- 1Department of Geriatrics, Affiliated Hospital of Medical School, Jinling Hospital, Nanjing University, Nanjing, China
- 2Nursing Department, Affiliated Hospital of Medical School, Jinling Hospital, Nanjing University, Nanjing, China
Background: Synovitis–acne–pustulosis–hyperostosis–osteitis (SAPHO) syndrome is a rare autoimmune disorder. The involvement of spinal and sacroiliac joint in SAPHO syndrome closely resembles the manifestations of postpartum lumbopelvic pain (LPP).
Case presentation: We report a case of a patient whose primary symptom was postpartum LPP, with recurrent episodes lasting 10 months without relief. Unexpectedly, she was diagnosed with SAPHO syndrome in the 11th month when she sought medical attention for severe palmoplantar pustulosis rather than LPP. After combined treatment with Tofacitinib citrate tablets and Etoricoxib tablets, all the pain symptoms disappeared.
Conclusion: For postpartum patients with concurrent palmoplantar scaling and recurrent LPP unresponsive to treatment, clinicians should consider SAPHO syndrome as a potential diagnosis.
Introduction
Lumbopelvic pain (LPP) is a common problem among postpartum women. It is characterized by lumbar pain [low back pain (LBP], pelvic girdle pain (PGP), or both. Studies indicate that 25% of postpartum women suffer from PGP and/or LBP (1), and 21% of these patients may experience LBP for up to 3 years after delivery (1, 2). Furthermore, 10% of patients have reported disability, reduced quality of life, and diminished capacity for full-time work, for up to 10 years postpartum (3).
Synovitis–acne–pustulosis–hyperostosis–osteitis (SAPHO) syndrome is a rare autoimmune disease (ORPHA:793) which was first described by Chamot et al. in 1987 (4). The estimated incidence of SAPHO syndrome is approximately 0.001% - 0.01%, with 1 to 3 new cases per million population annually (5).However, the actual incidence is difficult to determine, as SAPHO syndrome involves multiple medical specialties. It is characterized by sterile inflammatory osteitis and/or arthritis associated with various dermatological manifestations such as acne, palmoplantar pustulosis, and psoriasis. Osteoarticular involvement most commonly affects the anterior chest wall, followed by the spine, sacroiliac joints, and long bones (6). Patients with SAPHO syndrome are saddled with a heavy disease burden. Yet, the average diagnostic time for the disease is 3.8 ± 5.3 years, which results in significant negative impact on the quality of life of these patients (7).
Lumbopelvic pain (LPP) and SAPHO syndrome cause considerable harm to women. Therefore, there is need for early differential diagnosis, as well as prompt and appropriate treatment for the disease. There are very few studies on pregnancy in relation to SAPHO syndrome; we found only two reported cases of patients who became pregnant after being diagnosed with SAPHO (8, 9).We present the first reported case of a patient whose primary symptom was postpartum LPP characterized by recurrent episodes that were refractory to mitigation or treatment for 10 months. Subsequently, based on concurrent palmoplantar pustulosis, sterile spondylitis, sacroiliitis, and sternoclavicular arthritis, she was diagnosed with SAPHO syndrome. After combined therapy with Tofacitinib citrate and Etoricoxib, her symptoms resolved completely.
Case presentation
The patient is a nurse in her 30s who has previously had two live births via natural delivery: one in 2020 and the other in 2023. She developed postpartum lower back pain and pelvic girdle pain which persisted for several months without complete relief or cure. Her maternal uncle suffers from ankylosing spondylitis. Additionally, her maternal grandmother has a severe kyphosis, though undiagnosed. The timeline of her disease course is presented in Table 1.
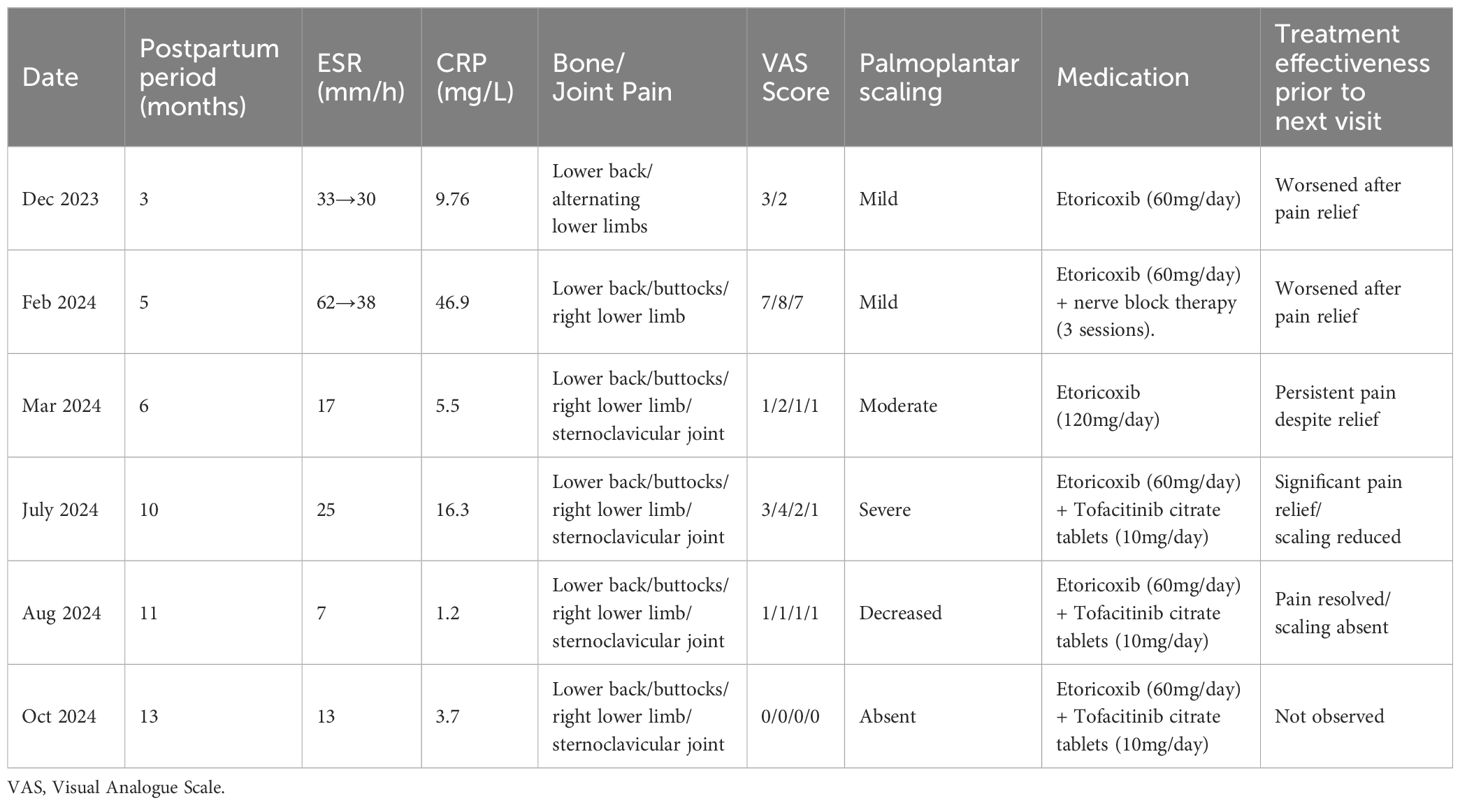
In December 2023 (3rd month postpartum), the patient was hospitalized in the Spine Surgery Department due to low back pain and alternating bilateral lower limb pain. Admission tests revealed the following results: erythrocyte sedimentation rate (ESR) value of 33 mm/h, and C-reactive protein (CRP) value of 9.76 mg/L. Blood culture showed no bacterial growth, but Next-Generation Sequencing (NGS) revealed Propionibacterium acnes. The patient had mild scaling on the palms and soles, which was overlooked. Results from MRI indicated end-plate inflammation at the opposing margins of L1-L3 vertebrae and the upper margins of L4-S1 vertebrae (Figures 1A1-A4). The staging of endplate inflammation is Modic stage I (Inflammation phase). She was diagnosed with low back pain and lumbar muscle strain. During hospitalization, her pain was reduced after oral administration of Etoricoxib at a dose of 60mg, given once daily. Pre-discharge tests showed ESR and CRP values of 30 mm/h and 7.0 mg/L, respectively.
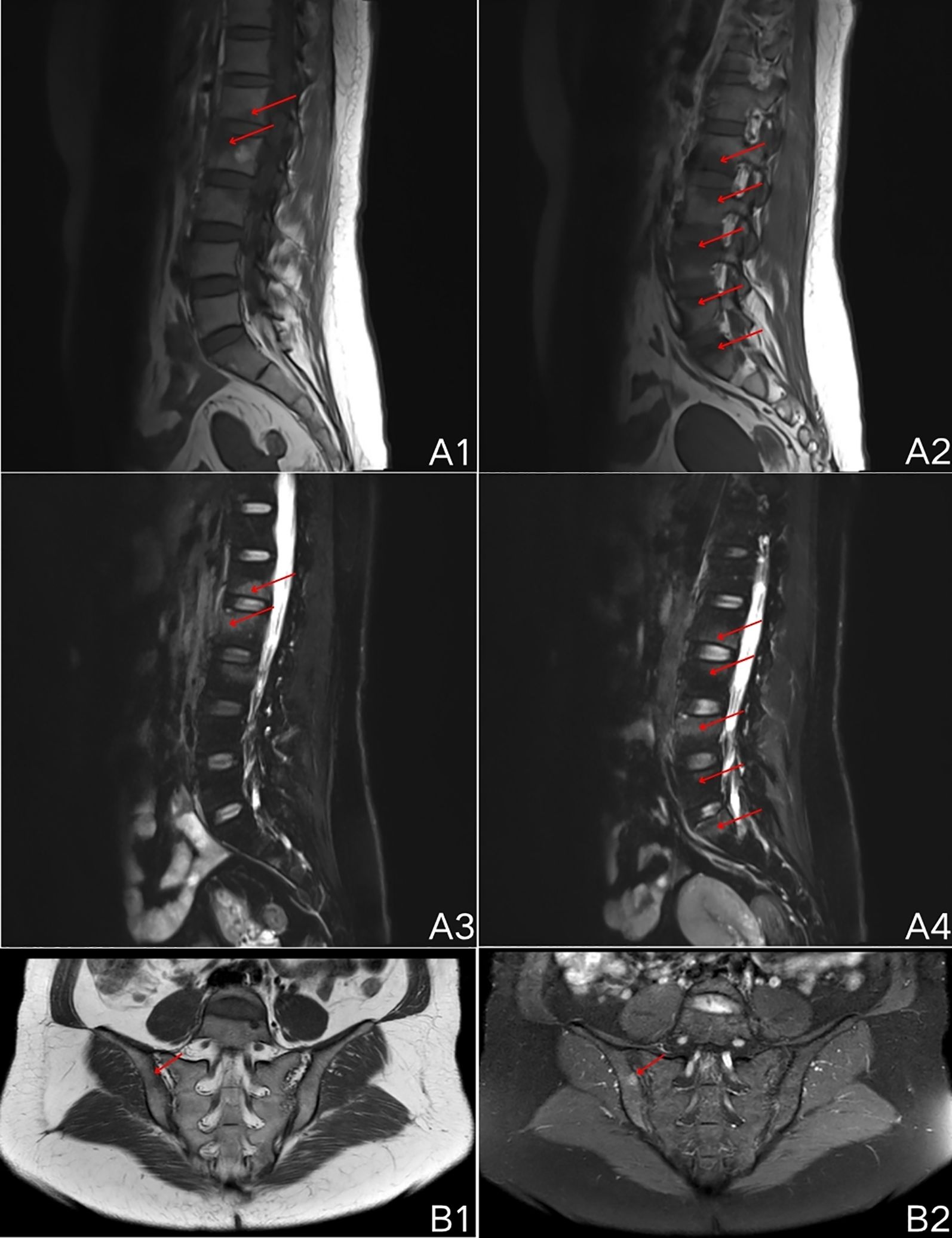
Figure 1. MRI scan results of lumbar spine and sacroiliac joint. (A1-A4), end-plate inflammation (Modic stage I, inflammatory phase) at the opposing margins of L1-L3 vertebrae and the superior margins of L4-S1 vertebrae, T1 sequence shows low signal, T2-FS sequence shows high signal; (B1, B2), abnormal bone signal intensity beneath the right sacroiliac joint surface, T1 sequence shows low signal, PDWI-FS sequence shows high signal.
In February 2024 (5th month postpartum), the patient was re-admitted in the Spine Surgery Department due to low back pain, hip pain, and persistent right lower limb pain for one month, with poor response to oral Etoricoxib. Admission tests revealed ESR and CRP values of 62 mm/h and 46.9 mg/L, respectively. Blood culture results revealed no bacterial growth. Human leukocyte antigen B27 (HLA-B27) test was negative, and X-ray showed no significant abnormalities in the chest. The patient had mild scaling on the palms and soles, which was overlooked. She was diagnosed with sciatica. During hospitalization, she underwent nerve block therapy three times, with postoperative pain relief. She continued taking oral Etoricoxib after discharge. On February 19, 2024, pre-discharge tests showed ESR value of 38 mm/h.
In March 2024 (6th month postpartum), the patient visited the Spine Surgery Outpatient Department due to sternoclavicular joint pain, lower back pain, hip pain, and right lower limb pain. Sacroiliac joint MRI indicated abnormal bone signal intensity beneath the right sacroiliac joint surface (Figures 1B1, B2). The patient exhibited significant scaling on the palms and soles, which was not taken seriously. She was diagnosed with inflammatory spondylopathy (spondyloarthritis), and treatment was continued with oral Etoricoxib (60mg once daily). Four days later, she returned to the outpatient clinic due to persistent nocturnal pain despite Etoricoxib use, and she was advised to increase the dose to 60mg once, twice daily. By April 2024 (7th month postpartum), her pain symptoms had reduced. Tests revealed ESR and CRP values of 17 mm/h and 5.5 mg/L, respectively. She was advised to gradually reduce the dose of Etoricoxib over the next two months.
In July 2024 (10th month postpartum), her pain symptoms showed no further reduction, with sternoclavicular joint pain, lower back pain, hip pain, and lower limb pain still persisting. This time around, she visited the Dermatology Department due to severe scaling on the palms and soles. Laboratory tests indicated ESR value of 25 mm/h, and CRP value of 16.3 mg/L. Results from SPECT bone scan revealed inflammation in the sternoclavicular joint and right sacroiliac joint (Figure 2). Based on NGS results, laboratory findings, imaging, and symptoms such as lower back pain, sternoclavicular joint pain, and palmoplantar scaling, she was diagnosed with a rare condition, i.e., SAPHO syndrome (10). This diagnosis was hinged on the 2003 diagnostic criteria described by Kahn et al. Several studies have confirmed the efficacy of tofacitinib in alleviating functional impairments associated with SAPHO syndrome (11–14). Therefore, her treatment regimen comprised Tofacitinib citrate tablets (5mg/tablet, twice daily) and a reduced dose of Etoricoxib (60mg/tablet, once daily).
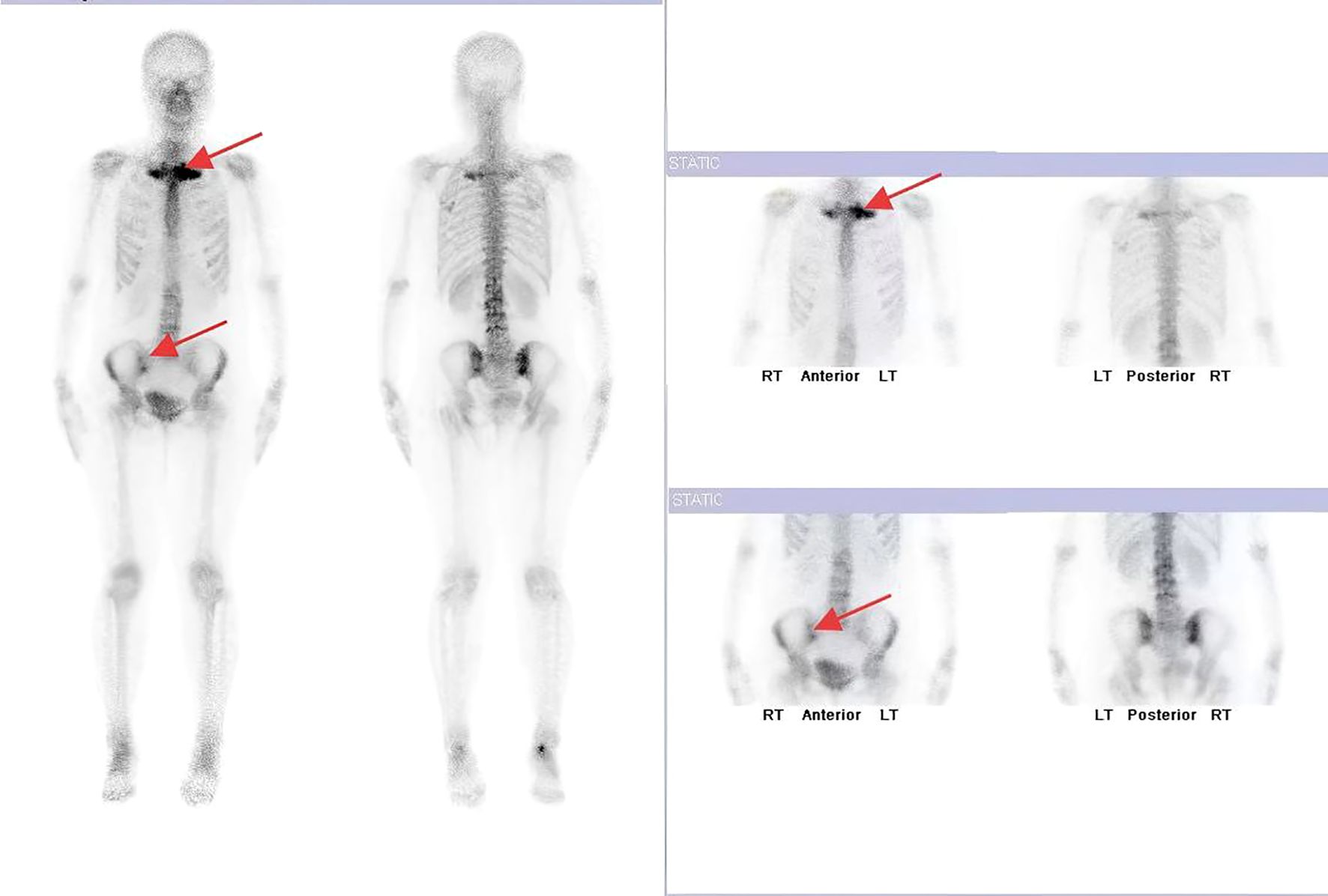
Figure 2. SPECT revealing abnormally increased bone metabolism in the sternoclavicular joints and right sacroiliac joint.
In the 11th month postpartum (August 2024), after continued use of Tofacitinib citrate tablets and Etoricoxib tablets, her pain symptoms were significantly reduced, and the palmoplantar scaling symptoms were alleviated. Laboratory tests indicated ESR and CRP levels of 7 mm/h and 1.2 mg/L, respectively.
By October 2024 (13th month postpartum), her pain symptoms had resolved, with only mild sternoclavicular joint pain remaining, and palmoplantar scaling symptoms had disappeared. These data are presented in Figure 3. Laboratory tests showed ESR value of 13 mm/h and CRP value of 3.7 mg/L. During this examination, the patient was diagnosed with influenza and bronchitis.
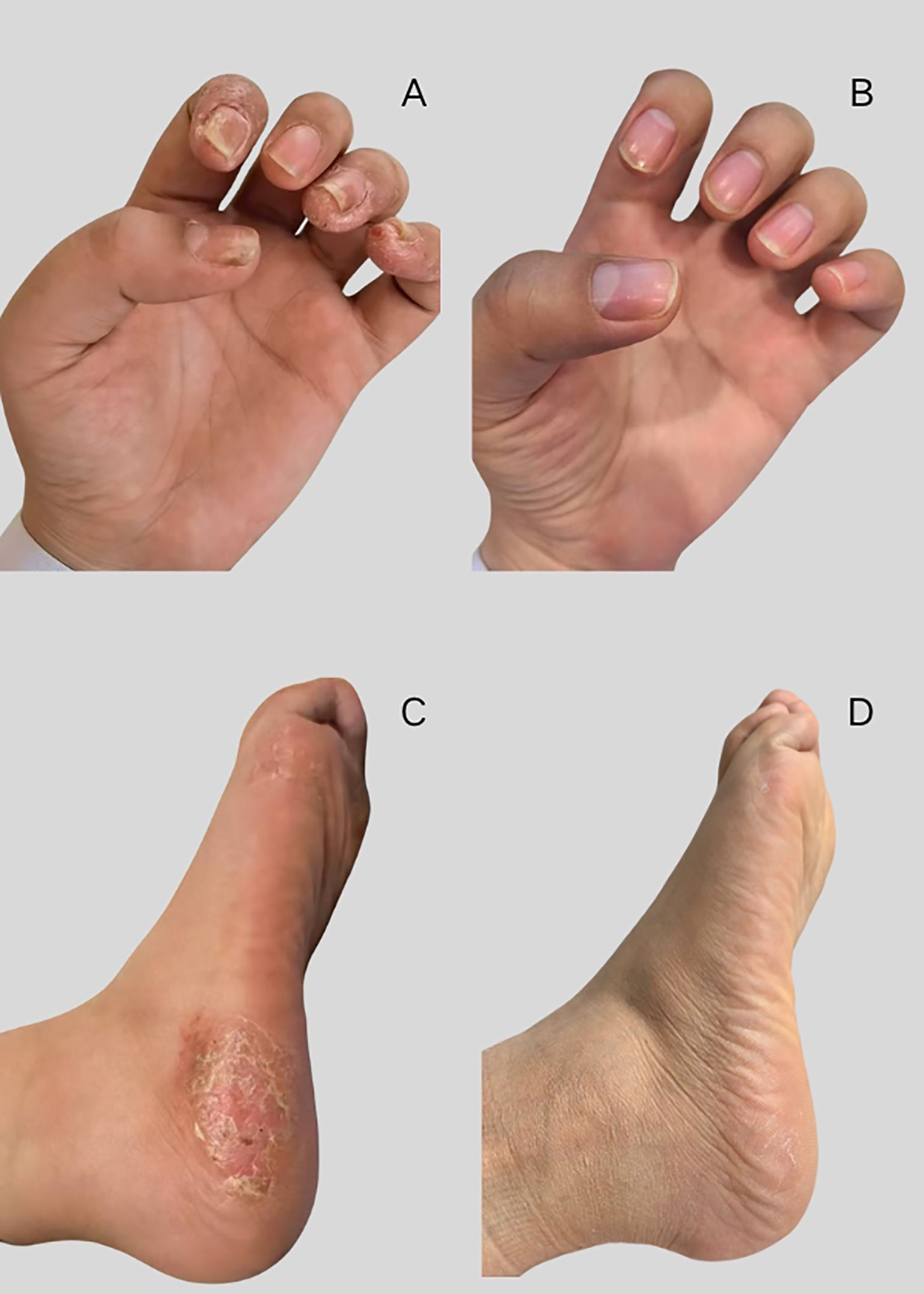
Figure 3. Changes in palmoplantar scaling symptoms. (A, B) palmoplantar scaling symptoms, (C, D) disappearance of palmoplantar scaling symptoms.
As of July 2025, all the patient’s pain symptoms and palmoplantar scaling symptoms had essentially disappeared. In July 2025, the latest MRI examination revealed that the edema in the patient’s sacroiliac joint had disappeared. The MRI showed endplate inflammation (Modic stage II, stable phase) on the contralateral edge of the L2-L3 vertebral bodies and the superior edge of the L4-S1 vertebral bodies. The inflammation on the contralateral edge of the L2-L3 vertebral bodies had resolved (Figure 4).
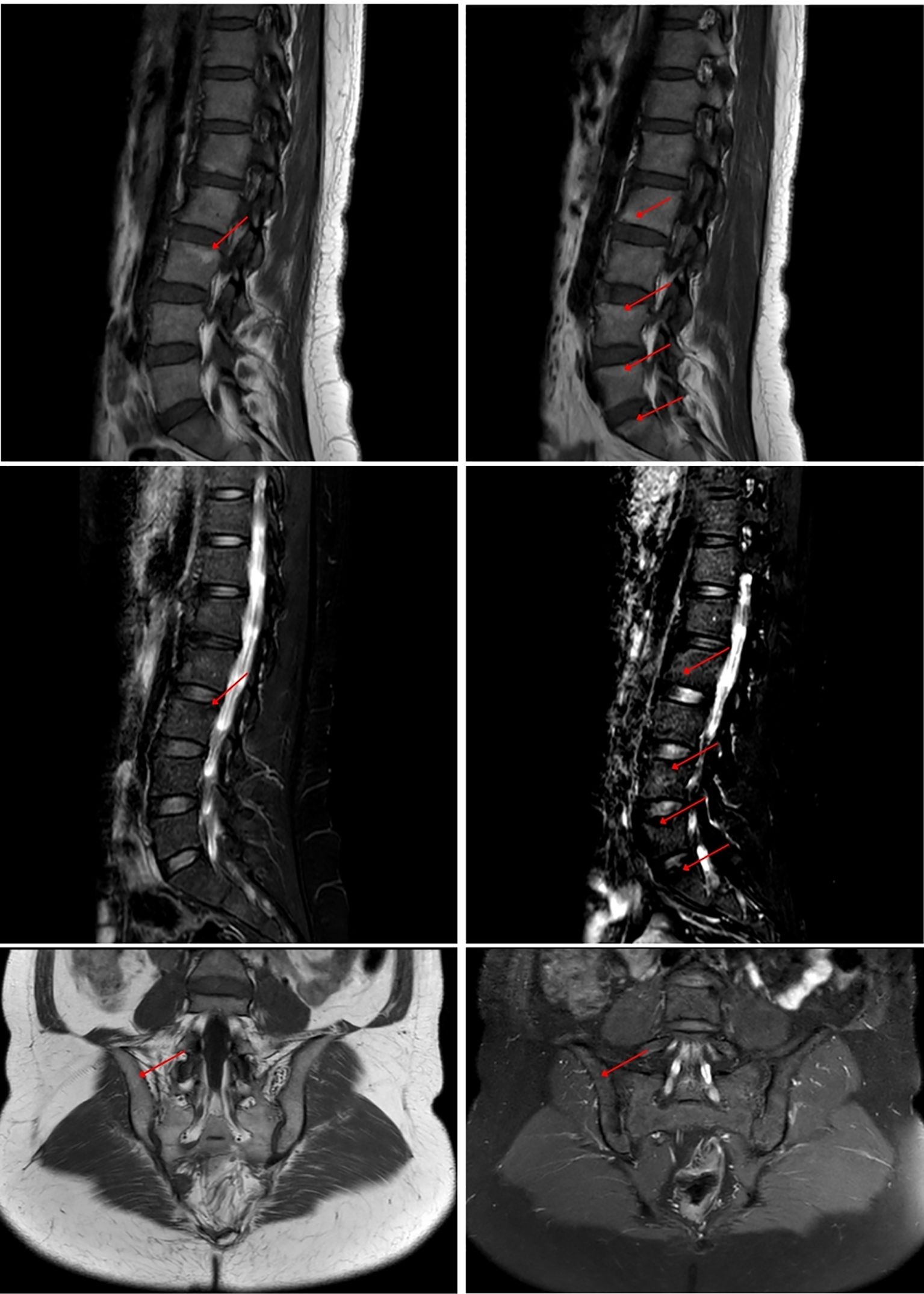
Figure 4. MRI showing end-plate inflammation (Modic stage II, stable phase) at the opposing margins of L2-L3 vertebrae and the superior margins of L4-S1 vertebrae. T1 sequence shows high signal, T2-FS sequence shows low signal.
Patient’s perspective
After being diagnosed with SAPHO syndrome, I felt a sense of relief, as if I would finally get better soon. I was certain this was the answer — the illness that had tormented me for so long and hadn’t improved despite so many medications had to be something rare.
Discussion
This article presents the first reported case of a postpartum patient with chronic lumbopelvic pain and lower limb pain ultimately diagnosed with SAPHO syndrome. Initial examinations by the patient’s physicians included blood cultures and NGS, in order to rule out infectious inflammation. Results from NGS revealed Propionibacterium acnes infection. In March 2024, the patient developed palmoplantar pustulosis. However, these manifestations were overlooked in the early stages, thereby delaying the diagnosis.
The etiology of postpartum LPP remains unclear, although mechanical stress on the sacroiliac joints (SI), which is associated with axial spondyloarthritis (SpA), may be a contributing factor. Studies have shown that 59% of women meet ASAS-defined sacroiliitis criteria at 3 months postpartum, and 56% do so at 6 months, while in 41% of women, the criteria persist even at 12 months postpartum (4).
The pathogenesis of SAPHO syndrome remains uncertain. However, it may likely arise from complex interactions among immune dysregulation, genetic predisposition, and environmental factors (15). The pathological features of SAPHO syndrome are axial SpA-like changes affecting sacroiliac joints, spine, and enthesitis, and these symptoms are similar to those of postpartum LPP (16, 17). Approximately 62% of SAPHO patients exhibit spinal/sacroiliac involvement (16, 17), while 94% demonstrate sternoclavicular joint involvement (16). In the case reported here, although sternoclavicular pain was not the initial symptom, it emerged in the 6th postpartum month. Dermatologically, most SAPHO patients (91.9%) present with palmoplantar pustulosis, followed by severe acne (14.3%) and psoriasis vulgaris (15.8%) (18). Notably, cutaneous and osteoarticular manifestations may exhibit asynchronous timing: changes in the skin may be absent, precede, coincide with, or follow joint involvement (15). In the present case report, the patient’s overt palmoplantar pustulosis appeared later than osteoarticular pain.
While there is no current evidence linking pregnancy to SAPHO syndrome, the significant hormonal changes during pregnancy could theoretically trigger the condition, similar to flare-ups seen in other autoimmune diseases (such as systemic lupus erythematosus or multiple sclerosis) (19, 20). Diagnosis remains challenging without specific biomarkers, but SAPHO should be considered when inflammatory arthritis or osteitis (especially in the anterior chest wall, sacroiliac joints, or spine) coexists with psoriasis or neutrophilic/acne-like skin lesions. For diagnosing SAPHO syndrome, the diagnostic criteria proposed by Kahn et al. (5, 10, 21) may serve as a reference, although these criteria have not yet been validated.
Tofacitinib is an inhibitor of JAK1 and JAK3. By inhibiting JAK3, it blocks the expressions of IL-2, IL-4, IL-6, IL-7, IL-9, IL-15, and IL-21, and through JAK1 inhibition, it suppresses IL-6, type 1 interferons, and interferon-γ (22). Several studies have demonstrated the effectiveness of tofacitinib in alleviating the debilitations associated with SAPHO syndrome (11–14). Notably, Li et al. treated 13 SAPHO patients and observed significant reductions in the visual analog scale score for overall osteoarticular pain in the 8th week, as well as marked improvements in the Nail Psoriasis Severity Index score in the 12th week (12). In this case report, the patient showed a significant reduction in joint pain and skin damage after receiving a combination treatment of tofacitinib and etaecoxib for 3 months, which is similar to the treatment duration reported in previous study (12). Slightly different, compared to receiving tofacitinib alone, patients showed a significant reduction in joint pain by the fourth week, while skin damage completely disappeared by the twelfth week.
Limitations
This study involves only a single patient. Whether pregnancy can trigger SAPHO syndrome, and whether the combination of tofacitinib and etoricoxib is effective in treating postpartum SAPHO, still require long-term follow-up or validation through larger cohort studies.
Conclusion
Part of the aim of this study was to highlight the diagnostic challenges associated with SAPHO. Clinically, SAPHO syndrome patients with low back pain or sternoclavicular joint pain often present with palmoplantar pustulosis. However, in the early stages, palmoplantar scaling may be subtle or overlooked, thereby complicating accurate diagnosis. Furthermore, if the SAPHO patient is a postpartum woman, the presence of LPP symptoms further obscures the correct diagnosis of SAPHO syndrome.
In summary, this case report reminds us that LPP in postpartum women may not necessarily be pregnancy-related. Therefore, it is advised that, for postpartum patients with concurrent palmoplantar scaling and recurrent LPP unresponsive to treatment, clinicians should consider SAPHO syndrome as a potential diagnosis.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Affiliated Hospital of Medical School, Jinling Hospital, Nanjing University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
ZW: Writing – original draft, Project administration, Methodology, Supervision, Data curation, Investigation, Writing – review & editing. ZJ: Writing – review & editing, Data curation, Investigation, Methodology. ZR: Investigation, Data curation, Funding acquisition, Writing – review & editing, Project administration.
Funding
The author(s) declare that no financial support was received for the research, and/or publication of this article.
Acknowledgments
The authors thank the patient who agreed to be included in this report for her cooperation and support for academic communication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wu WH, Meijer OG, Uegaki K, Mens JM, van Dieën JH, Wuisman PI, et al. Pregnancy-related pelvic girdle pain (PPP), I: Terminology, clinical presentation, and prevalence. Eur Spine J. (2004) 13:575–89. doi: 10.1007/s00586-003-0615-y
2. Tavares P, Barrett J, Hogg-Johnson S, Ho S, Corso M, Batley S, et al. Prevalence of low back pain, pelvic girdle pain, and combination pain in a postpartum ontario population. J Obstet Gynaecol Can. (2020) 42:473–80. doi: 10.1016/j.jogc.2019.08.030
3. Elden H, Gutke A, Kjellby-Wendt G, Fagevik-Olsen M, and Ostgaard HC. Predictors and consequences of long-term pregnancy-related pelvic girdle pain: a longitudinal follow-up study. BMC Musculoskelet Disord. (2016) 17:276. doi: 10.1186/s12891-016-1154-0
4. Kiil RM, Weber U, Loft AG, Maimburg RD, and Jurik AG. Evolution of magnetic resonance imaging lesions at the sacroiliac joints during and after pregnancy by serial magnetic resonance imaging from gestational week twenty to twelve months postpartum. Arthritis Rheumatol. (2023) 75:1166–75. doi: 10.1002/art.42457
5. Kahn MF and Khan MA. The SAPHO syndrome. Baillieres Clin Rheumatol. (1994) 8:333–62. doi: 10.1016/S0950-3579(94)80022-7
6. Okuno H, Watanuki M, Kuwahara Y, Sekiguchi A, Mori Y, Hitachi S, et al. Clinical features and radiological findings of 67 patients with SAPHO syndrome. Mod Rheumatol. (2018) 28:703–8. doi: 10.1080/14397595.2017.1372874
7. Witt M, Meier J, Hammitzsch A, Proft F, Schulze-Koops H, and Grunke M. Disease burden, disease manifestations and current treatment regimen of the SAPHO syndrome in Germany: results from a nationwide patient survey. Semin Arthritis Rheumatol. (2014) 43:745–50. doi: 10.1016/j.semarthrit.2013.10.010
8. Ha DE, Revaux A, Ait Hammou F, Westerman MN, and Colau JC. A pregnant woman with a SAPHO syndrome. Gynecol Obstet Fertil. (2006) 34:1151–3. doi: 10.1016/j.gyobfe.2006.10.013
9. Pons JC, Nekhlyudov L, and Delfraissy JF. The course of the SAPHO syndrome during pregnancy. Eur J Obstet Gynecol Reprod Biol. (1996) 70:215–6. doi: 10.1016/S0301-2115(95)02588-X
10. Kahn ME. Abstracts of the American College of Rheumatology 67th annual meeting and the Association of Rheumatology Health Professionals 38th annual meeting. October 23-28, 2003. Orlando, Florida, USA. Arthritis Rheumatol. (2003) 48:S35–750.
11. Li Y, Huo J, Cao Y, Yu M, Zhang Y, Li Z, et al. Efficacy of tofacitinib in synovitis, acne, pustulosis, hyperostosis and osteitis syndrome: a pilot study with clinical and MRI evaluation. Ann Rheum Dis. (2020) 79:1255–7. doi: 10.1136/annrheumdis-2020-217250
12. Li C, Li Z, Cao Y, Li L, Li F, Li Y, et al. Tofacitinib for the treatment of nail lesions and palmoplantar pustulosis in synovitis, acne, pustulosis, hyperostosis, and osteitis syndrome. JAMA Dermatol. (2021) 157:74–8. doi: 10.1001/jamadermatol.2020.3095
13. Alhayali M. Successful treatment of refractory synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome with tofacitinib: A case report. Cureus. (2024) 16:e66169. doi: 10.7759/cureus.66169
14. Yuan F, Luo J, and Yang Q. SAPHO syndrome complicated by ankylosing spondylitis successfully treated with tofacitinib: A case report. Front Immunol. (2022) 13:911922. doi: 10.3389/fimmu.2022.911922
15. Ferraioli M, Levani J, De Luca R, Matucci-Cerinic C, Gattorno M, Guiducci S, et al. What is new and what is next for SAPHO syndrome management: A narrative review. J Clin Med. (2025) 14. doi: 10.3390/jcm14041366
16. Li C, Xu H, Gong L, Wang A, Dong X, Yuan K, et al. Work productivity and activity in patients with SAPHO syndrome: a cross-sectional observational study. Orphanet J Rare Dis. (2022) 17:381. doi: 10.1186/s13023-022-02523-2
17. Yap FHX, Olsson-White D, Roddy J, Cook NJ, Langlands DR, Manners PJ, et al. Long-term clinical outcomes in synovitis, acne, pustulosis, hyperostosis, and osteitis syndrome. Mayo Clin Proc Innov Qual Outcomes. (2021) 5:574–82. doi: 10.1016/j.mayocpiqo.2021.02.009
18. Cao Y, Li C, Xu W, Wu X, Sun X, Zhang W, et al. Spinal and sacroiliac involvement in SAPHO syndrome: A single center study of a cohort of 354 patients. Semin Arthritis Rheumatol. (2019) 48:990–6. doi: 10.1016/j.semarthrit.2018.09.004
19. Khamashta MA, Ruiz-Irastorza G, and Hughes GR. Systemic lupus erythematosus flares during pregnancy. Rheum Dis Clin North Am. (1997) 23:15–30. doi: 10.1016/S0889-857X(05)70312-4
20. Schubert C, Steinberg L, Peper J, Ramien C, Hellwig K, Köpke S, et al. Postpartum relapse risk in multiple sclerosis: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. (2023) 94:718–25. doi: 10.1136/jnnp-2022-330533
21. Benhamou C, Chamot AM, and Kahn MF. Synovitis-acne-pustulosis-hyperostosis-osteitis (SAPHO) syndrome. Ann Dermatol Venereol. (1988) 115:613–8.
Keywords: synovitis-acne-pustulosis-hyperostosis-osteitis, SAPHO, lumbopelvic pain, pelvic girdle pain, postpartum women
Citation: Weiwei Z, Junhong Z and Rong Z (2025) Postpartum lumbopelvic pain could be SAPHO syndrome: a case report. Front. Immunol. 16:1614945. doi: 10.3389/fimmu.2025.1614945
Received: 23 April 2025; Accepted: 28 July 2025;
Published: 13 August 2025.
Edited by:
Yuanpei Cheng, Jilin University, ChinaReviewed by:
Zhangyu Bu, Hangzhou First People’s Hospital, ChinaJuan Frías-Ordoñez, National University of Colombia, Colombia
Mustafa Alhayali, Ibn Sina University for Medical and Pharmaceutical Sciences, Iraq
Copyright © 2025 Weiwei, Junhong and Rong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhang Rong, MTM4NTE5ODEyNDBAMTYzLmNvbQ==
 Zheng Weiwei1
Zheng Weiwei1 Zhang Rong
Zhang Rong