- 1Department of Orthopaedics, Santai People’s Hospital, Mianyang, China
- 2Department of Orthopaedics, The Sixth People’s Hospital of Chengdu, Chengdu, China
- 3Department of Orthopaedics, The Affiliated Hospital of Southwest Medical University, Luzhou, China
- 4Department of Rehabilitation, The Third Hospital of Mianyang, Sichuan Mental Health Center, Mianyang, China
Introduction: Traumatic fractures of the vertebral bodies in the thoracolumbar region are the most common type of spinal fractures. Some studies suggest that neurological deficits associated with these fractures may be linked to spinal canal compromise, kyphosis angle, and other factors. However, this relationship remains controversial. The present study aimed to identify the risk factors for neurologic deficits following thoracolumbar burst fractures (TBF).
Methods: This study included 322 patients with TBF, comprising 115 patients with lamina fractures (LF) and 207 patients without lamina fractures (NLF). Neurological deficits were classified according to the American Spinal Injury Association (ASIA) classification, with 75 patients exhibiting neurological deficits and 247 patients without deficits. Clinical data, ASIA classification, and imaging findings were analyzed and compared between the two groups. Risk factors were assessed using logistic regression.
Results: Compared with the NLF group, the LF group had higher ASIA classification scores (P < 0.05). Multivariate logistic regression identified laminar fracture (OR: 0.019, 95% CI: 0.005–0.070, P < 0.000), car accident (OR: 6.082, 95% CI: 1.248–29.636, P = 0.025), and falling accident (OR: 8.429, 95% CI: 2.143–33.153, P = 0.002) as independent variables associated with neurologic deficit. Additionally, the ROC curve revealed that laminar fractures and falling accidents had a high risk association value. A risk association equation, Logit (P) = −4.358 + 3.535 × laminar fracture – 1.353 × falling accidents, was established based on the high-value indicators.
Conclusion: Laminar fractures, car accidents, and falls were identified as independent risk factors for neurological deficits following TBF. Additionally, laminar fractures and falls demonstrated a high risk association value. These findings provide valuable insights for optimizing rehabilitation strategies and guiding surgical decision-making.
Introduction
Studies show that traumatic burst fractures of the thoracolumbar spine are the most prevalent type of spinal injury (1). These fractures involve the anterior and middle columns of the spine, with or without involvement of the posterior column (2). However, they can also result in disruption of the vertebral lamina and lead to spinal cord injury.
Thoracolumbar burst fractures (TBF) usually result from axial load mechanisms, which concentrate pressure on the medial column of the spine, leading to a widening of the gap between the pedicles and potentially causing a vertical laminar fracture. Laminar fractures, also known as “greenstick fractures,” typically occur in the ventral cortex of the lamina (3). Reports have shown a correlation between laminar fractures and dural tears (4). However, the role of laminar fractures in neurologic deficits is often underestimated, as the course of the injury is dynamic, and the lamina plays a crucial role in assessing stability across the fracture segment.
There are fewer relevant studies focusing on the risk factors for neurological deficits after TBF. In this study, we analyzed and compared patients’ clinical data, neurological deficit classification, and imaging findings, and assessed the risk factors using logistic regression. A better understanding of the risk-associated factors for neurological deficits following TBF enables clinicians to provide more accurate information to patients and their families and to develop more tailored treatment and rehabilitation programs based on expected outcomes.
Materials and methods
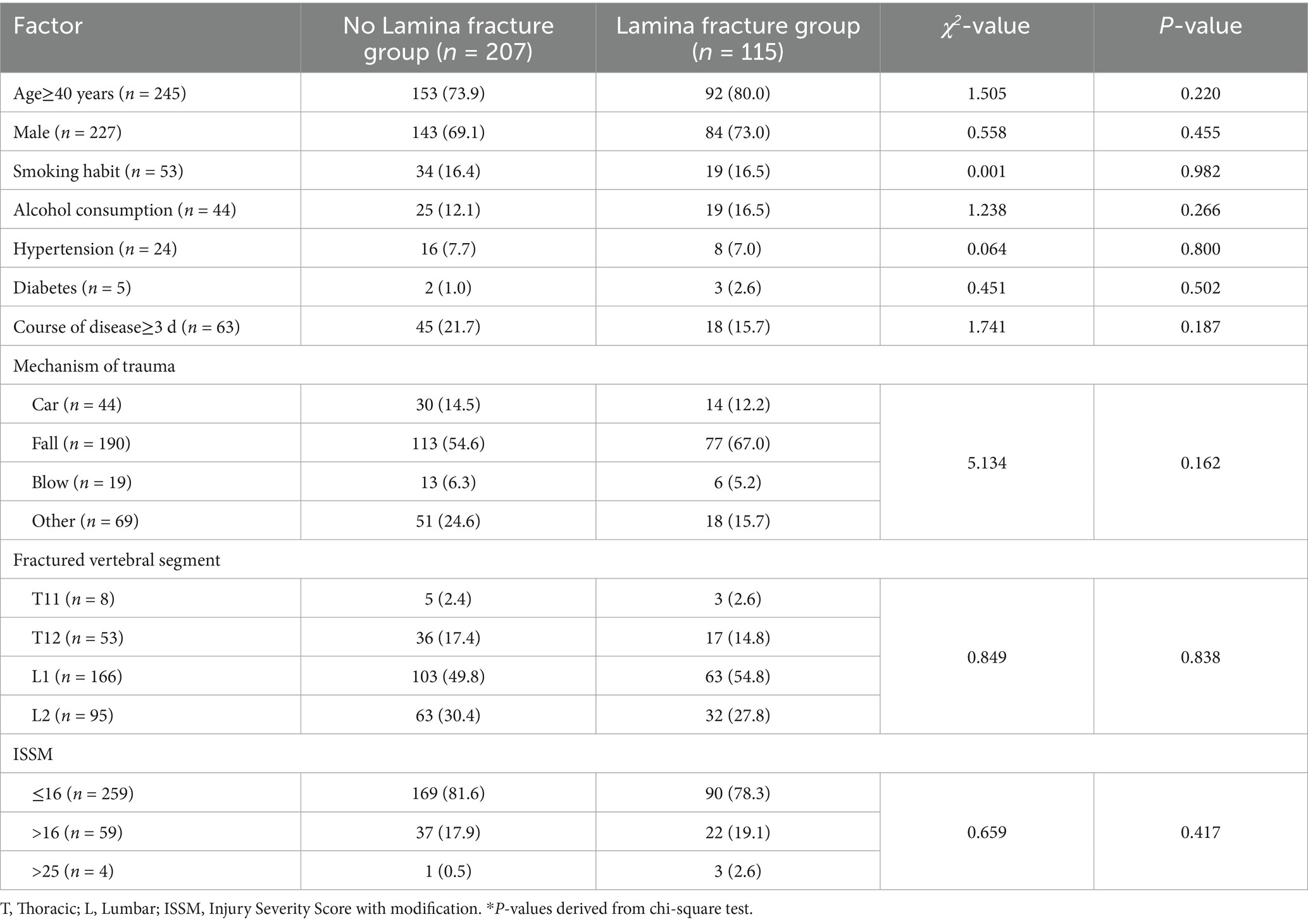
This study adhered to the principles outlined in the Helsinki Declaration and received approval from our institution’s medical ethics committee. Due to the retrospective nature of the study, the ethics committee waived the requirement for informed consent. We conducted a retrospective analysis of 322 patients with TBF who were admitted to our institution between November 2012 and November 2022. Among them, 115 had laminar fractures (LF), and 207 had no laminar fractures (NLF). Neurological deficits were classified according to the American Spinal Injury Association (ASIA) classification upon patient admission to the hospital (5). Patients with neurological deficits (ASIA A, ASIA B, ASIA C, and ASIA D) were grouped together and compared with those without neurological deficits (ASIA E), comprising 75 and 247 patients, respectively. The inclusion criteria were as follows: (1) TBF diagnosed according to Denis’ classification system (2); (2) a clear history of trauma; (3) fracture segment located between T11 and L2; and (4) clearly documented ASIA grading. The exclusion criteria included: (1) multiple contiguous or non-contiguous spinal fractures; (2) pathological or old fractures; (3) pre-existing neurological deficits; (4) penetrating injuries; and (5) incomplete clinical data.
After screening the cases that met the inclusion criteria, we collected and compared each patient’s age, gender, smoking status, alcohol consumption, history of hypertension and diabetes, disease duration, mechanism of trauma, fractured vertebral segment, ISSM score, ASIA classification, and presence of laminar fracture. The injury mechanisms included blows from falling objects, car accidents, falls, and other causes. Trauma severity was assessed using the Injury Severity Score (ISS) (6), which was determined based on the Abbreviated Injury Scale-2005 (7). In this study, to investigate the relationship between laminar fractures and neurological deficits, components related to neurological deficits and laminar fractures were excluded from the ISS calculation, resulting in a modified score, the ISSM.
Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences (SPSS) software version 23 and visualized with GraphPad Prism 9 software. Continuous variables were expressed as mean ± standard deviation (SD), and between-group comparisons were performed using independent t-tests. Categorical variables were presented as counts and percentages, with comparisons assessed using the chi-square test. Ordinal data were analyzed using the Kruskal-Wallis test. Binary logistic regression was conducted to identify risk factors. The Hosmer-Lemeshow test was used to evaluate the model’s goodness-of-fit, and the receiver operating characteristic (ROC) curve was analyzed to assess discrimination. All statistical tests were two-tailed, and a P-value < 0.05 was considered statistically significant.
Results
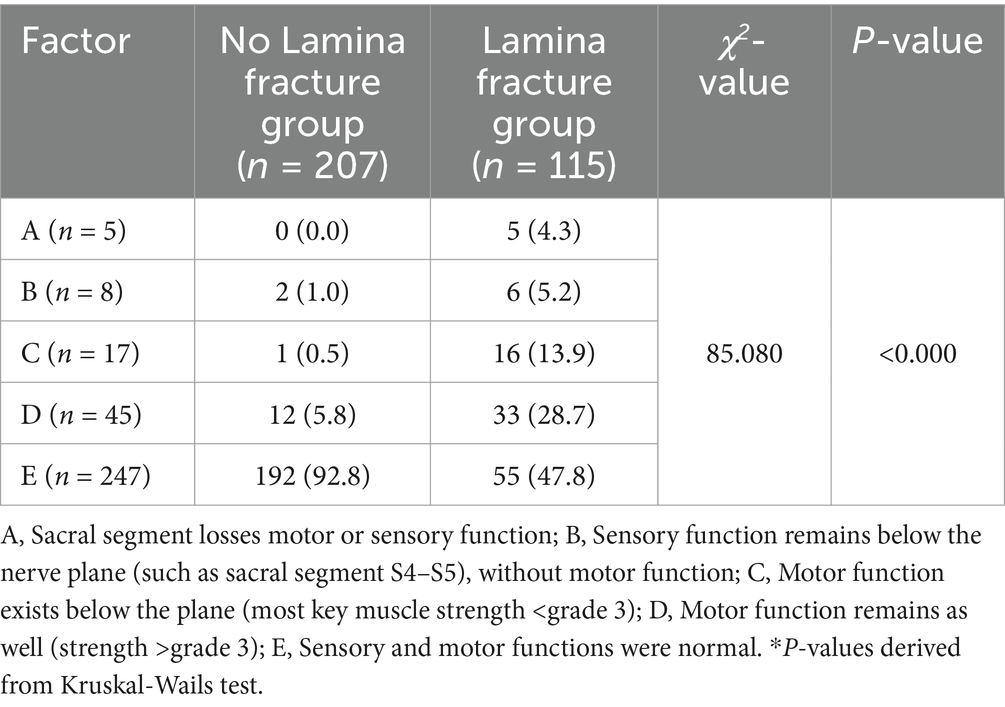
Clinical data and ASIA classification comparison
Clinical data, including age, gender, smoking status, alcohol consumption, hypertension, diabetes, disease course, mechanism of trauma, fractured vertebral segment, and ISSM score, showed no statistically significant differences between the LF and NLF groups (P > 0.05, Table 1). However, the ASIA classification score in the LF group was significantly higher than in the NLF group (P < 0.05, Table 2). In the LF group, 5 patients (4.3%) were classified as ASIA A, 6 patients (5.2%) as ASIA B, 16 patients (13.9%) as ASIA C, 33 patients (28.7%) as ASIA D, and 55 patients (47.8%) as ASIA E. In contrast, in the NLF group, no patients (0.0%) were classified as ASIA A, 2 patients (1.0%) as ASIA B, 1 patient (0.5%) as ASIA C, 12 patients (5.8%) as ASIA D, and 192 patients (92.8%) as ASIA E.
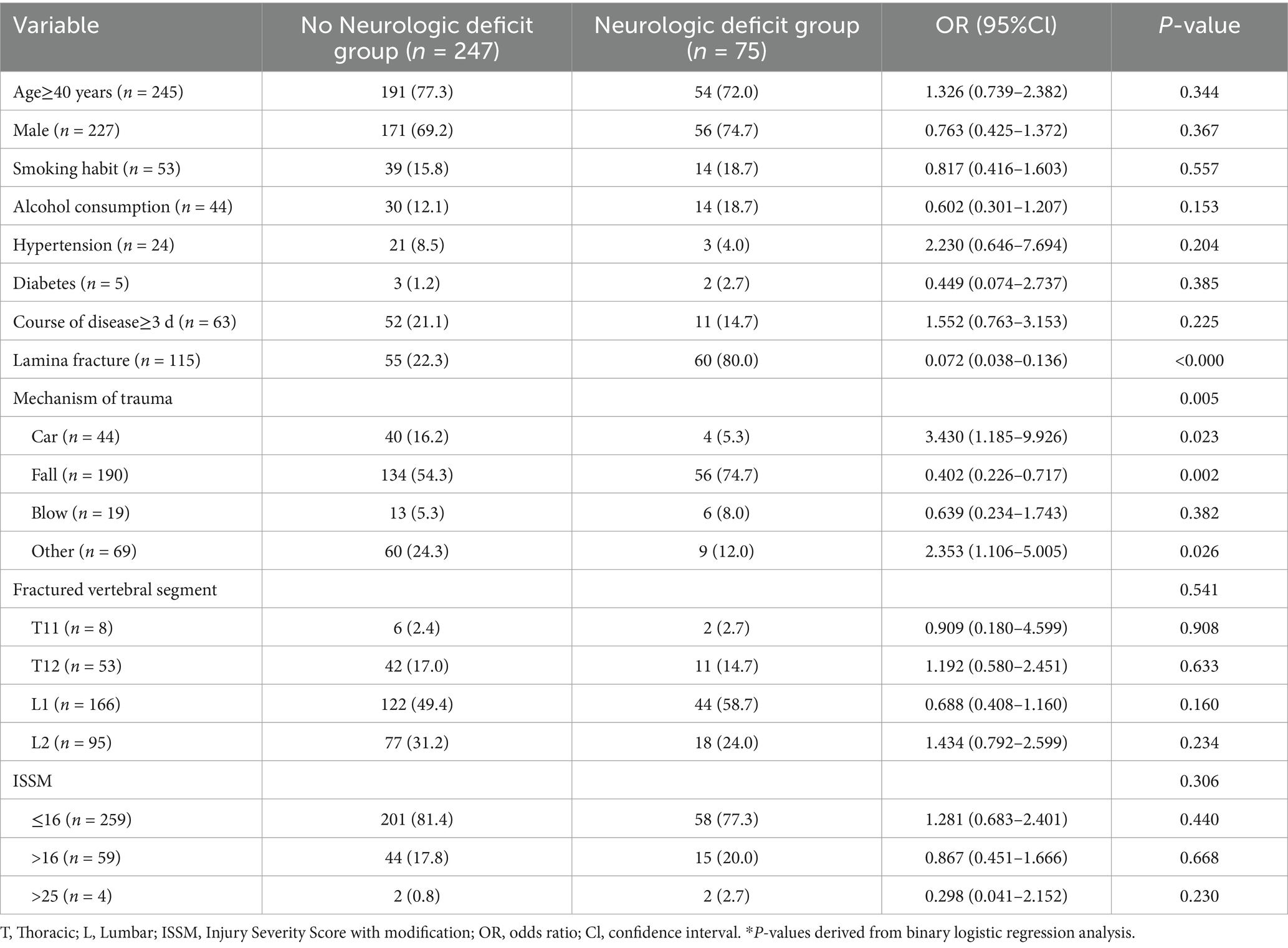
Risk factors of neurologic deficit after TBF
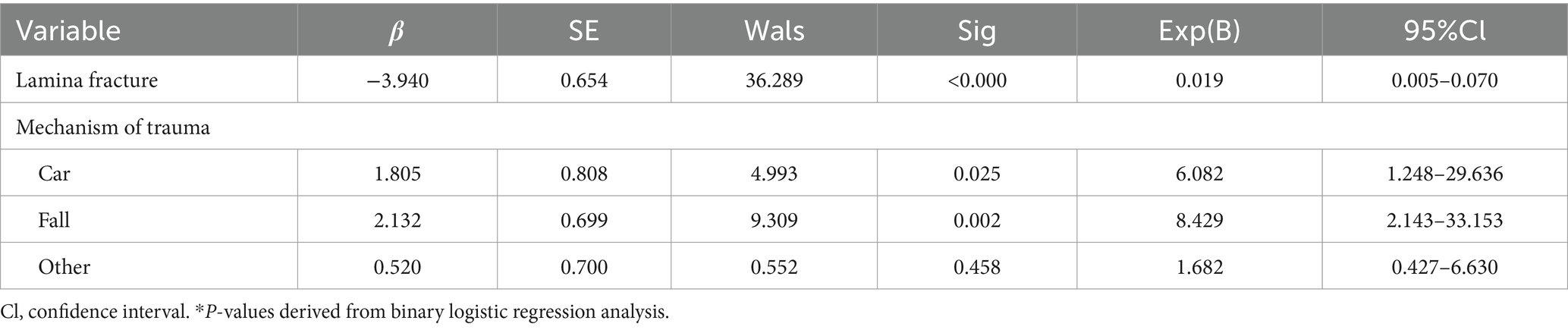
Univariate analysis revealed that laminar fractures and the mechanism of trauma (car accidents, falls, and other accidents) were associated with neurological deficits following TBF (P < 0.05, Table 3). Subsequently, variables showing significant differences were included in the logistic regression analysis and tested using the backward LR method. Laminar fractures (OR: 0.019, 95% CI: 0.005–0.070), car accidents (OR: 6.082, 95% CI: 1.248–29.636), and falls (OR: 8.429, 95% CI: 2.143–33.153) were independently associated with neurological deficits after TBF (P < 0.05, Table 4). Furthermore, ROC curves were plotted to assess the risk association value of each index for neurological deficits following TBF. The results indicated that laminar fractures and falls had a high risk association value (P < 0.01, Figure 1). Finally, the risk association equation Logit (P) = −4.358 + 3.535 × laminar fracture – 1.353 × falling accidents was established based on high-value indicators, and the goodness-of-fit was assessed using the Hosmer-Lemeshow test (P = 0.324). The area under the curve (AUC) for associating neurological deficits in TBF patients was 0.819 (95% CI: 0.769–0.869, P < 0.000), indicating good model performance.
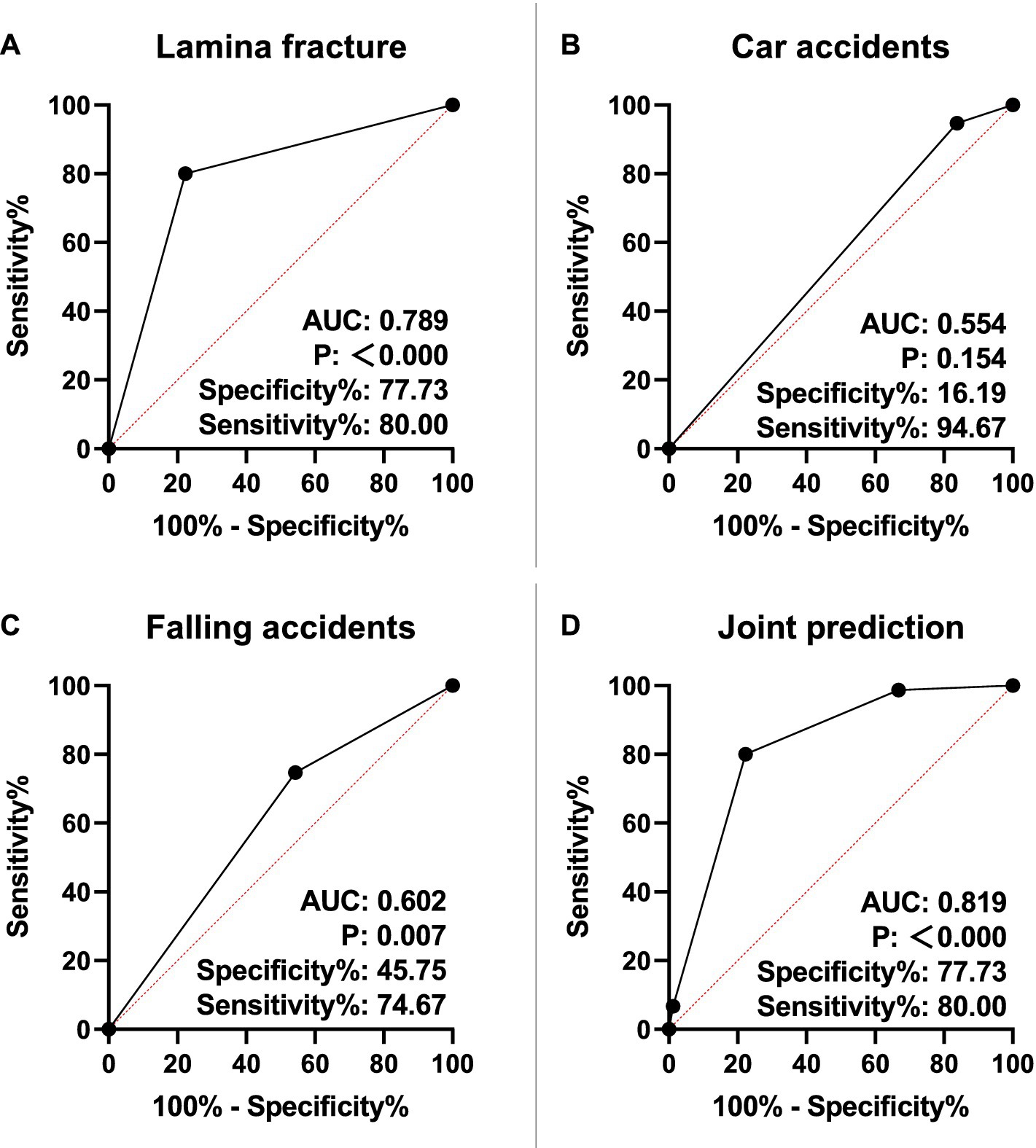
Figure 1. Value of lamina fracture, car and falling accidents in neurologic deficit. (A) Risk association value of lamina fracture in neurologic deficit. (B) Risk association value of car accidents in neurologic deficit. (C) Risk association value of falling accidents in neurologic deficit. (D) ROC curve of neurologic deficit associated by risk association equation. AUC, area under the curve.
Discussion
Due to advancements in modern urban infrastructure, more individuals are participating in the construction and transportation industries (8), leading to an increase in car accidents and falls. Reports indicate that nearly 90% of vertebral fractures occur in the thoracolumbar spine, with burst fractures accounting for 30–60% of all thoracolumbar fractures (9–12). TBF is characterized by a fall from height impacting the anterior margin of the vertebral body and injuring the posterior margin (13). Axial loading causes the vertebral body to fracture into multiple fragments, leading to lateral spreading of the pedicles and posterior elements, resulting in a vertical laminar fracture. Laminar fractures have been demonstrated as reliable indicators for assessing the severity of spinal lesions (3). An analysis of patients with TBF and vertebral plate fractures revealed significantly higher injury severity and greater spinal canal encroachment compared to the control group (14). These findings underscore the potential risk association value of laminar fractures in relation to neurologic deficits.
In this study, the ASIA classification was significantly higher in the LF group compared to the NLF group (P < 0.05). It is noteworthy that the injury process is dynamic. The presence of neurologic deficits following vertical laminar fractures may result from the impalement of the posteriorly displaced dural sac on the sharp edges of the laminar fracture at the moment of trauma. Additionally, the retraction of the laminar fracture fragments to their original position may lead to neurological deterioration by entrapment of the dural sac and nerve roots when the axial load dissipates (3, 15, 16). The literature has well documented the association between laminar fractures, dural tears, and the severity of spinal lesions (3, 14, 17). Researchers have also sought to identify specific clinical, radiological, or intraoperative factors predicting dural tears and nerve root entrapment (16). Furthermore, scholars have developed diagnostic and treatment methods for cauda equina entrapment in vertical laminar fractures associated with lumbar burst fractures (18). Our study also confirmed that laminar fractures (OR: 0.019, 95% CI: 0.005–0.070), car accidents (OR: 6.082, 95% CI: 1.248–29.636), and falling accidents (OR: 8.429, 95% CI: 2.143–33.153) were independently associated with neurologic deficits after TBF (P < 0.05). In both falls and car accidents, the vertebral body undergoes significant longitudinal compression during the injury process, causing the vertebral body to burst into multiple bone fragments. The compression force is transmitted from the vertebral body to the lamina through the pedicle, ultimately resulting in a fissure in the lamina, which leads to neurologic deficits. Additionally, we found that laminar fractures and falling accidents were highly risk association of neurologic deficits (P < 0.01). The risk association equation was Logit (P) = −4.358 + 3.535 × laminar fracture – 1.353 × falling accidents.
In the treatment of neurological injuries caused by TBF, internal fixation following decompression is commonly accepted (19). It has been suggested that patients with lumbar burst fractures, particularly those with greenstick laminar fractures or radiological evidence of posterior displacement of neural elements in the injured vertebrae, should undergo posterior surgical exploration (16, 17). Researchers have found that various laminar fracture characteristics impact the surgical outcome of TBF (3). Kyphotic angle (KA) is a critical factor influencing spinal cord injury and neurological deficits following spinal fractures. Studies consistently demonstrate that a greater KA is associated with increased spinal canal narrowing, higher risks of neurological impairment, and post-surgical correction loss (20–22). Particularly, a KA exceeding 20° is often considered a threshold for spinal instability and potential neurological deterioration (21, 22). The presence of posterior element injuries, such as laminar or facet fractures, further exacerbates the risk (20, 21). Imaging assessments, including Cobb angle measurement, play a crucial role in predicting neurological outcomes (22, 23). Early surgical correction of kyphotic deformity is recommended to prevent progressive spinal cord compression and optimize recovery (22). Although spinal canal compromise is widely recognized as a major determinant of neurological deficits and ASIA classification, the role of KA in this relationship remains an important but underexplored aspect. Given the strong association between KA and spinal canal narrowing, KA may serve as an additional predictive measure of neurological outcomes, potentially complementing or even exceeding the predictive value of laminar fractures. However, due to the limitations of the current dataset, a direct comparative analysis between KA, spinal canal compromise, and ASIA classification was not performed. Future studies should incorporate detailed radiological assessments, including spinal canal compromise and KA, to determine their relative contributions to neurological impairment more comprehensively.
However, this study has several limitations. Firstly, it included patients exclusively from a single hospital’s spine surgery department, necessitating a larger, multicenter study to minimize potential bias. Secondly, being retrospective, there is a risk of incomplete clinical data, which could introduce errors, especially given the small sample size. Additionally, potential confounders, such as different spinal fracture mechanisms (e.g., flexion-extension, axial loading), intravertebral MRI findings, and other clinical factors, may have influenced the observed association between laminar fractures and neurological deficits. Since these factors were not comprehensively analyzed in our study, they could contribute to residual confounding effects. Future studies should incorporate a more detailed analysis of fracture mechanisms and imaging characteristics to provide a clearer understanding of their impact on neurological outcomes. In future research, we aim to address these issues by gathering data from multiple centers, conducting prospective investigations, and integrating advanced imaging techniques.
Conclusion
In this study, we identified laminar fractures, car accidents, and falls as independent risk factors for neurological deficits in patients with TBF. Among them, laminar fractures and falls exhibited high risk association value for neurological impairment. These findings highlight the importance of assessing laminar fractures when evaluating spinal trauma severity and emphasize the need for early intervention in high-risk patients. Furthermore, the risk association model established in this study may provide a reference for clinical decision-making. However, this study has certain limitations. As a retrospective study conducted in a single center, potential selection bias and incomplete clinical data may exist. Future studies should incorporate multicenter prospective designs and advanced imaging techniques to further validate these findings and explore additional factors influencing neurological outcomes.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Medical Ethical Committee of the Affiliated Hospital of Southwest Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because of the retrospective nature of this study.
Author contributions
YL: Methodology, Writing – original draft, Writing – review & editing. SZ: Methodology, Writing – original draft, Writing – review & editing. DF: Formal analysis, Resources, Writing – review & editing. JL: Formal analysis, Funding acquisition, Resources, Writing – review & editing. HZ: Formal analysis, Funding acquisition, Resources, Writing – review & editing. LW: Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Special Scientific and Technological Research Project of the Administration of Traditional Chinese Medicine of Sichuan Province (2024MS492), the Scientific Research Project of the Sichuan Provincial Health Commission (21PJ183), and the Scientific Research Project of the Mianyang Municipal Health Commission (202359).
Acknowledgments
The authors would like to thank all the patients of the Affiliated Hospital of Southwest Medical University for allowing us to publish this paper and use their data collected during hospital admission. We also acknowledge Jia Hong from the Evidence-Based Medicine Center of Southwest Medical University, China, for his valuable assistance in reviewing and validating the statistical methods used in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that Gen AI was used in the creation of this manuscript. During the preparation of this work the author(s) used OpenAI ChatGPT in order to improve readability and language. After using this tool, the author(s) reviewed and edited the content as needed and take(s) full responsibility for the content of the publication.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wood, KB, Li, W, Lebl, DR, and Ploumis, A. Management of thoracolumbar spine fractures. Spine J. (2014) 14:145–64. doi: 10.1016/j.spinee.2012.10.041
2. Denis, F. The three-column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine. (1983) 8:817–31. doi: 10.1097/00007632-198311000-00003
3. Skiak, E, Karakasli, A, Harb, A, Satoglu, IS, Basci, O, and Havitcioglu, H. The effect of laminae lesion on thoraco-lumbar fracture reduction. Orthop Traumatol Surg Res. (2015) 101:489–94. doi: 10.1016/j.otsr.2015.02.011
4. Frank, P, Cammisa, J, Elsmont, FJ, and Green, BA. Dural laceration occurring with burst fractures and associated laminar fractures. J Bone Joint Surg Am. (1989) 71:1044–52. doi: 10.2106/00004623-198971070-00011
5. Frederick, M, Maynard, J, Bracken, MB, Creasey, G, John, F, Ditunno, J, et al. International standards for neurological functional classification of spinal cord injury. Spinal Cord. (1997) 35:266–74. doi: 10.1038/sj.sc.3100432
6. Baker, SP, Oneill, BW, Haddon, J, and Long, WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. (1974) 14:187–96. doi: 10.1097/00005373-197403000-00001
7. Gennarelli, T, and Wodzon, E. The abbreviated injury scale—2005. Des Plaines, IL: Association for the Advancement of Automotive Medicine (2005).
8. Xiahou, X, Yuan, J, Liu, Y, Tang, Y, and Li, Q. Exploring the driving factors of construction industrialization development in China. Int J Environ Res Public Health. (2018) 15:442. doi: 10.3390/ijerph15030442
9. Gertzbein, S. Scoliosis Research Society. Multicenter spine fracture study spine. Spine. (1992) 17:528–40. doi: 10.1097/00007632-199205000-00010
10. Liao, J-C, and Chen, W-J. Short-segment instrumentation with fractured vertebrae augmentation by screws and bone substitute for thoracolumbar unstable burst fractures. Biomed Res Int. (2019) 2019:1–8. doi: 10.1155/2019/4780426
11. Lee, KY, Kim, MW, Seok, SY, Kim, DR, and Im, CS. The relationship between superior disc-endplate complex injury and correction loss in young adult patients with thoracolumbar stable burst fracture. Clin Orthop Surg. (2017) 9:465–71. doi: 10.4055/cios.2017.9.4.465
12. Bruno, AG, Burkhart, K, Allaire, B, Anderson, DE, and Bouxsein, ML. Spinal loading patterns from biomechanical modeling explain the high incidence of vertebral fractures in the thoracolumbar region. J Bone Miner Res. (2017) 32:1282–90. doi: 10.1002/jbmr.3113
13. Magerl, F, Aebi, M, Gertzbein, S, Harms, J, and Nazarian, S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. (1994) 3:184–201. doi: 10.1007/BF02221591
14. Tisot, RA, and Avanzi, O. Laminar fractures as a severity marker in burst fractures of the thoracolumbar spine. J Orthop Surg. (2009) 17:261–4. doi: 10.1177/230949900901700302
15. Pickett, J, and Blumenkopf, B. Dural lacerations and thoracolumbar fractures. J Spinal Disord. (1989) 2:99–103. doi: 10.1097/00002517-198906000-00006
16. Ozturk, C, Ersozlu, S, and Aydinli, U. Importance of greenstick lamina fractures in low lumbar burst fractures. Int Orthop. (2006) 30:295–8. doi: 10.1007/s00264-005-0052-0
17. Aydinli, U, Karaeminogullari, O, Tiskaya, K, and Ozturk, C. Dural tears in lumbar burst fractures with greenstick lamina fractures. Spine. (2001) 26:E410–5. doi: 10.1097/00007632-200109150-00012
18. Denis, F, and Burkus, J. Diagnosis and treatment of cauda equina entrapment in the vertical lamina fracture of lumbar burst fractures. Spine. (1991) 16:S440–39. doi: 10.1097/00007632-199108001-00025
19. Li, H, Yang, L, Xie, H, Yu, L, Wei, H, and Cao, X. Surgical outcomes of mini-open Wiltse approach and conventional open approach in patients with single-segment thoracolumbar fractures without neurologic injury. J Biomed Res. (2015) 29:76–82. doi: 10.7555/JBR.29.20140083
20. Li, H, Chen, Q, Hu, J, Yu, J, Xiang, J, Li, K, et al. The association between vertical laminar fracture and recurrent kyphosis after implant removal of thoracolumbar burst fracture: a retrospective study. BMC Musculoskelet Disord. (2023) 24:53. doi: 10.1186/s12891-023-06139-w
21. Li, Y, Huang, M, Xiang, J, Lin, Y, Wu, Y, and Wang, X. Correlation of interpedicular distance with radiographic parameters, neurologic deficit, and posterior structures injury in thoracolumbar burst fractures. World Neurosurg. (2018) 118:e72–8. doi: 10.1016/j.wneu.2018.06.122
22. Eckert, MJ, and Martin, MJ. Trauma: Spinal Cord Injury. Surg Clin North Am. (2017) 97:1031–45. doi: 10.1016/j.suc.2017.06.008
Keywords: thoracolumbar, burst fracture, neurologic deficit, spinal fractures, risk factors
Citation: Liu Y, Zhang S, Feng D, Luo J, Zhang H and Wang L (2025) Risk factors of neurologic deficit after thoracolumbar burst fracture. Front. Neurol. 16:1542622. doi: 10.3389/fneur.2025.1542622
Edited by:
Fernando Zanela Arêas, Baylor Scott & White Research Institute (BSWRI), United StatesReviewed by:
Bradley Dengler, Uniformed Services University of the Health Sciences, United StatesHervé Monka Lekuya, Makerere University, Uganda
Copyright © 2025 Liu, Zhang, Feng, Luo, Zhang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Likun Wang, VzEyNTIyNTQ1MTZAMTYzLmNvbQ==
 Yuxi Liu1
Yuxi Liu1 Likun Wang
Likun Wang