- 1Department of Andrology, China-Japan Friendship Hospital, Beijing, China
- 2Graduate School, Beijing University of Chinese Medicine, Beijing, China
- 3Institute of Basic Medical Sciences, Chinese Academy of Medical Sciences, School of Basic Medicine, Peking Union Medical College, Beijing, China
A Correction on
Inflammation of the male reproductive system: clinical aspects and mechanisms
by Bao B, Wen H, Wang F, Han D and Liu B (2025). Front. Endocrinol. 16:1547020. doi: 10.3389/fendo.2025.1547020
In the published article, there was an error in Figure 3, Figure 4 and Figure 5 as published. Figure 3, Figure 4 and Figure 5 are positioned incorrectly in the published version. The figures have been swapped, although the figure captions remain correct and in their proper positions. The corrected Figure 3, Figure 4 and Figure 5 and its caption appear below.
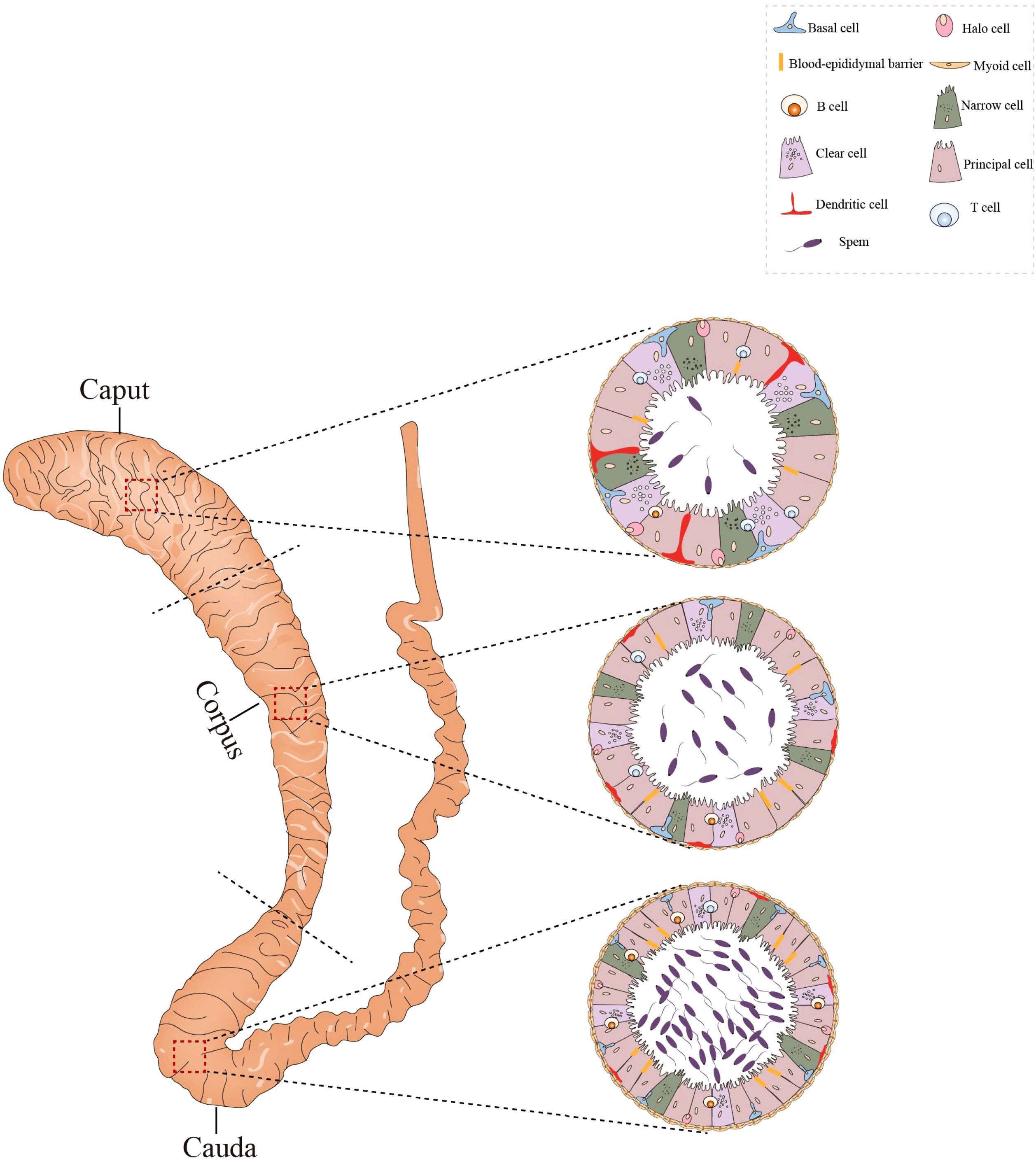
Figure 3. Histological structure and cellular components of the epididymis. The epididymis consists of three sections: the caput, corpus, and cauda. Its epithelium harbors diverse cell types, such as basal cells, lymphocytes, clear cells, dendritic cells, and macrophages. In the caput, dendritic cells can extend towards the tight junctions between epithelial cells. The caput contains a higher number of T cells compared to the cauda, whereas the concentration of B cells is greater in the cauda. All figures were drawn using Adobe Illustrator software.
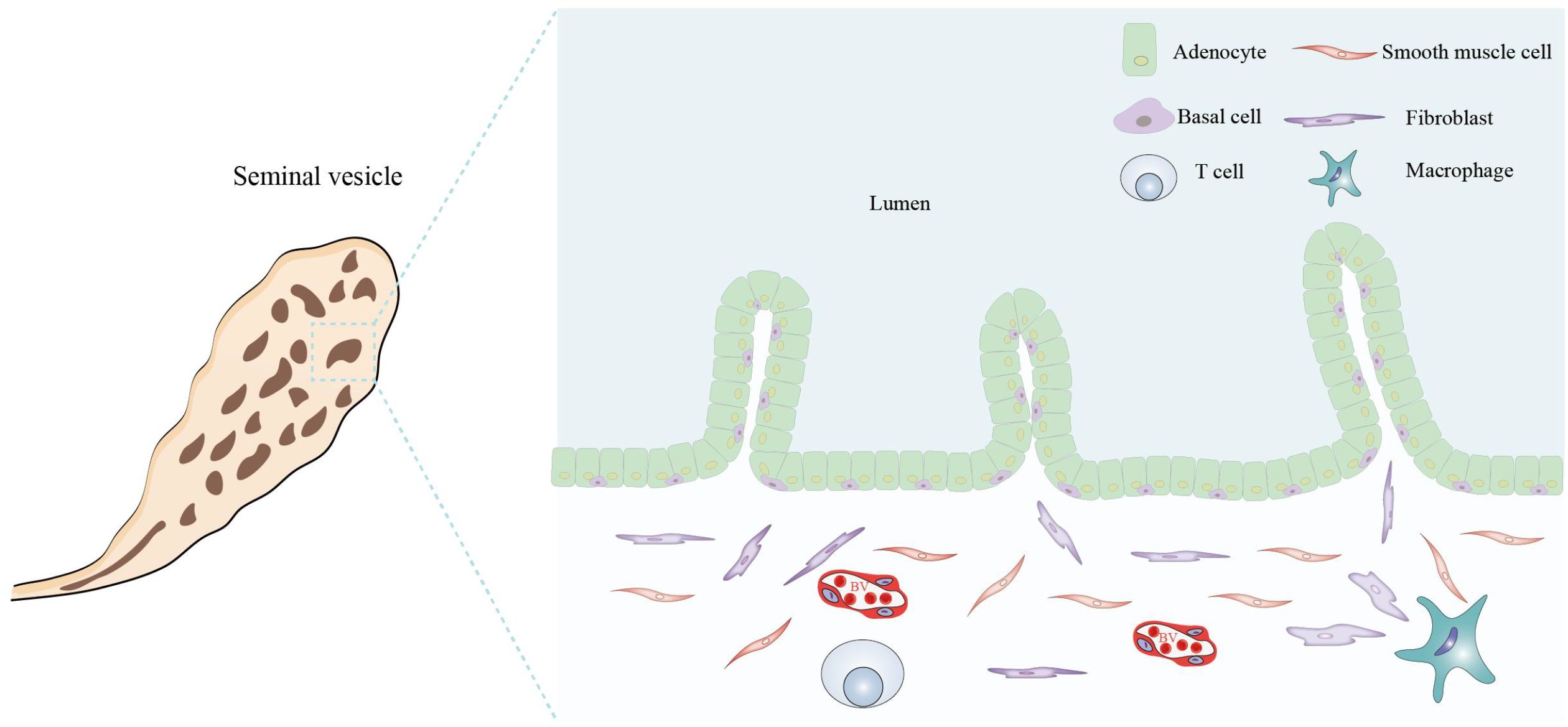
Figure 4. Histological structure and cellular components of the seminal vesicle. The seminal vesicle consists of a coiled tube with a blind end and contains several irregular vesicles within. It is primarily composed of a mucosal layer and a smooth muscle layer. The mucosal surface features non-ciliated, pseudostratified columnar epithelium, which includes glandular cells (adenocytes) and basal cells. The smooth muscle layer predominantly comprises smooth muscle cells, fibroblasts, macrophages, T cells, and BVs. All figures were drawn using Adobe Illustrator software.
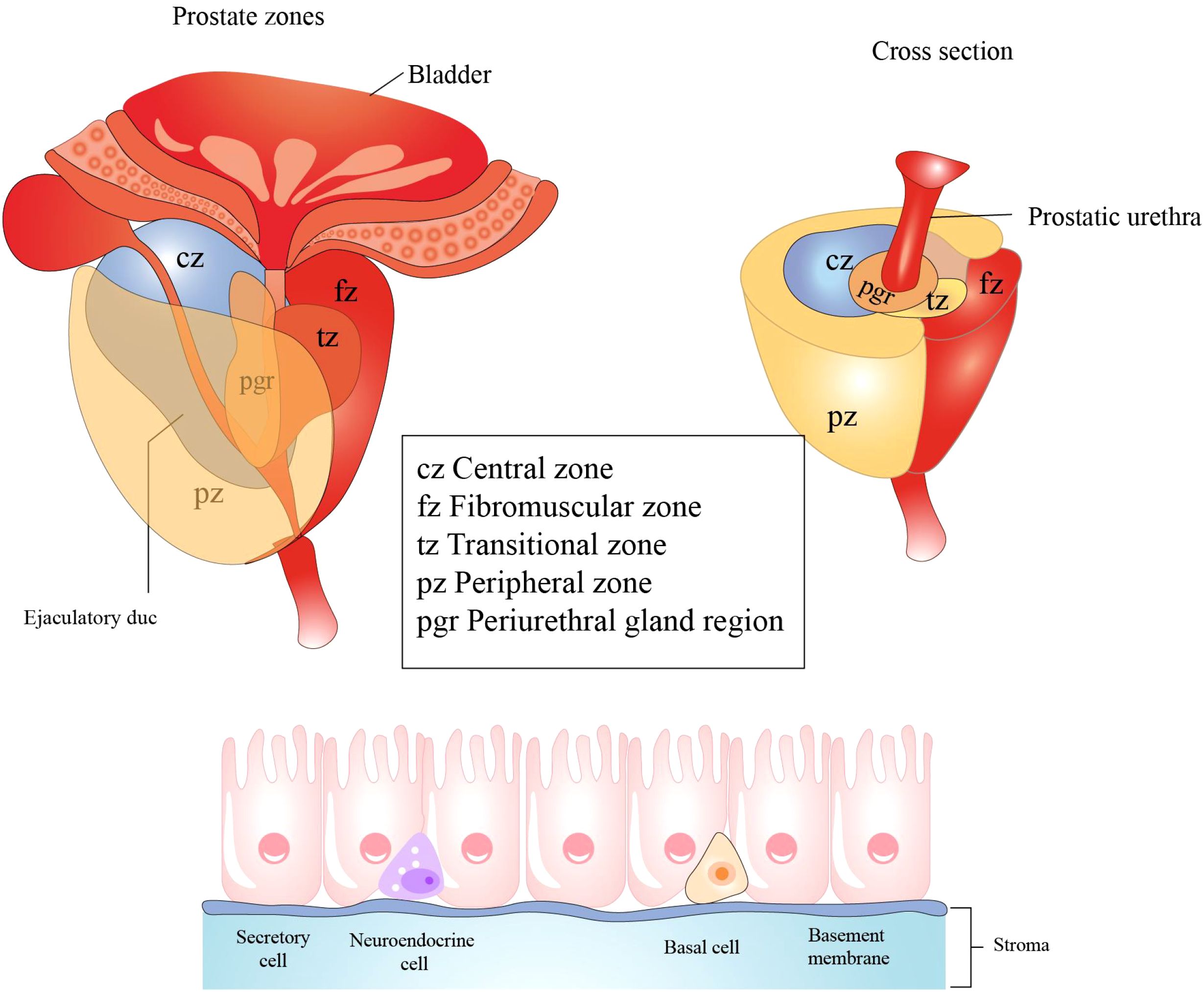
Figure 5. Histological structure and cellular components of the prostate. The prostate primarily consists of three regions: the central zone, situated around the ejaculatory ducts; the transition zone, encircling the urethra; the peripheral zone, which is the largest region. Prostatic epithelial cells play a crucial role in defending against microbial infections of the prostate by secreting antibacterial and antiviral substances. These cells predominantly comprise three cell types: secretory cells, basal cells, and neuroendocrine cells. All figures were drawn using Adobe Illustrator software.
The authors apologize for this error and state that this does not change the scientific conclusions of the article in any way. The original article has been updated.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Keywords: male reproductive system, inflammation, spermatozoa, diagnosis, treatment
Citation: Bao B, Wen H, Wang F, Han D and Liu B (2025) Correction: Inflammation of the male reproductive system: clinical aspects and mechanisms. Front. Endocrinol. 16:1649509. doi: 10.3389/fendo.2025.1649509
Received: 18 June 2025; Accepted: 23 June 2025;
Published: 02 July 2025.
Reviewed by:
Richard Ivell, University of Nottingham, United KingdomCopyright © 2025 Bao, Wen, Wang, Han and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Baoxing Liu, bGl1YmFveGluZ0B6cnloeXkuY29tLmNu
†These authors share first authorship
 Binghao Bao
Binghao Bao Haolang Wen
Haolang Wen Fei Wang3
Fei Wang3 Daishu Han
Daishu Han