- Department of Dermatology, Shanghai Skin Disease Hospital, Tongji University School of Medicine, Institute of Psoriasis, Tongji University School of Medicine, Shanghai, China
A 77-year-old Chinese male with a 10-year history of plaque psoriasis had recurrent episodes of symmetric hypertrophic verrucous plaques in the lower legs. The patient was monitored for the evolution of the disease over two years before he came to our attention. Because the lesions were resistant to topical glucocorticoids and vitamin D3 at another dermatological center, the patient was treated with secukinumab for one year. However, the verrucous lesions further worsened, and the patient visited the outpatient department of our hospital in March 2023. Treatment with guselkumab was started. It immediately attenuated the plaques of the trunk and limbs. Surprisingly, the verrucous plaques of both legs showed complete resolution in 6 months.
Introduction
Verrucous psoriasis (VP) is a scarce variant characterized by a bizarre, papilloma-like appearance with wart-like thick scales (1). Although the etiology remains unclear, it develops from pre-existing psoriasis and may be associated with varicose veins in the lower extremities or dysfunction of metabolic conditions such as obesity and diabetes mellitus (2). There is a higher prevalence in men (3). VP is often resistant to therapy. Treatment options are limited and based on published case reports which include topical and systemic agents (4). Here, we report a case of VP in the lower legs superimposed on pre-existing psoriatic plaques, who was treated with guselkumab.
Case report
A 77-year-old Chinese male with a 10-year history of plaque psoriasis had recurrent episodes of symmetric hypertrophic verrucous plaques of both lower legs superimposed on pre-existing psoriatic plaques. The patient was monitored for the evolution of the disease over two years before he came to our attention. In 2022, his lower legs had become swollen and covered with thick scales. The lesions gradually became cobblestone-like and continued to worsen despite the administration of secukinumab for 1 year at another dermatological center. Therefore, the patient visited the inpatient department of our hospital in March 2023. This patient showed symmetric hypertrophic verrucous plaques of both lower legs accompanied by erythematous plaques affecting 76% of the whole body (Figures 1a–d). The patient’s psoriasis severity index (PASI) score was 33.5. He had a 10-year history of hypertension, a 10-year history of prostate hyperplasia and mild obesity (body mass index, 26.4).

Figure 1. Clinical features of the patient at the first visit. (a) erythematous plaques of the trunk, (b–d) aggregation of multiple extensive verrucous, yellowish–gray plaques with a scaly surface on erythematous plaques on both lower legs.
Before starting treatment, a comprehensive set of laboratory and instrumental tests, including chest X-ray, electrocardiogram (ECG), complete blood count, complete liver profile, creatinine, antinuclear antibody, acquired immunodeficiency syndrome screening, rapid plasma regain test, hepatitis B virus serologic markers, hepatitis C virus antibody, and tuberculosis assay, yielded negative results, except for C-reactive protein (31.10 mg/L) erythrocyte sedimentation (23 mm/h), and total IgE (108 IU/L). Moreover, staphylococcus aureus and proteus mirabilis were detected on verrucous lesions. A biopsy from a verrucous lesion of the left leg revealed hyperkeratosis, neutrophil infiltration in the corner layer, wart-like hyperplasia of the epidermis, microabscess formed by the accumulation of neutrophils in the spinous layer (Figures 2a, b), PAS staining (–), anti-acid staining (–).
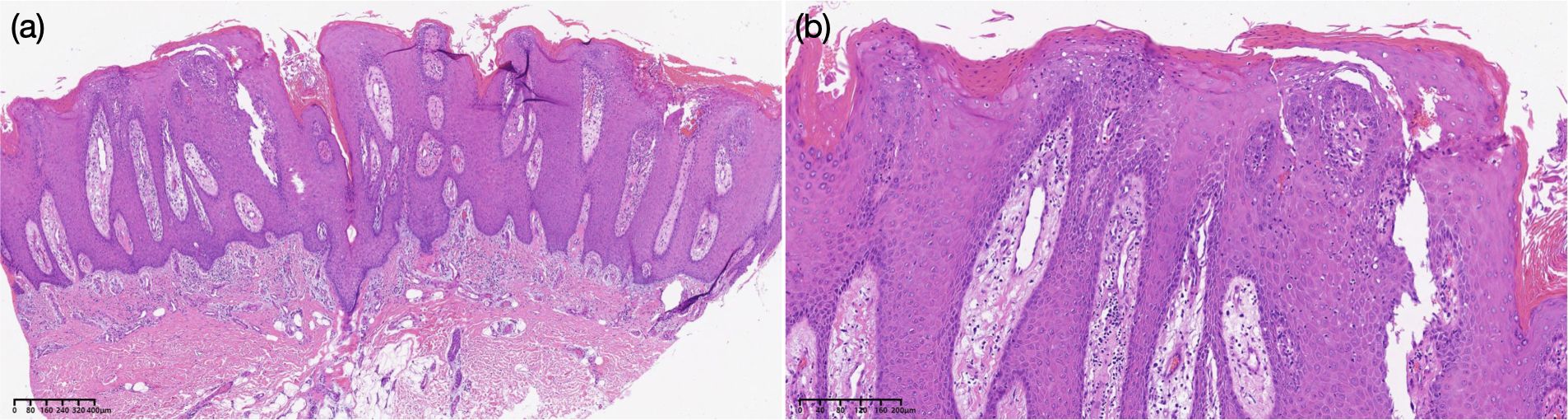
Figure 2. Histopathological findings of the nodule of the left leg [hematoxylin–eosin, original magnifications: (a) *20, (b) *200].
Based on the clinical and pathologic features, we started treating him with oral anti-psoriatic Chinese medicine, clindamycin, topical vitamin D3, and antibiotics, none of which, however, resulted in a favorable response on verrucous lesions. Two weeks after admission, the patient was administrated a dose of 100 mg guselkumab. Strikingly, soon after guselkumab was introduced, the plaque psoriasis on his trunk and limbs became flattened, and VP on both lower legs regressed. Unfortunately, the patient chose to interrupt the follow-up treatment.
6 months after his first treatment, we conducted our telephone follow-up of the patient, and the verrucous plaques of both legs showed complete resolution. In January 2024, due to the recurrence of plaque psoriasis, the patient visited the inpatient department of our hospital again. Physical examination revealed the presence of erythematous papules and plaques which involved the trunk and extremities (Figures 3a–c). The patient’s PASI score was 13.0, so he was given the second dose of 100 mg guselkumab.
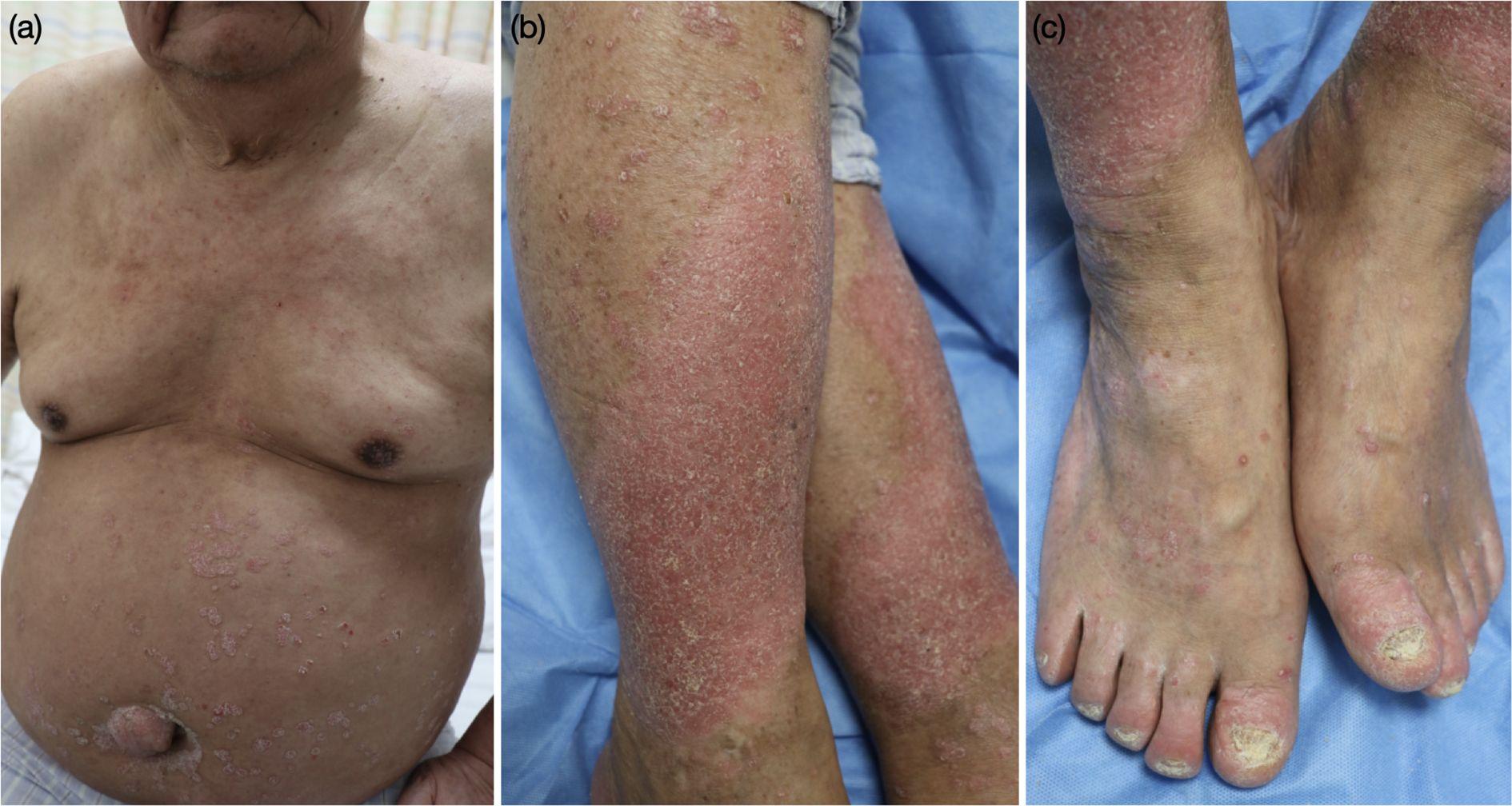
Figure 3. Clinical features of the patient at the second visit. (a–c) erythematous papules and plaques of the trunk and limbs.
Discussion
Guselkumab represents an anti-interleukin (IL)-23 monoclonal antibody that reduces inflammation in psoriatic lesions by directly inhibiting IL-23/Th17 signaling (5). It is approved for treating moderate-to-severe plaque psoriasis in cases eligible for systemic therapy or phototherapy (6). As we know, the IL-23/IL-17 axis is considered to play an important role (5). Particularly, IL-23 is a dimer comprising a specific subunit, p19, and a p40 subunit, also found in IL-12. These cytokines may activate two T-cell types, including helper T-cell types 1 and 17, which release psoriatic cytokines such as IL-17, interferon-γ, TNF-α, and IL-22 (7). This may explain why some patients previously administered anti-IL- 17 still showed an excellent response to guselkumab.
Diagnosing VP can be complex due to its similarity in clinical presentation and histopathology to other conditions, such as verruca vulgaris, epidermal nevus, squamous cell carcinoma, hypertrophic lichen planus, discoid lupus erythematosus, eczema, and fungal infection (8). In our case, the patient had shown symmetric hypertrophic verrucous plaques of both lower legs superimposed on pre-existing psoriatic plaques for two years, which had faced a diagnostic challenge. A diagnosis of VP was established based on the clinical and pathologic features after the patient visited the inpatient department of our hospital.
Regarding treatment, more extensive clinical studies of high methodological quality are not available due to the overall rarity of VP. Based on a limited number of case reports, published review articles have suggested multiple therapies including topical ointments, methotrexate, systemic retinoids, cyclosporin A, and biologics. However, their success rates are inconsistent. Therefore, there is a lack of standardized treatment guidelines for VP. Zhixuan Guo et al. (9) reported that a 61-year-old male patient had experienced significant improvement in his skin lesions upon starting secukinumab. However, the thick verrucous plaques on the patient’s limbs and trunk emerged after a year of secukimumab administration. Similarly, our patient was treated with secukinumab for one year. However, the verrucous lesions further worsened. In 2024, Artur Antonio Duarte et al. (10) reported that a 31-year-old female patient with verrucous psoriasis showed an excellent response to Adalimumab, reaching PASI 90 after 12 weeks of treatment. Luckily, our patient showed complete resolution 24 weeks after the first treatment.
So far, the pathology of VP has not been fully understood. Notably, our patient experienced pruritus, elevated IgE levels, and histological evidence of focal interface dermatitis, suggesting an immune-mediated reaction potentially aggravated by the immuno-modulatory effects of secukinumab. Furthermore, a recent report showed that apremilast could be documented as an effective agent in the treatment of VP (11). These findings underscore the indispensable role of inflammatory pathways in the regulation of keratinocyte differentiation.
Conclusion
To the best of our knowledge, this marks the inaugural utilization of guselkumab in the treatment of VP. Our case underscores the efficacy of guselkumab for VP and advocates its consideration in instances of conventional treatment-resistant VP. While specific studies have indicated the involvement of type 2 inflammation in VP pathogenesis, further clinical and foundational research is imperative to corroborate this conclusion.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Institutional Review Board of Shanghai Skin Disease Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article. Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
Author contributions
JZ: Writing – review & editing, Investigation, Writing – original draft, Formal analysis, Data curation. XY: Writing – review & editing, Resources. YS: Resources, Writing – review & editing, Project administration. YD: Writing – review & editing, Supervision, Resources, Validation, Project administration.
Funding
The author(s) declare that no financial support was received for the research, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Nakamura S, Mihara M, Hagari Y, and Shimao S. Psoriasis verrucosa showing peculiar histologic features. J Dermatol. (1994) 21:102–5. doi: 10.1111/j.1346-8138.1994.tb01423.x
2. Baba A, Fujii K, Arimura A, Tada K, Higashi Y, Matsushita S, et al. Psoriasis with verrucous appearance. Int J Dermatol. (2016) 55:e419–21. doi: 10.1111/ijd.13243
3. Ben Rejeb S, Dhaoui A, Ben Ghachem D, Souissi A, and Bellil K. Psoriasis with verrucous appearance: A case report. Our Dermatol Online. (2017) 8:63–5. doi: 10.7241/ourd.20171.17
4. Maejima H, Katayama C, Watarai A, Nishiyama H, and Katsuoka K. A case of psoriasis verrucosa successfully treated with adalimumab. J Drugs Dermatol. (2012) 11:e74–5.
5. Parham C, Chirica M, Timans J, Vaisberg E, Travis M, Cheung J, et al. A receptor for the heterodimeric cytokine IL-23 is composed of IL-12Rbeta1 and a novel cytokine receptor subunit, IL-23R. J Immunol. (2002) 168:5699–708. doi: 10.4049/jimmunol.168.11.5699
6. Markham A. Guselkumab: first global approval. Drugs. (2017) 77:1487–92. doi: 10.1007/s40265-017-0800-7
7. Kim J and Krueger JG. The immunopathogenesis of psoriasis. Dermatol Clin. (2015) 33:13–23. doi: 10.1016/j.det.2014.09.002
8. Shivers L and Montanez-Wiscovich ME. Verrucous psoriasis treated with methotrexate and acitretin combination therapy. Cutis. (2019) 104:E10–2.
9. Zhixuan G, Menger G, Guangji G, Yuhua L, and Xiangyun L. Emergence of verrucous psoriasis post-secukinumab therapy. J Dermal. (2025) 52:e26–7. doi: 10.1111/1346-8138.17402
10. Duarte AA, Andrade AGBF, Costa de Mendoca C, Ramos de Freitas M, and Felipe da Silva DL. Unilateral verrucous psoriasis successfully treated with adalimumab. Dermatol Pract Concept. (2024) 14:e2024032. doi: 10.5826/dpc.1401a32
Keywords: verrucous psoriasis, plaque psoriasis, secukinumab, guselkumab, case report
Citation: Zheng J, Yi X, Shi Y and Ding Y (2025) Case Report: Successful treatment of guselkumab in a patient with verrucous psoriasis unresponsive to secukinumab. Front. Immunol. 16:1596544. doi: 10.3389/fimmu.2025.1596544
Received: 19 March 2025; Accepted: 20 October 2025;
Published: 04 November 2025.
Edited by:
Rosaria Talarico, ERN ReCONNET Coordination Team, ItalyReviewed by:
Stelvio Tonello, University of Eastern Piedmont, ItalyPui-Ying Leong, Chung Shan Medical University Hospital, Taiwan
Copyright © 2025 Zheng, Yi, Shi and Ding. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuling Shi, c2hpeXVsaW5nMTk3M0AxMjYuY29t; Yangfeng Ding, ZGluZ3lhbmdmZW5nQGhvdG1haWwuY29t
†These authors share first authorship
 Jianfeng Zheng
Jianfeng Zheng Xuemei Yi
Xuemei Yi Yuling Shi*
Yuling Shi*