- 1Department of General Surgery, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 2Department of Molecular Diagnostics & Endocrinology, The Core Laboratory in Medical Center of Clinical Research, State Key Laboratory of Medical Genomics, Shanghai Ninth People’s Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, Shanghai, China
Objective: Thermal ablation is an effective treatment for thyroid nodules; however, the range of complications associated with thermal ablation is unclear. In this study, we analyzed the complications of thyroid nodule thermal ablation in our hospital in combination with data from different countries for further analysis to determine the complications.
Methods: 536 patients treated by thermal ablation at Shanghai Ninth People’s Hospital from Jan 2021 to Dec 2023 were enrolled in this retrospective study. The types and numbers of complications were recorded. Studies reporting complications of thermal ablation for thyroid nodules were identified in the PubMed database from Jan 2004 to Mar 2024. The incidence rate and types of complications were analyzed. Finally, we compared our data with those studies.
Results: Twelve types of complications associated with thermal ablation occurred to patients in our hospital. The overall incidence was 10.82%. The top five complications were pain, edema, voice changes, hematoma, and vascular reactions. In addition, 21 kinds of complications were reported across 13 countries, and the average incidence rate was 12.61%. The top five complications were pain, vocal changes, edema, hematoma, and fever. The total incidence rate did not significantly differ between our hospital and other countries (P ≥ 0.05), though the incidences of specific complications, including tracheal injury, vasovagal reaction, dyspnea, scarring, infection and fever, were significantly different (P < 0.05).
Conclusions: The incidence of complications associated with thermal ablation of thyroid nodules is similar across countries. However, the proportions and types of complications vary regionally.
1 Introduction
The thermal ablation (TA) procedure, proposed as a minimally invasive treatment method, has received increasing attention in recent years (1–4). TA methods include radiofrequency ablation (RFA), microwave ablation (MWA), laser ablation (LA), and high-frequency focused ultrasound (HIFU) (5). The principle of these methods involves the induction of tissue coagulation necrosis under extreme hyperthermic conditions (6). TA is a suitable treatment for benign thyroid nodules with ≥ 10% solid components (7). Compared with surgery, the advantages of thyroid TA include safety, efficacy, low cost, good tolerability and preservation of thyroid function (8, 9). The 2022 international multidisciplinary consensus explicitly stated that TA can be considered for symptomatic thyroid nodules (6). Furthermore, multiple other global follow-up studies have confirmed the effectiveness of TA for benign nodules and papillary thyroid microcarcinoma (PTMC) (10–14); however, the status of complications of TA is unclear. In this study, data regarding the complications of thyroid TA at our hospital were combined with those in different countries to analyze the range of complications associated with thyroid TA.
2 Materials and methods
The study was approved by the Ethics Committee of Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine (SH9H-2021-MT6-1) and informed consent for each procedure was obtained from all patients prior to the procedure.
2.1 Study population
A total of 536 patients who underwent thyroid MWA at our hospital (SHNH) from Jan 2021 to Dec 2023 were retrospectively enrolled in this study. All of the patients underwent ultrasound (US) prior to TA to record the tumor number, location, and volume, and fine-needle aspiration (FNA) was performed before TA to confirm the pathology. The clinical characteristics, volume of tumor change before and after TA, and complications associated with TA were recorded. The inclusion criteria included patients who were clearly diagnosed with symptomatic benign thyroid nodules (Bethesda II or III, diameter ≥ 25 mm) or low-risk PTMCs (diameter ≤ 10 mm) by FNA and who were treated with MWA. Complications were recorded immediately, at 3 months and at 6 months after MWA. The exclusion criteria were as follows: (1) Patients who had other types of thyroid cancer; (2) Patients who were confirmed to have central lymph node metastasis or lateral lymph node metastasis before the operation; (3) Patients who had a history of thyroid operations. Informed consent was obtained from all patients in this study. This retrospective study was approved by the institutional review board.
2.2 Surgical procedures
All patients underwent ultrasound to confirm the size and location of their thyroid nodules prior to TA. The patients lay flat on their back with a soft pillow under their shoulders and with their neck tilted backward. After disinfection, 1% lidocaine was used for local anesthesia and fluid isolation. Moving TA was used for large benign thyroid nodules, and fixing TA was used for PTMCs via 30 W MWA (Great Wall MTI-5A, China; XR-1610, China).
2.3 Literature search
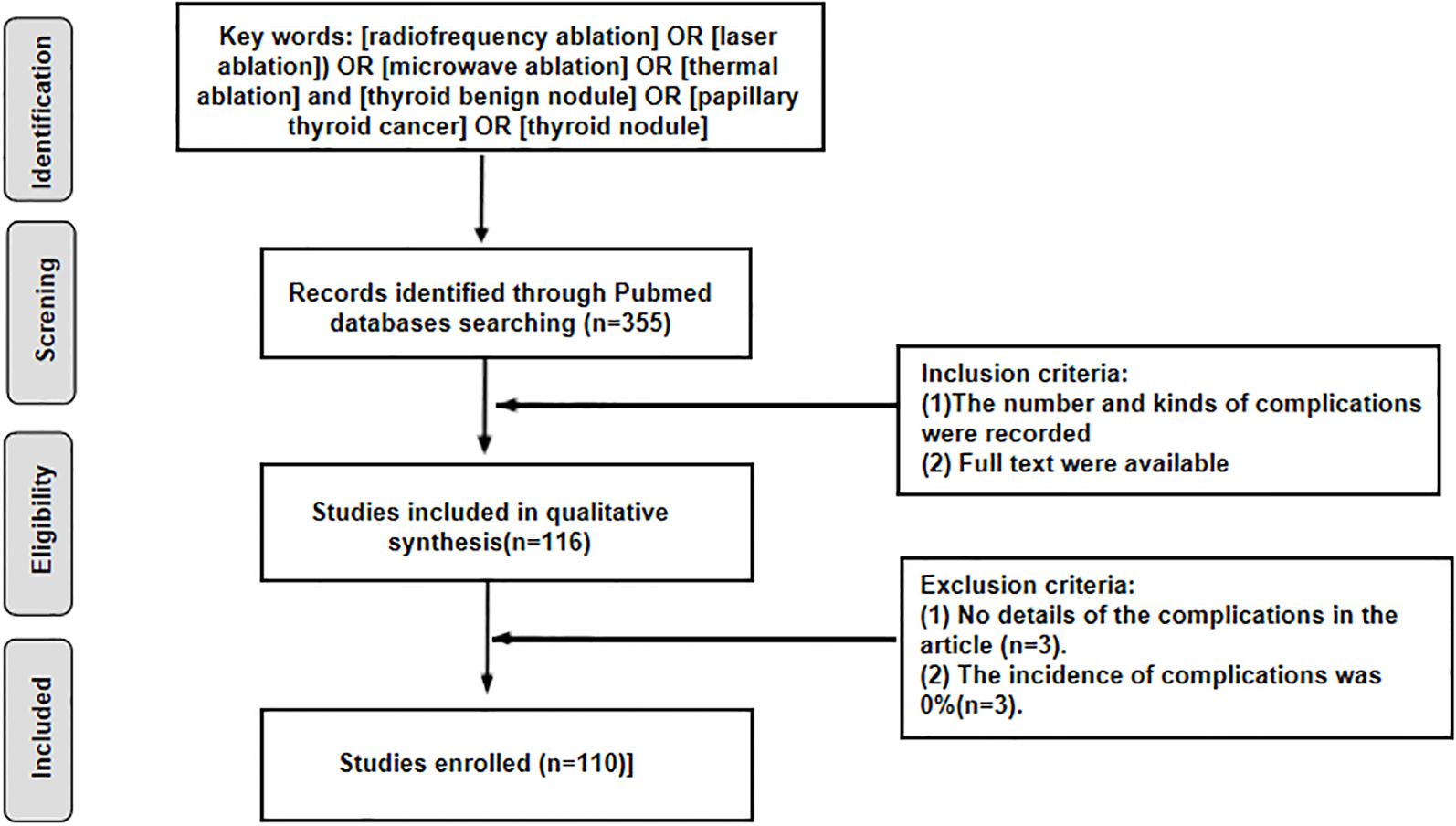
The PubMed database was searched for original literature regarding complications of thyroid TA from 2014–2024. Research reported in English was included in this study. The flowchart for article filtering is shown in Figure 1. The inclusion criteria were as follows: (1) patients with benign thyroid nodules or PTMCs ≤1 cm who underwent RFA, MWA, LA or HFU. (2) The incidence and types of complications of thyroid TA were reported. The exclusion criteria were as follows: (1) The details of the complications were not reported in the publication. (2) The incidence rate of TA was 0%. The included studies were classified and analyzed according to the country of origin.
2.4 Statistical analysis
In this study, continuous variables are presented as the means ± standard deviations (SDs). Categorical data are presented as numbers (%). Comparisons between the complication rates at SHNH and those in the reported studies were performed via the chi-square test. P < 0.05 was considered to indicate statistical significance. All the statistical analyses were conducted via R (version 4.3.1).
3 Results
3.1 Data analysis in SHNH
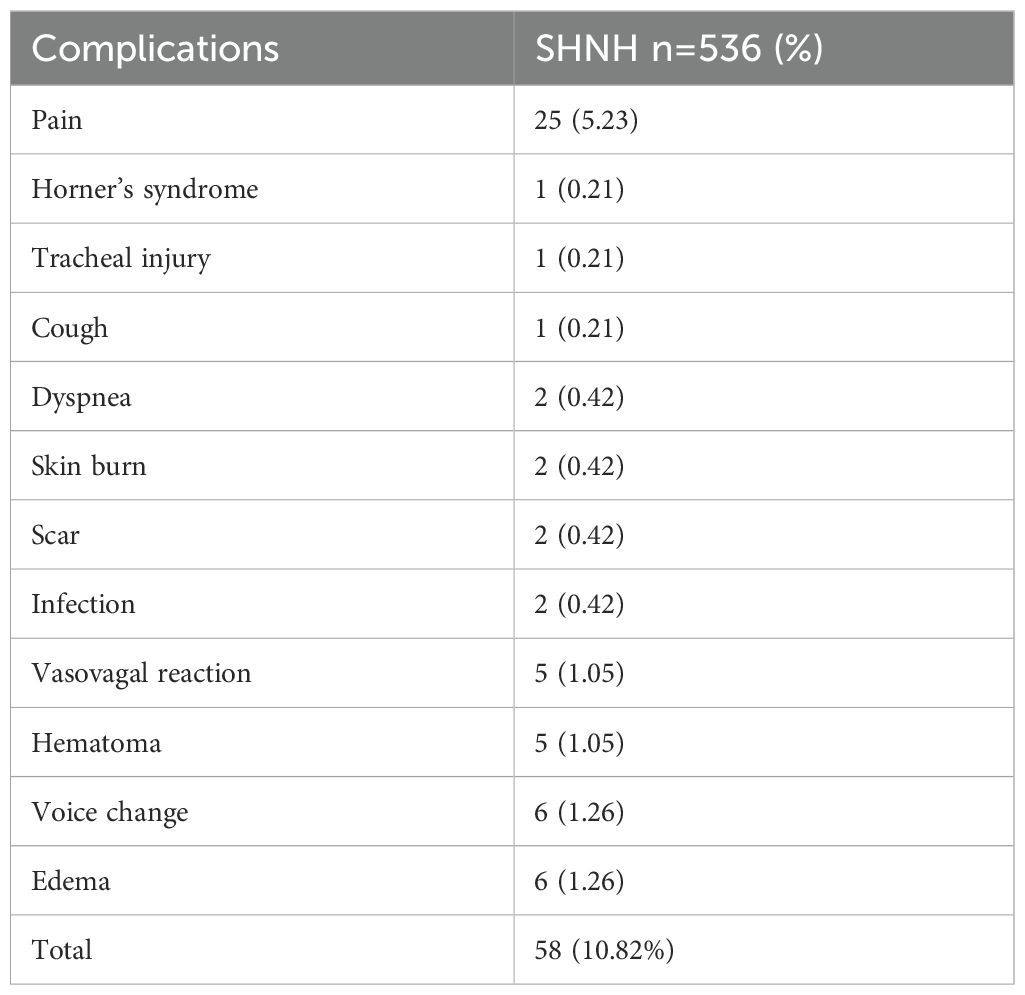
A total of 536 patients were included in this study, which included 418 females (78.0%) and 118 males (22.0%). The patients ranged in age from 16 to 81 years (48.49 ± 14.85 years). The numbers of thyroid nodules on the left side, right side and isthmus were 250 (46.6%), 275 (51.3%) and 11 (2.1%), respectively. The average volume of thyroid nodules before TA and 3 months after TA ranged from 17281.85 ± 25960.74 mm³ to 5531.97 ± 16482.36 mm³ (P < 0.05). There were 431 benign thyroid nodules and 105 PTMCs. A total of 78 patients with PTMC were less than 55 years old, and 27 patients with PTMC were 55 years old or older. A total of 12 complications were recorded, and the incidence of TA was 10.82%. The top five complications were pain (5.25%), edema (1.26%), voice changes (1.26%), hematoma (1.05%), and vascular reactions (1.05%) (Table 1). Only one patient experienced Horner’s syndrome, tracheal injury or cough (Table 1).
3.2 Related literature
A total of 110 studies involving a total of 14,668 patients from 13 countries were identified in the literature search. Sixty-nine studies employed RFA, 26 studies employed MWA, 17 studies employed LA, 5 studies employed HIFU, and three studies did not report the treatment methods. There was only one study each from Bulgaria and Singapore.
The five countries with the greatest number of patients with TA were China (5481), South Korea (3182), Italy (3029), the United States (1261) and Vietnam (341). The lowest number of cases were reported in the Netherlands (124), Bulgaria (20) and Singapore (10). The countries with the highest number of complications of TA were China (626, 11.42%), South Korea (260, 8.17%), Italy (515, 17.00%), the United States (94, 7.45%) and Vietnam (25, 7.33%) (Figure 2).
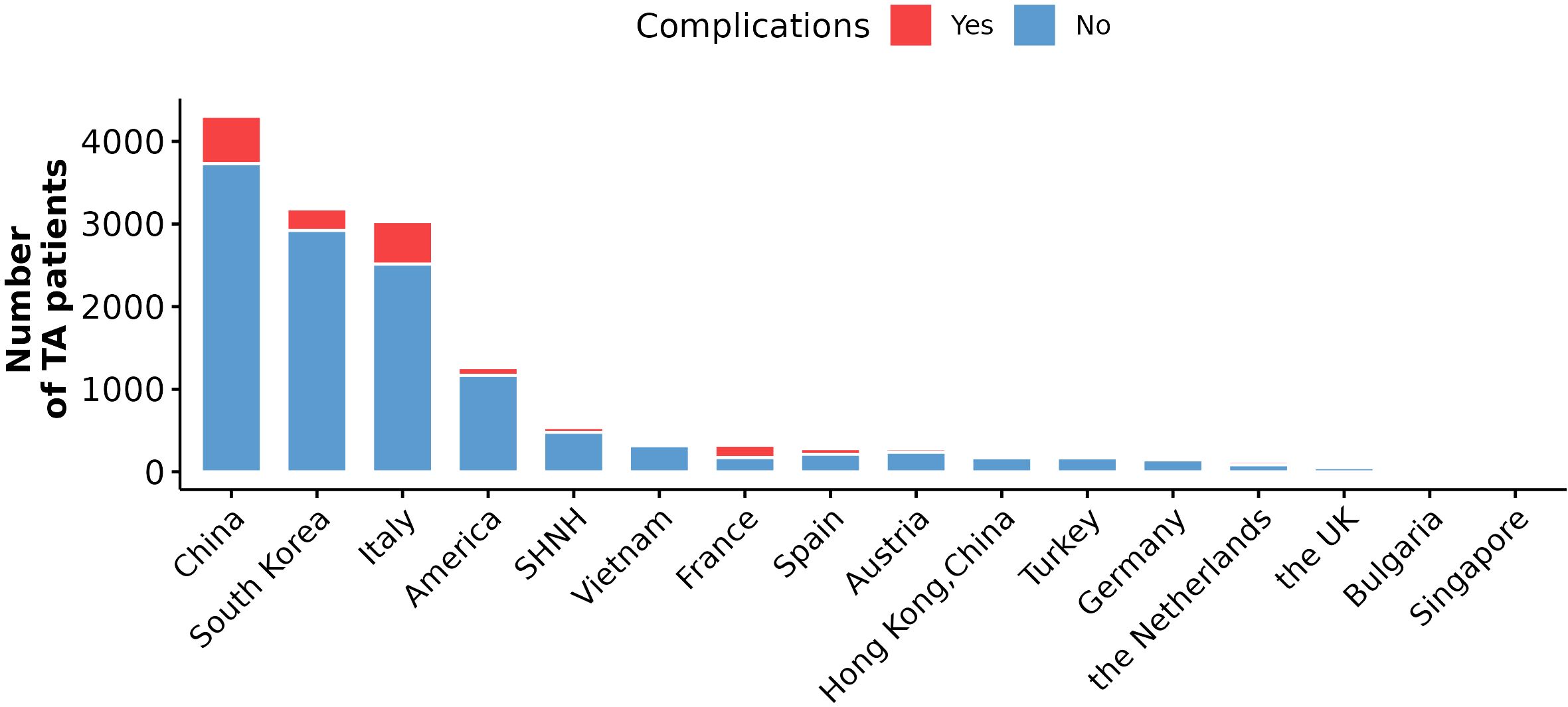
Figure 2. The number of TA patients and complications in different countries. Red bar indicates the number of TA patients with complications, and blue indicates the number of TA patients without any complications included in this study.
A total of 21 complications were reported. The top five complications were pain (861), voice changes (236), edema (192), hematoma (174), and fever (169). Pain was the most common complication, and the number of pain cases was more than three times greater than the number of voice changes and four to ten times greater than the number of other complications. Other complications included vasovagal reactions, postoperative hypothyroidism, nodule rupture, skin burn, nausea and vomiting, cough, postoperative hyperthyroidism, dysphagia, infection, Horner’s syndrome, other nerve injury, scarring, dyspnea, tracheal injury, and esophageal injury. Tracheal injury and esophageal injury were rare complications, with only one case reported (Figure 3).
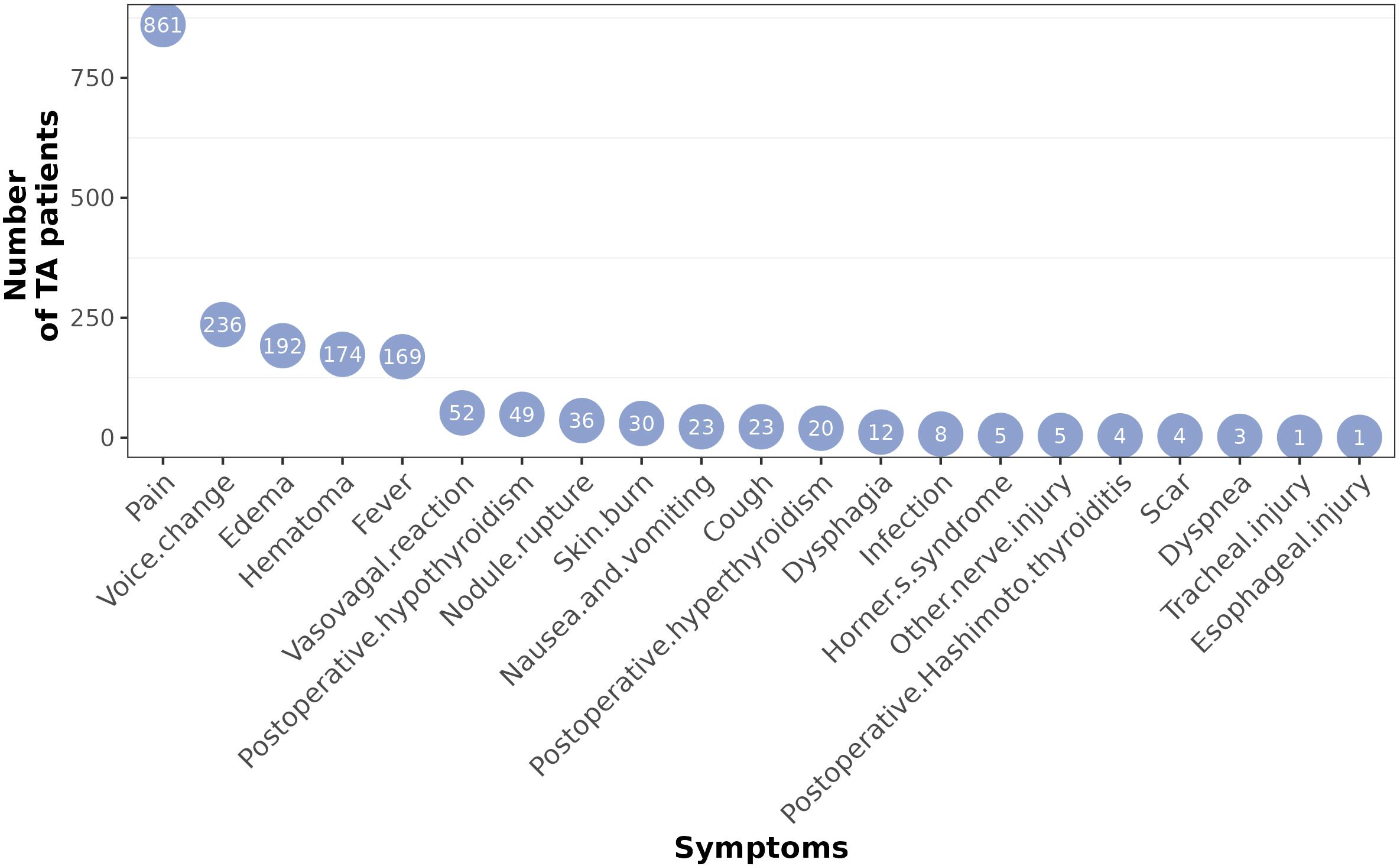
Figure 3. Number of different complications after thyroid TA. All countries were summarized together.
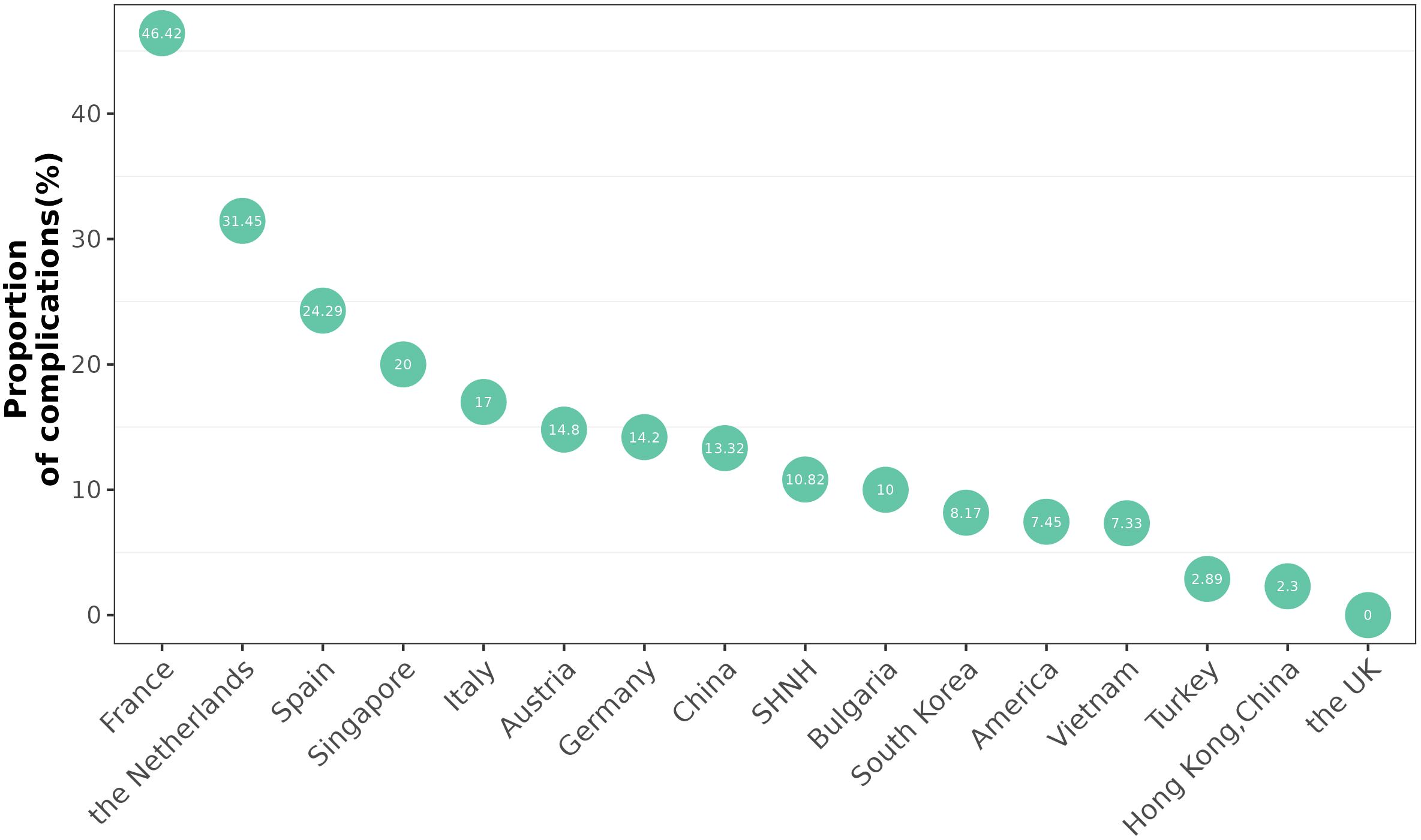
The five countries with the highest incidence of complications were France (46.62%), the Netherlands (31.45%), Spain (24.29%), Singapore (20%) and Italy (17%). The incidence of complications was lowest in Turkey (2.89%). The incidence of complications in China was 11.42% (Figure 4).
The proportions of various complications in different countries are shown in Figure 5. Voice change and postoperative hypothyroidism were the most common complications in the United States, and hematoma and dyspnea were the most common complications in Australia. Pain and fever were the most common complications in Italy. The composition of complications was similar in China and Korea (Figure 5).
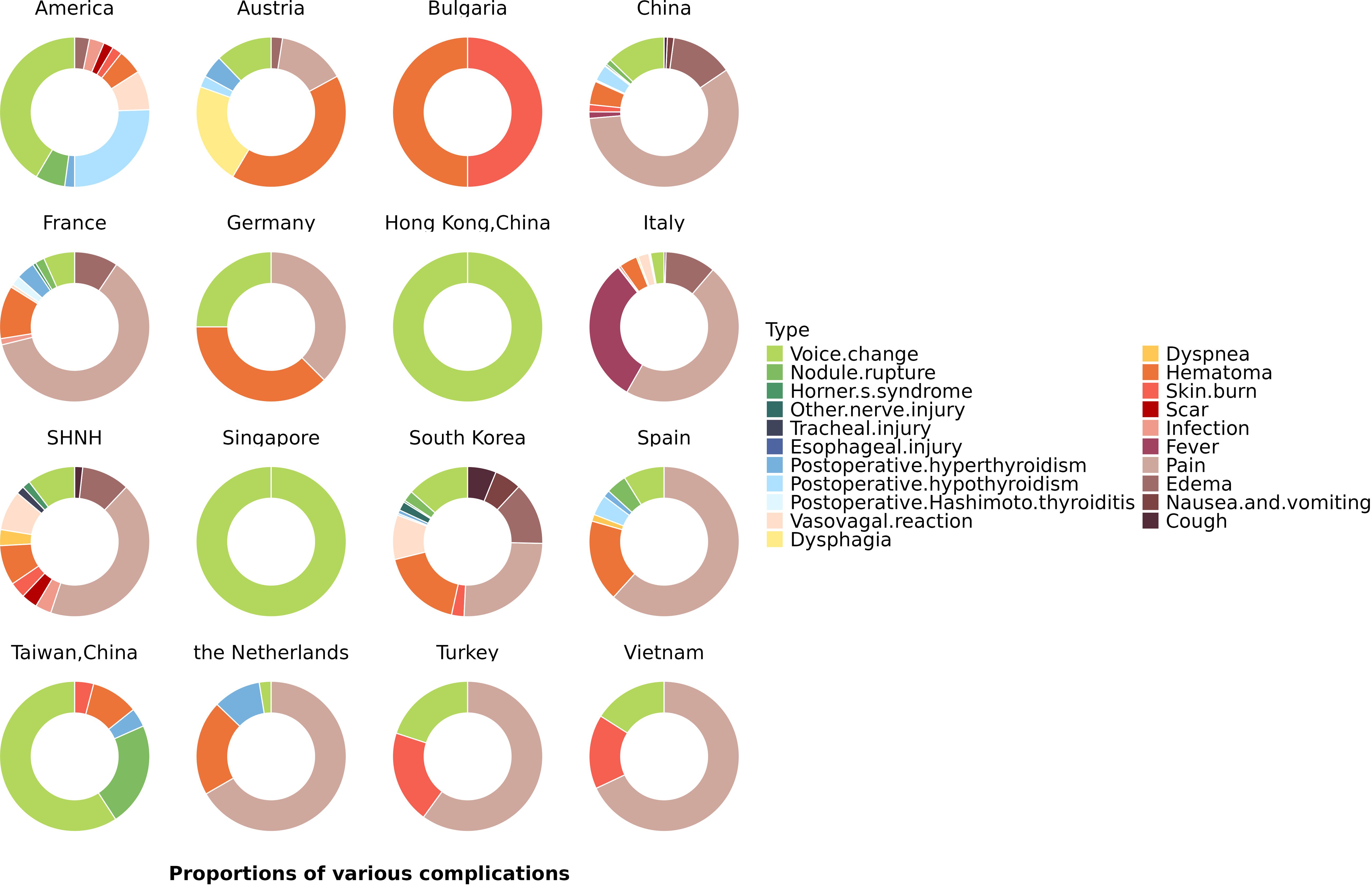
Figure 5. Different proportions of various complications in different countries. Pie charts showing the proportions of complications in each country.
There was no significant difference in the incidence of TA complications between SHNH (10.82%) and institutions in China (11.42%), though the incidences of vasovagal reactions (1.05%), dyspnea (0.42%), scarring (0.42%) and infection (0.42%) significantly differed between the two locations (P < 0.05). When the complications of thyroid TA in patients treated at SHNH and those treated in different countries were compared, the incidences of tracheal injury, vasovagal reactions, dyspnea, scarring, infection and fever were significantly different between SHNH patients and those in different countries (P < 0.05). However, there was no significant difference in the total incidence of complications at SHNH and in different countries (Table 2).
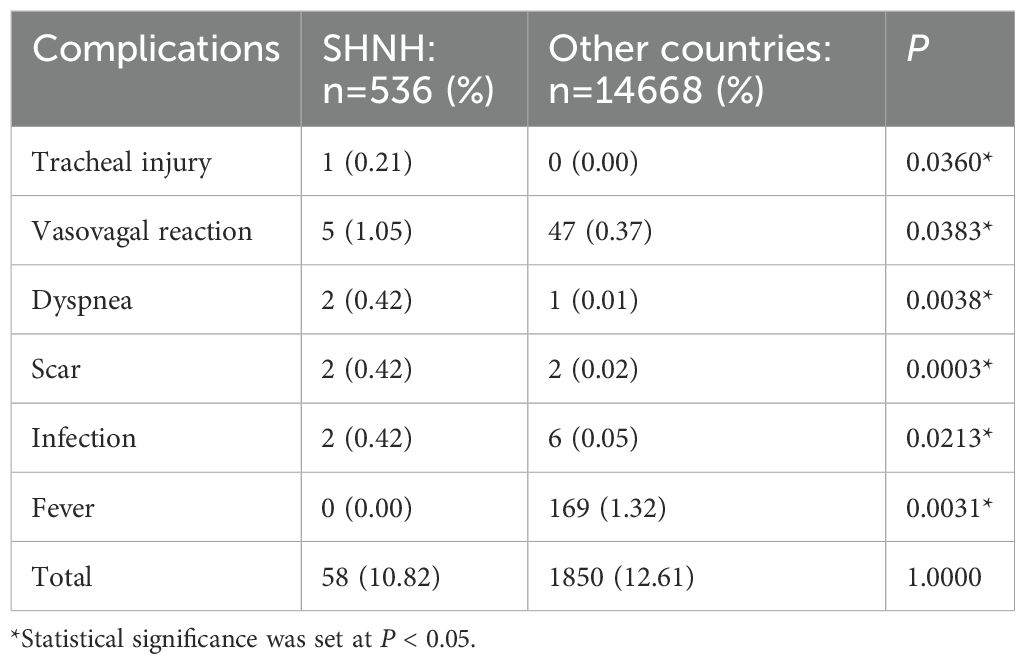
Table 2. Comparison of complication morbidity between SHNH patients and those in different countries.
4 Discussion
TA is widely used, though the indications for TA remain unclear. The existing guidelines are mostly for RFA and can be used for the treatment of benign thyroid nodules, PTMCs, and recurrent thyroid cancers (RTCs). Thermal ablation of thyroid cancer is only indicated for single low-risk PTMCs, the low degree of invasiveness should be verified prior to ablation. For patients with RTC, curative-intent RFA should be considered when complete removal of the tumor is possible in patients with RTC and a limited number (≤ 3) of small tumors (size ≤ 2 cm). RFA can be performed with curative or palliative intent for RTCs at the thyroidectomy bed, neck dissection site, or metastatic cervical lymph nodes for patients who refuse surgery or are at high surgical risk (15, 16).
Some studies have reported the use of RFA for other types of PTC, including PTC larger than 1 cm, and palliative treatment for recurrent and metastatic PTC. The results are encouraging and provide a safe and effective treatment option for patients with PTC who cannot undergo or refuse surgery. However, further research is needed (17).
The management of indeterminate nodules with TA is not recommended as it is difficult to achieve diagnostic needs and TA cannot prevent metastasis. In the 2023 Bethesda System for Reporting Thyroid Cytopathology, Bethesda category III is simplified as atypia of undetermined significance (AUS), which is subdivided into “AUS nuclear” and “AUS other” (18). AUSs with nuclear atypia have significantly greater ROMs and require more cautious clinical management, corresponding to research results since the publication of the second edition of the classification (19–21).
In the current study, all patients who received TA treatment at SHNH underwent biopsy to confirm the pathological diagnosis of benign nodule or PTMC, with no history of lymph node metastasis or previous thyroid surgery. TA was used as a minimally invasive initial treatment to alleviate patient pain, reduce costs, and improve safety and aesthetics. However, the probability of serious postoperative complications, such as tracheal injury, remains. Therefore, the indications for TA must be further clarified. Moreover, considering that the probability of serious complications still occurs, strict inclusion criteria for TAs are very important.
There are several reports and reviews involving TA complications. The 2022 international multidisciplinary consensus concluded that the two most common postoperative complications are recurrent laryngeal nerve injury and thyroid nodule rupture (6). These two situations can be separately treated by injection of a cold irrigant into the region of suspected thermal injury (22) and by conservative management (23). A meta-analysis of the incidence of common complications was conducted (24) and reported values of 1.0%-2.0%, 0.2%-0.5%, 1.0%-100%, 0.0%-17.0%, and 0.27%-3.7% for nerve injury, nodule rupture, pain, hematoma, and skin burns, respectively. However, comparisons across countries are lacking. In the present study, we compared the complications of thyroid TA across different countries with our own data for further statistical analysis. We found that TAs have been widely applied in China (25, 26), South Korea (27, 28) and Italy (29, 30). Common complications include pain, vocal changes, edema, hematoma, fever, etc. (31–33). Uncommon complications are tracheal injury and esophageal injury. Fu Q reported in 2021 that esophageal injury, which was located in the esophageal serosa, was caused by insufficient observation during the procedure. The patient experienced foreign body sensations while swallowing after ablation and recovered one month after the ablation procedure (34). Two case reports were analysed in the previously published literature. Patients experienced intense pain and difficulty breathing one to two weeks after the ablation procedure; possible contributing factors were an excessive thyroid nodule volume, a prolonged ablation time, and deep sedation anesthesia (35, 36). We also reported a case of airway fistula after MWA. The patient developed neck pain, fever, cough and increased sputum after surgery. CT revealed small air bubbles on the right side of the airway with inflammation of the neck tissue. The patient’s symptoms disappeared one month after anti-infective treatment.
Our study is the first to compare complications regionally. This retrospective study revealed that the region with the highest incidence rate of complications after ablation was Europe, including France (14, 37, 38) and the Netherlands (32, 39). France has the highest incidence rate of complications (46.42%). A total of 321 patients were included in three studies conducted in France; the incidence rates of TA complications were 15.6% (14), 6.2% (37) and 78.9% (38). The incidence in the Netherlands ranks second (21.45%). There are two reasons for the high incidence rates of TA complications in France and the Netherlands. One reason is that the number of thyroid TA procedures in these two countries was limited (France reported 321 cases, and the Netherlands reported 124 cases), and the proficiency of the operator was thus affected. The other reason is that most of the complications reported in France and the Netherlands involved pain, and this factor increased the proportion of complications. For example, Ben Hamou reported that 92 out of 166 patients experienced pain, leading to an incidence of up to 78.9% (39). In some countries, pain was not included in the reported complications.
In addition, we compared the complication data of various countries in the previous literature with those of our single centre, SHNH. There are significant differences in the incidence of certain single complications, but there is no significant difference in the incidence of overall complications.
This study has several limitations. The determination of some complications is subjective, which affects the results involving pain. In addition, the follow-up time of previous studies varied from six months to five years, and most of them were retrospective studies. Furthermore, there are very few cases reported in some countries, such as Singapore and Bulgaria. Further attention and research are needed in this area.
5 Conclusion
The incidence rate of complications associated with thyroid TA is approximately 10% to 15%. However, the proportions and types of complications vary reionally.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine (SH9H-2021-MT6-1). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
SW: Data curation, Writing – original draft, Writing – review & editing. YC: Data curation, Writing – review & editing. CZ: Conceptualization, Methodology, Writing – review & editing. XL: Data curation, Software, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2025.1608164/full#supplementary-material
References
1. Hahn SY, Shin JH, Na DG, Ha EJ, Ahn HS, Lim HK, et al. Ethanol ablation of the thyroid nodules: 2018 consensus statement by the Korean Society of Thyroid Radiology. Korean J Radiol. (2019) 20:609–20. doi: 10.3348/kjr.2018.0696
2. Papini E, Monpeyssen H, Frasoldati A, and Hegedüs L. 2020 European Thyroid Association clinical practice guideline for the use of image-guided ablation in benign thyroid nodules. Eur Thyroid J. (2020) 9:172–85. doi: 10.1159/000508484
3. Papini E, Pacella CM, Solbiati LA, Achille G, Barbaro D, Bernardi S, et al. Minimally-invasive treatments for benign thyroid nodules: a Delphi-based consensus statement from the Italian minimally-invasive treatments of the thyroid (MITT) group. Int J Hyperthermia. (2019) 36:375–81. doi: 10.1080/02656736.2019.1575482
4. Hossein Gharib MD, Enrico Papini MD, Garber JR, Duick DS, Harrell RM, Hegedüs L, et al. American association of clinical endocrinologists, American College of endocrinology, and associazione medici endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules-2016 update executive summary of recommendations. Endocrine Pract. (2016) 22:622. doi: 10.4158/EP161208.GL
5. Luster M, Aktolun C, Amendoeira I, Barczyński M, Bible KC, Duntas LH, et al. European perspective on 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: proceedings of an interactive international symposium. Thyroid. (2019) 29:7–26. doi: 10.1089/thy.2017.0129
6. Orloff LA, Noel JE, Stack BC Jr., Russell MD, Angelos P, Baek JH, et al. Radiofrequency ablation and related ultrasound-guided ablation technologies for treatment of benign and Malignant thyroid disease: An international multidisciplinary consensus statement of the American Head and Neck Society Endocrine Surgery Section with the Asia Pacific Society of Thyroid Surgery, Associazione Medici Endocrinologi, British Association of Endocrine and Thyroid Surgeons, European Thyroid Association, Italian Society of Endocrine Surgery Units, Korean Society of Thyroid Radiology, Latin American Thyroid Society, and Thyroid Nodules Therapies Association . Head Neck. (2022) 44:633–60. doi: 10.1002/hed.26960
7. Yang C, Hsu Y, and Liou JY. Efficacy of ethanol ablation for benign thyroid cysts and predominantly cystic nodules: a systematic review and meta-analysis. Endocrinol Metab. (2021) 36:81. doi: 10.3803/enm.2020.833
8. Bernardi S, Dobrinja C, Fabris B, Bazzocchi G, Sabato N, Ulcigrai V, et al. Radiofrequency ablation compared to surgery for the treatment of benign thyroid nodules. Int J Endocrinol. (2014) 2014:934595. doi: 10.1155/2014/934595
9. Che Y, Jin S, Shi C, Wang L, Zhang X, Li Y, et al. Treatment of benign thyroid nodules: comparison of surgery with radiofrequency ablation. Am J Neuroradiology. (2015) 36:1321–5. doi: 10.3174/ajnr.a4276
10. Russell JO, Desai D, Noel JE, Hussein M, Toraih E, Seo S, et al. Radiofrequency ablation of benign thyroid nodules: A prospective, multi-institutional North American experience. Surgery. (2024) 175:139–45. doi: 10.1016/j.surg.2023.07.046
11. Lin Y, Wu Z, Shi Y, Ding M, Tang XY, He Y, et al. Radiofrequency ablation of unifocal papillary thyroid microcarcinoma with BRAF V600E mutation. J Clin Endocrinol Metab. (2023) 108:1298–305. doi: 10.1210/clinem/dgad269
12. Lee MK and Lee SW. Analysis of 5 years' experience of a head and neck surgeon with radiofrequency ablation for benign thyroid nodule. Am J Otolaryngol. (2023) 44:103715. doi: 10.1016/j.amjoto.2022.103715
13. Mauri G, Papini E, Bernardi S, Barbaro D, Cesareo R, De Feo P, et al. Image-guided thermal ablation in autonomously functioning thyroid nodules. A retrospective multicenter three-year follow-up study from the Italian Minimally Invasive Treatment of the Thyroid (MITT) Group. Eur Radiol. (2022) 32(3):1738–46. doi: 10.1007/s00330-021-08289-8
14. Russ G, Ben Hamou A, Poirée S, Ghander C, Ménégaux F, Leenhardt L, et al. Learning curve for radiofrequency ablation of benign thyroid nodules. Int J Hyperthermia. (2021) 38:55–64. doi: 10.1080/02656736.2021.1871974
15. Mauri G, Hegedüs L, Bandula S, Cazzato RL, Czarniecka A, Dudeck O, et al. European thyroid association and cardiovascular and interventional radiological society of Europe 2021 clinical practice guideline for the use of minimally invasive treatments in Malignant thyroid lesions. Eur Thyroid J. (2021) 10:185–97. doi: 10.1159/000516469
16. Ha EJ, Lee MK, Baek JH, Lim HK, Ahn HS, Baek SM, et al. Radiofrequency ablation for recurrent thyroid cancers: 2025 Korean society of thyroid radiology guideline. Korean J Radiol. (2025) 26:10–28. doi: 10.3348/kjr.2024.0963
17. Zhao GZ and Zhang MB. Ultrasound-guided radiofrequency ablation for the treatment of papillary thyroid carcinoma: a review of the current state and future perspectives. Ultrasonography. (2024) 43:79–87. doi: 10.14366/usg.23091
18. Ali SZ, Baloch ZW, Cochand-Priollet B, Schmitt FC, Vielh P, and VanderLaan PA. The 2023 Bethesda system for reporting thyroid cytopathology. Thyroid. (2023) 33:1039–44. doi: 10.1089/thy.2023.0141
19. Sengul I and Sengul D. Blurred lines for management of thyroid nodules in the era of atypia of undetermined significance/ follicular lesion of undetermined significance: novel subdivisions of categories IIIA and IIIB in a possible forthcoming The Bethesda System for Reporting Thyroid Cytopathology, 3rd edition; amending versus unnecessary? Rev Assoc Med Bras (1992). (2021) 67:1385–6. doi: 10.1590/1806-9282.20210763
20. Sengul I and Sengul D. Focusing on thyroid nodules in suspense: 10–15 mm with repeat cytology, Category III, the Bethesda System for Reporting Thyroid Cytopathology, TBSRTC. Rev da Associacao Med Bras (1992). (2021) 67:166–7. doi: 10.1590/1806-9282.67.02.20200828
21. Sengul I and Sengul D. Comment on: "Evaluating treatment options in managing thyroid nodules with indeterminate cytology of TBSRTC in thyroidology: addendum aut non? Rev da Associacao Med Bras (1992). (2022) 68:973–4. doi: 10.1590/1806-9282.20220383
22. Chung SR, Baek JH, Choi YJ, and Lee JH. Management strategy for nerve damage during radiofrequency ablation of thyroid nodules. Int J Hyperthermia. (2019) 36:203–9. doi: 10.1080/02656736.2018.1554826
23. Chung SR, Suh CH, Baek JH, Park HS, Choi YJ, and Lee JH. Safety of radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: a systematic review and meta-analysis. Int J hyperthermia. (2017) 33:920–30. doi: 10.1080/02656736.2017.1337936
24. Lim JY and Kuo JH. Thyroid nodule radiofrequency ablation: complications and clinical follow up. Techniques Vasc interventional Radiol. (2022) 25:100824. doi: 10.1016/j.tvir.2022.100824
25. Cai W, Liu S, Yu X, Han Z, Cheng Z, Liu F, et al. Is partial ablation appropriate for benign thyroid nodules? A retrospective study with long-term follow-up after microwave ablation. Int J Hyperthermia. (2021) 38:923–30. doi: 10.1080/02656736.2021.1936217
26. Wu R, Luo Y, Tang J, Yang M, Li J, Zhang Y, et al. Ultrasound-guided radiofrequency ablation for papillary thyroid microcarcinoma: a retrospective analysis of 198 patients. Int J Hyperthermia. (2020) 37:168–74. doi: 10.1080/02656736.2019.1708480
27. Baek JH, Lee JH, Sung JY, Bae JI, Kim KT, Sim J, et al. Complications encountered in the treatment of benign thyroid nodules with US-guided radiofrequency ablation: a multicenter study. Radiology. (2012) 262:335–42. doi: 10.1148/radiol.11110416
28. Cho SJ, Baek SM, Lim HK, Lee KD, Son JM, and Baek JH. Long-term follow-up results of ultrasound-guided radiofrequency ablation for low-risk papillary thyroid microcarcinoma: more than 5-year follow-up for 84 tumors. Thyroid. (2020) 30:1745–51. doi: 10.1089/thy.2020.0106
29. Pacella CM, Mauri G, Achille G, Barbaro D, Bizzarri G, De Feo P, et al. Outcomes and risk factors for complications of laser ablation for thyroid nodules: a multicenter study on 1531 patients. J Clin Endocrinol Metab. (2015) 100:3903–10. doi: 10.1210/jc.2015-1964
30. Deandrea M, Garino F, Alberto M, Garberoglio R, Rossetto R, Bonelli N, et al. Radiofrequency ablation for benign thyroid nodules according to different ultrasound features: an Italian multicentre prospective study. Eur J Endocrinol. (2019) 180:79–87. doi: 10.1530/eje-18-0685
31. Kim C, Lee JH, Choi YJ, Kim WB, Sung TY, and Baek JH. Complications encountered in ultrasonography-guided radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers. Eur Radiol. (2017) 27:3128–37. doi: 10.1007/s00330-016-4690-y
32. Bom WJ, Joosten FBM, van Borren M, Bom EP, van Eekeren RRJP, and de Boer H. Radiofrequency ablation for symptomatic, non-functioning, thyroid nodules: a single-center learning curve. Endocrine connections. (2022) 11:210304. doi: 10.1530/ec-21-0304
33. Dobnig H and Amrein K. Monopolar radiofrequency ablation of thyroid nodules: a prospective Austrian single-center study. Thyroid. (2018) 28:472–80. doi: 10.1089/thy.2017.0547
34. Fu Q, Kang S, Wu C, Wang SY, Liu YY, Tian JW, et al. A study on the efficacy of microwave ablation for benign thyroid nodules and related influencing factors. Int J Hyperthermia. (2021) 38:1469–75. doi: 10.1080/02656736.2021.1988151
35. Morvan JB, Maso V, Pascaud D, and Marcy PY. Tracheal necrosis following thyroid radiofrequency ablation. Eur Ann Otorhinolaryngology Head Neck Dis. (2022) 139:29–32. doi: 10.1016/j.anorl.2021.08.004
36. van Baardewijk LJ, Plaisier ML, van den Broek FJC, van Poppel PCMW, Kurban S, and Kruimer JWH. Tracheal necrosis following radiofrequency ablation of a benign thyroid nodule. Cardiovasc Interventional Radiol. (2021) 44:170–1. doi: 10.1007/s00270-020-02632-0
37. Monpeyssen H, Ben Hamou A, Hegedüs L, Ghanassia É, Juttet P, Persichetti A, et al. High-intensity focused ultrasound (HIFU) therapy for benign thyroid nodules: a 3-year retrospective multicenter follow-up study. Int J Hyperthermia. (2020) 37:1301–9. doi: 10.1080/02656736.2020.1846795
38. Ben Hamou A, Ghanassia E, Espiard S, Abi Rached H, Jannin A, Correas JM, et al. Safety and efficacy of thermal ablation (radiofrequency and laser): should we treat all types of thyroid nodules. Int J Hyperthermia. (2019) 36:665–75. doi: 10.1080/02656736.2019.1627432
Keywords: ablation techniques, complication, thyroid nodule, papillary thyroid microcarcinoma, incidence
Citation: Wu S, Cai Y, Liu X and Zhu C (2025) Complications after thermal ablation for thyroid nodules across countries. Front. Endocrinol. 16:1608164. doi: 10.3389/fendo.2025.1608164
Received: 08 April 2025; Accepted: 04 July 2025;
Published: 29 July 2025.
Edited by:
Ilker Sengul, Giresun University, TürkiyeReviewed by:
Chiara Dobrinja, University of Trieste, ItalyDemet Sengul, Giresun University, Türkiye
Flavio Hojaij, University of São Paulo, Brazil
Copyright © 2025 Wu, Cai, Liu and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chenfang Zhu, c2FtbWl6ejE5NzdAMTI2LmNvbQ==; Xiaoyu Liu, eHlsaXViaW9AMTYzLmNvbQ==
†These authors have contributed equally to this work
 Shuang Wu
Shuang Wu Yantao Cai
Yantao Cai Xiaoyu Liu2*
Xiaoyu Liu2* Chenfang Zhu
Chenfang Zhu