- 1Multidisciplinary Research Unit, Government Medical College, Amritsar, Punjab, India
- 2Department of Ophthalmology, Georgetown University Medical Center, Washington DC, United States
- 3Department of Pharmacology, Government Medical College, Amritsar, Punjab, India
- 4Department of Pharmacology, Dr. Radhakrishnan Government Medical College, Hamirpur, Himachal Pradesh, India
- 5Ophthalmic Genetics and Visual Function Branch, National Eye Institute, National Institutes of Health, Bethesda, MD, United States
Background: Paraoxonases (PONs) are a unique family of calcium-dependent enzymes which are tightly associated with the high-density lipoprotein cholesterol (HDL-C), plays a crucial role in protecting the low-density lipoprotein cholesterol (LDL-C) from oxidation, thereby providing protection against atherosclerosis-a key factor for the pathogenesis of coronary artery disease (CAD). The activity of PON enzymes is influenced by genetic polymorphisms in the PON genes. The present case-control study was performed to investigate the association of PON1 (p.L55M, rs854560) and PON2 (p.S311C, rs7493) polymorphisms with CAD in the North Indian Punjabi population.
Methods and results: The present study included 211 CAD patients and 260 healthy controls genotyped using the polymerase chain reaction-reaction fragment length polymorphism (PCR-RFLP) technique. Binary logistic regression analysis revealed that the SC and CC genotypes of the PON2 (p.S311C) conferred 2-and 3.5-folds increased risk for CAD (OR: 2.03, 95%CI: 1.36-3.01, p=0.001; OR: 3.49, 95%CI: 1.86-6.55, p=0.001, respectively). Moreover, the dominant (OR: 2.29, 95%CI: 1.58-3.32, p=0.0001), co-dominant (OR: 1.62, 95%CI: 1.11-2.36, p=0.012), recessive (OR: 2.58, 95%CI: 1.41-4.72, p=0.001), and log-additive (OR: 1.92, 95%CI: 1.46-2.54, p=0.0001) are the best-fit inheritance models to predict the susceptible gene effects. Furthermore, the LC haplotype (PON1 and PON2) was found to be significantly and independently associated with the increased risk of CAD (OR: 2.34, 95%CI: 1.65-3.32, p=0.0001).
Conclusions: Our results indicate a significant and independent association of PON2 (p.S311C) polymorphism with CAD even after gender stratification in North Indian Punjabi population.
Introduction
Coronary artery disease (CAD) is a widespread and complex condition with a multifactorial etiology, where both genetic predispositions and environmental influences, along with their interactions, are critical in its pathogenesis (1). It is one of the leading causes of both morbidity and mortality globally (2). Cardiovascular diseases (CVDs) account for 31% of global deaths, with CAD responsible for approximately 7.4 million of these fatalities (3). Individuals from the South Asian subcontinent experience a higher mortality rate from CAD compared to other ethnic groups (4). The primary traditional risk factors for CAD include lipid abnormalities, diabetes, hypertension, smoking, obesity, gender, advanced age, and a family history of the disease (5). Additionally, oxidative modification of low-density lipoprotein cholesterol (LDL-C) is crucial in the formation of atherosclerotic plaques, which contributes to the onset and progression of CAD (5). Conversely, high-density lipoprotein cholesterol (HDL-C) provides a protective effect against atherosclerosis by preventing LDL oxidation (6), and is inversely related to CAD development (7). The protective role of HDL-C is attributed to its associated enzymes, such as paraoxonase (PON), platelet-activating factor acetylhydrolase, and lecithin-cholesterol acyltransferase, with PON being the most extensively studied (8). Paraoxonases (PONs) are a distinct group of calcium-dependent hydrolases and esterases located on the HDL surface that protect LDL from oxidation and possess antiatherogenic, antioxidative, and anti-inflammatory properties (9). PON activity is notably affected by genetic polymorphisms, making PON variants potential biomarkers for CAD due to their influence on LDL oxidation (10).
The paraoxonase (PON) gene family comprises PON1, PON2, and PON3, located on the long arm of chromosome 7 (7q21.3-q22.1) (11). Among these, PON1 is a key susceptibility gene involved in vascular pathology and is considered a promising biomarker for CAD. It is a 44-kDa glycoprotein enzyme that depends on calcium and is primarily produced in the liver, where it associates with the surface of high-density lipoproteins. In the bloodstream, PON1, which is predominantly linked to HDL, inhibits LDL oxidation, promotes cellular cholesterol efflux from macrophages (12), and reduces lipid peroxides within atherosclerotic plaques (13). PON1 exhibits several polymorphisms (14), with the p.L55M (rs854560) variant being particularly well-studied across different ethnic groups for its impact on CAD susceptibility (15). The leucine-to-methionine substitution at codon 55 (p.L55M) results in reduced stability and has been linked to decreased PON1 levels and activity (16). Lower PON1 activity contributes to the initiation and progression of atherosclerotic plaques and exacerbates the severity of related atherosclerosis-related conditions (17).
Human paraoxonase 2 (PON2) is a member of the paraoxonase gene family, known for its distinct anti-oxidative and anti-atherosclerotic properties. PON2 is an intracellular protein that is ubiquitously expressed, particularly in the human heart, endothelial cells, and aortic smooth muscle cells (18). It plays a critical role in preventing LDL oxidation, reversing the oxidation of mildly oxidized LDL, and protecting against atherosclerosis (19). Moreover, PON2 expression in macrophages increases under oxidative stress, suggesting that PON2 may serve as a selective antioxidant at the cellular level, thereby playing an anti-atherogenic role by reducing macrophage foam cell formation and oxidative stress (20). Additionally, PON2’s anti-apoptotic function contributes significantly to atherosclerotic protection (21). Given its role in preventing LDL oxidation, similar to PON1, PON2 has become a focus of extensive research to understand its contribution to CAD susceptibility across different ethnic groups. Various polymorphisms in PON2 have been studied in relation to different diseases. Among them, the p.S311C (rs7493) polymorphism has been widely investigated for its association with CAD development across many ethnic populations, where it is considered an important risk factor for CAD (9, 22–25). Notably, no studies from India have yet reported an association between the PON2 (p.S311C) polymorphism and CAD. The substitution of serine to cysteine at codon 311 (p.S311C) in PON2 (26) results in decreased enzyme activity, thereby reducing the protection of LDL from oxidation (27). Consequently, abnormal paraoxonase activity due to different genotypes may contribute to the higher incidence of CAD in individuals over 50 years of age (22). Population-based studies have shown inter-ethnic differences in allele frequencies for PON1 (p.L55M) and PON2 (p.S311C) polymorphisms. This variability indicates that ethnic differences, gene-gene interactions, and environmental susceptibility might influence the relationship between PON polymorphisms and CAD. These findings support the role of impaired PON1 activity in atherosclerosis and strengthen the rationale for investigating PON polymorphisms in CAD. Therefore, considering the significance of PON polymorphisms in CAD genetic susceptibility and the variation in allele frequencies among different ethnic groups, the present case-control study was designed. It aimed to explore the association of PON1 (p.L55M) and PON2 (p.S311C) polymorphisms with CAD in the North Indian Punjabi population.
Materials and methods
Patients and controls
The current study involved 211 patients diagnosed with CAD based on electrocardiographic (ECG) findings (such as ST-segment depression/elevation or T-wave inversions consistent with angina), echocardiographic alterations (including regional wall motion abnormalities or evidence of impaired left ventricular function consistent with ischemic heart disease), and positive results from treadmill testing (defined as ≥1 mm horizontal or downsloping ST-segment depression or elevation during exercise accompanied by typical anginal symptoms). These patients were recruited from the Government Medical College, Amritsar, with exclusions made for individuals with liver, lung, kidney, or thyroid disorders, as well as those with malignancies. The control group consisted of 260 healthy individuals from the general population, matched for age, sex, and ethnicity, with no current or past family history of CAD or other diseases. The study received approval from the Ethics Committee of Government Medical College, Amritsar, and adhered to the principles outlined in the Declaration of Helsinki. Clinical data, including age, gender, height, weight, body mass index (BMI), hip and waist circumference, and family history, were collected for all participants using a pre-designed proforma. All participants provided voluntary written informed consent. Blood pressure was measured using a mercury sphygmomanometer, following the American Heart Association’s standard procedures (28). A trained technician collected 5 ml of whole blood from each participant after an overnight fast, with 3 ml transferred into EDTA vials for DNA extraction and the remaining 2 ml into vials without anticoagulant for serum separation. Biochemical parameters, including total cholesterol (TC), triglycerides (TG), and high-density lipoprotein cholesterol, were measured using a semi-automated biochemical analyzer (Erba Chem-7) with commercially available kits (Erba). Low-density lipoprotein cholesterol and very-low-density lipoprotein cholesterol (VLDL-C) levels were calculated using Friedewald’s formula (29).
Genotyping
DNA was extracted from peripheral blood leukocytes using the phenol-chloroform method (30). Genotyping of the PON1 (p.L55M, rs854560) and PON2 (p.S311C, rs7493) variants was conducted through polymerase chain reaction-restriction fragment length polymorphism (PCR-RFLP). The primer sequences used were as follows: for PON1, forward: 5’-GAAGAGTGATGTATAGCCCCAG-3’ and reverse: 5’-ACACTCACAGAGCTAATGAAAGCC-3’; for PON2, forward: 5’-ACATGCATGTACGGTGGTCTTATA-3’ and reverse: 5’-AGCAATTCATAGATTAATTGTTA-3’. The PCR reactions were performed in a 15 µl total volume containing 50 ng of genomic DNA, 1.5 mM MgCl2, 0.2 mM of each dNTP, 10 μM of each primer, and 1 U of Taq DNA polymerase using a Mastercycler gradient thermal cycler (Eppendorf, Hamburg, Germany). The cycling conditions included an initial denaturation at 95°C for 5 minutes, followed by 35 cycles of denaturation at 95°C for 45 seconds, annealing at 52°C for PON1 (p.L55M) and 51°C for PON2 (p.S311C) for 45 seconds, extension at 72°C for 45 seconds, and a final extension at 72°C for 10 minutes. The amplified PCR products for PON1 (171 bp) and PON2 (265 bp) were digested with NlaIII and DdeI restriction enzymes (New England Biolabs, USA) respectively and then visualized on a 3% agarose gel stained with ethidium bromide. For the PON1 polymorphism, the undigested 171 bp fragment represents the L allele, while the 127 bp and 44 bp fragments correspond to the M allele. In the PON2 polymorphism, the 123 bp, 75 bp, and 67 bp fragments indicate the S allele, whereas the 142 bp and 123 bp fragments correspond to the C allele. To ensure genotyping accuracy, positive controls with known genotypes were included in each run, and 10% of samples per SNP were randomly re-genotyped to validate accuracy.
Statistical analysis
Data analyses were conducted using the Statistical Package for Social Sciences, version 31 (SPSS Inc., Chicago, IL, USA). Continuous variables were presented as mean ± standard deviation and analyzed using Student’s t-test. Categorical variables were reported as counts and percentages, with differences between categorical variables and genotype distributions assessed using the Chi-squared test with Yates correction. Comparisons of clinical and lipid parameters across different genotypes were performed using one-way ANOVA followed by Tukey’s post hoc test. Hardy-Weinberg equilibrium, haplotype analysis, and genetic models (dominant, co-dominant, recessive, and log-additive) were evaluated using SNPstats software. Binary logistic regression analysis was employed to calculate odds ratios (ORs) and 95% confidence intervals (CIs) for different PON1 (p.L55M) and PON2 (p.S311C) genotypes to assess CAD risk, both before and after adjusting for potential covariates such as age, gender, BMI, waist circumference, hypertension, and alcohol consumption. Power calculations were performed using the CaTS-Power Calculator (31) with the study achieving a statistical power of 90% at a significance level of 0.05 to detect an association with an OR of 1.5. A p-value of <0.05 was considered statistically significant, and for multiple comparisons, p-values were adjusted using the Bonferroni correction.
Results
Baseline characteristics of the study population
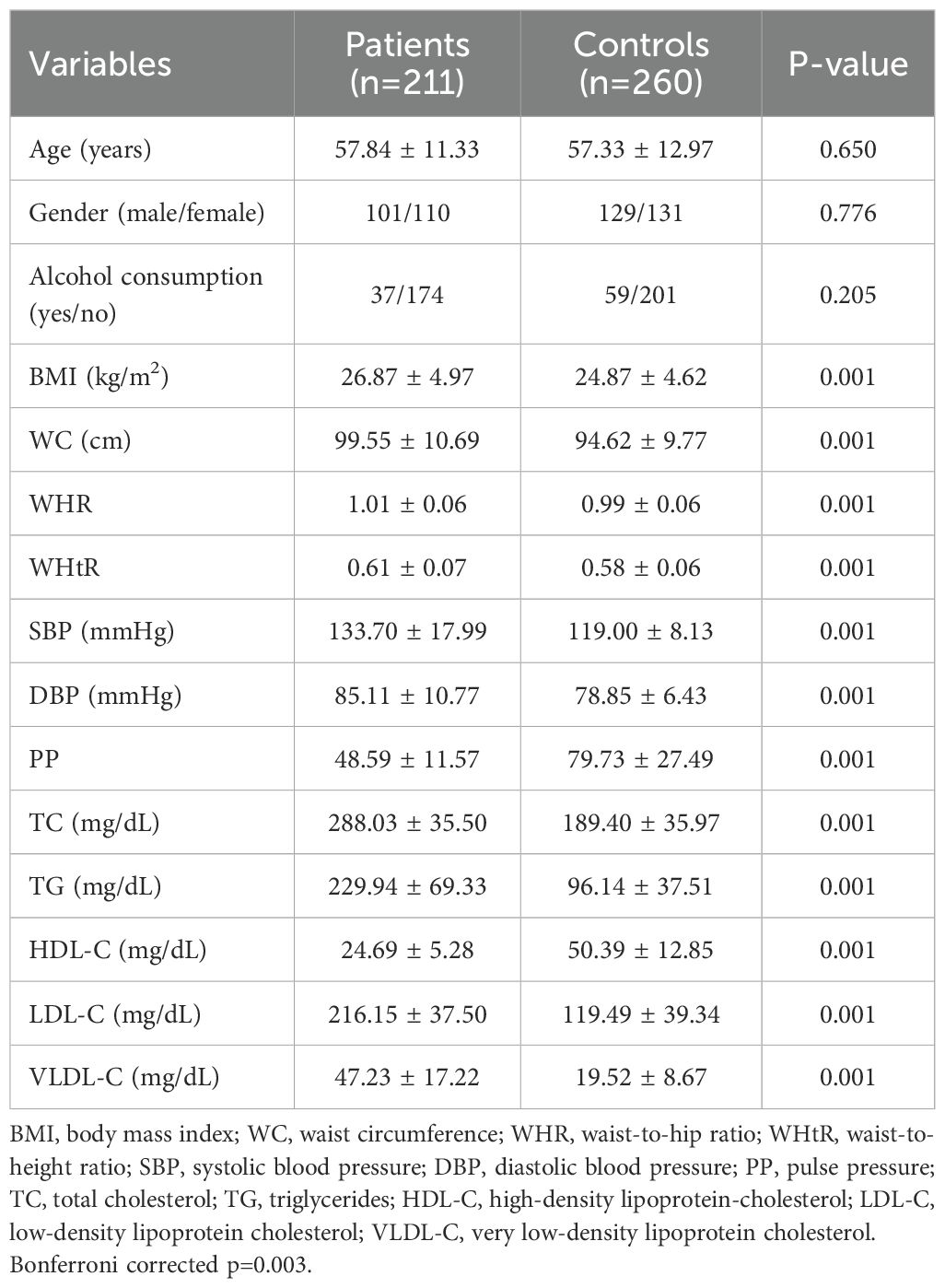
The baseline characteristics of the CAD patients and controls are shown in Table 1. CAD patients have significantly (p=0.001) higher values for BMI, waist circumference (WC), waist-hip ratio (WHR), waist-height ratio (WHtR), systolic blood pressure (SBP), and diastolic blood pressure (DBP) compared to healthy controls. Moreover, lipid levels (TC, TG, LDL-C, VLDL-C) were significantly (p=0.001) higher, while pulse pressure (PP) and HDL-C levels were significantly (p=0.001) lower in CAD patients than in controls. Gender-specific analysis shows that all variables, except for WHR in males were significantly (p=0.001) higher in CAD patients, with PP and HDL-C being significantly (p=0.001) lower in both male and female patients compared to their respective controls (Supplementary Table 1).
Genotype distribution in CAD patients and healthy controls
The genotype and allele frequency distributions of PON1 (p.L55M) and PON2 (p.S311C) polymorphisms are detailed in Table 2. The genotype distribution of PON1 and PON2 polymorphisms in both cases and controls were in agreement with those predicted by the Hardy-Weinberg equilibrium (p<0.05). The frequencies of SC and CC genotypes of PON2 (p.S311C) were significantly (p=0.0001) higher in CAD patients (43.1%, 16.1%) than in controls (31.9%, 6.9%), respectively. The C allele was observed to be more frequent in patients (37.7%) than in controls (22.9%). After gender stratification, the frequencies of SC and CC genotypes were observed to be significantly higher in male (43.6%, 18.8%) and female (42.7%, 13.6%) patients compared to their respective controls (34.9%, 7.7%) and (29%, 6.1%). The C allele was also more common in male and female patients (40.6%, 35%) than in corresponding controls (25.2%, 20.6%) (Supplementary Table 2). However, the genotype and allele distributions of PON1 (p.L55M) were not statistically significant in total (p=0.641, p=0.601) (Table 2) or when stratified by gender (0.907, p=0.915 in males), and (p=0.442, p=0.601 in females) (Supplementary Table 2). All observed associations remained persistent even after Bonferroni correction (p=0.025). This lack of association suggests that the PON1 (p.L55M) polymorphism may not play a major role in CAD susceptibility in the North Indian Punjabi population. It also highlights the potential influence of ethnic and genetic heterogeneity on the contribution of PON1 variants to CAD risk.

Table 2. Genotype and allele distributions of PON1 (L55M) and PON2 (S311C) polymorphisms in the study participants.
Association between PON polymorphisms and CAD
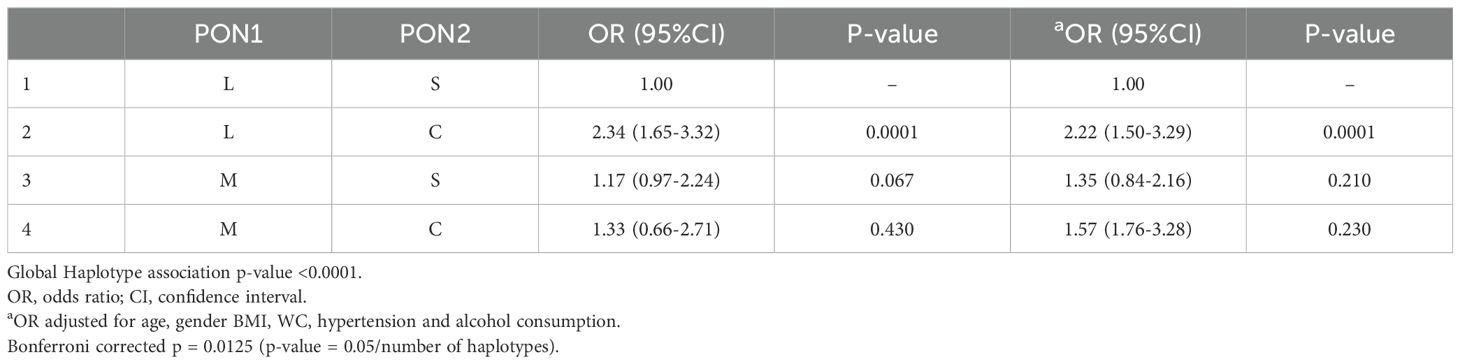
The association results of PON1 and PON2 polymorphisms are presented in Table 3. Binary logistic regression analysis revealed that the SC and CC genotypes of PON2 polymorphism exhibited 2-and 3.5-folds increased risk for CAD susceptibility (OR: 2.03, 95%CI: 1.36-3.01, p=0.001; OR: 3.49, 95%CI: 1.86-6.55, p=0.001, respectively). Even after adjusting for potential covariates such as age, gender, BMI, WC, hypertension and alcohol consumption, the SC and CC genotypes continued to demonstrate a 1.9-and 3.7-folds increased risk for CAD (OR: 1.96, 95%CI: 1.25-3.08, p=0.004; OR: 3.68, 95%CI: 1.84-7.33, p=0.001, respectively). In addition, the dominant (OR: 2.29, 95%CI: 1.58-3.32, p=0.0001), co-dominant (OR: 1.62, 95%CI: 1.11-2.36, p=0.012), recessive (OR: 2.58, 95%CI: 1.41-4.72, p=0.001), and log-additive (OR: 1.92, 95%CI: 1.46-2.54, p=0.0001) models have also shown significant association with the increased risk for CAD. These associations remained significant even after adjustment, the dominant (OR: 2.26, 95%CI: 1.48-3.45, p=0.0001), co-dominant (OR: 1.53, 95%CI: 1.00-2.23, p=0.051), recessive (OR: 2.75, 95%CI: 1.42-5.31, p=0.002), and log-additive (OR: 1.93, 95%CI: 1.42-2.63, p=0.0001).
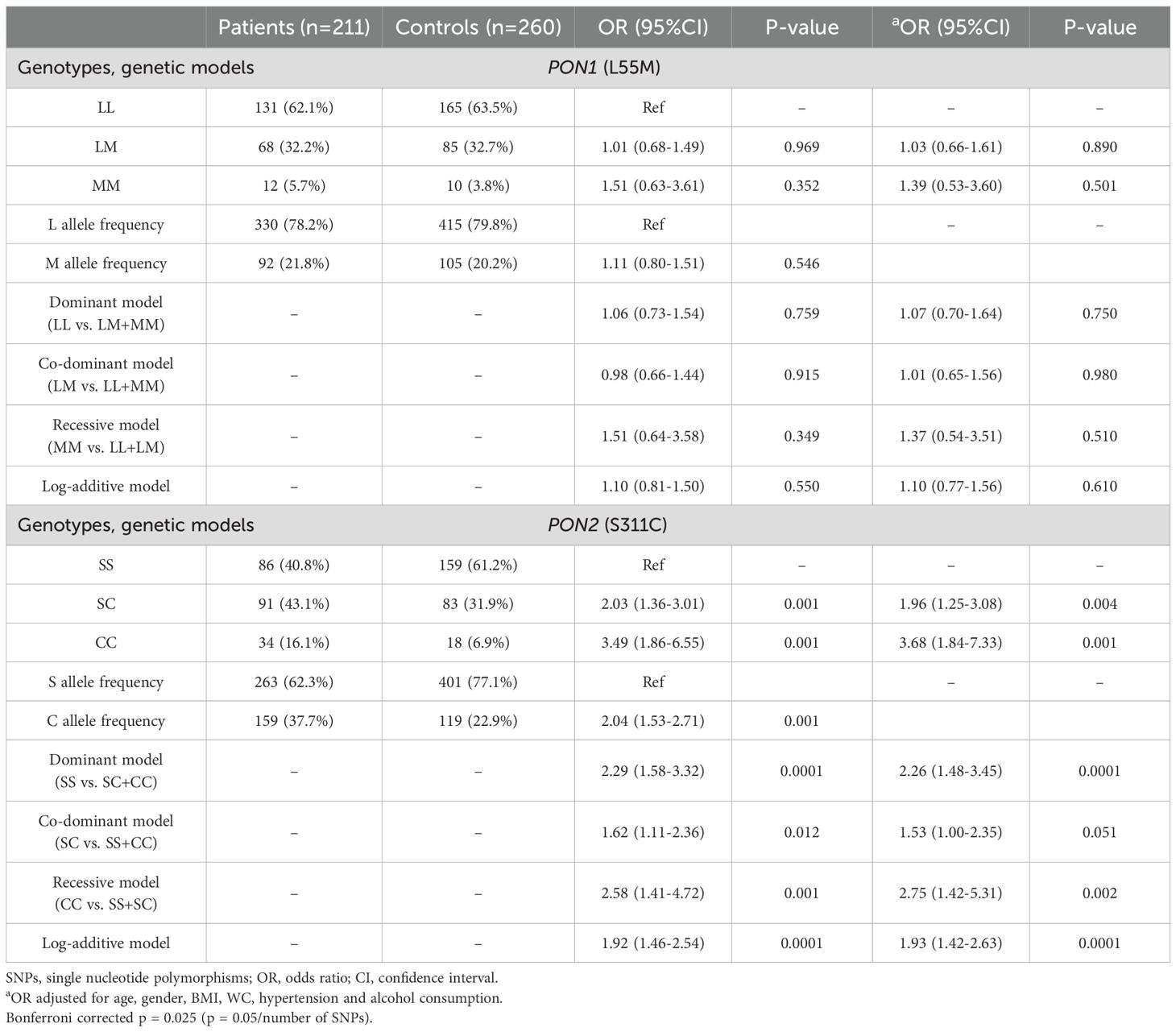
Table 3. Logistic regression analysis between PON1 (L55M) and PON2 (S311C) polymorphisms and CAD risk in the study participants.
On gender stratification, the SC (OR: 1.90, 95%CI: 1.08-3.37, p=0.027) and CC (OR: 3.70, 95%CI: 1.57-8.74, p=0.003) genotypes showed 1.9-and 3.7-folds increased risk for CAD in males and after adjustment, the SC genotype lost its risk (OR: 1.60, 95%CI: 0.84-3.04, p=0.151) while the CC genotype continued to exhibit a 3.9-fold increased risk for CAD (OR: 3.93, 95%CI: 1.51-10.22, p=0.005). Moreover, the dominant (OR: 2.23, 95%CI: 1.31-3.80, p=0.003), recessive (OR: 2.76, 95%CI: 1.22-6.23, p=0.012), and log-additive (OR: 1.92, 95%CI: 1.30-2.83, p=0.0008) models have also indicated increased risk for CAD. After adjustment, the dominant (OR: 1.98, 95%CI: 1.09-3.59, p=0.023), recessive (OR: 3.19, 95%CI: 1.29-7.91, p=0.011), and log-additive (OR: 1.86, 95%CI: 1.21-2.87, p=0.004) models continued to show significant and independent associations with the increased risk for CAD (Supplementary Table 3). Similarly, the SC and CC genotypes exhibited 2.2-and 3.3-folds increased risk for CAD in females (OR: 2.19, 95%CI: 1.26-3.82, p=0.006; OR: 3.32, 95%CI: 1.31-8.40, p=0.011, respectively) and after adjustment, the risk increased 2.5-fold for the SC genotype (OR: 2.52, 95%CI: 1.32-4.82, p=0.005) and 4.1-folds for the CC genotype (OR: 4.10, 95%CI: 1.46-11.55, p=0.008). In addition, the dominant (OR: 2.39, 95%CI: 1.42-4.02, p=0.0009), co-dominant (OR: 1.83, 95%CI: 1.07-3.11, p=0.026), recessive (OR: 2.43, 95%CI: 0.99-5.96, p=0.047), and log-additive (OR: 1.96, 95%CI: 1.31-2.96, p=0.0007) models also indicated an increased risk for CAD. After adjustment, these models continued to show significant and independent associations with the increased risk of CAD, the dominant (OR: 2.79, 95%CI: 1.03-7.50, p=0.042), co-dominant (OR: 1.99, 95%CI: 1.08-3.68, p=0.028), recessive (OR: 2.78, 95%CI: 1.03-7.50, p=0.028), and log-additive (OR: 2.19, 95%CI: 1.38-3.46, p=0.0006) (Supplementary Table 4). There were no differences in statistical significance even after the Bonferroni correction (p=0.025).
Clinical characteristics of the study participants stratified by genotypes
The clinical characteristics of the study participants stratified according to different genotypes of PON1 (p.L55M) and PON2 (p.S311C) are shown in Table 4. No significant differences for clinical variables were found among different genotypes, neither in the total group nor after gender stratification (Supplementary Tables 5, 6).
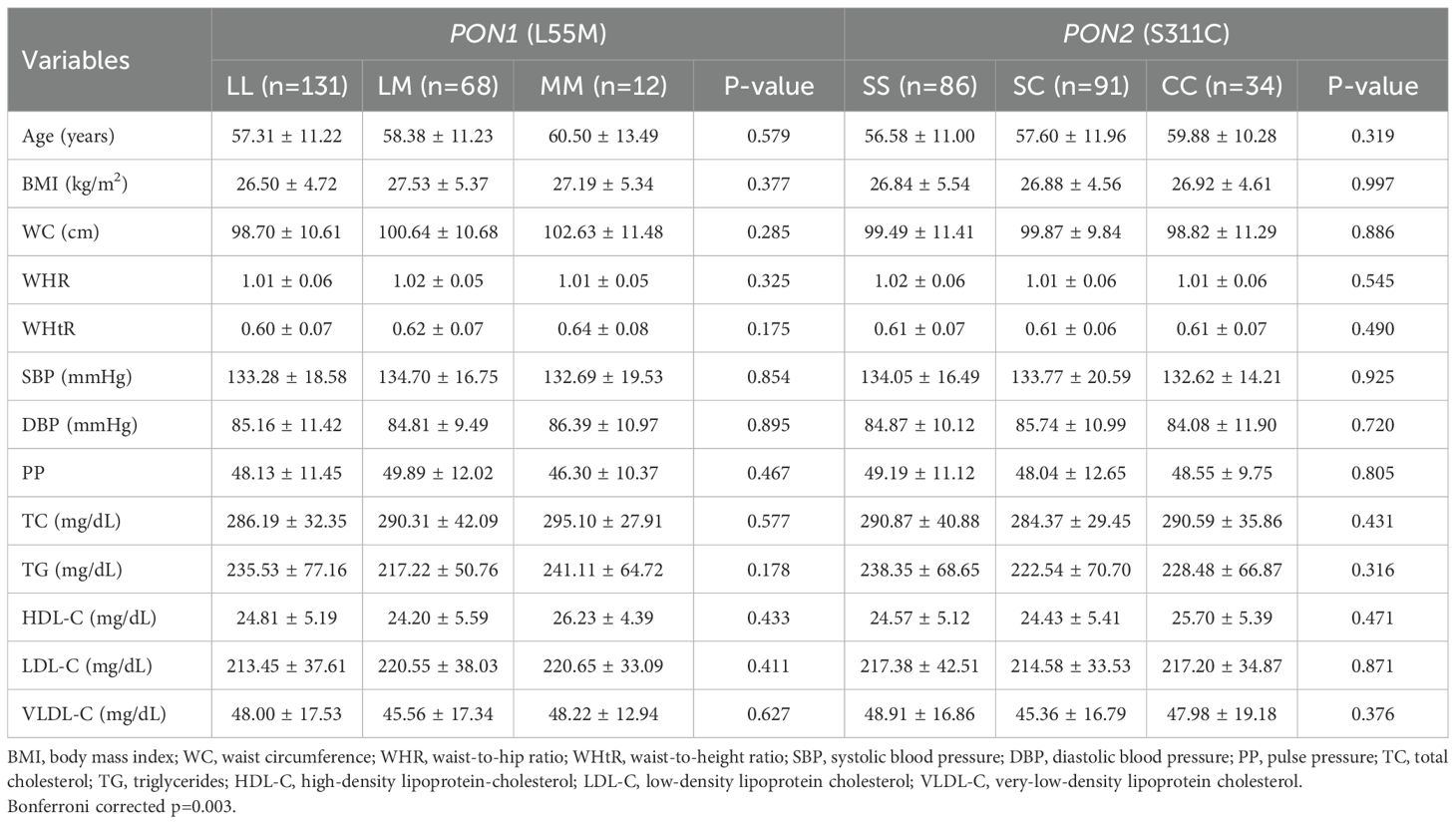
Table 4. Distribution of clinical parameters in different genotypes of PON1 (L55M) and PON2 (S311C) in the study participants.
Linkage disequilibrium and haplotype analysis
The PON1 (p.L55M) and PON2 (p.S311C) SNPs were not in LD in the total group (Figure 1A) or after gender stratification (Figures 1B, C) despite being located within the same gene cluster. Haplotype analysis (Table 5) revealed that the LC haplotype showed a 2.3-fold increased risk for CAD (OR: 2.34, 95%CI: 1.65-3.32, p=0.0001) and after adjustment, this risk remained at 2.2-fold (OR: 2.22, 95%CI: 1.50-3.29, p=0.0001). Gender-specific analysis showed that the LC haplotype conferred a 2.5-fold increased risk for CAD in males (OR: 2.52, 95% CI: 1.54-4.13, p=0.0003) and a 2.2-fold increased risk in females (OR: 2.22, 95% CI: 1.34-3.67, p=0.002) (Supplementary Table 7). After adjustment, the risk remained significant, with a 2.2-fold increase in males (OR: 2.21, 95% CI: 1.29-3.80, p=0.004) and a 2.4-fold increase in females (OR: 2.41, 95% CI: 1.36-4.27, p=0.003). The associations remained persistent after the Bonferroni correction (p=0.0125).
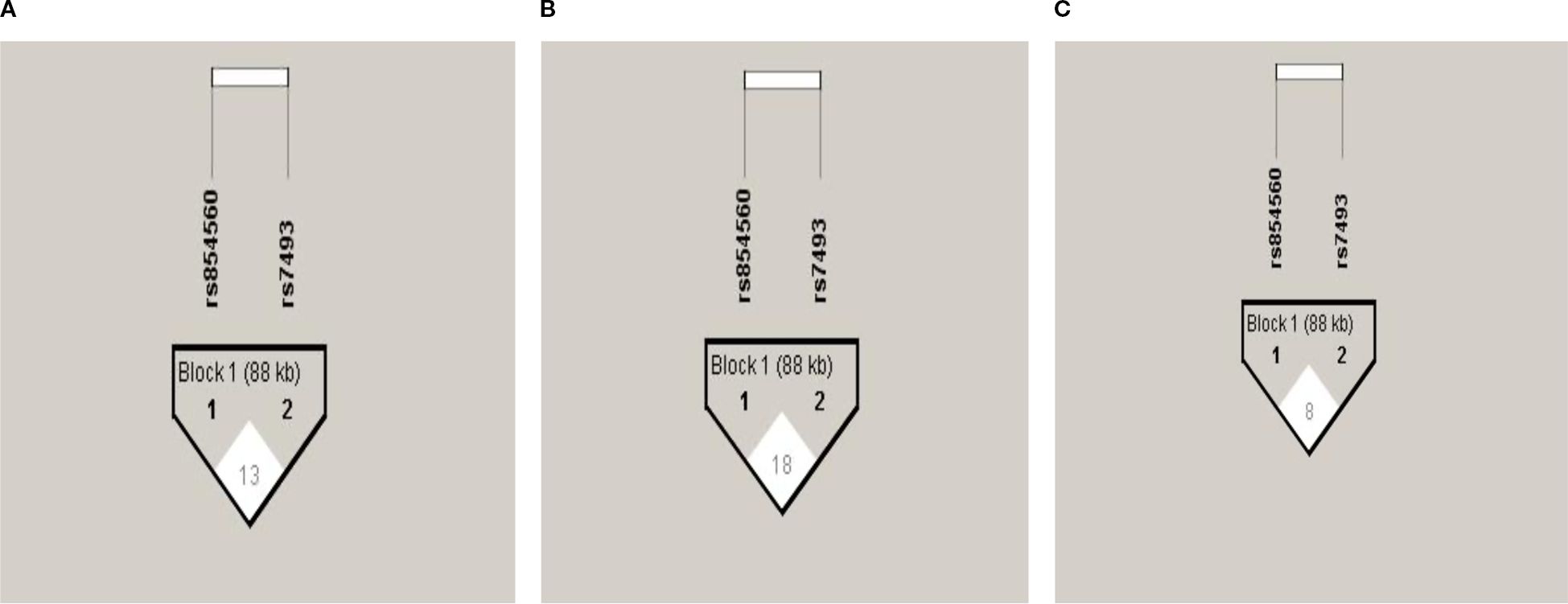
Figure 1. Pair-wise Linkage disequilibrium plot of PON1 (p.L55M) and PON2 (p.S311C) SNPs in the total group (A), males (B), and females (C). The hatch marks contain D’ values multiplied by 100 to indicate the strength of LD between the SNPs.
Discussion
Genetic susceptibility to CAD is influenced by the involvement of numerous genes that participate in metabolic pathways related to the pathogenesis and progression of atherosclerosis (32). Among these, the genes encoding paraoxonase-1 (PON1) and paraoxonase-2 (PON2) have been identified as contributing to genetic susceptibility to CAD. Polymorphisms in PON1 (p.L55M) and PON2 (p.S311C) are known to affect PON activity. Various studies have explored the association between these polymorphisms and their impact on CAD risk (33). In vivo animal studies have highlighted the anti-atherogenic properties of PON1 and PON2. Tward et al. (34) demonstrated that transgenic mice with elevated expression of the human PON1 gene produce high-density lipoproteins with enhanced anti-oxidative properties, offering protection against atherosclerosis compared to wild-type mice. Additionally, PON1-deficient mice have been found to have an increased risk of developing atherosclerosis compared to their wild-type counterparts (35). Similarly, PON2 has been shown to protect against low-density lipoprotein oxidation and inhibit monocyte transmigration in response to LDL oxidation in PON2-knockout mice (19). Interestingly, these PON2-knockout mice exhibit an increased number of foam cells and lipid droplets, along with significantly larger atherosclerotic lesions compared to wild-type mice (36). Previous studies indicate that PON2 can mitigate atherogenesis and reduce atherosclerotic lesions (37). These findings suggest that PON1 and PON2 polymorphisms may play a role in modulating atherogenesis, a critical factor in the initiation and progression of CAD. Consequently, we conducted a case-control study to investigate the association between PON1 (p.L55M) and PON2 (p.S311C) polymorphisms and CAD in the North Indian Punjabi population.
In this cohort, there was a statistically significant difference in the genotypic distribution of the PON2 (p.S311C) polymorphism between CAD patients and controls (p=0.0001), with a higher prevalence of the CC genotype in CAD patients (16.1%) compared to controls (6.9%). The SC and CC genotypes were associated with a 2-fold and 3.5-fold increased risk of developing CAD, respectively. After adjusting for potential confounding factors, the SC genotype remained associated with a 2-fold increased risk, while the CC genotype conferred a 3.7-fold increased risk. These findings indicate that the (p.S311C) polymorphism is significantly and independently linked to an elevated risk of CAD in the North Indian Punjabi population. When stratified by gender, the SC and CC genotypes were found to increase CAD risk by 1.9-fold and 3.7-fold in males, and by 2.2-fold and 3.3-fold in females, respectively, suggesting that both males and females carrying the 311Cys allele are more susceptible to developing CAD. These findings align with those of Jalilian et al. (38) and Ding et al. (17), who reported a significant association between the 311Cys allele and CAD in Iranian and Taiwanese populations, respectively. Additionally, Elnoamany et al. (24) documented the association of the 311Cys allele with CAD in the Egyptian population. In line with our findings, a recent study from a Polish cohort demonstrated that the PON2 311S allele was independently associated with a higher risk of complex type C coronary lesions, highlighting its potential role in lesion severity and CAD progression (39). However, our results differ from those of Sanghera et al. (22) and Pan et al. (9) who found an association between the 311Ser allele and CAD in Asian Indians (Singapore) and Taiwanese populations. Guxens et al. (23) also reported an association between the 311Ser allele and acute myocardial infarction in a Spanish population. Furthermore, studies in other ethnic groups, including Japanese, Brazilian, and Polish populations, have shown no association between the PON2 (p.S311C) polymorphism and CAD (40–42).
For the PON1 (p.L55M) polymorphism, no significant differences were observed in the genotype and allele frequency distributions between CAD cases and controls (p=0.641; p=0.601, respectively). Our findings are consistent with those of Munshi et al. (33), Aruljothi et al. (43), and Godbole et al. (44) who also reported no significant association between the PON1 (p.L55M) polymorphism and CAD in North and South Indian populations. Similarly, Gupta et al. (45) and Kaur et al. (46) found no significant association between the PON1 (L55M) polymorphism and CAD in North-West Indian Punjabis and Asian Indians, respectively. Other studies have also shown no association between the PON1 (p.L55M) polymorphism and CAD in North Indian, Turkish, South Indian and Polish populations (8, 39, 47, 48). A recent meta-analysis further supports the lack of a significant association between the PON1 (p.L55M) polymorphism and CAD (49). However, our results differ from those of Oliveira et al. (41) who identified a protective effect of the M allele of PON1 against CAD in a Brazilian population. Similarly, other studies reported a significant association between the PON1 (p.L55M) polymorphism and CAD in Australian, Turkish, Iranian and Bulgarian populations (15, 50–52). These discrepancies across different populations may be due to ethnic heterogeneity, population diversity, varying environmental and genetic backgrounds, differences in sample sizes, and diverse study designs (53). Additionally, association studies alone may not be sufficient to determine the role of specific SNPs, particularly in polymorphic genes where many SNPs are in LD.
In this study, we did not observe any significant differences in clinical parameters across different genotypes of PON1 (p.L55M) and PON2 (p.S311C) among CAD cases, including after gender-based analysis, consistent with previous findings (24, 46). Haplotype analysis revealed that the LC haplotype was significantly associated with an increased risk of developing CAD, even after adjusting for potential covariates. Furthermore, gender stratification indicated that the LS haplotype was linked to a higher risk for CAD in both males and females, both before and after adjustment. These findings suggest that PON2 modulates CAD risk independently and also synergistically with PON1 in the overall patient group, including when stratified by gender, in the North Indian Punjabi population. Previous studies have also suggested that PON2 may work synergistically with PON1 polymorphisms, independent of other risk factors (22).
In our cohort, the significant association of the PON2 (p.S311C) polymorphism with CAD suggests a possible genotype-phenotype correlation, as this variant has been implicated in modulating oxidative stress pathways that contribute to atherosclerotic progression. In contrast, the absence of association for the PON1 (p.L55M) polymorphism highlights the potential population-specific variability in genotype effects. Clinically, such findings underscore the importance of considering genetic diversity when assessing CAD risk and suggest that PON polymorphisms may serve as adjunctive markers for personalized risk stratification in the future.
The study entails some strengths and limitations. To the best of our knowledge, this is the first study that reported a significant and independent association of PON2 (p.S311C) polymorphism with CAD in the North Indian Punjabi population. The study also confirmed the interactive effect of PON2 and PON1 variants with CAD, implying that PON2 individually or in combination with PON1 plays a role in modulating CAD risk. However, there are some limitations to consider. The primary limitation was the small sample size, highlighting the need for more ethnic studies with larger sample sizes to confirm these results. Secondly, absence of enzyme activity measurements of PON1 and PON2 weakens the ability to directly establish the mechanistic link between genotype and phenotype. Hence, future studies integrating both genetic and functional analyses are necessary to better elucidate the biological role of these polymorphisms in CAD. Lastly, the study focused on only two SNPs, future research should analyze a broader range of SNPs together with functional characterization to better establish the role of these polymorphisms as risk factors for CAD.
Conclusion
The study reported a significant and independent association of PON2 (p.S311C) polymorphism with the increased risk of CAD in the North Indian Punjabi population even after being stratified by gender. To better understand the role of PON2 in CAD susceptibility, further research is needed across various ethnic populations, so that early preventive strategies could be initiated to manage and mitigate disease progression.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author/s.
Ethics statement
The study received approval from the Ethics Committee of Government Medical College, Amritsar, and adhered to the principles outlined in the Declaration of Helsinki. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
MB: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. JS: Conceptualization, Data curation, Supervision, Writing – original draft, Writing – review & editing. GL: Conceptualization, Data curation, Writing – original draft, Writing – review & editing. SG: Conceptualization, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, and/or publication of this article.
Acknowledgments
The authors are thankful to all the study participants for their cooperation and for providing valuable information.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2025.1688319/full#supplementary-material
Abbreviations
%, Percentage; °C, Degree celsius; BMI, Body mass index; Bp, Base pair; C, Cysteine; CAD, Coronary artery disease; CI, Confidence interval; CVD, Cardiovascular disease; DBP, Diastolic blood pressure; HDL-C, High-density lipoprotein cholesterol; kDa, Kilodaltons; L, Leucine; LD, Linkage disequilibrium; LDL-C, Low-density lipoprotein cholesterol; M, Methionine; min, Minute; mL, Milliliter; mM, Millimolar; OR, Odds ratio; PCR, Polymerase chain reaction; PONs, Paraoxonases; PON, Paraoxonase; PON1, Paraoxonase 1; PON2, Paraoxonase 2; PON3, Paraoxonase 3; PP, Pulse pressure; RFLP, Restriction fragment length polymorphism; S, Serine; SBP, Systolic blood pressure; sec, Second; TC, Total cholesterol; TG, Triglycerides; U, Unit; μl, Microliter; VLDL-C, Very-low-density lipoprotein cholesterol; WC, Waist circumference; WHR, Waist-hip ratio; WHtR, Waist-to-height ratio; µl, Microliter; µM, Micromolar; Ca2+, Calcium ion; ECG, Electrocardiogram; dNTPs, Deoxynucleotide triphosphates; MgCl2, Magnesium chloride; ANOVA, Analysis of variance; SNP, Single nucleotide polymorphisms; SPSS, Statistical package for social sciences.
References
1. Cooney MT, Dudina A, D’Agostino R, and Graham IM. Cardiovascular risk-estimation systems in primary prevention: do they differ? Do they make a difference? Can we see the future? Circulation. (2010) 122:300–10. doi: 10.1161/CIRCULATIONAHA.109.852756
2. Ahmed SW, Sultan FAT, Awan S, and Ahmed I. Prognostic significance of CMR findings in patients with known coronary artery disease - experience from a South Asian country. J Clin Imaging Sci. (2020) 10:75. doi: 10.25259/JCIS_153_2020
3. Shahid SU, Shabana NA, Rehman A, and Humphries S. GWAS implicated risk variants in different genes contribute additively to increase the risk of coronary artery disease (CAD) in the Pakistani subjects. Lipids Health Dis. (2018) 17:89. doi: 10.1186/s12944-018-0736-2
4. Goyal S and Sanghera DK. Genetic and non-genetic determinants of cardiovascular disease in South Asians. Curr Diabetes Rev. (2021) 17:e011721190373. doi: 10.2174/1573399817666210118103022
5. Iwanicka J, Iwanicki T, Niemiec P, Nowak T, Krauze J, Grzeszczak W, et al. Relationship between rs854560 PON1 gene polymorphism and tobacco smoking with coronary artery disease. Dis Markers. (2017) 2017:1540949. doi: 10.1155/2017/1540949
6. Marz W, Kleber ME, Scharnagl H, Speer T, Zewinger S, Ritsch A, et al. HDL cholesterol: reappraisal of its clinical relevance. Clin Res Cardiol. (2017) 106:663–75. doi: 10.1007/s00392-017-1106-1
7. Navab M, Reddy ST, Van Lenten BJ, and Fogelman AM. HDL and cardiovascular disease: atherogenic and atheroprotective mechanisms. Nat Rev Cardiol. (2011) 8:222–32. doi: 10.1038/nrcardio.2010.222
8. Lakshmy R, Ahmad D, Abraham RA, Sharma M, Vemparala K, Das S, et al. Paraoxonase gene Q192R & L55M polymorphisms in Indians with acute myocardial infarction & association with oxidized low density lipoprotein. Indian J Med Res. (2010) 131:522–9.
9. Pan JP, Lai ST, Chiang SC, Chou SC, and Chiang AN. The risk of coronary artery disease in population of Taiwan is associated with Cys-Ser 311 polymorphism of human paraoxonase (PON)-2 gene. Zhonghua Yi Xue Za Zhi (Taipei). (2002) 65:415–21.
10. Ombres D, Pannitteri G, Montali A, Candeloro A, Seccareccia F, Campagna F, et al. The gln-Arg192 polymorphism of human paraoxonase gene is not associated with coronary artery disease in italian patients. Arterioscler Thromb Vasc Biol. (1998) 18:1611–6. doi: 10.1161/01.ATV.18.10.1611
11. Humbert R, Adler DA, Disteche CM, Hassett C, Omiecinski CJ, and Furlong CE. The molecular basis of the human serum paraoxonase activity polymorphism. Nat Genet. (1993) 3:73–6. doi: 10.1038/ng0193-73
12. Kowalska K, Socha E, and Milnerowicz H. Review: The role of paraoxonase in cardiovascular diseases. Ann Clin Lab Sci. (2015) 45:226–33.
13. Deakin SP and James RW. Genetic and environmental factors modulating serum concentrations and activities of the antioxidant enzyme paraoxonase-1. Clin Sci (Lond). (2004) 107:435–47. doi: 10.1042/CS20040187
14. Richter RJ, Jarvik GP, and Furlong CE. Paraoxonase 1 status as a risk factor for disease or exposure. Adv Exp Med Biol. (2010) 660:29–35. doi: 10.1007/978-1-60761-350-3_4
15. Taskiran P, Cam SF, Sekuri C, Tuzun N, Alioglu E, Altintas N, et al. The relationship between paraoxanase gene Leu-Met (55) and Gln-Arg (192) polymorphisms and coronary artery disease. Turk Kardiyol Dern Ars. (2009) 37:473–8.
16. Mahrooz A and Mackness M. Epigenetics of paraoxonases. Curr Opin Lipidol. (2020) 31:200–5. doi: 10.1097/MOL.0000000000000687
17. Ding J, Chen Q, Zhuang X, Feng Z, Xu L, and Chen F. Low paraoxonase 1 arylesterase activity and high von Willebrand factor levels are associated with severe coronary atherosclerosis in patients with non-diabetic stable coronary artery disease. Med Sci Monit. (2014) 20:2421–9. doi: 10.12659/MSM.890911
18. Levy E, Trudel K, Bendayan M, Seidman E, Delvin E, Elchebly M, et al. Biological role, protein expression, subcellular localization, and oxidative stress response of paraoxonase 2 in the intestine of humans and rats. Am J Physiol Gastrointest Liver Physiol. (2007) 293:G1252–61. doi: 10.1152/ajpgi.00369.2007
19. Ng CJ, Bourquard N, Grijalva V, Hama S, Shih DM, Navab M, et al. Paraoxonase-2 deficiency aggravates atherosclerosis in mice despite lower apolipoprotein-B-containing lipoproteins: anti-atherogenic role for paraoxonase-2. J Biol Chem. (2006) 281:29491–500. doi: 10.1074/jbc.M605379200
20. Ng CJ, Wadleigh DJ, Gangopadhyay A, Hama S, Grijalva VR, Navab M, et al. Paraoxonase-2 is a ubiquitously expressed protein with antioxidant properties and is capable of preventing cell-mediated oxidative modification of low density lipoprotein. J Biol Chem. (2001) 276:44444–9. doi: 10.1074/jbc.M105660200
21. Horke S, Witte I, Wilgenbus P, Kruger M, Strand D, and Forstermann U. Paraoxonase-2 reduces oxidative stress in vascular cells and decreases endoplasmic reticulum stress-induced caspase activation. Circulation. (2007) 115:2055–64. doi: 10.1161/CIRCULATIONAHA.106.681700
22. Sanghera DK, Aston CE, Saha N, and Kamboh MI. DNA polymorphisms in two paraoxonase genes (PON1 and PON2) are associated with the risk of coronary heart disease. Am J Hum Genet. (1998) 62:36–44. doi: 10.1086/301669
23. Guxens M, Tomas M, Elosua R, Aldasoro E, Segura A, Fiol M, et al. Association between paraoxonase-1 and paraoxonase-2 polymorphisms and the risk of acute myocardial infarction. Rev Esp Cardiol. (2008) 61:269–75. doi: 10.1157/13116654
24. Elnoamany MF, Dawood AA, and Azmy RM. Paraoxonase 2 gene (Cys311-Ser) polymorphism and the risk of coronary artery disease World J Cardiovasc Dis. (2014) 4:11. doi: 10.4236/wjcd.2014.49056
25. Chen CC, Chen CC, Tu JD, Wu YL, and Leu SJ. Associations between genetic polymorphisms of paraoxonase genes and coronary artery disease in a Taiwanese population. Clin Biochem. (2013) 46:1664–7. doi: 10.1016/j.clinbiochem.2013.05.066
26. Gupta N, Gill K, and Singh S. Paraoxonases: structure, gene polymorphism & role in coronary artery disease. Indian J Med Res. (2009) 130:361–8.
27. Stoltz DA, Ozer EA, Recker TJ, Estin M, Yang X, Shih DM, et al. A common mutation in paraoxonase-2 results in impaired lactonase activity. J Biol Chem. (2009) 284:35564–71. doi: 10.1074/jbc.M109.051706
28. Perloff D, Grim C, Flack J, Frohlich ED, Hill M, McDonald M, et al. Human blood pressure determination by sphygmomanometry. Circulation. (1993) 88:2460–70. doi: 10.1161/01.CIR.88.5.2460
29. Friedewald WT, Levy RI, and Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. (1972) 18:499–502. doi: 10.1093/clinchem/18.6.499
30. Adeli K and Ogbonna G. Rapid purification of human DNA from whole blood for potential application in clinical chemistry laboratories. Clin Chem. (1990) 36:261–4. doi: 10.1093/clinchem/36.2.261
31. Skol AD, Scott LJ, Abecasis GR, and Boehnke M. Joint analysis is more efficient than replication-based analysis for two-stage genome-wide association studies. Nat Genet. (2006) 38:209–13. doi: 10.1038/ng1706
32. Samani NJ, Erdmann J, Hall AS, Hengstenberg C, Mangino M, Mayer B, et al. Genomewide association analysis of coronary artery disease. N Engl J Med. (2007) 357:443–53. doi: 10.1056/NEJMoa072366
33. Munshi R, Panchal F, Chaurasia A, and Rajadhyaksha G. Association between paraoxonase 1(PON1) gene polymorphisms and PON1 enzyme activity in Indian patients with coronary artery disease (CAD). Curr Pharmacogenomics Personalized Med. (2018) 16:219–29. doi: 10.2174/1875692117666181227112119
34. Tward A, Xia YR, Wang XP, Shi YS, Park C, Castellani LW, et al. Decreased atherosclerotic lesion formation in human serum paraoxonase transgenic mice. Circulation. (2002) 106:484–90. doi: 10.1161/01.CIR.0000023623.87083.4F
35. Shih DM, Gu L, Xia YR, Navab M, Li WF, Hama S, et al. Mice lacking serum paraoxonase are susceptible to organophosphate toxicity and atherosclerosis. Nature. (1998) 394:284–7. doi: 10.1038/28406
36. Ng CJ, Hama SY, Bourquard N, Navab M, and Reddy ST. Adenovirus mediated expression of human paraoxonase 2 protects against the development of atherosclerosis in apolipoprotein E-deficient mice. Mol Genet Metab. (2006) 89:368–73. doi: 10.1016/j.ymgme.2006.07.004
37. Rosenblat M, Draganov D, Watson CE, Bisgaier CL, La Du BN, and Aviram M. Mouse macrophage paraoxonase 2 activity is increased whereas cellular paraoxonase 3 activity is decreased under oxidative stress. Arterioscler Thromb Vasc Biol. (2003) 23:468–74. doi: 10.1161/01.ATV.0000059385.95664.4D
38. Jalilian A, Javadi E, Akrami M, Fakhrzadeh H, Heshmat R, Rahmani M, et al. Association of cys 311 ser polymorphism of paraoxonase-2 gene with the risk of coronary artery disease. Arch Iran Med. (2008) 11:544–9.
39. Paszek E, Godlewski J, Wołkow P, Żmudka K, Słowik A, Legutko J, et al. Paraoxonase 2 C311S single nucleotide polymorphism is associated with type C lesions in coronary atherosclerosis. Clin Biochem. (2022) 105-106:64–9. doi: 10.1016/j.clinbiochem.2022.04.009
40. Imai Y, Morita H, Kurihara H, Sugiyama T, Kato N, Ebihara A, et al. Evidence for association between paraoxonase gene polymorphisms and atherosclerotic diseases. Atherosclerosis. (2000) 149:435–42. doi: 10.1016/S0021-9150(99)00340-8
41. Oliveira SA, Mansur AP, Ribeiro CC, Ramires JA, and Annichino-Bizzacchi JM. PON1 M/L55 mutation protects high-risk patients against coronary artery disease. Int J Cardiol. (2004) 94:73–7. doi: 10.1016/j.ijcard.2003.05.011
42. Gluba A, Pietrucha T, Banach M, Piotrowski G, and Rysz J. The role of polymorphisms within paraoxonases (192 Gln/Arg in PON1 and 311Ser/Cys in PON2) in the modulation of cardiovascular risk: a pilot study. Angiology. (2010) 61:157–65. doi: 10.1177/0003319709351258
43. ArulJothi KN, Suruthi Abirami B, Irusappan S, Gautami A, Swathine C, and Devi A. L55M and Q192R polymorphism of Paraoxonase gene and the risk of myocardial infarction in South Indian Tamil population. Meta Gene. (2018) 15:55–9. doi: 10.1016/j.mgene.2017.11.004
44. Godbole C, Thaker S, Kerkar P, Nadkar M, Gogtay N, and Thatte U. Association of PON1 gene polymorphisms and enzymatic activity with risk of coronary artery disease. Future Cardiol. (2021) 17:119–26. doi: 10.2217/fca-2020-0028
45. Gupta N, Singh S, Maturu VN, Sharma YP, and Gill KD. Paraoxonase 1 (PON1) polymorphisms, haplotypes and activity in predicting cad risk in North-West Indian Punjabis. PloS One. (2011) 6:e17805. doi: 10.1371/journal.pone.0017805
46. Kaur S, Bhatti GK, Vijayvergiya R, Singh P, Mastana SS, Tewari R, et al. Paraoxonase 1 gene polymorphisms (Q192R and L55M) are associated with coronary artery disease susceptibility in Asian Indians. Dubai Diabetes Endocrinol J. (2018) 24:38–47. doi: 10.1159/000494508
47. Agrawal S, Tripathi G, Prajnya R, Sinha N, Gilmour A, Bush L, et al. Paraoxonase 1 gene polymorphisms contribute to coronary artery disease risk among north Indians. Indian J Med Sci. (2009) 63:335–44. doi: 10.4103/0019-5359.55884
48. Nasreen FJ and Balasubramaniam G. Paraoxonase gene polymorphisms: Understanding the biochemical and genetic basis of coronary artery disease. J Taibah Univ Med Sci. (2023) 18:257–64. doi: 10.1016/j.jtumed.2022.10.001
49. Ashiq S and Ashiq K. The role of paraoxonase 1 (PON1) gene polymorphisms in coronary artery disease: A systematic review and meta-analysis. Biochem Genet. (2021) 59:919–39. doi: 10.1007/s10528-021-10043-0
50. Schmidt H, Schmidt R, Niederkorn K, Gradert A, Schumacher M, Watzinger N, et al. Paraoxonase PON1 polymorphism leu-Met54 is associated with carotid atherosclerosis: results of the Austrian Stroke Prevention Study. Stroke. (1998) 29:2043–8. doi: 10.1161/01.STR.29.10.2043
51. Shahsavari G, Nouryazdan N, Adibhesami G, and Birjandi M. Genetic associations and serum paraoxonase levels with atherosclerosis in western Iranian patients. Mol Biol Rep. (2020) 47:5137–44. doi: 10.1007/s11033-020-05585-2
52. Doneva-Basheva KI, Gospodinov K, Tacheva T, Dimov D, and Vlaykova TI. Role of single nucleotide polymorphism L55M in the paraoxonase 1 gene as a risk and prognostic factor in acute coronary syndrome. Curr Issues Mol Biol. (2022) 44:5915–32. doi: 10.3390/cimb44120403
Keywords: coronary artery disease, PON1, PON2, polymorphisms, haplotype, North India
Citation: Bhat MA, Singh J, Lone GM and Goyal S (2025) Association of Paraoxonase-1 (p.L55M) and Paraoxonase-2 (p.S311C) polymorphisms with coronary artery disease in North Indian Punjabi population. Front. Endocrinol. 16:1688319. doi: 10.3389/fendo.2025.1688319
Received: 19 August 2025; Accepted: 23 September 2025;
Published: 07 October 2025.
Edited by:
Dora Janeth Fonseca, Rosario University, ColombiaReviewed by:
Maria Bayliak, Vasyl Stefanyk Precarpathian National University, UkraineBasak Gokce, Süleyman Demirel University, Türkiye
Copyright © 2025 Bhat, Singh, Lone and Goyal. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shiwali Goyal, Z295YWwuc2hpd2FsaUBnbWFpbC5jb20=
†ORCID: Shiwali Goyal, orcid.org/0000-0002-3126-774X
 Mohd Akbar Bhat
Mohd Akbar Bhat Jatinder Singh
Jatinder Singh Ghulam Mohd Lone4
Ghulam Mohd Lone4 Shiwali Goyal
Shiwali Goyal