- 1Medical Microbiology Unit, Department of Laboratory Diagnostic and Investigative Sciences, Faculty of Medicine and Health Sciences, University of Zimbabwe, Harare, Zimbabwe
- 2Department of Medical Sciences, Botswana Harvard Health Partnership, Gaborone, Botswana
- 3School of Allied Health Sciences, Faculty of Health Sciences, Gaborone, Botswana
- 4Department of Applied Biology and Biochemistry, National University of Science and Technology, Bulawayo, Zimbabwe
- 5Immunology Unit, Department of Laboratory Diagnostic and Investigative Sciences, Faculty of Medicine and Health Sciences, University of Zimbabwe, Harare, Zimbabwe
- 6Department of Clinical Veterinary Sciences, Faculty of Veterinary Sciences, University of Zimbabwe, Harare, Zimbabwe
- 7Department of Immunology and Infectious Diseases, Harvard T.H. Chan School of Public Health, Boston, MA, United States
- 8School of Health Systems and Public Health, University of Pretoria, Pretoria, South Africa
- 9Division of Medical Virology, Faculty of Medicine and Health Sciences, Stellenbosch University, Tygerberg, South Africa
Introduction: The Mycobacterium avium complex (MAC)—comprising M. colombiense, M. avium, andM. intracellulare—is an emerging group of opportunistic pathogens responsible for significant morbidity and mortality, particularly in immunocompromised individuals. Despite this growing burden, no vaccines currently provide cross-species protection. In silico vaccine design offers a rapid, cost-effective strategy to identify immunogenic epitopes and assemble multi-epitope constructs with optimized safety and efficacy. Accordingly, we aimed to develop a candidate multi-epitope vaccine (MEV) targeting conserved antigens across multiple MAC species.
Methods: From a genomic survey of nontuberculous mycobacteria (NTM) in Zimbabwe, we assembled complete genomes for M. colombiense (MCOL), M. avium (MAV), and M. intracellulare (MINT). Using both local and global reference datasets, we screened the conserved immunodominant proteins 85A, 85B, and 85C for high-affinity T-helper lymphocyte (THL) epitopes. Promising epitopes were further evaluated for antigenicity, immunogenicity, physicochemical stability, and population coverage.
Results: Epitope mapping across the nine target proteins yielded 82 THL epitopes predicted to bind 13 MHC class II (DRB*) alleles, ensuring broad coverage within Zimbabwean and pan-African populations. Clustering analyses consolidated 26 unique epitopes into 11 consensus peptides, 65.4% of which derived from the 85B proteins. In silico immune simulations predicted robust humoral and cellular responses, including elevated IgG titers, T-helper and T-cytotoxic cell proliferation and increased secretion of IFN-γ and IL-2 following MEV administration.
Conclusion: These findings indicate that our construct possesses strong immunogenic potential and cross-species applicability. We present here a rationally designed MEV candidate that merits further experimental validation as a broad-spectrum vaccine against multiple MAC species.
1 Introduction
Mycobacterium avium complex (MAC) encompasses a group of twelve species of mycobacteria that are opportunistic pathogens responsible for significant morbidity and mortality in both humans and animals (1, 2). To improve on clarity, may we request change of this statement to 'MAC species cause pulmonary disease in humans and animals. They are clinically significant both in immunocompromised patients—such as people living with HIV/AIDS or those with chronic lung disease—and, less commonly, in otherwise healthy individuals. (3). In animals, MAC infections pose significant threats to livestock and wildlife resulting in economic losses and serving as potential reservoirs for zoonotic transmission (4, 5). Infections due to MAC species are increasing globally, particularly among immunocompromised individuals and patients with underlying lung disease, with notable prevalence reported in Australia, America, Europe, and Asia, thereby underscoring the urgent need for effective vaccine strategies worldwide (1, 3, 6–9). The growing global burden of MAC infections and multidrug resistance among MAC calls for an urgent and constant ‘One Health Approach’ in development of effective prevention and control strategies in both humans and animals (2). This vaccine development effort aligns with the ‘One Health approach’ addressing human, animal and environmental health by targeting pathogens at the human-animal-environment interface. Despite the widespread use of Bacillus Calmette–Guérin (BCG) as a vaccine for tuberculosis and also providing partial immunity to NTM infections, further studies to either increase the efficacy of the BCG/recombinant BCG vaccine or to create new vaccines or booster vaccines that induce an optimal immune response against NTM is required (10). To address this waning efficacy, booster vaccines are essential as they help achieve long-term immunity (11). However, the recent advances in vaccine technology, in silico predictions provide a more efficient, cost-effective alternative for screening candidate epitopes that can elicit strong immune responses, identifying and optimizing vaccine candidates used in the development of therapeutics and vaccines.
Given that effective vaccines must enhance immune mechanisms responsible for pathogen elimination, understanding the nature of pathogen clearance becomes essential. Pathogen clearance often relies on multi-specific, polyclonal, and robust T cell-mediated responses. Major histocompatibility complexes (MHCs), known as human leukocyte antigens (HLAs) in humans, are crucial for the host immune system, presenting antigenic peptides (epitopes) to CD8+ cytotoxic T cells (CTLs) and CD4+ T helper (Th) cells [Helper T-lymphocytes (HTL)] (12–14). HLA class I molecules present endogenous peptides to CTLs, while HLA class II molecules present exogenous peptides to HTLs (13). The HTLs have a key role in adaptive immunity. These activate the B-cells along with the CTLs for production of antibodies and eventually killing infected/damaged cells (15). The HTL epitopes for the selected protein can be calculated using the prediction tool for MHC-II epitope (http://tools.iedb.org/main/tcell/).
Epitope-based vaccines represent a novel approach for generating a specific immune response and avoiding responses against other unfavourable epitopes (like epitopes that may drive immunopathogenic or immune modulating responses) in the complete antigen. Potential advantages of epitope-based vaccines also include increased safety, the opportunity to rationally engineer the epitopes for increased potency and breadth, and the ability to focus immune responses on conserved epitopes (16, 17). The repertoire of peptides presented by HLAs is influenced by the structural features of the HLA binding groove and the peptide’s amino acid composition (18, 19). In silico tools can predict MHC-presented epitopes and profile immune escape mutations, though such analyses remain complex and underexplored for bacterial genomes. Additionally, pathogens frequently mutate within immunogenic epitopes to evade recognition by T cells and agents, posing significant challenges for developing potent vaccines and therapeutics for diseases like tuberculosis (TB) and others (20).
The antigen 85 (Ag85) complex, comprising a cascade of 85A, 85B, and 85C proteins is the main secretory antigen playing an important role in the pathogenicity of mycobacteria (21). Ag85 complex molecules are widely being explored as tools in diagnostic methods and in vaccine research including recombinant attenuated vaccines, DNA vaccines and subunit vaccines because of their ability to allow bacteria to evade host immune responses through preventing formation of phagolysosomes (21). These highly conserved fibronectin-binding proteins also promote immune responses in host by inducing the production of IFN-g and have been shown to confer protection against TB (22). Research into Ag85 proteins continues to hold great promise for improving TB vaccines, particularly in high-burden settings.
By leveraging computational approaches, it is possible to predict T-cell from MAC antigens, assess their immunogenicity, and design multi-epitope vaccine constructs. In this study, we utilized immunoinformatics to analyze the 85A, 85B, and 85C proteins of MAV, MINT and MCOL, the commonly found strains in Zimbabwe, to identify candidate epitopes for vaccine development. This work aims to contribute to the development of safe and effective vaccines to combat MAC infections in both humans and animals, addressing a critical need in the global fight against mycobacterial diseases.
2 Materials and methods
2.1 Screening for Ag85A-C genes of the three MAC species
From a genomic survey project using NTM samples in Zimbabwe, we generated complete MAV, MINT and MCOL genomes. These genomes provided a foundational dataset for vaccine modelling, enabling a genotyping approach through whole genome sequencing (WGS) to identify immunologically relevant targets. To enhance the multi-epitope vaccine design, we screened for Ag85A-C genes across the three MAC species. The amino acid sequences of the target proteins Ag85A, Ag85B, and Ag85C of MAV, MINT and MCOL were retrieved from the National Center for Biotechnology Information (NCBI) (https://www.ncbi.nlm.nih.gov) in FASTA format. Subsequently, the nine protein sequences were grouped into three multiple sequence alignments (MSAs), corresponding to Ag85A, Ag85B, and Ag85C for MAV, MINT, and MCOL. Each MSA was visualized using AliView (https://github.com/AliView/AliView), and conserved regions were identified from the alignments. The Epitope Conservancy Analysis tool, available through the Immune Epitope Database (IEDB; http://tools.iedb.org/conservancy/), was used to evaluate the variability of epitopes based on the sequence alignment of the three MAC species.
2.2 Prediction of T-cell and designing of the multi-epitope subunit vaccine
We used NetMHCIIpan 4.3 to predict MHC class II-binding peptides (NetMHCIIpan 4.3 - DTU Health Tech - Bioinformatic Services) for all the 3 MSA containing proteins (Ag85A, Ag85B, and Ag85C) for multiple MAC species. Epitope selection thresholds were based on established immunoinformatics criteria. Only epitopes that fulfilled multiple criteria, high antigenicity, strong MHC binding, and IFN-γ induction were shortlisted for vaccine construct design. These selection thresholds have been widely adopted in previous epitope-based vaccine design studies to ensure that the predicted peptides are likely to be immunogenic and broadly recognized across different HLA types (16, 17, 23). As a selection criteria, the strong binding promiscuous epitopes were considered for downstream analyses towards final vaccine construct. To enhance vaccine efficacy, the GPGPG linker was used to connect amino acid sequences, ensuring optimal individual functionality (23, 24). GPGPG linkers reduced junctional immunogenicity. Since immune adjuvants are a key requirement in vaccine formulation and play a critical role in enhancing the efficacy of vaccines, the Mycobacterium tuberculosis 50S ribosomal protein L7/L12 (RL7_MYCTU), P9WHE3 was retrieved from the UniProt database (https://www.uniprot.org/) and used as an adjuvant for the immune interaction based on its ability to act as an agonist for TLR437 (25). P9WHE3 was then integrated at the N-terminal of the construct and connected to the antigenic epitopes using the EAAAK linker to ensure improved expression, bioactivity stability and structural integrity (26, 27). The final vaccine construct was meticulously designed by assembling the adjuvant, epitopes, and linkers into a unified, functional structure to maintain the structural stability and immunological independence of the epitopes and adjuvant. To analyze epitope similarity with human surface proteins and minimize the risk of autoimmune reactions, BLASTp was also used. Epitopes with a similarity below 70% to human proteins are considered acceptable (28). The analysis was conducted using the BLASTp tool.
2.3 Determination of physicochemical characteristics, immunogenicity and allergenicity prediction
We evaluated the immunogenicity of the multiepitope subunits using the VaxiJen (VaxiJen v3.0) and the ANTIGENpro module of the SCRATCH protein predictor (Scratch Protein Predictor). Allergenicity was assessed with the AllerTOP v. 2.0 (29) and AlgPred servers (http://crdd.osdd.net/raghava/algpred/) to identify potential allergic reactions, ensuring the safety and efficacy of the predicted vaccine candidates. We used the ProtParam tool of the EXPASY database server (http://web.expasy.org/protparam/) to determine the physicochemical parameters (molecular weight, half-life, atomic composition, stability index and mean hydrophilicity) of the vaccine candidates’ antigens.
2.4 3D modelling of immunogenic polypeptides and protein subunits
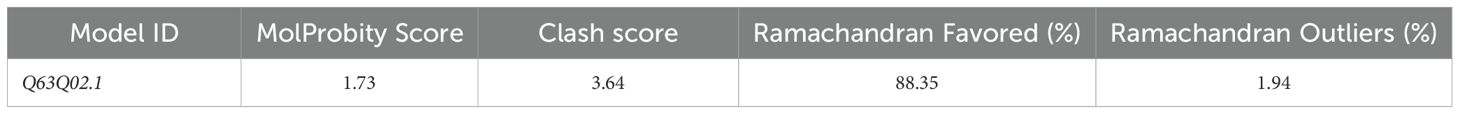
For ab initio modelling, we utilized the Swiss-model (SWISS-MODEL), submitting the designed full length chimeric peptide sequence with default settings. One model (Swiss-Model ID: Q63Q02.1) encompassed the entire multi-epitope construct, while the second returned only a truncated peptide fragment and was therefore excluded from further consideration. Model Q63Q02.1 was subsequently validated using MolProbity metrics—MolProbity score, clashscore, and Ramachandran analysis (Table 1)—to ensure stereochemical quality before downstream analyses. Functional insights into the targets were derived by rethreading the models through the BioLiP protein function database (BioLiP). The resulting 3D models were visually inspected using PyMOL (PyMOL | pymol.org) for structural validation and analysis. To further evaluate the protein’s flexibility and dynamics, Normal Mode Analysis (NMA) was performed using the iMODS server (https://imods.iqf.csic.es/), which provided insights into residue coupling through the covariance matrix and defined the elastic network model to identify regions of rigidity and flexibility based on the stiffness of atomic interactions.
2.5 Population coverage by HTL epitopes
Human leukocyte antigen (HLA) patterns differ across ethnic groups and geographical regions, making it essential to evaluate population coverage when designing effective vaccines. The IEDB population coverage tool (http://tools.iedb.org/population/) was used to calculate global human population coverage for the predicted HTL epitopes, ensuring their broad applicability. The 15-mer peptides overlapping by 14 amino acids were tested for binding to a set of 13 HLA class II alleles—HLA-DRB1*0101, DRB1*0301, DRB1*0302, DRB1*0401, DRB1*0701, DRB1*0802, DRB1*1101, DRB1*1102, DRB1*1301, DRB1*1302, DRB1*1501, and DRB5*0101—that have high population coverage in Zimbabwe and other African populations (http://www.allelefrequencies.net/hla6006a.asp?hla_population=2057).
3 Results
The amino acid sequences of nine proteins, 85A, 85B and 85C proteins of MAV, MINT and MCOL, were retrieved from the GenBank database to design a multi-epitope vaccine targeting MAC. The inclusion of Ag85 complex was guided by its high degree of conservation among mycobacterial species and its established immunogenicity as supported by its wide use in vaccine candidate development for TB (26, 30–32). Although nine proteins were selected, clustering and consensus analysis resulted in 11 distinct peptide sequences, reflecting inter-strain variability and epitope overlap. The eleven protein sequences were MSFIEKVRKLRGAAATMPR, MSFFEKLRGAAATMPRR, PRRLAIAAVGASLLSGVAVAAGGS, PRRLAIAAMGASLLSGL, RLAIAAVGASLLSGL, GLPVEYLEVPSPSMGRNI, SEKVRAWGRRLLVGAAAAVTLPGLIGIAGGAATAN, SEKVRAWGRRLLVGTAAAATLPG, AWGRRLVVGAAAAATLPGLIGLAGGAATAN, PGLPVEYLQVPSAGMGRNI and PVEYLQVPSAGMGRDIKVQFQS. SignalP 4.5 was used to assess functionality, revealing no signal peptides for proteins other than Ag85A/B/C. Functional protein sequences were then subjected to T-cell epitope prediction, identifying 17 high-affinity HTL epitopes for inclusion in the final vaccine construct. These epitopes overlapped with HTL epitopes (Table 2). A BLAST search against the UniProt database confirmed high conservation among the proteins, ranging from 27.7% to 100%.
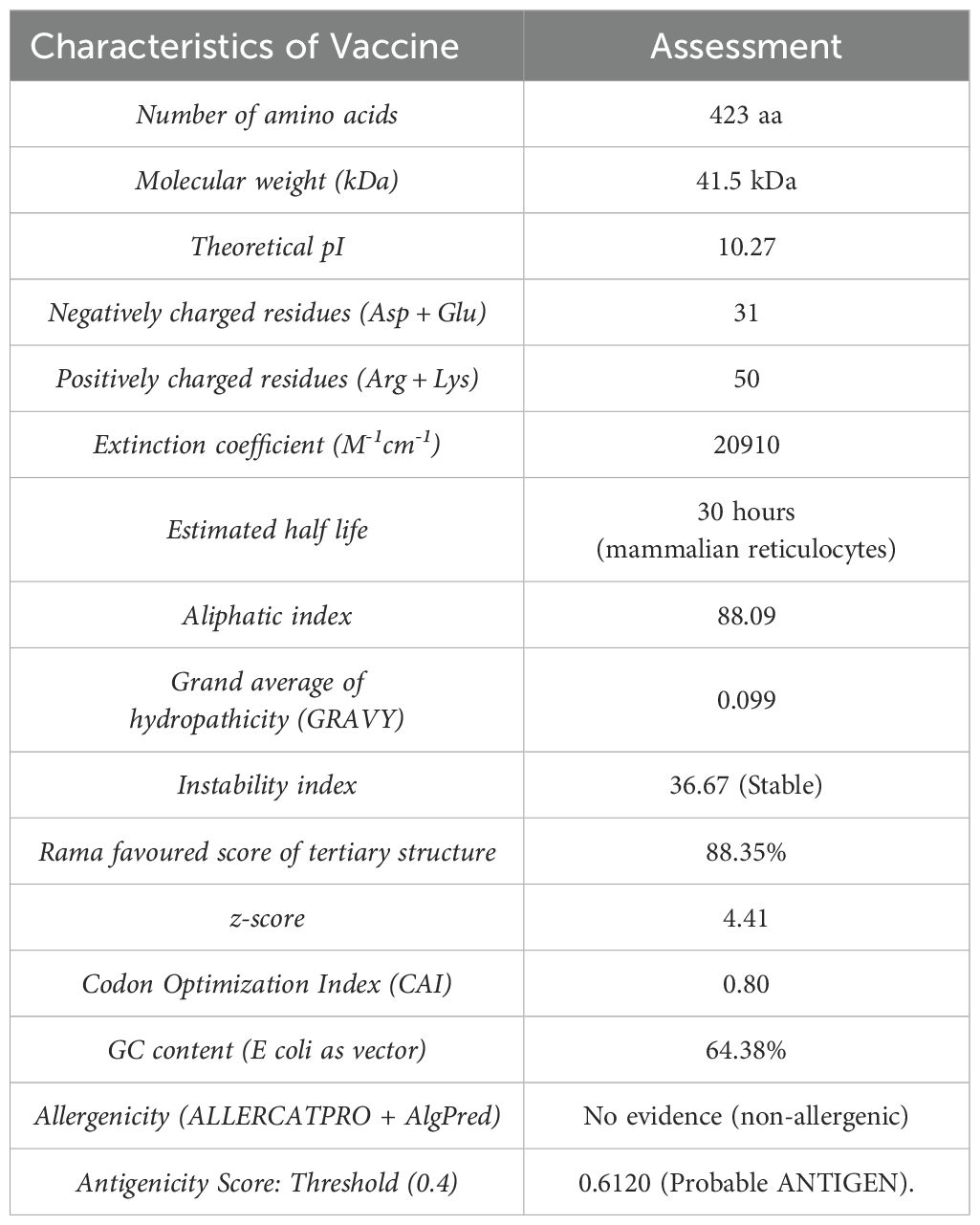
Table 2. Characteristics of the primary structure of proposed multi-epitope vaccine candidate for MAC species calculated through ProtParam tool.
3.1 Construction of multi-epitope subunit vaccine.
A total of 7 clusters of overlapping 14-mers high-binding HTL epitopes were predicted (Figure 1A). Consequently, 7 consensus sequences representing each cluster were generated at 100% threshold. These were used in designing the chimera using GPGPG linkers. Additionally, an adjuvant was added to the amino terminus of the vaccine peptide using an EAAAK linker in order to potentiate antigen-specific immune responses. The 50S ribosomal protein L7/L12 (RL7_MYCTU, UniProt ID: P9WHE3) was incorporated as an adjuvant at the N-terminal of the vaccine construct to enhance immunogenicity. The adjuvant RL7_MYCTU was an ideal adjuvant for enhancing cell-mediated immunity in this MEV vaccine construct as it is well-documented to have the ability to act as a potent immunostimulatory molecule inducing cytokine production, T cell activation and IFN-γ secretion (25). The final vaccine peptide generated consisted of 423 amino acid residues. The immunogenic peptide identified through epitope-mapping has been patented for further vaccine development.
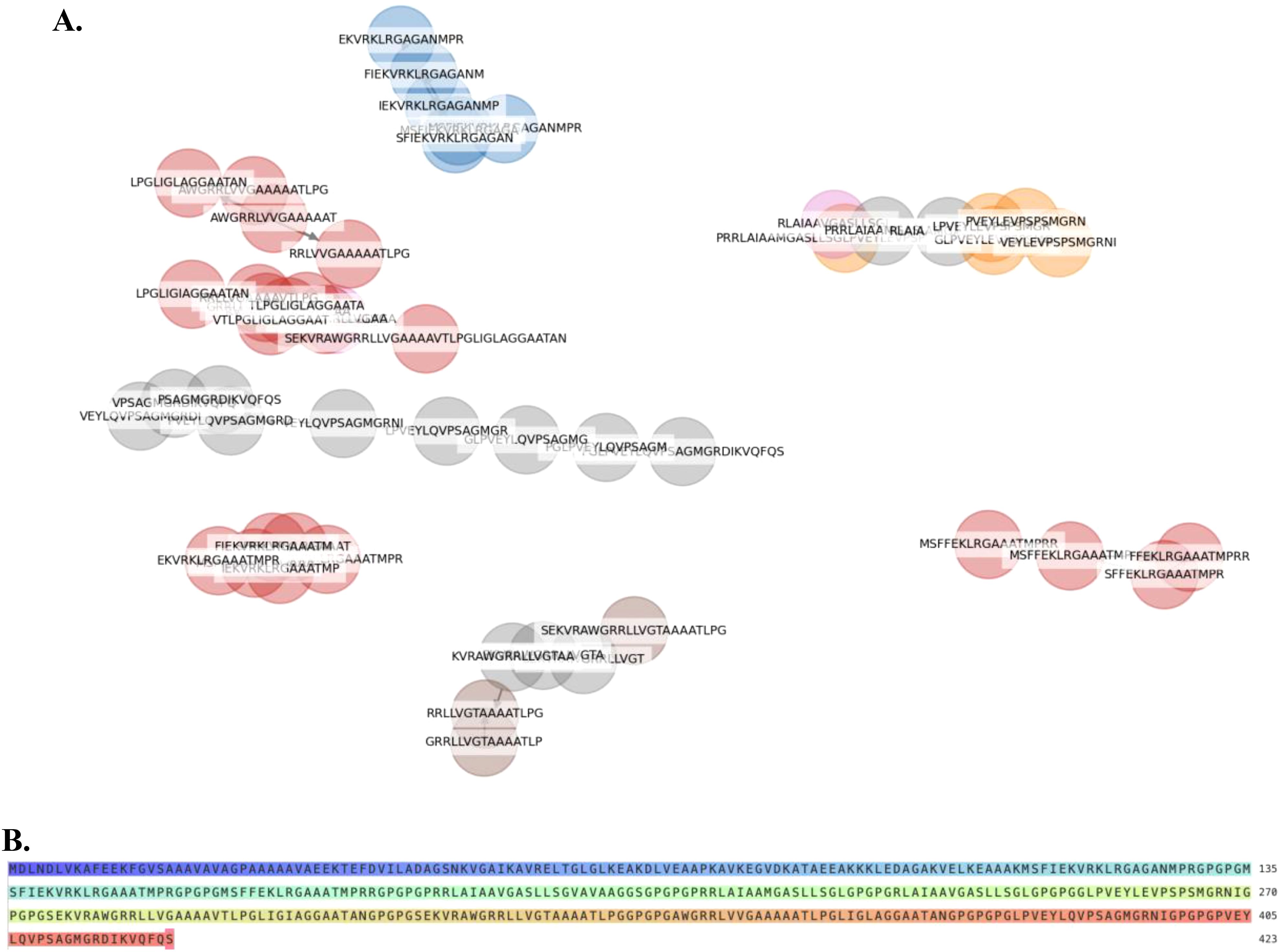
Figure 1. Helper T lymphocyte (HTL) Epitope Clustering and Multi-Epitope Vaccine Construct Design (A). Predicted HTL 14-mer epitopes were grouped into clusters based on sequence similarity of their core binding regions. (B) A multi-epitope-vaccine construct was designed using consensus sequences derived from each epitope cluster.
3.2 Physiochemical properties and solubility prediction
The molecular weight (MW), theoretical isoelectric point (pI), and half-life of the final protein [as assessed in mammalian reticulocytes (in vitro) and in yeast and E. coli (in vivo)] is summarized in Table 2. The protein demonstrated good solubility upon expression, with a solubility score and an Abs 0.1% (1 g/L) value of 0.505. Furthermore, the instability index (II) was calculated as 36.67, classifying the protein as stable, as proteins with an II >40 are typically considered unstable.
3.3 Secondary-structure analysis and tertiary-structure modeling of the chimeric MEV construct using Swiss-model server
The Swiss-Model server was used to generate the two tertiary structure models for the designed chimeric protein. Among these, the MSVQ63Q02.1 model was identified as the best as it represented the full-length MEV construct and achieved a favorable MolProbity score (1.73) and low clashscore (3.64) and thus was selected for presentation (Table 1, Figure 2A). Ramachandran plot analysis indicated that 88.35% of the residues were in favoured regions, with only 1.94% in disallowed regions (Table 1, Figure 2Bb). The quality and accuracy of the refined 3D model were evaluated using ProSA-web and ERRAT. The ERRAT analysis reported an overall quality factor of 97.5% (Figure 2C), while ProSA-web yielded a Z-score of -4.41 (Figure 2D), confirming the reliability of the refined vaccine protein model. The internal dynamics of the MEV model were further examined using normal mode analysis (NMA) via the iMODS server. The covariance matrix (Figure 2E) illustrated patterns of correlated and anti-correlated motions between residues, while the elastic network model (Figure 2F) highlighted stiffness variations across residue connections, indicating regions of structural rigidity and flexibility.

Figure 2. Protein 3D modelling, refinement and validation of designed MEV. (A) 3D structure of LpKWTc001 multi-epitope-based vaccine design for MAC species. (B) Ramachandran plot (C) ERRAT analysis report. (D) Xray based on ProSA (Protein Structural Analysis). The Z-score (dark spot) value was 4.41, within NMR (dark blue) and X-ray (light blue. (E) Covariance matrix indicating coupling between pairs of residues, i.e. whether they experience correlated (red), uncorrelated (white) or anti-correlated (blue) motions. (F) The elastic network model defining which pairs of atoms are connected by springs. Dots are coloured according to their stiffness, the darker greys indicate stiffer springs and vice versa.
3.4 IFN-γ inducing epitope prediction
This prediction was consistent with the simulated level of IFN-γ produced after immunization with the peptide using the C-ImmSim server (http://150.146.2.1/C-IMMSIM/index.php). The MEV model we designed managed to elicit a significant increase in T cell population following immunization. Furthermore, the antibody levels (IgM+IgG, IgG1+IgG2, IgM, and IgG) were found to increase during immunizations, accompanied by a decrease in antigen count (Figure 3A). Additionally, both CTL and HTL populations increased following secondary and tertiary immunization (Figures 3B–D).
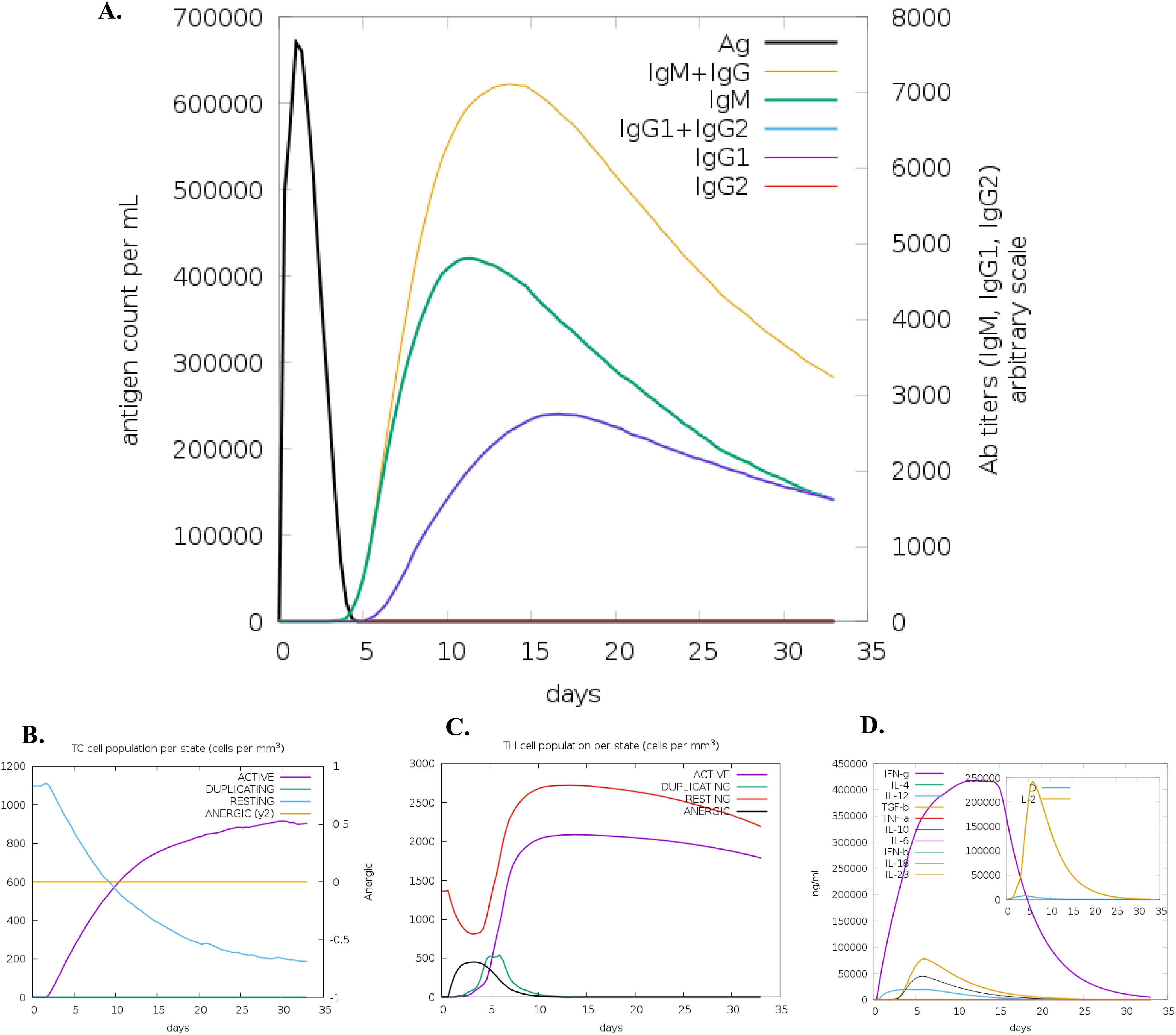
Figure 3. C-ImmSim simulation of the cytokine levels induced by the vaccine. (A) Antigen and immunoglobulins (antibodies are sub-divided per isotype); (B) CD8 T-cytotoxic lymphocytes count per entity-state; (C) T helper (TH) cell population, and (D) Concentration of cytokines and interleukins.
3.5 Codon optimization and the in vitro expression simulations
The Codon Optimization Tool (ExpOptimizer) tool (https://www.novoprolabs.com/tools/codon-optimization), was used for the multi-epitope vaccine model to enhance efficient translation and optimization of the codons for maximal expression in the prokaryotic host system E. coli (strain K12). In codon-optimized sequences of the designed vaccine (MEV-LpKwTC001), the codon adaptation index values were 0.80, and the GC content value 64.14%. Additionally, the adapted codon sequences were optimized with sticky end restriction sites of HindIII and NcoI at the N-terminus and C-terminus to facilitate restriction and cloning and inserted into the recombinant plasmid vector, pET-30a (+), using the Snapgene tool to design and effective cloning strategy (Figure 4).
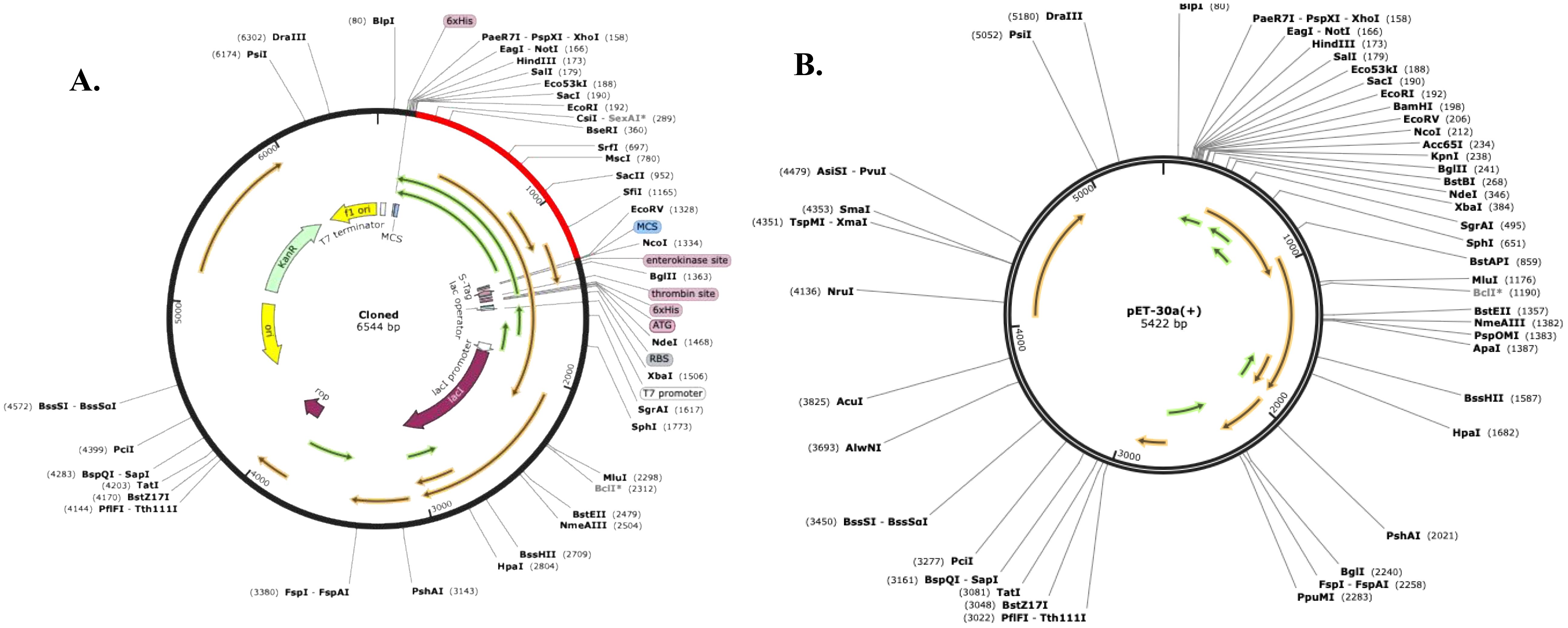
Figure 4. Codon optimisation and in silico restriction cloning of the multiple-epitope vaccine construct into the expression vector pET30a(+). The codon sequence of each multi-epitope vaccine was inserted in the multiple cloning site (MCS) of the (A) pET30a(+) expression vector using the Snapgene sequence alignment tool; (B) Final clone with fragment MEV-LpKwTC001.
4 Discussion
Paediatric administration of BCG vaccine is practiced in Zimbabwe. However, with M. tuberculosis being endemic and with the rise of NTM infections, there is a great need for new vaccines and booster vaccines for the BCG vaccines to fight both tuberculosis in adults as well as NTM infections particularly MAC infections. The rise of drug-resistant mycobacteria, limited BCG efficacy, and the need for vaccines targeting both humans and animals highlight significant challenges (33–35). The focus has recently shifted towards the development of subunit vaccines as they are associated with better safety profiles and are logistically more feasible, effective vaccines candidates that can be used to control MAC-related infections (36). Bioinformatics (in silico) is a good option to be used in designing and development of vaccines and diagnostics for newly emerged pathogens. The use of this approach reduces the time and cost. In order to construct a potent vaccine and effective diagnosis, understanding of the epitope and antibody interaction is required.
This work therefore focused on the in-silico design and development of a multi-epitope vaccine peptide generated using different MAC species (MCOL, MAV, MINT) and antigens (85A, 85B, and 85C) and has a potential for cross-protection (prophylactic and therapeutic). The proteins that we selected had exhibited potential to be vaccine candidates for in vitro studies (32). Epitope mapping of Ag85 protein complex has identified distinct peptides capable of stimulating human T cells, highlighting specific regions that could potentially trigger protective immune responses (37). More than 50% of vaccine candidates development for TB to date, some in advanced clinical trials, incorporated Ag85 (32). Conservation of the Ag85 complex across mycobacterial species also highlights their potential for cross-protection against related pathogens, including those in the MAC (30, 31).
We identified THL epitopes from selected proteins and fused them using linkers to create a multi-epitope peptide. Immuno-informatics showed the vaccine candidate contains many high-affinity MHC Class II epitopes from ag85B. Notably, multi-epitope vaccines are often poorly immunogenic and typically require adjuvants (38, 39); however, the designed protein demonstrated comparable antigenicity scores with or without an added adjuvant sequence. The antigenicity of the final sequence (including the adjuvant sequence) was shown to be probable antigen with a bacteria and also to be non-allergenic. we identified epitopes with accessibility, flexibility, hydrophilicity, and antigenic profiles for the Ag85. The vaccine candidate has a molecular weight of 41.5 kDa and is predicted to be soluble upon expression, aligning with its simulated immunogenicity. Solubility in an E. coli host is crucial for biochemical and functional studies.
Based on the predicted GRAVY score, which assesses maintenance ability in hydrophilic or hydrophobic environments, our MEV model displayed negative GRAVY value, suggesting a higher structural stability in a hydrophilic environment. This aspect can be correlated with solubility, critical in determining in vitro protein expression. Consequently, MEV-LpKwTC001, which demonstrated the highest solubility score, was selected for expression in E. coli. Furthermore, the predicting protein solubility is crucial for the selection of highly effective candidate proteins, as it can help avoid protein aggregation, which adversely affects biological activity and can lead to failures in the recombinant protein pipeline. The theoretical pI of 10.27 indicates the protein is alkaline, and the predicted instability index confirms its stability upon expression. The aliphatic index highlights the presence of hydrophobic aliphatic side chains, suggesting thermal stability, which is ideal for use in endemic regions like sub-Saharan Africa. These properties show that this is a potential vaccine design. To the best of our knowledge, no vaccine candidate is in phase III, nor licensed for use in the NTM infection with MAC species. To improve the immunogenicity of the vaccine antigen, we inserted adjuvant and linker sequences between the previously predicted epitopes to increase antigenicity. The fact that it has no allergenic properties further confirms its potential as a vaccine candidate.
Secondary structure analysis shows the protein is primarily composed of coils (67%), with 48% of residues disordered. These structural features, including natively unfolded regions and alpha-helical coiled coils, are known to serve as “structural antigens” capable of folding into native structures and being recognized by infection-induced antibodies. To evaluate conformational changes of the MEV, protein flexibility was examined using NMA. The MEV showed that a greater part of its peptide chains have high rigid regions which are crucial in the protein’s functional dynamics. The 3D structure, refined to improve its quality, exhibited favourable characteristics in the Ramachandran plot, with 85.16% of residues in allowed regions and minimal outliers, confirming the model’s reliability and suitability for vaccine design.
Immune simulation showed responses typical of a strong immune reaction, with increased activity after repeated antigen exposure. Following infection with MAC species, IgG1, IgG3, and IgE antibodies are critical for protection, and the vaccine candidate effectively stimulated memory B-cells and T-cells, with B-cell memory lasting several months. The simulations show that THL cells were strongly activated, and levels of IFN-γ and IL-2 spiked after the first injection, staying high with subsequent doses. This suggests strong TH cell activity and efficient antibody production, supporting a robust humoral response. The diversity of the immune response, indicated by the Simpson index, reflects the chimeric peptide’s design, which includes multiple B and T-cell epitopes. The dominant IFN-γ-driven TH1-type response, seen in naturally immune individuals, involves higher levels of TH1 cells, cytotoxic CD8+ T cells, neutrophils, and macrophages, further highlighting the vaccine’s potential effectiveness.
After obtaining the candidate vaccine, validating a candidate vaccine begins with screening for immunoreactivity using serological analysis, which requires expressing the recombinant protein in a suitable host. E coli expression systems, particularly strain K12, are preferred for producing recombinant proteins. To ensure high-level expression of the vaccine protein, codon optimization was performed in silico, yielding a favourable codon adaptability index (0.80) and GC content (64.14%).
While our vaccine candidate demonstrated favourable protein characteristics and strong immunogenicity, our study had certain limitations. Since the candidate was designed using human MHC epitopes, its efficacy must be assessed in a humanized mouse model. Additionally, we did not evaluate vaccine efficacy in vitro, which remains a limitation of our approach. However, this work represents a crucial foundational step toward experimental vaccine development. Notably, similar multi-epitope vaccines designed through utilization of immunoinformatic tools in silico have demonstrated strong immunogenicity in both in vitro and in vivo models, supporting the reliability of these methods (40–42). Moving forward, to advance the development of a preventive and therapeutic vaccine for MAC, we will validate the proposed vaccine through in vivo and in vitro studies to corroborate the predicted immunogenic potential.
Additionally, population coverage analysis for our vaccine candidate focused on HLA-DRB alleles. While this approach provides a robust estimation of coverage in African populations, the exclusion of HLA-DQ and HLA-DP loci may result in an underestimation of total MHC class II diversity, particularly in non-African populations. Future studies incorporating these additional loci are warranted to refine global population coverage estimates.
This study highlights a novel vaccine construct capable of eliciting a strong immune response against MAC species, potentially serving as a prototype for vaccines targeting other emerging infectious diseases. Vaccination is an important strategy to induce an immune response against the pathogen by specifically inducing the adaptive immune system. However, current challenges such as the absence of approved vaccines for MAC species, limited epitope-based research, and the lengthy development timelines and high costs associated with traditional vaccine approaches present significant gaps. Addressing these gaps is essential for comprehensive disease control and the reduction of MAC-associated morbidity across human and animal populations. This approach accelerates and lowers the cost of developing diagnostics and vaccines for MAC species, aiding future studies on epitope-based solutions to tackle the NTM challenge.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://www.ncbi.nlm.nih.gov/, BioProject ID PRJNA1205738.
Ethics statement
Joint Research Ethics Committee (JREC; under Approval No. JREC/168/22, dated 02.03.2023), Medical Research Council of Zimbabwe (MRCZ; under Approval No. MRCZ/A/29/03, dated 13.06.2023) and Zimbabwe’s National Animal Research and Ethics Committee (NAREC). The studies were conducted in accordance with the local legislation and institutional requirements. The human samples used in this study were acquired from a by- product of routine care or industry. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
LK: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. WC: Data curation, Formal Analysis, Software, Validation, Visualization, Writing – review & editing. TM: Investigation, Writing – review & editing. PN: Conceptualization, Methodology, Supervision, Writing – review & editing. RG: Supervision, Writing – review & editing. LZ: Funding acquisition, Project administration, Resources, Supervision, Writing – review & editing. NM: Conceptualization, Investigation, Methodology, Supervision, Writing – review & editing. SG: Formal Analysis, Writing – review & editing. SM: Data curation, Formal Analysis, Funding acquisition, Resources, Software, Validation, Visualization, Writing – review & editing. NC: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Research reported in this presentation was supported by the Trials of Excellence in Southern Africa (TESA) Addressing Gender and Diversity Regional Gaps in Clinical Research Capacity (TAGENDI) Project funded by the European and Developing Countries Clinical Trials Partnership (EDCTP) in partnership with the United Kingdom Department of Health and Social Care Award Number PSIA2020AGDG-3319. The content is solely the author’s responsibility and does not necessarily represent the official views of the funders.
Acknowledgments
The authors are grateful to EDCTP through TAGENDI Fellowship, the University of Zimbabwe, Medical Microbiology Unit, Department of Laboratory Diagnostic and Investigative Sciences, Faculty of Medicine and Health Sciences, Biomedical Research and Training Institute (BRTI), National Microbiology Reference Laboratories, Harare and National TB Reference Laboratories, Bulawayo, through the Ministry of Health and Child Care, Zimbabwe and Botswana Harvard AIDS Institute Partnership, Gaborone, Botswana.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Nishiuchi Y, Iwamoto T, and Maruyama F. Infection sources of a common non-tuberculous mycobacterial pathogen, mycobacterium avium complex. Front Med. (2017) 4:27. doi: 10.3389/fmed.2017.00027
2. Kaczmarkowska A, Didkowska A, Kwiecień E, Stefańska I, Rzewuska M, and Anusz K. The Mycobacterium avium complex – an underestimated threat to humans and animals. Ann Agric Environ Med. (2022) 29:22–7. doi: 10.26444/aaem/136398
3. Bhanushali J, Jadhav U, Ghewade B, and Wagh P. Unveiling the clinical diversity in nontuberculous mycobacteria (NTM) infections: A comprehensive review. Cureus. (2023) 15:e48270. doi: 10.7759/cureus.48270
4. Thorel MF, Huchzermeyer H, Weiss R, and Fontaine JJ. Mycobacterium avium infections in animals. Literature review. Vet Res. (1997) 28:439–47.
5. Inderlied CB, Kemper CA, and Bermudez LE. The Mycobacterium avium complex. Clin Microbiol Rev. (1993) 6:266–310. doi: 10.1128/CMR.6.3.266
6. Hoefsloot W, Van Ingen J, Andrejak C, Ängeby K, Bauriaud R, Bemer P, et al. The geographic diversity of nontuberculous mycobacteria isolated from pulmonary samples: an NTM-NET collaborative study. Eur Respir J. (2013) 42:1604–13. doi: 10.1183/09031936.00149212
7. Wetzstein N, Diricks M, Anton TB, Andres S, Kuhns M, Kohl TA, et al. Clinical and genomic features of Mycobacterium avium complex: a multi-national European study. Genome Med. (2024) 16:86. doi: 10.1186/s13073-024-01359-8
8. Prevots DR and Marras TK. Epidemiology of human pulmonary infection with nontuberculous mycobacteria. Clin Chest Med. (2015) 36:13–34. doi: 10.1016/j.ccm.2014.10.002
9. Adjemian J, Daniel-Wayman S, Ricotta E, and Prevots DR. Epidemiology of nontuberculous mycobacteriosis. Semin Respir Crit Care Med. (2018) 39:325–35. doi: 10.1055/s-0038-1651491
10. Orujyan D, Narinyan W, Rangarajan S, Rangchaikul P, Prasad C, Saviola B, et al. Protective Efficacy of BCG Vaccine against Mycobacterium leprae and Non-Tuberculous Mycobacterial Infections. Vaccines. (2022) 10:390. doi: 10.3390/vaccines10030390
11. Tao ZX, Li RP, Song YY, and Xu A. Basic immunization of vaccines is fundamental, and booster immunization is the guarantee: Booster immunization and its public health value. Zhonghua Yu Fang Yi Xue Za Zhi. (2022) 56:1401–10. doi: 10.3760/cma.j.cn112150-20220727-00760
12. Adegboro B, Kolawole OM, Lawani O, Folahan F, and Seriki AA. A review of the roles of Major Histocompatibility Complex (MHC) molecules in infections. Afr J Clin Exp Microbiol. (2022) 23:120–30. doi: 10.4314/ajcem.v23i2.2
13. Krensky AM. The HLA system, antigen processing and presentation. Kidney Int Suppl. (1997) 58:S2–7.
14. Thio CL, Thomas DL, Karacki P, Gao X, Marti D, Kaslow RA, et al. Comprehensive analysis of class I and class II HLA antigens and chronic hepatitis B virus infection. J Virol. (2003) 77:12083–7. doi: 10.1128/JVI.77.22.12083-12087.2003
15. Gaseitsiwe S and Maeurer MJ. Identification of MHC class II binding peptides: microarray and soluble MHC class II molecules. Methods Mol Biol Clifton NJ. (2009) 524:417–26. doi: 10.1007/978-1-59745-450-6_30
16. Pitaloka DAE, Izzati A, Amirah SR, and Syakuran LA. Multi epitope-based vaccine design for protection against mycobacterium tuberculosis and SARS-coV-2 coinfection. Adv Appl Bioinforma Chem. (2022) 15:43–57. doi: 10.2147/AABC.S366431
17. Zaib S, Rana N, Areeba, Hussain N, Alrbyawi H, Dera AA, et al. Designing multi-epitope monkeypox virus-specific vaccine using immunoinformatics approach. J Infect Public Health. (2023) 16:107–16. doi: 10.1016/j.jiph.2022.11.033
18. Sinigaglia F and Hammer J. Defining rules for the peptide-MHC class II interaction. Curr Opin Immunol. (1994) 6:52–6. doi: 10.1016/0952-7915(94)90033-7
19. Nielsen M, Andreatta M, Peters B, and Buus S. Immunoinformatics: predicting peptide–MHC binding. Annu Rev BioMed Data Sci. (2020) 3:191–215. doi: 10.1146/annurev-biodatasci-021920-100259
20. Ernst JD. Antigenic variation and immune escape in the MTBC. Adv Exp Med Biol. (2017) 1019:171–90. doi: 10.1007/978-3-319-64371-7_9
21. Karbalaei Zadeh Babaki M, Soleimanpour S, and Rezaee SA. Antigen 85 complex as a powerful Mycobacterium tuberculosis immunogene: Biology, immune-pathogenicity, applications in diagnosis, and vaccine design. Microb Pathog. (2017) 112:20–9. doi: 10.1016/j.micpath.2017.08.040
22. Yuk JM and Jo EK. Host immune responses to mycobacterial antigens and their implications for the development of a vaccine to control tuberculosis. Clin Exp Vaccine Res. (2014) 3:155–67. doi: 10.7774/cevr.2014.3.2.155
23. Livingston B, Crimi C, Newman M, Higashimoto Y, Appella E, Sidney J, et al. A rational strategy to design multiepitope immunogens based on multiple th lymphocyte epitopes1. J Immunol. (2002) 168(11):5499–506. doi: 10.4049/jimmunol.168.11.5499
24. Chao P, Zhang X, Zhang L, Yang A, Wang Y, and Chen X. Proteomics-based vaccine targets annotation and design of multi-epitope vaccine against antibiotic-resistant Streptococcus gallolyticus. Sci Rep. (2024) 14:4836. doi: 10.1038/s41598-024-55372-3
25. Lee SJ, Shin SJ, Lee MH, Lee MG, Kang TH, Park WS, et al. A potential protein adjuvant derived from mycobacterium tuberculosis rv0652 enhances dendritic cells-based tumor immunotherapy. PloS One. (2014) 9:e104351. doi: 10.1371/journal.pone.0104351
26. Yun JS, Kim AR, Kim SM, Shin E, Ha SJ, Kim D, et al. In silico analysis for the development of multi-epitope vaccines against Mycobacterium tuberculosis. Front Immunol. (2024) 15:1474346. doi: 10.3389/fimmu.2024.1474346
27. Meza B, Ascencio F, Sierra-Beltrán AP, Torres J, and Angulo C. A novel design of a multi-antigenic, multistage and multi-epitope vaccine against Helicobacter pylori: An in silico approach. Infect Genet Evol. (2017) 49:309–17. doi: 10.1016/j.meegid.2017.02.007
28. Adianingsih O and Kharisma V. Study of B cell epitope conserved region of the Zika virus envelope glycoprotein to develop multi-strain vaccine. J Appl Pharm Sci. (2019) 9:98–103. doi: 10.7324/JAPS.2019.90114
29. Dimitrov I, Bangov I, Flower DR, and Doytchinova I. AllerTOP v.2—a server for in silico prediction of allergens. J Mol Model. (2014) 20:2278. doi: 10.1007/s00894-014-2278-5
30. Belisle JT, Vissa VD, Sievert T, Takayama K, Brennan PJ, and Besra GS. Role of the major antigen of Mycobacterium tuberculosis in cell wall biogenesis. Science. (1997) 276:1420–2. doi: 10.1126/science.276.5317.1420
31. Chugh S, Bahal RK, Dhiman R, and Singh R. Antigen identification strategies and preclinical evaluation models for advancing tuberculosis vaccine development. NPJ Vaccines. (2024) 9:1–21. doi: 10.1038/s41541-024-00834-y
32. Sachdeva KS and Chadha VK. TB-vaccines: Current status & challenges. Indian J Med Res. (2024) 160:338–45. doi: 10.25259/IJMR_1478_2024
33. Morrison H and McShane H. BCG: past, present and future direction. In: : Christodoulides M, editor. Vaccines for Neglected Pathogens: Strategies, Achievements and Challenges : Focus on Leprosy, Leishmaniasis, Melioidosis and Tuberculosis. Springer International Publishing, Cham (2023). p. 171–95. doi: 10.1007/978-3-031-24355-4_8
34. Qu M, Zhou X, and Li H. BCG vaccination strategies against tuberculosis: updates and perspectives. Hum Vaccines Immunother. (2021) 17(12):5284–95. doi: 10.1080/21645515.2021.2007711
35. McMurray DN. A coordinated strategy for evaluating new vaccines for human and animal tuberculosis. Tuberculosis. (2001) 81:141–6. doi: 10.1054/tube.2000.0265
36. Zhuang L, Ye Z, Li L, Yang L, and Gong W. Next-generation TB vaccines: progress, challenges, and prospects. Vaccines. (2023) 11:1304. doi: 10.3390/vaccines11081304
37. Launois P, Drowart A, Bourreau E, Couppie P, Farber CM, Van Vooren JP, et al. T Cell Reactivity against Mycolyl Transferase Antigen 85 of M. tuberculosis in HIV-TB Coinfected Subjects and in AIDS Patients Suffering from Tuberculosis and Nontuberculous Mycobacterial Infections. J Immunol Res. (2011) 2011:640309. doi: 10.1155/2011/640309
38. Ghaffar SA, Tahir H, Muhammad S, Shahid M, Naqqash T, Faisal M, et al. Designing of a multi-epitopes based vaccine against Haemophilius parainfluenzae and its validation through integrated computational approaches. Front Immunol. (2024) 15:1380732. doi: 10.3389/fimmu.2024.1380732
39. Facciolà A, Visalli G, Laganà A, and Pietro AD. An overview of vaccine adjuvants: current evidence and future perspectives. Vaccines. (2022) 10:819. doi: 10.3390/vaccines10050819
40. Invenção M da CV, de Macêdo LS, de Moura IA, Santos LAB de O, Espinoza BCF, de Pinho SS, et al. Design and immune profile of multi-epitope synthetic antigen vaccine against SARS-coV-2: an in silico and in vivo approach. Vaccines. (2025) 13:149. doi: 10.3390/vaccines13020149
41. Shehata MM, Mahmoud SH, Tarek M, Al-Karmalawy AA, Mahmoud A, Mostafa A, et al. In silico and in vivo evaluation of SARS-coV-2 predicted epitopes-based candidate vaccine. Molecules. (2021) 26:6182. doi: 10.3390/molecules26206182
Keywords: Epitopes, Mycobacterium avium complex, Vaccine, Antigen85, mycolyltransferase, Th1 helper T-cell, immunodominance, promiscuous epitopes
Citation: Kashiri L, Choga WT, Musasa T, Nziramasanga P, Gutsire RB, Zijenah LS, Mukarati NL, Gaseitsiwe S, Moyo S and Chin’ombe N (2025) In silico multi-epitope-based vaccine design for Mycobacterium avium complex species. Front. Immunol. 16:1589083. doi: 10.3389/fimmu.2025.1589083
Received: 06 March 2025; Accepted: 14 May 2025;
Published: 05 June 2025.
Edited by:
Gurudeeban Selvaraj, Aarupadai Veedu Medical College & Hospital, IndiaReviewed by:
Deeksha Tripathi, University of Rajasthan, IndiaMd Sadique Hussain, Uttaranchal University, India
Copyright © 2025 Kashiri, Choga, Musasa, Nziramasanga, Gutsire, Zijenah, Mukarati, Gaseitsiwe, Moyo and Chin’ombe. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Leah Kashiri, bHBhZHlhQG1lZHNjaC51ei5hYy56dw==; Wonderful T. Choga, d2Nob2dhQGJocC5vcmcuYnc=
 Leah Kashiri
Leah Kashiri Wonderful T. Choga
Wonderful T. Choga Tinashe Musasa1
Tinashe Musasa1 Norman L. Mukarati
Norman L. Mukarati Simani Gaseitsiwe
Simani Gaseitsiwe Sikhulile Moyo
Sikhulile Moyo Nyasha Chin’ombe
Nyasha Chin’ombe