- 1Department of Biostatistics and Health Data Science, Indiana University School of Medicine, Indianapolis, IN, United States
- 2Department of Biomedical Engineering and Informatics, Indiana University Indianapolis, Luddy School of Informatics, Computing, and Engineering, Indianapolis, IN, United States
- 3Centre for Community Health and Wellbeing, Jaramogi Oginga University of Science and Technology, Bondo, Kenya
Malaria control efforts in Kenya face persistent challenges due to fragmented health information systems, despite notable digital innovations. This mini review evaluates implementations in western Kenya, contrasting successes like Siaya County's Electronic Community Health Information System (eCHIS), developed through collaborations between the Ministry of Health, local agencies, and frontline health workers, which reduces reporting delays through real-time mobile data collection, with ongoing struggles including paper-based records in health facilities and unreliable rural internet. We document how analytical methods, when properly supported, can transform surveillance. Methods such as spatiotemporal models using climate and case data can improve outbreak predictions, while machine learning techniques can optimize insecticide-treated bed net distributions by pinpointing high-risk households. However, these analytical tools remain underutilized due to data fragmentation and limited technical capacity. Key implementation challenges emerged, including device charging difficulties for community health workers, inconsistent data standards between systems, and privacy concerns under Kenya's new Digital Health Act that policymakers are currently addressing through revised guidelines. Key recommendations from this review include the expansion of digital health platforms with co-design input from end-users, improved data quality through standardized reporting mechanisms enforced by county health leadership, and the incorporation of predictive modeling to identify high-risk areas and optimize intervention timing. Investing in robust health information infrastructure will not only strengthen malaria control efforts in Kenya but also serve as a model for other malaria-endemic regions. Digital tools show tremendous potential when paired with sustained training, community engagement, and realistic maintenance solutions supported by public-private partnerships.
1 Introduction
Malaria is a life-threatening disease caused by Plasmodium parasites, transmitted to humans through the bites of infected Anopheles mosquitoes (1, 2). Despite being preventable and treatable, malaria continues to be a major public health burden, particularly in sub-Saharan Africa, with an estimated 263 million cases and 597,000 malaria deaths worldwide in 2023 with an increasing incidence rate from 58.6 in 2022 to 60.4 cases per 1,000 population at risk in 2023 (2). An estimated 95% of these cases are from the World Health Organization (WHO) African Region with a mortality rate of 13.7 per 1,000 population (2). However, in Kenya, approximately, 3.4 million malaria cases and over 12,000 deaths have been reported (3). Due to the scale-up of interventions which include insecticide-treated nets (ITNs), indoor spraying (IRS), and Artemisinin-based combination therapy, morbidity and mortality have reduced by 27% and 59% in sub-Saharan Africa between 2000 and 2020 (1, 3). Despite the reduction, the prevalence of malaria is still high in the region significantly hampering economic growth and development, particularly in malaria-endemic areas where recurrent infections limit productivity, increase healthcare costs, and weaken health systems (2).
Kenya is among the high-burden malaria countries in Africa, with transmission varying by region due to ecological and climatic factors (4, 5). The western region, particularly Siaya County, experiences some of the highest malaria prevalence rates in the country. Our recent study and surveys indicate that Siaya County has a shift of malaria burden and a malaria prevalence of over 30%, nearly double that of other endemic regions in Kenya (5–7). Several factors contribute to this high burden, including favorable environmental conditions for mosquito breeding, limited access to healthcare, and high rates of asymptomatic infections among school-aged children, which sustain ongoing transmission (4). Effective malaria control in Siaya County requires not only robust intervention strategies but also reliable data systems to track cases, monitor shift of malaria burden or increase of cases, and optimize resource allocation (8). Health information systems (HIS) play a critical role in strengthening disease surveillance, monitoring intervention effectiveness, and supporting data-driven decision-making. In many countries, digital health platforms have transformed disease management. For example, the use of mobile health (mHealth) applications for malaria surveillance has enhanced data collection, and communication in rural areas (9). However, in Kenya, the health information infrastructure remains fragmented, with multiple data systems operating in parallel, the data captured at point-of-care in the community and health facilities are mostly paper-based leading to delays in reporting, inconsistencies in data quality, and limited integration across platforms (10–12). Some major challenges are the lack of standardization in data formats and reporting protocols, making it difficult to merge datasets from different health facilities, community health workers, and research institutions (13–18). Additionally, infrastructure limitations such as unreliable internet access, insufficient digital tools, and gaps in training among healthcare workers further complicate data integration efforts (13, 14, 17, 18). These are among the barriers that hinder real-time malaria tracking, delaying responses to outbreaks and limiting the effectiveness of intervention programs.
The Climate Change and Epidemics 2024 Report by the CLIMADE Consortium highlights several urgent calls for action (19). One key priority is timely outbreak reporting, emphasizing the need for governments and health organizations to commit to immediate and transparent reporting of infectious disease outbreaks, ensuring open data sharing to enhance global preparedness and response. Another critical focus is prioritizing vulnerable populations, recognizing that climate change and infectious diseases disproportionately impact these communities. The report calls for investments in resilient healthcare systems, infrastructure, and disaster preparedness to protect those most at risk. Similarly, the WHO World Malaria Report 2024 emphasizes the need to address inequities in the global malaria response, advocating for better data systems and knowledge to improve surveillance, decision-making, and health outcomes (2).
This review aims to provide a comprehensive overview of the existing health information systems used for malaria surveillance in Kenya, with a specific focus on malaria hotspot area such as Siaya County. It will examine the statistical analyses currently applied within these systems, assess their strengths and limitations, and explore opportunities for improvement. By identifying gaps in data collection, reporting, and integration, this paper seeks to inform policymakers, researchers, and public health officials about potential strategies to enhance malaria surveillance and decision-making. Strengthening health information systems and employing advanced statistical methods will be critical in optimizing malaria control strategies and ultimately reducing the burden of the disease in Kenya and beyond.
2 Situation in Western Kenya
2.1 Literature search
While this study consist of a short review, we completed a structured search strategy to ensure a comprehensive review of existing health information systems and statistical approaches for malaria control in Western Kenya. We searched multiple academic databases, including PubMed, Web of Science, Scopus, and Google Scholar, using keywords such as “malaria surveillance AND health information systems,” “digital health platforms AND malaria reporting,” “predictive modeling AND malaria transmission,” and “statistical models AND malaria forecasting.” We consider the following studies: (1) peer-reviewed articles, reports, and policy documents published within the last 15 years, (2) studies focusing on malaria surveillance, predictive modeling, and statistical analyses, (3) research conducted in Kenya or similar endemic regions in sub-Saharan Africa, and (4) studies examining health information systems and digital health technologies. We also considered grey literature, such as reports from the World Health Organization (WHO), Kenya Ministry of Health (MOH), Kenya Medical Research Institute (KEMRI), and the CLIMADE Consortium, to incorporate policy-related insights and government initiatives.
2.2 Health information systems
The District Health Information Software 2 (DHIS2) is a free, open-source, web-based platform designed for the collection, validation, analysis, and presentation of aggregate and patient-based statistical data across multiple health programs (20). With its flexible metadata model and configurable user interface, DHIS2 allows countries to tailor their health information systems without custom programming. In Kenya, the Kenyan Health Information System (KHIS) is built on DHIS2, transforming fragmented, paper-based reporting into a unified electronic system (21). The KHIS allows for routine reporting of various diseases, including malaria, with individual counties being directly responsible for their own data collection, analysis, and dissemination (22). With this decentralized system, there have been multiple digital health systems aimed at strengthening data collection. However, they have been described as “uncoordinated, fragmented, and not integrated into a cohesive national health framework” (10). For instance, the HIS suffers from documented fragmentation: (1) not all systems are capable of KHIS integration; (2) manually transcribe paper records into digital systems causes delays; and (3) absent of auto synchronization force health workers to spend surveillance time reconciling duplicate entries. These health systems do not “facilitate the integration of different sources of health information within the health system”, ultimately meaning that healthcare providers are unable to share health-related information effectively and on time (23). The lack of interoperability impacts the quality of patient care, the effectiveness of care, and the usability of the data collected (19). This not only affects providers but can complicate data analysis and reporting. At present, the Kenya Health Information System (KHIS) operates as an electronic system that aggregates routine health data from health facilities across the country. However, the method of data capture at the facility and community levels varies. In many facilities, particularly in rural and under-resourced areas, data are initially recorded on paper before being digitized and uploaded into KHIS.
In 2020, the Kenyan government started developing a new program to address the issues previously discussed. The Electronic Community Health Information System (eCHIS), nationally launched in September 2023, has been referred to as the first of its kind in Kenya. The eCHIS follows a “standardized requirements framework,” ultimately leading to more accurate and efficient data collection, on the community level (24, 25). By connecting to DHIS2 via FHIR (Fast Healthcare Interoperability Resources) compliant APIs (Application Programming Interface), eCHIS automates the transfer of community level data into KHIS, reducing manual transcription delays and improving data completeness and timeliness (26). The eCHIS is a secure, interoperability program, that will be part of a broader Digital Health Platform in the future (21, 27). This system has significant implications for malaria control, as it enables Community Health Promoters (CHPs) to submit real-time malaria data, facilitating faster outbreak detection and response. Moreover, Kenya's partnership with Medic aims to “further strengthen eCHIS deployment, scaling it nationally” to improve malaria surveillance and intervention effectiveness (28), contributing to a cohesive, health information system.
Although eCHIS represents a promising advancement, its early testing phases revealed several limitations, including its dependence on sustained commitment from stakeholders and donors (24). During early digital health implementation efforts in Isiolo County (2019–2023) (29), CHPs reported that their responsibilities became increasingly demanding. The CHPs also mentioned operational issues like difficulty charging the phones and syncing data in areas that lack electricity and internet (29). Similar operational issues were also noted during the formal eCHIS pilot rollout in Migori County in 2022 (30), where approximately 1,500 CHPs were digitized with support from the Lwala Community Alliance and the CHU4UHC Platform (31). This can be particularly damaging since data quality may decrease, as CHPs may have to revert to paper-based reporting. This issue is particularly concerning for malaria surveillance, as delays in reporting may hinder rapid response efforts. The ongoing rollout of eCHIS aims to address these challenges, but as of now, both paper and electronic records are still commonly used in parallel. While Kenya has taken meaningful steps toward a unified digital health system, critical challenges remain in achieving full integration and efficiency. Ensuring that malaria-related data can be shared seamlessly across health facilities, CHPs, and research institutions requires not only interoperability but also investment in digital infrastructure, workforce training, and standardized reporting protocols. A fully integrated system will enable timely malaria case tracking, facilitate resource allocation, and enhance statistical analyses and predictions to prevent future outbreaks.
2.3 Data privacy and security
Although the Data Protection Act of 2019 enshrines the right to privacy and mandates lawful, fair, and transparent processing of personal and health data (32, 33), enforcement gaps exacerbated by delayed guidelines and limited regulatory oversight, have led to reported breaches, most notably during the COVID-19 pandemic when emergency surveillance measures compromised individual privacy rights (34). In response, the Office of the Data Protection Commissioner issued the Data Protection General Regulations in 2021, introducing requirements for data minimization, breach notification, and the registration of data controllers and processors, yet practical challenges in infrastructure, user training, and consistent enforcement persist (35). The Digital Health Act of 2023 further strengthened these safeguards by mandating that all digital health platforms explicitly comply with the Data Protection Act and by establishing a Digital Health Agency responsible for quality assurance, data governance, and national interoperability standards (36). This includes data security, a digital platform for the health sector, and proper data sharing to allow decision-making on any level (36). This act simultaneously addresses data privacy concerns, and regulation issues, and reiterates the need for a united digital health platform, with shareable data. The Act also creates a Digital Health Agency, whose main task is to “[establish and manage] an integrated health information system” (36). Nonetheless, the Finance Bill 2024s proposal to grant the Kenya Revenue Authority access to personal data without full adherence to the Data Protection Act has intensified debates over ethical governance and underscored the urgent need for robust, enforceable privacy frameworks that protect individual rights while enabling the rapid, secure data sharing essential for malaria surveillance and public health decision making (37).
2.4 Statistical analyses
Malaria modeling and surveillance in Kenya is a joint effort between the Kenyan government, Kenyan Institutions, and foreign entities. The Ministry of Health (MOH) tends to be at the center of these partnerships, with most reports coming directly from them. One of the main institutions performing statistical analyses on malaria is the Kenya National Bureau of Statistics (KNBS). The KNBS tends to report descriptive statistics on county demographics, malaria prevalence, and the efficiency of malaria prevention implementation. In the Kenya Demographic and Health Survey (KDHS), malaria is tracked nationally and county, among other community health factors (38, 39). A few metrics reported are percentages of homes with insecticide-treated nets (ITN) by endemicity zone and county, ITN usage, and reasons individuals may not use ITNs (38, 39). Since the KDHS reports on the overall health of the country, malaria is just a small portion of the report, with basic statistics recorded. In partnership with the MOH Division of National Malaria Program (DNMP), the KNBS completed an analysis for the Malaria Indicator Survey (MIS) as well. The MIS is a part of the international Roll Back Malaria initiative, with its final report dating 2020. This survey, like the KDHS, reported ITN usage and accessibility, malaria vaccinations, but also provided statistics on malaria prevalence by characteristics (i.e., child's age, sex, rurality, income, endemicity) and by malaria species (40). Through qualitative analysis, the MOH and KNBS can better recommend interventions to target individuals in high epidemic areas and keep track of trends. The MOH Division of National Malaria Program also provides reports of epidemiological and entomological factors, to monitor trends of malaria indicators. The Malaria Surveillance Bulletin (41), a quarterly report, records malaria prevalence and test positivity rates by region, seasonal transmission, and vector species composition. Like the MIS, this report tracks trends in malaria, with the most recent report being published for the April 2021–June 2021 quarter (41). One of the main objectives of the Kenya Malaria Strategy (KMS) is to strengthen malaria surveillance, ultimately leading to improved, evidence-based decision-making. With such a heavy emphasis on surveillance, the Kenyan government is laying a foundation to create a comprehensive malaria early warning system.
The Kenyan Meteorological Department, in partnership with the MOH and the Kenyan Medical Research Institute (KEMRI), frequently releases early warning predictions for malaria risk in the Kenyan highlands. These reports integrate climate variables such as maximum temperature, mean maximum temperature, temperature deviations, and rainfall into predictive models that estimate additive percentage risk (42). Comparing this additive risk to respective epidemic thresholds, the meteorological department and KEMRI assess the malaria epidemic risk in the upcoming months (42). These reports though, are limited to the Nandi, Kisii, and Kakamega districts (42), restricting their broader applicability.
To enhance malaria forecasting, researchers have explored advanced predictive models beyond Kenya. The Malaria Early Warning System (MEWS) integrates seasonal climate forecasts, routinely monitored climate data, and country vulnerability indices to predict malaria outbreaks (43). MEWS functions on a global scale, with reports covering multiple African countries, including Kenya. Additionally, machine learning approaches and Bayesian models have been increasingly utilized to predict malaria transmission patterns based on climate, entomological, and epidemiological data (44, 45). For instance, spatiotemporal models can identify hotspots of malaria transmission, while time-series models help in forecasting malaria case trends. While some research initiatives in Kenya incorporate predictive modeling, much of the MOH's malaria reporting remains surveillance based. Integrating predictive models into national reporting systems could significantly enhance emergency preparedness, optimize intervention strategies, and improve resource allocation for malaria control. Expanding early warning systems beyond the limited districts and incorporating machine learning-driven risk assessment tools could strengthen Kenya's malaria response framework, ultimately reducing disease burden and mortality (46, 47).
3 Discussion
To effectively combat malaria in high-burden regions like Siaya County, Kenya, strengthening health information systems is essential for improving disease surveillance, resource allocation, and intervention strategies (8, 11–14). As illustrated in Figure 1 (left pathway), the current fragmented system, reliant mostly on paper-based forms and manual data entry, introduce significant delays in data reporting (48, 49), potentially extending up to several weeks. In addition, it limits variables to basic metrics (e.g., rapid detection test results), restricting spatial-temporal analyses and perpetuating reactive outbreak responses. This review highlights the need for an integrated (14), secured (33, 35, 37), interoperable (10, 15, 26), and data-informed approach to malaria control (22), leveraging real-time digital tools (48, 49) (e.g., mobile apps) and advanced statistical models (e.g., Bayesian spatiotemporal frameworks) to transform decision-making (13, 25, 28, 42–47).
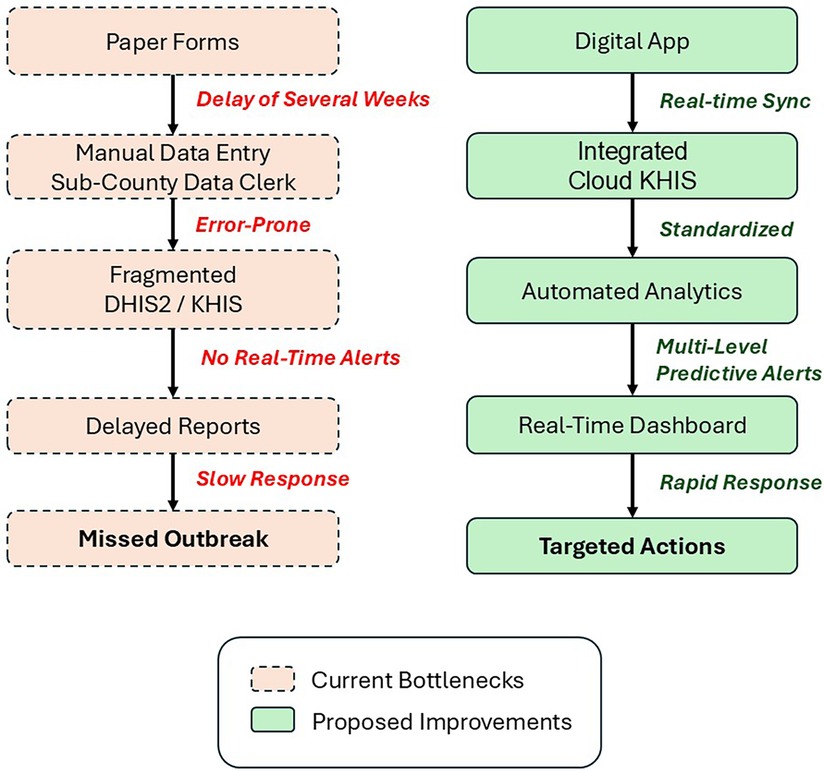
Figure 1. Comparison of malaria data flows in Kenya: current fragmented reporting vs. proposed integrated digital surveillance system. The left (red) side depicts Kenya's current system with paper-based delays and limited data, while the (green) shows proposed digital workflows enabling real-time analytics and targeted responses.
The proposed digital workflow (Figure 1, right pathway) demonstrates how innovations at five critical levels from community data collection to national policy, can address systemic gaps such as: (1) Faster reporting: Mobile apps (9, 11, 30, 31, 48) reduce latency from weeks to hours by auto-syncing GPS-tagged case data and prevention metrics (e.g., use of insecticide-treated nets and indoor residual spraying), (2) Richer variables: Inclusion of mosquito species, breeding site proximity, and treatment adherence timestamps enables hotspot mapping and targeted interventions, (3) Automated analytics: Cloud-integrated dashboards that applies spatiotemporal models and machine learning techniques to improve monitoring and predictions (42, 46).
However, several limitations must be acknowledged. First, the proposed digital solutions assume stable electricity and internet connectivity, which remain inconsistent in rural malaria-endemic areas where less than half of the health facilities in western Kenya report reliable power access. Second, cultural and behavioral barriers among healthcare workers may hinder adoption, as observed in the eCHIS pilot (30, 31) where more than 30% of community health volunteers reverted to paper reporting due to fear of new technology or hesitancy on its use. Third, predictive models require high-quality historical data that may not exist in regions with chronically weak surveillance systems.
Key recommendations include the expansion of digital health platforms, improved data quality through standardized reporting mechanisms, and the incorporation of predictive modeling to identify high-risk areas and optimize intervention timing. These interventions should be coupled with: (a) solar-powered devices for offline data collection, (b) competency-based training programs adapted to local literacy levels (9, 17, 18), and (c) phased model deployment starting with data-rich districts. Investing in robust health information infrastructure will not only strengthen malaria control efforts in Kenya but also serve as a model for other malaria-endemic regions (2). A multi-sectoral approach, combining government agencies, healthcare providers, researchers, and community health workers, is necessary to bridge existing data gaps and ensure evidence-based policy decisions. Notably, our review is constrained by the limited evaluation period of digital interventions—most projects like eCHIS have operated for <2–3 years, making long-term sustainability assessments difficult. In addition, there is a need for foreign entities to collaborate with the local academic institutions, especially universities or research centers in sub-Saharan Africa. Subsequently, these local academic institutions can sustainably build the capacity of other stakeholders on the peripheral application of digital technology not only to control malaria but other infections. As the global health community continues to push for malaria elimination, this work highlights the critical role of data-informed strategies in transforming public health outcomes. Success of such initiatives could pave the way for broader applications, reinforcing the idea that sustainable disease control begins with reliable, accessible, and actionable data.
In conclusion, this review reveals that Kenya's malaria surveillance is hampered by fragmented data systems, manual reporting delays, and interoperability gaps, which undermine timely decision-making. Recent digital initiatives—DHIS2-based KHIS and the eCHIS rollout—have improved data capture and integration but still face infrastructure, training, and privacy challenges. Statistical analyses remain largely descriptive, with predictive modeling underutilized despite proven value in outbreak forecasting. Closing these gaps requires a unified digital platform that incorporates automated data flows, advanced analytics, and strong privacy safeguards. Such an integrated, data-driven approach will be pivotal for enhancing malaria control efforts in Western Kenya and beyond.
Author contributions
TG: Writing – original draft. FP-R: Conceptualization, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. GA: Writing – review & editing. YZ: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. WHO. World Malaria Report 2024: Addressing Inequity in the Global Malaria Response. Geneva: World Health Organization (2024).
3. WHO. WHO World Malaria Report 2022. Geneva: World Health Organization (2022). Available at: https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2022 (Accessed February 15, 2025).
4. Villena OC, Arab A, Lippi CA, Ryan SJ, Johnson LR. Influence of environmental, geographic, socio-demographic, and epidemiological factors on presence of malaria at the community level in two continents. Sci Rep. (2024) 14(1):16734. doi: 10.1038/s41598-024-67452-5
5. Pabon-Rodriguez FM, Ayodo G. The influence of climatic factors on age-group-specific malaria burden in western Kenya. Public Health Challenges. (2025) 4(2):e70052. doi: 10.1002/puh2.70052
6. Okoyo C, Githinji E, Muia RW, Masaku J, Mwai J, Nyandieka L, et al. Assessment of malaria infection among pregnant women and children below five years of age attending rural health facilities of Kenya: a cross-sectional survey in two counties of Kenya. PLoS One. (2021) 16(9):e0257276. doi: 10.1371/journal.pone.0257276
7. Salgado C, Ayodo G, Macklin MD, Gould MP, Nallandhighal S, Odhiambo EO, et al. The prevalence and density of asymptomatic plasmodium falciparum infections among children and adults in three communities of western Kenya. Malar J. (2021) 20(1):371. doi: 10.1186/s12936-021-03905-w
8. Muinga N, Magare S, Monda J, Kamau O, Houston S, Fraser H, et al. Implementing an open source electronic health record system in Kenyan health care facilities: case study. JMIR Med Inform. (2018) 6(2):e22. doi: 10.2196/medinform.8403
9. Tine F, Marks S, Kallander K. Implementing mHealth Solutions to Improve Community Health Worker Motivation and Performance. London: Malaria Consortium (2016). Available at: https://www.malariaconsortium.org/media-downloads/878/implementing-mobile-health-solutions (Accessed April 29, 2025).
10. Nyangena J, Rajgopal R, Ombech EA, Oloo E, Luchetu H, Wambugu S, et al. Maturity assessment of Kenya’s health information system interoperability readiness. BMJ Health Care Inform. (2021) 28(1):e100241. doi: 10.1136/bmjhci-2020-100241
12. Soti DO, Kinoti SN, Omar AH, Logedi J, Mwendwa TK, Hirji Z, et al. Feasibility of an innovative electronic mobile system to assist health workers to collect accurate, complete and timely data in a malaria control programme in a remote setting in Kenya. Malar J. (2015) 14(1):430. doi: 10.1186/s12936-015-0965-z
13. Ojo A, Tolentino H, Yoon S. Strengthening eHealth systems to support universal health coverage in sub-Saharan Africa. Online J Public Health Inform. (2021) 13(3):e62628. doi: 10.5210/ojphi.v13i3.11550
14. Victor AA, Frank LJ, Makubalo LE, Kalu AA, Impouma B. Digital health in the African region should be integral to the health system’s strengthening. Mayo Clin Proc Digit Health. (2023) 1(3):425–34. doi: 10.1016/j.mcpdig.2023.06.003
15. Musabi AG, Kipkebut AK. Healthcare services interoperability in Kenya: challenges and opportunities. Ehealth Telecommun Syst Netw. (2024) 13(01):1–11. doi: 10.4236/etsn.2024.131001
16. Muinga N, Magare S, Monda J, English M, Fraser H, Powell J, et al. Digital health systems in Kenyan public hospitals: a mixed-methods survey. BMC Med Inform Decis Mak. (2020) 20(1):2. doi: 10.1186/s12911-019-1005-7
17. Asah FN, Kaasbøll JJ. Challenges and strategies for enhancing eHealth capacity building programs in African nations. J Pers Med. (2023) 13(10):1463. doi: 10.3390/jpm13101463
18. Ngugi PN, Were MC, Babic A. Users’ perception on factors contributing to electronic medical records systems use: a focus group discussion study in healthcare facilities setting in Kenya. BMC Med Inform Decis Mak. (2021) 21(1):362. doi: 10.1186/s12911-021-01737-x
19. CLIMADE Consortium. Climate Change and Epidemics 2024. Stellenbosch: Summary for Policymakers (2024).
20. Nyaga N, Melli E, Mwangi M, Gicheso M, Digre P, Wanyee S. Determining the total cost of ownership and end user perception of the Kenya national cancer registry (NaCaRE-KE): a DHIS2- based digital health system. Oxf Open Digit Health. (2025) 3:oqaf007. doi: 10.1093/oodh/oqaf007
21. CHISU Consortium. Country Health Information Systems and Data Use Project. Initiative funded by USADI and led by JSI Research & Training Institute (n.d.). Available at: https://chisuprogram.org/where-we-work/kenya (Accessed December 2, 2024).
22. Okello G, Molyneux S, Zakayo S, Gerrets R, Jones C. Producing routine malaria data: an exploration of the micro-practices and processes shaping routine malaria data quality in frontline health facilities in Kenya. Malar J. (2019) 18(1):420. doi: 10.1186/s12936-019-3061-y
23. Kenya Health Sector R of. Health Information System Policy. Nairobi: Kenya Ministry of Health (2014). Available at: https://extranet.who.int/countryplanningcycles/sites/default/files/country_docs/Kenya/health_information_system_policy.pdf (Accessed December 2, 2024).
24. Health Africa A. Digital Community Health Activated in Kenya: A Leap Towards Universal Health Coverage. Nairobi: Amref Health Africa (2024). Available at: https://newsroom.amref.org/blog/2024/07/digital-community-health-activated-in-kenya-a-leap-towards-universal-health-coverage/ (Accessed December 2, 2024).
25. Living Goods. Supporting Sustainable and Government-Led Digitized Community Health Systems in Kenya. Nairobi: Living Goods (2023). Available at: https://livinggoods.org/wp-content/uploads/2022/03/eCHIS-Factsheet_edits_2023_Print.pdf (Accessed December 2, 2024).
26. Mwago P. CHT Interoperability Reference Application: Adoption by Ministry of Health Kenya to Facilitate Data Exchange. Nairobi: Medic (2023). Available at: https://medic.org/stories/cht-interoperability-reference-application-adoption-by-ministry-of-health-kenya-to-facilitate-data-exchange/ (Accessed May 6, 2025).
27. Health Africa A. National Community Health Digitization Strategy 2020–2025. Nairobi: Ministry of Health (2021). Available at: https://www.eahealth.org/sites/www.eahealth.org/files/content/attachments/2021-08-02/eCHIS-Strategy-2020-2025.pdf (Accessed December 2, 2024).
28. Medic. Medic Partners with Kenyan Government to Transform Community Health. Nairobi: Medic (2023). Available at: https://medic.org/stories/medic-partners-with-kenyan-government-to-transform-community-health/ (Accessed December 2, 2024).
29. Mukungu B, Dodworth K, Olungah C. Research Insights Digitizing Community Health in Kenya Insights from Community Health Volunteers. Edinburgh: Research Insights, University of Edinburgh (n.d.). Available at: https://www.sps.ed.ac.uk/sites/default/files/assets/pdf/Digitizing%20Community%20Health%20in%20Kenya%20-%20digital.pdf (Accessed December 2, 2024).
30. Exemplars News. Kenya’s eCHIS: Revolutionizing Community Health with Digital Innovation. Exemplars in Global Health (2024).
31. CHU4UHC. CHU4UHC Platform 2022 Impact Report. (2023). Available at: https://chu4uhc.org/chu4uhc-platform-2022-impact-report/ (Accessed May 26, 2025).
32. Makulilo A. African Data Privacy Laws. Vol 33. In: Makulilo AB, editor. Springer International Publishing (2016). doi: 10.1007/978-3-319-47317-8
33. Makulilo AB, Boshe P. Data Protection in Kenya. Cham: Springer (2016). p. 317–35. doi: 10.1007/978-3-319-47317-8_15
34. Open Institute. Is Your Data at Risk? How Kenya’s Finance Bill Proposes Access to Citizens’ Data. Nairobi: Open Institute Trust (2024). Available at: https://openinstitute.africa/2024/06/26/is-your-data-at-risk-how-kenyas-finance-bill-proposes-access-to-citizens-data/ (Accessed May 6, 2025).
35. Office of the Data Protection Commissioner. The Data Protection (General) Regulations. Nairobi: Cabinet Secretary for Information, Communication, Technology, Innovation and Youth Affairs (2021).
36. Wanyama E. Does Kenya’s Digital Health Act Mark A New Era for Data Governance and Regulation? Kampala: CIPESA (2024). Available at: https://cipesa.org/2024/05/does-kenyas-digital-health-act-mark-a-new-era-for-data-governance-and-regulation/ (Accessed May 6, 2025).
37. Houghton I, Kiai M. Data protection act amendment in the finance bill is classic “big brother”, illegal and must be rejected by the National Assembly and Kenyans. Amnesty International Kenya Section, ARTICLE 19 Eastern Africa Regional Nairobi (2024). Available at: https://www.amnestykenya.org/data-protection-act-amendment-in-the-finance-bill-is-classic-big-brother-illegal-and-must-be-rejected-by-the-national-assembly-and-kenyans/ (Accessed May 23, 2024).
38. Health M of. Kenya Demographic and Health Survey 2022. Key Indicators Report. (2022). Available at: https://dhsprogram.com/pubs/pdf/PR143/PR143.pdf (Accessed December 2, 2024).
39. Health M of. Kenya Demographic and Health Survey 2022. Volume 1. Nairobi, and Rockville, MA: Kenya National Bureau of Statistics (KNBS) in collaboration with ICF International (2022). Available at: https://dhsprogram.com/pubs/pdf/FR380/FR380.pdf (Accessed December 2, 2024).
40. Health M of. Kenya Malaria Indicator Survey 2020. Final Report. (2021). Available at: https://dhsprogram.com/pubs/pdf/MIS36/MIS36.pdf (Accessed December 2, 2024).
41. NMCP. Malaria Surveillance Bulletin. Nairobi: Ministry of Health Division of Malaria Control (2021). Available at: https://nmcp.or.ke/wp-content/uploads/2024/05/SMEOR-malaria-surveillance-bulletin-issue-37.pdf (Accessed December 2, 2024).
42. Meteorological Department K. Malaria Epidemic Early Warning Prediction System for Western Kenya Highland for November 2024. Nairobi: Kenya Meteorological Department (2024). Available at: https://meteo.go.ke/sites/default/files/forecast/biometeorological/Malaria%20epidemic%20early%20warning%20prediction%20system%20for%20western%20kenya%20highland%20for%20November%202024.pdf (Accessed December 2, 2024)
43. Ceccato P. Malaria Early Warning System. Palisades, NY: International Research Institute for Climate Prediction, Columbia Climate School (2017). Available at: https://iridl.ldeo.columbia.edu/maproom/Health/Regional/Africa/Malaria/System.html (Accessed December 2, 2024).
44. Rotejanaprasert C, Ekapirat N, Sudathip P, Maude RJ. Bayesian spatio-temporal distributed lag modeling for delayed climatic effects on sparse malaria incidence data. BMC Med Res Methodol. (2021) 21(1):287. doi: 10.1186/s12874-021-01480-x
45. Damien BG, Sode AI, Bocossa D, Elanga-Ndille E, Aguemon B, Corbel V, et al. Bayesian spatial modelling of malaria burden in two contrasted eco-epidemiological facies in Benin (West Africa): call for localized interventions. BMC Public Health. (2022) 22(1):1754. doi: 10.1186/s12889-022-14032-9
46. Khan O, Ajadi JO, Hossain MP. Predicting malaria outbreak in the Gambia using machine learning techniques. PLoS One. (2024) 19(5):e0299386. doi: 10.1371/journal.pone.0299386
47. Zheng JX, Lu SN, Li Q, et al. Deciphering the climate-malaria nexus: a machine learning approach in rural southeastern Tanzania. Public Health. (2025) 238:124–30. doi: 10.1016/j.puhe.2024.11.013
48. CHU4UHC. The Journey Towards Digitizing Community Health in Kenya so far. Nyeri: Ministry of Health Division of Community Health (2022). Available at: https://chu4uhc.org/the-journey-towards-digitizing-community-health-in-kenya-so-far/ (Accessed May 26, 2025).
49. WHO. Kenya Breaks New Ground and Pilots its First Digital Health Campaign System. Geneva: World Health Organization (2025). Available at: https://www.afro.who.int/countries/kenya/news/kenya-breaks-new-ground-and-pilots-its-first-digital-health-campaign-system (Accessed May 26, 2025).
Keywords: malaria, statistical analysis, health information system, sub-Saharan Africa, surveillance, Kenya
Citation: Griffin T, Pabon-Rodriguez F, Ayodo G and Zhuang Y (2025) Strengthening health information systems and inherent statistical outputs for improved malaria control and interventions in western Kenya. Front. Epidemiol. 5:1591261. doi: 10.3389/fepid.2025.1591261
Received: 11 March 2025; Accepted: 3 June 2025;
Published: 19 June 2025.
Edited by:
Vidhan Jain, National Institute for Research in Tribal Health (ICMR), IndiaReviewed by:
Adilson José DePINA, Malaria Elimination Program, CCS-SIDA/MoH, Cabo VerdeCopyright: © 2025 Griffin, Pabon-Rodriguez, Ayodo and Zhuang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Felix Pabon-Rodriguez, ZnBhYm9ucm9kcmlndWV6QGdtYWlsLmNvbQ==
†ORCID:
Felix Pabon-Rodriguez
orcid.org/0000-0003-3528-2354
 Taliyah Griffin1
Taliyah Griffin1 Felix Pabon-Rodriguez
Felix Pabon-Rodriguez George Ayodo
George Ayodo Yan Zhuang
Yan Zhuang