- Department of Woman, Child and General and Specialized Surgery, University of Campania ‘Luigi Vanvitelli’, Naples, Italy
A Commentary on
Long COVID in pediatric age: an observational, prospective, longitudinal, multicenter study in Italy
By Esposito S, Puntoni M, Deolmi M, Ramundo G, Maglietta G, Poeta M, Zampogna S, Colomba C, Suppiej A, Cardinale F, Bosis S, Castagnola E, Midulla F, Giaquinto C, Giordano P, Biasucci G, Fainardi V, Nunziata F, Grandinetti R, Condemi A, Raiola G, Guarino A, Caminiti C and Long-Covid-Ped Italian Study Group (2025). Front. Immunol. 16:1466201. doi: 10.3389/fimmu.2025.1466201
The original research entitled ‘Long COVID in pediatric age: an observational, prospective, longitudinal, multicenter study in Italy’, conducted by Esposito et al., offers critical insight into the long-term consequences of SARS-CoV-2 infection in children and adolescents (1). By recruiting over 1,100 participants across 12 Italian centers and following them for 12 months, authors provide one of the most comprehensive pediatric long COVID datasets available to date. Using a standardized follow-up at 1–3, 3–6, and 6–12 months post-infection, and a child-adapted definition of long COVID aligned with World Health Organization (WHO) criteria, the study confirms that approximately 16% of infected children report persistent symptoms lasting over two months. These symptoms include respiratory complaints, fatigue, cognitive difficulties, sleep disturbances, and gastrointestinal issues. Importantly, the study reveals that while most children recover within a year, a significant subset continues to experience symptoms impacting their quality of life (1).
This well-designed multicenter study, with standardized outcomes and a control group, reveals that adolescents and females are especially vulnerable to neuropsychological sequelae. Despite lacking objective tests, it significantly advances understanding of pediatric long COVID (1).
However, despite the growing body of literature, a standardized follow-up protocol for children with suspected long COVID is still lacking. In this context, we would like to contribute to the discussion by sharing findings from two recent investigations conducted by our multidisciplinary team of pediatricians and child neuropsychiatrists at the Pediatric Clinic of the University of Campania “Luigi Vanvitelli” in Naples, Italy.
We implemented a structured follow-up protocol for all children presenting with persistent symptoms following confirmed SARS-CoV-2 infection. This included a clinical examination, spirometry, a six-minute walking test, and lung ultrasound (LUS), a non-invasive and radiation-free technique, to identify subclinical pulmonary abnormalities and assess their relationship with clinical and anthropometric parameters. We also evaluated psychological symptoms using two validated questionnaires: the Child Behavior Checklist (CBCL) and the Sleep Disturbance Scale for Children (SDSC) Figure 1.
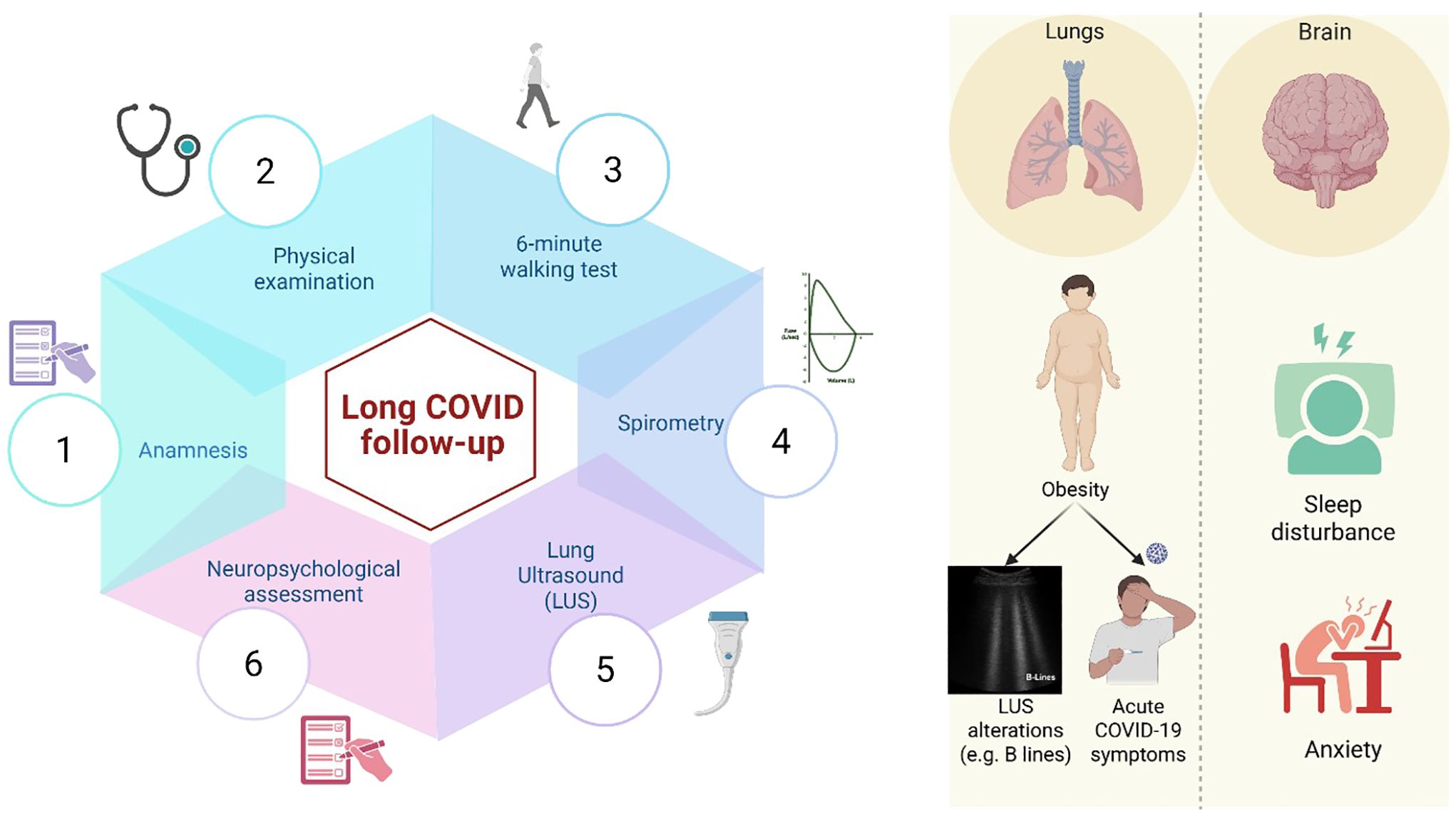
Figure 1. The figure illustrates the long COVID follow-up conducted at our Pediatric Clinic at the University of Campania “Luigi Vanvitelli” in Naples, Italy. We collected detailed medical histories, including SARS-CoV-2-related manifestations, conducted clinical examinations, a 6-minute walking test, spirometry, lung ultrasound (LUS), and a neuropsychological evaluation. Our findings confirmed that the most common long COVID symptoms in the pediatric population involve neuropsychological aspects and pulmonary manifestations. In particular, obesity was significantly associated with both the severity of the acute phase of the disease and the presence of LUS abnormalities. We also observed an increase in behavioral and sleep disturbances, especially among adolescents, with a broader impact on their physical and emotional well-being. These findings highlight the need for long-term, in-depth follow-up over the coming years. Figure created in https://BioRender.com.
In our first study, we evaluated respiratory outcomes in a cohort of 104 children and adolescents with persistent symptoms beyond four weeks after SARS-CoV-2 infection. Using LUS, we identified abnormal findings such as pleural line irregularities and coalescent B-lines in 27% of patients. These findings were not associated with a history of asthma or allergic disease/sensitization, but showed a significant correlation with overweight status (BMI >85th percentile). This suggests that obesity may not only increase the risk of acute COVID-19 complications but also predispose to subtle, long-lasting pulmonary alterations in the post-acute phase (2).
Our second study focused on the neuropsychiatric impact of long COVID, analyzing behavioral and sleep disturbances through the CBCL and SDSC in a matched case-control cohort of 107 children and adolescents. We found a significant increase in internalizing symptoms, particularly anxiety, depression, and somatic complaints in post-COVID cases compared to controls. These behavioral changes were paralleled by a higher prevalence of sleep disturbances, notably sleep-disordered breathing and alterations during the sleep-wake transition phase. A strong correlation emerged between behavioral and sleep domain scores, underscoring the intertwined nature of emotional well-being and sleep quality (3).
These findings suggest that long COVID extends beyond physical manifestations, significantly affecting children’s emotional well-being, sleep patterns, and social functioning. These alterations are likely supported by neuroinflammatory mechanisms, sustained immune activation, or the cumulative impact of psychosocial stressors experienced during and after infection. Disrupted peer relationships, decreased school attendance, and a persistent sense of health-related uncertainty can amplify emotional distress and contribute to the emergence of behavioral issues, particularly in vulnerable populations such as adolescents. These holistic consequences emphasize the urgent need to reframe pediatric care, shifting from a purely somatic approach toward comprehensive, multidisciplinary follow-up strategies. Such protocols should be designed to monitor and address both the immediate and long-term neurodevelopmental, emotional, and social sequelae associated with pediatric long COVID (4, 5).
We thank the authors for their valuable contribution and for encouraging continued dialogue on pediatric COVID-19. We hope our clinical experience will inform future research and improve management strategies for long COVID. In particular, we believe that our structured follow-up protocol and the demonstrated utility of LUS may support efforts to standardize long-term care in affected children.
Author contributions
CI: Writing – review & editing, Writing – original draft. AK: Writing – review & editing, Writing – original draft. GD: Writing – review & editing, Writing – original draft. CG: Writing – original draft, Writing – review & editing. MMM: Writing – original draft, Writing – review & editing. MMG: Writing – review & editing, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, and/or publication of this article.
Conflict of interest
The declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sposito S, Puntoni M, Deolmi M, Ramundo G, Maglietta G, Poeta M, et al. Long COVID in pediatric age: an observational, prospective, longitudinal, multicenter study in Italy. Front Immunol. (2025) 16:1466201. doi: 10.3389/fimmu.2025.1466201
2. Indolfi C, Klain A, Dinardo G, D’Addio E, Ferrara S, Decimo F, et al. COVID-19 pediatric follow-up: respiratory long COVID-associated comorbidities and lung ultrasound alterations in a cohort of Italian children. Children (Basel). (2024) 11:166. doi: 10.3390/children11020166
3. Miraglia Del Giudice M, Klain A, Dinardo G, D'Addio E, Bencivenga CL, Fontanella C, et al. Behavioral and sleep disorders in children and adolescents following COVID-19 disease: a case-control study. Children (Basel). (2023) 10:1189. doi: 10.3390/children10071189
4. Premraj L, Kannapadi NV, Briggs J, Seal SM, Battaglini D, Fanning J, et al. Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: a meta-analysis. J Neurol Sci. (2022) 434:120162. doi: 10.1016/j.jns.2022.120162
Keywords: long COVID, children, follow-up protocol, lung ultrasound, neuropsychological symptoms
Citation: Indolfi C, Klain A, Dinardo G, Grella C, Marrapodi MM and Miraglia del Giudice M (2025) Commentary: Long COVID in pediatric age: an observational, prospective, longitudinal, multicenter study in Italy. Front. Immunol. 16:1624011. doi: 10.3389/fimmu.2025.1624011
Received: 06 May 2025; Accepted: 29 August 2025;
Published: 12 September 2025.
Edited by:
Vijayakumar Velu, Emory University, United StatesReviewed by:
Sakthivel Govindaraj, Emory University, United StatesMaria Mendez, Hospital Germans Trias i Pujol, Spain
Copyright © 2025 Indolfi, Klain, Dinardo, Grella, Marrapodi and Miraglia del Giudice. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Giulio Dinardo, ZGluYXJkb2dpdWxpb0BnbWFpbC5jb20=; Carolina Grella, Y2Fyby5ncmVsbGE5NEBnbWFpbC5jb20=
†These authors have contributed equally to this work and share first authorship
 Cristiana Indolfi
Cristiana Indolfi Angela Klain
Angela Klain Giulio Dinardo
Giulio Dinardo Carolina Grella
Carolina Grella Maria Maddalena Marrapodi
Maria Maddalena Marrapodi Michele Miraglia del Giudice
Michele Miraglia del Giudice