- Department of Endocrinology and Pediatric Infectious Diseases, Poltava State Medical University, Poltava, Ukraine
Introduction: Type 2 diabetes mellitus (T2DM) is frequently associated with microvascular dysfunction that contributes to the development of complications such as neuropathy, nephropathy, and retinopathy. Early detection of these alterations is essential for effective prevention and personalized care.
Aim: To evaluate microcirculatory changes in patients with type 2 diabetes using laser Doppler flowmetry (LDF).
Materials and methods: This observational study included 25 individuals: 19 patients with T2DM and 6 healthy controls. Microcirculatory parameters were assessed using LDF, a non-invasive technique for evaluating perfusion in real time. Parameters such as endothelial nitric oxide–dependent activity, neurogenic and myogenic regulation, oxidative metabolism, and nutritive blood flow were measured and analyzed.
Results: Patients with T2DM demonstrated significant microcirculatory disturbances, including reduced endothelial NO-dependent activity, increased sympathetic adrenergic and myogenic activity, and elevated oxidative stress levels. A decreased coefficient of variation and increased nutritive flow suggested a compensatory adaptation of vascular tone regulation. A strong positive correlation was identified between the microcirculation index and regulatory system tension (r = 0.7561; p = 0.0002), indicating systemic vascular strain.
Conclusion: LDF proved to be an effective tool for the early detection of subclinical microvascular changes in patients with T2DM. These findings support the incorporation of LDF into clinical protocols for individualized risk stratification, early intervention, and treatment monitoring. Further longitudinal studies with larger cohorts are warranted to validate its role in precision diabetology.
Introduction
Diabetes mellitus is one of the most prevalent chronic endocrine disorders, significantly affecting patients’ quality of life. This disease is characterized by the development of microvascular complications such as diabetic retinopathy, nephropathy and neuropathy (1–4). Microcirculatory impairment plays a key role in the pathogenesis of these complications, as it is at this level that disturbances in blood flow and tissue gas exchange occur (1, 4, 5).
The study of the microcirculatory system is of great importance for the timely diagnosis and monitoring of the progression of diabetes-related complications (6–8). One of the up-to-date non-invasive methods for assessing microcirculation is LDF (9–11). This technique can be applied to the surface of any organ, most commonly on the skin or mucous membranes. In recent years, LDF has been the subject of numerous publications due to its ease of use, short measurement duration and the minimal training required for the operator. This method enables the evaluation of the functional state of the microvascular system by analyzing blood flow in real time, making it highly valuable in clinical practice (12, 13). LDF is a state-of-the-art, highly sensitive method for investigating the microcirculatory system and can be effectively utilized in diagnosing circulatory disorders in patients with diabetes mellitus. The method is based on analyzing changes in the frequency of laser radiation reflected from erythrocytes moving through microvessels. LDF can detect subclinical disturbances even in the early stages, when clinical symptoms may still be absent (9–13).
Materials and methods
This observational study included 25 patients aged 40–66 years (mean age: 58 ± 1.7 years) treated at the Endocrinology Department of the 2nd City Clinical Hospital in Poltava between March and August 2023. The study population was divided into two groups: the control group (n = 6), which included individuals without diabetes mellitus, and the study group (n = 19), composed of patients diagnosed with T2DM.
All participants provided written informed consent prior to inclusion in the study. The study protocol was approved by the Biomedical Ethics Committee of Poltava State Medical University (Protocol No. 235, dated February 20, 2025). This research is part of the broader project “Development of Means for the Correction of Pathological Changes in the Digestive System in the Context of Civilization-Related Diseases” (State registration number: 0124U001922; 2024–2028).
Microcirculatory assessment of the lower limbs (dorsal foot) was performed using the LASMA PF laser Doppler flowmeter. Measurements were taken in a resting state over a 6-minute period. The data were recorded as perfusion curves. The microcirculation index (MI) was calculated to reflect baseline tissue perfusion.
In addition to absolute perfusion, we evaluated the regulatory mechanisms influencing blood flow by analyzing both active and passive rhythmic oscillations in the LDF signal. Active components included endothelial (Ae), neurogenic (An), and myogenic (Am) activity, while passive components were associated with respiratory (Ad) and cardiac (Ac) influences. Functional adaptation of the vascular system was assessed using the coefficient of variation (Kv). The oxidative metabolism index (OMI) and nutritive blood flow (Mntr) were also calculated.
Wavelet analysis was used to decompose the LDF signal and quantify the contributions of the various frequency ranges corresponding to the described mechanisms. This enabled a comprehensive evaluation of the functional integrity of the microvascular regulatory system.
Statistical analysis was conducted using GraphPad Prism 5.03 and Microsoft Excel 2010. Normality of distribution was tested using the D’Agostino–Pearson omnibus test and Kolmogorov–Smirnov test. For normally distributed data, results are reported as mean ± standard error of the mean (M ± m); non-normal data are presented as median [25th–75th percentiles]. Between-group comparisons were performed using the Kruskal–Wallis test. For paired comparisons, the Student’s t-test or Wilcoxon signed-rank test was applied, depending on data distribution. Correlations between continuous variables were analyzed using Pearson’s or Spearman’s correlation coefficients. A p-value < 0.05 was considered statistically significant.
Results
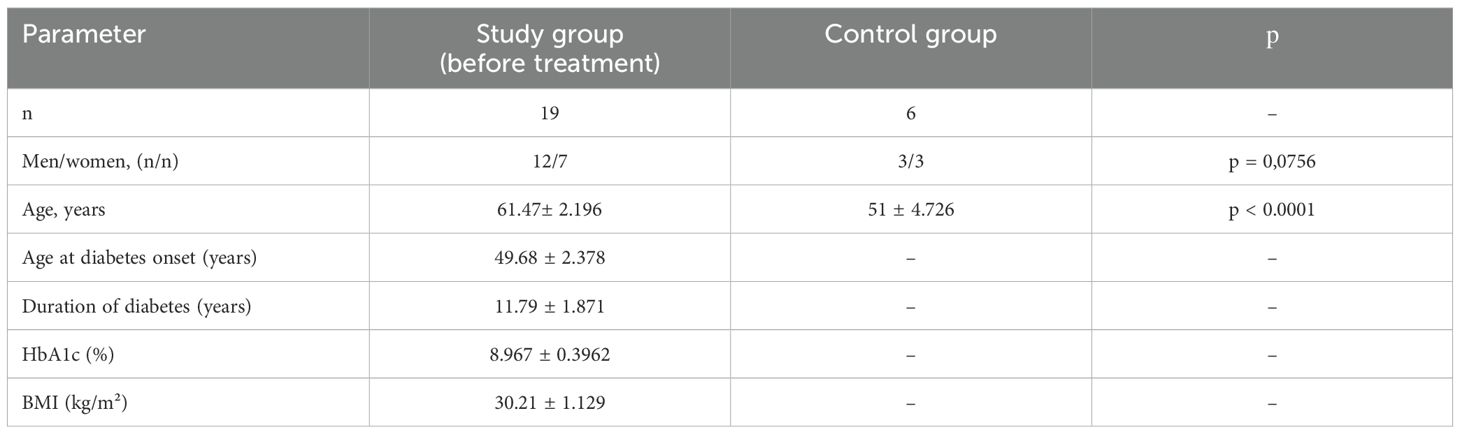
The mean age of patients in the study group was 61.47 ± 2.196 years, the average duration of diabetes mellitus was 11.79 ± 1.871 years, and the mean age at onset of diabetes was 49.68 ± 2.378 years (Table 1). No statistically significant difference was found between the study and control groups in terms of sex distribution (p=0.0756).
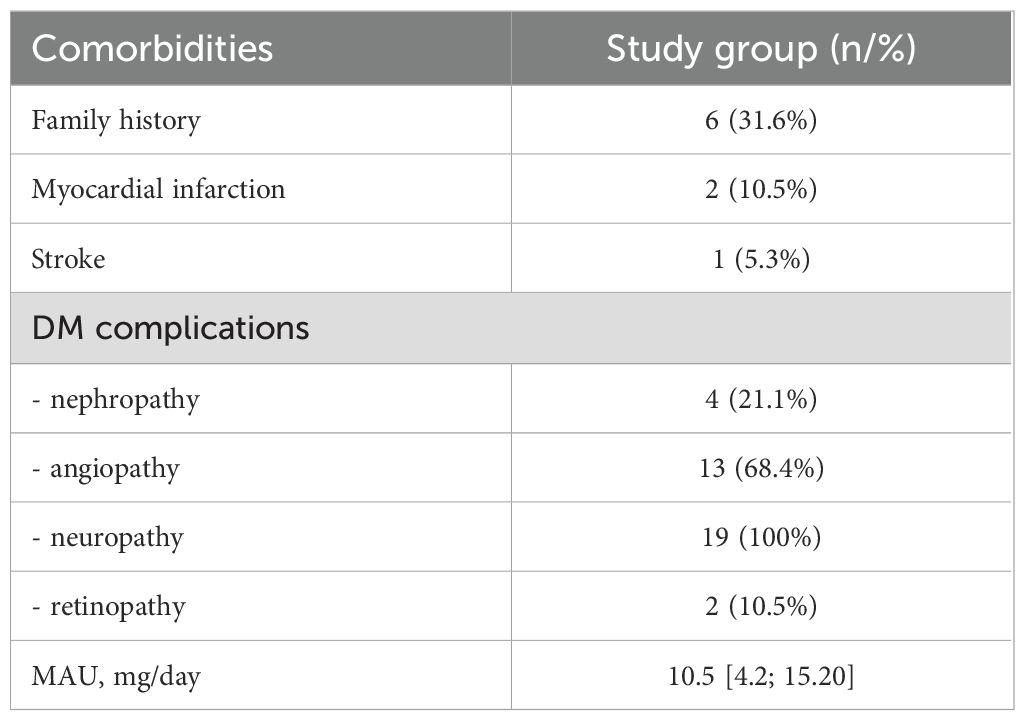
The analysis of comorbidities and complications in patients from the study group is presented in Table 2. A family history of diabetes mellitus was noted in 31.6% of patients, indicating a genetic predisposition to the development of this disease.
Among cardiovascular events, 10.5% of patients experienced a myocardial infarction, while stroke was documented in 5.3% of cases.
Complications of diabetes mellitus were highly prevalent in the study group. The most common complication was neuropathy, observed in all patients (100%). Angiopathy was identified in 68.4% of patients, while nephropathy was present in 21.1%. Diabetic retinopathy was documented in 10.5% of patients.
Additionally, the level of microalbuminuria (MAU) was assessed, which serves not only as a marker of renal impairment but also indicates an increased risk of cardiovascular complications. The mean MAU level in patients was 10.5 mg/day, with an interquartile range of [4.2; 15.20], suggesting the presence of early signs of renal dysfunction in a subset of patients. These findings underscore the high prevalence of micro- and macrovascular complications in patients with diabetes mellitus, highlighting the need for active monitoring and timely intervention to prevent their progression.
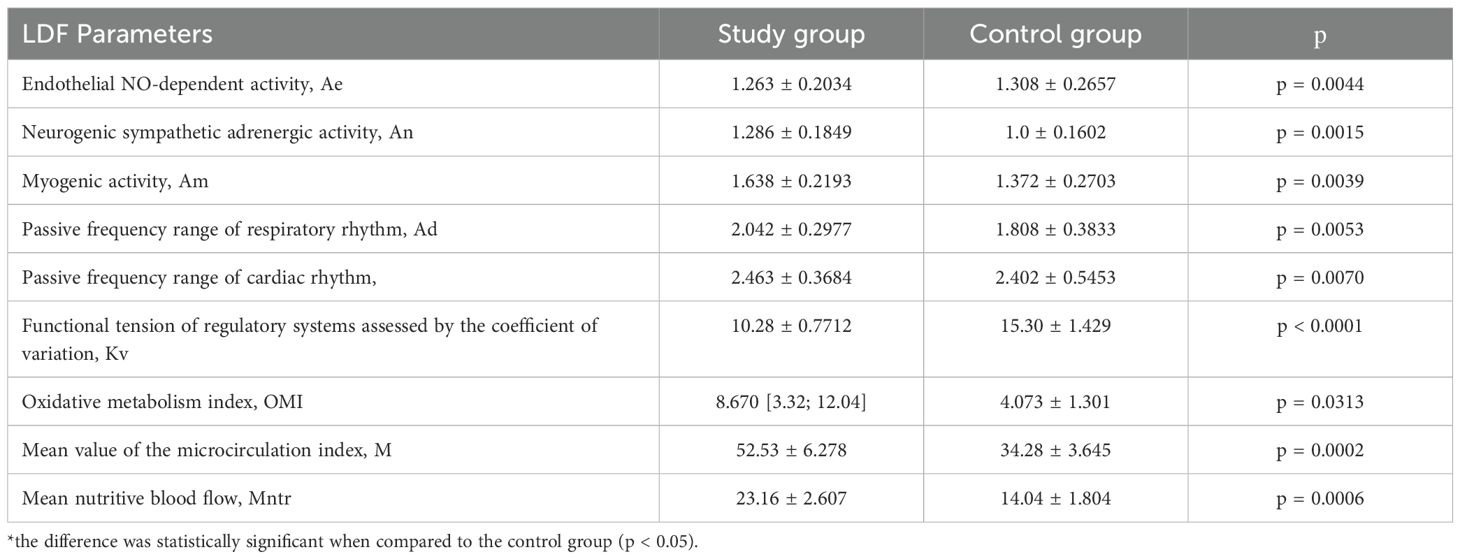
Table 3 presents the results of LDF, characterizing microcirculatory activity and the functioning of regulatory mechanisms in patients with type 2 diabetes mellitus (study group) compared to healthy individuals (control group). According to the obtained data, all LDF parameters differed significantly between the study and control groups (p<0.05).
The status of blood flow in the microvessels of the foot skin was evaluated by assessing the mean perfusion (M), which was 34.27 ± 3.64 perfusion units (PU) in the control group and 52.53 ± 6.27 PU in the study group. Thus, higher microcirculation index values were observed in patients with diabetes mellitus compared to controls. This finding can be explained by the impact of prolonged neuropathy on microcirculatory function, leading to increased cutaneous blood flow.
The endothelial NO-dependent activity index (Ae) in the study group was 1.263 ± 0.2034, which was significantly lower than that in the control group (1.308 ± 0.2657, p = 0.0044). This indicates a reduced capacity of the endothelium to synthesize nitric oxide (NO), thereby impairing vascular regulatory function.
Neurogenic sympathetic adrenergic activity (An) in patients with T2DM was elevated (1.286 ± 0.1849) compared to the control group (1.0 ± 0.1602, p=0.0015). This indicates hyperactivity of the sympathetic nervous system, which affects microcirculatory tone.
In the study group, the value of myogenic activity (Am) was significantly higher (1.638 ± 0.2193) compared to the control group (1.372 ± 0.2703, p=0.0039), indicating enhancement of myogenic regulation as a compensatory mechanism.
The study group exhibited significantly lower values of the coefficient of variation (Kv) (10.28 ± 0.7712) compared to the control group (15.30 ± 1.429, p<0.0001), indicating a high level of regulatory system stress in diabetes mellitus.
The oxidative metabolism index (OMI) showed a significantly higher median level in the study group (8.670 [3.32; 12.04]) compared to the control group (4.073 ± 1.301, p = 0.0313), indicating increased oxidative stress in patients with diabetes mellitus.
The nutritive blood flow index (Mntr) was significantly higher in the study group (23.16 ± 2.607) compared to the control group (14.04 ± 1.804, p=0.0006), reflecting compensatory activity aimed at providing tissues with energy.
Thus, patients with T2DM exhibit significant alterations in microcirculatory function, including reduced endothelial activity, increased sympathetic and myogenic activity, as well as elevated oxidative stress. These changes result from impaired regulation of vascular tone and metabolic imbalance characteristic of this disease. This underscores the importance of early monitoring of microcirculatory status in such patients.
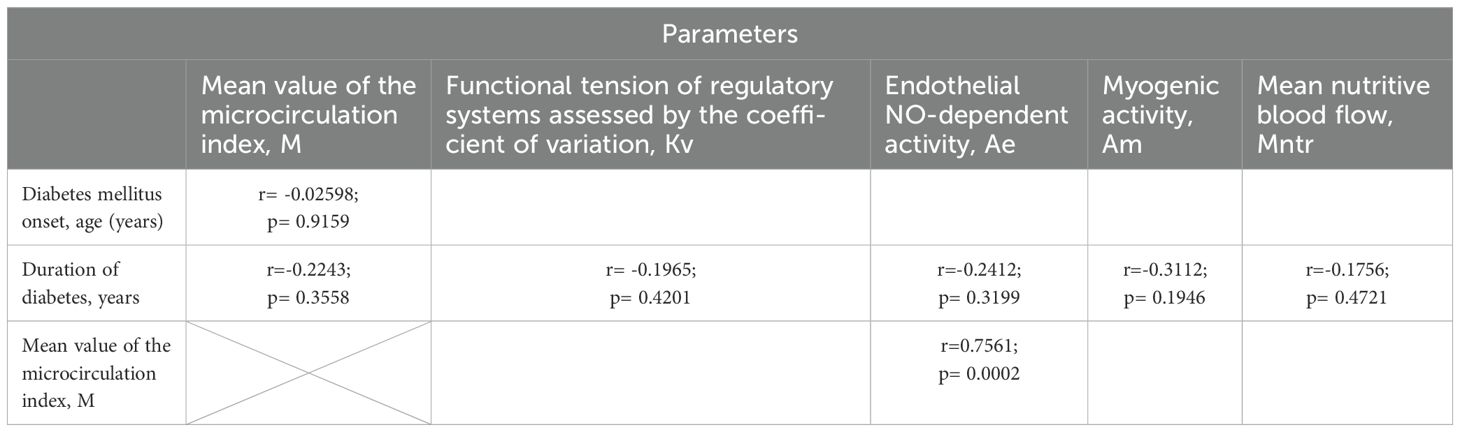
The analysis of correlation relationships between microcirculation parameters and clinical characteristics of patients with diabetes mellitus in the study group revealed the following results in Table 4.
The analysis of the correlation relationships between microcirculation parameters and clinical characteristics in patients with T2DM revealed several notable findings. No significant correlations were found between the age of diabetes onset and parameters of microcirculation, regulatory systems, or endothelial activity (r = –0.02598; p = 0.9159), indicating that the age at which the disease begins does not have a meaningful impact on these physiological markers. Furthermore, the duration of diabetes was not significantly associated with key microvascular indicators, including the mean microcirculation index (r = –0.2243; p = 0.3558), functional tension of regulatory systems (Kv) (r = –0.1965; p = 0.4201), endothelial NO-dependent activity (Ae) (r = –0.2412; p = 0.3199), myogenic activity (Am) (r = –0.3112; p = 0.1946), or nutritive blood flow (Mntr) (r = –0.1756; p = 0.4721). These weak and statistically non-significant relationships suggest that disease duration is not a primary determinant of microcirculatory changes in this cohort. In contrast, a strong positive correlation was observed between the mean microcirculation index (M) and the functional tension of regulatory systems (Kv), with r = 0.7561 and p = 0.0002. This indicates that increased microcirculatory activity is associated with a significant rise in regulatory load, likely reflecting compensatory adaptation mechanisms within the microvascular network in response to chronic vascular stress.
Discussion
Laser Doppler flowmetry is a state-of-the-art non-invasive method for studying microcirculation that finds applications across various medical specialties (11–13). This technique is utilized to evaluate skin microcirculation and has demonstrated clinical efficacy in rheumatology, dermatology, surgery and diabetology. In surgical practice, LDF aids in evaluating the severity of burns and facilitates decision-making regarding the initiation of therapy. The method is also effective for monitoring wound healing, including postoperative wounds. In rheumatology, LDF is employed for diagnosing conditions such as Raynaud’s phenomenon and systemic scleroderma. In dermatology, it is used to assess the severity of psoriasis and to evaluate treatment efficacy.
LDF holds particular value in diagnosing microcirculatory disturbances in patients with type 1 and type 2 diabetes mellitus (14, 15). This method is indispensable for this patient group because pathological changes in microcirculation occur earlier than the development of severe microangiopathic lesions. Timely detection of such changes allows for the implementation of preventive measures or the adaptation of therapy aimed at reducing the impact of hyperglycemia on the vasculature (16). Early intervention helps reduce the risk of progression of microvascular complications, prevent systemic consequences of diabetes, and significantly improve patients’ quality of life. Early diagnostic methods, such as LDF, enable the assessment of vascular responses to therapy, timely modification of treatment strategies, and ongoing monitoring of treatment efficacy (16). Considering its versatility, non-invasiveness and high sensitivity, LDF holds promise to become a standard tool for early diagnosis and monitoring of microcirculatory status across various clinical specialties, particularly in patients with diabetes mellitus (10, 12, 13).
Limitations
The primary limitation of this study is the small sample size, which may restrict the generalizability of the findings. Additionally, the cross-sectional design limits the ability to establish causality between microcirculatory changes and diabetes complications. Longitudinal studies with larger cohorts are needed to validate these findings and assess long-term outcomes.
Conclusions
T2DM is associated with significant alterations in the microcirculatory bed, including endothelial dysfunction, increased sympathetic nervous system activity and elevated oxidative stress. LDF1 is an effective non-invasive method for assessing the state of microcirculation. This technique enables real-time evaluation of tissue perfusion, regulatory mechanisms, and the functional status of vascular tone. Patients with T2DM exhibit enhanced compensatory mechanisms of blood flow regulation, such as increased myogenic activity, indicating adaptive processes in response to chronic microvascular damage. LDF detects preclinical microcirculatory changes, notably decreased endothelial activity (Ae) and increased sympathetic adrenergic activity (An), reflecting impaired regulation of the vascular bed. The findings emphasize the necessity of early monitoring of microcirculatory status in patients with T2DM for timely detection of complications such as neuropathy, angiopathy, and retinopathy, as well as for therapy adjustment. LDF holds promise as a standard tool for the diagnosis and monitoring of microvascular lesions in chronic endocrine disorders, including diabetes mellitus.
Data availability statement
The datasets presented in this article are not readily available because The dataset is anonymized and available upon reasonable request. It may not be used for commercial purposes without prior permission. Any reuse should cite the original article. No personally identifiable information is included. Requests to access the datasets should be directed to emxhdGFsaWdvbmVua29AZ21haWwuY29t.
Ethics statement
The studies involving humans were approved by Biomedical Ethics Committee of Poltava State Medical University, Poltava, Ukraine. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
ZS: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, and/or publication of this article.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor declared a past co-authorship with one of the authors ZS.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Li X, Wu L, Yang Z, Hu Y, Zhou C, Ji R, et al. Assessment of microcirculation in the type 2 diabetic and impaired glucose tolerance feet of elderly men by CEUS. Diabetes Metab Syndr Obes Targets Ther. (2021) 14:3647–52. doi: 10.2147/DMSO.S314727
2. Caballero AE. Microvascular and macrovascular complications in diabetes mellitus: distinct or continuum? G Ital Cardiol (Rome). (2017) 18:15–25. doi: 10.1714/2614.26988
3. Roden M and Shulman GI. The integrative biology of type 2 diabetes. Nature. (2019) 576:51–60. doi: 10.1038/s41586-019-1797-8
4. Kobyliak N, Abenavoli L, Mykhalchyshyn G, Falalyeyeva T, Tsyryuk O, Kononenko L, et al. Probiotics and smectite absorbent gel formulation reduce liver stiffness, transaminases and cytokine levels in NAFLD associated with type 2 diabetes: a randomized clinical study. Clin Diabetol. (2019) 8:205–14. doi: 10.5603/DK.2019.0016
5. Korotkyi O, Vovk A, Galenova T, Vovk T, Dvorschenko K, Luzza F, et al. Effect of probiotic on serum cytokines and matrix metalloproteinases profiles during monoiodoacetate-induced osteoarthritis in rats. Minerva Biotecnol. (2019) 31:68–73. doi: 10.23736/S1120-4826.19.02548-5
6. Pop-Busui R, Boulton AJ, Feldman EL, Bril V, Freeman R, Malik RA, et al. Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care. (2017) 40:136–54. doi: 10.2337/dc16-2042
7. Roustit M and Cracowski JL. Assessment of endothelial and neurovascular function in human skin microcirculation. Trends Pharmacol Sci. (2013) 34:373–84. doi: 10.1016/j.tips.2013.05.007
8. Kostenko V, Akimov O, Gutnik O, Kostenko H, Kostenko V, Romantseva T, et al. Modulation of redox-sensitive transcription factors with polyphenols as pathogenetically grounded approach in therapy of systemic inflammatory response. Heliyon. (2023) 9:e15551. doi: 10.1016/j.heliyon.2023.e15551
9. Makmatov-Rys MB, Chursinova YuV, Kulikov DA, Raznitsyna IA, Andreeva VV, Gerzhik AA, et al. Pilot study of laser fluorescence spectroscopy and optical oximetry in the diagnosis and assessment of scar lesions. Klin Dermatol Venerol. (2020) 19(4):506–13. doi: 10.17116/klinderma202019041506
10. Mrowietz C, Franke RP, Pindur G, Wolf U, and Jung F. Reference range and variability of laser-Doppler-fluxmetry. Clin Hemorheol Microcirc. (2017) 1:347–53. doi: 10.3233/CH-179215
11. Neubauer-Geryk J, Hoffmann M, Wielicka M, Piec K, Kozera G, Brzeziński M, et al. Current methods for the assessment of skin microcirculation: Part 1. Postepy Dermatol Alergol. (2019) 36:247–54. doi: 10.5114/ada.2019.83656
12. Shaienko ZO and Lihonenko OV. Perspectives of using laser Doppler flowmetry for the assessment of skin microcirculation in diabetes mellitus. Int Endocrinol J (Ukraine). (2021) 17:613–8. doi: 10.22141/2224-0721.17.8.2021.246793
13. Shaienko ZO. Laser Doppler flowmetry as the advanced non-invasive method of evaluation of microcirculation status in patients with diabetes mellitus. Clin Endocrinol Endocr Surg. (2021) 76:44–50. doi: 10.30978/CEES-2021-4-44
14. Yelins’ka AM, Akimov OY, and Kostenko VO. Role of AP-1 transcriptional factor in development of oxidative and nitrosative stress in periodontal tissues during systemic inflammatory response. Ukr Biochem J. (2019) 91:80–5. doi: 10.15407/ubj91.01.080
15. Chekalina NI, Kazakov YM, Mamontova TV, Vesnina LE, and Kaidashev IP. Resveratrol more effectively than quercetin reduces endothelium degeneration and level of necrosis factor α in patients with coronary artery disease. Wiad Lek. (2016) 69:475–9.
16. Shayenko Z, Akimov O, Neporada K, Ligonenko O, and Spivak M. The influence of nanodispersed cerium oxide on the development of oxidative stress and the production of nitric oxide in the blood of patients with type 2 diabetes mellitus. Int J Endocrinol (Ukraine). (2023) 19:183–7. doi: 10.22141/2224-0721.19.3.2023.1269
Keywords: diabetes mellitus, microcirculation, laser doppler flowmetry, microvascular disorders, endothelial dysfunction
Citation: Shaienko ZO (2025) Microcirculatory disturbances in type 2 diabetes: early detection using laser doppler flowmetry for personalized care. Front. Endocrinol. 16:1651525. doi: 10.3389/fendo.2025.1651525
Received: 21 June 2025; Accepted: 24 July 2025;
Published: 25 September 2025.
Edited by:
Tetyana Falalyeyeva, Taras Shevchenko National University of Kyiv, UkraineReviewed by:
Maksym Zhaivoronok, P. L. Shupyk National University of Health Care of Ukraine, UkraineOleh Dynnyk, Institute of Elastography LLC, Ukraine
Copyright © 2025 Shaienko. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zlatoslava O. Shaienko, WmxhdGFsaWdvbmVua29AZ21haWwuY29t
†ORCID: Zlatoslava O. Shaienko, orcid.org/0000-0002-8718-7589
 Zlatoslava O. Shaienko
Zlatoslava O. Shaienko