- 1Department of Biochemistry and Biomedical Sciences, Faculty of Health Sciences, McMaster University, Hamilton, ON, Canada
- 2McMaster Immunology Research Centre, Faculty of Health Sciences, McMaster University, Hamilton, ON, Canada
- 3Michael G. DeGroote Institute for Infectious, Diseases, McMaster University, Hamilton, ON, Canada
- 4Infectious Diseases Research Directorate, Ethiopian Public Health Institute, Addis Ababa, Ethiopia
- 5Department of Infectious Diseases, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
- 6Amsterdam Institute for Global Health and Development, Academic Medical Center – Amsterdam University, Amsterdam, Netherlands
- 7Department of Medicine, Faculty of Health Sciences, McMaster University, Hamilton, ON, Canada
- 8Firestone Institute for Respiratory Health, The Research Institute of St Joe’s, St Joseph’s Healthcare Hamilton, Hamilton, ON, Canada
- 9Health Sciences North Research Institute, Northern Ontario School of Medicine University, Sudbury, ON, Canada
Introduction: Little is known about the acute and long-term sequelae of COVID-19 and its pathophysiology in African patients, who are known to have a distinct immunological profile compared to Caucasian populations. Here, we established protein signatures to define severe outcomes of acute COVID-19 and determined whether unique protein signatures during the first week of acute illness predict the risk of post-acute sequelae of COVID-19 (Long COVID) in a low-income country (LIC) setting.
Method: Using the Olink inflammatory panel, we measured the abundance of 92 proteins in the plasma of COVID-19 patients (n=55) and non-COVID-19 individuals (n=23). We investigated distinct inflammatory protein signatures in acute severe COVID-19 individuals (n=22) compared to asymptomatic or mild/moderate COVID-19 cases (n=33), and non-COVID-19 controls.
Results: Levels of SLAMF1, CCL25, IL2RB, IL10RA, IL15RA, IL18 and CST5 were significantly upregulated in patients with critical COVID-19 illness compared to individuals negative for COVID-19. The cohort was followed for an average of 20 months, and 23 individuals developed Long COVID, based on the WHO’s case definition, while 32 COVID-19 patients recovered fully. Whereas upregulated levels of SLAMF1, TNF, TSLP, IL15RA, IL18, ADA, CXCL9, CXCL10, IL17C, and NT3 at the acute phase of the illness were associated with increased Long COVID risk, upregulated TRANCE was associated with a reduced risk of developing Long COVID. Protein levels of SLAMF1, IL15RA, and IL18 associated with critical illness during the acute phase of COVID-19 also predicted Long COVID risk.
Discussion: Patients with severe COVID-19 and Long COVID outcomes exhibited distinct proteomic signatures. Unravelling the pathophysiology of severe acute COVID-19 and Long COVID before its advent may contribute to designing novel interventions for diagnosing, treating, and monitoring of SARS-CoV-2 infection and its associated acute and long-term consequences.
Introduction
Acute COVID-19 is characterized by protean clinical manifestations, including asymptomatic, mild/moderate, severe, or critical conditions. Moreover, a multitude of complex symptoms persist in SARS-CoV-2 infected individuals post-acute phase, affecting the cardiovascular, respiratory, gastrointestinal, genitourinary, hematologic, musculoskeletal, central nervous, and other systems, collectively known as post-acute sequelae of COVID-19 or Long COVID (1, 2). The WHO defines Long COVID as an ongoing, relapsing, or new symptom or condition present three or more months from the onset of COVID-19 with symptoms that last for at least two months and cannot be explained by an alternative cause (3). However, other organizations use different definitions for Long COVID indicating the elusive characteristics of the condition (4, 5). Systematic reviews demonstrated that the burden of Long COVID ranges between 45% and 62% depending on the case definition, the study design, and the region where the study was conducted (6–8). Most of these data have been reported from high-income countries (HICs), and a significant knowledge gap exists in low-income country (LIC) settings (9, 10).
Though its exact cause remains unknown, age, sex, socio-economic conditions, ancestry, co-morbidities, severity during acute illness, reinfection, SARS-CoV-2 genotype, and vaccination appear to be associated with the risk of developing Long COVID (1, 2, 11–16). Persistence of replication-competent viruses, or viral components, reactivation of latent virus, autoimmunity, microbiota dysbiosis, and chronic inflammation have been proposed as the mechanism(s) leading to multiple organ damage in patients with Long COVID (2). Several biomarkers have been investigated to assess the risk of severe illness during acute COVID-19 or Long COVID in HICs (17–38). However, many of these biomarkers have not been validated and are not yet commonly used in clinical practice. Additionally, there is limited knowledge of the overall pathophysiology and molecular mechanisms underlying the acute and long-term sequelae of COVID-19 in LICs. In particular, the distinct immunological background, high burden of co-infections due to HIV-1, malaria, tuberculosis, helminths, and the diverse sociodemographic factors may impact the biological profile following infection with SARS-CoV-2 infection in African populations (39–42). Indeed, a recent report demonstrated distinct COVID-19 immune signatures associated with COVID-19 severity in Ugandan patients co-infected with HIV-1 (21). Given that Long COVID is a heterogeneous disease with complex symptoms, it is imperative to unravel the role of biomarkers that can predict the development of severe acute COVID-19 and Long COVID in the context of Africa.
In this study, we performed a longitudinal analysis of patients in Ethiopia with COVID-19. Specifically, we compared protein profiles between COVID-19 patients and COVID-19-negative individuals. In addition, we assessed plasma protein signals associated with severe outcomes following acute COVID-19 and determined whether unique proteins that appear early during the onset of acute COVID-19 illness predict Long COVID risk. Our findings show that differences in protein abundances represent immune dysregulation in COVID-19 individuals who develop critical illness as well as those who developed Long COVID. Understanding the pathophysiology of acute COVID-19 illness, and Long COVID before its advent may contribute to designing novel interventions related to diagnosing, treating, and monitoring acute COVID-19, Long COVID, and other chronic post-viral syndromes.
Methods
Patient recruitment and follow-up
This study (Clinicaltrials.gov: NCT04584424) is a prospective observational cohort study being undertaken in Ethiopia and the study protocol has been described in detail previously (43). The study was reviewed and approved by the Health Research Ethics Review Committee of the Ethiopian Public Health Institute in Ethiopia (EPHI-IRB-282-2020) and the Hamilton Integrated Research Ethics Board (HiREB:16956). Written informed consent was obtained by all participants, or their guardians, for participation in the study.
Adults 18 years and older presenting with respiratory infections attending hospital-based settings between August 2021 and February 2022 were recruited from Addis Ababa (Capital city of Ethiopia) and screened using real-time polymerase chain reaction (RT-PCR) and/or antigen tests, or anti-nucleocapsid antibody tests. Individuals with confirmed SARS-CoV-2 infection (i.e., positive in any of the tests mentioned above) were considered COVID-19 cases. Those with a negative SARS-CoV-2 PCR, or antigen, or no documented evidence of COVID-19 clinically were considered as COVID-19-negative non-COVID-19 controls. The controls were not tested for other pathogens although the patients had “influenza-like illness” at enrollment. Individuals without evidence of COVID-19 at enrollment who became infected during follow-up were excluded. In addition, individuals with co-infections including HIV-1, tuberculosis and malaria were excluded. Sociodemographic, clinical, and laboratory data were collected using standardized Case Record Forms (CRFs) adapted from the International Severe Acute Respiratory and Emerging Infection Consortium’s (ISARIC) CRFs for emerging severe acute respiratory infections (44). Data was entered using the REDcap software package. The baseline patient’s severity status was classified following the WHO criteria as asymptomatic, mild/moderate, severe (with dyspnea, respiratory rate ≥ 30 breaths per minute, O2 saturation ≤ 93%, lung infiltrates ≥ 50% of the lung fields within 24–48 hours), and critical (with respiratory failure, septic shock, and/or multiple organ failure) (45). Cohort follow-up was conducted for the survey of persistent symptoms occurring at any time from the onset of COVID-19 included in the WHO case definition and defined as the presence of at least one persistent symptom of > 2 months duration occurring 12 weeks from the onset of acute COVID-19 illness (3).
Sample collection and processing
Peripheral blood was collected using EDTA vacutainers within 1 to 21 days of SARS-CoV-2 diagnosis during acute illness, and follow-up samples were collected after 180 ( ± 30), and 365 ( ± 30) days post-symptom onset. Plasma was stored frozen at -80°C until analysis and transported to McMaster University for Olink protein analysis.
Protein analysis
The Olink targeted 96 inflammation proximal extension assay (PEA) platform (Uppsala, Sweden) was used as per the manufacturer’s guidelines (46). The Olink Target 92 Inflammation panel offers a broad selection of proteins associated with inflammatory and immune response processes. In brief, the PEA platform uses antibody pairs linked to unique DNA oligonucleotides, that bind to target proteins. The binding of the antibodies to their target proteins brings the DNA oligonucleotides into closer proximity and results in the hybridization and formation of a new DNA sequence. The DNA sequence is then amplified and quantified using real-time PCR. Normalized Protein concentrations (NPX), an arbitrary unit normalized into the log2 scale, are used to define the protein abundance level. Measurements that failed the internal quality control with a warning were excluded from the dataset.
Statistical analysis
Baseline characteristics with continuous variables were summarized as median [interquartile ranges (IQR)], and categorical variables as frequencies (percentages). Continuous variables were compared by Mann-Whitney U or Kruskal-Wallis tests, and categorical variables using χ² test or Fisher’s exact test. Cox proportional hazard (HR) was used to ascertain the association between explanatory variants (including age, sex, body-mass index, comorbidity, vaccination, reinfection, SARS-CoV-2 variant) and outcomes of interest, namely critical COVID-19 during acute illness and development of Long COVID. Multivariate HR was estimated by including all significant values (age above 50 years, comorbidity, and infection during the predominant circulating Delta variant) in univariate analysis.
Initial unsupervised clustering of groups was performed by principal component analysis (PCA) and heat maps. The difference in fold-change (log2) of protein abundance was estimated between the different groups. Multiple testing corrections were applied according to Benjamini and Hochberg’s procedure, and data were visualized using volcano plots and heatmaps. The association between the abundance of each protein and outcome (i.e. critical illness or Long COVID) was then compared using cox-proportional hazard. In addition, Cox proportional regression models were conducted to estimate the association of each biomarker level [as the dependent variable, categorized into high (≥ median NPX) or low (< median NPX) abundance] with incident Long COVID followed by adjustments for confounding covariates (47). Kaplan-Meier curves were created to visualize the effect of protein abundance levels on the risk of developing Long COVID. Statistical differences between groups were estimated by Log-rank test. Enricher was used for Gene Ontology (GO) terms and STRING was used for protein-protein interaction pathways analysis (48, 49). In addition, receiver operating curves (ROCs) was used to determine which protein significantly predicted symptoms. p-values < 0.05 were considered significant. R studio, GraphPad Prism, and STATA software were used for statistical analysis.
Results
Study participants and characteristics
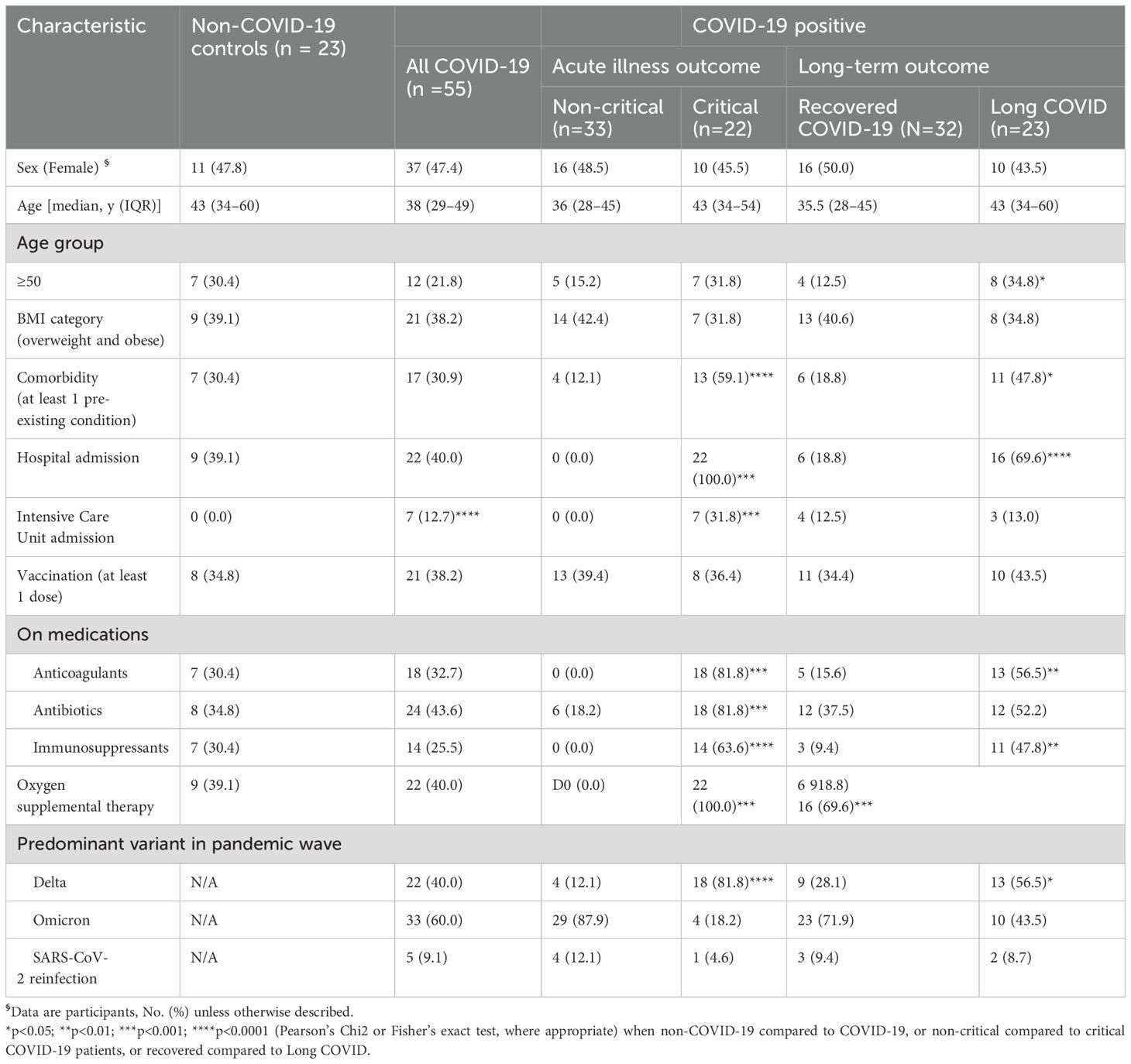
Study participants were recruited from an ongoing prospective observational cohort study in Ethiopia (43). A cohort of 55 patients with confirmed COVID-19 were recruited for this study. In addition, another 23 randomly selected COVID-19-negative individuals examined for other respiratory illnesses were enrolled as controls (Figure 1). There were no significant differences in sociodemographic or clinical factors, SARS-CoV-2 vaccine uptake, hospital admission status or medication taken among the two groups (Table 1). The average annual income was US$ 1.200, 33% were considered poor, 33% completed university education and 50% were employed in governmental or non-governmental offices. None of the participants admitted to being a smoker, but few admitted to being a social drinker. However, only COVID-19 patients were admitted to the intensive care unit (ICU) compared to non COVID-19 controls.
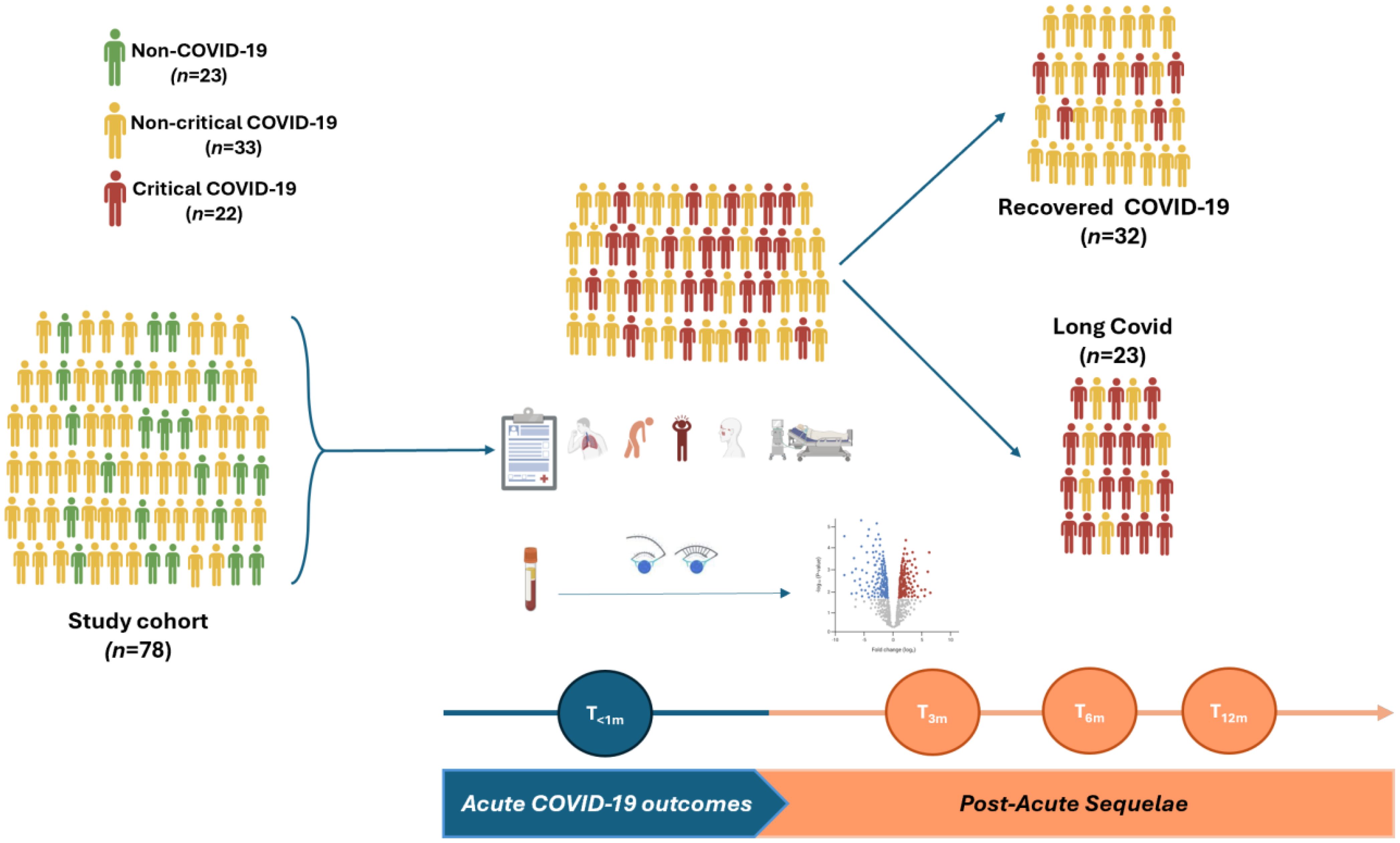
Figure 1. Study design and data analysis. (Made by BioRender).
Of the 55 individuals with COVID-19, 33 had mild or moderate (non-critical) disease and 22 were severe, requiring hospital admission without or with intensive care (critical). Fatigue/malaise (54.6%), arthralgia (52.7%), myalgia (50.9%), fever (50.9%), loss of smell (49.1), sore throat (47.3%), loss of taste (45.5%), headache (45.5%), anorexia (45.5%), cough (40.0%), and shortness of breath (30.9%) were the most frequent symptoms experienced by COVID-19 patients during the acute phase of COVID-19 illness (Supplementary Table 1). Critically ill COVID-19 cases were older than non-critical patients, had significantly more frequent symptoms, more comorbid conditions, as well as more frequent hospital and intensive-care unit (ICU) admissions. Anticoagulants, antibiotics, anti-inflammatory drugs, and oxygen supplementation were more frequently administered to critically ill COVID-19 patients than non-critical COVID-19 counterparts. SARS-CoV-2 Delta and Omicron were the two most dominant circulating variants during the pandemic wave in Ethiopia when the study was undertaken (Supplementary Figure 1) (50–52). As expected, the predominant circulating SARS-CoV-2 variant (i.e. Delta) at the time of enrollment was significantly associated with critical acute COVID-19 illness (Table 1).
Participants were followed for an average of 20 (IQR: 9-21) months. Overall, 41.8% (23 out of 55) of COVID-19 patients reported experiencing at least one persistent symptom, according to the WHO’s case definition for Long COVID (3). The most commonly reported symptoms among these patients were fatigue (47.8%), cough (47.8%), myalgia (47.8%), insomnia (30.4%), foggy brain (21.7%) and shortness of breath (21.7%). Notably, age > 50 years (HR=2.85, 95% CI: 1.19-6.86), having at least one comorbid condition (HR=2.63, 95% CI: 1.16-5.99), and being infected during the predominant circulating Delta SARS-CoV-2 variant phase of the pandemic wave (HR=2.58, 95% CI: 1.13-5.91) were associated with a significantly increased hazard of Long COVID (Figure 2B).
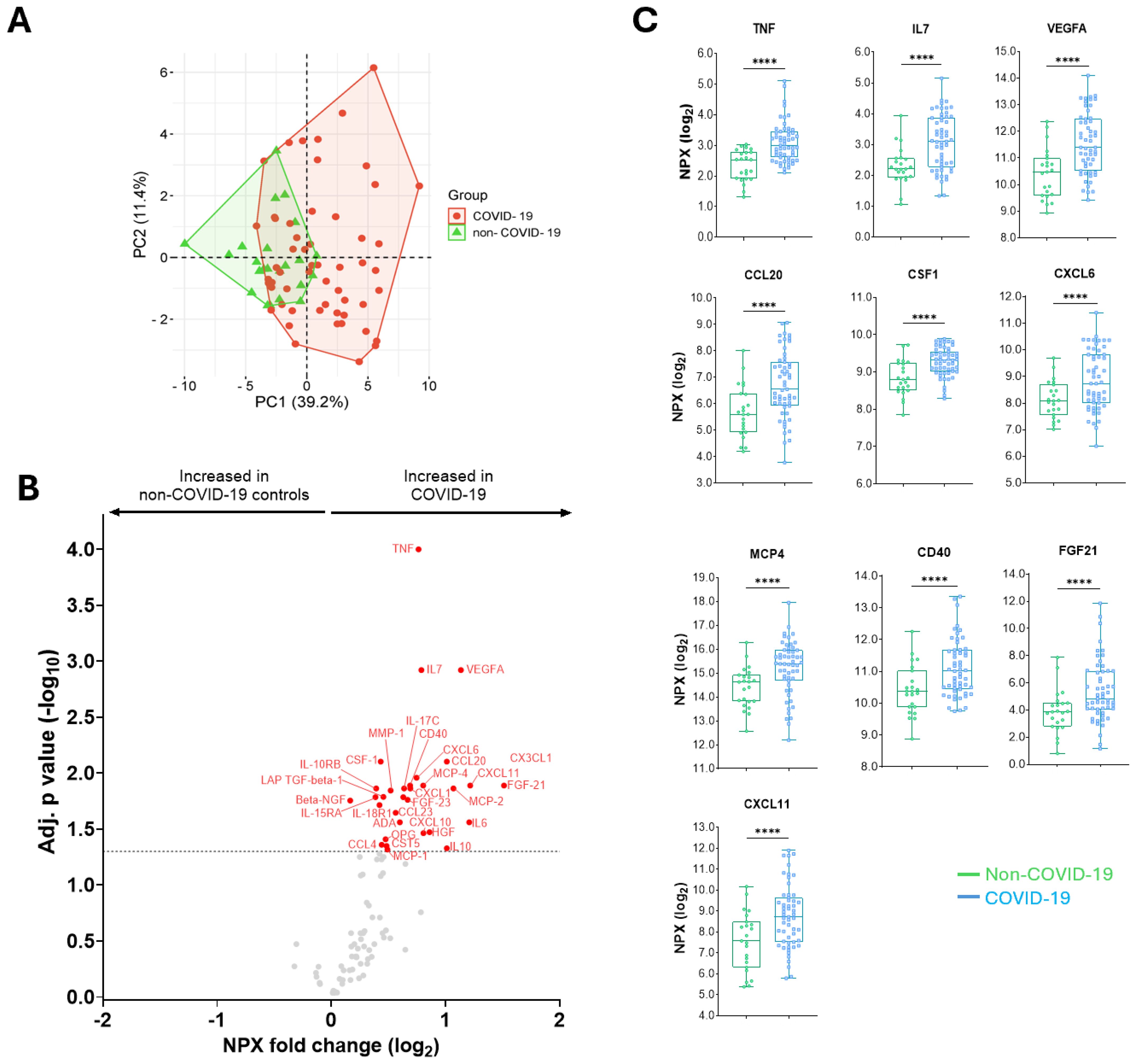
Figure 2. Differences in the abundance of inflammatory proteins in COVID-19 patients compared to non-COVID-19 controls. (A) A principal component analysis between COVID-19 and non-COVID-19 individuals. (B) A volcano plot showing differential abundance analysis comparing proteins from COVID-19 patients with non-COVID-19 controls. Red and blue dots represent significantly (adjusted for multiple testing by Benjamini-Hochberg) up- and down-regulated proteins, respectively. Gray dots indicate nonsignificant. (C) Median (IQR) levels of the 10 top proteins in non-COVID-19 controls compared to COVID-19 patients. P values: ****<0.0001 were calculated using Mann Whitney U test.
COVID-19 patients exhibited increased levels of inflammatory proteins
Overall, 14,076 protein levels in 153 samples (78 at baseline, 44 at 6-month and 31 at 12-month follow-up) derived from 78 individuals were measured using the Olink targeted 92 inflammation PEA platform. Initially, we compared the protein signatures of COVID-19 patients during the acute phase of COVID-19 illness (n=55) with the COVID-19-negative non-COVID-19 controls (n=23). Figure 2A shows the clustering of inflammatory protein profiles in individuals with COVID-19 compared to non-COVID-19 controls. Thirty-one proteins were significantly increased in COVID-19 patients compared to non-COVID-19 controls after adjustment for multiple testing (Figure 2B). The top ten significantly increased proteins were TNF, IL7, VEGFA, CCL20, CSF1, CXCL6, MCP4, CD40, FGF21, and CXCL11 (Figure 2C).
COVID-19 patients with critical illness exhibit a distinct plasma protein signature
Within the COVID-19 patient group, we then determined the protein signatures in those with critical outcomes (n=22) and compared them with those who did not develop critical COVID-19 (n=33), or non-COVID-19 controls (Figures 3A, B). We identified that only three proteins, namely TNF, SLAMF1, and CDCP1, were differentially abundant in critically ill COVID-19 patients compared to those with non-critical illness presentation. However, when critical COVID-19 patients were compared to non-COVID-19 controls, there was significant clustering between the two groups (Figure 3C), and the number of differentially abundant proteins increased significantly to 31 (Figures 3D, E). Of these, the top ten proteins were TNF, IL7, VEGFA, CCL20, CSF1, CXCL6, MCP4, CD40, FGF21, and CXCL11 (Figure 3F). After adjustment for confounding factors, seven proteins that were highly abundant and associated with an increased hazard of critical COVID-19 outcome were SLAMF1, CCL25, IL2RB, IL10RA, IL15RA, IL18 and CST5 (Figure 3G). Additionally, the predictive power assessed by the AUC curve showed that IL15RA (AUC=0.842), SLAMF1 (AUC=0.775) and IL18 (AUC=0.775) as the top three proteins predicting critical COVID-19 illness (Figure 3H). Gene Ontology (GO) analysis revealed significant enrichment in phagocytotic pathway, and protein-protein interaction pathways showed significant cytokine-cytokine, cytokine-cytokine receptor, and cytokine-chemokine, cytokine-chemokine receptor, chemokine-chemokine receptor interactions when critical and non-critical COVID-19 patients were compared (Figure 3I).

Figure 3. Differences in the abundance of inflammatory proteins in critical COVID-19 patients compared to non-critical COVID-19 patients or non-COVID-19 controls, and predicting power of differentially abundant proteins, gene enrichment and protein-protein interactions. A principal component analysis between critical COVID-19 and non-critical illness (A), or between critical COVID-19 and non-COVID-19 individuals (C). A volcano plot showing differential abundance analysis comparing proteins in critical COVID-19 patients vs. non-critical COVID-19 patients (B), or vs. non-COVID-19 controls (D). Red dots represent significantly (adjusted for multiple testing by Benjamini-Hochberg) upregulated proteins. Gray dots are insignificant. (E) Heat maps showing differential abundance of proteins in individuals without COVID-19, non-critical COVID-19, or critically ill COVID-19. (F) Median (IQR) levels of the most significant proteins in individuals with COVID-19 who developed Long COVID compared to recovered COVID-19 patients. P values: *<0.05, **0.01, ***<0.001, and ****<0.0001 were calculated using Kruskal Wallis with Dunn’s correction for multiple tests. (G) Adjusted cox-proportional hazard risk (HR) for critical illness. HR [(95% confidence intervals (CI)] in red color signifies increased risk of critically ill COVID-19 patients per unit change in log2-transformed NPX values of each protein. Gray colors are statistically not significant values. (H) Receiver operating characteristic (ROC) curve analysis of the upregulated proteins associated with Critical COVID-19 illness. (I) Gene enrichment and protein-protein interaction pathways of significantly expressed proteins in critical vs. non-critical COVID-19 patients.
Differences in plasma protein abundance levels during acute COVID-19 illness predict the risk of Long COVID
Next, we compared protein signatures in the study cohort with long-term outcomes – namely Long COVID. Protein abundance levels in recovered COVID-19 patients segregated clearly from those who eventually developed Long COVID (Figure 4A). Overall, COVID-19 patients who developed subsequent Long COVID exhibited 44 differentially abundant proteins compared to those who recovered (Figures 4B, D). Of these, ten proteins, namely SLAMF1, TNF, TSLP, IL15RA, IL18, ADA, CXCL10, IL17C, NT3, and CXCL9 were significantly increased (Figure 4C), and associated with an increased hazard of developing Long COVID after controlling for age, comorbidity and the Delta variant (Figure 4E). Notably, the abundance level of the protein TRANCE was reduced in patients who developed Long COVID compared to recovered COVID-19 patients and reduced the Long COVID risk (Figures 4C-E). After adjusting for age, comorbidity and SARS-CoV-2 variant, the hazard of Long COVID was 1.58 up to 4.12-fold in COVID-19 patients with upregulated baseline protein levels of SLAMF1, TNF, TSLP, IL15RA, IL18, ADA, CXCL10, IL17C, NT3, and CXCL9 (Figure 4E). On the contrary, it was only 0.50-fold in patients with a higher baseline TRANCE level (Figure 4E). Additionally, the predictive power assessed by the AUC curve showed that TNF (AUC=0.973), SLAMF1 (AUC=0.894) and IL18 (AUC=0.857) as the top three proteins predicting increased Long COVID, and TRANCE (AUC=0.700) predicted reduced Long COVID risk (Figure 4F). Gene Ontology (GO) analysis revealed significant enrichment in cytokine-, chemokine-, IL17-, TLR-signaling pathways, and protein-protein interaction pathways showed significant cytokine-cytokine, cytokine-cytokine receptor, and cytokine-chemokine, and chemokine-chemokine interactions when recovered COVID-19 and Long COVID patients were compared (Figure 4G).
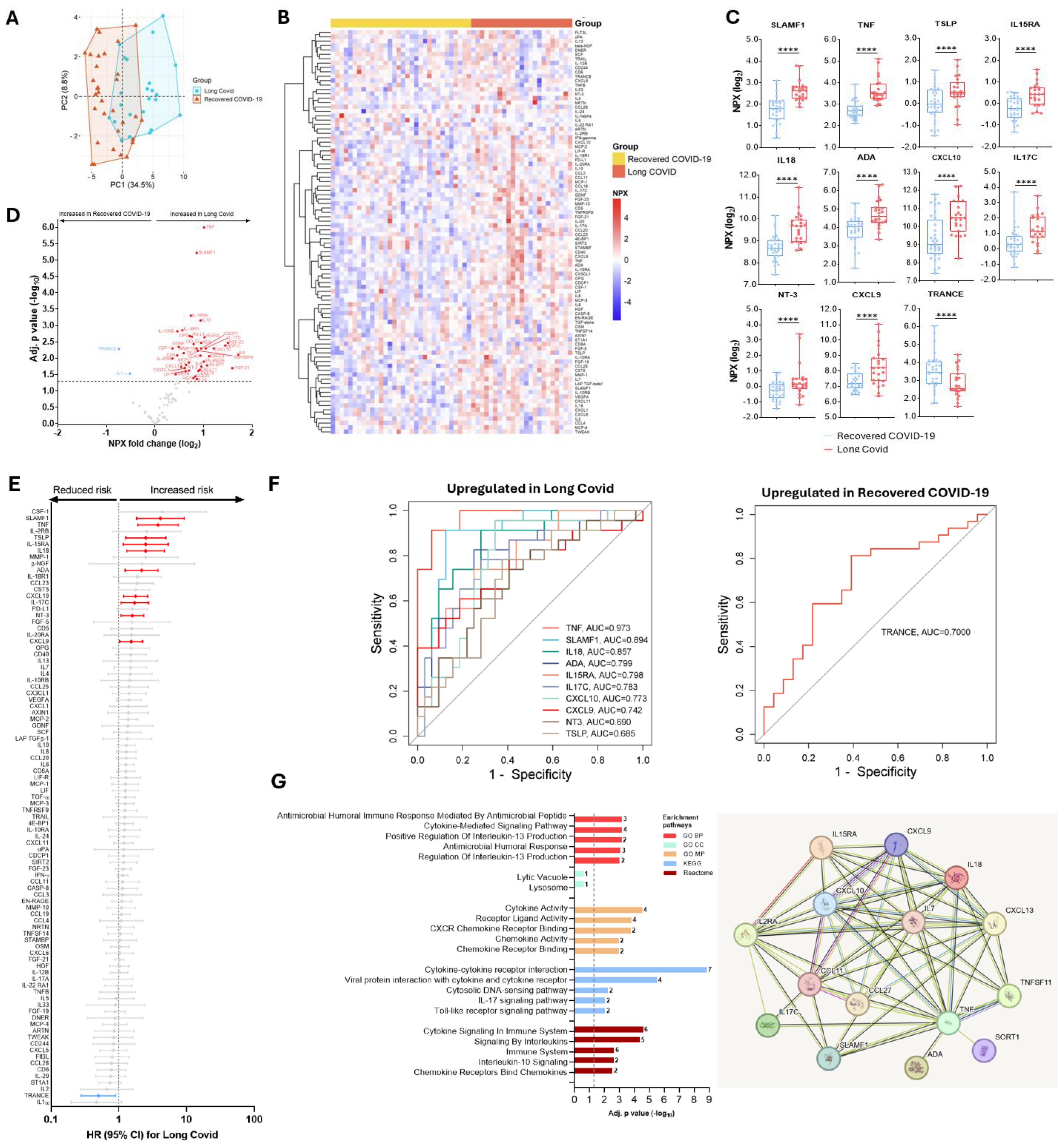
Figure 4. Differences in protein abundance in individuals with COVID-19 who developed Long COVID compared to recovered COVID-19 patients, and predicting power of differentially abundant proteins, gene enrichment and protein-protein interactions of significantly changed proteins in Long COVID. (A) A principal component analysis in recovered COVID-19 vs. Long COVID. (B) Heat maps showing differential abundance of proteins in non-COVID-19, recovered COVID-19, or Long COVID. (C) Median (IQR) levels of the most significant proteins in individuals with COVID-19 who developed Long COVID compared to recovered COVID-19 patients. P values, ****<0.0001 were calculated using Kruskal Wallis with Dunn’s correction for multiple tests. (D) A volcano plot showing differential abundance analysis comparing protein profile in those who developed Long COVID with those who recovered. Red and blue dots represent significantly (adjusted for multiple testing by Benjamini-Hochberg) up- and down-regulated proteins, respectively. Gray dots indicate nonsignificant. (E) Adjusted cox-proportional hazard risk (HR) for Long COVID. HR (95% CI) in red signifies an increased risk and blue signifies a reduced risk of Long COVID per unit change in log2-transformed NPX values of each protein. Gray colors are not significant. (F) Receiver operating characteristic (ROC) curve analysis of the upregulated or downregulated proteins associated with Long COVID risk. (G) Gene enrichment and protein-protein interaction pathways of significantly expressed proteins between recovered COVID-19 and Long COVID patients.
Interestingly, elevated levels of three proteins, namely SLAMF1, IL18 and IL15RA were associated with the risk of developing critical COVID-19 and Long COVID (Figure 5A). Whereas the combined AUC score of the three proteins was 0.836 for predicting critical COVID-19, the combined predictive AUC score of the three proteins in predicting Long COVID was 0.905 (Figures 5B, C).
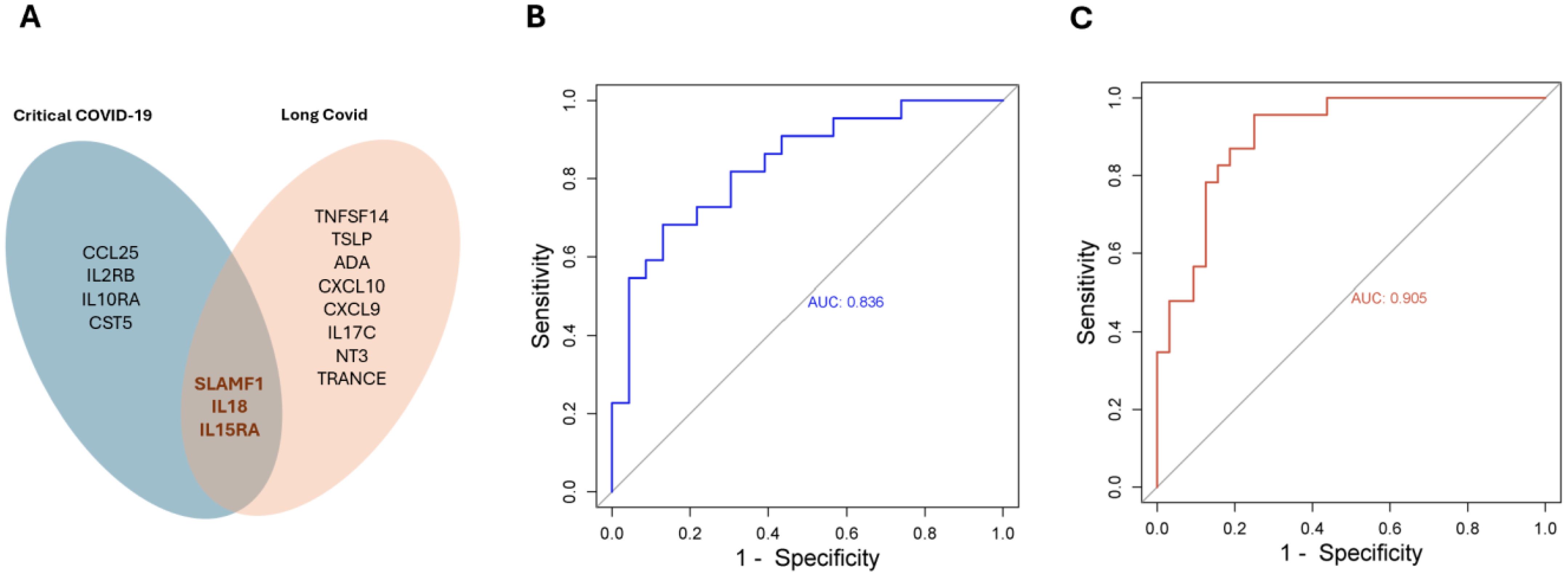
Figure 5. SLAMF1, IL18 and IL15RA are predictors in both acute - and long-term sequelae following SARS-COV-2 infection. (A) Venn diagram showing significantly expressed proteins in acute – and/or Long COVID. The combined predictive power of SLAMF1, IL18 and IL15RA in acute (B), or long-term sequelae (C) following SARS-COV-2 infection.
Differential protein signatures persist throughout post-acute sequelae of COVID-19
During the first year period following enrollment, plasma samples were obtained in a subset of recovered COVID-19 patients and those who developed Long COVID at an average of 6- and 12-months. Kaplan-Meier curves show a distinct clinical progression of Long COVID when individuals were segregated into high and low protein levels (Figure 6A). In Addition, the trends in the profile of protein levels were distinct between individuals who recovered from COVID-19 when compared to those who developed Long COVID (Figure 6B). Although we observed a tendency towards reduction, most of the proteins associated with the increased risk of Long COVID remained unchanged during the follow-up period, except TNF and IL18 which showed significant reductions (Figure 6A). On the contrary, IL17C and NT3 levels increased significantly among recovered COVID-19 patients. CXCL10 was the only protein that exhibited a significant reduction in both recovered and Long COVID patients. Although there was a tendency towards increases in TRANCE levels in both recovered and Long COVID cases, the difference was not significant.
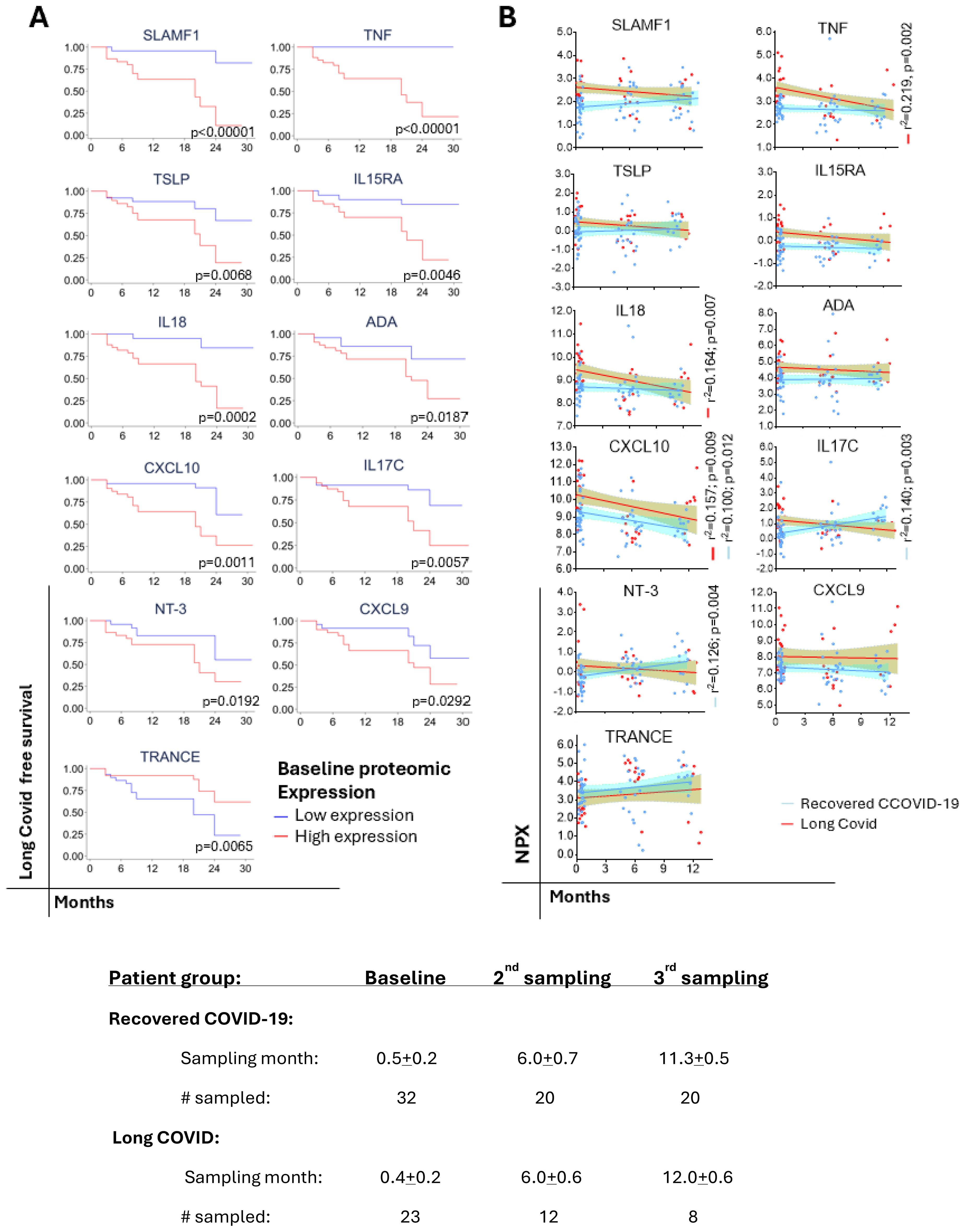
Figure 6. Predicting of progression to Long COVID and trajectories of protein levels over time. (A) Kaplan-Meier curves showing the clinical progression of Long COVID. Statistical differences between high (≥ median NPX) or low (< median NPX) protein levels were estimated by log-rank test. (B) Simple regression analysis of the significant protein levels trajectories in recovered COVID-19 vs. Long COVID.
Discussion
In this study, we demonstrated that circulating proteins is broadly dysregulated in COVID-19 patients and is associated with the risk of post-COVID-19 sequelae. To the best of our knowledge, the current study is the first to characterize the protein profiles of acute and long-term COVID-19 outcomes in the context of Sub-Saharan Africa.
Acute COVID-19 is characterized by immune activation and inflammation (53). Our data is consistent with other studies that find that COVID-19 patients exhibit increased levels of 31 unique proteins compared to non-COVID-19 controls (17–27). This includes proteins such as TNF, CD40, CSF, IL6, IL10, IL18RA, CCL23, CXCL10, CXCL11, MCP-2, and FGF21, which have been reported previously (17–27). Dysregulation of these cytokines and chemokines has been related to excessive inflammation and tissue damage in COVID-19 patients, particularly among COVID-19 patients with severe clinical outcomes (53). Here, we demonstrated that the unique signature featuring SLAMF1, CCL25, IL2-RB, IL10RA, IL15RA, IL18, and CST significantly increased the risk of critical illness in COVID-19 patients. Increased levels of SLAMF1 and IL18 in this patient group were similar to those reported previously (17–21). However, other investigators reported that CCL25 was lower in ICU-admitted patients than in non-ICU cases, and increased CCL25 was observed with clinical improvement (22). We were not able to confirm the findings in our setting; however, a major difference is that our study is derived from a setting in a LIC. Overall, these inflammatory response-related cytokines and chemokine ligands play a pivotal role in the pathogenesis of tissue injury associated with severe COVID-19.
High levels of the proteins SLAMF1, TNF, TSLP, IL15RA, IL17C, IL18, ADA, CXCL9, CXCL10 and NT3 during the acute phase of the illness was associated with an increased hazard of Long COVID in our cohort. Similar to our data, previous findings also showed increased levels of TNF, IL18, CXCL9, and CXCL10 associated with Long COVID (20, 30, 31). Notably, baseline protein levels of SLAMF1, IL15RA and IL18 associated with the critical illness during the acute phase of COVID-19 were also able to predict Long COVID risk. These biomarkers may play a pivotal role in the earlier identification of individuals who will succumb to severe disease during the acute phase of the illness as well as long-term sequelae. TSLP is a cytokine involved in the context of inflammation and allergy. Recent studies have shown that TSLP levels correlate with the duration of hospitalization in COVID-19 patients (54). This suggests that TSLP might play a role in the prolonged inflammatory responses seen in Long COVID. Most of the proteins associated with the increased Long COVID risk remained unchanged during the follow-up period indicating a sustained immune activation and inflammation. However, three proteins, namely TNF, IL18, and CXCL10, exhibited significant reductions, and the repeated measurement of these biomarkers may be relevant in monitoring treatment outcomes. Whereas studies concur with our result showing continuous reductions at 6 months of follow-up (30), others showed persistent elevations up to 18–24 months (20). In addition, persistent and sustained level of CXCL9 was observed in the current study as reported by others (20). Two proteins, namely IL17C and NT3 exhibited significantly increased levels among recovered COVID-19 patients. IL17C is a member of the IL17 family that plays a role in the immune response and enhances inflammatory responses by inducing the release of cytokines, such as IL1β, TNFα and IL6 (55). It might play a role in the persistent activation of the immune system contributing to the symptoms observed in Long COVID. NT3, a cytokine primarily known for its role in the nervous system (56), could be relevant in Long COVID through its role in immune regulation and tissue repair. By influencing the activity and survival of immune cells, NT3 might help modulate the persistence of immune activation and inflammation seen in Long COVID.
TRANCE, also known as RANKL, or TNFSF11, is known to be involved in the regulation of T cells and dendritic cells (57), which are key players in the immune response against SARS-CoV-2 (53). In this study, a high baseline level of TRANCE was associated with a reduced risk of developing Long COVID. Notably, a reduced abundance of TRANCE has been associated with severe COVID-19, including admission to the ICU (19, 26), and low levels of TRANCE in the CSF predicted Long COVID in patients followed for 13 months (58). Given that Long COVID has been linked to persistent viral replication (59–62), it is tempting to propose that this biomarker plays a role in modulating the anti-SARS-CoV-2 immune response.
The differences in the findings between our data and other studies may be attributed to differences in the case definitions for COVID-19 severity, Long COVID, follow-up duration, study design, and differences in patient population characteristics. We and others have previously demonstrated that acute COVID-19 illness in Africa is, in general, less severe than in HICs despite the intense transmission rate in LICs (11, 63, 64). Notably, an estimated 25-42% of COVID-19 individuals in HICs ended up being hospitalized or admitted into the intensive care unit (ICU), particularly during the earlier phases of the pandemic due to the ancestral variant (65–67). On the contrary, in the setting of LICs, only <5% of all COVID-19 patients develop severe COVID-19 (11, 63). This has been ascribed to pre-existing cross-immunity, immuno-modulation, or trained immunity (39–41). Likewise, we hypothesize that a similar mechanism operates in the pathogenesis of Long COVID showing a low burden of Long COVID in certain parasite-endemic areas in Africa (68).
A strength of our study includes the interrogation of proteins related to the pathophysiology of acute and long-term sequelae of SARS-CoV-2 infection in an LIC setting. Additionally, the plasma sampling time and the assessment of the baseline protein levels for predicting Long COVID risk. Several studies have included samples that were analyzed ranging between day <1 and >24 months (69–71). Adjustment for confounders which included age, comorbidity and SARS-CoV-2 variant associated with increased risk of Long COVID in our cohort is another strength of this study. Finally, albeit in a small number of patients, we also included the assessment of protein level trajectories over time that revealed some unique features that may help in Long COVID treatment outcomes. Nonetheless, our study has several limitations. Similar to several other studies, our cohort also suffers from analysis based on a relatively small sample size (69–71). Protein abundance studies with small sample size may fail to detect significant differences in protein abundance between groups (i.e. false negatives) due to statistical power. Another challenge with smaller sample size includes overestimation of the observed differences in protein abundance due to sampling variability. The latter has been addressed by normalizing into log2-scale of the protein concentrations. (46) Nonetheless, future studies need to be conducted by including a larger set of samples derived from diverse study participants. Second, we did not have SARS-CoV-2 genotype data although we have attempted to relate our analysis to the dominant variants circulating in the country during the enrollment period of our cohort participants (50–52). Finally, we determined 92 proteins focusing on inflammatory panels and we may have failed to detect all relevant protein biomarkers.
In conclusion, our data revealed that unique protein signatures are associated with severe COVID-19 and Long COVID in the African context. Dysregulation of protein pathways involved in cellular degranulation and proteolysis was significantly expressed among COVID-19 patients versus non-COVID-19 controls. Additionally, significantly increased unique protein profile in critically ill COVID-19 patients compared to non-COVID-19 controls or recovered COVID-19 patients compared to those who developed Long COVID exhibited inflammatory cytokines, chemoattractant for neutrophils, T cells, NK cells, monocytes, and endothelial cells. The findings should serve as baseline data informing future -omics studies in LMIC settings involving a larger sample size and more diverse additional protein panels related to cardiovascular, neurological, and metabolic dysregulations associated with post-COVID-19 sequelae (32–36). Additionally, this study provides critical insights into the pathophysiology of acute and long-term consequences of COVID-19, informing strategies and treatment approaches (70, 72).
Translating proteomic biomarkers into diagnostic and monitoring tools in LIC healthcare settings requires consideration of several factors. First, user-friendly and affordable be designed that can be used at point-of-care. For example, C-reactive protein (CRP) is a widely used biomarker for detecting inflammation and infections, such as bacterial pneumonia or sepsis, in several LIC settings. Second, assays designs should require minimal sample preparation reducing the need for a specialized equipment and training. Finally, the use of non-invasive or minimally invasive sampling methods, such as dried blood spots, saliva, or urine, that reduce patient discomfort and improve accessibility should be studied. Finaly, the developed tests should be validated in diverse populations in the context of LICs before implementation. Addressing these effectively would help the translation of biomarkers into diagnostic or monitoring tools in LIC healthcare settings to enhance the clinical relevance and potential real-world application of the findings.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
Ethics statement
The studies involving humans were approved by Health Research Ethics Review Committee of the Ethiopian Public Health Institute in Ethiopia (EPHI-IRB-282-2020) and the Hamilton Integrated Research Ethics Board (HiREB:16956). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
DW: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AGe: Formal analysis, Visualization, Writing – original draft. AL: Methodology, Writing – review & editing, Formal analysis, Visualization. MR: Conceptualization, Data curation, Investigation, Methodology, Project administration, Supervision, Writing – review & editing, Funding acquisition, Resources, Software, Writing – original draft. SA: Data curation, Investigation, Methodology, Writing – review & editing, Conceptualization, Funding acquisition, Project administration, Resources, Supervision. AG: Investigation, Methodology, Writing – review & editing, Data curation. WA: Methodology, Writing – review & editing, Investigation. TR: Methodology, Writing – review & editing, Conceptualization, Formal analysis, Writing – original draft. MH: Investigation, Methodology, Writing – review & editing. GTo: Funding acquisition, Investigation, Methodology, Resources, Writing – review & editing. GTa: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing. MT: Investigation, Writing – review & editing, Conceptualization, Data curation, Funding acquisition, Methodology, Project administration, Resources, Supervision, Writing – original draft. MM: Investigation, Writing – review & editing. AGi: Investigation, Writing – original draft, Writing – review & editing. DB: Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. CK: Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. CV: Formal analysis, Investigation, Methodology, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Funded by McMaster University. This work received grants from the Ethiopian Federal Ministry of Health, Addis Ababa, Ethiopia, and McMaster University, Hamilton, Canada.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that Generative AI was used in the creation of this manuscript. Grammarly for editing grammar.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2025.1575135/full#supplementary-material
References
1. Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med. (2021) 27:601–15. doi: 10.1038/s41591-021-01283-z
2. Mehandru S and Merad M. Pathological sequelae of long-haul COVID. Nat Immunol. (2022) 23:194–202. doi: 10.1038/s41590-021-01104-y
3. Soriano JB, Murthy S, Marshall JC, Relan P, Diaz JV, and WHO Clinical Case Definition Working Group on Post-COVID-19 Condition. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis. (2022) 22:e102–7. doi: 10.1016/S1473-3099(21)00703-9
4. Centers for Disease Control and Prevention (USA). Post-COVID conditions: information for healthcare providers (2022). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-covid-conditions.html (Accessed January 10, 2025).
5. National Institute for Health and Care Excellence (NICE) UK. COVID-19 rapid guideline: managing the long-term effects of COVID-19 (2020). Available online at: https://www.nice.org.uk/guidance/ng188 (Accessed January 10, 2025).
6. Chen C, Haupert SR, Zimmermann L, Shi X, Fritsche LG, and Mukherjee B. Global prevalence of post-coronavirus disease 2019 (COVID-19) condition or long COVID: A meta-analysis and systematic review. J Infect Dis. (2022) 226:1593–607. doi: 10.1093/infdis/jiac136
7. O’Mahoney LL, Routen A, Gillies C, Ekezie W, Welford A, Zhang A, et al. The prevalence and long-term health effects of Long COVID among hospitalized and non-hospitalized populations: A systematic review and meta-analysis. eClinicalMedicine. (2022) 55:101762. doi: 10.1016/j.eclinm.2022.101762
8. Tsampasian V, Elghazaly H, Chattopadhyay R, Debski M, Naing TKP, Garg P, et al. Risk factors associated with post-COVID-19 condition: A systematic review and meta-analysis. JAMA Intern Med. (2023) 183:566–80. doi: 10.1001/jamainternmed.2023.0750
9. Jassat W, Reyes LF, Munblit D, Caoili J, Bozza F, Hashmi M, et al. Long COVID in low-income and middle-income countries: the hidden public health crisis. Lancet. (2023) 402:1115–7. doi: 10.1016/S0140-6736(23)01685-9
10. Mehta N, Ndhlovu CE, and Makadzange T. Does long COVID exist in sub-saharan africa? COVID. (2023) 3:1024–30. doi: 10.3390/covid3070074
11. Abraha HE, Gessesse Z, Gebrecherkos T, Kebede Y, Weldegiargis AW, Tequare MH, et al. Clinical features and risk factors associated with morbidity and mortality among patients with COVID-19 in northern Ethiopia. Int J Infect Dis. (2021) 105:776–83. doi: 10.1016/j.ijid.2021.03.037
12. Jassat W, Mudara C, Vika C, Welch R, and Arendse T. A cohort study of post-COVID-19 condition across the Beta, Delta, and Omicron waves in South Africa: 6-month follow-up of hospitalized and nonhospitalized participants. Int J Infect Dis. (2023) 128:102–11. doi: 10.1016/j.ijid.2022.12.036
13. Byambasuren O, Stehlik P, Clark J, Alcorn K, and Glasziou P. Effect of covid-19 vaccination on long covid: systematic review. BMJ Med. (2023) 2:e000385. doi: 10.1136/bmjmed-2022-000385
14. Watanabe A, Iwagami M, Yasuhara J, Takagi H, and Kuno T. Protective effect of COVID-19 vaccination against long COVID syndrome: A systematic review and meta-analysis. Vaccine. (2023) 41:1783–90. doi: 10.1016/j.vaccine.2023.02.008
15. Boufidou F, Medić S, Lampropoulou V, Siafakas N, Tsakris A, and Anastassopoulou C. SARS-coV-2 reinfections and long COVID in the post-omicron phase of the pandemic. Int J Mol Sci. (2023) 24:12962–80. doi: 10.3390/ijms241612962
16. Al-Aly Z, Bowe B, and Xie Y. Long COVID after breakthrough SARS-CoV-2 infection. Nat Med. (2022) 28:1461–7. doi: 10.1038/s41591-022-01840-0
17. Suhre K, Sarwath H, Engelke R, Sohail MU, Cho SJ, Whalen W, et al. Identification of robust protein associations with COVID-19 disease based on five clinical studies. Front Immunol. (2022) 12:781100. doi: 10.3389/fimmu.2021.781100
18. Laudanski K, Jihane H, Antalosky B, Ghani D, Phan U, Hernandez R, et al. Unbiased analysis of temporal changes in immune serum markers in acute COVID-19 infection with emphasis on organ failure, anti-viral treatment, and demographic characteristics. Front Immunol. (2021) 12:650465. doi: 10.3389/fimmu.2021.650465
19. Zoodsma M, de Nooijer AH, Grondman I, Gupta MK, Bonifacius A, Koeken VACM, et al. Targeted proteins identifies circulating biomarkers associated with active COVID-19 and post-COVID-19. Front Immunol. (2022) 13:1027122. doi: 10.3389/fimmu.2022.1027122
20. Cummings MJ, Bakamutumaho B, Lutwama JJ, Owor N, Che X, Astorkia M, et al. COVID-19 immune signatures in Uganda persist in HIV co-infection and diverge by pandemic phase. Nat Commun. (2024) 15:1475. doi: 10.1038/s41467-024-45204-3
21. Jacobs LMC, Wintjens MSJN, Nagy M, Willems L, Ten Cate H, Spronk HMH, et al. Biomarkers of sustained systemic inflammation and microvascular dysfunction associated with post-COVID-19 condition symptoms at 24 months after SARS-CoV-2-infection. Front Immunol. (2023) 14:1182182. doi: 10.3389/fimmu.2023.1182182
22. Kuijpers Y, Chu X, Jaeger M, Moorlag SJCFM, Koeken VACM, Zhang B, et al. The genetic risk for COVID-19 severity is associated with defective immune responses. Front Immunol. (2022) 13:859387. doi: 10.3389/fimmu.2022.859387
23. Filbin MR, Mehta A, Schneider AM, Kays KR, Guess JR, Gentili M, et al. Longitudinal protein analysis of severe COVID-19 reveals survival-associated signatures, tissue-specific cell death, and cell-cell interactions. Cell Rep Med. (2021) 2:100287. doi: 10.1016/j.xcrm.2021.100287
24. Feyaerts D, Hédou J, Gillard J, Chen H, Tsai ES, Peterson LS, et al. Integrated plasma protein and single-cell immune signalling network signatures demarcate mild, moderate, and severe COVID-19. Cell Rep Med. (2022) 3:100680. doi: 10.1016/j.xcrm.2022.100680
25. Shen B, Yi X, Sun Y, Bi X, Du J, Zhang C, et al. Protein and metabolomic characterization of COVID-19 patient sera. Cell. (2020) 182:59–72.e15. doi: 10.1016/j.cell.2020.05.032
26. Harriott NC and Ryan AL. Protein profiling identifies biomarkers of COVID-19 severity. Heliyon. (2023) 10:e23320. doi: 10.1016/j.heliyon.2023.e23320
27. Al-Nesf MAY, Abdesselem HB, Bensmail I, Ibrahim S, Saeed WAH, Mohammed SSI, et al. Prognostic tools and candidate drugs based on plasma proteins of patients with severe COVID-19 complications. Nat Commun. (2022) 13:946. doi: 10.1038/s41467-022-28639-4
28. Babačić H, Christ W, Araújo JE, Mermelekas G, Sharma N, Tynell J, et al. Comprehensive proteins and meta-analysis of COVID-19 host response. Nat Commun. (2023) 14:5921. doi: 10.1038/s41467-023-41159-z
29. Iosef C, Knauer MJ, Nicholson M, Van Nynatten LR, Cepinskas G, Draghici S, et al. Plasma protein of Long-COVID patients indicates HIF-mediated vasculo-proliferative disease with impact on brain and heart function. J Transl Med. (2023) 21:377. doi: 10.1186/s12967-023-04149-9
30. Alonso-Domínguez J, Gallego-Rodríguez M, Martínez-Barros I, Calderón-Cruz B, Leiro-Fernández V, Pérez-González A, et al. High levels of IL1β, TNF-α and MIP-1α One month after the onset of the acute SARS-coV-2 infection, predictors of post COVID-19 in hospitalized patients. Microorganisms. (2023) 11:2396. doi: 10.3390/microorganisms11102396
31. Zhao J, Schank M, Wang L, Dang X, Cao D, Khanal S, et al. Plasma biomarkers for systemic inflammation in COVID-19 survivors. Proteins Clin Appl. (2022) 16:e2200031. doi: 10.1002/prca.202200031
32. Su Y, Yuan D, Chen DG, Ng RH, Wang K, Choi J, et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell. (2022) 185:881–895.e20. doi: 10.1016/j.cell.2022.01.014
33. Yin K, Peluso MJ, Luo X, Thomas R, Shin MG, Neidleman J, et al. Long COVID manifests with T cell dysregulation, inflammation and an uncoordinated adaptive immune response to SARS-CoV-2. Nat Immunol. (2024) 25:218–25. doi: 10.1038/s41590-023-01724-6
34. Talla A, Vasaikar SV, Szeto GL, Lemos MP, Czartoski JL, MacMillan H, et al. Persistent serum protein signatures define an inflammatory subcategory of long COVID. Nat Commun. (2023) 14:3417. doi: 10.1038/s41467-023-38682-4
35. Woodruff MC, Bonham KS, Anam FA, Walker TA, Faliti CE, Ishii Y, et al. Chronic inflammation, neutrophil activity, and autoreactivity splits long COVID. Nat Commun. (2023) 14:4201. doi: 10.1038/s41467-023-40012-7
36. Wang K, Khoramjoo M, Srinivasan K, Gordon PMK, Mandal R, Jackson D, et al. Sequential multi-omics analysis identifies clinical phenotypes and predictive biomarkers for long COVID. Cell Rep Med. (2023) 4:101254. doi: 10.1016/j.xcrm.2023.101254
37. Ryan FJ, Hope CM, Masavuli MG, Lynn MA, Mekonnen ZA, Yeow AEL, et al. Long-term perturbation of the peripheral immune system months after SARS-CoV-2 infection. BMC Med. (2022) 20:26. doi: 10.1186/s12916-021-02228-6
38. Klein J, Wood J, Jaycox JR, Dhodapkar RM, Lu P, Gehlhausen JR, et al. Distinguishing features of long COVID identified through immune profiling. Nature. (2023) 623:139–48. doi: 10.1038/s41586-023-06651-y
39. Wolday D, Gebrecherkos T, Arefaine ZG, Kiros YK, Gebreegzabher A, Tasew G, et al. Effect of co-infection with intestinal parasites on COVID-19 severity: A prospective observational cohort study. EClinicalMedicine. (2021) 39:101054. doi: 10.1016/j.eclinm.2021.101054
40. Adjobimey T, Meyer J, Terkeš V, Parcina M, and Hoerauf A. Helminth antigens differentially modulate the activation of CD4+ and CD8+ T lymphocytes of convalescent COVID-19 patients in vitro. BMC Med. (2022) 20:241. doi: 10.1186/s12916-022-02441-x
41. Achan J, Serwanga A, Wanzira H, Kyagulanyi T, Nuwa A, Magumba G, et al. Current malaria infection, previous malaria exposure, and clinical profiles and outcomes of COVID-19 in a setting of high malaria transmission: an exploratory cohort study in Uganda. Lancet Microbe. (2022) 3:e62–71. doi: 10.1016/S2666-5247(21)00240-8
42. Fonte L, Acosta A, Sarmiento ME, Norazmi MN, Ginori M, de Armas Y, et al. Overlapping of pulmonary fibrosis of postacute COVID-19 syndrome and tuberculosis in the helminth coinfection setting in sub-saharan Africa. Trop Med Infect Dis. (2022) 7:157. doi: 10.3390/tropicalmed7080157
43. Abdella S, Tessema M, Tasew G, Defar A, Deressa A, Regasa F, et al. Prognostic factors and outcomes of COVID-19 cases in Ethiopia: multi-center cohort study protocol. BMC Infect Dis. (2021) 21:956–62. doi: 10.1186/s12879-021-06652-0
44. International Severe Acute Respiratory and Emerging Infection Consortium (2020). ISARIC. Available online at: https://isaric.tghn.org/COVID-19-CRF/ (Accessed 28 August 2024). COVID-19 CRF.
45. World Health Organization. Report of the WHO–China Joint Mission on Coronavirus Disease 2019 (COVID-19) (2020). Geneva: WHO. Available online at: https://www.who.int/docs/default-source/coronaviruse/who-China-jointmission-on-covid-19-final-report.pdf (Accessed 28 August 2024).
46. Assarsson E, Lundberg M, Holmquist G, Björkesten J, Thorsen SB, Ekman D, et al. Homogenous 96-plex PEA immunoassay exhibiting high sensitivity, specificity, and excellent scalability. PloS One. (2014) 9:e95192. doi: 10.1371/journal.pone.0095192
47. Guo Y, You J, Zhang Y, Liu WS, Huang YY, Zhang YR, et al. Plasma protein profiles predict future dementia in healthy adults. Nat Aging. (2024) 4):247–60. doi: 10.1038/s43587-023-00565-0
48. Jones MR, Rouillard AD, Fernandez NF, Duan Q, Wang Z, et al. Enricher: a comprehensive gene set enrichment analysis web server 2016 update. Nucleic Acids Res. (2016) 44(W1):W90–W97. doi: 10.1093/nar/gkw377
49. Szklarczyk D, Kirsch R, Koutrouli M, Nastou K, Mehryary F, Hachilif R, et al. The STRING database in 2023: protein-protein association networks and functional enrichment analyses for any sequenced genome of interest. Nucleic Acids Res. (2023) 51:D638–46. doi: 10.1093/nar/gkac1000
50. Merkt S, Ali S, Gudina EK, Adissu W, Gize A, Muenchhoff M, et al. Long-term monitoring of SARS-CoV-2 seroprevalence and variants in Ethiopia provides prediction for immunity and cross-immunity. Nat Commun. (2024) 15:3463. doi: 10.1038/s41467-024-47556-2
51. Sisay A, Tshiabuila D, van Wyk S, Tesfaye A, Mboowa G, Oyola SO, et al. Molecular epidemiology and diversity of SARS-coV-2 in Ethiopia, 2020-2022. Genes. (2023) 14:705. doi: 10.3390/genes14030705
52. G/Meskel W, Desta K, Diriba R, Belachew M, Evans M, Cantarelli V, et al. SARS-CoV-2 variant typing using real-time reverse transcription-polymerase chain reaction-based assays in Addis Ababa, Ethiopia. IJID Reg. (2024) 11:100363. doi: 10.1016/j.ijregi.2024.100363
53. Tay MZ, Poh CM, Rénia L, MacAry PA, and Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. (2020) 20:363–74. doi: 10.1038/s41577-020-0311-8
54. Gerla L, Moitra S, Pink D, Govindasamy N, Duchesne M, Reklow E, et al. SARS-coV-2-induced TSLP is associated with duration of hospital stay in COVID-19 patients. Viruses. (2023) 15:556. doi: 10.3390/v15020556
55. Swedik S, Madola A, and Levine A. IL17C in human mucosal immunity: More than just a middle child. Cytokine. (2021) 146:155641. doi: 10.1016/j.cyto.2021.155641
56. Minnone G, De Benedetti F, and Bracci-Laudiero L. NGF and its receptors in the regulation of inflammatory response. Int J Mol Sci. (2017) 18:1028. doi: 10.3390/ijms18051028
57. Bachmann MF, Wong BR, Josien R, Steinman RM, Oxenius A, Choi Y, et al. TRANCE, a tumor necrosis factor family member critical for CD40 ligand-independent T helper cell activation. J Exp Med. (1999) 189:1025–31. doi: 10.1084/jem.189.7.1025
58. Etter MM, Martins TA, Kulsvehagen L, Pössnecker E, Duchemin W, Hogan S, et al. Severe Neuro-COVID is associated with peripheral immune signatures, autoimmunity and neurodegeneration: a prospective cross-sectional study. Nat Commun. (2022) 13:6777. doi: 10.1038/s41467-022-34068-0
59. Stein SR, Ramelli SC, Grazioli A, Chung JY, Singh M, Yinda CK, et al. SARS-CoV-2 infection and persistence in the human body and brain at autopsy. Nature. (2022) 612:758–63. doi: 10.1038/s41586-022-05542-y
60. Cheung CCL, Goh D, Lim X, Tien TZ, Lim JCT, Lee JN, et al. Residual SARS-CoV-2 viral antigens detected in GI and hepatic tissues from five recovered patients with COVID-19. Gut. (2022) 71:226–9. doi: 10.1136/gutjnl-2021-324280
61. Antar AAR, Yu T, Demko ZO, Hu C, Tornheim JA, Blair PW, et al. Long COVID brain fog and muscle pain are associated with longer time to clearance of SARS-CoV-2 RNA from the upper respiratory tract during acute infection. Front Immunol. (2023) 14:1147549. doi: 10.3389/fimmu.2023.1147549
62. Swank Z, Senussi Y, Manickas-Hill Z, Yu XG, Li JZ, Alter G, et al. Persistent circulating severe acute respiratory syndrome coronavirus 2 spike is associated with post-acute coronavirus disease 2019 sequelae. Clin Infect Dis. (2023) 76:e487–90. doi: 10.1093/cid/ciac722
63. Colebunders RL and Kenyon C. Extensive severe acute respiratory syndrome coronavirus 2 (SARS-coV-2) transmission associated with low mortality in kinshasa, democratic republic of the congo: for how long? Clin Infect Dis. (2022) 74:891–2. doi: 10.1093/cid/ciab593
64. Gudina EK, Ali S, Girma E, Gize A, Tegene B, Hundie GB, et al. Seroepidemiology and model-based prediction of SARS-CoV-2 in Ethiopia: longitudinal cohort study among front-line hospital workers and communities. Lancet Glob Health. (2021) 9:e1517–27. doi: 10.1016/S2214-109X(21)00386-7
65. Cummings MJ, Baldwin MR, Abrams D, Jacobson SD, Meyer BJ, Balough EM, et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet. (2020) 395:1763–70. doi: 10.1016/S0140-6736(20)31189-2
66. Garg S, Kim L, Whitaker M, O'Halloran A, Cummings C, Holstein R, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 – COVID-NET, 14 States, March 1-30, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:458–64. doi: 10.15585/mmwr.mm6915e3
67. Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. (2020) 323:1574–81. doi: 10.1001/jama.2020.5394
68. Müller SA, Isaaka L, Mumm R, Scheidt-Nave C, Heldt K, Schuster A, et al. Prevalence and risk factors for long COVID and post-COVID-19 condition in Africa: a systematic review. Lancet Glob Health. (2023) 11:e1713–24. doi: 10.1016/S2214-109X(23)00384-4
69. Thomas C, Faghy MA, Chidley C, Phillips BE, Bewick T, Ashton RE, et al. Blood biomarkers of long COVID: A systematic review. Mol Diagn Ther. (2024) 28:537–574. doi: 10.1007/s40291-024-00731-z
70. Lai YJ, Liu SH, Manachevakul S, Lee TA, Kuo CT, Bello D, et al. Biomarkers in long COVID-19: A systematic review. Front Med. (2023) 10:1085988. doi: 10.3389/fmed.2023.1085988
71. Espín E, Yang C, Shannon CP, Assadian S, He D, and Tebbutt SJ. Cellular and molecular biomarkers of long COVID: a scoping review. EBioMedicine. (2023) 91:104552. doi: 10.1016/j.ebiom.2023.104552
Keywords: COVID-19, SARS-CoV-2, critical, long Covid, Africa, low-income country, immune activation, inflammation
Citation: Wolday D, Gebrehiwot AG, Le Minh AN, Rameto MA, Abdella S, Gebreegziabxier A, Amogne W, Rinke de Wit TF, Hailu M, Tollera G, Tasew G, Tessema M, Miller M, Gillgrass A, Bowdish DME, Kaushic C and Verschoor CP (2025) Distinct proteomic signatures in Ethiopians predict acute and long-term sequelae of COVID-19. Front. Immunol. 16:1575135. doi: 10.3389/fimmu.2025.1575135
Received: 11 February 2025; Accepted: 21 April 2025;
Published: 22 May 2025.
Edited by:
Alexandre Keiji Tashima, Federal University of São Paulo, BrazilReviewed by:
Ivana Kawikova, National Institute of Mental Health, CzechiaErika Nishiduka, National Institutes of Health (NIH), United States
Copyright © 2025 Wolday, Gebrehiwot, Le Minh, Rameto, Abdella, Gebreegziabxier, Amogne, Rinke de Wit, Hailu, Tollera, Tasew, Tessema, Miller, Gillgrass, Bowdish, Kaushic and Verschoor. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dawit Wolday, d29sZGF5ZEBtY21hc3Rlci5jYQ==
 Dawit Wolday
Dawit Wolday Abrha G. Gebrehiwot1
Abrha G. Gebrehiwot1 An Nguyen Le Minh
An Nguyen Le Minh Atsbeha Gebreegziabxier
Atsbeha Gebreegziabxier Wondwossen Amogne
Wondwossen Amogne Messay Hailu
Messay Hailu Geremew Tasew
Geremew Tasew Masresha Tessema
Masresha Tessema Dawn M. E. Bowdish
Dawn M. E. Bowdish Chris P. Verschoor
Chris P. Verschoor