Abstract
Epidural hematoma typically manifests following craniocerebral trauma, stemming from injury to the meningeal artery or venous system, predominantly on one side. Instances of spontaneous epidural hematoma are uncommon, with occurrences of spontaneous bilateral epidural hematoma being exceedingly rare. Sickle cell disease, adjacent paranasal sinusitis, and tumor metastases are the most prevalent causes of spontaneous epidural hematoma. This case study presents an individual with abdominal liposarcoma exhibiting reduced coagulation factor XII activity, who experienced sudden unconsciousness due to spontaneous acute bilateral epidural hematoma, and subsequently achieved a favorable outcome following surgical intervention.
Introduction
An intracranial acute epidural hematoma (AEDH) commonly arises in the space between the skull and the dura mater following a skull fracture, due to the rupture of the middle meningeal artery or venous system as a result of head trauma (1). Non-traumatic acute epidural hematoma, also referred to as spontaneous acute epidural hematoma, is a rare occurrence with less than 100 reported cases documented in current literature (1–5). Spontaneous epidural hematoma typically presents unilaterally, with bilateral occurrences being exceedingly rare, as evidenced by only approximately 13 reported cases (2, 4, 6–16) (Table 1). This condition is commonly linked to various underlying pathologies, such as adjacent infection, extradural metastasis, dural vascular malformations, and coagulation disorders (17). The present study details a unique case of spontaneous acute bilateral epidural hematoma following abdominal liposarcomatosis and prolonged exudate of digestive juices, characterized by decreased activity of coagulation factor XII. The patient experienced sudden loss of consciousness, but achieved favorable outcomes following surgical intervention.
Table 1
| Authors & Year | Age | Sex | Site of EDH | Cause of EDH | |
|---|---|---|---|---|---|
| 1 | Kuwayama et al., 1985 (6) | 21 | Female | Temporal | Hypofibrinogenemia |
| 2 | Ishige et al., 1985 (7) | 34 | Male | Parietal & Occipital | SLE |
| 3 | Charles et al., 1987 (8) | 34 | Male | Occipital | Alcoholic brain atrophy |
| 4 | Grabel et al., 1989 (9) | 2 | Male | Unknown | Temporal |
| 5 | Dufour et al., 2001 (10) | 36 | Female | Parietal | Cavernous hemangioma |
| 6 | Melike et al., 2004 (11) | 9 | Male | Parietal | Eosinophilic granuloma of skull |
| 7 | Ng et al., 2004 (12) | 23 | Female | Frontal | Unknown |
| 8 | Verma et al., 2007 (13) | 3 | Male | Frontal | Scurvy |
| 9 | Li et al., 2012 (14) | 14 | Female | Temporal & parietal | Low intracranial pressure |
| 10 | Hettige et al., 2015 (15) | 7 | Female | Temporal | Sickle cell disease |
| 11 | Khursheed et al., 2017 (16) | 40 | Male | Frontal | Chronic kidney disease |
| 12 | Lin et al., 2023 (4) | 21 | Male | Frontal | Chronic sinusitis |
| 13 | Aljohani et al., 2024 (2) | 10 | Female | Parietal | Sickle cell disease |
Reported cases of spontaneous bilateral epidural hematomas.
Case presentation
A 45-year-old female patient was admitted to the local hospital 5 years ago due to persistent weight loss. Upon examination, extensive thickening of the abdominal colon, small intestine, mesentery, and greater omentum was observed, leading to the performance of surgical intervention. Postoperative pathology revealed a diagnosis of highly differentiated liposarcoma, prompting the initiation of adjuvant therapy. However, over 1 month following the operation, the patient experienced anastomotic abdominal wall leakage, resulting in the leakage of digestive juices through the skin. Despite repeated surgical repairs, there was no improvement in the patient’s condition. The patient was readmitted to the anorectal surgery department of our hospital due to an escalation of intestinal leakage. While hospitalized, the patient experienced sudden and persistent frontal pain in the evening, followed by unconsciousness and bilateral pupil dilation, with a Glasgow Coma Scale score of 7 (E1 + V1 + M5). An urgent head CT scan revealed a “double frontal epidural hematoma” (Figure 1), prompting emergency “craniotomy hematoma removal.” The patient had no history of trauma, nor did she have any family history of genetic disorders. Additionally, she had not taken anticoagulant drugs or oral contraceptives. During the surgical procedure, no apparent scalp or skull trauma was observed. Upon opening the skull, a significant epidural hematoma was discovered on both frontal lobes (Figure 2). There were no indications of dural vascular abnormalities or tumor metastasis, and no abnormal blood coagulation was noted on the day of the operation. Subsequent analysis of coagulation factors post-operation revealed a decrease in the activity of multiple factors. However, in subsequent follow-up examinations, it was observed that the activity of the other factors had returned to normal levels exception of factor XII (Table 2). The antinuclear antibodies, autoimmune disease-related antibodies, and thromboelastogram all exhibited normal results, except for a minor elevation in anti-Ro-52 antibody levels.
Figure 1

Preoperative intracranial epidural hematoma is shown from different sections: (A) cross-section, (B) sagittal section.
Figure 2
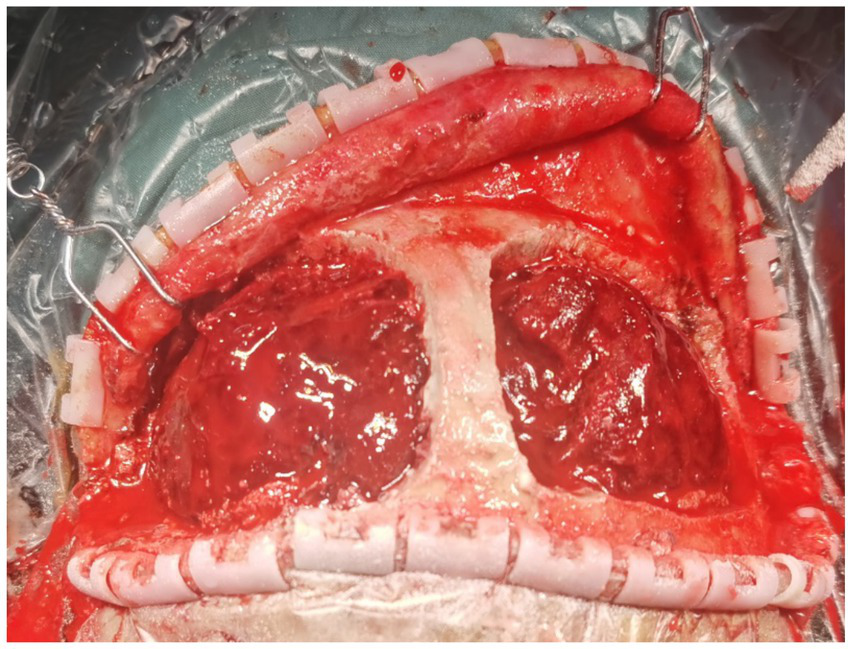
Intraoperatively, after opening the bilateral frontal bone flaps adjacent to the sagittal sinus, a large amount of epidural hematoma is observed.
Table 2
| Coagulation factor activity | 2023-11-24 | 2023-12-01 | 2023-12-15 |
|---|---|---|---|
| II (Factor II) | 61.3% (Low) | 84.8% (Normal) | 88.4% (Normal) |
| V (Factor V) | 79.3% (Normal) | 126.3% (High) | 98.7% (Normal) |
| VII (Factor VII) | 84.3% (Normal) | 72.7% (Normal) | 87.8% (Normal) |
| IX (Factor IX) | 61.7% (Low) | 77.3% (Normal) | 83.1% (Normal) |
| X (Factor X) | 69.9% (Low) | 84.2% (Normal) | 89.4% (Normal) |
| XI (Factor XI) | 43.7% (Low) | 69.8% (Low) | 88.9% (Normal) |
| XII (Factor XII) | 34.3% (Low) | 36.1% (Low) | 38.6% (Low) |
The results of coagulation factor activity assessed on the day of surgery and during two subsequent postoperative follow-up visits.
Following the surgical procedure, the patients exhibited restored consciousness, satisfactory limb movement, and absence of neurological deficits. Postoperative CT imaging confirmed successful clearance of the hematoma (Figure 3). At the six-month follow-up, the patients continued to recover without any recurrence of acute epidural hematoma.
Figure 3

Postoperatively, a cranial CT scan was performed: (A) cross-section, (B) sagittal section.
Discussion
Intracranial epidural hematoma is a relatively rare yet grave consequence of head trauma, often presenting concurrently with skull fracture and suture diastasis. Although its precise prevalence remains undetermined, estimates suggest it comprises 1–4% of traumatic head injury cases and 5–15% of postmortem examinations (17). Spontaneous occurrences of epidural hematoma are infrequent but constitute a particularly uncommon neurological emergency necessitating prompt evaluation and intervention (18).
In a comprehensive analysis of 77 cases of intracranial spontaneous acute epidural hematoma, Sickle cell disease (SCD), adjacent sinusitis, and metastatic hepatocellular carcinoma (HCC) were identified as the predominant etiologies, accounting for 32.5, 22.1, and 19.5% of cases, respectively (1). The suggested pathophysiological mechanisms underlying acute epidural hematoma in the context of SCD involve bone infarction, microfractures resulting from hematopoietic dilatation, and blood leakage due to the accumulation of sickle cells within the plate barrier vein (2). The presence of diffuse inflammation in the paranasal sinuses can lead to the infiltration of air into the epidural space from the sinuses, causing the separation of the dura mater from the skull. Sinusitis can progress to involve the meningeal artery wall through the blood vessels in the cranial plate barrier, resulting in hemorrhage from a weakened meningeal artery entering the epidural space (4). Cases of acute epidural hematoma (AEDH) have been reported in patients with metastatic tumors in the skull, such as those originating from lung, ovarian, esophageal, Ewing’s sarcoma, and Langerhans cell histiocytosis. While metastasis to the skull is a common occurrence in patients with lung, breast, and prostate cancer, it is relatively rare in patients with hepatocellular carcinoma (HCC) (8). However, cases of spontaneous acute epidural hematoma caused by tumor metastasis are predominantly associated with metastatic foci of HCC, a recognized risk factor for bleeding. When cancer cells metastasize to the dura mater or skull instead of the brain parenchyma, metastatic bleeding can extend to the epidural space (3).
Among the cohort of 14 patients diagnosed with bilateral spontaneous epidural hematoma, including the case under consideration, the etiology varied, with a higher prevalence in younger individuals and a lack of specificity in the hematoma’s location.
The patient under consideration in this case study presents with abdominal liposarcoma of high differentiation. While tumor metastasis can potentially result in epidural hematoma, there have been no documented instances of epidural hemorrhage stemming from liposarcoma metastasis. Furthermore, both the patient’s CT scans and intraoperative observations do not indicate evidence of tumor metastasis. The patient has a prolonged history of intestinal fistula following a previous abdominal liposarcoma operation; however, pre-and post-operative coagulation function tests reveal no significant abnormalities in PT, APTT, INR, or other relevant parameters. The sole anomaly observed in this patient was a reduction in coagulation factor XII activity. Acquired FXII deficiency is linked to diminished synthesis (as seen in liver disease), heightened loss (as seen in nephrotic syndrome), and excessive consumption (as seen in endotoxin-induced septicemia or disseminated intravascular coagulation), along with other coagulation irregularities. Instances of specific FXII inhibitors are uncommon. Additionally, FXII is spontaneously converted to FXIIa upon interaction with a negatively charged surface, contributing to the physiological mechanism of blood coagulation and serving a crucial role in anti-thrombotic and promoting fibrinolysis processes. Due to the crucial involvement of FXII in the endogenous coagulation pathway, its deficiency results in a marked prolongation of APTT. FXII deficiency typically does not predispose individuals to spontaneous bleeding, and there have been no reported instances of intracranial hemorrhage associated with this condition. Following a six-month follow-up period, the patient exhibited satisfactory recovery, apart from an abdominal intestinal fistula issue. Despite this, there was no recurrence of spontaneous intracranial hemorrhage. Consequently, the etiology of acute spontaneous epidural hematoma in this patient remains unclear.
Conclusion
While the occurrence of spontaneous acute intracranial epidural hematoma is rare, the rapid progression of the clinical course is attributed to heightened intracranial pressure and brain compression resulting from the hematoma. Timely craniotomy can lead to complete recovery from the hematoma. However, further investigation is required to identify the underlying cause of spontaneous bleeding and to implement appropriate treatment to prevent disease recurrence. Our medical records suggest that XII coagulation factor may play a role in spontaneous intracranial hemorrhage, which is worthy of our further study.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Zhejiang Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
ZT: Writing – original draft. MW: Funding acquisition, Validation, Writing – review & editing. TX: Visualization, Writing – review & editing. WL: Formal analysis, Writing – review & editing. HS: Data curation, Supervision, Writing – review & editing. JM: Project administration, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Natural Science Foundation of Zhejiang Province (LY21H090008) and Key Project Jointly Built by Zhejiang Province and the Ministry (WKJ-ZJ-2340).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Koketsu Y Tanei T Kato T Naito T Okada K Ito R et al . Intracranial idiopathic acute epidural hematoma presenting with a stroke-like attack and rapid neurological deterioration: a case report. NMC Case Rep J. (2022) 9:25–30. doi: 10.2176/jns-nmc.2021-0330
2.
Aljohani OI Almustafa RN Almalki BT Allehaibi MH . Non-traumatic bilateral epidural hematoma in a child with sickle cell anemia: a case report and a review of the literature. Childs Nerv Syst. (2024) 40:925–31. doi: 10.1007/s00381-023-06235-1
3.
Ahn KH Ryu HS Han MS Choi YD Joo SP . Spontaneous acute epidural hematoma associated with metastatic hepatocellular carcinoma: a case report. Korean J Neurotrauma. (2023) 19:384. doi: 10.13004/kjnt.2023.19.e40
4.
Yao L Luo Z Zhou Y Huang C Fang X Jiang X et al . Spontaneous bilateral epidural hematomas caused by chronic sinusitis: illustrative case. J Neurosurg Case Lessons. (2023) 5:CASE2310. doi: 10.3171/CASE2310
5.
Almesedin GS Alshmaily HO Alshammari KA Albalawi RS . Two case reports of Glanzmann thrombasthenia with intracranial hemorrhage and a review of the literature. Surg Neurol Int. (2023) 14:448. doi: 10.25259/SNI_680_2023
6.
Kuwayama N Takahashi S Sonobe M Sugita K . Spontaneous bilateral extradural hematomas. Case report. J Neurosurg. (1985) 62:139–41. doi: 10.3171/jns.1985.62.1.0139
7.
Ishige N Sunami K Sato A Watanabe O Sakurada M Ishihara K . A case of systemic lupus erythematosus associated with spontaneous bilateral epidural hematomas. No Shinkei Geka. (1985) 13:345–9. PMID:
8.
Agbi CB Victoratos G Turnbull IW . Bilateral extradural hematoma extending from the foramen magnum to the vertex. Surg Neurol. (1987) 28:123–8. doi: 10.1016/0090-3019(87)90085-1
9.
Grabel JC Sacher M Rothman AS . Bilateral extradural hematomas in a thrombocytopenic infant receiving anticoagulants_ case report. Neurosurgery. (1989) 25:828–30. doi: 10.1097/00006123-198911000-00024
10.
Dufour H Manera L Fuentes S do L Grisoli F . Spontaneous vertex extradural hematoma: considerations about causes. Case report and review of the literature. J Neurosurg. (2001) 94:633–6. doi: 10.3171/jns.2001.94.4.0633
11.
Mut M Cataltepe O Bakar B Cila A Akalan N . Eosinophilic granuloma of the skull associated with epidural haematoma: a case report and review of the literature. Childs Nerv Syst. (2004) 20:765–9. doi: 10.1007/s00381-004-0913-7
12.
Ng WH Yeo TT Seow WT . Non-traumatic spontaneous acute epidural haematoma – report of two cases and review of the literature. J Clin Neurosci. (2004) 11:791–4. doi: 10.1016/j.jocn.2003.12.002
13.
Verma S Sivanandan S Aneesh MK Gupta V Seth R Kabra S . Unilateral proptosis and extradural hematoma in a child with scurvy. Pediatr Radiol. (2007) 37:937–9. doi: 10.1007/s00247-007-0543-9
14.
Li Z-J Sun P Dou Y-H Lan X-L Xu J Zhang C-Y et al . Bilateral supratentorial epidural hematomas: a rare complication in adolescent spine surgery. Neurol Med Chir (Tokyo). (2012) 52:646–8. doi: 10.2176/nmc.52.646
15.
Hettige S Sofela A Bassi S Chandler C . A review of spontaneous intracranial extradural hematoma in sickle-cell disease. Acta Neurochir. (2015) 157:2025–9; discussion 2029. doi: 10.1007/s00701-015-2582-6
16.
Khan KA Sharma S Purohit D . Spontaneous extradural hematoma: a rare entity. Br J Neurosurg. (2017) 34:86–8. doi: 10.1080/02688697.2017.1409882
17.
Ruschel LG do Rego FMM Milano JB Jung GS Silva Jr LF Ramina R et al . Spontaneous intracranial epidural hematoma during rivaroxaban treatment. Rev Assoc Med Bras (1992). (2016) 62:721–4. doi: 10.1590/1806-9282.62.08.721
18.
Bullock MR Chesnut R Ghajar J Gordon D Hartl R W Newell D et al . Surgical management of acute epidural hematomas. Neurosurgery. (2006) 58:S2-7–S2-15. doi: 10.1227/01.NEU.0000210363.91172.A8
Summary
Keywords
intracranial, spontaneous, non-traumatic, epidural hematoma, coagulation factor XII
Citation
Tang Z, Wang M, Xiong T, Liu W, Sun H and Ma J (2024) A case of spontaneous bilateral epidural hematoma associated with decreased coagulation factor XII activity: case report and literature review. Front. Neurol. 15:1460073. doi: 10.3389/fneur.2024.1460073
Received
05 July 2024
Accepted
09 September 2024
Published
23 September 2024
Volume
15 - 2024
Edited by
Xuejian Wang, Affiliated Hospital 2 of Nantong University, China
Reviewed by
Kwaku Nyame, Komfo Anokye Teaching Hospital (KATH), Ghana
Fulvio Tartara, University Hospital of Parma, Italy
Updates
Copyright
© 2024 Tang, Wang, Xiong, Liu, Sun and Ma.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiangchun Ma, mjc588@163.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.