- 1Department of Epidemiology and Biostatistics, School of Public Health, Peking University, Beijing, China
- 2Key Laboratory of Major Disease Epidemiology, Ministry of Education (Peking University), Beijing, China
- 3Department of Endocrinology, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, Shandong, China
- 4Shandong Clinical Medical Centre of Endocrinology and Metabolism, Jinan, Shandong, China
- 5Shandong Institute of Endocrine and Metabolic Disease, Jinan, Shandong, China
- 6Research Center of Clinical Epidemiology, Peking University Third Hospital, Beijing, China
- 7Yinzhou District Center for Disease Control and Prevention of Ningbo, Ningbo, China
Objective: This study aimed to evaluate the effectiveness of levothyroxine, compared to non-levothyroxine treatment, in preventing adverse cardiovascular events and mortality in patients with hypothyroidism and cardiovascular disease (CVD).
Methods: This is a retrospective study utilizing medical record data from the Yinzhou Regional Health Care Database. The analysis included patients newly diagnosed with hypothyroidism between July 2006 and December 2021 who also had pre-existing CVD at the time when they received the first hypothyroidism diagnosis. The primary outcome measure was the occurrence of three-point major adverse cardiovascular events (3P-MACE), which included cardiovascular death, non-fatal myocardial infarction, and non-fatal stroke. Secondary outcomes comprised all-cause mortality, all-cause hospitalization, and cardiovascular-related hospitalization. Propensity score matching was used to match levothyroxine users with non-users on a 1:1 basis. Cox proportional hazard models were employed to compare the risk of outcomes between users and non-users, with hazard ratios (HRs) and 95% confidence intervals (CIs) reported.
Results: In the matched cohort (n = 1,332 in each group), 417 patients experienced 3P-MACE. Compared to those not treated with levothyroxine, patients receiving levothyroxine showed a significantly reduced risk of 3P-MACE (HR, 0.67; 95% CI, 0.55–0.82, p < 0.01), all-cause death (HR, 0.24; 95% CI, 0.16–0.35, p < 0.01), all-cause hospitalization (HR, 0.23; 95% CI, 0.21–0.26, p < 0.01), and cardiovascular-related hospitalization (HR, 0.69; 95% CI, 0.59–0.82, p < 0.01).
Conclusions: Levothyroxine may improve major cardiovascular outcomes and decrease all-cause hospital admissions in patients with hypothyroidism and CVD.
Introduction
Hypothyroidism is a prevalent pathological condition characterized by the thyroid gland’s inability to produce adequate thyroid hormones to fulfill the body’s metabolic needs (1). Hypothyroidism is primarily classified into overt hypothyroidism (OH) and subclinical hypothyroidism (SCH). The prevalence of OH and SCH in the general population ranges from 0.3% and 3.7% in the USA and from 0.2% and 5.3% in Europe, with variations depending on the specific definitions applied (2–7). A large cross-sectional study in China showed that the weighted prevalence of OH and SCH was 1.02% and 12.93%, respectively in adults (8). Untreated hypothyroidism can result in severe adverse health effects, including hypertension, dyslipidemia, infertility, cognitive impairments, and neuromuscular dysfunction, which can ultimately lead to death (1, 2). Additionally, population-based studies have also illustrated that SCH increases the incidence of heart failure, coronary heart disease, and stroke and thereby increases the risk of cardiovascular mortality and all-cause mortality (9–12).
The standard treatment for hypothyroidism is thyroid hormone replacement therapy with oral levothyroxine (LT4) on an empty stomach (2, 13). The latest guidelines from major endocrine societies unanimously recommend levothyroxine monotherapy as the first-line treatment for hypothyroidism (14). Thyroid hormones exert significant effects on the cardiovascular system, profoundly influencing cardiac function (15). Some studies have shown that levothyroxine may benefit the patients with concomitant cardiovascular disease (CVD) (16–18).
Although previous studies have indicated an association between hypothyroidism and several CVD risk factors, the findings were not consistent, as some observed improved outcomes, whereas others failed to identify a significant benefit (19–21). Moreover, there is a lack of large-scale observational studies that provide evidence on the association between levothyroxine treatment and CVD outcomes in a Chinese population. Therefore, this retrospective cohort study aimed to determine whether levothyroxine can prevent CVD in Chinese patients with hypothyroidism. In addition to CVD, this study also focused on other secondary outcomes, including all-cause mortality, first hospital admission, and first cardiovascular-related hospitalization.
Materials and methods
Data source
We used data from the Yinzhou Regional Health Care Database (YRHCD). The YRHCD amalgamated longitudinal data from a variety of sources, including electronic medical records (EMRs), disease monitoring and management systems, death registries, and other healthcare services within the Yinzhou District of Ningbo City, China (22–25). The YRHCD encompasses a diverse array of data types: (1) demographic details derived from population census records; (2) prescription information, which includes brand and generic names, Anatomical Therapeutic Chemical (ATC) Classification of Medications codes, prescription dates, dispensed quantities, and textual usage instructions; (3) data on physical activity, lifestyle, and clinical measurements sourced from health check records and disease surveillance and management systems; (4) diagnostic details from EMRs, covering diagnosis names, types, codes (the International Classification of Diseases, Tenth Revision), and dates; (5) laboratory test results and imaging examination data; and (6) mortality information from the death registry.
Participants and cohort
The study cohort comprised patients who received their first diagnosis of hypothyroidism and were diagnosed with CVD before their first hypothyroidism diagnosis between 1 July 2006 and 31 December 2021. To ensure newly diagnosed cases, we included only those with no prior diagnosis of hypothyroidism for at least 180 days before the initial diagnosis date. The index date was defined as the date of the first levothyroxine prescription following the first hypothyroidism diagnosis. For the non-user group, the index date was matched to the date of the first hypothyroidism diagnosis. The baseline period was established as the 180 days preceding the index date, inclusive of the index date. During this period, patient data were collected to establish baseline characteristics and covariates.
Outcome and follow-up
The primary outcome in this study is the incidence of the first three-point major adverse cardiovascular event (3P-MACE), defined as the occurrence of cardiovascular mortality, non-fatal myocardial infarction, or non-fatal stroke. The secondary outcomes assessed in this study were all-cause mortality, hospitalization, and CVD-related hospitalization. All-cause mortality was identified through death registry records. Hospitalization data included the date of admission and the reason for admission, which were coded using ICD classifications. Patients were then followed from the index date until the first occurrence of the following events: an outcome event, death (for outcomes other than mortality), loss to follow-up, or the study end date of 31 December 2022, whichever occurred first.
Statistical analyses
Descriptive statistics were utilized to summarize baseline covariates. To mitigate potential confounding bias and achieve balance in baseline covariates, a propensity score matching (PSM)-based methodology was used for primary and secondary outcome analyses. The PS was estimated via a multivariable logistic regression model, with levothyroxine use as the dependent variable and baseline covariates as predictors. Following PS estimation, each patient in the levothyroxine user group was matched to a patient in the non-user group using the nearest-neighbor method. The balance of covariates was assessed using standardized differences, with an absolute value <0.1 indicating a balance. Some variables’ SMD remained above 0.1 after PSM, and they were adjusted in the subsequent Cox regression models. In the PS-matched population, a Cox regression model was used to estimate the hazard ratio (HR) with a 95% confidence interval (CI), assessing the outcomes between levothyroxine users and non-users. The proportional hazards assumption was tested using scaled Schoenfeld residuals. Time-to-event analyses were conducted using the Kaplan–Meier method, with appropriate graphical summaries.
Statistical analysis was performed using R software version 4.2.2. The R package “mice” was used for missing data imputation. All statistical tests were conducted two-sided and a p-value of less than 0.05 was considered to indicate statistical significance. The study was approved by the ethics committee of Peking University Health Science Center (IRB00001052-23157) and Shandong Provincial Hospital (SWYX: No. 2023-557). Informed consent was not required owing to the use of anonymized routine data.
Subgroup analysis
A subgroup analysis based on baseline characteristics was conducted with particular interest in comparing the effectiveness of levothyroxine among patients with different age stages, sex, smoking status, drinking status, and type of hypothyroidism. All analyses were repeated separately for these subgroups in both the primary and secondary outcome analyses.
Sensitivity analysis
Several sensitivity analyses were conducted to evaluate the robustness of the study findings. First, an analysis was performed without applying PSM to examine the effects of levothyroxine use on the outcomes by multivariate Cox regression models. Second, in analyzing the primary and secondary objectives, we incorporated the Charlson Comorbidity Index (CCI) along with relevant baseline variables to adjust for comorbidities (26). The third sensitivity analysis focused on patients who had not experienced MACE within 6 months before their first hypothyroidism diagnosis. In the fourth sensitivity analysis, we limited the study to subjects whose laboratory markers [thyroid-stimulating hormone (TSH), FT3, and FT4] met the criteria for the initial diagnosis of hypothyroidism (SCH: TSH > 4.8 mIU/L, FT3 9–25 pmol/L and FT4 2.1–5.4 pmol/L; OH: TSH > 4.8 mIU/L and FT4 < 9 pmol/L), ensuring consistency in the diagnostic definition. Fifth, the Fine-Gray subdistribution hazard model was used to check possible competing risks by all-cause death when analyzing MACE, all-cause hospitalization, and CVD-related hospitalization. Sixth, we applied alternative PSM methods, caliper matching with a caliper value of 0.2, to assess their impact on the results. Seventh, we excluded patients in the user group who did not have their first prescription at the time of the first hypothyroidism diagnosis to exclude immortal time. Eighth, patients who had incident outcomes within 30 days (latent period) after the index date were excluded, to control reverse causation and unmeasured confounding by undiagnosed disease (27). Finally, we broadened the exposure definition by classifying any patient with at least one levothyroxine prescription record as treated.
Results
Basic characteristics
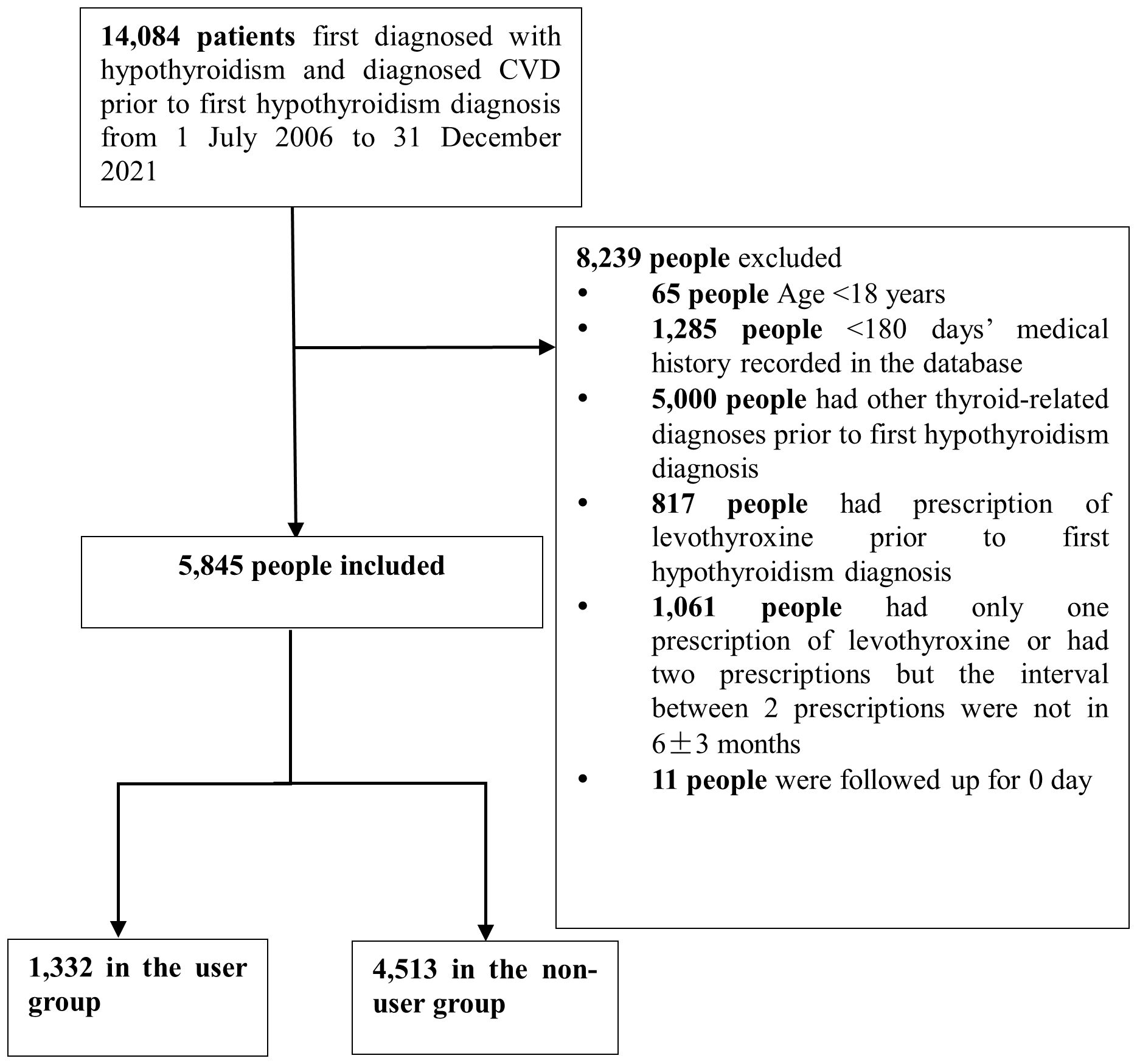
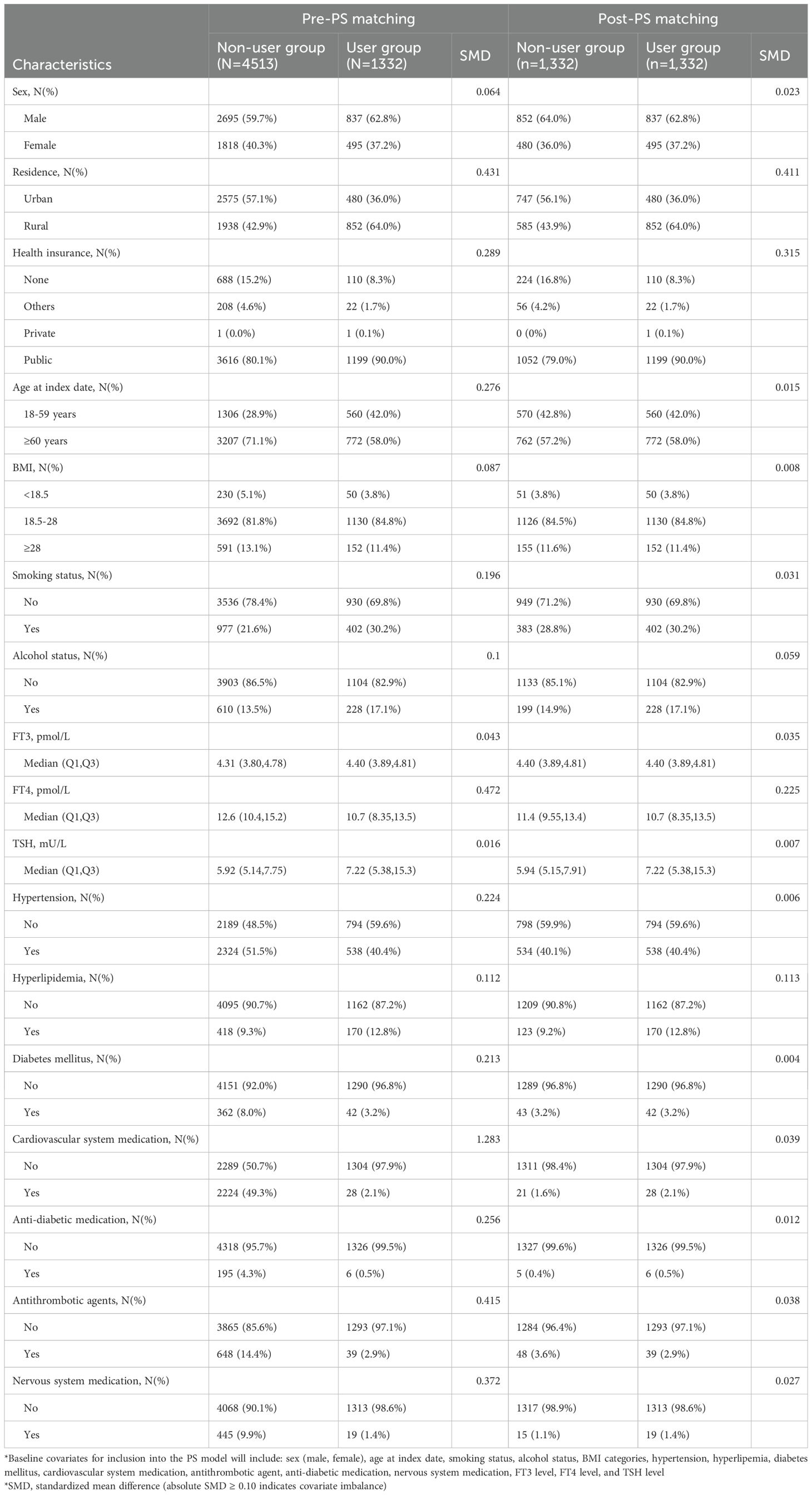
The primary cohort ultimately included 5,845 patients (age 65.2 ± 15.3 years, 60.4% female), of whom 1,332 (22.8%) were treated with levothyroxine (Figure 1). Before PS matching, compared with non-users, the medication group had a higher proportion of people over 45 years of age, a higher proportion of the urban population, a higher proportion of smokers and alcohol drinkers, and a lower proportion of hypertension, CVD, and diabetes, and the proportion of those who received cardiovascular system medications, antithrombotic agents, anti-diabetic medications, and nervous system medications was lower (Table 1). Baseline covariates for inclusion into the PS model included sex (male or female), age at index date, smoking status, alcohol status, body mass index (BMI) categories, hypertension, hyperlipemia, diabetes mellitus, cardiovascular system medication, antithrombotic agent, anti-diabetic medication, nervous system medication, FT3 level, FT4 level, and TSH level. After PSM, covariates except hyperlipemia and FT4 were effectively balanced between the exposure and comparison groups.
The secondary outcome cohort ultimately included 5,843 patients, comprising 1,332 levothyroxine users and 4,511 non-users (Supplementary Figure 1). The baseline characteristics before and after PS matching are detailed in Supplementary Tables 1–3.
Primary analyses
Primary outcome 3P-MACE
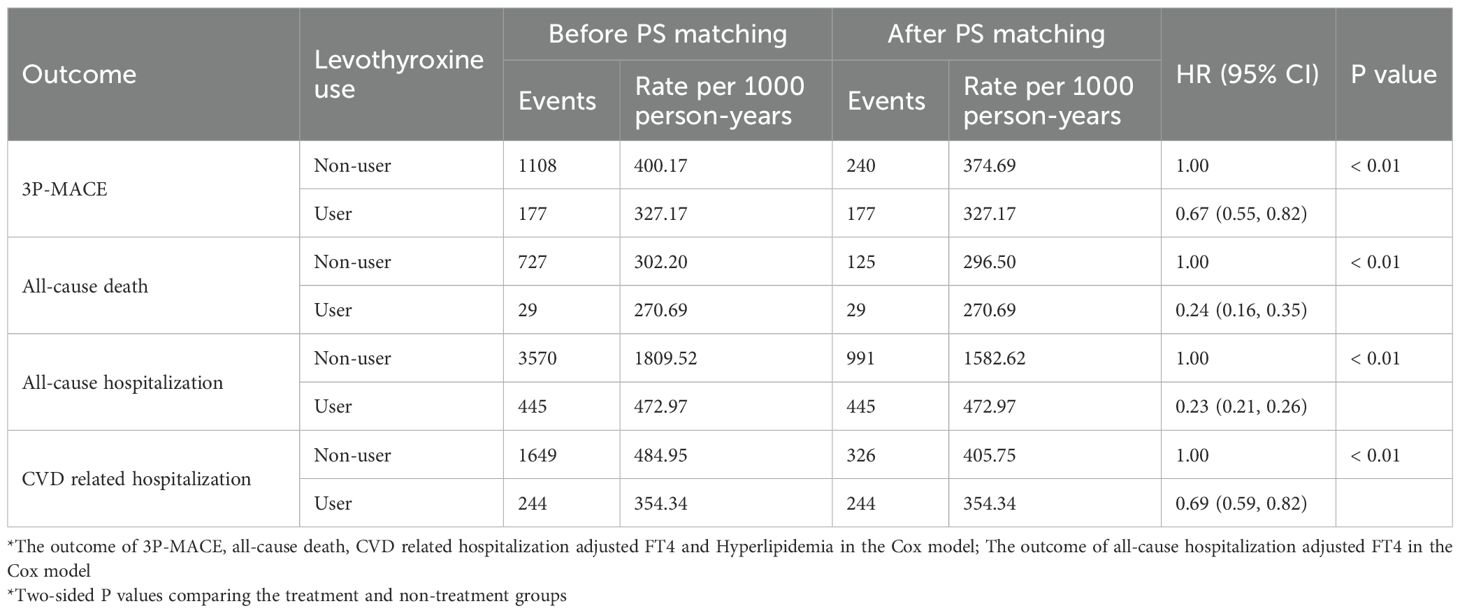
In the primary analyses, during a median follow-up time of 3.22 (95% CI, 3.11–3.38) years, 1,285 new-onset 3P-MACE occurred. The incidences of 3P-MACE were 400.17 and 327.17 per 1,000 person-years in non-users and levothyroxine users, respectively (Table 2). After PS matching, there were 417 cases of new-onset 3P-MACE. The Kaplan–Meier survival curve of 3P-MACE by treatment group is presented in Figure 2a. Levothyroxine use was associated with a lower risk of 3P-MACE incidence, with an HR of 0.67 (95% CI, 0.55–0.82) in the Cox model (p < 0.01).
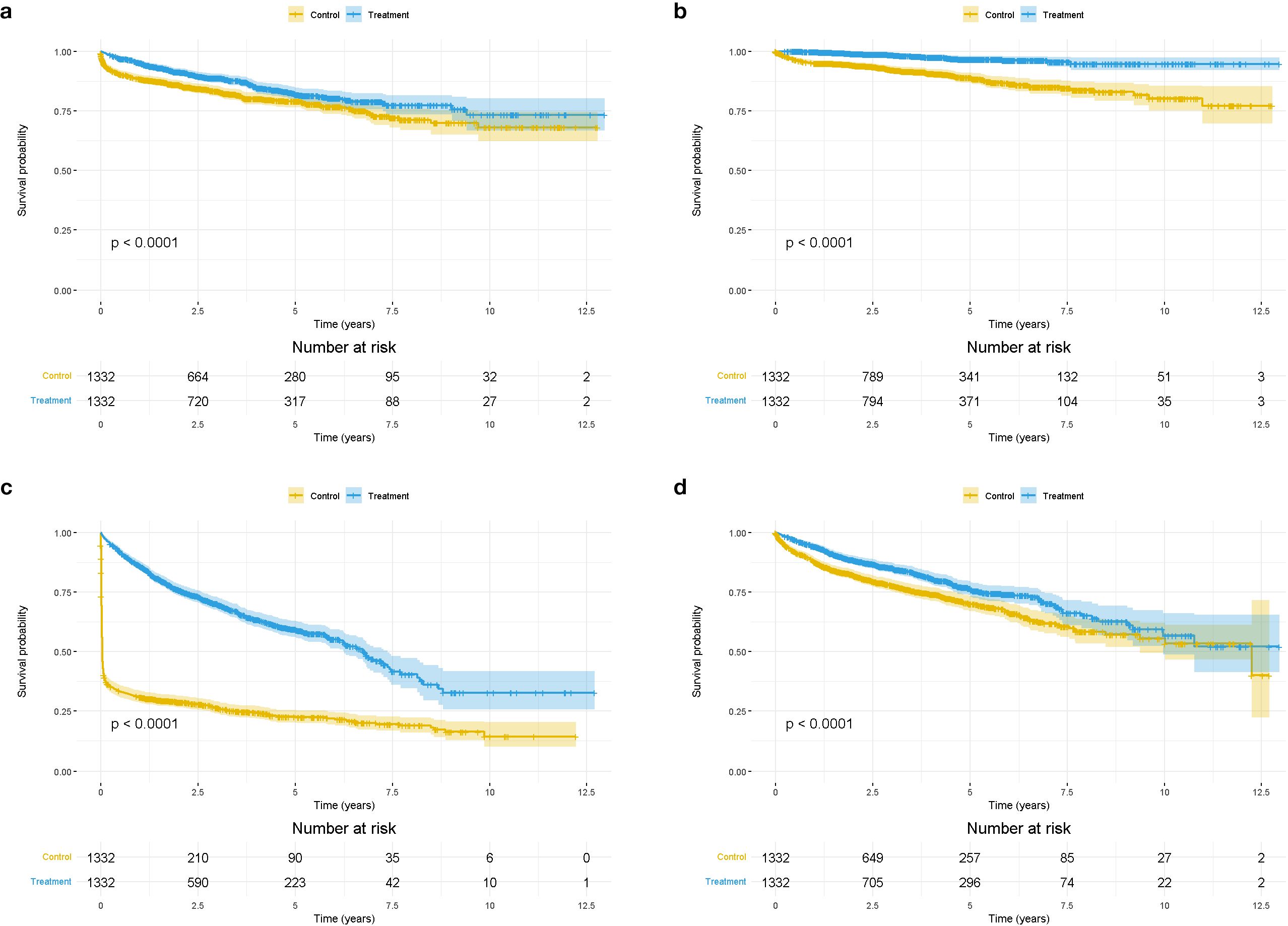
Figure 2. Kaplan-Meier survival curve of primary and secondary outcomes by levothyroxine use (a). The Kaplan-Meier survival curve of 3P-MACE by treatment group (b). The Kaplan-Meier survival curve of all-cause death by treatment group (c). The Kaplan-Meier survival curve of all-cause hospitalization by treatment group (d). The Kaplan-Meier survival curve of cardiovascular-related hospitalization by treatment group. *P for interaction <0.05.
Secondary outcome
Before PS matching, in the secondary outcome cohort, during a median follow-up time of 3.64 years (95% CI, 3.57–3.71), there were 756 incidents of all-cause death. The incidence rates of all-cause death were 302.20 and 270.69 per 1,000 person-years in non-users and users, respectively (Table 2). Figure 2b shows the Kaplan–Meier survival curve of all-cause death by treatment group after PS matching. A total of 154 new-onset all-cause deaths occurred. Levothyroxine use was associated with a reduced risk of all-cause death, with an HR of 0.24 (95% CI, 0.16–0.35).
The study also examined all-cause hospitalization. Before PS matching, there were a total of 4,015 new all-cause hospitalization. After matching, the number was 1,436 (Table 2). Figure 2c displays the Kaplan–Meier survival curve of all-cause hospitalization by treatment group. Levothyroxine use was associated with a significantly lower risk of all-cause hospitalization, with an HR of 0.23 (95% CI, 0.21–0.26).
During a median follow-up time of 3.41 (95% CI, 3.28–3.54) years, 1,893 incident cardiovascular-related hospitalization occurred. The incidences were 484.95 per 1,000 person-years in non-users and 354.34 per 1,000 person-years in users (Table 2). After PS matching, 570 new-onset cardiovascular-related hospitalization occurred. Figure 2d shows the Kaplan–Meier survival curve of cardiovascular-related hospitalization by treatment group. Levothyroxine use reduced the risk of CVD-related hospitalization, with an HR of 0.69 (95% CI, 0.59–0.82).
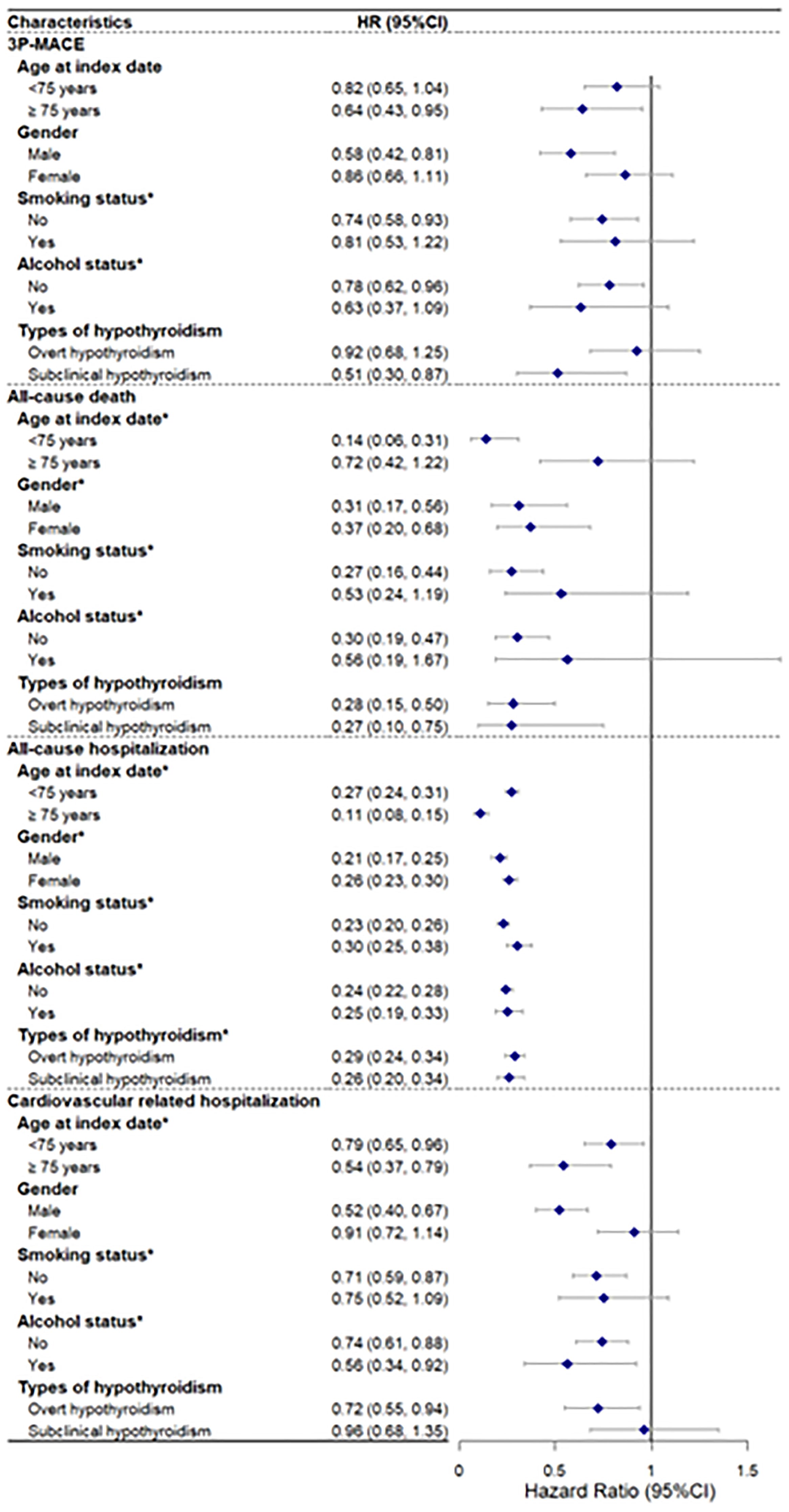
Subgroup analyses
In the subgroup analysis, the results showed consistent associations across different subgroups (Figure 3). Notably, smoking status and alcohol status had significant interactions for all outcomes, and age and gender had significant interactions for all-cause death and all-cause hospitalization, suggesting that these factors may modify the effect of the drug on these outcomes. Moreover, this study did not find differences between OH and SCH in the protective effects of levothyroxine on 3P-MACE, all-cause death, and CVD-related hospitalization. More details can be found in Supplementary Table 4.
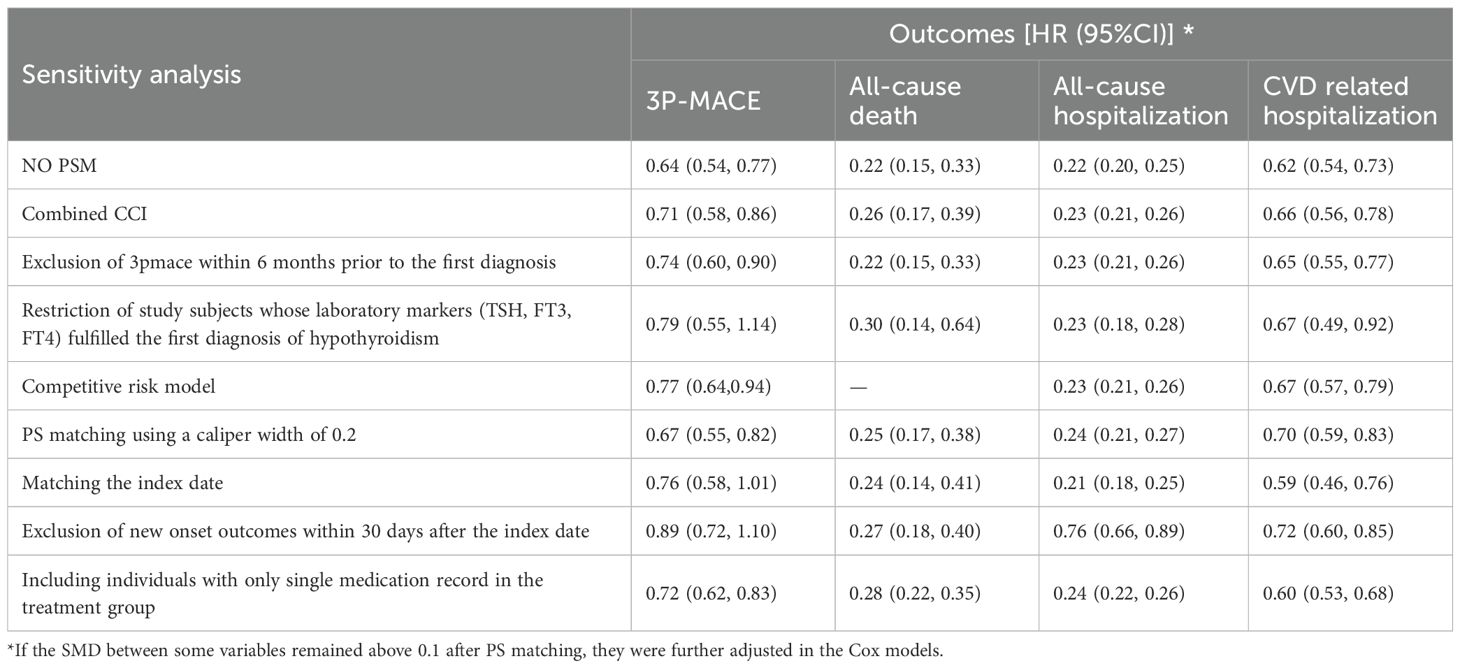
Sensitivity analyses
The results of sensitivity analyses are summarized in Table 3 (Supplementary Figure 2). First, when the analysis was performed without PSM, levothyroxine use was still associated with a lower risk of 3P-MACE, with an HR of 0.64 (95% CI, 0.54–0.77). The risks of all-cause death, all-cause hospitalization, and cardiovascular-related hospitalization were also reduced. Second, after including baseline CCI in PS matching, all Cox regression models showed consistent results with the primary analysis. Third, we excluded patients who had MACE within 6 months prior to their first diagnosis; the HR for 3P-MACE was 0.74 (95% CI, 0.60–0.90). The reduction in the risk of all-cause death, all-cause hospitalization, and CVD-related hospitalization also remained significant. Fourth, when the analysis was restricted to patients whose laboratory markers (TSH, FT3, and FT4) fulfilled the first diagnosis of hypothyroidism, the model for 3P-MACE showed no significant reduction (HR, 0.79; 95% CI, 0.55–1.14), while the risks of all-cause death, all-cause hospitalization, and CVD-related hospitalization were significantly lower. Fifth, the competing risk models presented that the results of HR were in line with that of the primary analysis, indicating no significant competing risk due to all-cause mortality. Sixth, after applying matching with a caliper value of 0.2, we obtained consistent HR estimations. Seventh, we excluded patients in the user group who did not have their first prescription at the time of the first hypothyroidism diagnosis, and the Cox models showed that the direction of HR was inconsistent with that of the primary analysis though there was no statistical difference for 3P-MACE. Eighth, after excluding patients who had outcome events within 30 days after the index date, the Cox models displayed a similar direction of HR. Finally, when levothyroxine exposure was broadened to include patients with at least one prescription, the treatment group rose from 1,332 to 2,383 individuals. Applying the same analytic approach as in the primary analysis, levothyroxine therapy remained significantly associated with reduced risks of 3P-MACE, all−cause mortality, all−cause hospitalization, and cardiovascular-related hospitalization. The sensitivity analyses confirmed the robustness of the primary and secondary outcome results.
Discussion
This retrospective cohort study found that levothyroxine use was associated with a significant reduction in the risk of 3P-MACE, all-cause death, all-cause hospitalization, and cardiovascular-related hospitalization. Primary results remained consistent in subgroup analyses and sensitivity analyses.
Levothyroxine is a commonly used therapeutic agent for hypothyroidism and may be beneficial to reduce CVD risk. Patients with hypothyroidism have elevated serum TSH and consecutively elevated levels of total cholesterol and low-density lipoprotein cholesterol (LDL-C) (28). Levothyroxine can promote the excretion of neutral cholesterol in feces (cholesterol and its derivatives such as bile acids), improve lipoprotein metabolism and anti-inflammatory and anti-oxidative stress, help reduce LDL-C and HDL-C levels, and thereby may improve lipid profiles, reduce vascular resistance, and enhance endothelial function, contractility, and cardiac mitochondrial function, which, in turn, improves cardiac function (29–32). Recent studies have further clarified the roles of thyroid hormones in cardiac remodeling and function, especially following coronary artery disease. Thyroid hormone signaling pathways, mediated by thyroid hormone receptors, can enhance myocardial mitochondrial function, reduce cardiac fibrosis, and improve endothelial function, thereby mitigating pathological cardiac remodeling and dysfunction following ischemic injury (33–35). Specifically, evidence from clinical studies indicates that acute triiodothyronine administration after myocardial infarction may improve ventricular remodeling and cardiac performance, potentially by promoting favorable myocardial metabolic adaptations and exerting anti-inflammatory effects (34). Additionally, preclinical research supports thyroid hormones’ beneficial effects on cardiomyocyte regeneration and repair mechanisms, further underscoring the potential for thyroid hormone-based treatments to positively impact long-term cardiovascular outcomes (35). These insights provide mechanistic context for the cardiovascular benefits associated with levothyroxine therapy observed in our study. When patients with SCH were treated with levothyroxine replacement therapy, in addition to the resolution of hypothyroidism symptoms, these patients also had improvement in atherogenic lipoprotein profiles, arterial stiffness, and intima-media thickening (30, 31, 36).
The available evidence on the protective effect of levothyroxine on adverse cardiovascular events in patients with hypothyroidism is mixed. For example, Razvi et al. analyzed the Whickham Survey and found that the treatment of SCH with levothyroxine appeared to attenuate ischemic heart disease (IHD)-related morbidity and mortality (16), but the sample size was small (SCH group n = 91). Another larger cohort study by Razvi et al. (18), based on the United Kingdom General Practitioner Research Database (CPRD), showed that levothyroxine treatment was associated with a reduction in IHD in younger individuals (aged 40–70 years), whereas this effect was not evident in older patients (aged >70 years). However, our study did not find a difference in the beneficial effects of levothyroxine therapy between younger and older patients. Compared to another study using the CPRD focused mainly on SCH, tightly defining the population by TSH ranges of 5–10 mU/L (37), we examined an OH and SCH population with established CVD and adjusted for key thyroid function parameters. Thereby, our study reflected a higher-risk population more representative of routine clinical practice. A systematic review and meta-analysis demonstrated that levothyroxine supplementation was effective in improving surrogate endpoints for cardiovascular events such as cardiac function indices, cardiac output, and left ventricular ejection fraction in patients with SCH (38). However, some studies have shown that, in some cases, levothyroxine treatment may not significantly decrease the risk of cardiovascular outcomes (19, 21, 39, 40). In a large real-world cohort study in Denmark, levothyroxine treatment in patients with SCH and heart disease was not associated with a significant benefit or risk of all-cause mortality, MACE, or hospital admission (40). Several randomized controlled trials also indicated that levothyroxine provided no apparent benefits (cardiovascular events, cardiovascular mortality, etc.) in older persons with SCH (21, 39). This suggests that the effects of levothyroxine therapy on CVD may vary according to individual differences (17). In addition, previous studies examining the association between levothyroxine use and cardiovascular outcomes have often neglected to consider thyroid status (19, 40), while in our study, TSH, FT3, and FT4 levels were adjusted in the matching analysis.
Notably, even after broadening our definition of levothyroxine treatment to include patients with at least one prescription during follow−up, the treatment rate among Chinese patients with hypothyroidism and CVD remained relatively low at 34.6 %. Our primary definition was designed to capture patients with sustained medication and a high probability of achieving normalization of thyroid function, because most studies indicate that a minimum of 4–6 months of continuous therapy is necessary for plasma TSH and FT4 levels to normalize (41). Nevertheless, treatment rates under both definitions were substantially lower than those reported in developed countries. For comparison, recent reports from Europe and the United States indicated significantly higher levothyroxine treatment rates, generally exceeding 60%–80% (42, 43).
To our knowledge, this is the first study to report levothyroxine treatment rates in Chinese patients with both hypothyroidism and CVD. The observed rate is similar to that of diabetes, another prevalent endocrine disorder in China, whose national treatment rate is approximately 32.4% (44). Although the underlying reasons for these low treatment rates are complex and multifactorial, contributing factors probably include environmental, socioeconomic, lifestyle, and health−policy influences specific to China (44–49). Our findings underscore the importance of appropriate levothyroxine therapy in patients with hypothyroidism, particularly those with co-existing CVD. Timely and adequate treatment of hypothyroidism can mitigate cardiovascular risks, improve patient outcomes, and potentially reduce healthcare costs associated with cardiovascular events and hospitalizations.
As far as we are aware, this study was the first cohort to assess the association between levothyroxine use and incident cardiovascular outcomes and hospital admissions in a Chinese population. Our study had several strengths, including the use of a real-world database, which provides evidence for post-marketing surveillance (PMS) for drugs. We adjusted for potential confounding factors through PSM and multivariable analysis, mitigating confounding by indication (50). In addition, our study specifically investigates the cardiovascular protective effects of levothyroxine treatment in patients with hypothyroidism with pre-existing CVD, which may provide additional insights beyond previous research. Moreover, we performed multiple subgroup analyses and sensitivity analyses, which confirmed the robustness of our results.
However, there were several limitations to our study. First, the patients enrolled in the study were from a single municipal district in China, which may limit the external validity of the findings. Second, despite adjustment for various baseline confounding factors, important time-varying covariates were not considered and residual confounding cannot be entirely excluded. Third, in this study, the initial points of exposure for the two groups were not entirely consistent, which may lead to immortal-time bias and overestimate the protective effect of the medication (51). However, since approximately two-thirds of the users in the cohort were prescribed their first levothyroxine prescription at the time of their first hypothyroidism diagnosis, we set the index date for the non-user group as the date of their first hypothyroidism diagnosis. The control group was much larger than the exposure group in our study, and immortal time accounted for a smaller proportion of the follow-up time in the exposure group; thus, immortal-time bias induced was relatively small (52). Fourth, the database did not record precise dosage information of drugs, and we did not explore the dose–response effect between levothyroxine use and 3P-MACE risk. Finally, this study mainly used coded information and did not conduct case validation for patients with cardiovascular events, which may lead to misclassification bias of outcomes.
Conclusion
In conclusion, this retrospective cohort study demonstrated that levothyroxine therapy was associated with a lower risk of major adverse cardiovascular events, all-cause mortality, and hospitalizations in Chinese patients with hypothyroidism. These results highlight the clinical benefits of levothyroxine and emphasize the importance of managing hypothyroidism to improve cardiovascular outcomes. Further prospective studies and randomized trials are needed to explore its long-term benefits and mechanisms.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee for Biomedical Research Involving Human Beings of Shandong Provincial Hospital and Peking University Biomedical Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. Informed consent was not required owing to the use of anonymized routine data.
Author contributions
LL: Conceptualization, Data curation, Formal Analysis, Methodology, Project administration, Writing – original draft, Writing – review & editing. HQZ: Conceptualization, Methodology, Project administration, Writing – review & editing. XC: Conceptualization, Data curation, Methodology, Writing – original draft. ZL: Conceptualization, Methodology, Writing – review & editing. HYZ: Methodology, Writing – review & editing. SM: Writing – review & editing. MZ: Writing – review & editing. PS: Writing – review & editing. YS: Writing – review & editing. HL: Writing – review & editing. SZ: Writing – review & editing. JZ: Conceptualization, Resources, Writing – review & editing. FS: Conceptualization, Data curation, Resources, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This study was funded by grants from Third Batch of Key Projects of Scientific Act for Drug Regulation of China (RS2024X006), Research Project of China Society for Drug Regulation (2025-Y-Y-012), National Key R&D Program of China (No. 2023YFC2508300 and 2023YFC2508306), and National Natural Science Foundation of China (82370793). This work received funding from Merck Serono, Co. Ltd., Beijing, China, an affiliate of Merck KGaA, Darmstadt, Germany. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2025.1640086/full#supplementary-material
References
1. Gaitonde DY, Rowley KD, and Sweeney LB. Hypothyroidism: an update. Am Fam Physician. (2012) 86:244–51. doi: 10.1080/20786204.2012.10874256
2. Taylor PN, Medici MM, Hubalewska-Dydejczyk A, and Boelaert K. Hypothyroidism. Lancet. (2024) 404:1347–64. doi: 10.1016/s0140-6736(24)01614-3
3. Taylor PN, Albrecht D, Scholz A, Gutierrez-Buey G, Lazarus JH, Dayan CM, et al. Global epidemiology of hyperthyroidism and hypothyroidism. Nat Rev Endocrinol. (2018) 14:301–16. doi: 10.1038/nrendo.2018.18
4. Asvold BO, Vatten LJ, and Bjøro T. Changes in the prevalence of hypothyroidism: the HUNT Study in Norway. Eur J Endocrinol. (2013) 169:613–20. doi: 10.1530/eje-13-0459
5. McGrogan A, Seaman HE, Wright JW, and de Vries CS. The incidence of autoimmune thyroid disease: a systematic review of the literature. Clin Endocrinol (Oxf). (2008) 69:687–96. doi: 10.1111/j.1365-2265.2008.03338.x
6. Razvi S, Korevaar TIM, and Taylor P. Trends, determinants, and associations of treated hypothyroidism in the United Kingdom, 2005-2014. Thyroid. (2019) 29:174–82. doi: 10.1089/thy.2018.0251
7. Canaris GJ, Manowitz NR, Mayor G, and Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med. (2000) 160:526–34. doi: 10.1001/archinte.160.4.526
8. Li Y, Teng D, Ba J, Chen B, Du J, He L, et al. Efficacy and safety of long-term universal salt iodization on thyroid disorders: epidemiological evidence from 31 Provinces of Mainland China. Thyroid. (2020) 30:568–79. doi: 10.1089/thy.2019.0067
9. Chaker L, Baumgartner C, den Elzen WP, Ikram MA, Blum MR, Collet TH, et al. Subclinical hypothyroidism and the risk of stroke events and fatal stroke: an individual participant data analysis. J Clin Endocrinol Metab. (2015) 100:2181–91. doi: 10.1210/jc.2015-1438
10. Nanchen D, Gussekloo J, Westendorp RG, Stott DJ, Jukema JW, Trompet S, et al. Subclinical thyroid dysfunction and the risk of heart failure in older persons at high cardiovascular risk. J Clin Endocrinol Metab. (2012) 97:852–61. doi: 10.1210/jc.2011-1978
11. Rodondi N, den Elzen WP, Bauer DC, Cappola AR, Razvi S, Walsh JP, et al. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. Jama. (2010) 304:1365–74. doi: 10.1001/jama.2010.1361
12. Inoue K, Ritz B, Brent GA, Ebrahimi R, Rhee CM, and Leung AM. Association of subclinical hypothyroidism and cardiovascular disease with mortality. JAMA Netw Open. (2020) 3:e1920745. doi: 10.1001/jamanetworkopen.2019.20745
13. Benvenga S and Carlé A. Levothyroxine formulations: pharmacological and clinical implications of generic substitution. Adv Ther. (2019) 36:59–71. doi: 10.1007/s12325-019-01079-1
14. Hennessey JV. The emergence of levothyroxine as a treatment for hypothyroidism. Endocrine. (2017) 55:6–18. doi: 10.1007/s12020-016-1199-8
15. Udovcic M, Pena RH, Patham B, Tabatabai L, and Kansara A. Hypothyroidism and the heart. Methodist Debakey Cardiovasc J. (2017) 13:55–9. doi: 10.14797/mdcj-13-2-55
16. Razvi S, Weaver JU, Vanderpump MP, and Pearce SH. The incidence of ischemic heart disease and mortality in people with subclinical hypothyroidism: reanalysis of the Whickham Survey cohort. J Clin Endocrinol Metab. (2010) 95:1734–40. doi: 10.1210/jc.2009-1749
17. Sue LY and Leung AM. Levothyroxine for the treatment of subclinical hypothyroidism and cardiovascular disease. Front Endocrinol (Lausanne). (2020) 11:591588. doi: 10.3389/fendo.2020.591588
18. Razvi S, Weaver JU, Butler TJ, and Pearce SH. Levothyroxine treatment of subclinical hypothyroidism, fatal and nonfatal cardiovascular events, and mortality. Arch Intern Med. (2012) 172:811–7. doi: 10.1001/archinternmed.2012.1159
19. Andersen MN, Olsen AM, Madsen JC, Faber J, Torp-Pedersen C, Gislason GH, et al. Levothyroxine substitution in patients with subclinical hypothyroidism and the risk of myocardial infarction and mortality. PloS One. (2015) 10:e0129793. doi: 10.1371/journal.pone.0129793
20. Jabbar A, Ingoe L, Junejo S, Carey P, Addison C, Thomas H, et al. Effect of levothyroxine on left ventricular ejection fraction in patients with subclinical hypothyroidism and acute myocardial infarction: A randomized clinical trial. Jama. (2020) 324:249–58. doi: 10.1001/jama.2020.9389
21. Stott DJ, Rodondi N, Kearney PM, Ford I, Westendorp RGJ, Mooijaart SP, et al. Thyroid hormone therapy for older adults with subclinical hypothyroidism. N Engl J Med. (2017) 376:2534–44. doi: 10.1056/NEJMoa1603825
22. Lin H, Tang X, Shen P, Zhang D, Wu J, Zhang J, et al. Using big data to improve cardiovascular care and outcomes in China: a protocol for the CHinese Electronic health Records Research in Yinzhou (CHERRY) Study. BMJ Open. (2018) 8:e019698. doi: 10.1136/bmjopen-2017-019698
23. Zhao H, Chen X, Sun Y, Shen P, Lin H, Sun F, et al. Associations between thiazolidinediones use and incidence of rheumatoid arthritis: A retrospective population-based cohort study. Arthritis Care Res (Hoboken). (2024) 76:486–96. doi: 10.1002/acr.25277
24. Zhao H, Liu Z, Zhuo L, Shen P, Lin H, Sun Y, et al. Sulfonylurea and cancer risk among patients with type 2 diabetes: A population-based cohort study. Front Endocrinol (Lausanne). (2022) 13:874344. doi: 10.3389/fendo.2022.874344
25. Zhao H, Zhuo L, Sun Y, Shen P, Lin H, and Zhan S. Thiazolidinedione use and risk of Parkinson’s disease in patients with type 2 diabetes mellitus. NPJ Parkinsons Dis. (2022) 8:138. doi: 10.1038/s41531-022-00406-8
26. Bannay A, Chaignot C, Blotière PO, Basson M, Weill A, Ricordeau P, et al. The best use of the Charlson comorbidity index with electronic health care database to predict mortality. Med Care. (2016) 54:188–94. doi: 10.1097/mlr.0000000000000471
27. Danaei G, Rodríguez LA, Cantero OF, Logan R, and Hernán MA. Observational data for comparative effectiveness research: an emulation of randomised trials of statins and primary prevention of coronary heart disease. Stat Methods Med Res. (2013) 22:70–96. doi: 10.1177/0962280211403603
28. Iqbal A, Jorde R, and Figenschau Y. Serum lipid levels in relation to serum thyroid-stimulating hormone and the effect of thyroxine treatment on serum lipid levels in subjects with subclinical hypothyroidism: the Tromsø Study. J Intern Med. (2006) 260:53–61. doi: 10.1111/j.1365-2796.2006.01652.x
29. Miettinen TA. Mechanism of serum cholesterol reduction by thyroid hormones in hypothyroidism. J Lab Clin Med. (1968) 71:537–47.
30. Meier C, Staub JJ, Roth CB, Guglielmetti M, Kunz M, Miserez AR, et al. TSH-controlled L-thyroxine therapy reduces cholesterol levels and clinical symptoms in subclinical hypothyroidism: a double blind, placebo-controlled trial (Basel Thyroid Study). J Clin Endocrinol Metab. (2001) 86:4860–6. doi: 10.1210/jcem.86.10.7973
31. Peleg RK, Efrati S, Benbassat C, Fygenzo M, and Golik A. The effect of levothyroxine on arterial stiffness and lipid profile in patients with subclinical hypothyroidism. Thyroid. (2008) 18:825–30. doi: 10.1089/thy.2007.0359
32. Ilic S, Tadic M, Ivanovic B, Caparevic Z, Trbojevic B, and Celic V. Left and right ventricular structure and function in subclinical hypothyroidism: the effects of one-year levothyroxine treatment. Med Sci Monit. (2013) 19:960–8. doi: 10.12659/msm.889621
33. Pantos CI, Grigoriou KP, Trikas AG, Alexopoulos NA, and Mourouzis IS. Translating thyroid hormone into clinical practice: lessons learned from the post-hoc analysis on data available from the ThyRepair study. Front Endocrinol (Lausanne). (2024) 15:1405251. doi: 10.3389/fendo.2024.1405251
34. Pantos CI, Trikas AG, Pissimisis EG, Grigoriou KP, Stougiannos PN, Dimopoulos AK, et al. Effects of acute triiodothyronine treatment in patients with anterior myocardial infarction undergoing primary angioplasty: evidence from a pilot randomized clinical trial (ThyRepair study). Thyroid. (2022) 32:714–24. doi: 10.1089/thy.2021.0596
35. Mantzouratou P, Malaxianaki E, Cerullo D, Lavecchia AM, Pantos C, Xinaris C, et al. Thyroid hormone and heart failure: charting known pathways for cardiac repair/regeneration. Biomedicines. (2023) 11. doi: 10.3390/biomedicines11030975
36. Monzani F, Caraccio N, Kozàkowà M, Dardano A, Vittone F, Virdis A, et al. Effect of levothyroxine replacement on lipid profile and intima-media thickness in subclinical hypothyroidism: a double-blind, placebo- controlled study. J Clin Endocrinol Metab. (2004) 89:2099–106. doi: 10.1210/jc.2003-031669
37. Yu OHY, Filliter C, Filion KB, Platt RW, Grad R, and Renoux C. Levothyroxine treatment of subclinical hypothyroidism and the risk of adverse cardiovascular events. Thyroid. (2024) 34:1214–24. doi: 10.1089/thy.2024.0227
38. Wang X, Wang H, Li Q, Wang P, Xing Y, Zhang F, et al. Effect of levothyroxine supplementation on the cardiac morphology and function in patients with subclinical hypothyroidism: A systematic review and meta-analysis. J Clin Endocrinol Metab. (2022) 107:2674–83. doi: 10.1210/clinem/dgac417
39. Zijlstra LE, Jukema JW, Westendorp RGJ, Du Puy RS, Poortvliet RKE, Kearney PM, et al. Levothyroxine treatment and cardiovascular outcomes in older people with subclinical hypothyroidism: pooled individual results of two randomised controlled trials. Front Endocrinol (Lausanne). (2021) 12:674841. doi: 10.3389/fendo.2021.674841
40. Andersen MN, Olsen AS, Madsen JC, Kristensen SL, Faber J, Torp-Pedersen C, et al. Long-term outcome in levothyroxine treated patients with subclinical hypothyroidism and concomitant heart disease. J Clin Endocrinol Metab. (2016) 101:4170–7. doi: 10.1210/jc.2016-2226
41. Roos A, Linn-Rasker SP, van Domburg RT, Tijssen JP, and Berghout A. The starting dose of levothyroxine in primary hypothyroidism treatment: a prospective, randomized, double-blind trial. Arch Intern Med. (2005) 165:1714–20. doi: 10.1001/archinte.165.15.1714
42. Wyne KL, Nair L, Schneiderman CP, Pinsky B, Antunez Flores O, Guo D, et al. Hypothyroidism prevalence in the United States: A retrospective study combining national health and nutrition examination survey and claims data, 2009-2019. J Endocr Soc. (2022) 7:bvac172. doi: 10.1210/jendso/bvac172
43. Møllehave LT, Eliasen MH, Strēle I, Linneberg A, Moreno-Reyes R, Ivanova LB, et al. Register-based information on thyroid diseases in Europe: lessons and results from the EUthyroid collaboration. Endocr Connect. (2022) 11. doi: 10.1530/ec-21-0525
44. Wang L, Peng W, Zhao Z, Zhang M, Shi Z, Song Z, et al. Prevalence and treatment of diabetes in China, 2013-2018. Jama. (2021) 326:2498–506. doi: 10.1001/jama.2021.22208
45. Wang L, Gao P, Zhang M, Huang Z, Zhang D, Deng Q, et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. Jama. (2017) 317:2515–23. doi: 10.1001/jama.2017.7596
46. Powell LM, Wada R, Krauss RC, and Wang Y. Ethnic disparities in adolescent body mass index in the United States: the role of parental socioeconomic status and economic contextual factors. Soc Sci Med. (2012) 75:469–76. doi: 10.1016/j.socscimed.2012.03.019
47. Di Cesare M, Khang YH, Asaria P, Blakely T, Cowan MJ, Farzadfar F, et al. Inequalities in non-communicable diseases and effective responses. Lancet. (2013) 381:585–97. doi: 10.1016/s0140-6736(12)61851-0
48. Zhao Z, Li M, Li C, Wang T, Xu Y, Zhan Z, et al. Dietary preferences and diabetic risk in China: A large-scale nationwide Internet data-based study. J Diabetes. (2020) 12:270–8. doi: 10.1111/1753-0407.12967
49. Yip W, Fu H, Chen AT, Zhai T, Jian W, Xu R, et al. 10 years of health-care reform in China: progress and gaps in Universal Health Coverage. Lancet. (2019) 394:1192–204. doi: 10.1016/s0140-6736(19)32136-1
50. Stürmer T, Wang T, Golightly YM, Keil A, Lund JL, and Jonsson Funk M. Methodological considerations when analysing and interpreting real-world data. Rheumatol (Oxford). (2020) 59:14–25. doi: 10.1093/rheumatology/kez320
51. Hernán MA, Sauer BC, Hernández-Díaz S, Platt R, and Shrier I. Specifying a target trial prevents immortal time bias and other self-inflicted injuries in observational analyses. J Clin Epidemiol. (2016) 79:70–5. doi: 10.1016/j.jclinepi.2016.04.014
Keywords: levothyroxine, MACE, hypothyroidism, pharmacoepidemiology, cohort study
Citation: Liu L, Zhang H, Chen X, Liu Z, Zhao H, Ma S, Zhao M, Shen P, Sun Y, Lin H, Zhan S, Zhao J and Sun F (2025) Effect of levothyroxine on major adverse cardiovascular events in patients with hypothyroidism and cardiovascular disease. Front. Endocrinol. 16:1640086. doi: 10.3389/fendo.2025.1640086
Received: 03 June 2025; Accepted: 31 July 2025;
Published: 26 August 2025.
Edited by:
Bernadette Biondi, University of Naples Federico II, ItalyReviewed by:
Giulia Brigante, University of Modena and Reggio Emilia, ItalyConstantinos Pantos, National and Kapodistrian University of Athens, Greece
Copyright © 2025 Liu, Zhang, Chen, Liu, Zhao, Ma, Zhao, Shen, Sun, Lin, Zhan, Zhao and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Feng Sun, c3VuZmVuZ0Biam11LmVkdS5jbg==; Jiajun Zhao, amp6aGFvQHNkdS5lZHUuY24=
†These authors have contributed equally to this work
 Lijia Liu
Lijia Liu Haiqing Zhang
Haiqing Zhang Xiaowei Chen1,2†
Xiaowei Chen1,2† Zuoxiang Liu
Zuoxiang Liu Houyu Zhao
Houyu Zhao Shizhan Ma
Shizhan Ma Meng Zhao
Meng Zhao Siyan Zhan
Siyan Zhan Jiajun Zhao
Jiajun Zhao Feng Sun
Feng Sun