- 1Department of Laboratory Medicine, Affiliated Hospital of Jiangsu University, Zhenjiang, China
- 2Department of Immunology, Jiangsu Key Laboratory of Laboratory Medicine, School of Medicine, Jiangsu University, Zhenjiang, China
- 3Department of Nuclear Medicine, Affiliated Hospital of Jiangsu University, Zhenjiang, China
Lupus nephritis (LN), a severe complication of systemic lupus erythematosus (SLE), is associated with increased morbidity and mortality. The pathogenesis of LN involves complex immune-mediated mechanisms that alter the biology of renal resident epithelial cells. Emerging evidence highlights the bidirectional interactions between immune cells and renal epithelial cells—including podocytes and tubular epithelial cells(TECs)—as critical contributors to disease progression. These interactions shape local immune responses, drive inflammatory injury, and disrupt renal function. However, the molecular and cellular basis of this crosstalk remains incompletely understood. Recent advances have uncovered key mechanisms underlying these interactions and identified potential therapeutic targets that may inform future treatment strategies. This review summarizes current findings on the immunological roles of renal epithelial cells in LN and discusses their relevance to the development of targeted and cell-specific therapeutic interventions.
1 Introduction
Systemic lupus erythematosus (SLE) is a prototypical systemic autoimmune disorder in which dysregulated immunity drives self-directed attacks on multiple tissues (1). Worldwide, its incidence ranges from 1 to 8.7 cases per 100 000 person-years and its prevalence from 8 to 180 cases per 100 000 population (2, 3).
The disease exhibits a striking female predominance, especially among women of reproductive age, with a female-to-male ratio of 6.1–13.3 : 1 (2, 3). Impaired clearance of apoptotic cells and loss of tolerance to endogenous antigens, such as double-stranded DNA (dsDNA), underlie persistent immune activation (4). Consequently, both innate and adaptive responses are amplified, driving high titers of anti-nuclear autoantibodies, formation of immune complexes (ICs), and complement activation (5). IC deposition in glomerular capillary walls provokes robust local inflammation and is a major determinant of lupus-related renal dysfunction, underscoring the kidney’s particular vulnerability in SLE (6–8).
Lupus nephritis (LN) is the most frequent and clinically devastating complication of SLE (9). It is defined by immune-complex–driven chronic inflammation that produces multi-compartmental renal injury (Table 1) (10). Nearly 40 % of patients develop LN within five years of an SLE diagnosis (11), and in some individuals the renal syndrome is the initial presentation that prompts recognition of underlying SLE (12, 13). LN substantially increases morbidity and mortality; 10–20 % of affected patients progress to end-stage renal disease (ESRD) within five years (14). ESRD refers to the stage of kidney disease that requires dialysis or kidney transplantation, and patients are usually accompanied by a severe symptom burden and multiple chronic conditions (MCC) (15). This disease has a particularly profound impact on patients’ quality of life (QoL) (16, 17). From the initiation of dialysis, the life expectancy of patients with ESRD is generally less than 3 years. Therefore, ESRD not only means that patients need lifelong dependence on renal replacement therapy but also brings a heavy economic and social burden to individuals and public health systems (18, 19). It is noteworthy that the prevalence and severity of LN show significant racial and ethnic differences. Large epidemiological studies have shown that the risk of disease is significantly higher in African, Asian, and Hispanic populations than in white populations (3, 9, 20–24), among which African and Asian patients also have a significantly increased risk of end-stage renal disease (25). An international inception cohort study showed that the incidence of LN in patients with systemic lupus erythematosus was 39.9% in African individuals, 49.3% in Hispanic individuals, 36.8% in Asian individuals, and 20.3% in white individuals (26). Similarly, a special study on SLE patients in the United States found that, compared with the white population, the risks of LN were higher in Black, Asian and Pacific Islander, and Hispanic populations (24). In addition, male SLE patients and those with childhood-onset disease are more likely to progress to severe renal lesions (26–34).
Immune-mediated renal inflammation in LN involves not only aberrant immune cell responses but also the dysfunction of resident renal cells, particularly podocytes and renal tubular epithelial cells (RTECs) (35). These two components together contribute to glomerular, tubulointerstitial, and vascular injury, ultimately driving the initiation and progression of LN (8). Podocytes, integral to the glomerular filtration barrier, express a variety of pattern recognition receptors—including Toll-like receptors (TLRs)—as well as complement-associated proteins (36, 37). Upon pathological stimulation, these receptors activate multiple intracellular pathways that lead to podocyte injury and disruption of barrier integrity.RTECs also play an active role in renal inflammation by secreting proinflammatory mediators and engaging in adaptive immune responses. For instance, anti-double-stranded DNA (anti-dsDNA) antibodies can stimulate RTECs to produce tumor necrosis factor-α (TNF-α), which enhances immune cell recruitment and triggers downstream inflammatory cascades (38). In parallel, various immune cell subsets—including neutrophils, T and B lymphocytes, dendritic cells, and macrophages—are robustly activated in LN. Through cytokine secretion, antibody production, and tissue infiltration, they exacerbate structural damage to the kidney (39). Renal epithelial cells and immune cells engage in a bidirectional regulatory interplay mediated by cytokine networks and direct cell–cell contact (40). This crosstalk cooperatively activates multiple proinflammatory signaling pathways (Table 2, Figure 1), thereby driving the immunopathological progression of LN. For instance, in vitro studies have shown that IL-6 secreted by podocytes acts on glomerular endothelial cells (GECs) to inhibit neutrophil recruitment, whereas neutrophils, in turn, compromise podocyte function by releasing proteolytic enzymes and other mediators (41), ultimately contributing to LN progression. This interplay amplifies renal inflammation and drives the immunopathogenesis of LN. This review highlights the complex crosstalk between renal epithelial cells and immune cells within the kidney and delineates their mechanistic roles in the development and progression of lupus nephritis.
Renal epithelial cells/immune cells regulate transcription through various signaling pathways, and the cytokines produced can affect immune cells/renal epithelial cells.
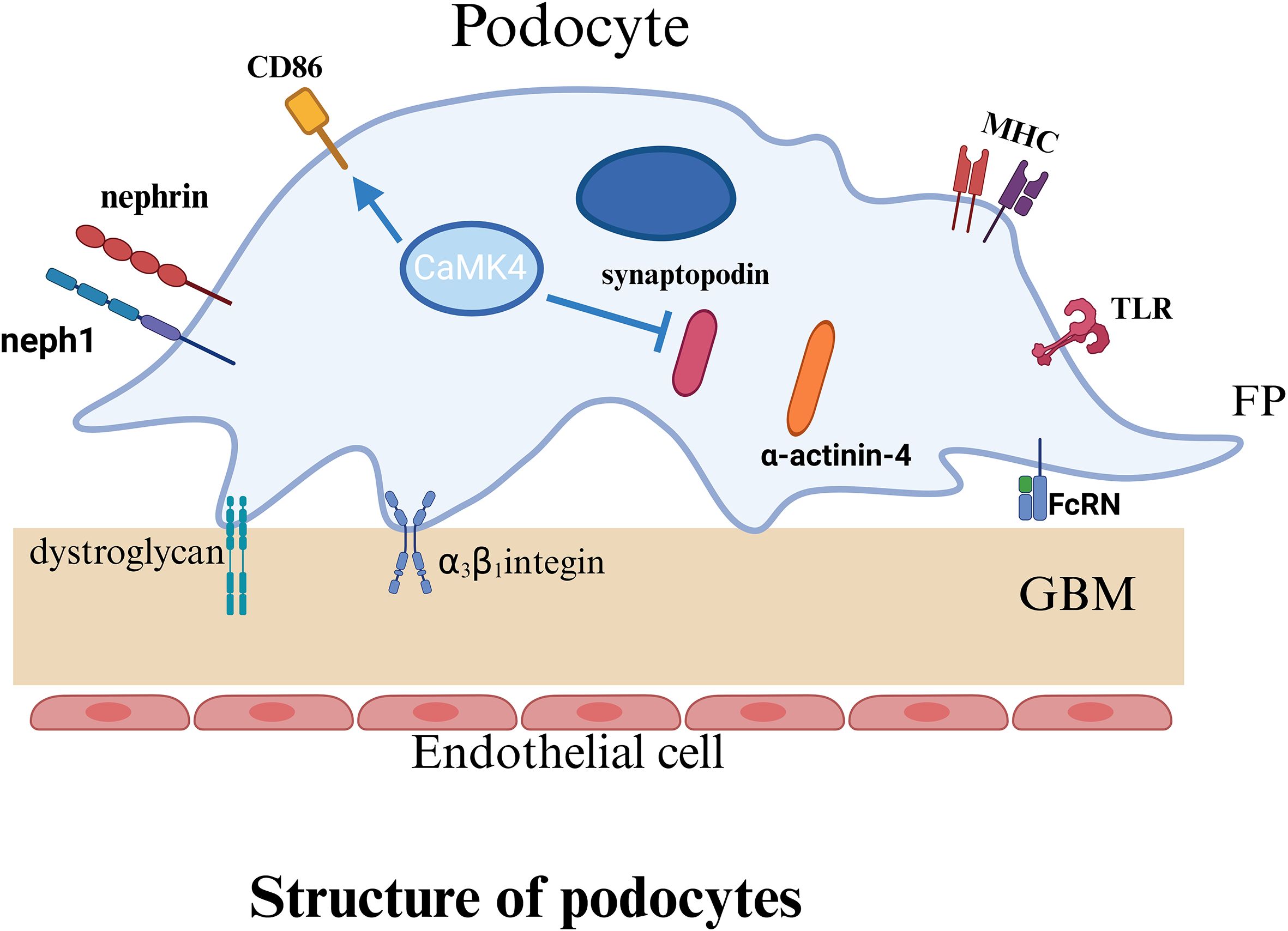
2 Basic structure and function of podocytes
Podocytes are an essential component of the glomerular filtration barrier, and their highly specialized morphology (see Figure 2) is critical for preserving filtration function. Interdigitating foot processes of podocytes form the slit diaphragm (SLD) (42, 43), a specialized junctional structure composed primarily of nephrin and podocin. These proteins, in conjunction with the actin cytoskeleton and adhesion molecules, establish a stable network that preserves the structural integrity of the filtration barrier (44, 45). Studies have shown that aberrant IgG glycosylation in patients with SLE contributes to podocyte injury in LN, leading to cytoskeletal remodeling, impaired motility, and reduced nephrin production (46). These alterations accelerate the progression of LN (46). Nephrin, a transmembrane immunoglobulin-like adhesion molecule (47), constitutes the structural backbone of the SLD and is essential for maintaining the mechanical cohesion and selective permeability between adjacent foot processes (48). Podocin, another key transmembrane protein, interacts with nephrin to stabilize its membrane localization (49) and link it to intracellular signaling pathways, thereby supporting podocyte architecture and function (50). Deficiency or dysfunction of either protein disrupts the integrity of the filtration barrier and leads to the development of proteinuria. Relevant studies have demonstrated that podocyte-associated proteins, such as nephrin, podocin, and podocalyxin, serve as important indicators for assessing podocyte injury in human glomerular diseases (51). Accordingly, the loss or dysfunction of nephrin and podocin not only disrupts the structural integrity of the slit diaphragm but also directly compromises the filtration barrier, ultimately leading to proteinuria.
The structural integrity of podocyte foot processes is primarily supported by actin, a highly dynamic cytoskeletal element essential for maintaining cellular morphology, adhesion, and motility (52). The reorganization of actin filaments is tightly regulated by synaptopodin (53), an actin-associated protein that reinforces cytoskeletal architecture and modulates podocyte migration. Synaptopodin interacts with α-actinin-4 to stabilize the structure and morphology of foot processes (54). It also protects the small GTPase RhoA from proteasomal degradation, thereby promoting stress fiber formation and regulating cytoskeletal tension and motility (55). For instance, studies in lupus-prone mouse models have revealed that synaptopodin expression is upregulated during podocyte apoptosis (56). Therefore, synaptopodin expression is closely associated with podocyte injury and may contribute to the progression of LN (56). In addition, podocytes adhere to the glomerular basement membrane (GBM) through integrins (such as α3β1) and α-/β-dystroglycans, which anchor the cells to the GBM and mediate outside-in signaling critical for maintaining filtration barrier stability (42, 53).
In LN, podocytes serve not only as structural targets but also as active participants in disease pathogenesis. Within the inflammatory milieu, cytokines and immune complexes generated by immune activation trigger reorganization of the actin cytoskeleton, effacement of foot processes, and disruption of the slit diaphragm, thereby aggravating proteinuria and impairing renal function. Podocytes in LN upregulate immune-related molecules such as TLRs, complement receptors, and MHC class II (57–59), and aberrantly express the neonatal Fc receptor (FcRn) under inflammatory stress (60–62), which facilitates immune complex transcytosis and deposition. Moreover, podocytes produce a range of cytokines (57), contributing to local immune modulation and amplifying inflammatory responses, while also possessing potential immunoregulatory functions. Importantly, podocytes can present antigens (63) and support the activation of T and B lymphocytes, thereby enhancing autoantibody production and perpetuating tissue injury (47, 64). The integrity of podocyte structure—dependent on cytoskeletal organization, slit diaphragm maintenance, and anchorage to the GBM—is disrupted by immune-mediated cytoskeletal remodeling, which is considered a central mechanism of podocyte injury in LN. This process is driven by a convergence of inflammatory insults, genetic predisposition, toxic exposures, and metabolic disturbances, ultimately leading to filtration barrier breakdown and disease progression (65).
A schematic illustration of the basic structure of the podocyte indicates the structure and important proteins of the podocyte. P, podocyte; FP, foot process; GBM, glomerular basement membrane; TLR, Toll like receptors; MHC, major histocompatibility complex; FcRn, Neonatal Fc receptor.
3 Crosstalk between podocytes and innate immune cells
Emerging evidence indicates that, beyond their structural role in preserving glomerular integrity, podocytes actively engage in reciprocal interactions with innate immune cells—including macrophages, neutrophils, and dendritic cells—which collectively orchestrate local inflammation and contribute to the pathogenesis of LN (Figure 3A). In this context, podocytes function not only as passive targets of immune-mediated injury but also as active regulators of renal inflammation. Upon stimulation, podocytes secrete various chemokines, such as CCL2, CXCL1, and CXCL13, which recruit monocytes (66), neutrophils (67), and dendritic cells (67) into the glomerulus, thereby amplifying inflammatory responses and promoting renal damage. Of note, dendritic cells represent a major source of CXCL13 (68), which binds to CXCR5 receptors expressed on podocytes and activates the ERK signaling pathway, subsequently inducing the expression of adhesion molecules ICAM-1 and VCAM-1 (69). Through chemotactic gradients, these chemokines facilitate the recruitment of innate immune cells, such as macrophages and neutrophils, to sites of inflammation, reinforcing the local immune response. Notably, blockade of CCL2 or its receptor CCR2 significantly reduces monocyte/macrophage recruitment to the kidney and alleviates glomerular and interstitial injury (70, 71). The infiltrating innate immune cells perform distinct immunological functions within the renal microenvironment, ultimately shaping the progression of LN pathology.
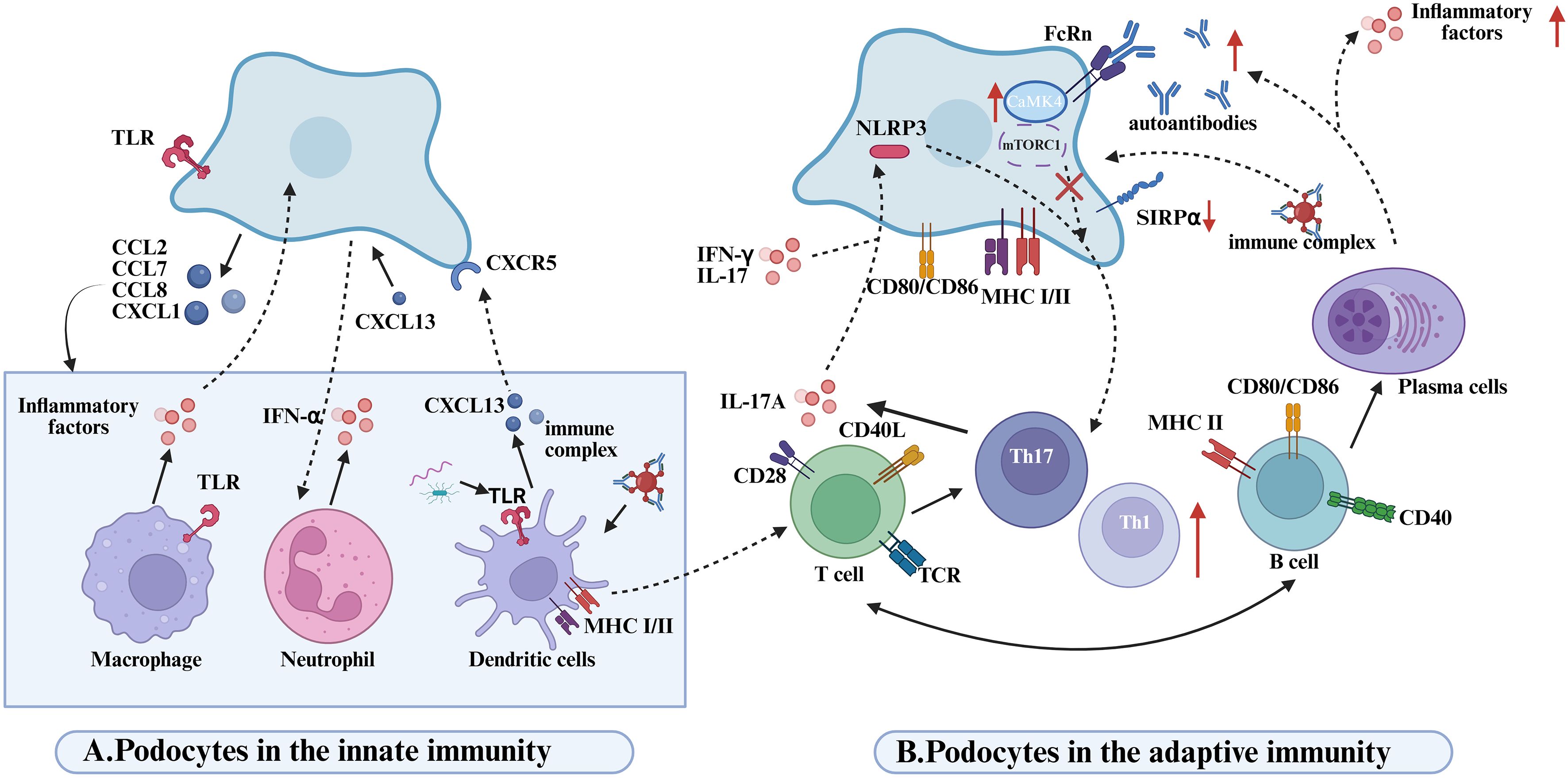
Figure 3. Disease mechanisms mediated by podocyte-immune cell interactions in lupus nephritis. (A) Podpcytes in the innate immunity. Podocytes recruit innate immune cells (macrophages, neutrophils, DCs) via chemokine secretion (CCL2/7/8, CXCL1), amplifying inflammation. Macrophage-derived proinflammatory cytokines drive proteinuria in glomerular diseases. TLRs on macrophages/DCs recognize PAMPs, activating innate immunity. Neutrophil infiltration and IFN-α release exacerbate renal inflammation in LN. CXCL13-stimulated podocyte media triggers neutrophil activation and local inflammation. DCs produce CXCL13, binding podocyte CXCR5 to activate ERK signaling and enhance proinflammatory secretion, worsening LN. DCs phagocytose apoptotic/immune complexes to promote Th17 differentiation.Th17-derived IL-17A directly damages podocytes and induces NLRP3 inflammasome/IL-1β release, sustaining inflammation. pDCs detect microbial/eukaryotic nucleic acids via TLR9, driving IFN-I production and systemic immune activation through costimulatory upregulation. (B) Podpcytes in the adaptive immunity. Podocytes activate T cells via MHC I/II and costimulatory molecule expression; CD80 enhances T-cell proliferation/aggregation. LN podocytes exhibit SIRPα downregulation, promoting Syk phosphorylation to boost antigen presentation and T-cell responses. IFN-α/γ and IL-17 modulate podocyte antigen presentation by targeting SIRPα.LN IgG enters podocytes via FcRn, inducing CaMK4-CD86 upregulation to amplify T-cell costimulation in a self-reinforcing loop.NLRP3 activation in injured podocytes biases Th17/Th1 differentiation; Th17-derived IL-17A disrupts podocyte cytoskeleton and triggers inflammation. Podocyte mTORC1 activation drives glomerulopathy via endothelial crosstalk, while T-cell mTORC1 hyperactivity expands Th1/Th17/DN T cells and suppresses Tregs. B cells directly damage kidneys via autoantibodies; B1 cells accumulate in LN kidneys, differentiating into autoantibody/cytokine-producing plasma cells.
Recruited macrophages infiltrate extensively into LN lesions and release pro-inflammatory cytokines such as TNF-α and IL-1β, which downregulate the expression of critical podocyte structural proteins, including nephrin (72). This disruption compromises the glomerular filtration barrier, ultimately resulting in proteinuria. The formation of a positive feedback loop between activated podocytes and infiltrating macrophages plays a pivotal role in sustaining renal inflammation during LN. Moreover, the synergistic activation of Toll-like receptors TLR2 and TLR4 further amplifies this inflammatory circuit. These receptors are broadly expressed on both podocytes and macrophages and can recognize pathogen-associated molecular patterns (PAMPs) as well as endogenous damage-associated molecular patterns (DAMPs), leading to downstream signal transduction and the production of inflammatory mediators such as TNF-α and IL-1β (73). TLR-mediated co-activation not only intensifies the pro-inflammatory capacity of macrophages but also enhances the immunological responsiveness of podocytes, thereby exacerbating glomerular inflammation and accelerating LN progression (74). In parallel, neutrophils are also markedly recruited into the renal tissues of LN patients (75), where they secrete interferon-α (IFN-α), reactive oxygen species (ROS), and proteolytic enzymes that contribute to tissue injury (41). Neutrophils undergoing cell death release neutrophil extracellular traps (NETs)—web-like structures composed of decondensed DNA and antimicrobial proteins—which can bind autoantigens and trigger immune activation. This process further amplifies the inflammatory cascade and promotes the pathophysiological progression of LN (41).
In macrophage-mediated podocyte injury, the activation state of macrophages is a key determinant of renal inflammatory outcomes. Macrophage phenotypes are largely shaped by cues from the local microenvironment (76) and are broadly categorized into pro-inflammatory M1 (classically activated) and anti-inflammatory M2 (alternatively activated) subsets (77). In LN, a disruption in the M1/M2 balance is closely linked to disease activity (78). The active phase of LN is typically dominated by M1 macrophages (79), which secrete high levels of inflammatory mediators such as TNF-α and IL-1β.These cytokines downregulate the expression of essential podocyte structural proteins, disrupt the glomerular filtration barrier, and exacerbate both proteinuria and tissue inflammation. In contrast, during disease remission, the prevalence of M2 macrophages increases (80). These cells release anti-inflammatory cytokines and tissue-reparative factors, which contribute to podocyte protection and restoration of glomerular barrier integrity. Transcriptomic profiling has revealed a dynamic shift of macrophages from an M1 to M2 phenotype during LN progression, accompanied by suppressed expression of pro-inflammatory genes (81). This phenotypic transition exerts protective effects on podocytes by attenuating inflammatory damage. Collectively, macrophage polarization from a pro-inflammatory to an anti-inflammatory state appears to mitigate podocyte injury (72) and may serve as an intrinsic regulatory mechanism during disease resolution (72, 80). Consequently, therapeutic strategies aimed at promoting M2 polarization have gained attention as a promising approach to slowing LN progression and preserving podocyte integrity (82).
In addition to interacting with macrophages and neutrophils, podocytes engage in dynamic and bidirectional crosstalk with DCs, actively shaping the local immune microenvironment in LN (83). DCs recruited to the kidney play a non-redundant role in LN immunopathogenesis (84, 85). Experimental studies have demonstrated that, despite persistent glomerular deposition of immune complexes, either genetic deficiency of Fcγ receptors or selective depletion of DCs can effectively prevent T cell activation and leukocyte infiltration in renal tissues. DCs contribute to the differentiation of Th17 cells by phagocytosing apoptotic bodies or immune complexes (83). In turn, Th17-derived IL-17A not only exerts direct cytotoxic effects on podocytes but also induces NLRP3 inflammasome activation and promotes IL-1β release, thereby amplifying the local inflammatory cascade (4). Furthermore, DCs activate autoreactive T cells through self-antigen presentation, which facilitates B cell-driven production of pathogenic autoantibodies, such as anti-dsDNA antibodies. These autoantibodies can form immune complexes with podocyte surface antigens, including α-actinin, and upon deposition in the glomeruli, activate the complement cascade. This leads to cytoskeletal rearrangement and disruption of the slit diaphragm architecture in podocytes, thereby exacerbating glomerular injury (86).
4 Crosstalk between podocytes and adaptive immune cells
Podocytes, once considered mere passive targets in LN, are now recognized as active participants in immune modulation. Through direct interaction with T and B lymphocytes, they shape adaptive immune responses and contribute to glomerular inflammation and injury (Figure 3B).
4.1 Podocytes and T lymphocytes
In the pathogenesis of LN, interactions between T cells and podocytes play a pivotal role in disrupting the glomerular filtration barrier and propagating inflammation. Inflammatory mediators released by autoreactive T cells amplify local renal immune responses, while certain autoantibodies—some of which cross-react with podocyte antigens such as α-actinin—further exacerbate renal tissue injury (87, 88). Increasing evidence highlights the crucial and diverse roles of dysregulated helper T (Th) cell subsets in mediating podocyte damage. Based on their cytokine profiles, Th cells are categorized into distinct functional subsets (89), each contributing differentially to the pathological processes involved in podocyte injury. Among them, Th17 cells predominantly produce IL-17A and IL-17F, whose receptors are broadly expressed across various renal cell types, including podocytes. These cytokines activate pro-inflammatory and pro-fibrotic pathways, promoting the release of cytokines and chemokines that sustain chronic inflammation and maladaptive tissue repair, ultimately resulting in fibrosis and disruption of renal architecture (90). IL-17A, in particular, has been shown to alter podocyte morphology and induce structural injury (91). Moreover, in LN, activation of the Th17 lineage and elevated IL-17 levels are associated with podocyte apoptosis, cytoskeletal rearrangement, foot process effacement, increased motility, reduced expression of homeostatic proteins, and heightened oxidative stress, along with activation of inflammasomes and caspase cascades within podocytes (92–94). Importantly, IL-17A can also engage surface receptors on podocytes to trigger NLRP3 inflammasome activation and subsequent IL-1β release, thereby amplifying local inflammatory responses (4, 95). The activation of NLRP3 inflammasomes within podocytes not only contributes to structural cell damage but may also reshape the local immune milieu, influencing adaptive immune responses. Hutton et al. (96) proposed that NLRP3 activation in podocytes facilitates the skewing of helper T cells toward the Th17 phenotype, further promoting podocyte injury in LN. Beyond Th17 involvement, Th2 cells have also been implicated in podocyte damage in specific LN subtypes.Th2-driven immune responses are thought to facilitate subepithelial immune complex deposition (97–99), leading to complement activation and formation of the membrane attack complex (C5b-9), which injures renal epithelial cells. Additionally, both inflammasomes and mTORC1 signaling pathways have been shown to regulate Th cell differentiation, thereby contributing to the immunopathological landscape of LN (100, 101). As a key component of the innate immune system, the NLRP3 inflammasome can be activated and assembled in response to a wide array of exogenous and endogenous danger signals (102).
Accumulating evidence has demonstrated that depletion of T cells or blockade of T cell activation significantly alleviates LN progression in lupus-prone mice (103, 104). Notably, podocytes themselves are not merely passive targets but active participants in modulating T cell responses. They express both MHC class I and class II molecules (63, 105), thereby possessing antigen-presenting capacity and directly contributing to the activation of CD4+ and CD8+T cells during LN pathogenesis. Conditional deletion of MHC class II in podocytes markedly reduces CD4+T cell activation, highlighting their immunoregulatory potential (63). In parallel, CD8+T cells recognizing disease-relevant antigens presented by podocytes can exert cytotoxic effects, contributing to crescent formation within glomeruli (106). Crescents—characterized by the proliferation of parietal epithelial cells and infiltration of inflammatory cells in Bowman’s space—are histological hallmarks of severe glomerular injury and are associated with poor clinical outcomes (106, 107). Furthermore, podocytes can enhance T cell activation through the expression of costimulatory molecules such as CD80 (B7-1) and CD86 (B7-2). Inflammatory stimuli, such as TLR activation, upregulate CD80 expression on podocytes (108, 109), which facilitates T cell proliferation and accumulation within renal tissue (81). Beyond its immunostimulatory role, CD80 also compromises slit diaphragm integrity, exacerbating podocyte injury and impairing glomerular filtration barrier function (110). CD80 and CD86 interact with T cell receptors CD28 or CTLA-4 to deliver activating or inhibitory signals, thereby fine-tuning the strength and outcome of T cell responses (111, 112). Elevated B7–1 expression has been observed in podocytes from LN patients, where its activation induces redistribution of key slit diaphragm proteins such as nephrin and podocin, correlating strongly with proteinuria severity (109). Moreover, podocytes are capable of internalizing immune complexes, particularly IgG, and can activate infiltrating T cells via cross-presentation mechanisms. This activation triggers the release of proinflammatory cytokines that contribute to podocyte dysfunction and apoptosis (105). FcRn plays a crucial role in IgG transcytosis in podocytes, facilitating antigen sampling and immune modulation. IgG internalization via FcRn induces the expression of CaMK4 (113), a key mediator downstream of TCR signaling that is aberrantly activated in T cells from SLE patients and contributes to immune dysregulation (36). In podocytes, CaMK4 upregulates CD86 expression (113), amplifying costimulatory signaling and further exacerbating local inflammation and tissue injury (62).
In addition to intrinsic immunogenic properties, the ability of podocytes to activate T cells is further modulated by the inflammatory milieu. Proinflammatory cytokines such as IFN-γ and IL-17 have been shown to enhance the antigen-presenting capacity of podocytes, thereby promoting antigen-specific T cell activation and contributing to podocyte injury and renal inflammation (114). Mechanistically, signal regulatory protein alpha (SIRPα), expressed in podocytes, functions as a negative regulator of antigen presentation. It exerts its inhibitory effect by suppressing phosphorylation of spleen tyrosine kinase (Syk), a key molecule in downstream immune signaling (114). However, proinflammatory cytokines including IFN-α, IFN-γ, and IL-17 can downregulate SIRPα expression, thereby relieving this inhibitory checkpoint and augmenting the ability of podocytes to activate T cells (115–120). Supporting this, exposure of podocytes to LN patient serum has been shown to induce T cell proliferation and increased IFN-γ production, suggesting that under inflammatory conditions, podocytes can acquire dendritic cell-like immunostimulatory properties (121). Notably, IFN-γ not only promotes T cell activation but also modulates podocyte function in a feedback manner by suppressing SIRPα expression, further amplifying local immune activation.
4.2 Podocytes and B lymphocytes
B lymphocytes play a pivotal role in the pathogenesis of LN (7, 122), primarily through the production of autoantibodies and pro-inflammatory cytokines that contribute to renal injury, particularly targeting podocytes (123). In LN, aberrantly activated B cells differentiate into plasma cells that secrete pathogenic autoantibodies, including anti-dsDNA antibodies (124).
The accumulation of autoantibodies within the kidney is a critical contributor to renal inflammation and dysfunction in lupus nephritis (125, 126). These autoantibodies directly target podocyte surface antigens, such as α-actinin-4, inducing cytoskeletal remodeling that leads to podocyte injury (124), dedifferentiation, apoptosis, or detachment (114). Concurrently, antibody binding activates the complement cascade, compromising the integrity of the podocyte filtration barrier and resulting in proteinuria (58, 88). ICs formed by the interaction of antibodies with glomerular basement membrane or podocyte antigens deposit in close proximity to podocytes, acting as principal mediators of podocyte-directed immune injury (127) and thereby impairing glomerular filtration function (128). Moreover, anti-nuclear antibodies associate with nucleosomes released from apoptotic cells to generate proinflammatory complexes localized within the glomerulus (129). Notably, anti-dsDNA antibodies are enriched in renal tissues compared to systemic circulation and can cross-react with podocyte α-actinin, disrupting podocyte stability (86). Importantly, podocytes actively participate in antibody-mediated pathology rather than remaining passive targets. Upregulation of Fc receptors on their surface, particularly FcRn, facilitates IgG uptake (130). Internalized IgG triggers upregulation of CaMK4, which modulates downstream signaling pathways including RhoA. This signaling enhances podocyte motility while suppressing the expression of key slit diaphragm proteins such as nephrin and synaptopodin (62, 131, 132). Collectively, these alterations undermine podocyte structural integrity and barrier function, thereby exacerbating proteinuria. Furthermore, in lupus nephritis patients, IgG is transcytosed into podocytes via FcRn (133), where it not only activates CaMK4 signaling (62, 134) but also induces CD86 expression (113). This upregulation of CD86 enhances podocyte capacity to form immunological synapses with T cells, amplifying local immune activation. Clinical studies further reveal that aberrant glycosylation of IgG in the sera of patients is closely linked to podocyte injury. Such glycosylation-modified IgGs, primarily produced by B cells, exacerbate podocyte dysfunction and contribute to disease progression (57, 62).
Podocyte injury mediated by B cells is not solely dependent on antibodies but can be exacerbated through synergistic interactions with T cells. Specifically, T cells can increase the survival, differentiation, and antibody production of autoreactive B cells (135) and promote inflammation and tissue damage through cytokine secretion. Although podocytes are not conventional antigen-presenting cells, they express MHC class II and costimulatory molecules in lupus nephritis, enabling them to activate CD4+T cells (83, 136). Through such crosstalk with T cells, podocytes can indirectly modulate B cell activation and subsequent antibody production. Dysregulation of T cell function disrupts peripheral tolerance, thereby promoting B cell activation and autoantibody generation. These autoantibodies can either directly target renal structural components or form immune complexes that deposit within the glomeruli, triggering local inflammation and tissue damage (137, 138).
5 Renal tubular epithelial cells
Proximal tubular epithelial cells (PTECs), a metabolically active and highly polarized subset of RTECs, play a central role in maintaining renal function. Responsible for reabsorbing approximately 80% of the glomerular filtrate—including glucose, electrolytes, and amino acids—PTECs are enriched in mitochondria and exhibit significantly higher metabolic demands compared to other renal cell types (139). In addition, they express multiple iron-handling proteins, such as transferrin receptor 1 (TfR1) and divalent metal transporter 1 (DMT1), and contribute to iron homeostasis via active endocytic pathways (140).
While RTECs have traditionally been recognized for their role in solute transport, growing evidence highlights their active involvement in the immunopathogenesis of renal parenchymal diseases (141, 142), particularly in mediating inflammation and fibrosis (143). In LN, the structural and metabolic features of RTECs render them particularly susceptible to immune-mediated injury. Tubulointerstitial fibrosis is a major contributor to LN progression toward ESRD (144), often associated with PTEC-derived pro-inflammatory cytokines that activate immune cells and initiate epithelial-to-mesenchymal transition (EMT) (145). Upon injury, RTECs acquire an inflammatory phenotype characterized by the production of cytokines such as CSF-1, CCL2, IL-6, TNF-α, IL-1β, and IL-18. These mediators amplify immune responses through autocrine signaling and promote leukocyte recruitment by secreting chemokines including CCL2, CCL5, and CXCL8, thereby exacerbating tubulointerstitial inflammation and tissue damage (146). Notably, deposition of immune complexes along the tubular basement membrane—often accompanied by immune cell infiltration and interstitial fibrosis—is a common pathological feature in LN (147), underscoring the immunoregulatory role of RTECs in disease progression.
5.1 Crosstalk between renal tubular epithelial cells and innate immune cells
RTECs play an active role in recruiting and activating innate immune cells, thereby amplifying inflammatory responses within the kidney (Figure 4A). Monocyte chemoattractant protein-1 (MCP-1/CCL2) is a well-established chemokine critical for monocyte recruitment in various inflammatory settings (71). In LN, MCP-1 expression is predominantly localized to the renal tubules rather than the glomeruli (148, 149), and its levels closely correlate with macrophage and T cell infiltration, thereby promoting local inflammation. Osteopontin (OPN), an inflammation-associated glycoprotein abundantly expressed by RTECs in both proximal and distal tubules, exhibits a positive correlation with the extent of monocyte/macrophage infiltration and severity of renal injury. Upregulated OPN expression has been documented across multiple glomerulonephritis models, where it facilitates monocyte adhesion and migration into the tubulointerstitial compartment through interaction with the CD44 receptor (149–151). Both clinical and experimental studies confirm that elevated OPN expression associates with increased tubular monocyte infiltration and tubular damage (152, 153), with significantly higher OPN levels observed in LN patients and murine models (154, 155). Moreover, upon stimulation by proinflammatory cytokines such as TNF-α, RTECs secrete chemerin, which recruits plasmacytoid dendritic cells (pDCs) to sites of inflammation via the ChemR23 receptor, thereby promoting local immune activation (156). RTECs also produce various chemokines that enhance dendritic cell recruitment and accumulation at lesion sites (157). Of particular interest is the infiltration of a distinct myeloid dendritic cell subset—type 3 conventional dendritic cells (DC3s)—within the renal tubulointerstitium. These DC3s are believed to act as intermediaries bridging interactions between intrinsic proximal tubular epithelial cells (iPTECs) and T cells (191). DC3s display high expression of costimulatory molecules such as CD86 and CD40, as well as chemokines including CXCL16 and CCL17, endowing them with potent antigen-presenting capacity. Consequently, they promote T cell polarization toward Th1 and Th17 phenotypes, thereby amplifying local inflammatory responses and ultimately contributing to progressive renal parenchymal injury (158). Beyond classical chemokines, recent evidence indicates that RTECs can indirectly modulate immune cell chemotaxis and activation in response to cytokine stimuli. For example, interleukin-22 (IL-22) has been shown to facilitate macrophage infiltration into the kidney in LN, indirectly exacerbating tubular epithelial cell injury and disease progression (159). In vitro studies demonstrate that recombinant IL-22 stimulation of primary murine renal tubular epithelial cells upregulates the expression of CCL2, CXCL10, and phosphorylated STAT3. Conditioned media from these cells exhibit potent macrophage chemotactic activity, underscoring the role of IL-22 in mediating RTEC-driven recruitment and activation of innate immune cells (159). Furthermore, tubular epithelial cells secrete additional chemokines such as IL-34 (160), CCL2, and CX3CL1 (161–163), which act synergistically to regulate macrophage recruitment and activation within the renal microenvironment.
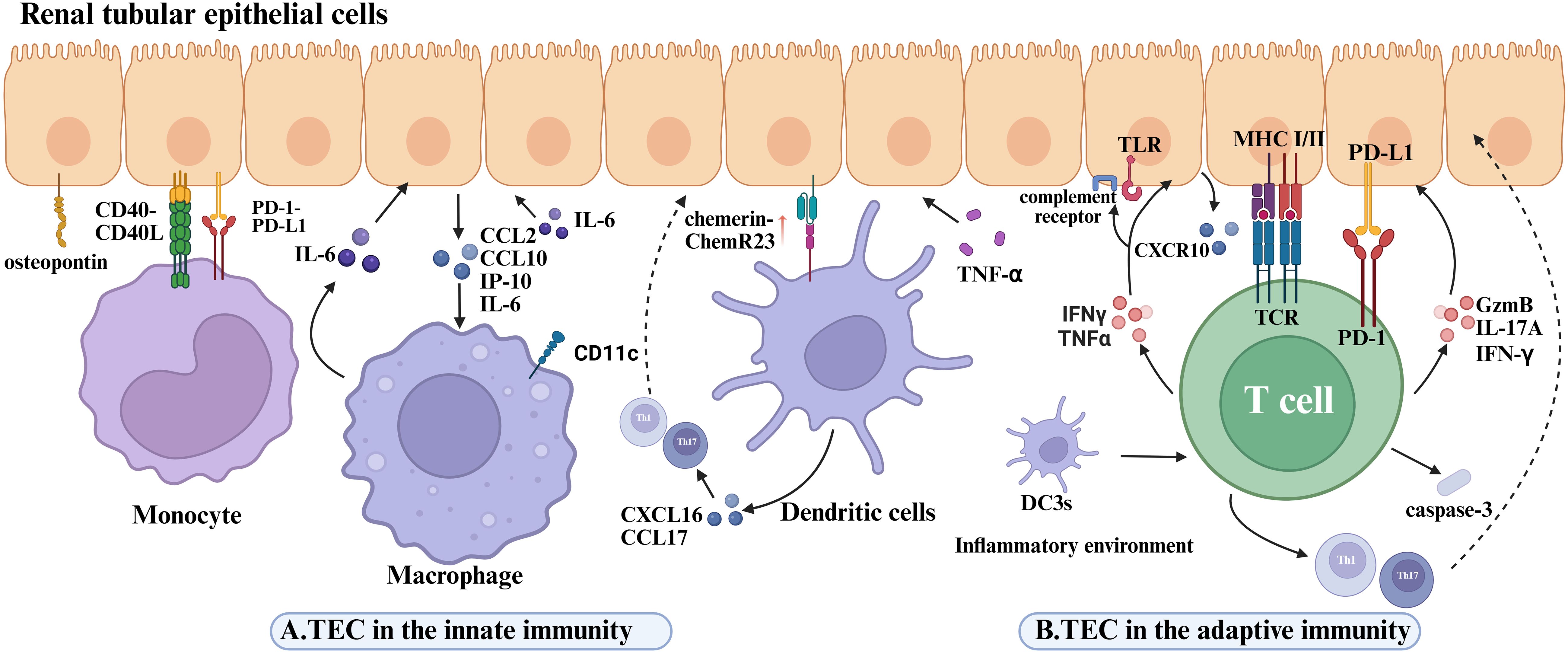
Figure 4. Disease mechanisms mediated by the interaction of renal tubular epithelial cells with immune cells in lupus nephritis. (A) The role of renal tubular epithelial cells in innate immunity. OPN expressed on RTECs is associated with monocyte infiltration and tubular injury. In LN, monocytes interact with RTECs through the CD40–CD40L axis to activate inflammatory pathways, while PD-L1 on RTECs suppresses excessive monocyte activation via PD-1. IL-22 stimulation upregulates CCL2, CXCL10, and pSTAT3 in RTECs. Macrophages are recruited to the tubulointerstitial compartment by CCL2 and CXCL10 secreted by TECs, and their released IL-6 aggravates TEC detachment and apoptosis by inducing fibronectin expression. RTECs recruit pDCs via TNF-α-induced chemerin-ChemR23 axis in LN. The tubulointerstitial DC3 subset expresses high levels of CXCL16 and CCL17, thereby exacerbating RTEC inflammatory injury. (B) The role of renal tubular epithelial cells in adaptive immunity. IFN-γ and TNF-α stimulation upregulate CXCL10 and CXCR3 expression in RTECs. In LN kidneys, damaged iPTECs overexpress proinflammatory mediators, promoting the recruitment of blood-derived DC3 cells to renal tissue. Renal DC3 cells are reprogrammed toward a proinflammatory phenotype within the milieu of tubular injury, driving Th1/Th17 adaptive immune responses and worsening RTEC inflammation. Injured PTECs upregulate MHC class II and costimulatory molecules and activate CD4+T cells through antigen presentation. RTECs also activate CD8+T cells via cross-presentation, inducing the release of GzmB, IL-17A, and IFN-γ. Direct contact between CD8+T cells and RTECs enhances caspase-3–mediated apoptosis and tubulointerstitial inflammation. Overexpression of PD-L1 on RTECs inhibits T-cell activation through PD-1, establishing an immunosuppressive microenvironment that counterbalances inflammatory injury.
Recruited innate immune cells and RTECs engage in bidirectional interactions through both direct contact and soluble mediators, forming an activation loop that perpetuates inflammation and initiates fibrotic processes. Specifically, RTECs interact with monocytes via surface costimulatory molecules such as CD40–CD40L, triggering intrinsic inflammatory signaling pathways within RTECs (164). This crosstalk not only amplifies the local inflammatory milieu but also contributes to tubulointerstitial fibrosis, underpinning the chronic progression of LN. As inflammation persists, RTECs continuously secrete chemokines including MCP-1 and OPN, which enhance the recruitment and accumulation of monocytes, macrophages, and other immune cells at sites of injury. Recruited macrophages, in turn, release IL-6, inducing TECs to upregulate fibronectin expression, thereby accelerating tubular epithelial cell detachment and death (165). This establishes a self-perpetuating positive feedback loop that exacerbates inflammation. Under these inflammatory conditions, TECs also become a primary source of colony-stimulating factor-1 (CSF-1) (166), which promotes macrophage survival, differentiation, and functional polarization, further driving both immune-dependent and independent kidney damage in LN (167). Beyond soluble factors, recent studies highlight that RTECs release functional exosomes to mediate intercellular communication with innate immune cells (168, 169). Zhang et al. (170) demonstrated that activated macrophages secrete exosomes enriched with miR-155, which upon uptake by tubular epithelial cells, target suppressor of cytokine signaling 1 (SOCS-1), a negative regulator of NF-κB signaling, thereby amplifying inflammation and aggravating TEC injury (170). Dual-luciferase reporter assays confirmed SOCS-1 as a direct miR-155 target in these cells (170). Furthermore, in vivo administration of miR-155-rich exosomes into renal tissue significantly worsened tubular injury.
Together, these findings underscore that in LN, RTECs orchestrate immune cell recruitment through multiple chemokines and engage in complex, bidirectional signaling with innate immune cells via costimulatory molecules, exosomes, and pro-inflammatory mediators, collectively amplifying inflammation and promoting tissue damage.
5.2 Crosstalk between renal tubular epithelial cells and adaptive immune cells
RTECs, particularly PTECs, are recognized as non-professional antigen-presenting cells (APCs) (171), capable of presenting antigens to CD4+T cells via MHC-II–restricted pathways (172). Under physiological conditions, MHC-II expression on PTECs is minimal (172–174); however, it is markedly upregulated in inflamed renal tissues (173, 175–177), along with increased expression of costimulatory molecules such as CD80 and CD86 (178–180). These changes collectively facilitate CD4+T cell activation and amplify local immune responses. Additionally, RTECs possess the machinery for antigen cross-presentation, enabling them to process internalized soluble antigens for presentation via MHC-I, thereby activating CD8+T cells and inducing their secretion of IFN-γ, IL-17A, and granzyme B (GzmB).These cytotoxic mediators contribute to RTEC apoptosis and drive tubulointerstitial inflammation (171). In LN murine models, direct contact between CD8+T cells and RTECs has been associated with increased epithelial cell apoptosis and elevated caspase-3 activation, underscoring the pathogenic role of CD8+T cell–mediated cytotoxicity in tubular injury (171). Importantly, RTECs also modulate T cell responses through expression of the immune checkpoint ligand PD-L1. By engaging PD-1 on T cells, PD-L1 transmits inhibitory signals that establish an immunosuppressive microenvironment, partially restraining disease progression in LN (181). However, this protective mechanism may be compromised under inflammatory stimuli such as IFN-γ, which diminishes PD-L1–mediated suppression and leads to heightened T cell activation and exacerbation of immune-mediated injury. This dual function underscores the dynamic role of RTECs in balancing proinflammatory activation and immune suppression (Figure 4B).
B cells play a central pathogenic role in LN. Studies have shown that B cell-deficient lupus-prone mice are protected against nephritis, whereas passive transfer of autoantibodies derived from lupus models into wild-type mice can induce lupus-like kidney disease (182, 183). These findings underscore the critical role of B cells and the autoantibodies they produce in the pathogenesis of LN. B cell activating factor (BAFF) is considered a key cytokine essential for B cell survival and maturation (184). Recognized as a growth and differentiation factor for B cells, BAFF supports the survival of autoreactive B cells and enables them to escape peripheral tolerance (144, 185–187). BAFF is also regarded as a crucial cytokine in LN (144). In LN, BAFF promotes the further differentiation of B cells located in the renal interstitial space of patients (137). Notably, RTECs have been identified as an important source of BAFF (184). In lupus-prone MRL-Faslpr mice and renal biopsy samples from LN patients, tubular expression of BAFF correlates with disease activity (188). Experimental evidence also shows that the interaction between BAFF and its receptor (BAFF-R) induces the production of colony-stimulating factor 1 (CSF-1), which in turn stimulates further expression of BAFF. Additionally, in CSF-1–pretreated RTECs, BAFF stimulation has been shown to enhance cytotoxicity (188). These complex BAFF-dependent signaling pathways in RTECs may therefore contribute to the tubular cell death and atrophy observed in LN (189). Beyond modulating B cell function through BAFF signaling, B cells themselves can regulate the inflammatory response of tubular epithelial cells via co-stimulatory molecule expression. For example, B cell-expressed CD40L can engage CD40 on RTECs and myeloid cells, enhancing the pro-inflammatory activation of these innate cells and further exacerbating inflammation in the interstitial and glomerular microenvironments (164). The CD40/CD40L axis plays a specific role in B cell biology (190), including promoting B cell activation, proliferation, survival, class switching, germinal center formation, and memory B cell development (191). Accordingly, blocking this pathway has been shown to suppress disease progression in rodent models of systemic lupus nephritis with severe impairment of B cell tolerance (192, 193).
Collectively, renal structural cells such as podocytes and tubular epithelial cells function not only as passive targets but also as immunologically active participants within the inflammatory milieu of LN (194).
(A)TEC in the innate immunity. OPN on RTECs correlates with monocyte infiltration and tubular injury. In LN, monocyte-RTEC interactions via CD40-CD40L activate inflammatory pathways; RTEC PD-L1 suppresses monocyte overactivation via PD-1. CD11c+macrophage infiltration correlates with RTEC damage severity; in vitro, rIL-22-stimulated RTECs secrete CCL2/CXCL10/pSTAT3 to recruit macrophages. RTEC-derived CXCL10 recruits CXCR3+CD11c+macrophages, whose IL-6 induces fibronectin-mediated RTEC shedding/apoptosis. Macrophage-driven IL-6 further promotes RTEC apoptosis, amplifying tubular injury. RTECs recruit pDCs via TNF-α-induced chemerin-ChemR23 axis in LN. Tubulointerstitial DC3 subsets express high CXCL16/CCL17 and enhance immune priming.(B)TEC in the adaptive immunity. IFN-γ/TNF-α stimulation upregulates CXCL10 and CXCR3 expression in tubular epithelial cells at both mRNA and protein levels. In LN kidneys, injured iPTECs overexpress proinflammatory mediators, promoting blood-derived DC3 recruitment to renal tissues. Renal DC3s reprogram into proinflammatory phenotypes within the tubular injury microenvironment, driving Th1/Th17 adaptive immunity. Amplified crosstalk between Th1/Th17 and DC3s forms a proinflammatory feedback loop, synergistically aggravating renal parenchymal damage. Injured PTECs upregulate MHC-II and co-stimulatory molecules to activate CD4+T cells via antigen presentation. RTECs activate CD8+T cells through cross-presentation, inducing GzmB, IL-17A, and IFN-γ release. Direct CD8+T cell-RTEC contact enhances caspase-3-mediated apoptosis and tubulointerstitial inflammation.PD-L1 overexpression on RTECs suppresses T cell activation via PD-1, establishing an immunosuppressive microenvironment that counterbalances inflammatory injury.
6 New therapeutic targets and intervention strategies
6.1 Targeting renal epithelial cells
6.1.1 Podocytes
Podocyte injury is a central pathological event in LN that leads to glomerular filtration barrier disruption and proteinuria (195). In recent years, multiple studies have identified several key signaling pathways and inflammatory mechanisms that regulate podocyte function, suggesting these as important targets for therapeutic intervention in LN.
A20–UCH-L1–NF-κB axis. A20, also known as tumor necrosis factor alpha-induced protein 3 (TNFAIP3), is a cytoplasmic protein that functions by inhibiting inflammation and immune responses.UCH-L1, a member of the deubiquitinating enzyme family, can catalyze the hydrolysis of Lys48-linked ubiquitin chains (196), and its expression is significantly upregulated in LN podocytes (197), resulting in podocyte injury. A20 maintains podocyte structural integrity and alleviates LN progression by suppressing NF-κB signaling, downregulating UCH-L1 expression, and reducing ubiquitin accumulation (198).
Notch1–NLRP3 pathway. Notch1 signaling is abnormally activated in LN podocytes and can induce NLRP3 inflammasome activation, triggering the release of proinflammatory cytokines and cellular injury. The γ-secretase inhibitor DAPT can effectively suppress NLRP3 activation by blocking the Notch1 pathway (195), thereby improving tissue pathology, suggesting this axis as a potential therapeutic target. Considering the complexity of intracellular signaling networks, targeting upstream regulators of inflammasome activation may represent a more effective strategy to prevent podocyte injury in LN (195). Nevertheless, the study has notable limitations, particularly the absence of validation using podocyte-specific conditional knockout models (195). Thus, the proposed mechanism warrants further investigation in rigorous animal models and clinical settings.
miR-155–SOCS1–JAK1/STAT1 pathway. In both LN patients and animal models, miR-155 is significantly upregulated and positively correlates with disease activity.SOCS1 is an important negative feedback regulator in the JAK/STAT signaling pathway, modulating inflammatory responses by inhibiting JAK1 activity and regulating STAT1 phosphorylation (199).Studies have shown that miR-155 promotes inflammatory signaling by downregulating SOCS1, thereby relieving its inhibition of the JAK1/STAT1 pathway, which enhances M1 macrophage polarization and indirectly exacerbates podocyte injury. In vivo experiments confirm that silencing miR-155 significantly reduces the proportion of M1 macrophages and alleviates podocyte structural damage and renal inflammation. In vitro studies further demonstrate that miR-155 overexpression not only promotes M1 polarization but also directly induces podocyte apoptosis (200). These findings suggest that miR-155 plays a critical role in podocyte injury and immune dysregulation by modulating the SOCS1/JAK1–STAT1 pathway, offering a novel molecular target for LN therapy (200). Although these findings provide a scientific rationale for targeting miR-155, large-scale clinical investigations remain scarce. Future multicenter clinical trials are warranted to validate the translational potential of this pathway in LN management (200).
NLRP3 Inflammasome. The NLRP3 (NOD-, LRR-, and pyrin domain–containing protein 3) inflammasome, a member of the NOD-like receptor (NLR) family, plays a pivotal role in sterile inflammation (201, 202). In LN, aberrant activation of NLRP3 has been identified in both podocytes and macrophages, correlating strongly with disease activity (203). Excessive activation of the NLRP3 inflammasome promotes the release of proinflammatory cytokines such as IL-1β and IL-18, thereby amplifying local glomerular inflammation, accelerating renal fibrosis, and contributing to podocyte injury (204).
In podocytes, activation of the NLRP3 inflammasome suppresses the expression of the key slit diaphragm protein nephrin, thereby disrupting the filtration barrier and inducing proteinuria. Experimental studies demonstrated that in LN patients and lupus-prone mouse models, the selective NLRP3 inhibitor MCC950 effectively ameliorated proteinuria, renal histopathological injury, and podocyte foot process effacement (95), underscoring its therapeutic potential in podocyte protection. Moreover, fibroblast growth factor 21 (FGF21) restored podocyte function by upregulating Irgm1, inhibiting NLRP3 inflammasome activity, and reducing the expression of pro-inflammatory mediators such as IL-1β and Caspase-1 (205). Emerging evidence also suggests that metabolic regulation may exert renoprotective effects through modulation of the NLRP3 pathway. In renal tissues from LN patients and nephritic MRL/lpr mice, the sodium-glucose cotransporter 2 (SGLT2) inhibitor empagliflozin attenuated proteinuria by enhancing autophagy to preserve cellular homeostasis and suppressing NLRP3 inflammasome activation, highlighting the need for further investigation into the renoprotective mechanisms of SGLT2 inhibitors in LN (206). Recent clinical trials(NCT05748925)further demonstrated that the addition of empagliflozin to standard therapy significantly reduced proteinuria in LN patients, suggesting its clinical potential (207). Thus, large-scale clinical trials are warranted to validate the renoprotective role of SGLT2 inhibitors in LN. Collectively, both direct and indirect NLRP3 inhibitors hold promise as future therapeutic strategies for LN; however, current evidence remains scarce and is largely limited to animal models. Beyond pharmacological interventions, gene-editing technologies also offer novel therapeutic avenues (208). A recent study by Xu et al. employed CRISPR/Cas9, a third-generation gene-editing tool, to directly disrupt NLRP3 in macrophages, thereby ameliorating various inflammatory conditions. Deletion of NLRP3 inhibited inflammasome activation in vitro and in vivo, demonstrating therapeutic promise for NLRP3-dependent inflammatory diseases (209).
6.1.2 Renal tubular epithelial cells
In LN, RTECs serve not only as targets of immune-mediated injury but also as active contributors to the amplification of inflammation and the progression of fibrosis. Although glomerular lesions have been widely investigated, tubulointerstitial damage—more strongly correlated with adverse clinical outcomes—has historically received insufficient attention (210). Through a variety of signaling pathways, RTECs orchestrate local inflammatory cascades and have emerged as promising targets for therapeutic intervention.
Interferon Signaling and the Immunoproteasome. RTECs are highly responsive to IFN-α signaling, which promotes antigen presentation, immune activation, and inflammatory cytokine release (211). Activation of this pathway induces the expression of immunoproteasome subunits, thereby intensifying tubulointerstitial inflammation. Notably, inhibition of the type I interferon axis or its downstream immunoproteasome components has been shown to significantly mitigate tubular injury in experimental LN models (211).
mTOR Signaling Pathway. The mammalian target of rapamycin (mTOR) pathway is a central regulator of cell growth, metabolism, and immune equilibrium, comprising two functionally distinct complexes: mTOR complex 1 (mTORC1) and mTOR complex 2 (mTORC2) (212). Among them, mTORC1 drives tubulointerstitial remodeling by modulating cellular proliferation and protein biosynthesis and is increasingly recognized as a critical molecular mechanism underlying both SLE and its renal manifestation, LN (213). In LN patients, RTECs display persistent activation of both mTORC1 and mTORC2, with aberrant mTORC1 activation strongly linked to tubular injury and inflammatory amplification. Pharmacological inhibition of mTORC1 with rapamycin effectively suppresses this signaling pathway, reduces immune complex accumulation, and ameliorates tubular damage, offering a promising alternative for LN patients refractory to standard therapies (100). Notably, rapamycin, a selective mTORC1 inhibitor, effectively suppresses pathway activity, reduces renal immune complex deposition, alleviates tubular injury, and ameliorates disease manifestations while prolonging survival in lupus-prone mice (209, 214, 215). Furthermore, clinical studies have shown that long-term rapamycin treatment demonstrates acceptable tolerability and therapeutic efficacy in some patients with proliferative LN (100, 216), thereby highlighting mTORC1 as a promising target for the development of novel therapeutic strategies.
Vitamin D Receptor (VDR)–NLRP3 Inflammasome Axis. The vitamin D receptor (VDR) signaling pathway plays a multifaceted immunoregulatory role in controlling inflammation, including suppression of NF-κB activation, enhancement of anti-inflammatory cytokine production, and regulation of T cell differentiation (217, 218). In LN, VDR expression is markedly reduced in renal tissue and inversely correlates with disease activity and severity, highlighting its potential protective role (219). The VDR agonist paricalcitol mitigates tubulointerstitial injury through inhibition of NF-κB–driven NLRP3 inflammasome activation and attenuation of renal tubular epithelial cell (RTEC) apoptosis (220). These findings not only underscore the anti-inflammatory effects of VDR in LN but also highlight its potential as a therapeutic target. Mechanistically, nuclear-localized VDR can directly interact with NLRP3, thereby interfering with inflammasome assembly. Notably, NLRP3 activation is a critical mediator of RTEC pyroptosis, and its inhibition contributes to the preservation of tubular epithelial homeostasis. Similarly, the natural compound piperine has been reported to significantly attenuate RTEC pyroptosis and renal tissue injury through blockade of NLRP3 activation, offering a promising therapeutic strategy for LN management (221).
TGF-β–Senescence and Fibrosis Pathway. Transforming growth factor-β (TGF-β) promotes tubulointerstitial fibrosis in LN by inducing RTEC senescence and activating fibroblasts (222). One of its mechanisms is upregulation of the cyclin-dependent kinase inhibitor p15INK4B, which induces G1 phase cell cycle arrest, thereby inhibiting cell proliferation and driving RTECs into a senescent state. In addition, TGF-β can induce senescence-related phenotypes in various cell types, thereby contributing to persistent inflammation and tissue remodeling. TGF-β induces or accelerates cellular senescence and associated phenotypes by upregulating p15INK4B and causing G1 cell cycle arrest (186, 223).
Fisetin (3,3′,4′,7-tetrahydroxyflavone) is a natural flavonoid senolytic agent found in various fruits and vegetables (224), and has been shown to effectively clear senescent cells (225, 226). It alleviates chronic inflammation and fibrosis by inducing apoptosis in senescent RTECs (224, 227, 228). Further studies have demonstrated that fisetin selectively eliminates senescent RTECs and attenuates TGF-β–driven interstitial fibrosis via inhibition of anti-apoptotic signaling pathways such as PI3K/AKT/mTOR, in a Smad-independent manner. These findings suggest that TGF-β–induced RTEC senescence plays a key role in LN-associated fibrosis, and senolytic therapies represented by fisetin may serve as a potential intervention to delay structural kidney damage (222). Notably, the PI3K/AKT/mTOR signaling pathway functions not only as a downstream effector of fisetin but also as a pivotal driver of LN pathogenesis in murine models. Aberrant activation of this pathway amplifies inflammatory and fibrotic responses. Thus, assessing PI3K/AKT/mTOR activation may yield novel insights into disease mechanisms and facilitate the development of more personalized and less toxic therapeutic strategies for LN (209).
6.2 Targeting immune cells
Renal epithelial cells are primary targets of immune-mediated injury in LN. Additionally, interactions between podocytes and infiltrating immune cells aggravate tissue damage, highlighting immune cells themselves as critical therapeutic targets.
6.2.1 T cells
T cells play a pivotal immunoregulatory role in LN pathogenesis and represent a major focus in the development of targeted therapies. While conventional treatment approaches—including nonsteroidal anti-inflammatory drugs, glucocorticoids, and immunosuppressants (229)—remain the standard of care, their considerable toxicity and high relapse rates have driven efforts to develop more selective and less toxic immunomodulatory strategies (230).
Among numerous potential therapeutic strategies, the immunomodulatory properties of natural products have garnered significant attention. Cordyceps sinensis polysaccharide (WCP), a bioactive complex derived from the parasitic relationship between Cordyceps sinensis fungus and Lepidoptera larvae, has been shown to exert immunoregulatory effects. Previous studies indicate that Cordyceps sinensis possesses therapeutic efficacy in LN by modulating immune responses (231). Mechanistically, WCP inhibits key signaling pathways including IL-12–STAT4, IFN-γ–STAT1, and PI3K–AKT, thereby blocking Th1 cell differentiation and attenuating inflammation. Concurrently, WCP suppresses the TLR4–MyD88–MAPK signaling cascade, leading to decreased chemokine expression and reduced T cell recruitment into the kidney, ultimately conferring renal protection (232).
In addition to Th1 cells, Th17 cells are critically involved in the pathogenesis of LN. Th17-derived IL-17 activates multiple pro-inflammatory and pro-fibrotic pathways, contributing to renal dysfunction and disease progression. Therapeutic approaches targeting the Th17 axis are rapidly expanding. For instance, CaMK4 inhibitors (e.g., KN-93) can restore the Treg/Th17 balance, reduce IL-17 secretion, and improve renal function, as evidenced by reduced proteinuria (36), thereby emerging as a potential therapeutic strategy in LN. Moreover, monoclonal antibodies against IL-17A (e.g., secukinumab) or RORγt inhibitors (e.g., α-mangostin) suppress IL-17 signaling and alleviate T cell–mediated renal injury. These therapeutic approaches are currently under clinical investigation to assess their efficacy, safety, and tolerability in patients with active lupus nephritis (92). The dysregulation of the Treg/Th17 balance is a key mechanism underlying LN development. Tregs are essential for maintaining immune tolerance and suppressing autoimmunity, while Th17 cells contribute to inflammation and fibrosis through IL-17 secretion (233, 234). Multiple studies have reported a common Treg/Th17 imbalance in LN patients. Low-dose interleukin-2 (IL-2) therapy selectively expands Treg populations, significantly ameliorating renal pathology and inducing disease remission, with encouraging results from several clinical trials (233, 234). Additionally, novel chimeric antigen receptor regulatory T cell (CAR-Treg) therapies are under investigation to enhance Treg function and restore immune homeostasis, offering promising precision immunotherapeutic options for LN (235). Meanwhile, mesenchymal stem cells (MSCs), known for their dual roles in immunomodulation and tissue repair, represent another promising strategy for T cell-targeted treatment. Studies demonstrate that transplantation of umbilical cord-derived MSCs can increase Treg numbers, suppress Th17 responses (236–238), and modulate the balance of TGF-β and TNF-α, thereby improving the inflammatory microenvironment within the kidney.
Beyond the development of novel therapies, optimizing existing drugs offers additional strategies for T cell-targeted treatment. Voclosporin (VOC), a next-generation calcineurin inhibitor, reduces proteinuria by inhibiting T cell activation and, in part, through non-immune mechanisms. In phase III clinical trials(NCT02141672), the combination of VOC with mycophenolate mofetil (MMF) and low-dose glucocorticoids (GC) achieved superior renal response rates and facilitated glucocorticoid dose reduction, leading to its approval by the FDA as the first oral therapy for lupus nephritis (14, 239, 240). Interleukin-6 (IL-6), a critical mediator of T cell activation and pro-inflammatory responses, also plays a pivotal role in LN pathogenesis. Elevated IL-6 levels in systemic lupus erythematosus patients have been associated with increased disease activity (241). Tocilizumab, a humanized monoclonal antibody targeting the IL-6 receptor, significantly reduces CD4+T cell activation (242) and modulates multiple immune pathways involved in LN pathology. This agent is emerging as a valuable adjunct to T cell-directed therapies.
6.2.2 B cells
B cells are central contributors to the pathogenesis of LN and constitute a key therapeutic target. Their survival and maturation rely on signaling mediated by surface molecules such as BAFF, CD19, and CD20 (243), making these molecules attractive targets for monoclonal antibody–based therapies.
Rituximab is a classic Type I anti-CD20 monoclonal antibody (RTX) that reduces the generation of autoantibodies by depleting CD20+B cells, thereby inhibiting immune complex-mediated renal injury (39, 244). In vitro studies have demonstrated that RTX exerts its effects through four distinct mechanisms: in the presence of FcγR-bearing cells, it induces apoptosis, complement-dependent cytotoxicity (CDC), antibody-dependent cellular cytotoxicity (ADCC), and antibody-dependent cellular phagocytosis (ADCP) (245–247). However, these findings have not convinced all researchers, prompting the re-assessment of RTX therapy (NCT01773616) in the more controlled, randomized RITUXILUP study, which investigated rituximab and mycophenolate mofetil without oral steroids for lupus nephritis treatment. Furthermore, observational studies and real-world data have shown promising results in refractory or relapsing LN patients, with an overall response rate of 50%-80%. Based on this evidence, the KDIGO 2024 guidelines have recommended rituximab as an option for patients with insufficient response to initial treatment, rather than as a first-line therapy (240). Obinutuzumab, a second-generation CD20 antibody, has a modified Fc region with enhanced glycosylation, increasing its affinity for FcγRIII and significantly improving ADCC and ADCP effects (248, 249). In refractory LN, obinutuzumab has demonstrated superior B-cell depletion efficacy and higher clinical remission rates (250). Recently, in a phase II, double-blind, randomized controlled trial (NCT02550652), obinutuzumab, in combination with mycophenolate mofetil and corticosteroids, showed superior outcomes compared to placebo (39). Moreover, obinutuzumab has shown favorable safety, with guidelines suggesting that it may overcome some limitations of rituximab by providing more effective and durable B-cell depletion. However, the long-term efficacy and safety of obinutuzumab require further validation through phase III clinical trials to determine its precise role in the therapeutic landscape of lupus nephritis (240).
BAFF, a member of the TNF superfamily secreted by myeloid cells, facilitates the transition of immature to mature B cells and promotes plasma cell survival and sustained autoantibody production (251). Belimumab, a humanized IgG1λ monoclonal antibody, selectively neutralizes soluble BAFF and blocks receptor engagement, thereby reducing CD20+B cells and plasma cells, leading to diminished autoantibody titers (39). In the phase III BLISS-LN trial (NCT01639339), the addition of belimumab to standard therapy significantly increased the proportion of patients achieving primary renal efficacy response at two years compared with placebo plus standard therapy. Multiple clinical trials have demonstrated that belimumab confers significant clinical benefits in LN, including higher remission rates, delayed progression of renal dysfunction, and reduced relapse rates, while maintaining a favorable safety profile. On this basis, the KDIGO 2024 guidelines recommend belimumab as a first-line therapeutic option (240). Its efficacy is especially pronounced in patients receiving concomitant MMF therapy (240).
Additionally, phosphoinositide 3-kinase alpha (PI3Kα), a lipid kinase expressed in multiple tissues, plays a crucial role in B cell activation, metabolism, and migration (252). Pharmacological inhibition of PI3Kα has been shown to suppress proinflammatory cytokine secretion, reduce B cell–mediated immune responses, attenuate autoantibody production, and mitigate glomerular complement deposition (253). These findings highlight PI3Kα as a promising therapeutic target in LN.
6.2.3 Therapeutic targeting of costimulatory pathways
Effective T cell activation requires not only antigen recognition via the MHC–antigen complex (signal one) but also a second, costimulatory signal. Costimulatory molecules CD80 and CD86 on APCs or B cells engage CD28 on naïve T cells, promoting their activation and clonal expansion. Cytotoxic T lymphocyte–associated antigen 4 (CTLA4), expressed on activated T cells, competes with CD28 for binding to CD80/CD86, thereby dampening the T cell response. Abatacept, a CTLA4–Ig fusion protein, acts as a selective costimulatory modulator by binding CD80/CD86 and inhibiting CD28-mediated T cell activation (14).
Another critical costimulatory pathway involves CD40 and its ligand CD40L. CD40L is predominantly expressed on activated T cells, while CD40 is present on B cells, dendritic cells, and intrinsic renal cells such as proximal tubular epithelial cells (254, 255). Activation of this axis facilitates autoantibody production, promotes their deposition in renal tissue, and amplifies local inflammation through enhanced B cell expansion and activation of myeloid and epithelial cells. These effects collectively exacerbate glomerular and tubulointerstitial injury in LN (164). Preclinical studies have shown marked upregulation of CD40 expression in the kidneys of LN models, and blockade of the CD40–CD40L interaction significantly attenuates renal inflammation and immunopathology (164). Collectively, these findings underscore the therapeutic potential of costimulatory blockade in LN. Targeting early T cell–costimulatory interactions offers a promising strategy to suppress aberrant immune activation and prevent immune-mediated renal damage.
7 Future perspectives
Although emerging therapies demonstrate notable short-term benefits and steroid-sparing effects, their long-term safety remains to be carefully assessed. For instance, voclosporin (VOC) may aggravate hypertension and reduce glomerular filtration rate (GFR), whereas belimumab has been associated with neuropsychiatric adverse events such as insomnia and anxiety (256–259). Similarly, the risk of chronic nephrotoxicity from calcineurin inhibitors (CNIs) and immunosuppression-related infections induced by biologics highlights the necessity of continuous monitoring of long-term safety profiles (260–263). These challenges underscore the urgent need to move toward precision and individualized therapeutic strategies. By integrating molecular subtyping and biomarkers (e.g., anti-dsDNA antibodies and renal transcriptomic signatures) with artificial intelligence–based algorithms, it may become possible to more accurately stratify patients and optimize therapeutic decision-making (264). In parallel, emerging technologies are opening new avenues for mechanistic exploration. Single-cell RNA sequencing enables the mapping of interaction networks between immune cells and renal epithelial cells, while urinary proteomics provides promising opportunities for noninvasive disease monitoring and patient stratification (42). Building upon these advances, multitarget combination strategies may represent a pivotal approach to balancing efficacy and safety. Combinations such as belimumab with VOC, or with complement inhibitors, hold potential to broaden the therapeutic landscape (265). Collectively, these developments not only address the limitations of single-target therapies but also pave the way for transitioning lupus nephritis management from conventional immunosuppression toward precision immunomodulation.
8 Conclusion
LN represents a severe manifestation of systemic lupus erythematosus, wherein intricate crosstalk between renal epithelial cells and immune cells plays a pivotal role in disease pathogenesis. Podocytes, as integral components of the glomerular filtration barrier, are susceptible to injury by autoantibodies, immune complexes, and inflammatory mediators. Beyond serving as passive targets, podocytes actively participate in immune regulation by expressing molecules such as MHC and costimulatory proteins, thereby contributing to antigen presentation and activation of T and B lymphocytes, further amplifying local immune responses and tissue damage. RTECs, similarly, are not merely victims of immune attack. They actively secrete cytokines and chemokines that recruit and modulate immune cells and undergo EMT, promoting tubulointerstitial fibrosis. On the immune side, dysregulation of T cell subsets—particularly Th17 cells—drives podocyte injury via proinflammatory cytokines, while antigen presentation interactions between T cells and RTECs exacerbate inflammation. B cells contribute through the production of pathogenic autoantibodies and engage in direct crosstalk with RTECs to potentiate immune-mediated injury. Innate immune cells, including macrophages, dendritic cells, and neutrophils, further aggravate renal damage through cytokine release, antigen presentation, and oxidative stress. These cell populations form a complex and dynamic communication network, mediated by cytokines, chemokines, and cell-surface interactions. Elucidating these intercellular mechanisms is essential for identifying novel therapeutic targets and developing more precise and effective treatment strategies aimed at improving long-term outcomes in patients with LN.
Author contributions
JC: Writing – original draft. ZC: Writing – original draft. XM: Writing – review & editing. KR: Funding acquisition, Writing – review & editing. JT: Conceptualization, Funding acquisition, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This work was supported by the National Natural Science Foundation of China (Grant Nos.82171771, 82271854), the Jiangsu Provincial Key Research and Development Program (Grant number BE2023758), Major Project of Basic Science Research in Higher Education Institutions of Jiangsu Province (23KJA320001), Jiangsu Association for Science and Technology's Young Talents Nurturing Program (TJ-2023-027), Postgraduate Research & Practice Innovation Program of Jiangsu Province (KYCX24_4032). Figures were created with BioRender.com.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kiriakidou M and Ching CL. Systemic lupus erythematosus. Ann Intern Med. (2020) 172:Itc81–itc96. doi: 10.7326/AITC202006020
2. Borchers AT, Naguwa SM, Shoenfeld Y, and Gershwin ME. The geoepidemiology of systemic lupus erythematosus. Autoimmun Rev. (2010) 9:A277–87. doi: 10.1016/j.autrev.2009.12.008
3. Stojan G and Petri M. Epidemiology of systemic lupus erythematosus: an update. Curr Opin Rheumatol. (2018) 30:144–50. doi: 10.1097/BOR.0000000000000480
4. Liu R, Wen X, Peng X, Zhao M, Mi L, Lei J, et al. Immune podocytes in the immune microenvironment of lupus nephritis (Review). Mol Med Rep. (2023) 28(5):204. doi: 10.3892/mmr.2023.13091
5. Zhang L, Qing P, Yang H, Wu Y, Liu Y, and Luo Y. Gut microbiome and metabolites in systemic lupus erythematosus: link, mechanisms and intervention. Front Immunol. (2021) 12:686501. doi: 10.3389/fimmu.2021.686501
6. Van Bavel CC, Fenton KA, Rekvig OP, Van der Vlag J, and Berden JH. Glomerular targets of nephritogenic autoantibodies in systemic lupus erythematosus. Arthritis Rheum. (2008) 58:1892–9. doi: 10.1002/art.23626
7. Schwartz N, Goilav B, and Putterman C. The pathogenesis, diagnosis and treatment of lupus nephritis. Curr Opin Rheumatol. (2014) 26:502–9. doi: 10.1097/BOR.0000000000000089
8. Davidson A. What is damaging the kidney in lupus nephritis? Nat Rev Rheumatol. (2016) 12:143–53. doi: 10.1038/nrrheum.2015.159
9. Hanly JG, O'Keeffe AG, Su L, Urowitz MB, Romero-Diaz J, Gordon C, et al. The frequency and outcome of lupus nephritis: results from an international inception cohort study. Rheumatol (Oxford). (2016) 55:252–62. doi: 10.1093/rheumatology/kev311
10. Parks CG, D’Aloisio AA, and Sandler DP. Early life factors associated with adult-onset systemic lupus erythematosus in women. Front Immunol. (2016) 7:103. doi: 10.3389/fimmu.2016.00103
11. Hoover PJ and Costenbader KH. Insights into the epidemiology and management of lupus nephritis from the US rheumatologist’s perspective. Kidney Int. (2016) 90:487–92. doi: 10.1016/j.kint.2016.03.042
12. Pons-Estel GJ, Serrano R, Plasín MA, Espinosa G, and Cervera R. Epidemiology and management of refractory lupus nephritis. Autoimmun Rev. (2011) 10:655–63. doi: 10.1016/j.autrev.2011.04.032
13. Cervera R, Khamashta MA, Font J, Sebastiani GD, Gil A, Lavilla P, et al. Morbidity and mortality in systemic lupus erythematosus during a 10-year period: a comparison of early and late manifestations in a cohort of 1,000 patients. Med (Baltimore). (2003) 82:299–308. doi: 10.1097/01.md.0000091181.93122.55
14. Yu C, Li P, Dang X, Zhang X, Mao Y, and Chen X. Lupus nephritis: new progress in diagnosis and treatment. J Autoimmun. (2022) 132:102871. doi: 10.1016/j.jaut.2022.102871
15. Murtagh FE, Addington-Hall J, and Higginson IJ. The prevalence of symptoms in end-stage renal disease: a systematic review. Adv Chronic Kidney Dis. (2007) 14:82–99. doi: 10.1053/j.ackd.2006.10.001
16. Davison SN and Jhangri GS. Impact of pain and symptom burden on the health-related quality of life of hemodialysis patients. J Pain Symptom Manage. (2010) 39:477–85. doi: 10.1016/j.jpainsymman.2009.08.008
17. Tsay SL and Healstead M. Self-care self-efficacy, depression, and quality of life among patients receiving hemodialysis in Taiwan. Int J Nurs Stud. (2002) 39:245–51. doi: 10.1016/S0020-7489(01)00030-X
18. Levy N, Cheung W, McDonald H, Banez MC, Shang J, Stone PW, et al. Symptom management in Chinese adults with end stage renal disease (ESRD). Appl Nurs Res. (2022) 64:151549. doi: 10.1016/j.apnr.2021.151549
19. Saran R, Robinson B, Abbott KC, Agodoa LY, Albertus P, Ayanian J, et al. US renal data system 2016 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis. (2017) 69:A7–a8. doi: 10.1053/j.ajkd.2017.01.036
20. Seligman VA, Lum RF, Olson JL, Li H, and Criswell LA. Demographic differences in the development of lupus nephritis: a retrospective analysis. Am J Med. (2002) 112:726–9. doi: 10.1016/S0002-9343(02)01118-X
21. Bastian HM, Roseman JM, McGwin G, Jr., Alarcón GS, Friedman AW, Fessler BJ, et al. Systemic lupus erythematosus in three ethnic groups. XII. Risk factors for lupus nephritis after diagnosis. Lupus. (2002) 11:152–60. doi: 10.1191/0961203302lu158oa
22. Feldman CH, Hiraki LT, Liu J, Fischer MA, Solomon DH, Alarcón GS, et al. Epidemiology and sociodemographics of systemic lupus erythematosus and lupus nephritis among US adults with Medicaid coverage, 2000–2004. Arthritis Rheum. (2013) 65:753–63. doi: 10.1002/art.37795
23. Jakes RW, Bae SC, Louthrenoo W, Mok CC, Navarra SV, and Kwon N. Systematic review of the epidemiology of systemic lupus erythematosus in the Asia-Pacific region: prevalence, incidence, clinical features, and mortality. Arthritis Care Res (Hoboken). (2012) 64:159–68. doi: 10.1002/acr.20683
24. Maningding E, Dall'Era M, Trupin L, Murphy LB, and Yazdany J. Racial and ethnic differences in the prevalence and time to onset of manifestations of systemic lupus erythematosus: the california lupus surveillance project. Arthritis Care Res (Hoboken). (2020) 72:622–9. doi: 10.1002/acr.23887
25. Anders HJ, Saxena R, Zhao MH, Parodis I, Salmon JE, and Mohan C. Lupus nephritis. Nat Rev Dis Primers. (2020) 6:7. doi: 10.1038/s41572-019-0141-9
26. Garcia MA, Marcos JC, Marcos AI, Pons-Estel BA, Wojdyla D, Arturi A, et al. Male systemic lupus erythematosus in a Latin-American inception cohort of 1214 patients. Lupus. (2005) 14:938–46. doi: 10.1191/0961203305lu2245oa
27. Chang DM, Chang CC, Kuo SY, Chu SJ, and Chang ML. The clinical features and prognosis of male lupus in Taiwan. Lupus. (1998) 7:462–8. doi: 10.1191/096120398678920479
28. Mok CC, Lau CS, Chan TM, and Wong RW. Clinical characteristics and outcome of southern Chinese males with systemic lupus erythematosus. Lupus. (1999) 8:188–96. doi: 10.1191/096120399678847605
29. Andrade RM, Alarcón GS, Fernández M, Apte M, Vilá LM, and Reveille JD. Accelerated damage accrual among men with systemic lupus erythematosus: XLIV. Results from a multiethnic US cohort. Arthritis Rheum. (2007) 56:622–30. doi: 10.1002/art.22375
30. Stefanidou S, Benos A, Galanopoulou V, Chatziyannis I, Kanakoudi F, Aslanidis S, et al. Clinical expression and morbidity of systemic lupus erythematosus during a post-diagnostic 5-year follow-up: a male:female comparison. Lupus. (2011) 20:1090–4. doi: 10.1177/0961203311403640
31. Carreño L, López-Longo FJ, Monteagudo I, Rodríguez-Mahou M, Bascones M, González CM, et al. Immunological and clinical differences between juvenile and adult onset of systemic lupus erythematosus. Lupus. (1999) 8:287–92. doi: 10.1191/096120399678847786
32. Bader-Meunier B, Armengaud JB, Haddad E, Salomon R, Deschênes G, Koné-Paut I, et al. Initial presentation of childhood-onset systemic lupus erythematosus: a French multicenter study. J Pediatr. (2005) 146:648–53. doi: 10.1016/j.jpeds.2004.12.045
33. Ramírez Gómez LA, Uribe Uribe O, Osio Uribe O, Grisales Romero H, Cardiel MH, Wojdyla D, et al. Childhood systemic lupus erythematosus in Latin America. The GLADEL experience in 230 children. Lupus. (2008) 17:596–604. doi: 10.1177/0961203307088006
34. Hoffman IE, Lauwerys BR, De Keyser F, Huizinga TW, Isenberg D, Cebecauer L, et al. Juvenile-onset systemic lupus erythematosus: different clinical and serological pattern than adult-onset systemic lupus erythematosus. Ann Rheum Dis. (2009) 68:412–5. doi: 10.1136/ard.2008.094813
35. Zhou XJ, Klionsky DJ, and Zhang H. Podocytes and autophagy: a potential therapeutic target in lupus nephritis. Autophagy. (2019) 15:908–12. doi: 10.1080/15548627.2019.1580512
36. Ferretti AP, Bhargava R, Dahan S, Tsokos MG, and Tsokos GC. Calcium/calmodulin kinase IV controls the function of both T cells and kidney resident cells. Front Immunol. (2018) 9:2113. doi: 10.3389/fimmu.2018.02113
37. Zhang C, Boini KM, Xia M, Abais JM, Li X, Liu Q, et al. Activation of Nod-like receptor protein 3 inflammasomes turns on podocyte injury and glomerular sclerosis in hyperhomocysteinemia. Hypertension. (2012) 60:154–62. doi: 10.1161/HYPERTENSIONAHA.111.189688
38. Yung S, Tsang RC, Sun Y, Leung JK, and Chan TM. Effect of human anti-DNA antibodies on proximal renal tubular epithelial cell cytokine expression: implications on tubulointerstitial inflammation in lupus nephritis. J Am Soc Nephrol. (2005) 16:3281–94. doi: 10.1681/ASN.2004110917
39. Frangou E, Georgakis S, and Bertsias G. Update on the cellular and molecular aspects of lupus nephritis. Clin Immunol. (2020) 216:108445. doi: 10.1016/j.clim.2020.108445
40. Chernova I. Lupus nephritis: immune cells and the kidney microenvironment. Kidney360. (2024) 5:1394–401. doi: 10.34067/KID.0000000000000531
41. Rovin BH and Parikh SV. Lupus nephritis: the evolving role of novel therapeutics. Am J Kidney Dis. (2014) 63:677–90. doi: 10.1053/j.ajkd.2013.11.023
42. Ichinose K. The role of podocytes in lupus nephritis: Insights and implications. Clin Immunol. (2024) 262:110180. doi: 10.1016/j.clim.2024.110180
43. Sakhi H, Moktefi A, Bouachi K, Audard V, Hénique C, Remy P, et al. Podocyte injury in lupus nephritis. J Clin Med. (2019) 8(9):1340. doi: 10.3390/jcm8091340
44. Nagata M. Podocyte injury and its consequences. Kidney Int. (2016) 89:1221–30. doi: 10.1016/j.kint.2016.01.012
45. D’Agati VD, Kaskel FJ, and Falk RJ. Focal segmental glomerulosclerosis. N Engl J Med. (2011) 365:2398–411. doi: 10.1056/NEJMra1106556
46. Bhargava R, Upadhyay R, Zhao C, Katakam P, Wenderfer S, Chen J, et al. Aberrant glycosylation of igG in children with active lupus nephritis alters podocyte metabolism and causes podocyte injury. Arthritis Rheumatol. (2025) 77(10):1421–32. doi: 10.1002/art.43200
48. Grahammer F, Schell C, and Huber TB. The podocyte slit diaphragm–from a thin grey line to a complex signalling hub. Nat Rev Nephrol. (2013) 9:587–98. doi: 10.1038/nrneph.2013.169
49. Garg P, Verma R, Nihalani D, Johnstone DB, and Holzman LB. Neph1 cooperates with nephrin to transduce a signal that induces actin polymerization. Mol Cell Biol. (2007) 27:8698–712. doi: 10.1128/MCB.00948-07
50. Afsar B, Afsar RE, Demiray A, Covic A, and Kanbay M. Deciphering nutritional interventions for podocyte structure and function. Pharmacol Res. (2021) 172:105852. doi: 10.1016/j.phrs.2021.105852
51. Okabe M, Koike K, Yamamoto I, Tsuboi N, Matsusaka T, and Yokoo T. Early growth response 1 as a podocyte injury marker in human glomerular diseases. Clin Kidney J. (2024) 17:sfad289. doi: 10.1093/ckj/sfad289
52. Dominguez R and Holmes KC. Actin structure and function. Annu Rev Biophys. (2011) 40:169–86. doi: 10.1146/annurev-biophys-042910-155359
53. Sever S and Schiffer M. Actin dynamics at focal adhesions: a common endpoint and putative therapeutic target for proteinuric kidney diseases. Kidney Int. (2018) 93:1298–307. doi: 10.1016/j.kint.2017.12.028
54. Asanuma K, Kim K, Oh J, Giardino L, Chabanis S, Faul C, et al. Synaptopodin regulates the actin-bundling activity of alpha-actinin in an isoform-specific manner. J Clin Invest. (2005) 115:1188–98. doi: 10.1172/JCI200523371
55. Asanuma K, Yanagida-Asanuma E, Faul C, Tomino Y, Kim K, and Mundel P. Synaptopodin orchestrates actin organization and cell motility via regulation of RhoA signalling. Nat Cell Biol. (2006) 8:485–91. doi: 10.1038/ncb1400
56. Huang C, Meng M, Li S, Liu S, Li L, Su Y, et al. Umbilical cord mesenchymal stem cells ameliorate kidney injury in MRL/ipr mice through the TGF-β1 pathway. Front Cell Dev Biol. (2022) 10:876054. doi: 10.3389/fcell.2022.876054
57. Bhargava R and Tsokos GC. The immune podocyte. Curr Opin Rheumatol. (2019) 31:167–74. doi: 10.1097/BOR.0000000000000578
58. Mason LJ, Ravirajan CT, Rahman A, Putterman C, and Isenberg DA. Is alpha-actinin a target for pathogenic anti-DNA antibodies in lupus nephritis? Arthritis Rheum. (2004) 50:866–70. doi: 10.1002/art.20103
59. Bruschi M, Galetti M, Sinico RA, Moroni G, Bonanni A, Radice A, et al. Glomerular autoimmune multicomponents of human lupus nephritis in vivo (2): planted antigens. J Am Soc Nephrol. (2015) 26:1905–24. doi: 10.1681/ASN.2014050493
60. Roopenian DC and Akilesh S. FcRn: the neonatal Fc receptor comes of age. Nat Rev Immunol. (2007) 7:715–25. doi: 10.1038/nri2155
61. Olaru F, Luo W, Suleiman H, St John PL, Ge L, Mezo AR, et al. Neonatal Fc receptor promotes immune complex-mediated glomerular disease. J Am Soc Nephrol. (2014) 25:918–25. doi: 10.1681/ASN.2013050498
62. Ichinose K, Ushigusa T, Nishino A, Nakashima Y, Suzuki T, Horai Y, et al. Lupus nephritis igG induction of calcium/calmodulin-dependent protein kinase IV expression in podocytes and alteration of their function. Arthritis Rheumatol. (2016) 68:944–52. doi: 10.1002/art.39499
63. Goldwich A, Burkard M, Olke M, Daniel C, Amann K, Hugo C, et al. Podocytes are nonhematopoietic professional antigen-presenting cells. J Am Soc Nephrol. (2013) 24:906–16. doi: 10.1681/ASN.2012020133
64. Maeda K, Abdi R, and Tsokos GC. The role of podocytes in lupus pathology. Curr Rheumatol Rep. (2024) 27:10. doi: 10.1007/s11926-024-01175-4
65. Cellesi F, Li M, and Rastaldi MP. Podocyte injury and repair mechanisms. Curr Opin Nephrol Hypertens. (2015) 24:239–44. doi: 10.1097/MNH.0000000000000124
66. Mysore V, Tahir S, Furuhashi K, Arora J, Rosetti F, Cullere X, et al. Monocytes transition to macrophages within the inflamed vasculature via monocyte CCR2 and endothelial TNFR2. J Exp Med. (2022) 219(5):e20210562. doi: 10.1084/jem.20210562
67. Kim HS, Lee HK, Kim K, Ahn GB, Kim MS, Lee TY, et al. Mesenchymal stem cells enhance CCL8 expression by podocytes in lupus-prone MRL.Fas(lpr) mice. Sci Rep. (2023) 13:13074. doi: 10.1038/s41598-023-40346-8
68. Ishikawa S, Sato T, Abe M, Nagai S, Onai N, Yoneyama H, et al. Aberrant high expression of B lymphocyte chemokine (BLC/CXCL13) by C11b+CD11c+ dendritic cells in murine lupus and preferential chemotaxis of B1 cells towards BLC. J Exp Med. (2001) 193:1393–402. doi: 10.1084/jem.193.12.1393
69. Worthmann K, Gueler F, von Vietinghoff S, Davalos-Mißlitz A, Wiehler F, Davidson A, et al. Pathogenetic role of glomerular CXCL13 expression in lupus nephritis. Clin Exp Immunol. (2014) 178:20–7. doi: 10.1111/cei.12380
70. Pérez de Lema G, Maier H, Franz TJ, Escribese M, Chilla S, Segerer S, et al. Chemokine receptor Ccr2 deficiency reduces renal disease and prolongs survival in MRL/lpr lupus-prone mice. J Am Soc Nephrol. (2005) 16:3592–601. doi: 10.1681/ASN.2005040426
71. Tesch GH, Maifert S, Schwarting A, Rollins BJ, and Kelley VR. Monocyte chemoattractant protein 1-dependent leukocytic infiltrates are responsible for autoimmune disease in MRL-Fas(lpr) mice. J Exp Med. (1999) 190:1813–24. doi: 10.1084/jem.190.12.1813
72. Takano Y, Yamauchi K, Hayakawa K, Hiramatsu N, Kasai A, Okamura M, et al. Transcriptional suppression of nephrin in podocytes by macrophages: roles of inflammatory cytokines and involvement of the PI3K/Akt pathway. FEBS Lett. (2007) 581:421–6. doi: 10.1016/j.febslet.2006.12.051
73. Lleo A, Invernizzi P, Gao B, Podda M, and Gershwin ME. Definition of human autoimmunity–autoantibodies versus autoimmune disease. Autoimmun Rev. (2010) 9:A259–66. doi: 10.1016/j.autrev.2009.12.002
74. Devarapu SK and Anders HJ. Toll-like receptors in lupus nephritis. J BioMed Sci. (2018) 25:35. doi: 10.1186/s12929-018-0436-2
75. Nishi H and Mayadas TN. Neutrophils in lupus nephritis. Curr Opin Rheumatol. (2019) 31:193–200. doi: 10.1097/BOR.0000000000000577
76. Lavin Y, Winter D, Blecher-Gonen R, David E, Keren-Shaul H, Merad M, et al. Tissue-resident macrophage enhancer landscapes are shaped by the local microenvironment. Cell. (2014) 159:1312–26. doi: 10.1016/j.cell.2014.11.018
77. Viola A, Munari F, Sánchez-Rodríguez R, Scolaro T, and Castegna A. The metabolic signature of macrophage responses. Front Immunol. (2019) 10:1462. doi: 10.3389/fimmu.2019.01462
78. Funes SC, Rios M, Escobar-Vera J, and Kalergis AM. Implications of macrophage polarization in autoimmunity. Immunology. (2018) 154:186–95. doi: 10.1111/imm.12910
79. Labonte AC, Kegerreis B, Geraci NS, Bachali P, Madamanchi S, Robl R, et al. Identification of alterations in macrophage activation associated with disease activity in systemic lupus erythematosus. PloS One. (2018) 13:e0208132. doi: 10.1371/journal.pone.0208132
80. Zhang Z, Niu L, Tang X, Feng R, Yao G, Chen W, et al. Mesenchymal stem cells prevent podocyte injury in lupus-prone B6.MRL-Faslpr mice via polarizing macrophage into an anti-inflammatory phenotype. Nephrol Dial Transplant. (2019) 34:597–605. doi: 10.1093/ndt/gfy195
81. Arazi A, Rao DA, Berthier CC, Davidson A, Liu Y, Hoover PJ, et al. The immune cell landscape in kidneys of patients with lupus nephritis. Nat Immunol. (2019) 20:902–14. doi: 10.1038/s41590-019-0398-x
82. Horuluoglu B, Bayik D, Kayraklioglu N, Goguet E, Kaplan MJ, and Klinman DM. PAM3 supports the generation of M2-like macrophages from lupus patient monocytes and improves disease outcome in murine lupus. J Autoimmun. (2019) 99:24–32. doi: 10.1016/j.jaut.2019.01.004
83. Jiang H, Shen Z, Zhuang J, Lu C, Qu Y, Xu C, et al. Understanding the podocyte immune responses in proteinuric kidney diseases: from pathogenesis to therapy. Front Immunol. (2023) 14:1335936. doi: 10.3389/fimmu.2023.1335936
84. Tsuboi N, Asano K, Lauterbach M, and Mayadas TN. Human neutrophil Fcgamma receptors initiate and play specialized nonredundant roles in antibody-mediated inflammatory diseases. Immunity. (2008) 28:833–46. doi: 10.1016/j.immuni.2008.04.013
85. Teichmann LL, Ols ML, Kashgarian M, Reizis B, Kaplan DH, and Shlomchik MJ. Dendritic cells in lupus are not required for activation of T and B cells but promote their expansion, resulting in tissue damage. Immunity. (2010) 33:967–78. doi: 10.1016/j.immuni.2010.11.025
86. Dos Santos M, Poletti PT, Milhoransa P, Monticielo OA, and Veronese FV. Unraveling the podocyte injury in lupus nephritis: Clinical and experimental approaches. Semin Arthritis Rheum. (2017) 46:632–41. doi: 10.1016/j.semarthrit.2016.10.005
87. Crispín JC, Liossis SN, Kis-Toth K, Lieberman LA, Kyttaris VC, Juang YT, et al. Pathogenesis of human systemic lupus erythematosus: recent advances. Trends Mol Med. (2010) 16:47–57. doi: 10.1016/j.molmed.2009.12.005
88. Renaudineau Y, Deocharan B, Jousse S, Renaudineau E, Putterman C, and Youinou P. Anti-alpha-actinin antibodies: a new marker of lupus nephritis. Autoimmun Rev. (2007) 6:464–8. doi: 10.1016/j.autrev.2007.02.001
89. Raphael I, Nalawade S, Eagar TN, and Forsthuber TG T cell subsets and their signature cytokines in autoimmune and inflammatory diseases. Cytokine. (2015) 74:5–17. doi: 10.1016/j.cyto.2014.09.011
90. May CJ, Welsh GI, Chesor M, Lait PJ, Schewitz-Bowers LP, Lee RWJ, et al. Human Th17 cells produce a soluble mediator that increases podocyte motility via signaling pathways that mimic PAR-1 activation. Am J Physiol Renal Physiol. (2019) 317:F913–f21. doi: 10.1152/ajprenal.00093.2019
91. Yan J, Li Y, Yang H, Zhang L, Yang B, Wang M, et al. Interleukin-17A participates in podocyte injury by inducing IL-1β secretion through ROS-NLRP3 inflammasome-caspase-1 pathway. Scand J Immunol. (2018) 87:e12645. doi: 10.1111/sji.12645
92. Paquissi FC and Abensur H. The th17/IL-17 axis and kidney diseases, with focus on lupus nephritis. Front Med (Lausanne). (2021) 8:654912. doi: 10.3389/fmed.2021.654912
93. Zhou X, Chen H, Wei F, Zhao Q, Su Q, Lei Y, et al. α-mangostin attenuates pristane-induced lupus nephritis by regulating Th17 differentiation. Int J Rheum Dis. (2020) 23:74–83. doi: 10.1111/1756-185X.13743
94. Zhou X, Chen H, Wei F, Zhao Q, Su Q, Liang J, et al. 3β-acetyloxy-oleanolic acid attenuates pristane-induced lupus nephritis by regulating th17 differentiation. J Immunol Res. (2019) 2019:2431617. doi: 10.1155/2019/2431617
95. Fu R, Guo C, Wang S, Huang Y, Jin O, Hu H, et al. Podocyte activation of NLRP3 inflammasomes contributes to the development of proteinuria in lupus nephritis. Arthritis Rheumatol. (2017) 69:1636–46. doi: 10.1002/art.40155
96. Hutton HL, Ooi JD, Holdsworth SR, and Kitching AR. The NLRP3 inflammasome in kidney disease and autoimmunity. Nephrol (Carlton). (2016) 21:736–44. doi: 10.1111/nep.12785
97. Hirayama K, Ebihara I, Yamamoto S, Kai H, Muro K, Yamagata K, et al. Predominance of type-2 immune response in idiopathic membranous nephropathy. Cytoplasmic cytokine analysis. Nephron. (2002) 91:255–61. doi: 10.1159/000058401
98. Kawasaki Y, Suzuki J, Sakai N, Isome M, Nozawa R, Tanji M, et al. Evaluation of T helper-1/-2 balance on the basis of IgG subclasses and serum cytokines in children with glomerulonephritis. Am J Kidney Dis. (2004) 44:42–9. doi: 10.1053/j.ajkd.2004.03.029
99. Masutani K, Taniguchi M, Nakashima H, Yotsueda H, Kudoh Y, Tsuruya K, et al. Up-regulated interleukin-4 production by peripheral T-helper cells in idiopathic membranous nephropathy. Nephrol Dial Transplant. (2004) 19:580–6. doi: 10.1093/ndt/gfg572
100. Mao Z, Tan Y, Tao J, Li L, Wang H, Yu F, et al. Renal mTORC1 activation is associated with disease activity and prognosis in lupus nephritis. Rheumatol (Oxford). (2022) 61:3830–40. doi: 10.1093/rheumatology/keac037
101. Liu X, Mao Z, Yuan M, Li L, Tan Y, Qu Z, et al. Glomerular mTORC1 activation was associated with podocytes to endothelial cells communication in lupus nephritis. Lupus Sci Med. (2023) 10(1):e000896. doi: 10.1136/lupus-2023-000896
102. Lamkanfi M and Dixit VM. Mechanisms and functions of inflammasomes. Cell. (2014) 157:1013–22. doi: 10.1016/j.cell.2014.04.007
103. Wofsy D, Ledbetter JA, Hendler PL, and Seaman WE. Treatment of murine lupus with monoclonal anti-T cell antibody. J Immunol. (1985) 134:852–7. doi: 10.4049/jimmunol.134.2.852
104. Schiffer L, Sinha J, Wang X, Huang W, von Gersdorff G, Schiffer M, et al. Short term administration of costimulatory blockade and cyclophosphamide induces remission of systemic lupus erythematosus nephritis in NZB/W F1 mice by a mechanism downstream of renal immune complex deposition. J Immunol. (2003) 171:489–97. doi: 10.4049/jimmunol.171.1.489
105. Li S, Liu Y, He Y, Rong W, Zhang M, Li L, et al. Podocytes present antigen to activate specific T cell immune responses in inflammatory renal disease. J Pathol. (2020) 252:165–77. doi: 10.1002/path.5508
106. Kitching AR and Alikhan MA. CD8+ cells and glomerular crescent formation: outside-in as well as inside-out. J Clin Invest. (2018) 128:3231–3. doi: 10.1172/JCI122045
107. Singh SK, Jeansson M, and Quaggin SE. New insights into the pathogenesis of cellular crescents. Curr Opin Nephrol Hypertens. (2011) 20:258–62. doi: 10.1097/MNH.0b013e32834583ec
108. Ishimoto T, Shimada M, Gabriela G, Kosugi T, Sato W, Lee PY, et al. Toll-like receptor 3 ligand, polyIC, induces proteinuria and glomerular CD80, and increases urinary CD80 in mice. Nephrol Dial Transplant. (2013) 28:1439–46. doi: 10.1093/ndt/gfs543
109. Reiser J, von Gersdorff G, Loos M, Oh J, Asanuma K, Giardino L, et al. Induction of B7–1 in podocytes is associated with nephrotic syndrome. J Clin Invest. (2004) 113:1390–7. doi: 10.1172/JCI20402
110. Reiser J and Alachkar N. Proteinuria: abate or applaud abatacept in proteinuric kidney disease? Nat Rev Nephrol. (2014) 10:128–30. doi: 10.1038/nrneph.2013.276
111. Abbas AK and Sharpe AH. T-cell stimulation: an abundance of B7s. Nat Med. (1999) 5:1345–6. doi: 10.1038/70905
112. Henry J, Miller MM, and Pontarotti P. Structure and evolution of the extended B7 family. Immunol Today. (1999) 20:285–8. doi: 10.1016/S0167-5699(98)01418-2
113. Ichinose K, Juang YT, Crispín JC, Kis-Toth K, and Tsokos GC Suppression of autoimmunity and organ pathology in lupus-prone mice upon inhibition of calcium/calmodulin-dependent protein kinase type IV. Arthritis Rheum. (2011) 63:523–9. doi: 10.1002/art.30085
114. Qian B, Lu R, Mao S, Chen Y, Yang M, Zhang W, et al. Podocyte SIRPα reduction aggravates lupus nephritis via promoting T cell inflammatory responses. Cell Rep. (2024) 43:114249. doi: 10.1016/j.celrep.2024.114249
115. Postal M, Vivaldo JF, Fernandez-Ruiz R, Paredes JL, Appenzeller S, Niewold TB, et al. Type I interferon in the pathogenesis of systemic lupus erythematosus. Curr Opin Immunol. (2020) 67:87–94. doi: 10.1016/j.coi.2020.10.014
116. Lech M and Anders HJ. The pathogenesis of lupus nephritis. J Am Soc Nephrol. (2013) 24:1357–66. doi: 10.1681/ASN.2013010026
117. Koga T, Ichinose K, and Tsokos GC. T cells and IL-17 in lupus nephritis. Clin Immunol. (2017) 185:95–9. doi: 10.1016/j.clim.2016.04.010
118. Apostolidis SA, Crispín JC, and Tsokos GC. IL-17-producing T cells in lupus nephritis. Lupus. (2011) 20:120–4. doi: 10.1177/0961203310389100
119. Koga T, Ichinose K, Kawakami A, and Tsokos GC. The role of IL-17 in systemic lupus erythematosus and its potential as a therapeutic target. Expert Rev Clin Immunol. (2019) 15:629–37. doi: 10.1080/1744666X.2019.1593141
120. Koga T, Ichinose K, Kawakami A, and Tsokos GC. Current insights and future prospects for targeting IL-17 to treat patients with systemic lupus erythematosus. Front Immunol. (2020) 11:624971. doi: 10.3389/fimmu.2020.624971
121. Cai M, Zhou T, Wang X, Shang M, Zhang Y, Luo M, et al. DC-SIGN expression on podocytes and its role in inflammatory immune response of lupus nephritis. Clin Exp Immunol. (2016) 183:317–25. doi: 10.1111/cei.12723
122. Enghard P, Rieder C, Kopetschke K, Klocke JR, Undeutsch R, Biesen R, et al. Urinary CD4 T cells identify SLE patients with proliferative lupus nephritis and can be used to monitor treatment response. Ann Rheum Dis. (2014) 73:277–83. doi: 10.1136/annrheumdis-2012-202784
123. Maria NI and Davidson A. Protecting the kidney in systemic lupus erythematosus: from diagnosis to therapy. Nat Rev Rheumatol. (2020) 16:255–67. doi: 10.1038/s41584-020-0401-9
124. Liu Y and Anders HJ. Lupus nephritis: from pathogenesis to targets for biologic treatment. Nephron Clin Pract. (2014) 128:224–31. doi: 10.1159/000368581
125. Durcan L, O’Dwyer T, and Petri M. Management strategies and future directions for systemic lupus erythematosus in adults. Lancet. (2019) 393:2332–43. doi: 10.1016/S0140-6736(19)30237-5
126. Fava A and Petri M. Systemic lupus erythematosus: Diagnosis and clinical management. J Autoimmun. (2019) 96:1–13. doi: 10.1016/j.jaut.2018.11.001
127. Tsai CY, Li KJ, Shen CY, Lu CH, Lee HT, Wu TH, et al. Decipher the immunopathological mechanisms and set up potential therapeutic strategies for patients with lupus nephritis. Int J Mol Sci. (2023) 24(12):10066. doi: 10.3390/ijms241210066
128. Abbate M, Zoja C, Corna D, Rottoli D, Zanchi C, Azzollini N, et al. Complement-mediated dysfunction of glomerular filtration barrier accelerates progressive renal injury. J Am Soc Nephrol. (2008) 19:1158–67. doi: 10.1681/ASN.2007060686
129. Kalaaji M, Mortensen E, Jørgensen L, Olsen R, and Rekvig OP. Nephritogenic lupus antibodies recognize glomerular basement membrane-associated chromatin fragments released from apoptotic intraglomerular cells. Am J Pathol. (2006) 168:1779–92. doi: 10.2353/ajpath.2006.051329
130. Haymann JP, Levraud JP, Bouet S, Kappes V, Hagège J, Nguyen G, et al. Characterization and localization of the neonatal Fc receptor in adult human kidney. J Am Soc Nephrol. (2000) 11:632–9. doi: 10.1681/ASN.V114632
131. Maeda K, Otomo K, Yoshida N, Abu-Asab MS, Ichinose K, Nishino T, et al. CaMK4 compromises podocyte function in autoimmune and nonautoimmune kidney disease. J Clin Invest. (2018) 128:3445–59. doi: 10.1172/JCI99507
132. Bhargava R, Maeda K, Tsokos MG, Pavlakis M, Stillman IE, and Tsokos GC. N-glycosylated IgG in patients with kidney transplants increases calcium/calmodulin kinase IV in podocytes and causes injury. Am J Transplant. (2021) 21:148–60. doi: 10.1111/ajt.16140
133. Andersen JT, Daba MB, Berntzen G, Michaelsen TE, and Sandlie I. Cross-species binding analyses of mouse and human neonatal Fc receptor show dramatic differences in immunoglobulin G and albumin binding. J Biol Chem. (2010) 285:4826–36. doi: 10.1074/jbc.M109.081828
134. Qi YY, Zhou XJ, Cheng FJ, Hou P, Ren YL, Wang SX, et al. Increased autophagy is cytoprotective against podocyte injury induced by antibody and interferon-α in lupus nephritis. Ann Rheum Dis. (2018) 77:1799–809. doi: 10.1136/annrheumdis-2018-213028
135. Tsokos GC. Systemic lupus erythematosus. N Engl J Med. (2011) 365:2110–21. doi: 10.1056/NEJMra1100359
136. Bhargava R, Lehoux S, Maeda K, Tsokos MG, Krishfield S, Ellezian L, et al. Aberrantly glycosylated IgG elicits pathogenic signaling in podocytes and signifies lupus nephritis. JCI Insight. (2021) 6(9):e147789. doi: 10.1172/jci.insight.147789
137. Chang A, Henderson SG, Brandt D, Liu N, Guttikonda R, Hsieh C, et al. In situ B cell-mediated immune responses and tubulointerstitial inflammation in human lupus nephritis. J Immunol. (2011) 186:1849–60. doi: 10.4049/jimmunol.1001983
138. Suárez-Fueyo A, Bradley SJ, Klatzmann D, and Tsokos GC. T cells and autoimmune kidney disease. Nat Rev Nephrol. (2017) 13:329–43. doi: 10.1038/nrneph.2017.34
139. Bhargava P and Schnellmann RG. Mitochondrial energetics in the kidney. Nat Rev Nephrol. (2017) 13:629–46. doi: 10.1038/nrneph.2017.107
140. Van Raaij S, Van Swelm R, Bouman K, Cliteur M, van den Heuvel MC, Pertijs J, et al. Tubular iron deposition and iron handling proteins in human healthy kidney and chronic kidney disease. Sci Rep. (2018) 8:9353. doi: 10.1038/s41598-018-27107-8
141. Dai C, Liu Z, Zhou H, and Li L. Monocyte chemoattractant protein-1 expression in renal tissue is associated with monocyte recruitment and tubulo-interstitial lesions in patients with lupus nephritis. Chin Med J (Engl). (2001) 114:864–8.
142. Tang WW, Feng L, Xia Y, and Wilson CB. Extracellular matrix accumulation in immune-mediated tubulointerstitial injury. Kidney Int. (1994) 45:1077–84. doi: 10.1038/ki.1994.144
143. Magil AB and Tyler M. Tubulo-interstitial disease in lupus nephritis. A morphometric study. Histopathology. (1984) 8:81–7. doi: 10.1111/j.1365-2559.1984.tb02324.x
144. Hong S, Healy H, and Kassianos AJ. The emerging role of renal tubular epithelial cells in the immunological pathophysiology of lupus nephritis. Front Immunol. (2020) 11:578952. doi: 10.3389/fimmu.2020.578952
145. Qi R and Yang C. Renal tubular epithelial cells: the neglected mediator of tubulointerstitial fibrosis after injury. Cell Death Dis. (2018) 9:1126. doi: 10.1038/s41419-018-1157-x
146. Liu BC, Tang TT, Lv LL, and Lan HY. Renal tubule injury: a driving force toward chronic kidney disease. Kidney Int. (2018) 93:568–79. doi: 10.1016/j.kint.2017.09.033
147. Yung S and Chan TM. Molecular and immunological basis of tubulo-interstitial injury in lupus nephritis: a comprehensive review. Clin Rev Allergy Immunol. (2017) 52:149–63. doi: 10.1007/s12016-016-8533-z
148. Noris M, Bernasconi S, Casiraghi F, Sozzani S, Gotti E, Remuzzi G, et al. Monocyte chemoattractant protein-1 is excreted in excessive amounts in the urine of patients with lupus nephritis. Lab Invest. (1995) 73:804–9.
149. Tucci M, Calvani N, Richards HB, Quatraro C, and Silvestris F. The interplay of chemokines and dendritic cells in the pathogenesis of lupus nephritis. Ann N Y Acad Sci. (2005) 1051:421–32. doi: 10.1196/annals.1361.084
150. Weber GF, Ashkar S, Glimcher MJ, and Cantor H. Receptor-ligand interaction between CD44 and osteopontin (Eta-1). Science. (1996) 271:509–12. doi: 10.1126/science.271.5248.509
151. Kwant LE, Vegting Y, Tsang ASMWP, Kwakernaak AJ, Vogt L, Voskuyl AE, et al. Macrophages in Lupus Nephritis: Exploring a potential new therapeutic avenue. Autoimmun Rev. (2022) 21:103211. doi: 10.1016/j.autrev.2022.103211
152. Pichler R, Giachelli CM, Lombardi D, Pippin J, Gordon K, Alpers CE, et al. Tubulointerstitial disease in glomerulonephritis. Potential role of osteopontin (uropontin). Am J Pathol. (1994) 144:915–26.
153. Yu XQ, Nikolic-Paterson DJ, Mu W, Giachelli CM, Atkins RC, Johnson RJ, et al. A functional role for osteopontin in experimental crescentic glomerulonephritis in the rat. Proc Assoc Am Physicians. (1998) 110:50–64.
154. Okada H, Moriwaki K, Konishi K, Kobayashi T, Sugahara S, Nakamoto H, et al. Tubular osteopontin expression in human glomerulonephritis and renal vasculitis. Am J Kidney Dis. (2000) 36:498–506. doi: 10.1053/ajkd.2000.9790
155. Wüthrich RP, Fan X, Ritthaler T, Sibalic V, Yu DJ, Loffing J, et al. Enhanced osteopontin expression and macrophage infiltration in MRL-Fas(lpr) mice with lupus nephritis. Autoimmunity. (1998) 28:139–50. doi: 10.3109/08916939808996282
156. De Palma G, Castellano G, Del Prete A, Sozzani S, Fiore N, Loverre A, et al. The possible role of ChemR23/Chemerin axis in the recruitment of dendritic cells in lupus nephritis. Kidney Int. (2011) 79:1228–35. doi: 10.1038/ki.2011.32
157. Woltman AM, de Fijter JW, van der Kooij SW, Jie KE, Massacrier C, Caux C, et al. MIP-3alpha/CCL20 in renal transplantation and its possible involvement as dendritic cell chemoattractant in allograft rejection. Am J Transplant. (2005) 5:2114–25. doi: 10.1111/j.1600-6143.2005.00997.x
158. Chen W, Jin B, Cheng C, Peng H, Zhang X, Tan W, et al. Single-cell profiling reveals kidney CD163(+) dendritic cell participation in human lupus nephritis. Ann Rheum Dis. (2024) 83:608–23. doi: 10.1136/ard-2023-224788
159. Hu L, Hu J, Chen L, Zhang Y, Wang Q, Yang X, et al. Interleukin-22 from type 3 innate lymphoid cells aggravates lupus nephritis by promoting macrophage infiltration in lupus-prone mice. Front Immunol. (2021) 12:584414. doi: 10.3389/fimmu.2021.584414
160. Wada Y, Gonzalez-Sanchez HM, Weinmann-Menke J, Iwata Y, Ajay AK, Meineck M, et al. IL-34-dependent intrarenal and systemic mechanisms promote lupus nephritis in MRL-fas(lpr) mice. J Am Soc Nephrol. (2019) 30:244–59. doi: 10.1681/ASN.2018090901
161. Jia P, Xu S, Ren T, Pan T, Wang X, Zhang Y, et al. LncRNA IRAR regulates chemokines production in tubular epithelial cells thus promoting kidney ischemia-reperfusion injury. Cell Death Dis. (2022) 13:562. doi: 10.1038/s41419-022-05018-x
162. Jia P, Xu S, Wang X, Wu X, Ren T, Zou Z, et al. Chemokine CCL2 from proximal tubular epithelial cells contributes to sepsis-induced acute kidney injury. Am J Physiol Renal Physiol. (2022) 323:F107–f19. doi: 10.1152/ajprenal.00037.2022
163. Kassianos AJ, Wang X, Sampangi S, Afrin S, Wilkinson R, and Healy H Fractalkine-CX3CR1-dependent recruitment and retention of human CD1c+ myeloid dendritic cells by in vitro-activated proximal tubular epithelial cells. Kidney Int. (2015) 87:1153–63. doi: 10.1038/ki.2014.407
164. Ramanujam M, Steffgen J, Visvanathan S, Mohan C, Fine JS, and Putterman C. Phoenix from the flames: Rediscovering the role of the CD40-CD40L pathway in systemic lupus erythematosus and lupus nephritis. Autoimmun Rev. (2020) 19:102668. doi: 10.1016/j.autrev.2020.102668
165. Kim J, Jeong JH, Jung J, Jeon H, Lee S, Lim JS, et al. Immunological characteristics and possible pathogenic role of urinary CD11c+ macrophages in lupus nephritis. Rheumatol (Oxford). (2020) 59:2135–45. doi: 10.1093/rheumatology/keaa053
166. Jang MH, Herber DM, Jiang X, Nandi S, Dai XM, Zeller G, et al. Distinct in vivo roles of colony-stimulating factor-1 isoforms in renal inflammation. J Immunol. (2006) 177:4055–63. doi: 10.4049/jimmunol.177.6.4055
167. Menke J, Rabacal WA, Byrne KT, Iwata Y, Schwartz MM, Stanley ER, et al. Circulating CSF-1 promotes monocyte and macrophage phenotypes that enhance lupus nephritis. J Am Soc Nephrol. (2009) 20:2581–92. doi: 10.1681/ASN.2009050499
168. Lv LL, Feng Y, Wen Y, Wu WJ, Ni HF, Li ZL, et al. Exosomal CCL2 from tubular epithelial cells is critical for albumin-induced tubulointerstitial inflammation. J Am Soc Nephrol. (2018) 29:919–35. doi: 10.1681/ASN.2017050523
169. Lv LL, Feng Y, Wu M, Wang B, Li ZL, Zhong X, et al. Exosomal miRNA-19b-3p of tubular epithelial cells promotes M1 macrophage activation in kidney injury. Cell Death Differ. (2020) 27:210–26. doi: 10.1038/s41418-019-0349-y
170. Zhang Z, Chen H, Zhou L, Li C, Lu G, Wang L, et al. Macrophage−derived exosomal miRNA−155 promotes tubular injury in ischemia−induced acute kidney injury. Int J Mol Med. (2022) 50(3):116. doi: 10.3892/ijmm.2022.5172
171. Linke A, Cicek H, Müller A, Meyer-Schwesinger C, Melderis S, Wiech T, et al. Antigen cross-presentation by murine proximal tubular epithelial cells induces cytotoxic and inflammatory CD8(+) T cells. Cells. (2022) 11(9):1510. doi: 10.3390/cells11091510
172. Hagerty DT and Allen PM. Processing and presentation of self and foreign antigens by the renal proximal tubule. J Immunol. (1992) 148:2324–30. doi: 10.4049/jimmunol.148.8.2324
173. Gastl G, Ebert T, Finstad CL, Sheinfeld J, Gomahr A, Aulitzky W, et al. Major histocompatibility complex class I and class II expression in renal cell carcinoma and modulation by interferon gamma. J Urol. (1996) 155:361–7. doi: 10.1016/S0022-5347(01)66661-8
174. Mayrhofer G and Schon-Hegrad MA. Ia antigens in rat kidney, with special reference to their expression in tubular epithelium. J Exp Med. (1983) 157:2097–109. doi: 10.1084/jem.157.6.2097
175. Wuthrich RP, Glimcher LH, Yui MA, Jevnikar AM, Dumas SE, and Kelley VE. MHC class II, antigen presentation and tumor necrosis factor in renal tubular epithelial cells. Kidney Int. (1990) 37:783–92. doi: 10.1038/ki.1990.46
176. Sinclair GD, Wadgymar A, and Halloran PF. Graft-vs-host reactions induce H-2 class II gene transcription in host kidney cells. Immunogenetics. (1984) 20:503–11. doi: 10.1007/BF00364353
177. Benson EM, Colvin RB, and Russell PS. Induction of IA antigens in murine renal transplants. J Immunol. (1985) 134:7–9. doi: 10.4049/jimmunol.134.1.7
178. Breda PC, Wiech T, Meyer-Schwesinger C, Grahammer F, Huber T, Panzer U, et al. Renal proximal tubular epithelial cells exert immunomodulatory function by driving inflammatory CD4(+) T cell responses. Am J Physiol Renal Physiol. (2019) 317:F77–f89. doi: 10.1152/ajprenal.00427.2018
179. Niemann-Masanek U, Mueller A, Yard BA, Waldherr R, and van der Woude FJ. B7-1 (CD80) and B7-2 (CD 86) expression in human tubular epithelial cells in vivo and in vitro. Nephron. (2002) 92:542–56. doi: 10.1159/000064084
180. Wu Q, Jinde K, Endoh M, and Sakai H. Clinical significance of costimulatory molecules CD80/CD86 expression in IgA nephropathy. Kidney Int. (2004) 65:888–96. doi: 10.1111/j.1523-1755.2004.00477.x
181. Ding H, Wu X, and Gao W. PD-L1 is expressed by human renal tubular epithelial cells and suppresses T cell cytokine synthesis. Clin Immunol. (2005) 115:184–91. doi: 10.1016/j.clim.2005.01.005
182. Shlomchik MJ, Madaio MP, Ni D, Trounstein M, and Huszar D. The role of B cells in lpr/lpr-induced autoimmunity. J Exp Med. (1994) 180:1295–306. doi: 10.1084/jem.180.4.1295
183. Vlahakos DV, Foster MH, Adams S, Katz M, Ucci AA, Barrett KJ, et al. Anti-DNA antibodies form immune deposits at distinct glomerular and vascular sites. Kidney Int. (1992) 41:1690–700. doi: 10.1038/ki.1992.242
184. Mackay F and Schneider P. Cracking the BAFF code. Nat Rev Immunol. (2009) 9:491–502. doi: 10.1038/nri2572
185. Jamaly S, Rakaee M, Abdi R, Tsokos GC, and Fenton KA. Interplay of immune and kidney resident cells in the formation of tertiary lymphoid structures in lupus nephritis. Autoimmun Rev. (2021) 20:102980. doi: 10.1016/j.autrev.2021.102980
186. Mackay F, Woodcock SA, Lawton P, Ambrose C, Baetscher M, Schneider P, et al. Mice transgenic for BAFF develop lymphocytic disorders along with autoimmune manifestations. J Exp Med. (1999) 190:1697–710. doi: 10.1084/jem.190.11.1697
187. Cancro MP and Smith SH. Peripheral B cell selection and homeostasis. Immunol Res. (2003) 27:141–8. doi: 10.1385/IR:27:2-3:141
188. Schwarting A, Relle M, Meineck M, Föhr B, Triantafyllias K, Weinmann A, et al. Renal tubular epithelial cell-derived BAFF expression mediates kidney damage and correlates with activity of proliferative lupus nephritis in mouse and men. Lupus. (2018) 27:243–56. doi: 10.1177/0961203317717083
189. Mistry P and Kaplan MJ. Cell death in the pathogenesis of systemic lupus erythematosus and lupus nephritis. Clin Immunol. (2017) 185:59–73. doi: 10.1016/j.clim.2016.08.010
190. Banchereau J, Bazan F, Blanchard D, Brière F, Galizzi JP, van Kooten C, et al. The CD40 antigen and its ligand. Annu Rev Immunol. (1994) 12:881–922. doi: 10.1146/annurev.iy.12.040194.004313
191. Van Kooten C and Banchereau J. Functions of CD40 on B cells, dendritic cells and other cells. Curr Opin Immunol. (1997) 9:330–7. doi: 10.1016/S0952-7915(97)80078-7
192. Kalled SL, Cutler AH, Datta SK, and Thomas DW. Anti-CD40 ligand antibody treatment of SNF1 mice with established nephritis: preservation of kidney function. J Immunol. (1998) 160:2158–65. doi: 10.4049/jimmunol.160.5.2158
193. Vogel LA and Noelle RJ. CD40 and its crucial role as a member of the TNFR family. Semin Immunol. (1998) 10:435–42. doi: 10.1006/smim.1998.0145
194. Cantaluppi V, Quercia AD, Dellepiane S, Ferrario S, Camussi G, and Biancone L. Interaction between systemic inflammation and renal tubular epithelial cells. Nephrol Dial Transplant. (2014) 29:2004–11. doi: 10.1093/ndt/gfu046
195. Wu D, Jiang T, Zhang S, Huang M, Zhu Y, Chen L, et al. Blockade of notch1 signaling alleviated podocyte injury in lupus nephritis via inhibition of NLRP3 inflammasome activation. Inflammation. (2024) 47:649–63. doi: 10.1007/s10753-023-01935-x
196. Osaka H, Wang YL, Takada K, Takizawa S, Setsuie R, Li H, et al. Ubiquitin carboxy-terminal hydrolase L1 binds to and stabilizes monoubiquitin in neuron. Hum Mol Genet. (2003) 12:1945–58. doi: 10.1093/hmg/ddg211
197. Cui JH and Xie X. UCH-L1 expressed by podocytes: a potentially therapeutic target for lupus nephritis? Inflammation. (2017) 40:657–65. doi: 10.1007/s10753-017-0512-x
198. Sun L, Zou LX, Han YC, Wu L, Chen T, Zhu DD, et al. A20 overexpression exerts protective effects on podocyte injury in lupus nephritis by downregulating UCH-L1. J Cell Physiol. (2019) 234:16191–204. doi: 10.1002/jcp.28282
199. Ying J, Qiu X, Lu Y, and Zhang M. SOCS1 and its potential clinical role in tumor. Pathol Oncol Res. (2019) 25:1295–301. doi: 10.1007/s12253-019-00612-5
200. Pang J, Huang P, Huang H, Ma J, He L, Lin X, et al. Molecular mechanism and role of miRNA-155 ribonucleic acid in podocyte apoptosis in lupus nephritis: SOCS1 protein expression regulates JAK/STAT pathway transduction. Int J Biol Macromol. (2025) 304(Pt 1):140810. doi: 10.1016/j.ijbiomac.2025.140810
201. Lu R, Zhang L, and Yang X. Interaction between autophagy and the NLRP3 inflammasome in Alzheimer’s and Parkinson’s disease. Front Aging Neurosci. (2022) 14:1018848. doi: 10.3389/fnagi.2022.1018848
202. Ertuglu LA, Elijovich F, Laffer CL, and Kirabo A. Salt-sensitivity of blood pressure and insulin resistance. Front Physiol. (2021) 12:793924. doi: 10.3389/fphys.2021.793924
203. Luo Z, Lu G, Yang Q, Ding J, Wang T, and Hu P. Identification of shared immune cells and immune-related co-disease genes in chronic heart failure and systemic lupus erythematosus based on transcriptome sequencing. J Inflammation Res. (2023) 16:2689–705. doi: 10.2147/JIR.S418598
204. Li X, Yan Z, Carlström M, Tian J, Zhang X, Zhang W, et al. Mangiferin ameliorates hyperuricemic nephropathy which is associated with downregulation of AQP2 and increased urinary uric acid excretion. Front Pharmacol. (2020) 11:49. doi: 10.3389/fphar.2020.00049
205. Zou Y, Wang D, Sun W, Wu Q, Liu S, Ren Z, et al. Fibroblast growth factor 21 mitigates lupus nephritis progression via the FGF21/Irgm 1/NLRP3 inflammasome pathway. Int Immunopharmacol. (2024) 131:111875. doi: 10.1016/j.intimp.2024.111875
206. Zhao XY, Li SS, He YX, Yan LJ, Lv F, Liang QM, et al. SGLT2 inhibitors alleviated podocyte damage in lupus nephritis by decreasing inflammation and enhancing autophagy. Ann Rheum Dis. (2023) 82:1328–40. doi: 10.1136/ard-2023-224242
207. Morales E and Galindo M. SGLT2 inhibitors in lupus nephropathy, a new therapeutic strategy for nephroprotection. Ann Rheum Dis. (2022) 81:1337–8. doi: 10.1136/annrheumdis-2022-222512
208. Oliveira CB, Lima CAD, Vajgel G, and Sandrin-Garcia P. The role of NLRP3 inflammasome in lupus nephritis. Int J Mol Sci. (2021) 22(22):12476. doi: 10.3390/ijms222212476
209. Stylianou K, Petrakis I, Mavroeidi V, Stratakis S, Vardaki E, Perakis K, et al. The PI3K/Akt/mTOR pathway is activated in murine lupus nephritis and downregulated by rapamycin. Nephrol Dial Transplant. (2011) 26:498–508. doi: 10.1093/ndt/gfq496
210. Nath KA. Tubulointerstitial changes as a major determinant in the progression of renal damage. Am J Kidney Dis. (1992) 20:1–17. doi: 10.1016/S0272-6386(12)80312-X
211. Castellano G, Cafiero C, Divella C, Sallustio F, Gigante M, Pontrelli P, et al. Local synthesis of interferon-alpha in lupus nephritis is associated with type I interferons signature and LMP7 induction in renal tubular epithelial cells. Arthritis Res Ther. (2015) 17:72. doi: 10.1186/s13075-015-0588-3
212. Laplante M and Sabatini DM. mTOR signaling in growth control and disease. Cell. (2012) 149:274–93. doi: 10.1016/j.cell.2012.03.017
213. Perl A. mTOR activation is a biomarker and a central pathway to autoimmune disorders, cancer, obesity, and aging. Ann N Y Acad Sci. (2015) 1346:33–44. doi: 10.1111/nyas.12756
214. Zhang C, Chan CCY, Cheung KF, Chau MKM, Yap DYH, Ma MKM, et al. Effect of mycophenolate and rapamycin on renal fibrosis in lupus nephritis. Clin Sci (Lond). (2019) 133:1721–44. doi: 10.1042/CS20190536
215. Lui SL, Yung S, Tsang R, Zhang F, Chan KW, Tam S, et al. Rapamycin prevents the development of nephritis in lupus-prone NZB/W F1 mice. Lupus. (2008) 17:305–13. doi: 10.1177/0961203307088289
216. Yap DYH, Tang C, Chan GCW, Kwan LPY, Ma MKM, Mok MMY, et al. Longterm data on sirolimus treatment in patients with lupus nephritis. J Rheumatol. (2018) 45:1663–70. doi: 10.3899/jrheum.180507
217. Bakdash G, van Capel TM, Mason LM, Kapsenberg ML, and de Jong EC. Vitamin D3 metabolite calcidiol primes human dendritic cells to promote the development of immunomodulatory IL-10-producing T cells. Vaccine. (2014) 32:6294–302. doi: 10.1016/j.vaccine.2014.08.075
218. Barragan M, Good M, and Kolls JK. Regulation of dendritic cell function by vitamin D. Nutrients. (2015) 7:8127–51. doi: 10.3390/nu7095383
219. Sun J, Zhang S, Liu JS, Gui M, and Zhang H. Expression of vitamin D receptor in renal tissue of lupus nephritis and its association with renal injury activity. Lupus. (2019) 28:290–4. doi: 10.1177/0961203319826704
220. Huang J, An Q, Ju BM, Zhang J, Fan P, He L, et al. Role of vitamin D/VDR nuclear translocation in down-regulation of NF-κB/NLRP3/caspase-1 axis in lupus nephritis. Int Immunopharmacol. (2021) 100:108131. doi: 10.1016/j.intimp.2021.108131
221. Peng X, Yang T, Liu G, Liu H, Peng Y, and He L. Piperine ameliorated lupus nephritis by targeting AMPK-mediated activation of NLRP3 inflammasome. Int Immunopharmacol. (2018) 65:448–57. doi: 10.1016/j.intimp.2018.10.025
222. Ijima S, Saito Y, Nagaoka K, Yamamoto S, Sato T, Miura N, et al. Fisetin reduces the senescent tubular epithelial cell burden and also inhibits proliferative fibroblasts in murine lupus nephritis. Front Immunol. (2022) 13:960601. doi: 10.3389/fimmu.2022.960601
223. Papageorgis P. Complex interplay between aging and cancer: role of TGF-β Signaling. Crit Rev Oncog. (2017) 22:313–21. doi: 10.1615/CritRevOncog.2017025134
224. Zhu Y, Doornebal EJ, Pirtskhalava T, Giorgadze N, Wentworth M, Fuhrmann-Stroissnigg H, et al. New agents that target senescent cells: the flavone, fisetin, and the BCL-X(L) inhibitors, A1331852 and A1155463. Aging (Albany NY). (2017) 9:955–63. doi: 10.18632/aging.101202
225. Yousefzadeh MJ, Zhu Y, McGowan SJ, Angelini L, Fuhrmann-Stroissnigg H, Xu M, et al. Fisetin is a senotherapeutic that extends health and lifespan. EBioMedicine. (2018) 36:18–28. doi: 10.1016/j.ebiom.2018.09.015
226. Kirkland JL and Tchkonia T. Cellular senescence: A translational perspective. EBioMedicine. (2017) 21:21–8. doi: 10.1016/j.ebiom.2017.04.013
227. Kirkland JL and Tchkonia T. Senolytic drugs: from discovery to translation. J Intern Med. (2020) 288:518–36. doi: 10.1111/joim.13141
228. Camell CD, Yousefzadeh MJ, Zhu Y, Prata L, Huggins MA, Pierson M, et al. Senolytics reduce coronavirus-related mortality in old mice. Science. (2021) 373(6552):eabe4832. doi: 10.1126/science.abe4832
229. Mejia-Vilet JM, Malvar A, Arazi A, and Rovin BH. The lupus nephritis management renaissance. Kidney Int. (2022) 101:242–55. doi: 10.1016/j.kint.2021.09.012
230. Kale A, Lech M, Anders HJ, and Gaikwad AB. Lupus nephritis: new and emerging biologic and targeted therapies. BioDrugs. (2023) 37:463–75. doi: 10.1007/s40259-023-00597-3
231. Wang J, Nie S, Kan L, Chen H, Cui SW, Phillips AO, et al. Comparison of structural features and antioxidant activity of polysaccharides from natural and cultured Cordyceps sinensis. Food Sci Biotechnol. (2017) 26:55–62. doi: 10.1007/s10068-017-0008-3
232. Liao Z, Yang X, He L, Bai J, Zhou X, Yang J, et al. Cordyceps protein alleviates renal injury by inhibiting T cell infiltration and Th1 cell differentiation in lupus nephritis mice. Int Immunopharmacol. (2024) 138:112566. doi: 10.1016/j.intimp.2024.112566
233. Shao M, He J, Zhang R, Zhang X, Yang Y, Li C, et al. Interleukin-2 deficiency associated with renal impairment in systemic lupus erythematosus. J Interferon Cytokine Res. (2019) 39:117–24. doi: 10.1089/jir.2018.0016
234. He J, Zhang R, Shao M, Zhao X, Miao M, Chen J, et al. Efficacy and safety of low-dose IL-2 in the treatment of systemic lupus erythematosus: a randomised, double-blind, placebo-controlled trial. Ann Rheum Dis. (2020) 79:141–9. doi: 10.1136/annrheumdis-2019-215396
235. Li Y, Tang D, Yin L, and Dai Y. New insights for regulatory T cell in lupus nephritis. Autoimmun Rev. (2022) 21:103134. doi: 10.1016/j.autrev.2022.103134
236. Wang Q, Qian S, Li J, Che N, Gu L, Wang Q, et al. Combined transplantation of autologous hematopoietic stem cells and allogenic mesenchymal stem cells increases T regulatory cells in systemic lupus erythematosus with refractory lupus nephritis and leukopenia. Lupus. (2015) 24:1221–6. doi: 10.1177/0961203315583541
237. Goklemez S, Hasni S, Hakim FT, Muraro PA, Pirsl F, Rose J, et al. Long-term follow-up after lymphodepleting autologous haematopoietic cell transplantation for treatment-resistant systemic lupus erythematosus. Rheumatol (Oxford). (2022) 61:3317–28. doi: 10.1093/rheumatology/keab877
238. Wang D, Huang S, Yuan X, Liang J, Xu R, Yao G, et al. The regulation of the Treg/Th17 balance by mesenchymal stem cells in human systemic lupus erythematosus. Cell Mol Immunol. (2017) 14:423–31. doi: 10.1038/cmi.2015.89
239. Wooden B and Radhakrishnan J. The role of anti-B cell activating factor therapy for treating lupus nephritis. Clin J Am Soc Nephrol. (2022) 17:1583–5. doi: 10.2215/CJN.11340922
240. KDIGO. Clinical practice guideline for the management of LUPUS NEPHRITIS. Kidney Int. (2024) 105:S1–s69. doi: 10.1016/j.kint.2023.09.002
241. Cui YX, Fu CW, Jiang F, Ye LX, and Meng W. Association of the interleukin-6 polymorphisms with systemic lupus erythematosus: a meta-analysis. Lupus. (2015) 24:1308–17. doi: 10.1177/0961203315588971
242. Shirota Y, Yarboro C, Fischer R, Pham TH, Lipsky P, and Illei GG. Impact of anti-interleukin-6 receptor blockade on circulating T and B cell subsets in patients with systemic lupus erythematosus. Ann Rheum Dis. (2013) 72:118–28. doi: 10.1136/annrheumdis-2012-201310
243. KDIGO. Clinical practice guideline for the management of glomerular diseases. Kidney Int. (2021) 100:S1–s276. doi: 10.1016/j.kint.2021.05.021
244. Zampeli E, Klinman DM, Gershwin ME, and Moutsopoulos HM. A comprehensive evaluation for the treatment of lupus nephritis. J Autoimmun. (2017) 78:1–10. doi: 10.1016/j.jaut.2016.12.011
245. Anolik JH, Campbell D, Felgar RE, Young F, Sanz I, Rosenblatt J, et al. The relationship of FcgammaRIIIa genotype to degree of B cell depletion by rituximab in the treatment of systemic lupus erythematosus. Arthritis Rheum. (2003) 48:455–9. doi: 10.1002/art.10764
246. Mössner E, Brünker P, Moser S, Püntener U, Schmidt C, Herter S, et al. Increasing the efficacy of CD20 antibody therapy through the engineering of a new type II anti-CD20 antibody with enhanced direct and immune effector cell-mediated B-cell cytotoxicity. Blood. (2010) 115:4393–402. doi: 10.1182/blood-2009-06-225979
247. Tipton TR, Roghanian A, Oldham RJ, Carter MJ, Cox KL, Mockridge CI, et al. Antigenic modulation limits the effector cell mechanisms employed by type I anti-CD20 monoclonal antibodies. Blood. (2015) 125:1901–9. doi: 10.1182/blood-2014-07-588376
248. Freeman CL and Sehn LH. A tale of two antibodies: obinutuzumab versus rituximab. Br J Haematol. (2018) 182:29–45. doi: 10.1111/bjh.15232
249. Furie RA, Aroca G, Cascino MD, Garg JP, Rovin BH, Alvarez A, et al. B-cell depletion with obinutuzumab for the treatment of proliferative lupus nephritis: a randomised, double-blind, placebo-controlled trial. Ann Rheum Dis. (2022) 81:100–7. doi: 10.1136/annrheumdis-2021-220920
250. Lee EJ, Kwon OC, Ghang B, Lim DH, Kim DH, Hong S, et al. Immunoglobulin binding protein 1 as a potential urine biomarker in patients with lupus nephritis. Int J Mol Sci. (2019) 20(10):2606. doi: 10.3390/ijms20102606
251. Hoffman W, Lakkis FG, and Chalasani G. B cells, antibodies, and more. Clin J Am Soc Nephrol. (2016) 11:137–54. doi: 10.2215/CJN.09430915
252. Bilanges B, Posor Y, and Vanhaesebroeck B. PI3K isoforms in cell signalling and vesicle trafficking. Nat Rev Mol Cell Biol. (2019) 20:515–34. doi: 10.1038/s41580-019-0129-z
253. Yamaguchi J, Isnard P, Robil N, de la Grange P, Hoguin C, Schmitt A, et al. PIK3CA inhibition in models of proliferative glomerulonephritis and lupus nephritis. J Clin Invest. (2024) 134(15):e176402. doi: 10.1172/JCI176402
254. Peters AL, Stunz LL, and Bishop GA. CD40 and autoimmunity: the dark side of a great activator. Semin Immunol. (2009) 21:293–300. doi: 10.1016/j.smim.2009.05.012
255. Schönbeck U and Libby P. The CD40/CD154 receptor/ligand dyad. Cell Mol Life Sci. (2001) 58:4–43. doi: 10.1007/PL00000776
256. Chalmers SA, Ayilam Ramachandran R, Garcia SJ, Der E, Herlitz L, Ampudia J, et al. The CD6/ALCAM pathway promotes lupus nephritis via T cell-mediated responses. J Clin Invest. (2022) 132(1):e147334. doi: 10.1172/JCI147334
257. Roveta A, Parodi EL, Brezzi B, Tunesi F, Zanetti V, Merlotti G, et al. Lupus nephritis from pathogenesis to new therapies: an update. Int J Mol Sci. (2024) 25(16):8981. doi: 10.3390/ijms25168981
258. Rovin BH, Teng YKO, Ginzler EM, Arriens C, Caster DJ, Romero-Diaz J, et al. Efficacy and safety of voclosporin versus placebo for lupus nephritis (AURORA 1): a double-blind, randomised, multicentre, placebo-controlled, phase 3 trial. Lancet. (2021) 397:2070–80. doi: 10.1016/S0140-6736(21)00578-X
259. Saxena A, Ginzler EM, Gibson K, Satirapoj B, Santillán AEZ, Levchenko O, et al. Safety and efficacy of long-term voclosporin treatment for lupus nephritis in the phase 3 AURORA 2 clinical trial. Arthritis Rheumatol. (2024) 76:59–67. doi: 10.1002/art.42657
260. Jardine AG. Assessing the relative risk of cardiovascular disease among renal transplant patients receiving tacrolimus or cyclosporine. Transpl Int. (2005) 18:379–84. doi: 10.1111/j.1432-2277.2005.00080.x
261. Naesens M, Kuypers DR, and Sarwal M. Calcineurin inhibitor nephrotoxicity. Clin J Am Soc Nephrol. (2009) 4:481–508. doi: 10.2215/CJN.04800908
262. Farouk SS and Rein JL. The many faces of calcineurin inhibitor toxicity-what the FK? Adv Chronic Kidney Dis. (2020) 27:56–66. doi: 10.1053/j.ackd.2019.08.006
263. Roy J and Cyert MS. Identifying new substrates and functions for an old enzyme: calcineurin. Cold Spring Harb Perspect Biol. (2020) 12(3):a035436. doi: 10.1101/cshperspect.a035436
264. De Vriese AS, Sethi S, and Fervenza FC. Lupus nephritis: redefining the treatment goals. Kidney Int. (2025) 107:198–211. doi: 10.1016/j.kint.2024.10.018
265. Mok CC, Teng YKO, Saxena R, and Tanaka Y. Treatment of lupus nephritis: consensus, evidence and perspectives. Nat Rev Rheumatol. (2023) 19:227–38. doi: 10.1038/s41584-023-00925-5
266. Almaani S, Meara A, and Rovin BH. Update on lupus nephritis. Clin J Am Soc Nephrol. (2017) 12:825–35. doi: 10.2215/CJN.05780616
267. Ortega LM, Schultz DR, Lenz O, Pardo V, and Contreras GN. Review: Lupus nephritis: pathologic features, epidemiology and a guide to therapeutic decisions. Lupus. (2010) 19:557–74. doi: 10.1177/0961203309358187
268. Parikh SV, Almaani S, Brodsky S, and Rovin BH. Update on lupus nephritis: core curriculum 2020. Am J Kidney Dis. (2020) 76:265–81. doi: 10.1053/j.ajkd.2019.10.017
269. Parikh SV and Rovin BH. Current and emerging therapies for lupus nephritis. J Am Soc Nephrol. (2016) 27:2929–39. doi: 10.1681/ASN.2016040415
270. Rojas-Rivera JE, García-Carro C, Ávila AI, Espino M, Espinosa M, Fernández-Juárez G, et al. Diagnosis and treatment of lupus nephritis: a summary of the Consensus Document of the Spanish Group for the Study of Glomerular Diseases (GLOSEN). Clin Kidney J. (2023) 16:1384–402. doi: 10.1093/ckj/sfad055
271. Wang S, Spielman A, Ginsberg M, Petri M, Rovin BH, Buyon J, et al. Short- and long-term progression of kidney involvement in systemic lupus erythematosus patients with low-grade proteinuria. Clin J Am Soc Nephrol. (2022) 17:1150–8. doi: 10.2215/CJN.01280122
272. Rich SA. De novo synthesis and secretion of a 36-kD protein by cells that form lupus inclusions in response to alpha-interferon. J Clin Invest. (1995) 95:219–26. doi: 10.1172/JCI117643
273. Bajema IM, Wilhelmus S, Alpers CE, Bruijn JA, Colvin RB, Cook HT, et al. Revision of the International Society of Nephrology/Renal Pathology Society classification for lupus nephritis: clarification of definitions, and modified National Institutes of Health activity and chronicity indices. Kidney Int. (2018) 93:789–96. doi: 10.1016/j.kint.2017.11.023
274. Gasparotto M, Gatto M, Binda V, Doria A, and Moroni G. Lupus nephritis: clinical presentations and outcomes in the 21st century. Rheumatol (Oxford). (2020) 59:v39–51. doi: 10.1093/rheumatology/keaa381
275. Weening JJ, D'Agati VD, Schwartz MM, Seshan SV, Alpers CE, Appel GB, et al. The classification of glomerulonephritis in systemic lupus erythematosus revisited. Kidney Int. (2004) 65:521–30. doi: 10.1111/j.1523-1755.2004.00443.x
276. Furness PN and Taub N. Interobserver reproducibility and application of the ISN/RPS classification of lupus nephritis-a UK-wide study. Am J Surg Pathol. (2006) 30:1030–5. doi: 10.1097/00000478-200608000-00015
277. Kawai T and Akira S. TLR signaling. Semin Immunol. (2007) 19:24–32. doi: 10.1016/j.smim.2006.12.004
278. Liao Z, Ye Z, Xue Z, Wu L, Ouyang Y, Yao C, et al. Identification of renal long non-coding RNA RP11-2B6.2 as a positive regulator of type I interferon signaling pathway in lupus nephritis. Front Immunol. (2019) 10:975. doi: 10.3389/fimmu.2019.00975
279. Li Q and Verma IM. NF-kappaB regulation in the immune system. Nat Rev Immunol. (2002) 2:725–34. doi: 10.1038/nri910
280. Liu T, Zhang L, Joo D, and Sun SC. NF-κB signaling in inflammation. Signal Transduct Target Ther. (2017) 2:17023. doi: 10.1038/sigtrans.2017.23
281. Zhang H, Fu R, Guo C, Huang Y, Wang H, Wang S, et al. Anti-dsDNA antibodies bind to TLR4 and activate NLRP3 inflammasome in lupus monocytes/macrophages. J Transl Med. (2016) 14:156. doi: 10.1186/s12967-016-0911-z
282. Goropevšek A, Holcar M, and Avčin T. The role of STAT signaling pathways in the pathogenesis of systemic lupus erythematosus. Clin Rev Allergy Immunol. (2017) 52:164–81. doi: 10.1007/s12016-016-8550-y
283. Abroun S, Saki N, Ahmadvand M, Asghari F, Salari F, and Rahim F. STATs: an old story, yet mesmerizing. Cell J. (2015) 17:395–411. doi: 10.22074/cellj.2015.1
284. Shang Y, Smith S, and Hu X. Role of Notch signaling in regulating innate immunity and inflammation in health and disease. Protein Cell. (2016) 7:159–74. doi: 10.1007/s13238-016-0250-0
285. Zhou B, Lin W, Long Y, Yang Y, Zhang H, Wu K, et al. Notch signaling pathway: architecture, disease, and therapeutics. Signal Transduct Target Ther. (2022) 7:95. doi: 10.1038/s41392-022-00934-y
286. Cheng HT and Kopan R. The role of Notch signaling in specification of podocyte and proximal tubules within the developing mouse kidney. Kidney Int. (2005) 68:1951–2. doi: 10.1111/j.1523-1755.2005.00627.x
287. Vooijs M, Ong CT, Hadland B, Huppert S, Liu Z, Korving J, et al. Mapping the consequence of Notch1 proteolysis in vivo with NIP-CRE. Development. (2007) 134:535–44. doi: 10.1242/dev.02733
288. Waters AM, Wu MY, Onay T, Scutaru J, Liu J, Lobe CG, et al. Ectopic notch activation in developing podocytes causes glomerulosclerosis. J Am Soc Nephrol. (2008) 19:1139–57. doi: 10.1681/ASN.2007050596
289. Liu M, Liang K, Zhen J, Zhou M, Wang X, Wang Z, et al. Sirt6 deficiency exacerbates podocyte injury and proteinuria through targeting Notch signaling. Nat Commun. (2017) 8:413. doi: 10.1038/s41467-017-00498-4
290. Guo A, Sun Y, Xu X, and Xing Q. MicroRNA-30a targets notch1 to alleviate podocyte injury in lupus nephritis. Immunol Invest. (2022) 51:1694–706. doi: 10.1080/08820139.2022.2027440
291. Li LS and Liu ZH. Epidemiologic data of renal diseases from a single unit in China: analysis based on 13,519 renal biopsies. Kidney Int. (2004) 66:920–3. doi: 10.1111/j.1523-1755.2004.00837.x
292. Quillard T and Charreau B. Impact of notch signaling on inflammatory responses in cardiovascular disorders. Int J Mol Sci. (2013) 14:6863–88. doi: 10.3390/ijms14046863
293. Zhang Q, Shan Y, Shen L, Ni Q, Wang D, Wen X, et al. Renal remodeling by CXCL10-CXCR3 axis-recruited mesenchymal stem cells and subsequent IL4I1 secretion in lupus nephritis. Signal Transduct Target Ther. (2024) 9:325. doi: 10.1038/s41392-024-02018-5
294. Gao J, Wu L, Wang S, and Chen X. Role of chemokine (C-X-C motif) ligand 10 (CXCL10) in renal diseases. Mediators Inflammation. (2020) 2020:6194864. doi: 10.1155/2020/6194864
295. Reddy PS, Legault HM, Sypek JP, Collins MJ, Goad E, Goldman SJ, et al. Mapping similarities in mTOR pathway perturbations in mouse lupus nephritis models and human lupus nephritis. Arthritis Res Ther. (2008) 10:R127. doi: 10.1186/ar2541
296. Henley T, Kovesdi D, and Turner M. B-cell responses to B-cell activation factor of the TNF family (BAFF) are impaired in the absence of PI3K delta. Eur J Immunol. (2008) 38:3543–8. doi: 10.1002/eji.200838618
297. Shor B, Cavender D, and Harris C. A kinase-dead knock-in mutation in mTOR leads to early embryonic lethality and is dispensable for the immune system in heterozygous mice. BMC Immunol. (2009) 10:28. doi: 10.1186/1471-2172-10-28
298. Fruman DA. Phosphoinositide 3-kinase and its targets in B-cell and T-cell signaling. Curr Opin Immunol. (2004) 16:314–20. doi: 10.1016/j.coi.2004.03.014
299. Wu D, Ai L, Sun Y, Yang B, Chen S, Wang Q, et al. Role of NLRP3 inflammasome in lupus nephritis and therapeutic targeting by phytochemicals. Front Pharmacol. (2021) 12:621300. doi: 10.3389/fphar.2021.621300
300. Zhao Y, Zhang AP, Bao BY, Fan H, and Yang XY. Sirt1 protects lupus nephritis by inhibiting the NLRP3 signaling pathway in human glomerular mesangial cells. Open Life Sci. (2025) 20:20221038. doi: 10.1515/biol-2022-1038
301. Ma ZZ, Sun HS, Lv JC, Guo L, and Yang QR. Expression and clinical significance of the NEK7-NLRP3 inflammasome signaling pathway in patients with systemic lupus erythematosus. J Inflammation (Lond). (2018) 15:16. doi: 10.1186/s12950-018-0192-9
302. Ryge J, Winther O, Wienecke J, Sandelin A, Westerdahl AC, Hultborn H, et al. Transcriptional regulation of gene expression clusters in motor neurons following spinal cord injury. BMC Genomics. (2010) 11:365. doi: 10.1186/1471-2164-11-365
303. Hayden MS and Ghosh S. Signaling to NF-kappaB. Genes Dev. (2004) 18:2195–224. doi: 10.1101/gad.1228704
304. Doerner AM and Zuraw BL. TGF-beta1 induced epithelial to mesenchymal transition (EMT) in human bronchial epithelial cells is enhanced by IL-1beta but not abrogated by corticosteroids. Respir Res. (2009) 10:100. doi: 10.1186/1465-9921-10-100
305. Moustakas A, Souchelnytskyi S, and Heldin CH. Smad regulation in TGF-beta signal transduction. J Cell Sci. (2001) 114:4359–69. doi: 10.1242/jcs.114.24.4359
306. Thompson CB. Distinct roles for the costimulatory ligands B7–1 and B7–2 in T helper cell differentiation? Cell. (1995) 81:979–82. doi: 10.1016/S0092-8674(05)80001-7
307. King CL, Xianli J, June CH, Abe R, and Lee KP. CD28-deficient mice generate an impaired Th2 response to Schistosoma mansoni infection. Eur J Immunol. (1996) 26:2448–55. doi: 10.1002/eji.1830261027
308. Hart DN. Dendritic cells: unique leukocyte populations which control the primary immune response. Blood. (1997) 90:3245–87. doi: 10.1182/blood.V90.9.3245
309. Zang X and Allison JP. The B7 family and cancer therapy: costimulation and coinhibition. Clin Cancer Res. (2007) 13:5271–9. doi: 10.1158/1078-0432.CCR-07-1030
Keywords: lupus nephritis, podocytes, tubular epithelial cells, immune cells, immune responses
Citation: Chen J, Chen Z, Mou X, Rui K and Tian J (2025) Podocyte, tubular epithelial-immune cell interplay in the pathogenesis of lupus nephritis. Front. Immunol. 16:1682075. doi: 10.3389/fimmu.2025.1682075
Received: 08 August 2025; Accepted: 03 November 2025; Revised: 13 September 2025;
Published: 25 November 2025.
Edited by:
Ana Belén Arroyo, Santa Lucía University General Hospital, SpainReviewed by:
Kayaho Maeda, Nagoya University, JapanWadih Issa, University of Texas Southwestern Medical Center, United States
Copyright © 2025 Chen, Chen, Mou, Rui and Tian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ke Rui, cnVpa2VAdWpzLmVkdS5jbg==; Jie Tian, dGlhbmppZUB1anMuZWR1LmNu; Xiao Mou, MTAwMDAxMjExNEB1anMuZWR1LmNu
†These authors have contributed equally to this work
 Jingyi Chen1,2†
Jingyi Chen1,2† Zixiang Chen
Zixiang Chen Ke Rui
Ke Rui Jie Tian
Jie Tian