- 1Department of Neurosurgery, Dengzhou People’s Hospital, Dengzhou, Henan, China
- 2Department of Biopharmaceutics, School of Pharmacy, Air Force Medical University, Xi’an, China
- 3Department of Neurosurgery, Brain Hospital Affiliated to Tongji University, Shanghai, China
- 4Department of Medicine, Sanford Stem Cell Institute, and Moores Cancer Center, University of California San Diego, La Jolla, CA, United States
Brain metastases (BM), represent the most common intracranial malignancies in adults and remain a major clinical challenge due to their poor prognosis and limited therapeutic options. Although immunotherapy has emerged and offers a promising strategy, its efficacy in BM is often compromised by the immunosuppressive tumor microenvironment (TME) and limited immune cell infiltration. This review highlights the critical role of cytokines and growth factors as key modulators of immune dynamics in the TME, exploring their utility as predictive and prognostic biomarkers for immune response. We examine selected categories of biomarkers including genomic, proteomic, immunological, circulating, and microenvironmental, specifically through the lens of cytokine and growth factor regulation. Additionally, we highlight how advanced technologies, including next-generation sequencing (NGS), single-cell RNA sequencing (scRNA-seq), spatial transcriptomics, and liquid biopsies, contribute to the identification and validation of these biomarkers. By addressing current challenges and proposing future directions, this review underscores the translational value of cytokine- and growth factor-related biomarkers in optimizing precision immunotherapy for patient s with BM.
1 Introduction
Brain metastases (BM) are among the most devastating complications in cancer patients, with lung cancer, breast cancer, and melanoma accounting for the majority of cases (1, 2). These secondary brain tumors significantly compromise neurological function and overall survival, representing a critical unmet need in oncology (3, 4). Although advances in imaging and systemic therapies have prolonged survival in patient with advanced malignancies, they have also contributed to a rising incidence of BM, emphasizing the urgency for more effective therapeutic strategies to improve patient outcomes (3, 5).
Historically, patients with BM were excluded from early immunotherapy clinical trials due to concerns about blood-brain barrier permeability and potential neurotoxicity. As a result, data on immunotherapy efficacy in this population have remained limited and often inconclusive (6, 7).
Immunotherapy has emerged as a transformative approach, offering renewed hope for patients with BM (8, 9). However, its clinical success remains hindered by the heterogeneity of BM and the highly immunosuppressive tumor microenvironment (TME). Within this context, cytokines and growth factors play pivotal roles, modulating immune cell infiltration, tumor progression, and therapeutic resistance (10, 11). Key mediators, such as interleukins, interferons, and chemokines, orchestrate immune responses, while factors such as vascular endothelial growth factor (VEGF) promotes angiogenesis and support an immunosuppressive niche (11, 12).
Biomarkers derived from cytokine and growth factor pathways offer substantial potential for guiding and refining immunotherapy strategies. Genomic alterations, proteomic profiles, and immunological markers such as PD-L1 expression and tumor-infiltrating lymphocytes (TILs), provide valuable insights into the molecular and immune landscape of BM (13, 14). Emerging platforms like next-generation sequencing (NGS), single-cell RNA sequencing (scRNA-seq), and liquid biopsy platforms, has further refined the discovery and validation of these biomarkers, facilitating their translation into clinical applications (15–17).
This review explores the evolving landscape of immunotherapy biomarkers in BM, focusing specifically on cytokines and growth factors and their regulatory roles with in the TME. By addressing existing knowledge gaps and outlining future directions, we aim to highlight the translational potential of biomarker-guided strategies in advancing precision immunotherapy for patients with BM.
2 Current landscape of biomarkers in BM
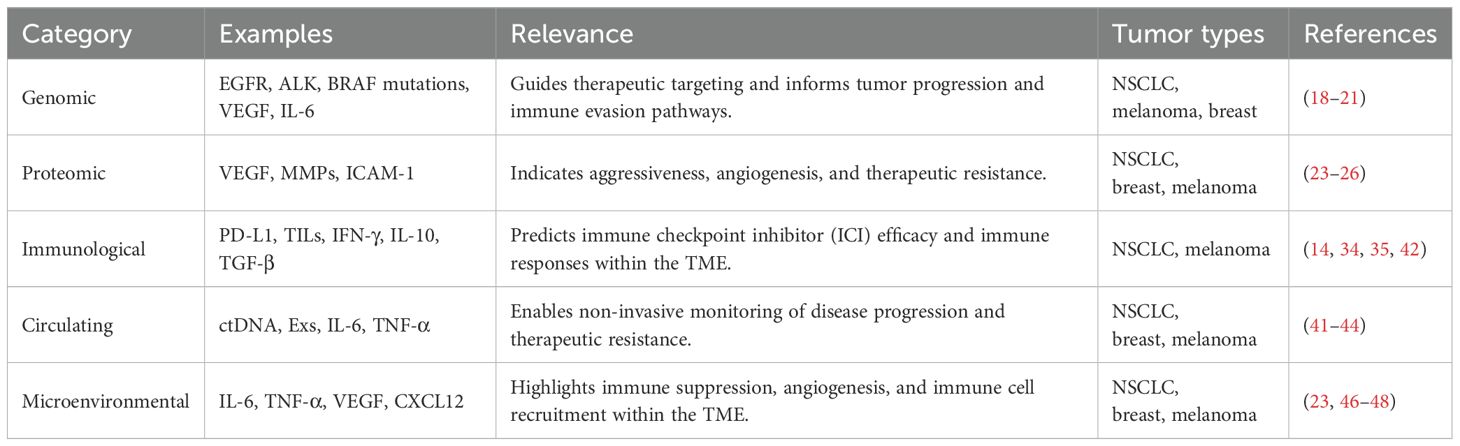
Biomarkers are critical for understanding and treating BM by providing insights into their genetic, proteomic, immunological, and microenvironmental characteristics. This section explores key categories of biomarkers relevant to BM, including genomic, proteomic, immunological, circulating, and microenvironmental markers.
2.1 Genomic biomarkers
Genomic biomarkers illuminate the molecular drivers of BM and enable the development of targeted therapies. Common alterations, including mutations in epidermal growth factor receptor (EGFR), anaplastic lymphoma kinase (ALK), and B-Raf proto-oncogene serine/threonine kinase (BRAF), are frequently observed in metastases derived from primary lung, breast, and melanoma tumors (18, 19). These mutations influence tumor progression, prognosis, and responsiveness to therapies. Additionally, genes encoding cytokines and growth factor receptors, such as vascular endothelial growth factor (VEGF) and interleukin-6 (IL-6), have been implicated in promoting angiogenesis and contributing to immune evasion within the TME (20, 21). Next-generation sequencing (NGS) enables comprehensive profiling these genetic alterations, guiding therapeutic decisions and refining precision oncology approaches (22).
2.2 Proteomic biomarkers
Proteomic biomarkers reveal protein expression patterns associated with BM, offering insights into tumor behavior and therapy resistance. Proteins such as matrix metalloproteinases (MMPs) and VEGF are linked to angiogenesis and tumor invasion, and aggressive disease phenotypes (23, 24). Advances in mass spectrometry (MS) have facilitated the identification of differentially expressed proteins that may serve as therapeutic targets (25). Additionally, cytokine-induced proteins, including intercellular adhesion molecule-1 (ICAM-1) are emerging as indicators of tumor progression and immune modulation, although not all are directly linked to EGFR pathways (26). Integrating proteomic data with genomic and immunological markers enhances the multidimensional understanding of tumor biology (27, 28).
2.3 Immunological biomarkers
The immune landscape of BM is shaped by a complex network of cytokines and growth factors that orchestrate anti-tumor responses and immune evasion mechanisms (29). Key immunological biomarkers such as programmed cell death ligand 1 (PD-L1) and tumor-infiltrating lymphocytes (TILs) are widely used to predict responsiveness to immune checkpoint inhibitors (ICIs) (30, 31). Cytokines like interferon-gamma (IFN-γ) play a regulatory role in PD-L1 expression and correlate with better response to ICIs (32, 33). Additionally, the quantity and composition of TILs, particularly cytotoxic T cells (CTLs) and regulatory T cells (Tregs), are influenced by cytokines such as IL-10 and transforming growth factor beta (TGF-β), both of which contribute to immune suppression and tumor tolerance within the TME (34, 35). Recent advances in technologies single-cell RNA sequencing (scRNA-seq) and high-dimensional immunophenotyping have enhanced the ability to delineate immune cell heterogeneity and cytokine-driven subpopulations in BM, offering novel insights into immunophenotyping biomarkers (36, 37).
2.4 Circulating biomarkers
Circulating biomarkers provide a non-invasive means to monitor BM progression and treatment response (38, 39). Key biomarkers include circulating tumor DNA (ctDNA), exosomes (Exs), and soluble cytokines. ctDNA reflects tumor-specific mutations and copy number alterations, while exosomes (Exs) carry tumor-derived proteins and RNA (40, 41). Circulating cytokines, including IL-6, IL-8, and tumor necrosis factor-alpha (TNF-α), correlate with systemic inflammation, tumor burden, and immunotherapy resistance (42, 43). Advances in liquid biopsy technologies continue to improve sensitivity and specificity in detecting these markers (41, 44).
2.5 Microenvironmental biomarkers
The TME in BM is a dynamic ecosystem that mediates immune escape, therapy resistance, and tumor progression (29, 45). Key microenvironmental biomarkers include cytokines, chemokines, and stromal factors that reflect and shape immune dynamics. Elevated levels of IL-6 and TNF-α promote a pro-tumorigenic inflammatory state, while VEGF drives angiogenesis and hampers immune infiltration (46, 47). VEGF facilitates angiogenesis and disrupts immune surveillance, immunosuppressive mediators like TGF-β contributes to immunosuppressive niches (23, 48). Chemokines such as C-X-C motif chemokine ligand 12 (CXCL12) regulate spatial immune cell recruitment and promote tumor-immune crosstalk within the brain TME (42, 49). Targeting these microenvironmental signals, particularly those involving cytokine and chemokine axes, may enhance the efficacy of immunotherapies by reversing immune suppression and enabling T cell infiltration (42, 50).
The diverse array of biomarkers in BM underscores the complexity of tumor-immune interactions and highlights the importance of multi-modal strategies for personalized immunotherapy. Future research should prioritize validating these biomarkers across diverse cohorts and integrating them into clinical practice. Future efforts should focus on validating these biomarkers in diverse patient cohorts and integrating them into clinical workflows to enhance diagnostic accuracy, treatment selection, and patient outcomes (12, 51).
Table 1 provides a consolidated overview of the major biomarker categories discussed above, highlighting representative examples, their clinical relevance, and associated references in the context of BM.
3 Emerging biomarkers for immunotherapy
The rapid advancement of molecular and cellular technologies has significantly enhanced biomarker discovery for immunotherapy in BM (13, 52, 53). These emerging biomarkers provide opportunities for personalized medicine, enabling improved prediction of treatment responses and therapy customization (54–56). This section focuses on advanced approaches that are shaping biomarker discovery, particularly those related to cytokines and growth factors.
3.1 Integration of NGS and scRNA-seq
NGS and scRNA-seq are complementary technologies that together provide a comprehensive view of the tumor and immune landscape. NGS enables high-throughput identification of genetic alterations, such as mutations in VEGF, IL-6, and TGF-β, which play pivotal roles in the TME and influence immunotherapy responses (57, 58). By offering detailed genomic profiles, NGS facilitates the identification of actionable targets and enhances patient stratification for tailored treatments (59, 60).
ScRNA-seq adds another layer of granularity by analyzing gene expression at the single-cell level, uncovering rare cell populations and their functional states (36, 61). For instance, tumor-associated macrophages (TAMs) producing IL-10 or TGF-β contribute to immunosuppression, while CD8+ T cells secreting IFN-γ exhibit anti-tumor activity (62, 63). Together, these tools enable a multifaceted view of tumor heterogeneity and cytokine-driven dynamics, paving the way for developing precise and adaptive immunotherapy strategies (64).
To better understand the complexity of cytokine- and growth factor–mediated signaling in BM, Figure 1 illustrates how integrated technologies such as NGS, scRNA-seq, and spatial transcriptomics converge to uncover relevant biomarkers, enabling both mechanistic insight and translational application in immunotherapy. Figure 1 illustrates the integration of NGS, scRNA-seq, and spatial transcriptomics, showcasing their complementary roles in uncovering tumor and immune heterogeneity and advancing biomarker discovery for precision oncology.
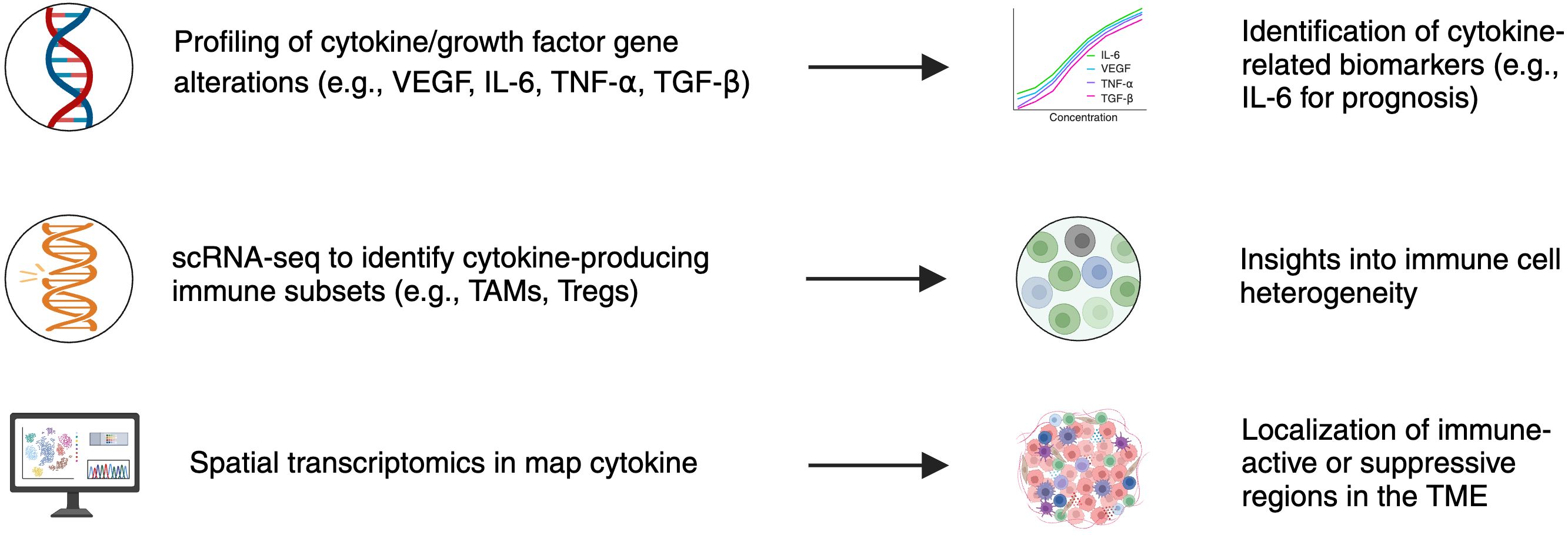
Figure 1. Integration of multi-omic technologies in cytokine- and growth factor-driven biomarker discovery for brain metastases. This schematic illustrates how next-generation sequencing (NGS), single-cell RNA sequencing (scRNA-seq), and spatial transcriptomics each contribute unique insights into tumor and immune biology. NGS enables profiling of gene alterations in cytokine and growth factor pathways (e.g., VEGF, IL-6, TNF-α, TGF-β), supporting biomarker identification such as IL-6 for prognosis. ScRNA-seq identifies cytokine-producing immune subsets (e.g., TAMs, Tregs), revealing immune cell heterogeneity. Spatial transcriptomics localizes cytokine activity within the TME, distinguishing immune-active or immunosuppressive regions. Together, these platforms enable mechanistic insight and translational application in precision immunotherapy.
3.2 Spatial transcriptomics
Spatial transcriptomics offers a novel perspective by mapping gene expression within the spatial context of tissue architecture. This technology is particularly valuable for examining how the TME shapes tumor progression and response to therapy. Spatial mapping reveals distinct molecular niches within BM, such as areas enriched with chemokines like CXCL12 that recruit immune cells (65, 66). By integrating spatial data with transcriptomic profiles, researchers can identify localized immune evasion mechanisms and develop targeted therapies to overcome them (67, 68). Future applications may include combining spatial transcriptomics with advanced imaging modalities for a comprehensive understanding of tumor biology (69).
3.3 Proteomics and MS
Proteomics, driven by advancements in MS, provides detailed insights into the protein landscape of BM. MS-based approaches detect critical cytokine- and growth factor-related proteins, such as VEGF, MMPs, and ICAM-1, which are involved in angiogenesis, tumor invasion, and immune modulation (23, 59). Proteomics also uncovers post-translational modifications, such as phosphorylation of cytokine receptors, which can influence therapeutic responses (70, 71). By integrating proteomic findings with genomic and transcriptomic data, researchers can refine therapeutic strategies and identify new biomarkers for treatment personalization (72–74).
3.4 Liquid biopsy technologies
Liquid biopsy technologies provide non-invasive methods for tracking disease progression and treatment responses in real-time. These approaches analyze ctDNA, Exs, and cytokines to monitor tumor dynamics. For instance, circulating cytokines like IL-6, TNF-α, and VEGF serve as markers of systemic inflammation and immune activity, correlating with therapy resistance and tumor progression (75, 76), carrying cytokine-related proteins and RNA fragments reflect the molecular state of tumors and hold promise for biomarker discovery (77, 78). Despite challenges in assay sensitivity and specificity, advancements in liquid biopsy technologies are improving their reliability and potential for integration into routine clinical workflows (17, 79).
Emerging technologies, including NGS, scRNA-seq, spatial transcriptomics, proteomics, and liquid biopsies, are transforming biomarker discovery for BM (80). These innovations enhance our understanding of tumor biology and provide tools for developing personalized and adaptive immunotherapy strategies (81, 82). Future efforts should focus on validating these biomarkers in clinical settings and addressing challenges related to standardization, cost, and accessibility (83). Collaborative approaches combining technological innovation and interdisciplinary research are critical for advancing biomarker-driven precision oncology (84, 85).
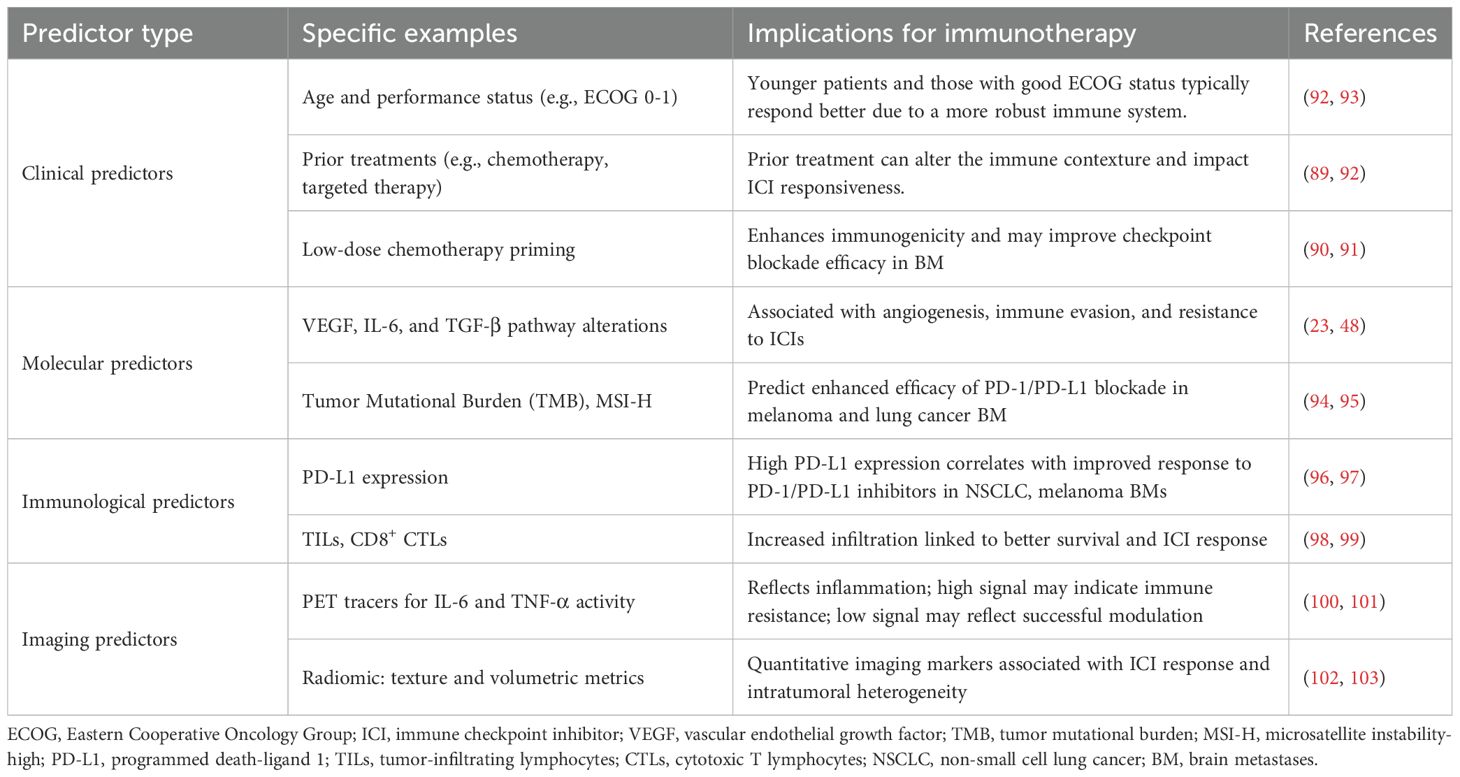
4 Predictive indicators of immunotherapy response
Understanding and identifying predictive indicators of immunotherapy response are essential for optimizing treatment strategies for BM (52, 86). These indicators guide clinicians in selecting appropriate patients and help tailor treatment regimens to enhance efficacy. This section explores predictive indicators, including clinical, molecular, immunological, and imaging through the lens of cytokine and growth factor activity, while incorporating recent technological advances that enable more precise immune profiling.
4.1 Clinical predictors
Clinical predictors include demographic and treatment-related variables that influence immunotherapy outcomes. Factors such as age, performance status, and prior treatments are routinely evaluated in clinical settings. Elevated cytokines like IL-6 and TNF-α are correlated with systemic inflammation and poorer prognoses (87). Younger patients with a good Eastern Cooperative Oncology Group (ECOG) score (0–1) generally demonstrate better outcomes, likely due to preserved immune system (88). Additionally, prior therapies such as chemotherapy or targeted agents may modulate the immune landscape and thus affect responsiveness to ICIs (89). Recent evidence suggests that low-dose chemotherapy may act as a priming agent, enhancing immunogenicity and improving responsiveness to ICIs in patients with BM (90). Additional studies also indicate that low-dose chemotherapy may serve as an immunogenic primer, boosting antigen presentation and improving the efficacy of subsequent immunotherapy in BM patients (91). These insights underscore the importance of individualized treatment planning based on clinical predictors and their interplay with immune mechanisms.
Identifying these predictors enables effective patient stratification and personalized treatment plans to optimize therapeutic outcomes. The key predictors of immunotherapy response, categorized into clinical, molecular, immunological, and imaging domains, are summarized in Table 2, along with specific examples and their implications for treatment strategies.
4.2 Molecular predictors
Molecular predictors reveal intrinsic tumor properties that influence immunotherapy response. Key alterations in cytokine and growth factor pathways, such as VEGF, IL-6, and TGF-β drive, angiogenesis, immune escape, and resistance to ICIs (42, 48). Gene expression profiles, including EGFR, ALK, and BRAF mutations, are linked to differential responses to ICIs (104). Furthermore, tumors with high tumor mutational burden (TMB) or microsatellite instability-high (MSI-H) status indicate increased neoantigen loads, often translating into better responses to PD-1/PD-L1 inhibitors (105).
New technologies such as NGS enable deep genomic profiling of these alterations, while transcriptomic approaches allow for the identification of cytokine-driven gene expression programs. This facilitates personalized treatment strategies that target not only mutations but also aberrant signaling pathways relevant to immune modulation (13, 54, 57).
4.3 Immunological predictors
Immunological predictors provide insights into baseline immune competence and tumor-immune interactions. Biomarkers like PD-L1expression and tumor-infiltrating lymphocytes (TILs), particularly CD8+ cytotoxic T lymphocytes (CTLs), are well-established indicators of ICI response (33, 106, 107). Beyond surface marker expression, recent advances in single-cell RNA sequencing (scRNA-seq) and spatial transcriptomics allow for the high-resolution mapping of immune cell subtypes and their spatial distribution in the TME. These tools can uncover cytokine-rich niches or immunosuppressive zones, offering a nuanced understanding of immune heterogeneity in BMs. For example, IL-10 and IFN-γ signaling profiles can be inferred from scRNA-seq datasets, helping to predict ICI sensitivity at the single-cell level (108).
4.4 Imaging predictors
Imaging biomarkers offer a non-invasive tool to evaluate tumor burden, immune activity, and treatment response in BM. Functional imaging techniques, particularly positron emission tomography (PET) and magnetic resonance imaging (MRI), provide quantitative data on tumor metabolism, structural heterogeneity, and the immunologic landscape (109).
PET tracers such as 18F-fluorodeoxyglucose (18F-FDG) are commonly used to measure glucose metabolism in BM, correlating with tumor aggressiveness and immune evasion, particularly in NSCLC- and melanoma-derived BM. More advanced tracers like 89Zr-labeled atezolizumab, a radiolabeled anti-PD-L1 antibody, have been shown early promise in evaluating immune checkpoint activity and predicting ICI response (110, 111). Additionally, PET tracers targeting cytokine signaling, such as 64Cu-IL-6 and 68Ga-TNF-α analogs, visualize inflammatory niches and immune cell infiltration, serving as surrogate markers of immune activation or suppression (101, 112).
High uptake of these tracers suggests immune-active or cytokine-driven inflammatory regions, while reduced uptake may reflect effective immune modulation or tumor regression post-treatment (113, 114). On the structural imaging front, MRI-derived radiomic features such as texture, entropy, and volumetric indices are being explored for their predictive value in ICI responsiveness (115). These features may indicate underlying biological processes like necrosis, edema, or immune infiltration, aiding in patient stratification.
Integrating these imaging biomarkers into clinical practice enables real-time monitoring of treatment efficacy, facilitates adaptive therapy adjustments, and supports early identification of responders versus non-responders. Alongside clinical, molecular, immunological markers, and imaging predictors play a vital role in driving precision immunotherapy in BM (116, 117). Continued validation and integration into routine workflows are essential to fully realize the potential of personalized oncology in this complex setting (118).
5 Technological advances in biomarker discovery
The rapid progress in molecular profiling tools and high-throughput platforms has significantly enhanced our ability to discover and validate biomarkers for BM, particularly in the context of immunotherapy (7, 13). These innovations improve the precision and efficacy of cancer treatments by enabling the identification of cytokine- and growth factor-related biomarkers. This section focuses on the applications of NGS, single-cell technologies, MS, proteomics, and liquid biopsies in advancing biomarker discovery (25, 54).
5.1 NGS and single-cell technologies
NGS has transformed biomarker discovery by enabling comprehensive analysis of genetic alterations in cytokine and growth factor pathways, such as VEGF, IL-6, and TGF-β (13, 42). By providing detailed genomic profiles, NGS supports personalized treatment strategies, particularly for predicting immunotherapy responses and refining patient stratification (119).
ScRNA-seq complements NGS by offering insights into tumor heterogeneity and the immune microenvironment at a single-cell resolution. It identifies cytokine-producing cells, including TAMs secreting IL-10 or TGF-β and CD8+ T cells producing IFN-γ, which influence immunotherapy outcomes (11, 63, 120). The integration of bulk and single-cell data provides a comprehensive view of tumor biology, facilitating the discovery of biomarkers that address the complexities of BM and their resistance to therapy (36, 63).
5.2 Proteomics and MS
Proteomics, driven by MS, enables high-sensitivity analysis of protein expression, post-translational modifications, and protein-protein interactions. This approach has been pivotal in identifying biomarkers linked to tumor progression and therapeutic responses (121, 122). For instance, MS-based techniques have detected cytokine-induced proteins, such as MMPs and VEGF, that are critical for angiogenesis and immune modulation (23, 42, 123).
The ability of MS to detect post-translational modifications, like phosphorylation of cytokine receptors, provides deeper insights into protein functionality within the TME (124). Integrating proteomic data with genomic and transcriptomic profiles allows researchers to develop multidimensional biomarkers, enhancing the precision of personalized immunotherapy strategies (13).
5.3 Liquid biopsies
Liquid biopsies represent a non-invasive method for monitoring disease progression and treatment response. These technologies analyze ctDNA, exosomes, and cytokines present in bodily fluids, offering real-time insights into tumor dynamics (125). Liquid biopsies are particularly advantageous for their reduced invasiveness and ability to enable repeated sampling to track tumor evolution and therapeutic response.
Advanced assays quantify circulating cytokines and chemokines, such as IL-6, TNF-α, and CXCL12, which reflect the immune microenvironment and tumor progression (126, 127). Additionally, exosomes containing cytokine-related proteins and RNA fragments provide valuable insights into treatment resistance and immune activity (77, 128). Despite challenges in sensitivity and specificity, ongoing advancements in assay technologies improve the accuracy of liquid biopsies, making them indispensable tools for personalizing immunotherapy (38, 41).
Figure 2 illustrates the workflow of liquid biopsy and proteomics-driven biomarker discovery, from sample collection and preparation to advanced molecular analyses and clinical applications, emphasizing its potential to revolutionize precision oncology.
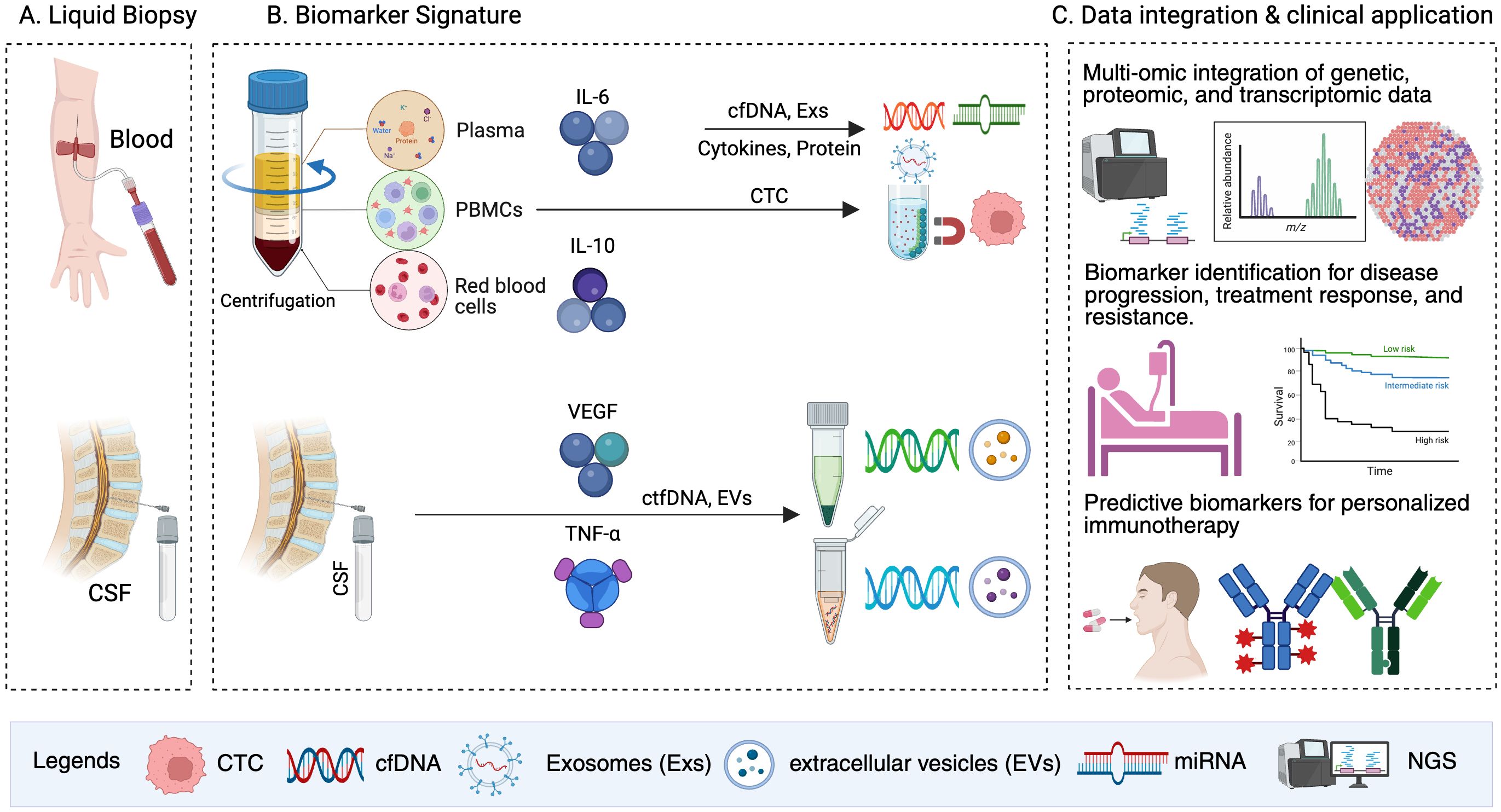
Figure 2. Liquid biopsy and biomarker discovery for personalized immunotherapy. This figure illustrates a streamlined workflow for liquid biopsy and cytokine/growth factor application. (A) Liquid biopsy: Blood and CSF are collected as sources of biomarkers. (B) Biomarker signature: Following centrifugation, plasma, PBMCs, and red blood cells are analyzed for key biomarkers such as IL-6, IL-10, VEGF, and TNF-α. Analytes including cfDNA, CTCs, Exs, and EVs are extracted for profiling. (C) Data integration and clinical application: multi-omic integration of genetic, proteomic, and transcriptomic data enables the identification of predictive biomarkers associated with disease progression, treatment response, and resistance. These insights inform treatment decisions and support personalized immunotherapy strategies.
Technological advancements, including NGS, scRNA-seq, MS, and liquid biopsies, drive significant progress in biomarker discovery for BM (129). By deepening our understanding of tumor biology and the immune microenvironment, these innovations pave the way for adaptive and personalized immunotherapy strategies (41, 130–132). Continued research and integration of these technologies into clinical workflows are critical for improving patient outcomes and advancing precision oncology (21, 133).
6 Challenges and future directions
The field of biomarker discovery for immunotherapy in BM is rapidly evolving. However, numerous challenges related to cytokine and growth factor biomarkers remain. Addressing these challenges across technical, biological, and clinical domains is essential. Furthermore, future research must prioritize integrating these biomarkers into clinical practice to achieve meaningful advancements.
6.1 Technical challenges
Quantifying low-abundance cytokines and growth factors in complex biological matrices like blood or cerebrospinal fluid presents significant technical challenges (42, 134). These molecules exist at picomolar concentrations, necessitating the use of highly sensitive and specific detection methods, such as advanced multiplex assays or MS-based techniques (130, 135). Additionally, the structural similarity among many cytokines and growth factors complicates assay specificity, requiring the development of next-generation detection platforms (136). Standardizing protocols across laboratories is crucial to improve reproducibility and facilitate biomarker validation (137). Automated workflows and high-throughput technologies should be prioritized to address scalability and minimize variability in biomarker quantification, thereby expediting their clinical adoption.
6.2 Biological challenges
The variability in cytokine and growth factor expression, driven by tumor heterogeneity and systemic inflammation, complicates their utility as reliable biomarkers. BM exhibit significant spatial and temporal heterogeneity, resulting in distinct cytokine profiles that evolve in response to treatment interventions and tumor-immune dynamics (84). For instance, IL-6 overexpression may signify both tumor progression and systemic inflammation, complicating its interpretation as a biomarker (13, 138). Additionally, the dynamic nature of cytokines and growth factors necessitates longitudinal studies to account for fluctuations during disease progression or therapy response. Technologies like scRNA-seq and spatial transcriptomics are essential for providing high-resolution insights into cytokine-producing cells and their spatial distribution, revealing actionable targets for therapeutic interventions (139).
6.3 Clinical challenges
Overcoming logistical, ethical, and regulatory barriers is critical for integrating cytokine and growth factor biomarkers into clinical practice. Biomarker testing workflows must be streamlined to ensure cost-effectiveness and avoid delays in patient care (140). Ethical considerations, such as obtaining informed consent and addressing disparities in access to advanced diagnostic technologies, must be addressed to promote equitable healthcare delivery (141). From a regulatory perspective, cytokine and growth factor assays must meet stringent criteria for analytical validity, clinical utility, and scalability (54). Collaborative efforts among researchers, clinicians, and regulatory agencies are necessary to demonstrate the clinical relevance of these biomarkers in predicting treatment responses and guiding therapy (142). Such collaborations will facilitate broader adoption and regulatory approval.
The integration of technological, biological, and clinical strategies is essential for overcoming these challenges and advancing biomarker-driven immunotherapy. Figure 3 provides an overview of key challenges in biomarker discovery and corresponding solutions aimed at improving the clinical utility of cytokine and growth factor biomarkers.
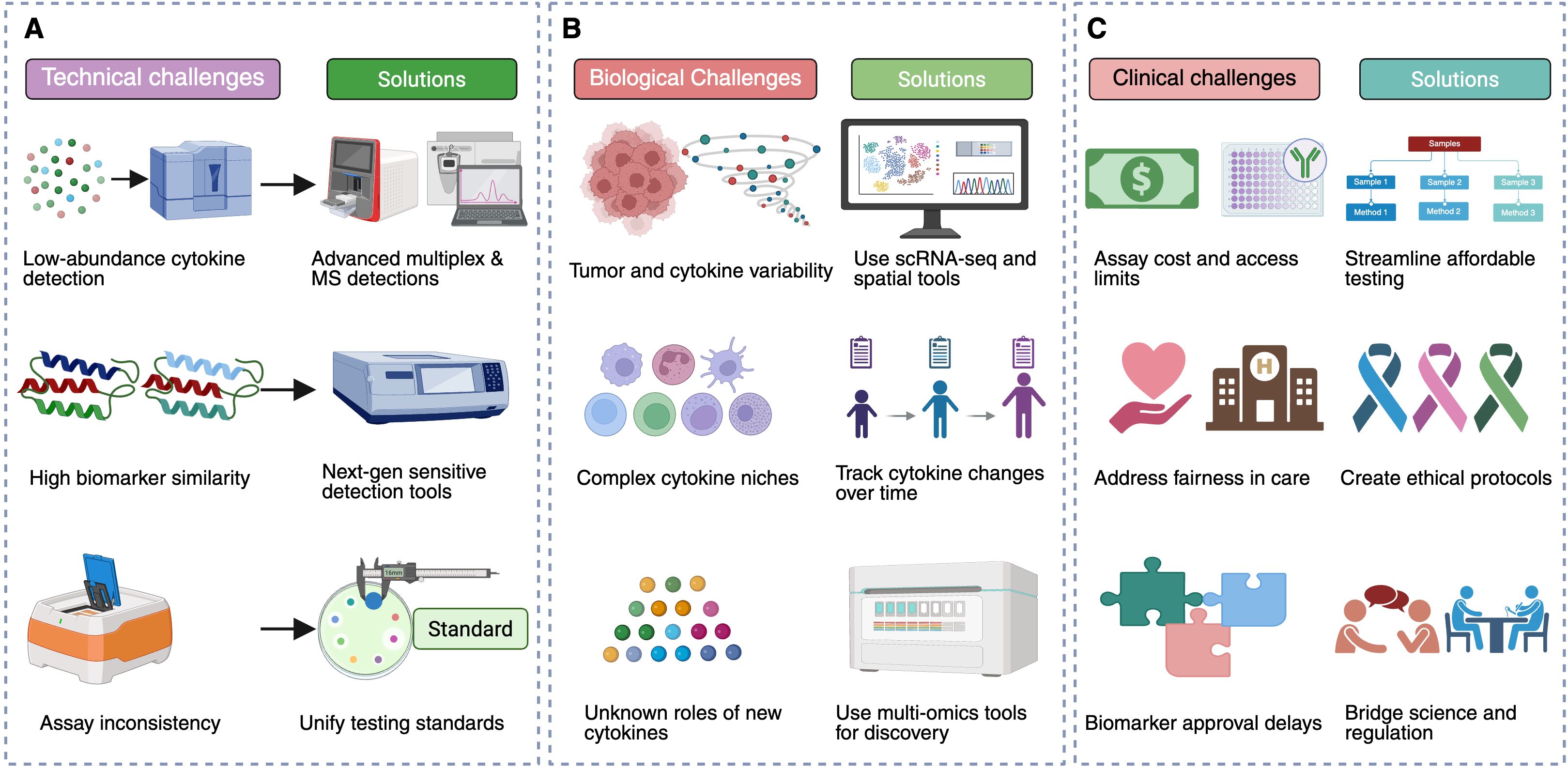
Figure 3. Challenges and solutions in biomarker discovery for immunotherapy. This figure summarizes key technical, biological, and clinical challenges in biomarker discovery for immunotherapy and presents potential solutions to address them. (A) Technical challenges include the detection of low-abundance cytokines and growth factors, high structural similarity among biomarkers, and lack of assay standardization. Solutions involve utilizing advanced multiplex and MS-based assays, developing next-generation detection platforms with improved sensitivity, and standardizing protocols across laboratories. (B) Biological challenges stem from tumor heterogeneity, fluctuating cytokine levels, complexity within cytokine-driven immune niches, and limited knowledge of novel cytokines. Proposed solutions include employing scRNA-seq and spatial transcriptomics, conducting longitudinal studies to track cytokine dynamics, and exploring multi-omic assays for novel discoveries. (C) Clinical challenges include logistical barriers such as assay cost and accessibility, ethical concerns in equitable healthcare delivery, and regulatory hurdles for biomarker validation. Solutions emphasize prioritizing scalable, cost-effective workflows, building ethical frameworks for advanced testing, and fostering collaboration among researchers and regulatory bodies to streamline biomarker validation.
6.4 Future research directions
Future research should focus on discovering novel cytokine and growth factor biomarkers, particularly underexplored molecules like IL-10, TGF-β, and CXCL12, which influence immune evasion and tumor progression (143). Leveraging multi-omic approaches, including genomics, transcriptomics, proteomics, and metabolomics, can elucidate cytokine-driven pathways and their implications for immunotherapy (144). Rigorous clinical validation through prospective trials and real-world studies is critical for establishing the, and prognostic value of these biomarkers (145). Artificial computational tools, such as AI and ML, should be employed to analyze complex multi-omic datasets, uncovering patterns that might otherwise remain undetected (146). Moreover, developing scalable and user-friendly assays is vital to ensure these biomarkers can be adopted across diverse healthcare settings.
Despite substantial progress in cytokine and growth factor biomarker discovery, addressing technical, biological, and clinical challenges is essential to fully realize their potential (13). By prioritizing the development of robust detection platforms, understanding cytokine variability, and integrating validated biomarkers into clinical workflows, the field can drive innovation in personalized immunotherapy strategies (13, 54, 147). These efforts promise not only improved outcomes for patients with BM but also significant advancements in precision oncology.
7 Conclusion
The evolving landscape of immunotherapy biomarkers in BM underscores the central role of cytokines and growth factors in modulating immune responses within the TME (52, 148). Through this review, we synthesized evidence across genomic, proteomic, immunological, circulating, and microenvironmental domains, highlighting how these biomarkers inform prognosis and therapeutic decision-making (13, 54).
7.1 Key findings
Cytokine and growth factor pathways influence tumor progression, immune evasion, and treatment response (42). Advances in high-throughput technologies such as NGS, scRNA-seq, spatial transcriptomics, and liquid biopsies have enabled deeper profiling of immune landscapes, facilitating biomarker discovery and risk stratification (149).
7.2 Translational potential
To translate these findings into clinical impact, future efforts must address key barriers, including assay variability, tumor heterogeneity, and limited validation across populations (13, 54). Integrating multi-omic data will enhance biomarker precision and support personalized immunotherapy approaches (144, 150, 151).
7.3 Future directions
Moving forward, interdisciplinary collaboration is essential to optimize biomarker platforms, ensure regulatory alignment, and drive multicenter validation (84, 152, 153). The integration of AI and machine learning will further refine predictive models, accelerating the clinical adoption of biomarker-driven strategies for BM (154–156).
Author contributions
ML: Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing. YZ: Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing. DY: Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing. YY: Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Writing – original draft, Writing – review & editing, Formal Analysis. WM: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The figures were created with BioRender.com.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AI, artificial intelligence; BRAF, B-Raf proto-oncogene serine/threonine kinase; ctDNA, circulating tumor DNA; CXCL12, C-X-C motif chemokine ligand 12; CTLs, including cytotoxic T cells; DCs, dendritic cells; ECOG, eastern cooperative oncology group; EGFR, epidermal growth factor receptor; ICAM-1, intercellular adhesion molecule-1; ICIs, immune checkpoint inhibitors; IFN-γ, interferon gamma; IL, interleukin; ML, machine leaning; MMPs, matrix metalloproteinases; MRI, magnetic resonance imaging; MS, mass spectrometry; MSI-H, microsatellite instability-high; NSG, next-generation sequencing; PD-L1, programmed death-ligand 1; PET, positron emission tomography; scRNA-seq, single-cell RNA sequencing; PBMCs, peripheral blood mononuclear cells; TGF-β, transforming growth factor beta; TAMs, tumor-associated macrophages; TILs, tumor-infiltrating lymphocytes; TMB, tumor mutational burden; TME, tumor microenvironment; TNF-α, tumor necrosis factor alpha; Treg, regulatory T cells; VEGF, vascular endothelial growth factor.
References
1. Raghavendra AS and Ibrahim NK. Breast cancer brain metastasis: A comprehensive review. JCO Oncol Pract. (2024) 20:1348–59. doi: 10.1200/OP.23.00794
2. Park S, Baldry R, Jung HA, Sun JM, Lee SH, Ahn JS, et al. Phase ii efficacy and safety of 80 mg osimertinib in patients with leptomeningeal metastases associated with epidermal growth factor receptor mutation-positive non-small cell lung cancer (Blossom). J Clin Oncol. (2024) 42:2747–56. doi: 10.1200/JCO.24.00708
3. Amouzegar A, Haig S, Kahn AM, Tawbi HA, Jones JA, and Goldberg SB. Navigating the complexities of brain metastases management. Am Soc Clin Oncol Educ Book. (2024) 44:e433694. doi: 10.1200/edbk_433694
4. Muller V, Bachelot T, Curigliano G, de Azambuja E, Furtner J, Gempt J, et al. Expert consensus on the prevention of brain metastases in patients with her2-positive breast cancer. Cancer Treat Rev. (2025) 132:102860. doi: 10.1016/j.ctrv.2024.102860
5. Podder V, Ganiyani MA, Ahmad S, Bellur SS, Khokhar MA, Ayoobkhan FS, et al. Treatment outcomes of brain metastasis from primary renal cell carcinoma in United States: A national cancer database analysis. J Clin Oncol. (2024) 42:4561. doi: 10.1200/JCO.2024.42.16_suppl.4561
6. Yan X, Qu F, and Zhou Y. Progress of immune checkpoint inhibitors therapy for non-small cell lung cancer with brain metastases. Lung Cancer. (2023) 184:107322. doi: 10.1016/j.lungcan.2023.107322
7. Paisana E, Cascao R, Alvoeiro M, Felix F, Martins G, Guerreiro C, et al. Immunotherapy in lung cancer brain metastases. NPJ Precis Oncol. (2025) 9:130. doi: 10.1038/s41698-025-00901-0
8. Sandhbor P, John G, Bhat S, and Goda JS. Immune response recalibration using immune therapy and biomimetic nano-therapy against high-grade gliomas and brain metastases. Asian J Pharm Sci. (2025) 20(2):101021. doi: 10.1016/j.ajps.2025.101021
9. Liu Y, Zhou F, Ali H, Lathia JD, and Chen P. Immunotherapy for glioblastoma: current state, challenges, and future perspectives. Cell Mol Immunol. (2024) 21:1354–75. doi: 10.1038/s41423-024-01226-x
10. Nishida A and Andoh A. The role of inflammation in cancer: mechanisms of tumor initiation, progression, and metastasis. Cells. (2025) 14:488. doi: 10.3390/cells14070488
11. Shao S, Miao H, and Ma W. Unraveling the enigma of tumor-associated macrophages: challenges, innovations, and the path to therapeutic breakthroughs. Front Immunol. (2023) 14:1295684. doi: 10.3389/fimmu.2023.1295684
12. Xu S, Wang Q, and Ma W. Cytokines and soluble mediators as architects of tumor microenvironment reprogramming in cancer therapy. Cytokine Growth Factor Rev. (2024) 76:12–21. doi: 10.1016/j.cytogfr.2024.02.003
13. Zhou Y, Tao L, Qiu J, Xu J, Yang X, Zhang Y, et al. Tumor biomarkers for diagnosis, prognosis and targeted therapy. Signal Transduct Target Ther. (2024) 9:132. doi: 10.1038/s41392-024-01823-2
14. Lin X, Kang K, Chen P, Zeng Z, Li G, Xiong W, et al. Regulatory mechanisms of pd-1/pd-L1 in cancers. Mol Cancer. (2024) 23:108. doi: 10.1186/s12943-024-02023-w
15. Albarran Fernandez V, Ballestin Martinez P, Stoltenborg Granhoj J, Borch TH, Donia M, and Marie Svane I. Biomarkers for response to til therapy: A comprehensive review. J Immunother Cancer. (2024) 12:e008640. doi: 10.1136/jitc-2023-008640
16. Xu S, Li X, and Ma W. Redefining the tumor microenvironment with emerging therapeutic strategies. Oncol Res. (2024) 32:1701–8. doi: 10.32604/or.2024.055161
17. Bao Y, Zhang D, Guo H, and Ma W. Beyond blood: advancing the frontiers of liquid biopsy in oncology and personalized medicine. Cancer Sci. (2024) 115:1060–72. doi: 10.1111/cas.16097
18. Li X and Shi W. Outcomes of egfr, alk, ros1, braf, met, and ret mutated non-small cell lung cancer with brain metastases (Nsclc bm). J Clin Oncol. (2024) 42:201. doi: 10.1200/JCO.2024.42.23_suppl.201
19. Wang W, Lian B, Xu C, Wang Q, Li Z, Zheng N, et al. Expert consensus on the diagnosis and treatment of solid tumors with braf mutations. Innovation. (2024) 5:100661. doi: 10.1016/j.xinn.2024.100661
20. Xu S, Ma Y, Jiang X, Wang Q, and Ma W. Cd39 transforming cancer therapy by modulating tumor microenvironment. Cancer Lett. (2024) 20(2):101021. doi: 10.1016/j.canlet.2024.217072
21. Yu B, Shao S, and Ma W. Frontiers in pancreatic cancer on biomarkers, microenvironment, and immunotherapy. Cancer Lett. (2025) 610:217350. doi: 10.1016/j.canlet.2024.217350
22. Lu Q, Wang N, Jiang K, Zhou H, Zhang P, Zhang J, et al. Comprehensive genomic profiling to identify actionable alterations for breast cancer brain metastases in the chinese population. ESMO Open. (2024) 9:102389. doi: 10.1016/j.esmoop.2024.102389
23. Liu ZL, Chen HH, Zheng LL, Sun LP, and Shi L. Angiogenic signaling pathways and anti-angiogenic therapy for cancer. Signal Transduct Target Ther. (2023) 8:198. doi: 10.1038/s41392-023-01460-1
24. Chilla A, Anceschi C, Frediani E, Scavone F, Del Rosso T, Pelagio G, et al. Inhibition of mmps supports amoeboid angiogenesis hampering vegf-targeted therapies via mlc and erk 1/2 signaling. J Transl Med. (2023) 21:102. doi: 10.1186/s12967-023-03954-6
25. Yu B and Ma W. Biomarker discovery in hepatocellular carcinoma (Hcc) for personalized treatment and enhanced prognosis. Cytokine Growth Factor Rev. (2024) 79:29–38. doi: 10.1016/j.cytogfr.2024.08.006
26. Kang JH, Uddin N, Kim S, Zhao Y, Yoo KC, Kim MJ, et al. Tumor-intrinsic role of icam-1 in driving metastatic progression of triple-negative breast cancer through direct interaction with egfr. Mol Cancer. (2024) 23:230. doi: 10.1186/s12943-024-02150-4
27. Li Y, Dou Y, Da Veiga Leprevost F, Geffen Y, Calinawan AP, Aguet F, et al. Proteogenomic data and resources for pan-cancer analysis. Cancer Cell. (2023) 41:1397–406. doi: 10.1016/j.ccell.2023.06.009
28. Zhang J, Sun R, Lyu Y, Liu C, Liu Y, Feng Y, et al. Proteomic profiling of gliomas unveils immune and metabolism-driven subtypes with implications for anti-nucleotide metabolism therapy. Nat Commun. (2024) 15:10005. doi: 10.1038/s41467-024-54352-5
29. de Visser KE and Joyce JA. The evolving tumor microenvironment: from cancer initiation to metastatic outgrowth. Cancer Cell. (2023) 41:374–403. doi: 10.1016/j.ccell.2023.02.016
30. Angelico G, Broggi G, Tinnirello G, Puzzo L, Vecchio GM, Salvatorelli L, et al. Tumor infiltrating lymphocytes (Tils) and pd-L1 expression in breast cancer: A review of current evidence and prognostic implications from pathologist's perspective. Cancers (Basel). (2023) 15:4479. doi: 10.3390/cancers15184479
31. Zhang Y, Cheng R, Ding T, and Wu J. Discrepancies in pd-L1 expression, lymphocyte infiltration, and tumor mutational burden in non-small cell lung cancer and matched brain metastases. Transl Lung Cancer Res. (2024) 13:3590–602. doi: 10.21037/tlcr-24-735
32. Sanchez-Magraner L, Gumuzio J, Miles J, Quimi N, Martinez Del Prado P, Abad-Villar MT, et al. Functional engagement of the pd-1/pd-L1 complex but not pd-L1 expression is highly predictive of patient response to immunotherapy in non-small-cell lung cancer. J Clin Oncol. (2023) 41:2561–70. doi: 10.1200/JCO.22.01748
33. Di Federico A, Alden SL, Smithy JW, Ricciuti B, Alessi JV, Wang X, et al. Intrapatient variation in pd-L1 expression and tumor mutational burden and the impact on outcomes to immune checkpoint inhibitor therapy in patients with non-small-cell lung cancer. Ann Oncol. (2024) 35:902–13. doi: 10.1016/j.annonc.2024.06.014
34. Li Y, Zhang C, Jiang A, Lin A, Liu Z, Cheng X, et al. Potential anti-tumor effects of regulatory T cells in the tumor microenvironment: A review. J Transl Med. (2024) 22:293. doi: 10.1186/s12967-024-05104-y
35. Goswami TK, Singh M, Dhawan M, Mitra S, Emran TB, Rabaan AA, et al. Regulatory T cells (Tregs) and their therapeutic potential against autoimmune disorders - advances and challenges. Hum Vaccin Immunother. (2022) 18:2035117. doi: 10.1080/21645515.2022.2035117
36. Van de Sande B, Lee JS, Mutasa-Gottgens E, Naughton B, Bacon W, Manning J, et al. Applications of single-cell rna sequencing in drug discovery and development. Nat Rev Drug Discov. (2023) 22:496–520. doi: 10.1038/s41573-023-00688-4
37. Yeo AT, Rawal S, Delcuze B, Christofides A, Atayde A, Strauss L, et al. Single-cell rna sequencing reveals evolution of immune landscape during glioblastoma progression. Nat Immunol. (2022) 23:971–84. doi: 10.1038/s41590-022-01215-0
38. Robinson SD, de Boisanger J, Pearl FMG, Critchley G, Rosenfelder N, and Giamas G. A brain metastasis liquid biopsy: where are we now? Neurooncol Adv. (2024) 6:vdae066. doi: 10.1093/noajnl/vdae066
39. Erez N, Furth N, Fedyuk V, Wadden J, Aittaleb R, Adam T, et al. Single-molecule systems for the detection and monitoring of plasma-circulating nucleosomes and oncoproteins in diffuse midline glioma. Cell Rep Med. (2025) 6:101918. doi: 10.1016/j.xcrm.2024.101918
40. Wang X, Wang L, Lin H, Zhu Y, Huang D, Lai M, et al. Research progress of ctc, ctdna, and evs in cancer liquid biopsy. Front Oncol. (2024) 14:1303335. doi: 10.3389/fonc.2024.1303335
41. Ma L, Guo H, Zhao Y, Liu Z, Wang C, Bu J, et al. Liquid biopsy in cancer current: status, challenges and future prospects. Signal Transduct Target Ther. (2024) 9:336. doi: 10.1038/s41392-024-02021-w
42. Yi M, Li T, Niu M, Zhang H, Wu Y, Wu K, et al. Targeting cytokine and chemokine signaling pathways for cancer therapy. Signal Transduct Target Ther. (2024) 9:176. doi: 10.1038/s41392-024-01868-3
43. Orange ST, Leslie J, Ross M, Mann DA, and Wackerhage H. The exercise il-6 enigma in cancer. Trends Endocrinol Metab. (2023) 34:749–63. doi: 10.1016/j.tem.2023.08.001
44. Alix-Panabieres C and Pantel K. Advances in liquid biopsy: from exploration to practical application. Cancer Cell. (2024) 43(2):161–5. doi: 10.1016/j.ccell.2024.11.009
45. Zhang L, Wang Z, Liu K, Liu Y, Wang S, Jiang W, et al. Targets of tumor microenvironment for potential drug development. MedComm – Oncol. (2024) 3:e68. doi: 10.1002/mog2.68
46. Deichaite I, Sears TJ, Sutton L, Rebibo D, Morgan K, Nelson T, et al. Differential regulation of tnfα and il-6 expression contributes to immune evasion in prostate cancer. J Trans Med. (2022) 20:527. doi: 10.1186/s12967-022-03731-x
47. Florescu DN, Boldeanu MV, Serban RE, Florescu LM, Serbanescu MS, Ionescu M, et al. Correlation of the pro-inflammatory cytokines il-1beta, il-6, and tnf-alpha, inflammatory markers, and tumor markers with the diagnosis and prognosis of colorectal cancer. Life (Basel). (2023) 13:2261. doi: 10.3390/life13122261
48. Deng Z, Fan T, Xiao C, Tian H, Zheng Y, Li C, et al. Tgf-beta signaling in health, disease, and therapeutics. Signal Transduct Target Ther. (2024) 9:61. doi: 10.1038/s41392-024-01764-w
49. Anastasiadou DP, Quesnel A, Duran CL, Filippou PS, and Karagiannis GS. An emerging paradigm of cxcl12 involvement in the metastatic cascade. Cytokine Growth Factor Rev. (2024) 75:12–30. doi: 10.1016/j.cytogfr.2023.10.003
50. Stanilov N, Velikova T, and Stanilova S. Navigating the cytokine seas: targeting cytokine signaling pathways in cancer therapy. Int J Mol Sci. (2024) 25:1009. doi: 10.3390/ijms25021009
51. Liu B, Zhou H, Tan L, Siu KTH, and Guan XY. Exploring treatment options in cancer: tumor treatment strategies. Signal Transduct Target Ther. (2024) 9:175. doi: 10.1038/s41392-024-01856-7
52. Li T, Sun S, Li Y, Zhang Y, and Wei L. Immunotherapy revolutionizing brain metastatic cancer treatment: personalized strategies for transformative outcomes. Front Immunol. (2024) 15:1418580. doi: 10.3389/fimmu.2024.1418580
53. He F, Aebersold R, Baker MS, Bian X, Bo X, Chan DW, et al. Pi-hub: the proteomic navigator of the human body. Nature. (2024) 636:322–31. doi: 10.1038/s41586-024-08280-5
54. Passaro A, Al Bakir M, Hamilton EG, Diehn M, Andre F, Roy-Chowdhuri S, et al. Cancer biomarkers: emerging trends and clinical implications for personalized treatment. Cell. (2024) 187:1617–35. doi: 10.1016/j.cell.2024.02.041
55. Zhou J, Yan P, Ma W, and Li J. Cytokine modulation and immunoregulation of uterine nk cells in pregnancy disorders. Cytokine Growth Factor Rev. (2024) 14:1332057. doi: 10.1016/j.cytogfr.2024.11.007
56. Chen Q, Jia G, Zhang X, and Ma W. Targeting her3 to overcome egfr tki resistance in nsclc. Front Immunol. (2023) 14:1332057. doi: 10.3389/fimmu.2023.1332057
57. Xie N, Shen G, Gao W, Huang Z, Huang C, and Fu L. Neoantigens: promising targets for cancer therapy. Signal Transduct Target Ther. (2023) 8:9. doi: 10.1038/s41392-022-01270-x
58. Zhang S, Xiao X, Yi Y, Wang X, Zhu L, Shen Y, et al. Tumor initiation and early tumorigenesis: molecular mechanisms and interventional targets. Signal Transduct Target Ther. (2024) 9:149. doi: 10.1038/s41392-024-01848-7
59. Ghalehbandi S, Yuzugulen J, Pranjol MZI, and Pourgholami MH. The role of vegf in cancer-induced angiogenesis and research progress of drugs targeting vegf. Eur J Pharmacol. (2023) 949:175586. doi: 10.1016/j.ejphar.2023.175586
60. Brastianos PK, Carter SL, Santagata S, Cahill DP, Taylor-Weiner A, Jones RT, et al. Genomic characterization of brain metastases reveals branched evolution and potential therapeutic targets. Cancer Discov. (2015) 5:1164–77. doi: 10.1158/2159-8290.CD-15-0369
61. Stancill JS, Kasmani MY, Cui W, and Corbett JA. Single cell rnaseq analysis of cytokine-treated human islets: association of cellular stress with impaired cytokine responsiveness. Function. (2024) 5:zqae015. doi: 10.1093/function/zqae015
62. Wang J, Zhu N, Su X, Gao Y, and Yang R. Novel tumor-associated macrophage populations and subpopulations by single cell rna sequencing. Front Immunol. (2023) 14:1264774. doi: 10.3389/fimmu.2023.1264774
63. Tirosh I and Suva ML. Cancer cell states: lessons from ten years of single-cell rna-sequencing of human tumors. Cancer Cell. (2024) 42:1497–506. doi: 10.1016/j.ccell.2024.08.005
64. Zhang Q, Gao Z, Qiu R, Cao J, Zhang C, Qin W, et al. Single-cell rna sequencing elucidates cellular plasticity in esophageal small cell carcinoma following chemotherapy treatment. Front Genet. (2024) 15:1477705. doi: 10.3389/fgene.2024.1477705
65. Dong ZR, Zhang MY, Qu LX, Zou J, Yang YH, Ma YL, et al. Spatial resolved transcriptomics reveals distinct cross-talk between cancer cells and tumor-associated macrophages in intrahepatic cholangiocarcinoma. biomark Res. (2024) 12:100. doi: 10.1186/s40364-024-00648-z
66. Li C, Guo H, Zhai P, Yan M, Liu C, Wang X, et al. Spatial and single-cell transcriptomics reveal a cancer-associated fibroblast subset in hnscc that restricts infiltration and antitumor activity of cd8+ T cells. Cancer Res. (2024) 84:258–75. doi: 10.1158/0008-5472.CAN-23-1448
67. Glaviano A, Lau HS, Carter LM, Lee EHC, Lam HY, Okina E, et al. Harnessing the tumor microenvironment: targeted cancer therapies through modulation of epithelial-mesenchymal transition. J Hematol Oncol. (2025) 18:6. doi: 10.1186/s13045-024-01634-6
68. Du Y, Ding X, and Ye Y. The spatial multi-omics revolution in cancer therapy: precision redefined. Cell Rep Med. (2024) 5:101740. doi: 10.1016/j.xcrm.2024.101740
69. Jin Y, Zuo Y, Li G, Liu W, Pan Y, Fan T, et al. Advances in spatial transcriptomics and its applications in cancer research. Mol Cancer. (2024) 23:129. doi: 10.1186/s12943-024-02040-9
70. Bogdan B, Hossein A, Mohammad HF, and Ashkan A. Novel proteomics-based plasma test for early detection of multiple cancers in the general population. BMJ Oncol. (2024) 3:e000073. doi: 10.1136/bmjonc-2023-000073
71. Belczacka I, Latosinska A, Metzger J, Marx D, Vlahou A, Mischak H, et al. Proteomics biomarkers for solid tumors: current status and future prospects. Mass Spectrom Rev. (2019) 38:49–78. doi: 10.1002/mas.21572
72. Hao B, Chen K, Zhai L, Liu M, Liu B, and Tan M. Substrate and functional diversity of protein lysine post-translational modifications. Genomics Proteomics Bioinf. (2024) 22:qzae019. doi: 10.1093/gpbjnl/qzae019
73. Kohler D, Tsai TH, Verschueren E, Huang T, Hinkle T, Phu L, et al. Msstatsptm: statistical relative quantification of posttranslational modifications in bottom-up mass spectrometry-based proteomics. Mol Cell Proteomics. (2023) 22:100477. doi: 10.1016/j.mcpro.2022.100477
74. Savage SR, Yi X, Lei JT, Wen B, Zhao H, Liao Y, et al. Pan-cancer proteogenomics expands the landscape of therapeutic targets. Cell. (2024) 187:4389–407 e15. doi: 10.1016/j.cell.2024.05.039
75. Bialecka M, Rac M, Dziedziejko V, Safranow K, Chlubek D, and Rac ME. An evaluation of plasma tnf, vegf-a, and il-6 determination as a risk marker of atherosclerotic vascular damage in early-onset cad patients. J Clin Med. (2024) 13:1742. doi: 10.3390/jcm13061742
76. Walsh MJ, Ali LR, Lenehan P, Kureshi CT, Kureshi R, Dougan M, et al. Blockade of innate inflammatory cytokines tnfα, il-1β, or il-6 overcomes virotherapy-induced cancer equilibrium to promote tumor regression. Immunotherapy Adv. (2023) 3:ltad011. doi: 10.1093/immadv/ltad011
77. Kumar MA, Baba SK, Sadida HQ, Marzooqi SA, Jerobin J, Altemani FH, et al. Extracellular vesicles as tools and targets in therapy for diseases. Signal Transduct Target Ther. (2024) 9:27. doi: 10.1038/s41392-024-01735-1
78. Araujo-Abad S, Berna JM, Lloret-Lopez E, Lopez-Cortes A, Saceda M, and de Juan Romero C. Exosomes: from basic research to clinical diagnostic and therapeutic applications in cancer. Cell Oncol (Dordr). (2024) 48(2):269–93. doi: 10.1007/s13402-024-00990-2
79. Foser S, Maiese K, Digumarthy SR, Puig-Butille JA, and Rebhan C. Looking to the future of early detection in cancer: liquid biopsies, imaging, and artificial intelligence. Clin Chem. (2024) 70:27–32. doi: 10.1093/clinchem/hvad196
80. Huang D, Ma N, Li X, Gou Y, Duan Y, Liu B, et al. Advances in single-cell rna sequencing and its applications in cancer research. J Hematol Oncol. (2023) 16:98. doi: 10.1186/s13045-023-01494-6
81. Piwecka M, Rajewsky N, and Rybak-Wolf A. Single-cell and spatial transcriptomics: deciphering brain complexity in health and disease. Nat Rev Neurol. (2023) 19:346–62. doi: 10.1038/s41582-023-00809-y
82. Gong D, Arbesfeld-Qiu JM, Perrault E, Bae JW, and Hwang WL. Spatial oncology: translating contextual biology to the clinic. Cancer Cell. (2024) 42:1653–75. doi: 10.1016/j.ccell.2024.09.001
83. Kumar P, Gupta S, and Das BC. Saliva as a potential non-invasive liquid biopsy for early and easy diagnosis/prognosis of head and neck cancer. Transl Oncol. (2024) 40:101827. doi: 10.1016/j.tranon.2023.101827
84. Dong W, Sheng J, Cui JZM, Zhao H, and Wong STC. Systems immunology insights into brain metastasis. Trends Immunol. (2024) 45:903–16. doi: 10.1016/j.it.2024.09.010
85. Khalifa M and Albadawy M. Artificial intelligence for clinical prediction: exploring key domains and essential functions. Comput Methods Programs Biomedicine Update. (2024) 5:100148. doi: 10.1016/j.cmpbup.2024.100148
86. Liu Y, Altreuter J, Bodapati S, Cristea S, Wong CJ, Wu CJ, et al. Predicting patient outcomes after treatment with immune checkpoint blockade: A review of biomarkers derived from diverse data modalities. Cell Genom. (2024) 4:100444. doi: 10.1016/j.xgen.2023.100444
87. Lippitz BE and Harris RA. Cytokine patterns in cancer patients: A review of the correlation between interleukin 6 and prognosis. Oncoimmunology. (2016) 5:e1093722. doi: 10.1080/2162402X.2015.1093722
88. Mollica V, Rizzo A, Marchetti A, Tateo V, Tassinari E, Rosellini M, et al. The impact of ecog performance status on efficacy of immunotherapy and immune-based combinations in cancer patients: the mouseion-06 study. Clin Exp Med. (2023) 23:5039–49. doi: 10.1007/s10238-023-01159-1
89. Tang T, Huang X, Zhang G, Hong Z, Bai X, and Liang T. Advantages of targeting the tumor immune microenvironment over blocking immune checkpoint in cancer immunotherapy. Signal Transduct Target Ther. (2021) 6:72. doi: 10.1038/s41392-020-00449-4
90. Catanzaro E, Beltran-Visiedo M, Galluzzi L, and Krysko DV. Immunogenicity of cell death and cancer immunotherapy with immune checkpoint inhibitors. Cell Mol Immunol. (2025) 22:24–39. doi: 10.1038/s41423-024-01245-8
91. Sordo-Bahamonde C, Lorenzo-Herrero S, Gonzalez-Rodriguez AP, Martinez-Perez A, Rodrigo JP, Garcia-Pedrero JM, et al. Chemo-immunotherapy: A new trend in cancer treatment. Cancers (Basel). (2023) 15:2912. doi: 10.3390/cancers15112912
92. Wang SL and Chan TA. Navigating established and emerging biomarkers for immune checkpoint inhibitor therapy. Cancer Cell. (2025) 43:641–64. doi: 10.1016/j.ccell.2025.03.006
93. Mojsak D, Kuklinska B, Minarowski L, and Mroz RM. Current state of knowledge on immunotherapy in ecog ps 2 patients. A systematic review. Adv Med Sci. (2021) 66:381–7. doi: 10.1016/j.advms.2021.07.005
94. Andrews MC, Li G, Graf RP, Fisher VA, Mitchell J, Aboosaiedi A, et al. Predictive impact of tumor mutational burden on real-world outcomes of first-line immune checkpoint inhibition in metastatic melanoma. JCO Precis Oncol. (2024) 8:e2300640. doi: 10.1200/PO.23.00640
95. Aggarwal C, Ben-Shachar R, Gao Y, Hyun SW, Rivers Z, Epstein C, et al. Assessment of tumor mutational burden and outcomes in patients with diverse advanced cancers treated with immunotherapy. JAMA Netw Open. (2023) 6:e2311181. doi: 10.1001/jamanetworkopen.2023.11181
96. Nimmagadda S. Imaging pd-L1 expression in melanoma brain metastases. J Nucl Med. (2022) 63:897–8. doi: 10.2967/jnumed.121.263209
97. Placke JM, Kimmig M, Griewank K, Herbst R, Terheyden P, Utikal J, et al. Correlation of tumor pd-L1 expression in different tissue types and outcome of pd-1-based immunotherapy in metastatic melanoma - analysis of the decog prospective multicenter cohort study adoreg/trim. EBioMedicine. (2023) 96:104774. doi: 10.1016/j.ebiom.2023.104774
98. Peyraud F, Guegan J-P, Vanhersecke L, Brunet M, Teyssonneau D, Palmieri L-J, et al. Tertiary lymphoid structures and cancer immunotherapy: from bench to bedside. Med. (2025) 6:100546. doi: 10.1016/j.medj.2024.10.023
99. Zhang H, Chen L, Li L, Liu Y, Das B, Zhai S, et al. Prediction and analysis of tumor infiltrating lymphocytes across 28 cancers by tilscout using deep learning. NPJ Precis Oncol. (2025) 9:76. doi: 10.1038/s41698-025-00866-0
100. Toner YC, Prevot G, van Leent MMT, Munitz J, Oosterwijk R, Verschuur AVD, et al. Macrophage pet imaging in mouse models of cardiovascular disease and cancer with an apolipoprotein-inspired radiotracer. NPJ Imaging. (2024) 2:12. doi: 10.1038/s44303-024-00009-3
101. Stefano A. Challenges and limitations in applying radiomics to pet imaging: possible opportunities and avenues for research. Comput Biol Med. (2024) 179:108827. doi: 10.1016/j.compbiomed.2024.108827
102. Sako C, Duan C, Maresca K, Kent S, Schmidt TG, Aerts H, et al. Real-world and clinical trial validation of a deep learning radiomic biomarker for pd-(L)1 immune checkpoint inhibitor response in advanced non-small cell lung cancer. JCO Clin Cancer Inform. (2024) 8:e2400133. doi: 10.1200/CCI.24.00133
103. Bernatowicz K, Amat R, Prior O, Frigola J, Ligero M, Grussu F, et al. Radiomics signature for dynamic monitoring of tumor inflamed microenvironment and immunotherapy response prediction. J Immunother Cancer. (2025) 13:e009140. doi: 10.1136/jitc-2024-009140
104. Wang H, Cheng L, Zhao C, Zhou F, Jiang T, Guo H, et al. Efficacy of immune checkpoint inhibitors in advanced non-small cell lung cancer harboring braf mutations. Transl Lung Cancer Res. (2023) 12:219–29. doi: 10.21037/tlcr-22-613
105. Hu X, Guo J, Shi J, Li D, Li X, and Zhao W. A 20-gene mutation signature predicts the efficacy of immune checkpoint inhibitor therapy in advanced non-small cell lung cancer patients. BMC Pulm Med. (2023) 23:223. doi: 10.1186/s12890-023-02512-6
106. Maiorano BA, Di Maio M, Cerbone L, Maiello E, Procopio G, Roviello G, et al. Significance of pd-L1 in metastatic urothelial carcinoma treated with immune checkpoint inhibitors: A systematic review and meta-analysis. JAMA Network Open. (2024) 7:e241215–e. doi: 10.1001/jamanetworkopen.2024.1215
107. Muhammad S, Fan T, Hai Y, Gao Y, and He J. Reigniting hope in cancer treatment: the promise and pitfalls of il-2 and il-2r targeting strategies. Mol Cancer. (2023) 22:121. doi: 10.1186/s12943-023-01826-7
108. Liu XH, Wang GR, Zhong NN, Wang WY, Liu B, Li Z, et al. Multi-omics in immunotherapy research for hnscc: present situation and future perspectives. NPJ Precis Oncol. (2025) 9:93. doi: 10.1038/s41698-025-00886-w
109. Bai JW, Qiu SQ, and Zhang GJ. Molecular and functional imaging in cancer-targeted therapy: current applications and future directions. Signal Transduct Target Ther. (2023) 8:89. doi: 10.1038/s41392-023-01366-y
110. Perez RC, Kim D, Maxwell AWP, and Camacho JC. Functional imaging of hypoxia: pet and mri. Cancers (Basel). (2023) 15:3336. doi: 10.3390/cancers15133336
111. An YS, Kim SH, Roh TH, Park SH, Kim TG, and Kim JH. Correlation between (18)F-fdg uptake and immune cell infiltration in metastatic brain lesions. Front Oncol. (2021) 11:618705. doi: 10.3389/fonc.2021.618705
112. Gangadaran P, Onkar A, Rajendran RL, Goenka A, Oh JM, Khan F, et al. Noninvasive in vivo imaging of macrophages: understanding tumor microenvironments and delivery of therapeutics. biomark Res. (2025) 13:20. doi: 10.1186/s40364-025-00735-9
113. Mori Y, Dendl K, Cardinale J, Kratochwil C, Giesel FL, and Haberkorn U. Fapi pet: fibroblast activation protein inhibitor use in oncologic and nononcologic disease. Radiology. (2023) 306:e220749. doi: 10.1148/radiol.220749
114. Lukovic D, Gyongyosi M, Pavo IJ, Mester-Tonczar J, Einzinger P, Zlabinger K, et al. Increased [(18)F]Fdg uptake in the infarcted myocardial area displayed by combined pet/cmr correlates with snrna-seq-detected inflammatory cell invasion. Basic Res Cardiol. (2024) 119:807–29. doi: 10.1007/s00395-024-01064-y
115. Tompkins AG, Gray ZN, Dadey RE, Zenkin S, Batavani N, Newman S, et al. Radiomic analysis of patient and interorgan heterogeneity in response to immunotherapies and braf-targeted therapy in metastatic melanoma. J Immunother Cancer. (2025) 13:e009568. doi: 10.1136/jitc-2024-009568
116. Roisman LC, Kian W, Anoze A, Fuchs V, Spector M, Steiner R, et al. Radiological artificial intelligence - predicting personalized immunotherapy outcomes in lung cancer. NPJ Precis Oncol. (2023) 7:125. doi: 10.1038/s41698-023-00473-x
117. Wei J, Li W, Zhang P, Guo F, and Liu M. Current trends in sensitizing immune checkpoint inhibitors for cancer treatment. Mol Cancer. (2024) 23:279. doi: 10.1186/s12943-024-02179-5
118. Kim AE, Nieblas-Bedolla E, de Sauvage MA, and Brastianos PK. Leveraging translational insights toward precision medicine approaches for brain metastases. Nat Cancer. (2023) 4:955–67. doi: 10.1038/s43018-023-00585-0
119. Colomer R, Miranda J, Romero-Laorden N, Hornedo J, González-Cortijo L, Mouron S, et al. Usefulness and real-world outcomes of next generation sequencing testing in patients with cancer: an observational study on the impact of selection based on clinical judgement. eClinicalMedicine. (2023) 60:102029. doi: 10.1016/j.eclinm.2023.102029
120. Kirschenbaum D, Xie K, Ingelfinger F, Katzenelenbogen Y, Abadie K, Look T, et al. Time-resolved single-cell transcriptomics defines immune trajectories in glioblastoma. Cell. (2024) 187:149–65.e23. doi: 10.1016/j.cell.2023.11.032
121. Wu S, Zhang S, Liu C-M, Fernie AR, and Yan S. Recent advances in mass spectrometry-based protein interactome studies. Mol Cell Proteomics. (2025) 24:100887. doi: 10.1016/j.mcpro.2024.100887
122. Jia D, Jiang Z, Cui M, and Ding X. Proteomics efforts for hepatocellular carcinoma drug development. Clin Cancer Bull. (2024) 3:22. doi: 10.1007/s44272-024-00027-7
123. Giloteaux L, Li J, Hornig M, Lipkin WI, Ruppert D, and Hanson MR. Proteomics and cytokine analyses distinguish myalgic encephalomyelitis/chronic fatigue syndrome cases from controls. J Trans Med. (2023) 21:322. doi: 10.1186/s12967-023-04179-3
124. Lee T-A, Tsai E-Y, Liu S-H, Hsu Hung S-D, Chang S-J, Chao C-H, et al. Post-translational modification of pd-1: potential targets for cancer immunotherapy. Cancer Res. (2024) 84:800–7. doi: 10.1158/0008-5472.Can-23-2664
125. Batool SM, Yekula A, Khanna P, Hsia T, Gamblin AS, Ekanayake E, et al. The liquid biopsy consortium: challenges and opportunities for early cancer detection and monitoring. Cell Rep Med. (2023) 4:101198. doi: 10.1016/j.xcrm.2023.101198
126. Abdul-Rahman T, Ghosh S, Badar SM, Nazir A, Bamigbade GB, Aji N, et al. The paradoxical role of cytokines and chemokines at the tumor microenvironment: A comprehensive review. Eur J Med Res. (2024) 29:124. doi: 10.1186/s40001-024-01711-z
127. Shishido SN, Hart O, Jeong S, Moriarty A, Heeke D, Rossi J, et al. Liquid biopsy approach to monitor the efficacy and response to car-T cell therapy. J ImmunoTherapy Cancer. (2024) 12:e007329. doi: 10.1136/jitc-2023-007329
128. Zhang C, Li T, Zhao Q, Ma R, Hong Z, Huang X, et al. Advances and prospects in liquid biopsy techniques for Malignant tumor diagnosis and surveillance. Small. (2024) 20:2404709. doi: 10.1002/smll.202404709
129. Zhan T, Betge J, Schulte N, Dreikhausen L, Hirth M, Li M, et al. Digestive cancers: mechanisms, therapeutics and management. Signal Transduction Targeted Ther. (2025) 10:24. doi: 10.1038/s41392-024-02097-4
130. Kim YJ, Rho W-Y, Park S-M, and Jun B-H. Optical nanomaterial-based detection of biomarkers in liquid biopsy. J Hematol Oncol. (2024) 17:10. doi: 10.1186/s13045-024-01531-y
131. Wu Y, Yang F, Luo S, Li X, Gu Z, Fan R, et al. Single-cell rna sequencing reveals epithelial cells driving brain metastasis in lung adenocarcinoma. iScience. (2024) 27:109258. doi: 10.1016/j.isci.2024.109258
132. Biricioiu MR, Sarbu M, Ica R, Vukelic Z, Kalanj-Bognar S, and Zamfir AD. Advances in mass spectrometry of gangliosides expressed in brain cancers. Int J Mol Sci. (2024) 25:1335. doi: 10.3390/ijms25021335
133. Karalis VD. The integration of artificial intelligence into clinical practice. Appl Biosci. (2024) 3:14–44. doi: 10.3390/applbiosci3010002
134. Steiner HL, Williams S, Banerjee M, Saporita A, Gilliam B, and Qiang X. Establishing an immunological profile of 96 cytokines, chemokines, and growth factors in human biofluids via milliplex® Multiplex immunoassay. J Immunol. (2023) 210:243.15–.15. doi: 10.4049/jimmunol.210.Supp.243.15
135. Birhanu AG. Mass spectrometry-based proteomics as an emerging tool in clinical laboratories. Clin Proteomics. (2023) 20:32. doi: 10.1186/s12014-023-09424-x
136. Jiang P, Zhang Y, Ru B, Yang Y, Vu T, Paul R, et al. Systematic investigation of cytokine signaling activity at the tissue and single-cell levels. Nat Methods. (2021) 18:1181–91. doi: 10.1038/s41592-021-01274-5
137. Li Y, Luo L, Kong Y, Li Y, Wang Q, Wang M, et al. Recent advances in molecularly imprinted polymer-based electrochemical sensors. Biosensors Bioelectronics. (2024) 249:116018. doi: 10.1016/j.bios.2024.116018
138. Dadgar N, Sherry C, Zimmerman J, Park H, Lewis C, Donnenberg A, et al. Targeting interleukin-6 as a treatment approach for peritoneal carcinomatosis. J Trans Med. (2024) 22:402. doi: 10.1186/s12967-024-05205-8
139. Zhang Y, Li T, Wang G, and Ma Y. Advancements in single-cell rna sequencing and spatial transcriptomics for central nervous system disease. Cell Mol Neurobiol. (2024) 44:65. doi: 10.1007/s10571-024-01499-w
140. Zheng Y, Wagner PD, Singal AG, Hanash SM, Srivastava S, Huang Y, et al. Designing rigorous and efficient clinical utility studies for early detection biomarkers. Cancer Epidemiology Biomarkers Prev. (2024) 33:1150–7. doi: 10.1158/1055-9965.Epi-23-1594
141. Harishbhai Tilala M, Kumar Chenchala P, Choppadandi A, Kaur J, Naguri S, Saoji R, et al. Ethical considerations in the use of artificial intelligence and machine learning in health care: A comprehensive review. Cureus. (2024) 16:e62443. doi: 10.7759/cureus.62443
142. Lawler M, Keeling P, Kholmanskikh O, Minnaard W, Moehlig-Zuttermeister H, Normanno N, et al. Empowering effective biomarker-driven precision oncology: A call to action. Eur J Cancer. (2024) 209:114225. doi: 10.1016/j.ejca.2024.114225
143. Galassi C, Chan TA, Vitale I, and Galluzzi L. The hallmarks of cancer immune evasion. Cancer Cell. (2024) 42:1825–63. doi: 10.1016/j.ccell.2024.09.010
144. Liu X, Peng T, Xu M, Lin S, Hu B, Chu T, et al. Spatial multi-omics: deciphering technological landscape of integration of multi-omics and its applications. J Hematol Oncol. (2024) 17:72. doi: 10.1186/s13045-024-01596-9
145. Sako C, Duan C, Maresca K, Kent S, Schmidt TG, Aerts HJWL, et al. Real-world and clinical trial validation of a deep learning radiomic biomarker for pd-(L)1 immune checkpoint inhibitor response in advanced non–small cell lung cancer. JCO Clin Cancer Inf. (2024) 8):e2400133. doi: 10.1200/cci.24.00133
146. Ahmed Z, Wan S, Zhang F, and Zhong W. Artificial intelligence for omics data analysis. BMC Methods. (2024) 1:4. doi: 10.1186/s44330-024-00004-5
147. Emens LA, Romero PJ, Anderson AC, Bruno TC, Capitini CM, Collyar D, et al. Challenges and opportunities in cancer immunotherapy: A society for immunotherapy of cancer (Sitc) strategic vision. J ImmunoTherapy Cancer. (2024) 12:e009063. doi: 10.1136/jitc-2024-009063
148. Wang M, Yang J, Wang S, Gill H, and Cheng H. Immunotherapy and the tumor microenvironment in brain metastases from non-small cell lung cancer: challenges and future directions. Curr Oncol. (2025) 32:171. doi: 10.3390/curroncol32030171
149. Molla Desta G and Birhanu AG. Advancements in single-cell rna sequencing and spatial transcriptomics: transforming biomedical research. Acta Biochim Pol. (2025) 72:13922. doi: 10.3389/abp.2025.13922
150. Marques L, Costa B, Pereira M, Silva A, Santos J, Saldanha L, et al. Advancing precision medicine: A review of innovative in silico approaches for drug development, clinical pharmacology and personalized healthcare. Pharmaceutics. (2024) 16:132. doi: 10.3390/pharmaceutics16030332
151. Saliev T and Singh PB. From bench to bedside: translating cellular rejuvenation therapies into clinical applications. Cells. (2024) 13:2052. doi: 10.3390/cells13242052
152. Feng Y, Hu X, Zhang Y, and Wang Y. The role of microglia in brain metastases: mechanisms and strategies. Aging Dis. (2024) 15:169–85. doi: 10.14336/AD.2023.0514
153. Brancato V, Esposito G, Coppola L, Cavaliere C, Mirabelli P, Scapicchio C, et al. Standardizing digital biobanks: integrating imaging, genomic, and clinical data for precision medicine. J Transl Med. (2024) 22:136. doi: 10.1186/s12967-024-04891-8
154. Bao R, Hutson A, Madabhushi A, Jonsson VD, Rosario SR, Barnholtz-Sloan JS, et al. Ten challenges and opportunities in computational immuno-oncology. J Immunother Cancer. (2024) 12:e009721. doi: 10.1136/jitc-2024-009721
155. Sharma A, Lysenko A, Jia S, Boroevich KA, and Tsunoda T. Advances in ai and machine learning for predictive medicine. J Hum Genet. (2024) 69:487–97. doi: 10.1038/s10038-024-01231-y
Keywords: biomarkers, immunotherapy, brain metastases, cytokines, tumor microenvironment (TME), transcriptomics
Citation: Li M, Zhang Y, Yu D, Yu Y and Ma W (2025) Immunotherapy biomarkers in brain metastases: insights into tumor microenvironment dynamics. Front. Immunol. 16:1600261. doi: 10.3389/fimmu.2025.1600261
Received: 26 March 2025; Accepted: 28 July 2025;
Published: 13 August 2025.
Edited by:
Chuan Shao, Chongqing General Hospital, ChinaReviewed by:
Rong-Hua Tao, University of Texas MD Anderson Cancer Center, United StatesHaitao Zhu, Northwest Women’s and Children’s Hospital, China
Alexandre Bertucci, Independent Researcher, Marseille, France
Copyright © 2025 Li, Zhang, Yu, Yu and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yaoyu Yu, eXV5YW95dTY2NkBhbGl5dW4uY29t; Wenxue Ma, d21hQGhlYWx0aC51Y3NkLmVkdQ==
†These authors have contributed equally to this work
 Mu Li1†
Mu Li1† Wenxue Ma
Wenxue Ma