- 1The First Affiliated Hospital of Zhejiang Chinese Medical University (Zhejiang Provincial Hospital of Chinese Medicine), Hangzhou, Zhejiang, China
- 2State Key Laboratory of Systems Medicine for Cancer, Shanghai Cancer Institute, Renji Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
Liver cancer is a major global health burden, with hepatocellular carcinoma (HCC) being the most common type. Liver cancer tumor-initiating cells (TICs) are responsible for recurrence, metastasis, and therapeutic resistance, thereby presenting formidable treatment challenges. This review provides a comprehensive summary of the biological features of liver cancer TICs, including their potential cellular origins, diagnostic difficulties, key signaling pathways, and complex interactions with the tumor immune microenvironment. Special emphasis is placed on immunotherapeutic strategies, which have shown notable progress but remain limited by TIC-induced immune resistance. The review discusses current approaches such as immune checkpoint inhibitors (ICIs), adoptive cell therapies, and tumor vaccines, as well as combination strategies integrating immunotherapy with chemotherapy, targeted therapy, and locoregional interventions. Furthermore, emerging strategies including gene editing, targeted tyrosine kinase inhibition, and artificial intelligence-based tumor prediction are being explored for their potential to improve therapeutic efficacy. The significance of this review lies in highlighting the importance of surmounting the challenges presented by TICs to boost the efficacy of liver cancer treatment. In conclusion, although existing treatment approaches have demonstrated promise, further research is warranted to elucidate the origins of TICs, establish accurate diagnostic methods, and overcome resistance, ultimately enhancing the efficacy of liver cancer treatment and improving patient outcomes.
1 Introduction
Liver cancer poses a significant global health burden, ranking as the sixth most common cancer and the fourth leading cause of cancer-related deaths worldwide, with hepatocellular carcinoma (HCC) accounting for approximately 90% of cases (1, 2). Despite advancements in diagnosis and treatment, the five-year survival rate for liver cancer remains suboptimal, primarily due to high rates of recurrence, metastasis, and therapeutic resistance (3–5).
Tumor-initiating cells (TICs) in liver cancer, a subpopulation within tumors, contribute to these therapeutic challenges owing to their self-renewal capacity, high plasticity, and tumorigenic potential (6, 7). These cells exhibit distinct molecular signatures, including the expression of surface markers such as CD133 and EpCAM, and they mediate dysregulated signaling pathways such as Wnt/β-catenin and Sonic Hedgehog (SHH) (8–10). Furthermore, interactions between liver cancer TICs and the tumor microenvironment (TME)—particularly through metabolic crosstalk with cancer-associated fibroblasts (CAFs) and immunosuppressive functions mediated by immune cells—establish a complex niche that significantly complicates therapeutic interventions (11, 12).
Immunotherapy is a breakthrough treatment for Liver cancer TICs. However, the heterogeneity and adaptive resistance mechanisms of Liver cancer TICs limit their efficacy (13, 14). To overcome these obstacles, current therapeutic strategies employ combination therapies, such as atezolizumab and bevacizumab, to enhance treatment response rates (15). Despite progress, debates continue regarding the cellular origins of liver cancer TICs and their role in tumor heterogeneity, highlighting the need for further research to better understand their biological and clinical significance (16).
This review explores the role of TICs in liver cancer, current diagnostic techniques, and therapeutic strategies, while also discussing emerging technologies and future perspectives, particularly in immunotherapy, to enhance liver cancer treatment.
2 Controversies and challenges in liver cancer TICs research
2.1 Contested origins of liver cancer TICs
The origin of liver cancer TICs remains debated. One prominent hypothesis suggests that TICs may stem from hepatic progenitor cells (HPCs). Specifically, CD34+ HPCs, essential for liver regeneration, have been proposed as a potential source of liver cancer stem cells (LCSCs). In a study by Park et al., CD34+ cells isolated from the PLC/PRF/5 hepatoma cell line were found to function as TICs, capable of generating HCC, cholangiocarcinoma (CC), and combined hepatocellular cholangiocarcinoma (CHC) in immunodeficient mice (17). These cells expressed both hepatic and hematopoietic markers, suggesting they might result from the fusion of hepatobiliary stem cells and myeloid precursors. This fusion likely provides tumor cells with cross-lineage characteristics, which contribute to tumor heterogeneity and malignant progression (18). Moreover, subpopulations of TICs that express specific surface antigens like CD133, CD44, and CD90 show distinct tumorigenic potentials, further contributing to the histological diversity observed in liver cancers (17).
An alternative theory involves the plasticity of mature hepatocytes. Evidence indicates that mature hepatocytes can serve as the origin of intrahepatic cholangiocarcinoma (ICC) cells. Mesencephalic astrocyte-derived neurotrophic factor (MANF), upregulated in ICC, promotes the transformation of mature hepatocytes into ICC cells via its interaction with CK19 and activation of the Notch signaling pathway (19). Furthermore, hepatocytes have the potential to transform directly into cancer cells following sequential genomic damage and dedifferentiate into precursor cells expressing progenitor cell markers (20).
2.2 Challenges in diagnosing liver cancer TICs
The diagnosis of liver cancer TICs is fraught with challenges, primarily stemming from the lack of specific biomarkers. While markers such as CD133, EpCAM, and certain lncRNAs have been associated with liver TICs, their diagnostic accuracy remains constrained due to non-exclusive expression in other liver or tumor microenvironment cell types, which can lead to false positives or negatives (21). Compounding this issue is the complexity of the TME, where immunosuppressive factors—including immune cell infiltration, stromal components, and secreted molecules—can modify biomarker expression and compromise detection accuracy (22, 23). Additionally, the spatial and temporal heterogeneity of liver tumors, characterized by variations in genetic mutations, epigenetic changes, and cellular composition across different tumor regions, further hinders the development of universal diagnostic methods (24, 25). Clinically, the difficulty of early-stage detection in primary liver cancer, coupled with limited treatment options, exacerbates the challenge of identifying TICs at actionable stages. Classic biomarkers like AFP and des-gamma-carboxy prothrombin (DCP) exhibit low sensitivity and specificity for early detection (26), while newer biomarkers identified through proteomic, metabolomic, and genomic analyses hold promise but require validation for routine clinical use (27).
2.3 Resistance mechanisms of liver cancer TICs to therapy
Therapeutic resistance poses a significant obstacle in managing liver TICs. A key example is the response of TICs to sorafenib, a first-line treatment for advanced hepatocellular carcinoma. While sorafenib initially suppresses the proliferation of certain HCC cell lines, it paradoxically causes a transient expansion of TIC populations. These TICs activate the YAP signaling pathway, a potent oncogenic transcriptional coactivator that enhances tumor cell survival, proliferation, and invasion (28). Resistant TICs display increased sphere-forming ability, higher proportions of EpCAM-positive cells, and upregulated YAP expression (29), all of which are associated with stemness and aggressive tumor behavior. Notably, combining sorafenib with a YAP inhibitor has shown synergistic anti-tumor effects, suggesting potential for dual pathway inhibition.
Epigenetic reprogramming also contributes to TIC-mediated resistance. In sorafenib-resistant HCC, EZH2 overexpression enhances NOTCH1 signaling through H3K27me3-mediated chromatin modifications, supporting TIC self-renewal and tumorigenicity (30). Inhibiting EZH2 can restore sorafenib sensitivity by suppressing NOTCH1 and weakening TIC properties, offering a promising strategy to overcome resistance.
3 Role and molecular pathways of TICs in liver cancer pathogenesis
3.1 Molecular mechanisms underpinning stemness and progression of liver cancer TICs
Liver cancer TICs rely on multiple molecular pathways to sustain their stemness and drive liver Cancer progression. A crucial pathway in this process is the Wnt/β-catenin pathway. For instance, LncTIC1 interacts with the N-terminal of β-catenin, inhibiting its phosphorylation and stabilizing the protein to activate Wnt/β-catenin signaling, thereby promoting TIC self-renewal and tumorigenesis (9). Similarly, TFAP4 amplifies this signaling cascade by directly binding to the promoters of DVL1 and LEF1, further reinforcing TIC characteristics (31). Additionally, activation of the Wnt/β-catenin pathway promotes M2 polarization of tumor-associated macrophages (TAMs), which facilitate immune evasion by secreting immunosuppressive cytokines such as IL-10 and TGF-β (32). Another critical regulator of liver cancer TICs is the interleukin-8 (IL-8) signaling axis. CD133+ liver TICs exhibit significant dysregulation of this pathway, evidenced by genomic and proteomic overexpression of IL-8 (8). This aberrant expression promotes endothelial cell proliferation, tube formation, and TIC stemness maintenance. Mechanistically, NTS binding to NTSR1/2 on CD133+ TICs triggers MAPK phosphorylation, driving IL-8 and CXCL1 production. IL-8 then acts via CXCR1/2 in an autocrine/paracrine manner to sustain MAPK activation, forming a positive feedback loop (8).
Epigenetic regulation by non-coding RNAs further modulates TICs stemness and metastatic potential. For instance, the circular RNA cia-MAF binds to the MAFF promoter and recruits the TIP60 histone acetyltransferase complex, driving MAFF expression which is a transcription factor critical for TIC self-renewal and metastasis. Likewise, the long non-coding RNA lncHOXA10 interacts with SNF2L and recruits the NURF chromatin remodeling complex to the HOXA10 promoter in liver cancer TICs, contributing to HOXA10 expression and liver cancer progression (33). These epigenetic mechanisms also synergize with canonical signaling pathways. For example, SHH signaling, activated by the PARD3-aPKC interaction, upregulates stemness genes such as SOX2 and correlates with advanced tumor stages (10) (Figure 1).
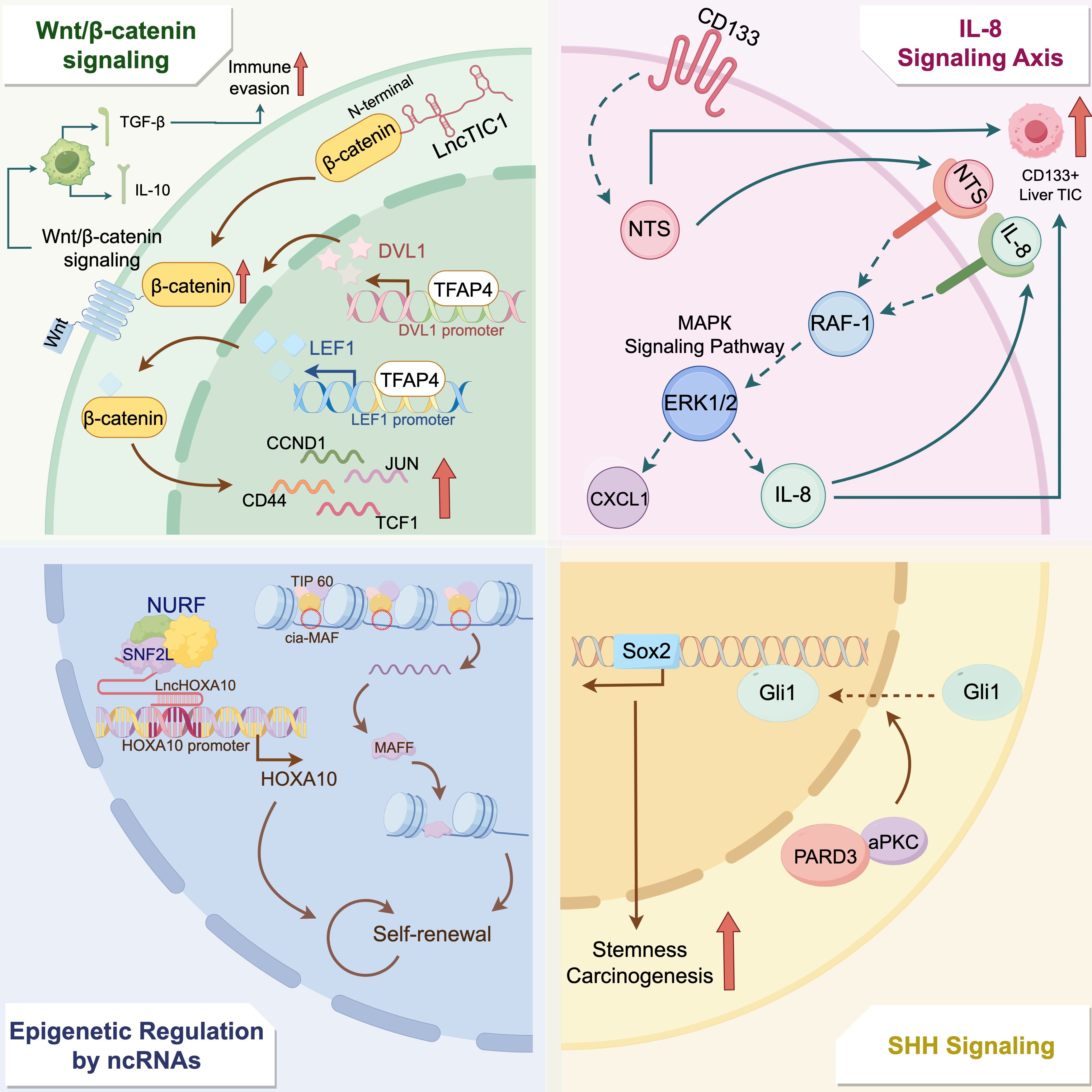
Figure 1. Molecular mechanisms regulating liver cancer tumor-initiating cells stemness and tumor progression. This figure illustrates the intricate molecular pathways that regulate the stemness and tumorigenic potential of liver cancer tumor-initiating cells (TICs). The interaction between LncTIC1 and β-catenin increases the stability of β-catenin, thereby activating the Wnt/β-catenin pathway. TFAP4 binds to the promoters of DVL1 and LEF1, further enhancing β-catenin stability and activating the expression of downstream genes such as CCND1, CD44, JUN, and TCF1. Additionally, this pathway promotes M2 macrophage polarization, facilitating immune evasion through the secretion of IL-10 and TGF-β. The IL-8 signaling axis, dysregulated in CD133+ liver TICs, contributes to TIC stemness by enhancing MAPK signaling and forming a positive feedback loop via IL-8 and CXCL1. Moreover, epigenetic regulation by non-coding RNAs, such as cia-MAF and lncHOXA10, modulates TIC self-renewal. Circular RNA cia-MAF binds to the MAFF promoter and recruits the TIP60 histone acetyltransferase complex, driving MAFF expression, while the long non-coding RNA lncHOXA10 interacts with SNF2L and recruits the NURF chromatin remodeling complex to the HOXA10 promoter in liver cancer TICs. Finally, SHH signaling, mediated by the PARD3-aPKC interaction, contributes to the upregulation of stemness genes such as SOX2, which correlates with increased stemness and carcinogenesis.
3.2 TICs-TME crosstalk in liver cancer progression
The TME, which consists of a variety of non-cancerous cells, extracellular matrix components, and soluble factors, plays a critical role in influencing the behavior of liver cancer TICs. A case in point is CAFs, key stromal cells in the TME, interact with TICs to promote tumor progression. In a three-dimensional (3D) co-culture organoid model of primary murine liver tumors, the presence of CAFs significantly increased the number of LGR5+ TICs in the tumor compared to organoids lacking CAFs. This observation suggests that CAFs support LGR5+ liver cancer TICs, facilitating tumor formation, growth, and metastasis (34). Additionally, CAFs can enhance the stemness of TICs by secreting cytokines such as interleukin-6 (IL-6), which activate signaling pathways like IL-6-STAT3-NOTCH, thereby promoting tumor progression (35).
TICs interact with immune cells within the TME to establish an immunosuppressive milieu. Specifically, TREM2 macrophages are associated with glycolysis and PKM2 expression in HCC cells, likely mediated by the secretion of IL-1β, which promotes malignant phenotypes of HCC cells (36). Meanwhile, CD49f-high TICs recruit tumor-promoting neutrophils through the CXCL2-CXCR2 axis, establishing an immunosuppressive environment within the TME (12). This crosstalk between TICs and immune cells highlights the intricate tumor-immune microenvironment and holds important implications for the development of effective immunotherapy strategies (37).
4 Therapeutic strategies targeting liver cancer TICs
4.1 Immunotherapy approaches for liver cancer TICs
Immunotherapy is a promising therapeutic approach for liver cancer TICs. Among various immunotherapeutic agents, immune checkpoint inhibitors (ICIs) are a prominent class. In the treatment of HCC, the combination of the anti-programmed cell death ligand 1 (PD-L1) antibody atezolizumab and the VEGF-neutralizing antibody bevacizumab has demonstrated significant efficacy. Consequently, this regimen is now recommended as the first-line systemic therapy for advanced HCC (15). Additionally, combining different ICIs, like nivolumab and ipilimumab, has yielded promising outcomes in second-line treatments, as evidenced by the CheckMate 040 study (38). Nevertheless, ICI monotherapy demonstrates limited efficacy in HCC, with objective response rates of 10–20% and no significant overall survival (OS) improvement observed in phase III clinical trials such as CheckMate 459 and KEYNOTE-240 (39).
Adoptive cell therapy (ACT) and peptide- or dendritic cell (DC)-based vaccines are also under active investigation. ACT, including chimeric antigen receptor T-cell (CAR-T) therapy targeting tumor-associated antigens (TAA) like glypican-3 (GPC3) and alpha-fetoprotein (AFP), has demonstrated encouraging results in early-phase clinical trials by specifically recognizing and eliminating tumor cells without MHC restriction (40).
Peptide-based vaccines, exemplified by GPC3-targeted formulations, induce cytotoxic T lymphocyte (CTL) infiltration into tumors and can improve overall survival in HCC patients (41). Similarly, DC vaccines targeting tumor antigens or neoantigens help remodel the immunosuppressive TME, by activating tumor-reactive T cells, showing good safety and immunogenicity profiles in early trials (42, 43). However, the liver’s unique immune microenvironment limits immune cell infiltration and function, reducing the effectiveness of these therapies. Therefore, identifying predictive biomarkers for immunotherapy response remains crucial.
4.2 Combination therapies for liver cancer TICs
4.2.1 Synergizing immunotherapy with chemotherapy
Cytotoxic chemotherapy, when combined with ICIs, has demonstrated improved antitumor efficacy against liver cancer TICs. Recent clinical studies have shown that the FOLFOX regimen combined with immunotherapy achieves an objective response rate of approximately 60%, with around 25% of patients successfully converted to surgical candidates (44). Conjugates linking irinotecan with TDO inhibitors demonstrated enhanced cellular uptake and cytotoxicity in TDO-overexpressing HepG2 cells, induced G2 phase arrest and mitochondrial apoptosis, and inhibited kynurenine production and aryl hydrocarbon receptor signaling, thereby promoting T cell activation (45).
4.2.2 Synergizing immunotherapy with targeted agents
The combination of immunotherapy and molecular-targeted therapies is actively being explored. For instance, combining PD-1 blockade with pegylated interferon-α (Peg-IFNα) has been shown to increase cytotoxic CD8+ T-cell infiltration, restore anti-tumor immunity, promote tumor cell apoptosis, and reduce angiogenesis in HCC models (46). Another study by Hsieh et al. demonstrated that the combination of bavituximab and pembrolizumab increased the response rate in HCC patients from 16% to 32%, highlighting the potential of combination therapies (47).
4.2.3 Combining systemic immunotherapy with locoregional therapies
Locoregional therapies combined with systemic immunotherapy represent a promising strategy for targeting liver cancer TICs. One innovative approach, transcatheter arterial chemo-immuno-embolization (TACIE), integrates transcatheter arterial chemoembolization (TACE) with immune adjuvants like TLR9 agonists. This combination has exhibited synergistic antitumor effects in preclinical models by enhancing systemic immunity and promoting tumor regression, while maintaining safety (48). This method has shifted treatment strategies from “total embolization,” aimed at complete tumor necrosis, to “partial embolization,” which reduces tumor burden while preserving liver function. It also provides an immune boost that enhances the effects of immunotherapy and targeted agents (49).
In addition, radiofrequency ablation (RFA) combined with ICIs can boost systemic immune activation via neoantigen release and abscopal effects (50). Stereotactic body radiation therapy (SBRT), in conjunction with ICIs, is also being explored to target oligometastases and improve rates of radical cure (51) (Table 1).
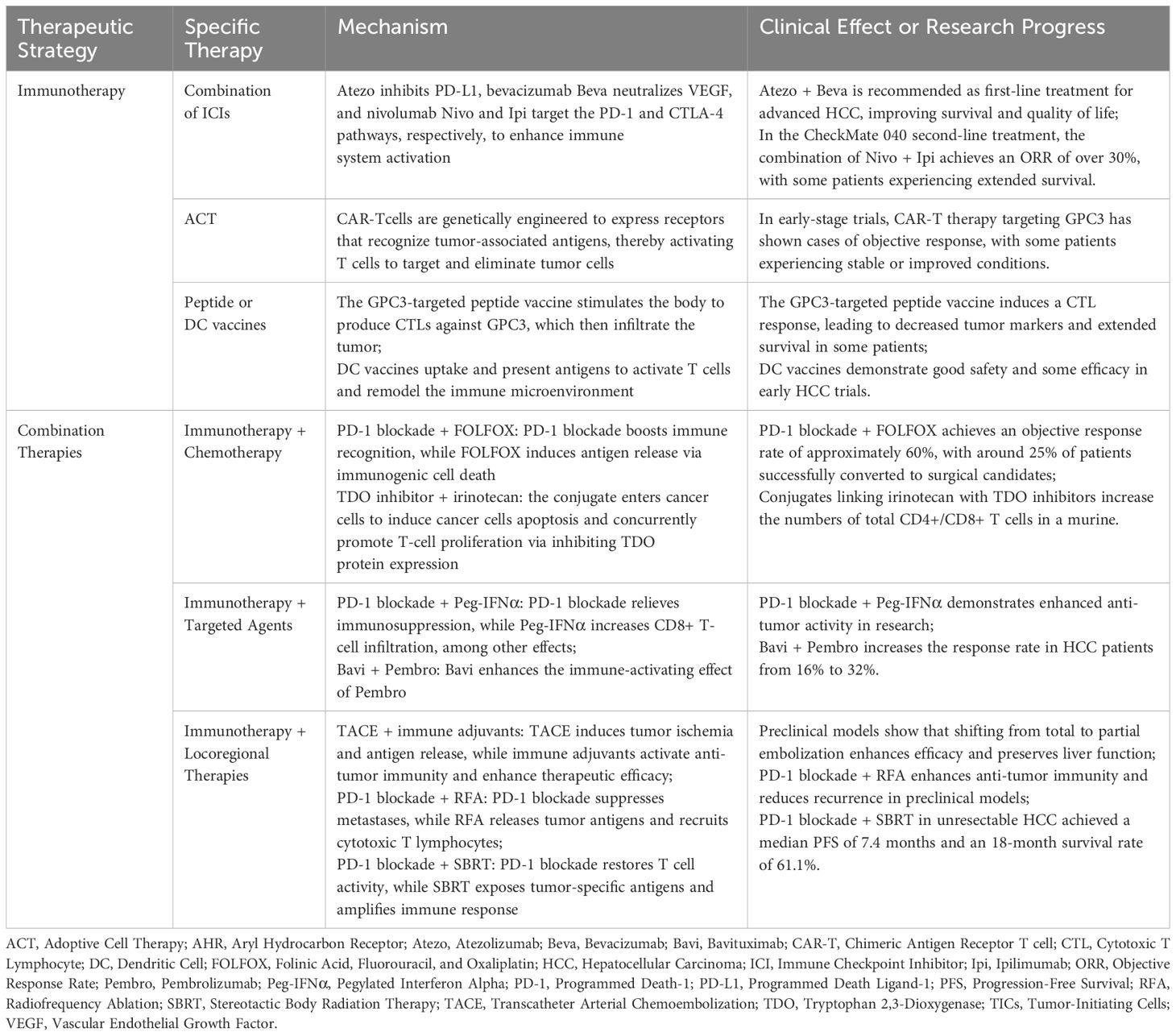
Table 1. Immunotherapeutic approaches and combinatorial strategies targeting liver cancer tumor-initiating cells.
4.3 Emerging therapeutic strategies for liver cancer TICs
Multiple therapeutic strategies are being developed to address the challenges posed by liver cancer TICs. The Wnt/β-catenin pathway is crucial in liver cancer, and 6-C-(E-phenylethenyl) naringenin (6-CEPN) inhibits TIC self-renewal, migration, and invasion by activating GSK3β, leading to the degradation and suppression of the Wnt/β-catenin pathway (52). In addition, selective tyrosine kinase inhibitors, such as Indo5, target the c-Met and Trk receptor tyrosine kinases, which are frequently co-activated in HCC and associated with poor prognosis (53). By blocking these pathways, Indo5 disrupts the related signaling and suppresses tumor growth. Equally important, Bio-SS-TS, a compound combining biotin and taraxasterol (TS), exploits the overexpression of biotin receptors on tumor cells for targeted delivery (54). It enhances mitochondria-dependent apoptosis and inhibits tumor development.
In parallel, genome editing also holds great promise in targeting liver cancer TICs. Marayati et al. used CRISPR/Cas9 to knockout PIM3 in hepatoblastoma cells, leading to reduced cell proliferation, viability, and stemness (55). Regarding non-coding RNAs, they are emerging as crucial therapeutic targets. Li et al. engineered an artificially designed lncRNA that functions as a molecular sponge, sequestering multiple oncogenic miRNAs and inhibiting tumor growth in xenograft HCC mouse models (56). Yao et al. demonstrated that miR-186 suppresses the expansion of liver CSCs by targeting PTPN11 (57). These advances suggest promising avenues for personalized TIC-targeted therapies.
4.4 Emerging therapeutic strategies for liver cancer TICs
Overcoming the liver’s immunosuppressive microenvironment is a key area for future research. Recent studies have identified several mechanisms by which TICs facilitate immune suppression and resistance (58). The overexpression of CD155 on TICs interacts with immune checkpoint receptors, leading to T cell exhaustion. Combining CD155 blockade with anti-PD-1/PD-L1 therapy has shown enhanced anti-tumor responses in preclinical models (12).
Additionally, a unique subset of TAMs expressing CD19 has been discovered in HCC. CD19+ TAMs exhibit immunosuppressive functions by upregulating PD-L1 and CD73, thereby inhibiting T cell activity, and direct targeting with anti-CD19 CAR-T cells has been shown to suppress tumor growth (59).
The immunosuppressive TME in HCC is further characterized by diverse immune cell populations and signaling pathways that impede effective immune responses (7). Strategies to overcome this include the use of inhibitors targeting the TGF-β/IL-10 pathway and metabolic modulators to enhance immune activation (60, 61). Moreover, accurately assessing and predicting tumor responses to immunotherapy remain critical challenges. Artificial intelligence (AI) integrating imaging, pathology, genomics, and clinical data show promise in predicting treatment responses and survival outcomes in HCC patients undergoing immunotherapy (62). Furthermore, MRI-based response criteria, particularly 3D quantitative enhancement tools (qEASL), have significant potential for predicting overall survival and identifying non-responders (63).
5 Conclusion
Liver cancer remains a major global health challenge, largely driven by TICs, characterized by robust self-renewal capabilities, plasticity, and immunosuppressive properties. These TICs actively remodel the TME employing mechanisms such as the overexpression of immune checkpoint molecules like CD155, recruitment of immunosuppressive macrophages including CD19-positive TAMs, and regulation of metabolic and cytokine pathways such as TGF-β and IL-10, collectively enabling immune evasion and sustained therapeutic resistance. Consequently, despite advances in immunotherapy, the efficacy of ICIs, adoptive cell therapies, and tumor vaccines is constrained by these sophisticated TIC-mediated immune escape mechanisms.
Emerging therapeutic strategies aim to integrate multimodal approaches that comprehensively disrupt TIC-driven immune suppression and resistance. Combination therapies merging immunotherapy with cytotoxic chemotherapy, molecular-targeted agents, and locoregional interventions such as TACE and RFA have shown clinical promise by enhancing antigen release, promoting immune cell infiltration, and reversing immunosuppressive metabolic states. Cutting-edge technologies, including genome editing via CRISPR/Cas9 for targeting TIC-specific pathways, nanotechnology-enhanced drug delivery systems, and novel cellular therapies directed against immunosuppressive cell populations, offer substantial promise for refining treatment efficacy. Furthermore, advanced predictive models leveraging AI and integrating multi-omics and imaging data may significantly enhance patient stratification and optimize immunotherapeutic outcomes.
However, several critical scientific challenges remain unresolved in the context of TIC-directed immunotherapy. These include the precise identification of TIC subpopulations most responsible for immune evasion, the dynamic evolution of their phenotypes under therapeutic and immune pressure, and the absence of reliable biomarkers to predict treatment responsiveness. Furthermore, the molecular mechanisms underlying the crosstalk between TICs and immunosuppressive stromal components are not yet fully elucidated. Addressing these gaps is essential for future progress in liver cancer therapy, which hinges on acquiring deeper mechanistic insights into TIC biology, immune resistance dynamics, and the complex interactions between TICs and their microenvironment. An improved understanding of these networks will provide a foundation for the development of durable and personalized immunotherapeutic strategies, ultimately aiming to enhance clinical efficacy and improve patient outcomes.
Author contributions
YC: Writing – original draft, Writing – review & editing, Conceptualization, Data curation. TX: Writing – original draft, Writing – review & editing, Data curation. XC: Writing – review & editing, Supervision, Validation. BC: Writing – review & editing, Supervision. XD: Writing – original draft, Writing – review & editing. ZZ: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We thank the Figdraw online platform (https://www.figdraw.com/) for providing the tools used to create the figures in this manuscript and gratefully acknowledge the functionality and support it offers.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that Generative AI was used in the creation of this manuscript. The authors utilized ChatGPT-4.0 to assist with language refinement during the preparation of this work. All content was subsequently reviewed and revised by the authors, who take full responsibility for the final version of the publication.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sankar K, Gong J, Osipov A, Miles SA, Kosari K, Nissen NN, et al. Recent advances in the management of hepatocellular carcinoma. Clin Mol Hepatol. (2024) 30:1–15. doi: 10.3350/cmh.2023.0125
2. Llovet JM, Kelley RK, Villanueva A, Singal AG, Pikarsky E, Roayaie S, et al. Hepatocellular carcinoma. Nat Rev Dis Primers. (2021) 7:6. doi: 10.1038/s41572-020-00240-3
3. Llovet JM, Villanueva A, Marrero JA, Schwartz M, Meyer T, Galle PR, et al. Trial design and endpoints in hepatocellular carcinoma: AASLD consensus conference. Hepatology. (2021) 73 Suppl 1:158–91. doi: 10.1002/hep.31327
4. Ladd AD, Duarte S, Sahin I, and Zarrinpar A. Mechanisms of drug resistance in HCC. Hepatology. (2024) 79:926–40. doi: 10.1097/hep.0000000000000237
5. Guo Q, Zhu X, Beeraka NM, Zhao R, Li S, Li F, et al. Projected epidemiological trends and burden of liver cancer by 2040 based on GBD, CI5plus, and WHO data. Sci Rep. (2024) 14:28131. doi: 10.1038/s41598-024-77658-2
6. Qureshi-Baig K, Ullmann P, Haan S, and Letellier E. Tumor-Initiating Cells: a criTICal review of isolation approaches and new challenges in targeting strategies. Mol Cancer. (2017) 16:40. doi: 10.1186/s12943-017-0602-2
7. Huang H, Tsui YM, and Ng IO. Fueling HCC dynamics: interplay between tumor microenvironment and tumor initiating cells. Cell Mol Gastroenterol Hepatol. (2023) 15:1105–16. doi: 10.1016/j.jcmgh.2023.01.007
8. Tang KH, Ma S, Lee TK, Chan YP, Kwan PS, Tong CM, et al. CD133(+) liver tumor-initiating cells promote tumor angiogenesis, growth, and self-renewal through neurotensin/interleukin-8/CXCL1 signaling. Hepatology. (2012) 55:807–20. doi: 10.1002/hep.24739
9. Chen Z, Yao L, Liu Y, and Zhu P. LncTIC1 interacts with β-catenin to drive liver TIC self-renewal and liver tumorigenesis. Cancer Lett. (2018) 430:88–96. doi: 10.1016/j.canlet.2018.05.023
10. Wu J, Tan HY, Chan YT, Lu Y, Feng Z, Yuan H, et al. PARD3 drives tumorigenesis through activating Sonic Hedgehog signalling in tumour-initiating cells in liver cancer. J Exp Clin Cancer Res. (2024) 43:42. doi: 10.1186/s13046-024-02967-3
11. Yang H, Li J, Niu Y, Zhou T, Zhang P, Liu Y, et al. Interactions between the metabolic reprogramming of liver cancer and tumor microenvironment. Front Immunol. (2025) 16:1494788. doi: 10.3389/fimmu.2025.1494788
12. Yang C, Geng H, Yang X, Ji S, Liu Z, Feng H, et al. Targeting the immune privilege of tumor-initiating cells to enhance cancer immunotherapy. Cancer Cell. (2024) 42:2064–81.e19. doi: 10.1016/j.ccell.2024.10.008
13. Machida K and Tahara SM. Immunotherapy and microbiota for targeting of liver tumor-initiating stem-like cells. Cancers (Basel). (2022) 14:2381. doi: 10.3390/cancers14102381
14. Mei-Mei L, Yi-Ti H, Jie-Kai L, Xin-Yuan G, Ning-Fang M, and Ming L. Cancer stem cell-mediated therapeutic resistance in hepatocellular carcinoma. Hepatoma Res. (2022) 8:36. doi: 10.20517/2394-5079.2022.43
15. Ruff SM, Shannon AH, Beane JD, and Pawlik TM. Highlighting novel targets in immunotherapy for liver cancer. Expert Rev Gastroenterol Hepatol. (2022) 16:1029–41. doi: 10.1080/17474124.2022.2150841
16. Lee TK, Guan XY, and Ma S. Cancer stem cells in hepatocellular carcinoma - from origin to clinical implications. Nat Rev Gastroenterol Hepatol. (2022) 19:26–44. doi: 10.1038/s41575-021-00508-3
17. Park SC, Nguyen NT, Eun JR, Zhang Y, Jung YJ, Tschudy-Seney B, et al. Identification of cancer stem cell subpopulations of CD34(+) PLC/PRF/5 that result in three types of human liver carcinomas. Stem Cells Dev. (2015) 24:1008–21. doi: 10.1089/scd.2014.0405
18. Zeng C, Zhang Y, Park SC, Eun JR, Nguyen NT, Tschudy-Seney B, et al. CD34(+) liver cancer stem cells were formed by fusion of hepatobiliary stem/progenitor cells with hematopoietic precursor-derived myeloid intermediates. Stem Cells Dev. (2015) 24:2467–78. doi: 10.1089/scd.2015.0202
19. Mei Q, Zhang Y, Li H, Ma W, Huang W, Wu Z, et al. Hepatic factor MANF drives hepatocytes reprogramming by detaining cytosolic CK19 in intrahepatic cholangiocarcinoma. Cell Death Differ. (2025). doi: 10.1038/s41418-025-01460-4
20. Sia D, Villanueva A, Friedman SL, and Llovet JM. Liver cancer cell of origin, molecular class, and effects on patient prognosis. Gastroenterology. (2017) 152:745–61. doi: 10.1053/j.gastro.2016.11.048
21. Chan AW, Tong JH, Chan SL, Lai PB, and To KF. Expression of stemness markers (CD133 and EpCAM) in prognostication of hepatocellular carcinoma. Histopathology. (2014) 64:935–50. doi: 10.1111/his.12342
22. Lu C, Rong D, Zhang B, Zheng W, Wang X, Chen Z, et al. Current perspectives on the immunosuppressive tumor microenvironment in hepatocellular carcinoma: challenges and opportunities. Mol Cancer. (2019) 18:130. doi: 10.1186/s12943-019-1047-6
23. Sun F, Wang J, Sun Q, Li F, Gao H, Xu L, et al. Interleukin-8 promotes integrin β3 upregulation and cell invasion through PI3K/Akt pathway in hepatocellular carcinoma. J Exp Clin Cancer Res. (2019) 38:449. doi: 10.1186/s13046-019-1455-x
24. Yan J, Jiang Z, Zhang S, Yu Q, Lu Y, Miao R, et al. Spatial–temporal heterogeneities of liver cancer and the discovery of the invasive zone. Clin Transl Med. (2025) 15:e70224. doi: 10.1002/ctm2.70224
25. Wu L, Yan J, Bai Y, Chen F, Zou X, Xu J, et al. An invasive zone in human liver cancer identified by Stereo-seq promotes hepatocyte-tumor cell crosstalk, local immunosuppression and tumor progression. Cell Res. (2023) 33:585–603. doi: 10.1038/s41422-023-00831-1
26. Piñero F, Dirchwolf M, and Pessôa MG. Biomarkers in hepatocellular carcinoma: diagnosis, prognosis and treatment response assessment. Cells. (2020) 9:1370. doi: 10.3390/cells9061370
27. Yi H and Xu H. Novel biomarkers for hepatocellular carcinoma detection and treatment. Hepatobiliary Surg Nutr. (2024) 13:901–4. doi: 10.21037/hbsn-24-517
28. Morciano G, Vezzani B, Missiroli S, Boncompagni C, Pinton P, and Giorgi C. An updated understanding of the role of YAP in driving oncogenic responses. Cancers (Basel). (2021) 13:3100. doi: 10.3390/cancers13123100
29. Castven D, Czauderna C, Becker D, Pereira S, Schmitt J, Weinmann A, et al. Acquired resistance to antiangiogenic therapies in hepatocellular carcinoma is mediated by yes-associated protein 1 activation and transient expansion of stem-like cancer cells. Hepatol Commun. (2022) 6:1140–56. doi: 10.1002/hep4.1869
30. Wang S, Cai L, Zhang F, Shang X, Xiao R, and Zhou H. Inhibition of EZH2 attenuates sorafenib resistance by targeting NOTCH1 activation-dependent liver cancer stem cells via NOTCH1-related microRNAs in hepatocellular carcinoma. Transl Oncol. (2020) 13:100741. doi: 10.1016/j.tranon.2020.01.002
31. Song J, Xie C, Jiang L, Wu G, Zhu J, Zhang S, et al. Transcription factor AP-4 promotes tumorigenic capability and activates the Wnt/β-catenin pathway in hepatocellular carcinoma. Theranostics. (2018) 8:3571–83. doi: 10.7150/thno.25194
32. Yang Y, Ye YC, Chen Y, Zhao JL, Gao CC, Han H, et al. Crosstalk between hepatic tumor cells and macrophages via Wnt/β-catenin signaling promotes M2-like macrophage polarization and reinforces tumor Malignant behaviors. Cell Death Dis. (2018) 9:793. doi: 10.1038/s41419-018-0818-0
33. Shao M, Yang Q, Zhu W, Jin H, Wang J, Song J, et al. LncHOXA10 drives liver TICs self-renewal and tumorigenesis via HOXA10 transcription activation. Mol Cancer. (2018) 17:173. doi: 10.1186/s12943-018-0921-y
34. Zhang M, Fang Y, Fu X, Liu J, Liu Y, Zhu Z, et al. Cancer-associated fibroblasts nurture LGR5 marked liver tumor-initiating cells and promote their tumor formation, growth, and metastasis. Cancer Med. (2023) 12:18032–49. doi: 10.1002/cam4.6408
35. Xiong S, Wang R, Chen Q, Luo J, Wang J, Zhao Z, et al. Cancer-associated fibroblasts promote stem cell-like properties of hepatocellular carcinoma cells through IL-6/STAT3/Notch signaling. Am J Cancer Res. (2018) 8:302–16.
36. Guo H, Wang M, Ni C, Yang C, Fu C, Zhang X, et al. TREM2 promotes the formation of a tumor-supportive microenvironment in hepatocellular carcinoma. J Exp Clin Cancer Res. (2025) 44:20. doi: 10.1186/s13046-025-03287-w
37. Ma Y, Lv H, Xing F, Xiang W, Wu Z, Feng Q, et al. Cancer stem cell-immune cell crosstalk in the tumor microenvironment for liver cancer progression. Front Med. (2024) 18:430–45. doi: 10.1007/s11684-023-1049-z
38. Yau T, Kang YK, Kim TY, El-Khoueiry AB, Santoro A, Sangro B, et al. Efficacy and safety of nivolumab plus ipilimumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib: the checkMate 040 randomized clinical trial. JAMA Oncol. (2020) 6:e204564. doi: 10.1001/jamaoncol.2020.4564
39. Kudo M. Limited impact of anti-PD-1/PD-L1 monotherapy for hepatocellular carcinoma. Liver Cancer. (2020) 9:629–39. doi: 10.1159/000512170
40. Rochigneux P, Chanez B, De Rauglaudre B, Mitry E, Chabannon C, and Gilabert M. Adoptive cell therapy in hepatocellular carcinoma: biological rationale and first results in early phase clinical trials. Cancers (Basel). (2021) 13:271. doi: 10.3390/cancers13020271
41. Sawada Y, Yoshikawa T, Nobuoka D, Shirakawa H, Kuronuma T, Motomura Y, et al. Phase I trial of a glypican-3-derived peptide vaccine for advanced hepatocellular carcinoma: immunologic evidence and potential for improving overall survival. Clin Cancer Res. (2012) 18:3686–96. doi: 10.1158/1078-0432.Ccr-11-3044
42. Hassan M, Nasr SM, Amin NA, El-Ahwany E, Zoheiry M, and Elzallat M. Circulating liver cancer stem cells and their stemness-associated MicroRNAs as diagnostic and prognostic biomarkers for viral hepatitis-induced liver cirrhosis and hepatocellular carcinoma. Noncoding RNA Res. (2023) 8:155–63. doi: 10.1016/j.ncrna.2022.12.006
43. Lee JH, Lee Y, Lee M, Heo MK, Song JS, Kim KH, et al. A phase I/IIa study of adjuvant immunotherapy with tumour antigen-pulsed dendritic cells in patients with hepatocellular carcinoma. Br J Cancer. (2015) 113:1666–76. doi: 10.1038/bjc.2015.430
44. Lu YC, Yang YC, Ma D, Wang JQ, Hao FJ, Chen XX, et al. FOLFOX-HAIC combined with targeted immunotherapy for initially unresectable hepatocellular carcinoma: a real-world study. Front Immunol. (2024) 15:1471017. doi: 10.3389/fimmu.2024.1471017
45. Liu Q, Hua S, Wang X, Chen F, and Gou S. The introduction of immunosuppressor (TDO inhibitor) significantly improved the efficacy of irinotecan in treating hepatocellular carcinoma. Cancer Immunol Immunother. (2021) 70:497–508. doi: 10.1007/s00262-020-02697-3
46. Zhu Y, Chen M, Xu D, Li TE, Zhang Z, Li JH, et al. The combination of PD-1 blockade with interferon-α has a synergistic effect on hepatocellular carcinoma. Cell Mol Immunol. (2022) 19:726–37. doi: 10.1038/s41423-022-00848-3
47. Hsiehchen D, Beg MS, Kainthla R, Lohrey J, Kazmi SM, Khosama L, et al. The phosphatidylserine targeting antibody bavituximab plus pembrolizumab in unresectable hepatocellular carcinoma: a phase 2 trial. Nat Commun. (2024) 15:2178. doi: 10.1038/s41467-024-46542-y
48. Kim H, Choi B, Mouli SK, Choi H, Harris KR, Kulik LM, et al. Preclinical development and validation of translational temperature sensitive iodized oil emulsion mediated transcatheter arterial chemo-immuno-embolization for the treatment of hepatocellular carcinoma. Adv Healthc Mater. (2023) 12:e2300906. doi: 10.1002/adhm.202300906
49. Kudo M. A Changing Role of Transarterial Chemoembolization in the Era of Immune Checkpoint Inhibitor plus Anti-VEGF/TKI plus Transarterial Chemoembolization: From Total Embolization to Partial Embolization (Immune Boost Transarterial Chemoembolization). Liver Cancer. (2024) 13:335–43. doi: 10.1159/000539301
50. Kudo M. Combination cancer immunotherapy in hepatocellular carcinoma. Liver Cancer. (2018) 7:20–7. doi: 10.1159/000486487
51. Chen Y, Hong H, Fang W, Zhang X, Luo H, Chen Z, et al. Toripalimab in combination with Anlotinib for unresectable hepatocellular carcinoma after SBRT: A prospective, single-arm, single-center clinical study. Front Oncol. (2023) 13:1113389. doi: 10.3389/fonc.2023.1113389
52. Kang Q, Gong J, Wang M, Wang Q, Chen F, and Cheng KW. Correction to 6-C-(E-phenylethenyl)Naringenin attenuates the stemness of hepatocellular carcinoma cells by suppressing wnt/β-catenin signaling. J Agric Food Chem. (2020) 68:1505. doi: 10.1021/acs.jafc.0c00226
53. Luo T, Zhang SG, Zhu LF, Zhang FX, Li W, Zhao K, et al. A selective c-Met and Trks inhibitor Indo5 suppresses hepatocellular carcinoma growth. J Exp Clin Cancer Res. (2019) 38:130. doi: 10.1186/s13046-019-1104-4
54. Li J, Qin Y, Li M, Shang J, Chen H, Liu Y, et al. Bio-SS-TS as a targeted antitumor drug exerts an anti-liver cancer effect by enhancing mitochondria-dependent apoptosis. Biol Proced Online. (2025) 27:11. doi: 10.1186/s12575-025-00272-7
55. Marayati R, Stafman LL, Williams AP, Bownes LV, Quinn CH, Markert HR, et al. CRISPR/Cas9-mediated knockout of PIM3 suppresses tumorigenesis and cancer cell stemness in human hepatoblastoma cells. Cancer Gene Ther. (2022) 29:558–72. doi: 10.1038/s41417-021-00334-4
56. Li X, Su Y, Sun B, Ji W, Peng Z, Xu Y, et al. An artificially designed interfering lncRNA expressed by oncolytic adenovirus competitively consumes oncomiRs to exert antitumor efficacy in hepatocellular carcinoma. Mol Cancer Ther. (2016) 15:1436–51. doi: 10.1158/1535-7163.Mct-16-0096
57. Yao H, Yang Z, Lou Y, Huang J, Yang P, Jiang W, et al. miR-186 inhibits liver cancer stem cells expansion via targeting PTPN11. Front Oncol. (2021) 11:632976. doi: 10.3389/fonc.2021.632976
58. Zheng J, Wang S, Xia L, Sun Z, Chan KM, Bernards R, et al. Hepatocellular carcinoma: signaling pathways and therapeutic advances. Signal Transduct Target Ther. (2025) 10:35. doi: 10.1038/s41392-024-02075-w
59. Wang J, Cao W, Huang J, Zhou Y, Zheng R, Lou Y, et al. Tumor-associated CD19+ Macrophages induce immunosuppressive microenvironment in hepatocellular carcinoma. (2025).
60. Shiri AM, Zhang T, Bedke T, Zazara DE, Zhao L, Lücke J, et al. IL-10 dampens antitumor immunity and promotes liver metastasis via PD-L1 induction. J Hepatol. (2024) 80:634–44. doi: 10.1016/j.jhep.2023.12.015
61. Xin X, Cheng X, Zeng F, Xu Q, and Hou L. The role of TGF-β/SMAD signaling in hepatocellular carcinoma: from mechanism to therapy and prognosis. Int J Biol Sci. (2024) 20:1436–51. doi: 10.7150/ijbs.89568
62. Calderaro J, Seraphin TP, Luedde T, and Simon TG. Artificial intelligence for the prevention and clinical management of hepatocellular carcinoma. J Hepatol. (2022) 76:1348–61. doi: 10.1016/j.jhep.2022.01.014
Keywords: tumor-initiating cells, liver cancer, tumor microenvironment, therapeutic resistance, immunotherapy, nanotechnology, genome editing, non-coding RNAs
Citation: Chai Y, Xu T, Chen X, Chen B, Du X and Zhang Z (2025) Immunotherapy targeting liver cancer tumor-initiating cells: challenges, mechanisms, and emerging therapeutic horizons. Front. Immunol. 16:1621243. doi: 10.3389/fimmu.2025.1621243
Received: 30 April 2025; Accepted: 28 May 2025;
Published: 11 June 2025.
Edited by:
Chen Yang, Southern Medical University, ChinaReviewed by:
Hongpan Zhang, Affiliated Hospital of North Sichuan Medical College, ChinaShunxiang Gao, Shanghai Jiao Tong University, China
Copyright © 2025 Chai, Xu, Chen, Chen, Du and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhezhong Zhang, emhhbmd6aGV6aG9uZzIwMjNAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Yinying Chai1†
Yinying Chai1† Tinghui Xu
Tinghui Xu Zhezhong Zhang
Zhezhong Zhang