 0.81), and electroacupuncture emerged as the best intervention to improve the motor conduction velocity of the median nerve (SUCRA = 0.83). Numerous studies have found that patients with DPN have extensive cerebral cortex thinning or reduced grey matter volume in the central nervous system (especially the brain, not just the peripheral nervous system) and that extensive structural damage to the brain may be the underlying cause of the motor dysfunction that occur in patients. Previous studies have also found that acupuncture (including electroacupuncture) improves motor function by modulating spinal motor neurons, including the cerebellum (possibly by promoting neuronal repair and regeneration) (136, 137). The above evidence explains the findings of EMG-related indicators well.
Our study strictly followed the Cochrane Collaboration and PRISMA flowcharts. An extensive search was conducted for current TCM RCTs for DPN by developing detailed search strategies. Reliable results were reported in performing both pairwise meta-analysis and NMA; most were statistically significant (P < 0.05) in meta-analysis. When performing NMA, we evaluated the model by the Brooks-Gelman-Rubin method, where the model fit was determined by the Potential Scale Reduction Factor (PSRF), and the PSRF values in this study were all close to 1, demonstrating that the model convergence was acceptable. In addition, the results were stable when sensitivity analyses of the primary outcome indicators were performed. Since some studies were outside the 95% CI in the funnel plot when assessing publication bias, proving that there appeared to be minor sample effects, in order to assess whether these small sample effects had an impact on the results of the study, an Egger test was also done, the result of Egger test showed that they did not affect the reliability of the results.
Despite some valuable findings, this study has some limitations. First, the risk of bias and the quality of evidence of the included studies impacted the results. Some of the studies were defined as high-risk due to randomization and blinding; therefore, the quality of evidence was downgraded, affecting the credibility of the results. Indeed, implementing blinding in TCM RCTs faces inherent challenges. These difficulties stem from the fundamental conflict between TCM’s holistic nature, individualized diagnosis, treatment approach, and the standardized requirements of RCTs. Particularly for non-pharmacological therapies like acupuncture, double-blinding is unattainable, which inevitably limits the strength of our evidence. When summarizing the characteristics of the included studies (Table 1), we observed that some RCTs failed to provide detailed descriptions of the duration and stage of DPN, with some even lacking data on age and disease duration. In studies utilizing TCM decoctions or Chinese patent medicine, the compositions of the herbal formulations were not standardized. Similarly, acupuncture studies lacked consistency in the acupoints selected. These factors contributed to substantial heterogeneity in some outcomes (I² > 50%). Consequently, we performed subgroup analyses. These analyses revealed that neither different TCM herbal formulations nor varying acupuncture durations for nerve conduction velocity showed significant differences in effect sizes. Regrettably, due to limitations in the original studies, we could not conduct subgroup analyses on other potential sources of heterogeneity, such as age, disease duration, and follow-up periods. As evident in Table 1, several studies lacked data on age, disease duration, and follow-up periods. The results are regrettable despite our efforts to contact authors for missing data. Therefore, our findings cannot provide reliable references for patients with DPN of different ages or disease durations. Furthermore, the long-term efficacy of TCM-related therapies for DPN remains uncertain due to the scarcity of follow-up data, highlighting an important area for future research. The NMA results indicate that the 95% confidence intervals for some of the two-by-two comparisons of interventions are quite broad, particularly evident when comparing TCM Decoction + Acupuncture with WM. Such wide intervals may be attributed to the limited sample sizes in the original studies or the inherent heterogeneity of the combination therapies, including variations in herbal prescriptions, dosages, needling techniques, and duration. This underscores the necessity for future studies involving larger sample sizes and more rigorously standardized intervention protocols to provide more conclusive evidence. Despite these uncertainties, sensitivity analysis indicated that our results are reliable. However, the limited number of original studies prevented a quantitative analysis of HbA1c. Additionally, the pairwise comparisons of TCSS, FBG, and 2hPG did not reach statistical significance. Consequently, this study cannot conclude whether TCM therapies improve the TCSS or glycemic control in DPN patients. Future well-designed studies are warranted to validate these findings. It is important to note that the safety data for this study were derived from only eight RCTs, all of which reported minor adverse events related to TCM therapies. Although TCM therapies are generally considered safe, this finding presents some limitations that could restrict the applicability and reproducibility of the results across a broader range of populations, including different subgroups and individuals with comorbidities. Therefore, high-quality studies are necessary to assess the safety of TCM therapies for treating DPN further and to provide more reliable clinical guidance for decision-makers in healthcare.
Conclusions
The comprehensive TCM therapy can be an effective and relatively safe treatment for DPN. The conservative clinical stratification recommendation sequence is as follows:
1. Motor conduction velocity of common peroneal nerve: TCM Decoction + Acupuncture, TCM Decoction + Chinese Herbal Footbath, and electroacupuncture.
2. Sensory conduction velocity of common peroneal nerve: TCM Decoction + Chinese Herbal Footbath, TCM Decoction + Acupuncture, and TCM Decoction.
3. Motor conduction velocity of median nerve: electroacupuncture, TCM Decoction + Acupuncture, TCM Decoction.
4. Sensory conduction velocity of median nerve: TCM Decoction + Acupuncture, electroacupuncture, and Chinese Patent Medicine.
However, due to limitations in the quality of the included studies, larger sample sizes and high-quality research are still needed.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Author contributions
JH: Conceptualization, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. HW: Writing – original draft, Writing – review & editing. XH: Data curation, Resources, Writing – review & editing. TP: Resources, Software, Writing – review & editing. XL: Resources, Software, Writing – review & editing. XZ: Methodology, Resources, Software, Visualization, Writing – review & editing. SW: Methodology, Resources, Software, Visualization, Writing – review & editing. YG: Resources, Software, Writing – review & editing. LW: Investigation, Resources, Software, Writing – review & editing. SD: Investigation, Resources, Software, Writing – review & editing. XC: Supervision, Writing – review & editing. XW: Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This study was supported by the Science and Technology Program of the Education Department of Jilin Province (No. JJKH20250638K).
Acknowledgments
This study is gratefully acknowledged to all the authors of the RCTs who provided original data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2025.1596924/full#supplementary-material
References
1. Ahmad E, Lim S, Lamptey R, Webb DR, and Davies MJ. Type 2 diabetes. Lancet (London England). (2022) 400:1803–20. doi: 10.1016/S0140-6736(22)01655-5
2. Selvarajah D, Kar D, Khunti K, Davies MJ, Scott AR, Walker J, et al. Diabetic peripheral neuropathy: advances in diagnosis and strategies for screening and early intervention. Lancet Diabetes Endocrinol. (2019) 7:938–48. doi: 10.1016/S2213-8587(19)30081-6
3. Sun J, Wang Y, Zhang X, Zhu S, and He H. Prevalence of peripheral neuropathy in patients with diabetes: A systematic review and meta-analysis. Prim Care Diabetes. (2020) 14:435–44. doi: 10.1016/j.pcd.2019.12.005
4. Gordois A, Scuffham P, Shearer A, Oglesby A, and Tobian JA. The health care costs of diabetic peripheral neuropathy in the US. Diabetes Care. (2003) 26:1790–5. doi: 10.2337/diacare.26.6.1790
5. Tchero H, Kangambega P, Lin L, Mukisi-Mukaza M, Brunet-Houdard S, Briatte C, et al. Cost of diabetic foot in France, Spain, Italy, Germany and United Kingdom: A systematic review. Annales d’endocrinologie. (2018) 79:67–74. doi: 10.1016/j.ando.2017.11.005
6. Icks A, Scheer M, Morbach S, Genz J, Haastert B, Giani G, et al. Time-dependent impact of diabetes on mortality in patients after major lower extremity amputation: survival in a population-based 5-year cohort in Germany. Diabetes Care. (2011) 34:1350–4. doi: 10.2337/dc10-2341
7. Zhu J, Hu Z, Luo Y, Liu Y, Luo W, Du X, et al. Diabetic peripheral neuropathy: pathogenetic mechanisms and treatment. Front Endocrinol. (2023) 14:1265372. doi: 10.3389/fendo.2023.1265372
8. Callaghan BC, Cheng HT, Stables CL, Smith AL, and Feldman EL. Diabetic neuropathy: clinical manifestations and current treatments. Lancet Neurol. (2012) 11:521–34. doi: 10.1016/S1474-4422(12)70065-0
9. Callaghan BC, Little AA, Feldman EL, and Hughes RA. Enhanced glucose control for preventing and treating diabetic neuropathy. Cochrane Database systematic Rev. (2012) 2012:CD007543. doi: 10.1002/14651858.CD007543.pub2
10. Zaccara G, Gangemi P, Perucca P, and Specchio L. The adverse event profile of pregabalin: a systematic review and meta-analysis of randomized controlled trials. Epilepsia. (2011) 52:826–36. doi: 10.1111/j.1528-1167.2010.02966.x
11. Dworkin RH, Jensen MP, Gammaitoni AR, Olaleye DO, and Galer BS. Symptom profiles differ in patients with neuropathic versus non-neuropathic pain. J Pain. (2007) 8:118–26. doi: 10.1016/j.jpain.2006.06.005
12. Fuzier R, Serres I, Guitton E, Lapeyre-Mestre M, and Montastruc JL. Adverse drug reactions to gabapentin and pregabalin: a review of the French pharmacovigilance database. Drug Saf. (2013) 36:55–62. doi: 10.1007/s40264-012-0006-6
13. Moore RA, Derry S, Aldington D, Cole P, and Wiffen PJ. Amitriptyline for neuropathic pain in adults. Cochrane Database systematic Rev. (2015) 2015:CD008242. doi: 10.1002/14651858.CD008242.pub3
14. Pop-Busui R, Boulton AJ, Feldman EL, Bril V, Freeman R, Malik RA, et al. Diabetic neuropathy: A position statement by the American diabetes association. Diabetes Care. (2017) 40:136–54. doi: 10.2337/dc16-2042
15. Jensen TS, Karlsson P, Gylfadottir SS, Andersen ST, Bennett DL, Tankisi H, et al. Painful and non-painful diabetic neuropathy, diagnostic challenges and implications for future management. Brain: J Neurol. (2021) 144:1632–45. doi: 10.1093/brain/awab079
16. Fu Y, Wang Y, Li Z, Huang K, Gao Y, Xu S, et al. Evidence mapping of traditional Chinese medicine in diabetic peripheral neuropathy treatment. Front Pharmacol. (2024) 15:1325607. doi: 10.3389/fphar.2024.1325607
17. Meyer-Hamme G, Friedemann T, Greten J, Gerloff C, and Schroeder S. Electrophysiologically verified effects of acupuncture on diabetic peripheral neuropathy in type 2 diabetes: The randomized, partially double-blinded, controlled ACUDIN trial. J Diabetes. (2021) 13:469–81. doi: 10.1111/1753-0407.13130
18. Li YY, Guan RQ, Hong ZB, Wang YL, and Pan LM. Advances in the treatment of diabetic peripheral neuropathy by modulating gut microbiota with traditional Chinese medicine. World J Diabetes. (2024) 15:1712–6. doi: 10.4239/wjd.v15.i8.1712
19. Zhang Y, Wu X, Yao W, Ni Y, and Ding X. Advances of traditional Chinese medicine preclinical mechanisms and clinical studies on diabetic peripheral neuropathy. Pharm Biol. (2024) 62:544–61. doi: 10.1080/13880209.2024.2369301
20. Zhao B, Zhang Q, He Y, Cao W, Song W, and Liang X. Targeted metabolomics reveals the aberrant energy status in diabetic peripheral neuropathy and the neuroprotective mechanism of traditional Chinese medicine JinMaiTong. J Pharm Anal. (2024) 14:225–43. doi: 10.1016/j.jpha.2023.09.007
21. Yang K, Wang Y, Li YW, Chen YG, Xing N, Lin HB, et al. Progress in the treatment of diabetic peripheral neuropathy. Biomed pharmacother = Biomed pharmacotherapie. (2022) 148:112717. doi: 10.1016/j.biopha.2022.112717
22. Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ (Clinical Res ed.). (2008) 336:924–6. doi: 10.1136/bmj.39489.470347.AD
23. Wu G and Fu J. Buyang Huanwu decoction combined with acupuncture and moxibustion in the treatment of diabetic peripheral neuropathy of qi deficiency and blood stasis type. Chin Med Mod Distance Educ China.. (2024) 2:106–9. doi: 10.3969/j.issn.1672-2779.2024.02.034
24. Li J and Yu H. Clinical observation on acupuncture combined with Yiqi Tongluo decoction in the treatment of diabetic peripheral neuropathy. Chin Med Mod Distance Educ China.. (2023) 5:97–9. doi: 10.3969/j.issn.1672-2779.2023.05.036
25. Liu J, Pan W, Peng L, Luo L, Xiao J, and Liang J. Clinical observation on curative effect of Huangdi internal acupuncture combined with Wenyang Jianbu decoction in the treatment of painful diabetic peripheral neuropathy with deficiency-cold type. J Guangzhou Univ Tradit Chin Med. (2022) 39:1090–6. doi: 10.13359/j.cnki.gzxbtem.2022.05.018
26. Ding Q, Reyimu ASA, Shen Y, Liu T, and Hu X. Effect of compound Qiying granule on SOD, MDA and 8-OHdG of patients with diabetic peripheral neuropathy. Guangming J Chin Med. (2022) 37:425–8. doi: 10.3969/j.issn.1003-8914.2022.03.024
27. Cui J, Liu M, Feng Z, Hu C, Yan J, and Wang C. Clinical observation on Huangqi Guizhi Wuwu decoction in Synopsis of the Golden Chamber in the treatment of diabetic peripheral neuropathy with qi deficiency and blood stasis syndrome. Chin Med Mod Distance Educ China.. (2022) 20:85–8. doi: 10.3969/j.issn.1672-2779.2022.14.031
28. Ma J, Zhang W, Qi L, and Wang J. Clinical effect of Yiqi Qingre Tongmai recipe in the treatment of qi deficiency and blood stasis type diabetic peripheral neuropathy. Diabetes New World.. (2022) 25:183–6. doi: 10.16658/j.cnki.1672-4062.2022.07.183
29. Zhao Y. Observation of the efficacy of Shenqi pills combined with Danggui Sini decoction in the treatment of yang deficiency and cold coagulation syndrome of diabetic peripheral neuropathy. Qinghai Med J. (2022) 52:49–51.
30. Han B. Clinical observation on Danggui Sini decoction combined with Chinese medicine fumigation and washing in the treatment of diabetic peripheral neuropathy. Chin Med Mod Distance Educ China.. (2021) 19:81–2. doi: 10.3969/j.issn.1672-2779.2021.24.029
31. Wang Q, Chen Q, Li C, and Chen D. Effect of acupuncture combined with Jianwei Huangqi Guizhi Wuwu decoction on nerve conduction velocity in patients with diabetic peripheral neuropathy. Zhejiang J Tradit Chin Med. (2021) 56:604–5. doi: 10.13633/j.cnki.zjtcm.2021.08.036
32. Jin S, Chen Q, Yao Z, and Lu H. Clinical observation of Shenxie Zhitong capsule in treating diabetic peripheral neuropathy of stagnant blockade of collaterals. Chin J Exp Tradit Med Formulae.. (2021) 27:81–7. doi: 10.13422/j.cnki.syfjx.20202430
33. Hu X and Zeng D. The effects of the Huangqi Guizhi Wuwu decoction on diabetic peripheral neuropathy and nerve conduction velocity. Clin J Chin Med. (2021) 13:89–91. doi: 10.3969/j.issn.1674-7860.2021.14.027
34. Yang R, Zhang Z, Zhu X, Zhang F, and Sun X. Effect of Yiqi Yangxue Tongbi decoction on clinical symptoms and nerve conduction velocity of diabetic peripheral neuropathy. Shaanxi J Tradit Chin Med. (2021) 42:608–11. doi: 10.3969/j.issn.1000-7369.2021.05.016
35. Bai Y. Effects of Shengmai San on TCM syndrome score and neuropathy score in diabetic peripheral neuropathy patients. Clin Res. (2021) 29:5–7.
36. Wu Q. Analysis on the clinical effect and safety of Tangshen in treating diabetic peripheral neuropathy. Chin Med Mod Distance Educ China.. (2021) 19:32–4. doi: 10.3969/j.issn.1672-2779.2021.24.013
37. Li L. Clinical observation of Erxian Dihuang decoction in the treatment of diabetic peripheral neuropathy. Guangming J Chin Med. (2021) 36:1399–401. doi: 10.3969/j.issn.1003-8914.2021.09.012
38. Jiang X and Fan Z. The effect of traditional Chinese medicine on the treatment of diabetic peripheral neuropathy patients. Med Equipment.. (2021) 34:102–3.
39. Liu H. To explore the clinical effect of Danggui Sini decoction Jiawei and external washing in the treatment of diabetic peripheral neuropathy. Cardiovasc Dis Electron J Integr Tradit Chin West Med. (2020) 8:175–8. doi: 10.16282/j.cnki.cn11-9336/r.2020.02.140
40. Dai W. Clinical study of Huangqi Guizhi Wuwu decoction combined with traditional Chinese herbal footbath in the treatment of diabetic peripheral neuropathy. Guangming J Chin Med. (2020) 35:1957–60. doi: 10.3969/j.issn.1003-8914.2020.13.004
41. Chen W. Clinical effect analysis of Huangqi Guizhi Wuwu Decoction combined with traditional Chinese medicine footbath in the treatment of diabetic peripheral neuropathy. J Pract Diabetol. (2020) 16:113–4.
42. Cheng Y and Feng X. Observation on therapeutic effect of modified Huangqi Guizhi Wuwu Decoction combined with acupuncture and moxibustion in the treatment of diabetic peripheral neuropathy. Chin Community Doctors.. (2020) 36:107–8. doi: 10.3969/j.issn.1007-614X.2020.26.052
43. Guo C. Effect of "Guben Tongluo" electro-acupuncture on levels of IGF-1, BDNF and NGF in patients with DPN. J Clin Acupunct Moxibustion.. (2020) 11:46–50.
44. Lin X and Wei A. Clinical study on compound Xueshuantong capsules for type 2 diabetic peripheral neuropathy. New Chin Med. (2020) 52:106–9. doi: 10.13457/j.cnki.jncm.2020.13.032
45. Cheng D, Xia H, and Huang F. Clinical observation on treatment of diabetic peripheral neuropathy with traditional Chinese medicine decoction. China Contin Med Educ. (2020) 12:161–3. doi: 10.3969/j.issn.1674-9308.2020.16.066
46. Song J and Tong X. Effect of modified Danggui Niantong decoction in the treatment of diabetic peripheral neuropathy. Chin Med Herald.. (2020) 17:130–3. doi: 10.20047/j.issn1673-7210.2020.23.033
47. Zhi L, Cao E, and Hua W. Clinical study of Huoluo Zhixiao prescription for diabetic peripheral neuropathy. Pharm Clin Chin Mater Med. (2020) 4:184–7. doi: 10.13412/j.cnki.zyyl.2020.04.024
48. Dai A, Wei S, and Dai H. Observation of the clinical effect of Yiqi Huayu Tongbi formula in the treatment of diabetic peripheral neuropathy with qi and yin deficiency. Shaanxi J Tradit Chin Med. (2020) 41:914–6. doi: 10.3969/j.issn.1000-7369.2020.07.022
49. Shi L. Clinical observation on Yigi Huoxue Tongbi decoction in the treatment of diabetic peripheral neuropathy. Chin Med Mod Distance Educ China.. (2020) 18:90–2. doi: 10.3969/j.issn.1672-2779.2020.02.037
50. Pang X, Pang X, Cong Y, Fang Y, and Li Y. Clinical study of Chuanwu Tongluo recipe in the treatment of diabetic peripheral neuropathy. China Contin Med Educ. (2020) 12:142–4. doi: 10.3969/j.issn.1674-9308.2020.01.063
51. Jian L. Analysis of clinical effect of Shuanghe decoction in the treatment of diabetic peripheral neuropathy. Diabetes New World.. (2020) 22:190. doi: 10.16658/j.cnki.1672-4062.2020.22.190
52. Zhang J. To investigate the clinical efficacy of Huangqi Guizhi Wuwu decoction in the treatment of diabetic peripheral neuropathy. Electron J Clin Med Lit.. (2019) 6:147–50. doi: 10.16281/j.cnki.jocml.2019.90.108
53. Zhang G and Peng D. Clinical observation of Taohong Siwu decoction combined with Shaoyao Gancao decoction combined with footbath formula in the treatment of diabetic peripheral neuropathy. China’s Naturopathy.. (2019) 1:55–7. doi: 10.19621/j.cnki.11-3555/r.2019.0134
54. Deng J. Clinical observation of Huangqi Guizhi Wuwu decoction combined with traditional Chinese medicine footbath in the treatment of diabetic peripheral neuropathy. China’s Naturopathy.. (2019) 11:50–1. doi: 10.19621/j.cnki.11-3555/r.2019.1128
55. Meng Q, Li X, Huang D, Jiang N, Jiang W, Li T, et al. Treating 99 cases of diabetic lower extremity peripheral neuropathy with TCM medicine plus foot bath. Clin J Chin Med. (2019) 17:52–5.
56. Chai H. Observation of the efficacy of Huangqi Guizhi Wuwu decoction combined with acupuncture in the treatment of diabetic peripheral neuropathy. World Latest Med Inf. (2019) 19:185–6. doi: 10.19613/j.cnki.1671-3141.2019.64.125
57. Guo J and Zhen Z. Analysis of the clinical efficacy of compound Danshen dripping pills in the treatment of blood stasis diabetic peripheral neuropathy. Strait Pharm J. (2019) 1:155–6.
58. Song T. Observation of the clinical efficacy of Duhuo Jisheng decoction in the treatment of peripheral neuropathy of type 2 diabetes. Clin J Chin Med. (2019) 31:19–21.
59. Shi H. Clinical effect of Huangqi Danshen Tongluo formula on diabetic peripheral neuropathy. Clin Res Pract. (2019) 21:114–5. doi: 10.19347/j.cnki.2096-1413.201921048
60. Xu C and Fu X. Clinical observation of Jiawei Huangqi Guizhi Wuwu decoction in the treatment of diabetic peripheral neuropathy. Shaanxi J Tradit Chin Med. (2019) 35:44.
61. Dai Y. Observation of the efficacy of Buyang Huanwu decoction Jiawei in the treatment of diabetic peripheral neuropathy. Electron J Clin Med Lit.. (2019) 6:159. doi: 10.16281/j.cnki.jocml.2019.07.139
62. Zhao Y, Liu Z, Dong N, Wang S, Ran X, and Zhang J. Application of Danggui Sini decoction in diabetic peripheral neuropathy and its effect on neuroelectrophysiological level. Chin Arch Tradit Chin Med. (2019) 37. doi: 10.13193/j.issn.1673-7717.2019.11.045
63. Hu Z. Observation of the clinical application effect and application value analysis of Huangqi Guizhi Wuwu decoction in the treatment of diabetic peripheral neuropathy. Diabetes New World.. (2019) 18:183–4. doi: 10.16658/j.cnki.1672-4062.2019.18.183
64. Fan G. Clinical observation of Huangqi Guizhi Wuwu decoction in the treatment of diabetic peripheral neuropathy. Med Diet Health. (2019) 12:83–4.
65. Yang L. Observation of the efficacy of Danggui Sini decoction with flavor and external washing in the treatment of diabetic peripheral neuropathy. J Pract Tradit Chin Med. (2018) 34:409–10.
66. Fan W. Observation of the efficacy of Buyang Huanwu decoction combined with traditional Chinese herbal footbath in the treatment of diabetic peripheral neuropathy. World Latest Med Inf. (2018) 62:164–5. doi: 10.19613/j.cnki.1671-3141.2018.62.080
67. Yu Z. The therapeutic effect of acupuncture combined with Ma Tong decoction on diabetic peripheral neuropathy. Chin J Mod Drug Appl. (2018) 12:101–2. doi: 10.14164/j.cnki.cn11-5581/r.2018.01.061
68. Xiao Q. Clinical observation of tongxinluo capsules in the treatment of diabetic peripheral neuropathy. BioMed Res. (2018) 3:519–22.
69. Dai Q and Xu X. Clinical study on the treatment of diabetic peripheral neuropathy with Huangqi Guizhi Wuwu decoction combined with Yunv decoction. Shaanxi J Tradit Chin Med. (2018) 39:482–4.
70. Sun L, Wu Q, and Ai Z. Buyang Huanwu decoction combined with Guizhi Fuling pills was used to treat 40 cases of diabetic peripheral neuropathy. Zhejiang J Tradit Chin Med. (2018) 53:808. doi: 10.13633/j.cnki.zjtcm.2018.11.017
71. Cao B. Clinical observation of Danggui Sini decoction in the treatment of cold coagulation and blood stasis type diabetic peripheral neuropathy. Guide China Med. (2018) 16:188–9. doi: 10.15912/j.cnki.gocm.2018.19.143
72. Zhang A. Clinical observation on treating 160 cases of diabetic peripheral neuropathy by TCM medicine fumigation plus point injection. Clin J Chin Med. (2017) 9:64–5.
73. Chen X. Clinical eficacy of point injection plus TCM medicine fumigation on diabetic peripheral neuropathy of lower limbs. Clin J Chin Med. (2017) 9:102–04. doi: 10.3969/j.issn.1674-7860.2017.19.051
74. Wang H. Observation of the clinical efficacy of Danggui Sini decoction in the treatment of diabetic peripheral neuropathy. Electronic J Pract Gynecological Endocrinol. (2017) 4. doi: 10.16484/j.cnki.issn2095-8803.2017.36.050
75. Zhang L. Clinical study of self-proposed Tongmai decoction in the treatment of diabetic peripheral neuropathy. Traditional Chin Med Rehabil. (2017) 8:58–9. doi: 10.19787/j.issn.1008-1879.2017.18.027
76. Gong L, Li Y, Zhang J, Zhang Y, Qiao X, and Zhang J. Clinical observation of Buyang Huanwu Decoction in the treatment of diabetic peripheral neuropathy. J Pract Traditional Chin Med. (2017) 33:1364–65.
77. Zhang K. Clinical efficacy analysis of Yiqi Huoxue Tongbi Decoction in the treatment of diabetic peripheral neuropathy. Electronic J Clin Med Literature. (2017) 4:20215–18. doi: 10.16281/j.cnki.jocml.2017.a3.012
78. Cheng Y. Clinical effeet of Yigi Huoxue Tongbi decoction in the treatment of diabetic peripheral neuropathy. China Pract Med. (2017) 12:116–18. doi: 10.14163/j.cnki.11-5547/r.2017.12.058
79. Deng H. Efficacy observation of Oigui Tangtongning formula on diabetic peripheral neuropathy. Shanxi J Traditional Chin Med. (2017) 33:10–1.
80. Liu M. Observation of the clinical efficacy of Yiqi Huoxue Tongbi Decoction in the treatment of diabetic peripheral neuropathy. Chin J Modern Drug Appl. (2017) 11:175–77. doi: 10.14164/j.cnki.cn11-5581/r.2017.06.089
81. Chou M. Clinical effect observation of Yiqi Huayu Tongbi formula in treating diabetic peripheral neuropathy. Clin J Chin Med. (2017) 9:47–8.
82. Xu D. Analysis of the improvement of nerve conduction velocity and efficacy of Danggui Sini decoction in the treatment of peripheral neuropathy of blood deficiency and cold coagulation diabetes. Modern Diagnosis Treat. (2017) 28:228–30.
83. Dong H, Zhang X, Liu M, Feng J, Wang X, Guo F, et al. Assess clinical effects of fuyang tongluo tang in treatment 80 patients of diabetic peripheral neuropathy with yang defciency and blood stasis syndrome. World Latest Med Inf. (2017) 17:142–43. doi: 10.3969/j.issn.1671-3141.2017.02.12
84. Zhang J. Observation of the efficacy of acupoint injection combined with traditional Chinese medicine fumigation in the treatment of diabetic peripheral neuropathy. Med Equip. (2016) 29:28–9.
85. Pan Y, Zeng J, Zeng Z, Huang Y, and Xu X. Clinical analysis of acupuncture combined with Huangqi Xiaoke formula in the treatment of diabetic peripheral neuropathy. J Pract Traditional Chin Med. (2016) 32:640–42.
86. Lu M, Li K, and Wang J. Acupuncture for distal symmetric multiple peripheral neuropathy of diabetes mellitus: a randomized controlled trial. Chin Acupuncture Moxibustion. (2016) 36:481–84. doi: 10.13703/j.0255-2930.2016.05.009
87. Zhao J and Zhang S. Observation of curative effect of eight confluence points acupuncture treatment in cure diabetic peripheral neuropathy. Shaanxi J Traditional Chin Med. (2016) 37:97–9. doi: 10.3969/j.issn.1000-7369.2016.01.050
88. Lin Q. Acupuncture of the collateral veins treated 35 cases of diabetic peripheral neuropathy. Fujian J Traditional Chin Med. (2016) 47:62–3. doi: 10.13260/j.cnki.jfjtcm.011270
89. Zhao H. Clinical study of Yiqi Huoxue Tongbi Decoction in the treatment of diabetic peripheral neuropathy. Cardiovasc Dis Electronic J Integrated Traditional Chin Western Med. (2016) 4:168. doi: 10.16282/j.cnki.cn11-9336/r.2016.34.242
90. Deng Z. Eficacy of the Huangqi Guizhi Wuwu decoction on diabetic peripheral neuropathy. Clin J Chin Med. (2016) 8:23–5. doi: 10.3969/j.issn.1674-7860.2016.29.009
91. Liu C. Clinical observation of 40 cases of diabetic neuropathy with flavored astragalus and Guizhi Wuwu decoction. Tianjin J Traditional Chin Med. (2016) 33:536–37.
92. Ding W, Chen W, and Li J. Clinical Study of Cold Congealing and Blood Stasis Type DiabeticPeripheral Neuropathy Treating by Danggui Sini Decoction. J Liaoning Univ Traditional Chin Med. (2016) 18:123–25. doi: 10.13194/j.issn.1673-842x.2016.09.037
93. Ma Z. Clinical observation of Jiawei Buyang Huanwu Decoction in the treatment of diabetic peripheral neuropathy. Chin Foreign Med Res. (2016) 14:45–6. doi: 10.14033/j.cnki.cfmr.2016.19.023
94. Qin S, Zhang X, and Wei M. Observation of the efficacy of Yiqi Huoxue Tongbi Decoction in the treatment of diabetic peripheral neuropathy. Electronic J Clin Med Literature. (2016) 3:3286–87. doi: 10.16281/j.cnki.jocml.2016.16.106
95. Zhou Y. To study the clinical efficacy of Yiqi Huoxue Tongbi Decoction in the treatment of diabetic peripheral neuropathy. For All Health. (2016) 10:129.
96. Ma Z. Study on the efficacy of Danggui Sini Decoction in the treatment of diabetic peripheral neuropathy. Med Inf. (2016) 29:112–13. doi: 10.3969/j.issn.1006-1959.2016.08.075
97. Zou P and Yang C. Discussion on the efficacy of Buyang Huanwu Decoction in the treatment of diabetic peripheral neuropathy. J Front Med. (2016) 6:354.
98. Mo S and Qiu X. The Observation on the Clinical Effect of Yangyin Jiedu Decoction in theTreatment of Diabetic Peripheral Neuropathy of Qi and Yin Deficiencywith Blood Stasis Type. World J Integrated Traditional Western Med. (2016) 11:692–95. doi: 10.13935/j.cnki.sjzx.160524
99. Huang P. Observation of the efficacy of Danggui Sini decoction in the treatment of diabetic peripheral neuropathy. Shenzhen J Integrated Traditional Chin Western Med. (2016) 25:53–4. doi: 10.16458/j.cnki.1007-0893.2015.23.028
100. Zhang D. Clinical observation of Yanghe Decoction and Buyang Huanwu Decoction in the treatment of diabetic peripheral neuropathy. J Chengde Med Univ. (2015) 32:220–21. doi: 10.15921/j.cnki.cyxb.2015.03.020
101. Xue L, Chen H, Yang Y, and Zhang Z. Clinical observation of 42 cases of diabetic peripheral neuropathy with Jiawei Liuteng Shuilu Shexian Decoction. J Sichuan Traditional Chin Med. (2015) 33:59–61.
102. Shi F. clinical Analysis of Huoxue Bushen Decoction in the Treatment of Diabetic Peripheral Neuropathy. Med Inf. (2015) 28:297–98. doi: 10.3969/j.issn.1006-1959.2015.35.449
103. Li S and Wang Y. Clinical study of compound Danshen dripping pills for the treatment of blood stasis diabetic peripheral neuropathy. China Foreign Med Treat. (2014) 151:137–38. doi: 10.16662/j.cnki.1674-0742.2014.24.006
104. Tang F. Curative etect observationot xiao Ke 5 prescription in the treatment of diabetic peripheral neuropathy with Qi Xu Xue Yu syndrome. Chin Community Doctors. (2014) 30:90–1.
105. Ye X, Qin B, Zhang W, and Zhang T. Electroacupuncture Kai Si Guan is used to treat diabetic peripheral neuropathy. Chin Med Modern Distance Educ China. (2014) 12:45–7. doi: 10.3969/j.issn.1672-2779.2014.02.030
106. Chen L. Analysis of the clinical efficacy of Buyang Huanwu Decoction in the treatment of diabetic peripheral neuropathy in 42 cases. Contemp Med. (2012) 18:153. doi: 10.3969/j.issn.1009-4393.2012.2.117
107. Ji X, Wang C, Zhang P, Zhang X, and Zhang Z. Effeet of Spleen-stomach Requlation-needling on Nerve Conduction Activity in Patients with Dia-betic Peripheral Neuropathy. Acupuncture Res. 35:443–47. doi: 10.13702/j.1000-0607.2010.06.009
108. Zhang C, Ma Y, and Yan Y. Clinical Effects of Acupuncture for Diabetic Peripheral Neuropathy. J Tradit Chin Med. 30:13–4.
109. Ma S. Clinical observation of 68 cases of acupuncture in the treatment of diabetic peripheral neuropathy. Contemp Med. (2010) 34:140–41. doi: 10.3969/j.issn.1009-4393.2010.34.106
110. Chen Y, Ma X, Hou W, Cen Y, Yu X, and Zhang L. Effects of penetrating acupuncture on peripheral nerve conduction velocity in patients with diabetic peripheral neuropathy: a randomized controlled trial. J Integr Med. (2009) 7:273–75.
111. Zhao H, Gao X, Gao Y, and Qu Y. Clinical Observation on Effeet of Acupuneture in Treating Diabetic Peripheral Neuropathy. Chin J Integrated Traditional Western Med. (2007) 27:312–14.
112. He X, Wang B, and Zhan G. Observation of clinical efficacy of acupuncture in the treatment of diabetic peripheral neuropathy. Chin J Rehabil Theory Pract. (2005) 11:396.
113. Xue L, Ji X, Yu S, and Zhang Z. Clinical observation of 34 cases of electroacupuncture in the treatment of diabetic peripheral neuropathy. J Tianjin Univ Traditional Chin Med. (2004) 23:152–53.
114. Jin J, Chen H, and Zhang Z. Clinical study of traditional Chinese medicine Tangmaitong tablets in the treatment of diabetic peripheral neuropathy. Henan Traditional Chin Med. (2003) 23:19–21. doi: 10.16367/j.issn.1003-5028.2003.12.013
115. Yang M, Lu B, and Shen L. Clinical observation of electroacupuncture in the treatment of diabetic peripheral neuropathy. Shaanxi J Traditional Chin Med. (2002) 23:261–62.
116. Pan J. Clinical observation of Huatan and Zhuyu treatment of diabetic peripheral neuropathy. Beijing J Traditional Chin Med. (2002) 21:161–62.
117. Li Y, Kang E, and Zheng H. Clinical study of the treatment of diabetic peripheral neuropathy by Guben Tongluo electroacupuncture. J Clin Acupuncture Moxibustion. (2000) 16:13–6.
118. Savelieff MG, Elafros MA, Viswanathan V, Jensen TS, Bennett DL, and Feldman EL. The global and regional burden of diabetic peripheral neuropathy. Nat Rev Neurol. (2025) 21:17–31. doi: 10.1038/s41582-024-01041-y
119. Xu L, Zang D, Li H, Sulitang A, Li Y, Ma J, et al. Five traditional Chinese medicine external treatment methods combined with mecobalamin for diabetic peripheral neuropathy: A network meta-analysis. Evidence-Based complementary Altern medicine: eCAM. (2022) 2022:4251022. doi: 10.1155/2022/4251022
120. Elafros MA, Andersen H, Bennett DL, Savelieff MG, Viswanathan V, Callaghan BC, et al. Towards prevention of diabetic peripheral neuropathy: clinical presentation, pathogenesis, and new treatments. Lancet Neurol. (2022) 21:922–36. doi: 10.1016/S1474-4422(22)00188-0
121. Zhang K, Peng P, Huang J, Chen M, Liu F, Zhu C, et al. Integrating plasma metabolomics and gut microbiome to reveal the mechanisms of Huangqi Guizhi Wuwu Decoction intervene diabetic peripheral neuropathy. J Ethnopharmacol. (2024) 319:117301. doi: 10.1016/j.jep.2023.117301
122. Wang Y, Chen Z, Ye R, He Y, Li Y, and Qiu X. Protective effect of Jiaweibugan decoction against diabetic peripheral neuropathy. Neural Regen Res. (2013) 8:1113–21. doi: 10.3969/j.issn.1673-5374.2013.12.006
123. Hu Y, Chen C, Liang Z, Liu T, Hu X, Wang G, et al. Compound Qiying Granules alleviates diabetic peripheral neuropathy by inhibiting endoplasmic reticulum stress and apoptosis. Mol Med (Cambridge Mass.). (2023) 29:98. doi: 10.1186/S10020-023-00698-3
124. Ben Y, Hao J, Zhang Z, Xiong Y, Zhang C, Chang Y, et al. Astragaloside IV inhibits mitochondrial-dependent apoptosis of the dorsal root ganglion in diabetic peripheral neuropathy rats through modulation of the SIRT1/p53 signaling pathway. Diabetes Metab syndrome obesity: Targets Ther. (2021) 14:1647–61. doi: 10.2147/DMSO.S301068
125. Hussain Z, Thu HE, Amjad MW, Hussain F, Ahmed TA, and Khan S. Exploring recent developments to improve antioxidant, anti-inflammatory and antimicrobial efficacy of curcumin: A review of new trends and future perspectives. Materials Sci engineering C Materials Biol Appl. (2017) 77:1316–26. doi: 10.1016/j.msec.2017.03.226
126. Kumar A and Sharma SS. NF-kappaB inhibitory action of resveratrol: a probable mechanism of neuroprotection in experimental diabetic neuropathy. Biochem Biophys Res Commun. (2010) 394:360–5. doi: 10.1016/j.bbrc.2010.03.014
127. Cho E and Kim W. Effect of acupuncture on diabetic neuropathy: A narrative review. Int J Mol Sci. (2021) 22:9. doi: 10.3390/ijms22168575
128. Manni L, Florenzano F, and Aloe L. Electroacupuncture counteracts the development of thermal hyperalgesia and the alteration of nerve growth factor and sensory neuromodulators induced by streptozotocin in adult rats. Diabetologia. (2011) 54:1900–8. doi: 10.1007/s00125-011-2117-5
129. Yin Y, Wang L, Zhao L, Lin L, and Shen X. Effect of 10.6 mum laser moxibustion on inflammation in diabetic peripheral neuropathy rats. Front Endocrinol. (2023) 14:1203677. doi: 10.3389/fendo.2023.1203677
130. Yu X, Chen X, Liu W, Jiang M, Wang Z, and Tao J. Proteomics analysis of the spinal dorsal horn in diabetic painful neuropathy rats with electroacupuncture treatment. Front Endocrinol. (2021) 12:608183. doi: 10.3389/fendo.2021.608183
131. Chen YK, Liu TT, Teia F, and Xie MZ. Exploring the underlying mechanisms of obesity and diabetes and the potential of Traditional Chinese Medicine: an overview of the literature. Front Endocrinol. (2023) 14:1218880. doi: 10.3389/fendo.2023.1218880
132. Tian J, Jin D, Bao Q, Ding Q, Zhang H, Gao Z, et al. Evidence and potential mechanisms of traditional Chinese medicine for the treatment of type 2 diabetes: A systematic review and meta-analysis. Diabetes Obes Metab. (2019) 21:1801–16. doi: 10.1111/dom.13760
133. Ferris JK, Inglis JT, Madden KM, and Boyd LA. Brain and body: A review of central nervous system contributions to movement impairments in diabetes. Diabetes. (2020) 69:3–11. doi: 10.2337/db19-0321
134. Selvarajah D, Wilkinson ID, Maxwell M, Davies J, Sankar A, Boland E, et al. Magnetic resonance neuroimaging study of brain structural differences in diabetic peripheral neuropathy. Diabetes Care. (2014) 37:1681–8. doi: 10.2337/dc13-2610
135. Yang F, Qu M, Zhang Y, Zhao L, Xing W, Zhou G, et al. Aberrant brain network integration and segregation in diabetic peripheral neuropathy revealed by structural connectomics. Front Neurosci. (2020) 14:585588. doi: 10.3389/fnins.2020.585588
136. Li SS, Hua XY, Zheng MX, Wu JJ, Ma ZZ, Xing XX, et al. Electroacupuncture treatment improves motor function and neurological outcomes after cerebral ischemia/reperfusion injury. Neural Regen Res. (2022) 17:1545–55. doi: 10.4103/1673-5374.330617
137. Peng J, Su J, Song L, Lv Q, Gao Y, Chang J, et al. Altered functional activity and functional connectivity of seed regions based on ALFF following acupuncture treatment in patients with stroke sequelae with unilateral limb numbness. Neuropsychiatr Dis Treat. (2023) 19:233–45. doi: 10.2147/NDT.S391616
Keywords: traditional Chinese medicine, TCM, diabetic peripheral neuropathy, network meta-analysis, meta-analysis
Citation: Hu J, Wang H, Hao X, Pan T, Li X, Zhou X, Wang S, Gong Y, Wu L, Dong S, Chen X and Wang X (2025) Traditional Chinese medicine for diabetic peripheral neuropathy: a network meta-analysis. Front. Endocrinol. 16:1596924. doi: 10.3389/fendo.2025.1596924
Received: 20 March 2025; Accepted: 28 July 2025;
Published: 27 August 2025.
Edited by:
Ahsan H. Khandoker, Khalifa University, United Arab EmiratesReviewed by:
Siying Weng, Ningbo Municipal Hospital of TCM, ChinaXiaofei Yang, Beijing University of Chinese Medicine, China
Copyright © 2025 Hu, Wang, Hao, Pan, Li, Zhou, Wang, Gong, Wu, Dong, Chen and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xinhua Chen, MTg3MDk4MTkwQHFxLmNvbQ==; Xichen Wang, d2FuZ3hjQGNjdWNtLmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
 Jinglin Hu
Jinglin Hu Haili Wang
Haili Wang Xiaogang Hao2
Xiaogang Hao2 Xuefeng Li
Xuefeng Li Xue Zhou
Xue Zhou Yubo Gong
Yubo Gong Shuo Dong
Shuo Dong Xinhua Chen
Xinhua Chen