Abstract
Post-traumatic benign paroxysmal positional vertigo (BPPV) is a common but frequently underrecognized cause of dizziness following trauma. Unlike idiopathic BPPV, trauma-related BPPV arises from diverse injury mechanisms and is often characterized by heterogeneous canal involvement, greater need for repeated treatment, and frequent coexistence with broader vestibular dysfunction. These features contribute to diagnostic delays and variable clinical outcomes, particularly in the trauma and emergency care settings. We conducted a structured literature search and synthesized clinical, epidemiological, mechanistic, and implementation-focused evidence across diverse trauma contexts. This review aimed to synthesize current evidence on the mechanisms, epidemiology, and clinical characteristics of post-traumatic BPPV, contrast it with idiopathic BPPV, and propose a pragmatic clinical pathway to improve early recognition and management. We reviewed the clinical, epidemiological, mechanistic, and implementation-focused literature on post-traumatic BPPV across trauma contexts, including head injury, concussion, whiplash, sports-related injury, and traumatic brain injury. Evidence from cohort studies, comparative analyses, meta-analyses, and qualitative and feasibility studies was integrated to inform a clinically oriented framework. Accumulating evidence suggests that post-traumatic BPPV should not be regarded solely as a mechanical disorder of displaced otoconia. Trauma may disrupt the otolithic membrane, promote otoconial detachment, and induce utricular dysfunction, leading to canalithiasis or cupulolithiasis and potential interaction with central vestibular injury. Compared with idiopathic BPPV, post-traumatic cases more frequently involve horizontal or multiple canals, often require repeated canalith repositioning maneuvers, and demonstrate variable recurrence patterns. System-level barriers, including limited screening, insufficient training, and fragmented care pathways, further contribute to underdiagnosis and suboptimal management. Post-traumatic BPPV represents a distinct clinical phenotype within the spectrum of trauma-related vestibular disorders. Early identification through systematic screening, comprehensive positional testing, and timely canal-specific interventions provides practical opportunities to improve outcomes. We propose a structured clinical pathway emphasizing early recognition, planned reassessment, and escalation to integrated vestibular care when symptoms persist. Future research should clarify the relationships between trauma biomechanics and BPPV phenotypes, identify predictors of recurrence, and evaluate the real-world effectiveness of pathway-based care models across diverse trauma populations.
1 Introduction
Benign paroxysmal positional vertigo (BPPV) is the most common cause of peripheral vertigo and has traditionally been regarded as an idiopathic condition resulting from the displacement of otoconia into the semicircular canals (1). However, a substantial proportion of BPPV cases are secondary to identifiable conditions, with trauma consistently recognized as the leading cause of secondary BPPV (2). Population-based and clinical cohort studies indicate that the risk of developing BPPV increases after head trauma compared with the general population, even after injuries that are clinically categorized as mild (3). Investigations of trauma-specific risk factors further highlight the need to consider BPPV proactively rather than incidentally in affected patients (4).
Post-traumatic BPPV encompasses a wide spectrum of injury mechanisms. It has been described after direct head impact and mild head trauma (5), as well as after sports-related concussions in adolescents and young adults (6) and in pediatric concussion (7). BPPV has also been reported following whiplash injuries without direct head impact (8) and chronic symptom complexes, including whiplash-associated disorders, have been discussed in relation to chronic or recurrent BPPV phenotypes (9) In addition, blast- or vibration-related exposures have been implicated in cases attributed to cannon fire and similar sources (10). More recently, emerging or unusual triggers have been proposed in case-based literature, such as “earbuds-induced” BPPV, illustrating both the breadth of hypothesized mechanisms and the need for careful clinical adjudication (11).
Clinically, post-traumatic BPPV may be overlooked or misdiagnosed, particularly in acute trauma or emergency settings, where dizziness is often attributed to central injury or post-concussive syndromes. Comprehensive reviews of post-concussive dizziness emphasize the heterogeneity of vestibular and non-vestibular contributors, which can obscure treatable peripheral diagnoses such as BPPV (12). Studies of vestibular dysfunction in acute traumatic brain injury (TBI) further demonstrate that vestibular abnormalities are common early after injury, reinforcing the need for targeted bedside evaluation (13).
Accumulating evidence suggests that post-traumatic BPPV may differ from idiopathic BPPV in clinically meaningful ways, including canal distribution, treatment response, and recurrence patterns. Several comparative studies have directly contrasted post-traumatic and idiopathic phenotypes (1, 14, 15), and more recent work has examined these differences using a retrospective design (16). A meta-analysis has synthesized evidence on treatment response and recurrence differences between traumatic and idiopathic BPPV, illustrating both shared features and substantial heterogeneity across studies (17).
Finally, practical barriers to diagnosis and treatment in trauma settings are increasingly recognized. Mixed-methods and qualitative investigations have described why patients with acute TBI are not routinely assessed or treated for vestibular dysfunction and have explored the perspectives in trials of acute post-traumatic BPPV management (18–20). These implementation gaps render post-traumatic BPPV a particularly suitable subject for a clinically oriented review incorporating a pragmatic care pathway proposal.
In this review, we summarize the current evidence regarding the mechanisms, epidemiology, and clinical characteristics of post-traumatic BPPV; contrast these features with idiopathic BPPV; and propose a practical clinical pathway emphasizing early recognition, structured assessment, and appropriate follow-up.
2 Methods: literature search strategy and study selection
We conducted a structured literature search to identify studies relevant to post-traumatic benign paroxysmal positional vertigo (BPPV). PubMed/MEDLINE and Embase were searched from inception to December 2025 using combinations of keywords and controlled vocabulary terms including “benign paroxysmal positional vertigo,” “BPPV,” “post-traumatic,” “head trauma,” “concussion,” “whiplash,” and “traumatic brain injury.” Eligible articles included human clinical studies addressing mechanisms, epidemiology, clinical phenotypes, canal involvement patterns, treatment response, recurrence, or care delivery and implementation issues in trauma-related BPPV. Systematic reviews and meta-analyses were included when available. Case reports were selectively included only when they provided unique insights into rare phenotypes (e.g., bilateral or multicanal disease) or uncommon trauma contexts (e.g., blast or vibration exposure). Studies focusing solely on non-positional dizziness without evidence of BPPV were excluded. The final reference list was curated to provide a clinically oriented synthesis across diverse trauma settings.
3 Mechanisms of post-traumatic BPPV
3.1 Trauma-induced otoconial detachment and canalithiasis/cupulolithiasis
The most widely accepted mechanism of post-traumatic BPPV is trauma-induced detachment of otoconia from the otolithic membrane—most commonly the utricular macula—followed by migration into the semicircular canals, resulting in canalithiasis or, less frequently, cupulolithiasis (1). A survey examining the nature of trauma in post-traumatic BPPV supports the concept that diverse traumatic forces may precede symptom onset, consistent with a mechanical trigger for otoconial displacement (21). Importantly, the occurrence of BPPV following mild head trauma suggests that substantial intracranial injury is not required to destabilize otoconia and that relatively modest biomechanical insults may be sufficient to initiate this process (3, 5).
3.2 Whiplash and non-impact mechanisms
A distinctive feature of post-traumatic BPPV is that it may occur after acceleration–deceleration injuries without direct head impact. Whiplash-associated BPPV has been explicitly examined, raising the possibility that rapid rotational or torsional forces transmitted to the labyrinth can precipitate otoconial detachment (8). In broader clinical discussions, chronic BPPV in individuals with a history of trauma has been considered in relation to symptom triggers and overlapping syndromes, including whiplash-associated disorders (9). Although causality and directionality remain complex, these reports collectively support a mechanism in which inertial forces, rather than impacts per se, destabilize otolith structures.
3.3 Vibration, blast, and other unusual exposures
Post-traumatic BPPV after intense vibrations or blast-like exposure has also been reported. A case report attributed the onset of BPPV to cannon fire, suggesting that high-energy acoustic or vibrational forces may contribute to otoconial instability in susceptible individuals (10). Similarly, recent discussion of possible “earbuds-induced” BPPV—although not traumatic in the conventional sense—highlights ongoing exploration of how repeated vibration or mechanical stimulation might relate to positional vertigo, while emphasizing the importance of cautious interpretation and differential diagnosis (11). Dental procedures have also been proposed as potential triggers for BPPV, possibly due to sustained head positioning and exposure to high-frequency vibrational stimuli during treatment, which may facilitate otoconial detachment in susceptible individuals (16). These observations broaden the proposed mechanistic framework while underscoring that evidence quality varies, and that mechanistic claims should remain proportionate to study design.
3.4 Otolith dysfunction and recurrence susceptibility
Beyond the initial mechanical insult, trauma may induce more diffuse otolith organ dysfunction, potentially increasing susceptibility to recurrence. Otolith dysfunction in recurrent BPPV following mild TBI has been demonstrated using vestibular-evoked myogenic potentials, supporting the concept that utricular impairment may contribute to recurrent or refractory disease (22). This interpretation aligns with clinical observations that post-traumatic BPPV often requires repeated canalith repositioning maneuvers and may recur unpredictably (16, 17).
3.5 TBI as a setting for combined peripheral and central vestibular injury
Vestibular symptoms following TBI often reflect a combination of peripheral and central injuries. Studies on acute TBI have documented vestibular dysfunction and have highlighted that vestibular end-organ injury may coexist with impairment of central vestibular pathways (13). In this context, BPPV may represent only one component of a broader dizziness syndrome, which can influence symptom persistence and complicate assessment of treatment response after repositioning maneuvers (12, 23).
Taken together, accumulating evidence suggests that post-traumatic BPPV should not be conceptualized solely as a mechanical disorder caused by displaced otoconia. Rather, trauma may disrupt the otolithic membrane, promote otoconial detachment, and induce utricular dysfunction, with downstream development of canalithiasis or cupulolithiasis and potential interaction with central vestibular injury in the setting of TBI (Figure 1).
Figure 1

Proposed mechanisms of post-traumatic benign paroxysmal positional vertigo.
4 Epidemiology and trauma phenotypes
4.1 Risk and frequency across settings
The risk of developing BPPV after head trauma has been quantified in cohort studies, demonstrating an increased incidence compared with non-trauma populations (3). In a prospective study of 117 adults with minimal-to-moderate head injury, 21% developed definite traumatic BPPV within 3 months (95% CI, 14%–29%), with most cases occurring within the first 2 weeks after trauma (3). Within the broader landscape of secondary BPPV, multicenter data underscore the clinical importance of identifiable causes and frame trauma-related BPPV as a major, potentially actionable subset (2). In a nationwide multicenter study, secondary BPPV accounted for 14.5% of all BPPV cases, and head trauma was the most common presumed etiology (2). Risk factor analyses performed within trauma cohorts may further inform future screening strategies; in a Korean trauma database study, BPPV prevalence was approximately 1.0%, and head-and-neck injury was a significant risk factor (OR 10.556, 95% CI 1.029–108.262) (4).
4.2 Mild head trauma, concussion, and sports-related phenotypes
The trauma phenotypes associated with post-traumatic BPPV are summarized in Table 1. A recurring phenotype is BPPV following mild traumatic injury, including concussion. Adolescents and young adults with recent concussions have been studied, with reports describing clinical outcomes across BPPV diagnoses in these populations (6). Similarly, pediatric sports-related concussion cohorts include documented cases of post-concussion BPPV, reinforcing that traumatic BPPV is not confined to older adults (7). In sports contexts, BPPV has been reported in adolescent rugby players (24), and its evaluation has been described in American football players (25). Soccer-related cases have also been reported, illustrating that even noncollisional repetitive head impacts or sports exposure may be relevant in some individuals (26). Collectively, these studies support the practical implication that positional testing should be considered during the evaluation of post-concussion dizziness across age groups.
Table 1
| Trauma phenotype | Representative context | Characteristic features | Key references |
|---|---|---|---|
| Mild head trauma | Falls, minor accidents | BPPV without imaging abnormalities | Gordon et al. (1); Balatsouras et al. (5) |
| Concussion/mild TBI | Sports-related concussion | Often under-recognized; may require repeated CRM | Bowman et al. (6); Kim et al. (23) |
| Moderate–severe TBI | High-energy trauma | Coexisting central vestibular deficits | Marcus et al. (13) |
| Whiplash injury | Acceleration–deceleration injury | BPPV without direct head impact | Dispenza et al. (8) |
| Sports-related trauma | Rugby, football, soccer | Horizontal canal or multi-canal BPPV | Bashir et al. (24); Warming et al. (26) |
| Pediatric trauma | Youth sports concussion | Delayed diagnosis common | Reimer et al. (7) |
| Craniofacial trauma | Mandibular fracture | Mechanical force transmission to the labyrinth | Bashir et al. (27) |
| Blast/vibration exposure | Cannon fire, blast | Rare, but illustrative of unusual triggers | Kauffman (10) |
| Complex/refractory | Bilateral or multi-canal involvement | Treatment-resistant | Maslovara et al. (28); Dundar et al. (29) |
Trauma phenotypes associated with post-traumatic benign paroxysmal positional vertigo.
BPPV, benign paroxysmal positional vertigo; TBI, traumatic brain injury; CRM, canalith repositioning maneuvers.
4.3 Whiplash-associated and neck-injury phenotypes
Whiplash-associated BPPV remains a debated phenotype but has been repeatedly described, including studies that directly question whether BPPV following whiplash injury represents a myth or a clinical reality (8). In some clinical discussions, chronic BPPV in individuals with a history of trauma has been considered in relation to symptom triggers within broader syndromic contexts, including whiplash-associated disorders (9). Although the strength of evidence varies, these reports collectively justify including whiplash and neck injuries as clinical triggers for screening for positional vertigo.
4.4 Blast, vibration, and rare trauma mechanisms
Beyond conventional trauma mechanisms, the case-based literature describes unusual exposures, such as cannon fire-related traumatic BPPV (10). Mandibular fracture–associated BPPV has also been reported, emphasizing that craniofacial trauma and transmitted forces may be relevant, even when the primary injury is not intracranial (27). Although such reports are not suitable for prevalence estimation, they are valuable for broadening clinical awareness of possible phenotypes and diagnostic considerations.
4.5 Canal involvement patterns and atypical presentations
Trauma-related BPPV is frequently characterized by greater heterogeneity in canal involvement, with increased reports of horizontal canal involvement and multi-canal disease compared with idiopathic BPPV (14, 15). Rare presentations, such as bilateral post-traumatic BPPV, have been published (28), and refractory multicanal BPPV has also been described in case reports (29). Additionally, trauma-induced unilateral horizontal canal BPPV with apogeotropic nystagmus has been documented in adolescents, underscoring the need to consider less common variants in younger patients with trauma (30). Finally, the relationship between focal TBI location and canal involvement has been explored, suggesting that injury distribution may influence clinical patterns; however, further validation is required (31).
4.6 Age-specific considerations: pediatric and older adults
Post-traumatic BPPV has important age-specific implications. In children and adolescents, trauma is frequently reported as a major precipitating factor for BPPV, particularly in the context of sports-related concussion, and delayed recognition may prolong symptoms and interfere with return-to-school or return-to-play protocols (23, 32, 33). In older adults, post-traumatic BPPV is clinically relevant not only because falls may precipitate otoconial detachment, but also because untreated BPPV itself increases the risk of recurrent falls and related morbidity (25, 26). Therefore, positional testing should be considered systematically in older adults presenting after a fall or minor head injury, especially when dizziness, imbalance, or motion-provoked symptoms are reported (25, 26).
5 Clinical characteristics compared with idiopathic BPPV
Evidence increasingly supports clinically meaningful differences between post-traumatic and idiopathic BPPV, with implications for diagnostic evaluation, treatment planning, and follow-up strategies. The key clinical distinctions between post-traumatic and idiopathic BPPV are summarized in Table 2.
Table 2
| Feature | Post-traumatic BPPV | Idiopathic BPPV |
|---|---|---|
| Typical etiology | Head injury, concussion, whiplash, craniofacial trauma, or sports-related injury | Age-related otolithic degeneration |
| Affected population | All ages, including pediatric and young adults | Predominantly middle-aged and older adults |
| Time to symptom onset | Immediate or delayed (days to months) | Usually spontaneous |
| Underlying mechanism | Trauma-induced otoconial detachment ± utricular dysfunction | Degenerative otoconial detachment |
| Canal involvement | Higher frequency of horizontal canal, bilateral, or multi-canal disease | Mostly posterior canal |
| Atypical presentations | Frequent (bilateral, refractory, apogeotropic) | Uncommon |
| Associated vestibular deficits | Common, especially in TBI | Rare |
| Response to CRM | Often requires repeated sessions | Typically resolves with 1–2 sessions |
| Recurrence pattern | Variable and sometimes unpredictable | Relatively predictable |
| Management focus | Early screening, structured follow-up, and integrated care | Standard repositioning maneuvers |
Comparison between post-traumatic and idiopathic benign paroxysmal positional vertigo.
BPPV, benign paroxysmal positional vertigo; TBI, traumatic brain injury; CRM, canalith repositioning maneuvers.
5.1 Canal distribution and complexity
Compared with idiopathic BPPV, post-traumatic cases appear more likely to involve the horizontal canals, multiple canals, or bilateral disease across several cohorts (14, 15). Such distributions may produce more complex nystagmus patterns and often require comprehensive testing beyond a single Dix–Hallpike maneuver. Comparative analyses of traumatic versus idiopathic BPPV have emphasized differences in disease characteristics and outcomes (14), and personal-experience series have similarly highlighted the need to anticipate atypical or multicanal involvement in post-traumatic BPPV (15). Case-based literature further underscores that bilateral involvement can occur following trauma (28) and that refractory multicanal disease may pose substantial clinical challenges (29).
5.2 Treatment response and the need for repeated maneuvers
Multiple studies have indicated that post-traumatic BPPV may require a greater number of repositioning maneuvers to achieve symptom resolution than idiopathic BPPV. Comparative analyses of symptom resolution rates between post-traumatic and non-traumatic BPPV support clinically relevant differences in recovery trajectories (32). More recently, a retrospective comparison of post-traumatic and idiopathic BPPV identified differences in clinical characteristics, aligning with the concept that trauma-related BPPV may follow a more treatment-intensive course (16). Additional analyses of disease, treatment, and outcome characteristics further suggest that traumatic BPPV may present features relevant to management planning (14). A meta-analysis comparing treatment and recurrence outcomes between traumatic and idiopathic BPPV provided a broader synthesis and demonstrated heterogeneity across studies (17).
5.3 Recurrence: variability and proposed contributors
Recurrence patterns in post-traumatic BPPV vary across studies and may depend on injury phenotype, canal involvement, duration of follow-up, and the presence of concomitant vestibular damage. Early studies questioned whether post-traumatic BPPV differs meaningfully from idiopathic BPPV, highlighting the need for careful comparative interpretation (1). Meta-analytic synthesis has demonstrated variability in recurrence outcomes, reinforcing that “one-size-fits-all” assumptions regarding recurrence are inappropriate (17). Otolith dysfunction, particularly utricular impairment, has been implicated in recurrent BPPV after mild TBI, suggesting a plausible biological link between trauma and recurrence susceptibility (22).
5.4 Comorbidity, underlying medical conditions, and broader dizziness syndromes
Trauma-related dizziness often coexists with other vestibular and neurological symptoms. Reviews of post-concussive dizziness emphasize that persistent dizziness may reflect multiple underlying mechanisms and that treatable peripheral causes, such as BPPV, should not be overlooked (12). In addition, differences in the clinical course of BPPV according to underlying medical conditions have been reported, suggesting that host factors and comorbidities may modulate symptom trajectories and recurrence risk across BPPV phenotypes (33). Some hypotheses have linked chronic trauma-related BPPV with symptom triggers in vestibular migraines or other syndromic contexts; however, these relationships require careful interpretation and should not substitute for standard diagnostic criteria (9).
6 Post-traumatic BPPV in traumatic brain injury
TBI represents a clinical context in which post-traumatic BPPV is both relevant and frequently underrecognized. Vestibular dysfunction is prevalent in the acute phase of TBI, and associated symptoms may reflect a combination of peripheral and central pathologies (13). Because dizziness is often attributed to central mechanisms or nonspecific post-concussive syndromes, systematic positional testing may be omitted, thereby delaying the diagnosis and treatment of BPPV (12, 19).
Clinical studies have examined BPPV after TBI and have described characteristic features of this population. For example, BPPV following TBI has been characterized in clinical cohorts, emphasizing that TBI-associated dizziness may include treatable positional vertigo (23). This observation aligns with broader evidence that mild head trauma can precipitate BPPV and that clinical vigilance should not be reserved exclusively for severe injuries (3, 5).
A key clinical challenge is that BPPV often does not occur in isolation in the setting of TBI. Vestibular dysfunction in acute TBI may include oculomotor abnormalities, balance impairment, and central processing disturbances, such that symptom persistence after successful repositioning may be misinterpreted as “failed” BPPV treatment rather than residual non-BPPV vestibular pathology (12, 13). This consideration underscores the importance of integrated assessment and longitudinal follow-up rather than single-episode, maneuver-centric care.
7 Management considerations: what should be different?
Although canalith repositioning maneuvers remain the cornerstone of treatment, the management of post-traumatic BPPV differs from that of idiopathic BPPV in several practical aspects, including the need for early recognition in non-otologic settings, anticipation of repeated treatment sessions, attention to coexisting vestibular deficits, and structured follow-up.
7.1 Early recognition and intervention in trauma settings
Evidence supports the clinical value of early identification and management of BPPV in trauma populations. Early management of post-traumatic BPPV has been investigated in injured patients, demonstrating that prompt assessment and treatment are feasible and may improve recovery trajectories (34). Similarly, feasibility trials indicate that structured approaches to BPPV management in acute TBI settings are possible and can be studied systematically (18). Nevertheless, qualitative research has highlighted that patients with acute TBI are not routinely assessed or treated for vestibular dysfunction in some healthcare systems because of barriers such as unclear clinical responsibility, time constraints, and limited provider training (19).
7.2 Counseling and expectation management: repeated maneuvers and variable recovery
As post-traumatic BPPV often requires repeated repositioning sessions, clinicians should explicitly counsel patients that symptom resolution may require multiple treatments and that scheduled reassessment is appropriate (14, 16, 32). A meta-analytic synthesis supports the conclusion that outcomes and recurrence are more variable in traumatic BPPV than in idiopathic BPPV, reinforcing the need for individualized counseling and follow-up planning (17).
7.3 Integrated care for persistent symptoms
Persistent dizziness after successful canalith repositioning is common in the context of trauma and may reflect coexisting vestibular dysfunction rather than persistent BPPV. Reviews of post-concussive dizziness emphasize that clinicians should evaluate multiple contributing mechanisms and may need to implement vestibular rehabilitation strategies alongside canalith repositioning maneuvers (12). Data from acute TBI populations further support the observation that vestibular dysfunction is prevalent and not limited to canalithiasis, making integrated vestibular care clinically appropriate (13). Where available, targeted vestibular rehabilitation can address residual imbalance, motion sensitivity, and oculomotor deficits after BPPV resolution.
7.4 System-level barriers and implementation priorities
Implementation barriers are not purely clinical; they are organizational in nature. Qualitative studies have described why vestibular assessment is not routinely incorporated into acute TBI care and how both patients and clinicians perceive trial participation and proposed care pathways (19, 20). These data suggest several practical interventions, including focused training for non-otologic clinicians (such as emergency physicians, trauma teams, and rehabilitation providers), the use of simple screening triggers, and the establishment of clear referral pathways. In addition, trial feasibility studies provide a foundation for pathway development and iterative refinement (18).
7.5 Why post-traumatic BPPV may be more refractory to repositioning maneuvers
Although the exact reasons remain incompletely understood, several factors may explain why post-traumatic BPPV often requires repeated canalith repositioning maneuvers and may appear more difficult to treat than idiopathic BPPV (22). First, traumatic cases more frequently involve horizontal canal, multicanal, or bilateral disease, which increases diagnostic complexity and may require sequential or repeated maneuvers (19, 20). Second, trauma may induce broader otolith organ dysfunction (particularly utricular impairment), potentially increasing the likelihood of recurrent otoconial detachment and symptom relapse even after initially successful treatment (15, 16). Third, in patients with concussion or traumatic brain injury, persistent dizziness after repositioning may reflect coexisting central vestibular dysfunction, oculomotor abnormalities, or balance impairment rather than ongoing BPPV, which can be misinterpreted as treatment failure (13, 32, 33). Finally, associated cervical pain or limited range of motion after head–neck trauma may restrict optimal positioning during maneuvers and delay symptom resolution (12, 31). These considerations support planned reassessment and integrated vestibular care in patients with persistent symptoms.
8 Clinical pathway proposal: a practical approach to post-traumatic BPPV
Considering the predictable diagnostic gaps and management challenges in trauma settings, we propose a structured clinical pathway that emphasizes early screening, comprehensive positional testing, timely canal-specific treatment, planned reassessment, and escalation to integrated vestibular care when symptoms persist (Figure 2).
Figure 2
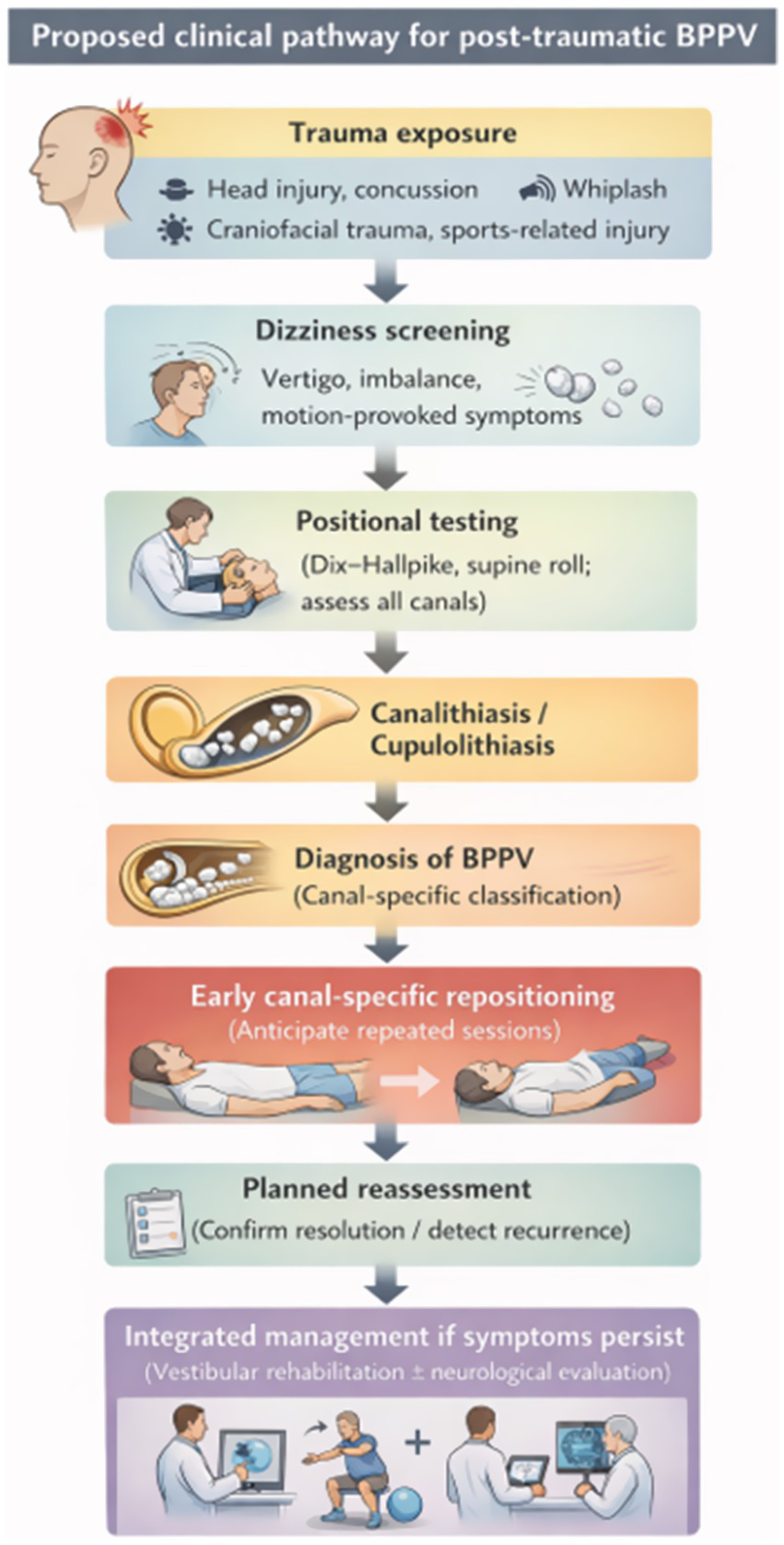
Proposed clinical pathway for post-traumatic benign paroxysmal positional vertigo.
8.1 Step 1: screening trigger (who should be tested?)
Any trauma patient reporting vertigo, dizziness, imbalance, or motion-provoked symptoms should be considered for positional testing, regardless of injury severity or imaging findings (3, 23). Screening should include not only direct head impact but also whiplash mechanisms and craniofacial injuries, consistent with reports of whiplash-related and mandibular fracture–associated BPPV (8, 27). In adolescent and sports-concussion populations, vestibular screening should be routine, as BPPV has been reported in these settings and may be readily treatable within a broader post-concussion care plan (6, 7, 24).
8.2 Step 2: standardized positional testing (test all relevant canals)
Because trauma-related BPPV more frequently involves horizontal canals and multi-canal patterns, positional testing should be comprehensive and include both the Dix–Hallpike and supine roll tests, rather than being limited to suspected posterior canal disease (14, 15). Clinicians should remain alert to less common variants, such as apogeotropic horizontal canal BPPV, which has been described in trauma-related adolescent cases (30). Careful documentation and repeat testing are essential in suspected bilateral or refractory cases, as bilateral BPPV and refractory multicanal presentations have been reported following trauma (28, 29).
8.3 Step 3: early canal-specific treatment and planned reassessment
Once diagnosed, canal-specific repositioning maneuvers should be performed as early as feasible. Evidence supports the early management of traumatically injured patients, and feasibility trial data further support pathway-based intervention approaches in acute TBI care (18, 34). Given the higher likelihood of requiring repeated sessions in post-traumatic BPPV, the pathway should incorporate planned reassessment rather than relying solely on symptom-driven return visits (16, 32). Meta-analytical evidence indicates heterogeneity in recurrence rates and treatment response, reinforcing the need for structured follow-up (17).
8.4 Step 4: evaluate persistent symptoms and refer for integrated care when needed
If dizziness persists after successful BPPV treatment, the pathway should prompt assessment for coexisting peripheral vestibular or central contributors and consideration of vestibular rehabilitation (12, 13). The high prevalence of vestibular dysfunction in TBI cohorts supports integrating BPPV treatment within a broader, multidisciplinary dizziness care framework (13, 23). When recurrence is suspected, clinicians may consider the adjunctive evaluation of otolith function, acknowledging the evidence of utricular dysfunction in recurrent BPPV following mild TBI (22).
8.5 Step 5: implementation and patient-centered outcomes
Pathway implementation should explicitly address barriers identified in qualitative studies, such as unclear professional responsibility, limited training, and time constraints inherent to acute care settings (19). Patient perspectives derived from trial participation suggest that early diagnosis and treatment may reduce anxiety and improve confidence in recovery, supporting the value of pathway-based care beyond symptom resolution alone (20). In sports contexts, incorporating positional testing into post-concussion protocols can reduce prolonged symptoms in adolescents and young adults (6, 7). Finally, unusual triggers reported in the literature, such as blast exposure or vibration-related hypotheses, should encourage diagnostic openness while maintaining a rigorous differential diagnosis (10, 11).
9 Knowledge gaps and future directions
Despite the growing literature, several knowledge gaps continue to limit the delivery of precision care for post-traumatic BPPV.
9.1 Linking injury biomechanics to phenotype
It remains unclear how trauma type, direction, and severity influence canal involvement, bilaterality, and treatment response. Existing studies suggest that focal TBI location may be associated with specific canal involvement; however, validation across larger cohorts and diverse injury mechanisms is required (31). Similarly, the relationship between whiplash injury and BPPV remains debated, and prospective studies are needed to clarify causal relationships and risk gradients (8, 9).
9.2 Predicting recurrence and refractory disease
Reliable predictors of recurrence and refractory disease are currently lacking. Evidence of utricular dysfunction in recurrent BPPV following mild TBI suggests that otolith testing may help stratify recurrence risk; however, optimal clinical workflows and predictive utility remain to be established (22). A systematic synthesis reported variable recurrence outcomes between traumatic and idiopathic BPPV, highlighting the heterogeneity that future stratified studies should address (17).
9.3 Standardizing care pathways and evaluating real-world effectiveness
Feasibility trials provide an initial foundation for pathway-based care in acute TBI settings; however, larger pragmatic studies are needed to evaluate real-world effectiveness, sustainability, and cost implications (18). Qualitative research demonstrates persistent barriers to vestibular assessment and treatment in trauma settings, and implementation studies should test targeted training models and role-delineation strategies to address these challenges (19, 20). Early management strategies in traumatically injured patients should also be extended across diverse health systems and populations, including sports and pediatric settings (6, 7, 34).
9.4 Expanding phenotype characterization across age groups and triggers
Pediatric and adolescent phenotypes warrant dedicated studies, as sports-related concussion cohorts demonstrate the occurrence of BPPV; however, standardized screening approaches remain inconsistent across settings (6, 7). Evaluations and case reports from contact sports, including rugby, American football, and soccer, highlight the need for consistent clinical algorithms (24–26). Finally, emerging hypotheses regarding vibration-related triggers (e.g., blast exposure and so-called “earbuds-induced” cases) raise questions that require careful epidemiologic and mechanistic investigation to distinguish true associations from coincidental temporal relationships (10, 11).
10 Conclusion
Post-traumatic BPPV is a common yet frequently under-recognized cause of dizziness following trauma. Compared with idiopathic BPPV, trauma-related cases arise from diverse mechanisms, including head impact, concussion, whiplash, craniofacial injuries, and unusual vibrational exposures, and may exhibit greater heterogeneity in canal involvement and clinical course (8, 10, 16, 21). Evidence suggests that post-traumatic BPPV more often requires repeated repositioning maneuvers and may present with variable recurrence patterns, possibly influenced by broader otolith dysfunction and multisystem vestibular injury (13, 17, 22, 32).
Because post-traumatic dizziness is frequently attributed to central or nonspecific post-concussive mechanisms, systematic positional testing is essential for identifying BPPV as a treatable contributor, including in mild injuries and pediatric/sports contexts (6, 7, 12, 23). Early assessment and canal-specific treatment, supported by structured follow-up and integrated management of persistent symptoms, represent practical opportunities to improve patient outcomes (18, 34).
A pragmatic clinical pathway—including screening, comprehensive positional testing, early intervention, planned reassessment, and escalation to integrated vestibular care when needed—can address predictable diagnostic gaps and standardize care across emergency, trauma, and rehabilitation settings (19, 20). Future studies should clarify how trauma biomechanics shape BPPV phenotypes, identify objective predictors of recurrence, and evaluate the effectiveness of pathway-based models across diverse populations.
Statements
Author contributions
TK: Data curation, Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing. YS: Conceptualization, Project administration, Writing – review & editing.
Funding
The author(s) declared that financial support was received for this work and/or its publication. This research was supported by the Regional Innovation System & Education (RISE) program through the Gangwon RISE Center, funded by the Ministry of Education (MOE) and Gangwon State (G.S.), Republic of Korea (2025-RISE-10-006).
Conflict of interest
The author(s) declared that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declared that Generative AI was used in the creation of this manuscript. Generative AI was used for language editing and improving the clarity and readability of the manuscript. All content was reviewed, verified, and approved by the authors, who take full responsibility for the manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Gordon CR Levite R Joffe V Gadoth N . Is posttraumatic benign paroxysmal positional vertigo different from the idiopathic form?Arch Neurol. (2004) 61:1590–3. doi: 10.1001/archneur.61.10.1590,
2.
Na S Jeon EJ Kim MB Lee JY Kim CH Nam SI et al . Clinical features of secondary BPPV: a nation-wide multicenter study. J Vestib Res. (2025) 35:193–204. doi: 10.1177/09574271251319775,
3.
Andersson H Jablonski GE Nordahl SHG Nordfalk K Helseth E Martens C et al . The risk of benign paroxysmal positional vertigo after head trauma. Laryngoscope. (2022) 132:443–8. doi: 10.1002/lary.29851,
4.
Kim M Lee DS Hong TH Joo Cho H . Risk factor of benign paroxysmal positional vertigo in trauma patients: a retrospective analysis using Korean trauma database. Medicine (Baltimore). (2018) 97:e13150. doi: 10.1097/MD.0000000000013150,
5.
Balatsouras DG Koukoutsis G Aspris A Fassolis A Moukos A Economou NC et al . Benign paroxysmal positional vertigo secondary to mild head trauma. Ann Otol Rhinol Laryngol. (2017) 126:54–60. doi: 10.1177/0003489416674961,
6.
Bowman TG Thibault R Radack BM Davis A Elam P . Clinical outcomes for various benign paroxysmal positional vertigo (BPPV) diagnoses in adolescents and young adults with recent concussions. Phys Ther Sport. (2024) 65:90–4. doi: 10.1016/j.ptsp.2023.12.004,
7.
Reimer K Ellis V Cordingley DM Russell K Ellis MJ . Benign paroxysmal positional vertigo after pediatric sports-related concussion. Clin J Sport Med. (2020) 30:412–5. doi: 10.1097/JSM.0000000000000617,
8.
Dispenza F De Stefano A Mathur N Croce A Gallina S . Benign paroxysmal positional vertigo following whiplash injury: a myth or a reality?Am J Otolaryngol. (2011) 32:376–80. doi: 10.1016/j.amjoto.2010.07.009,
9.
Tjell C Iglebekk W Borenstein P . Can a chronic BPPV with a history of trauma be the trigger of symptoms in vestibular migraine, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), and whiplash associated disorders (WAD)? A retrospective cohort study. Otol Neurotol. (2019) 40:96–102. doi: 10.1097/MAO.0000000000002020,
10.
Kauffman RD . Traumatic benign paroxysmal positional vertigo caused by cannon fire. BMJ Case Rep. (2020) 13:e233239. doi: 10.1136/bcr-2019-233239,
11.
Eyal Y Tsur N Trotzky ZA Pachys G Trotzky D . Earbuds induced benign paroxysmal positional vertigo?Ear Nose Throat J. (2025) 139:18–21. doi: 10.1177/01455613251329718,
12.
Gianoli GJ . Post-concussive dizziness: a review and clinical approach to the patient. Front Neurol. (2021) 12:718318. doi: 10.3389/fneur.2021.718318,
13.
Marcus HJ Paine H Sargeant M Wolstenholme S Collins K Marroney N et al . Vestibular dysfunction in acute traumatic brain injury. J Neurol. (2019) 266:2430–3. doi: 10.1007/s00415-019-09403-z,
14.
Luryi AL LaRouere M Babu S Bojrab DI Zappia J Sargent EW et al . Traumatic versus idiopathic benign positional vertigo: analysis of disease, treatment, and outcome characteristics. Otolaryngol Head Neck Surg. (2019) 160:131–6. doi: 10.1177/0194599818797892,
15.
Di Cesare T Tricarico L Passali GC Sergi B Paludetti G Galli J et al . Traumatic benign paroxysmal positional vertigo: personal experience and comparison with idiopathic BPPV. Int J Audiol. (2021) 60:393–7. doi: 10.1080/14992027.2020.1821253,
16.
Kim M Jeon EK Seo YJ Kong TH . A retrospective comparison of clinical characteristics of post-traumatic and idiopathic benign paroxysmal positional vertigo. Ear Hear. (2025) 46:1379–84. doi: 10.1097/AUD.0000000000001675,
17.
Chen G Zhao X Yu G Jian H Li Y Xu G . Otolith dysfunction in recurrent benign paroxysmal positional vertigo after mild traumatic brain injury. Acta Otolaryngol. (2019) 139:18–21. doi: 10.1080/00016489.2018.1562214,
18.
Smith RM Marroney N Beattie J Newdick A Tahtis V Burgess C et al . A mixed methods randomised feasibility trial investigating the management of benign paroxysmal positional vertigo in acute traumatic brain injury. Pilot Feasibility Stud. (2020) 6:130. doi: 10.1186/s40814-020-00669-z,
19.
Smith RM Burgess C Tahtis V Marsden J Seemungal BM . Why are patients with acute traumatic brain injury not routinely assessed or treated for vestibular dysfunction in the UK? A qualitative study. BMJ Open. (2023) 13:e067967. doi: 10.1136/bmjopen-2022-067967,
20.
Smith RM Sahu B Burgess C Beattie J Newdick A Tahtis V et al . What are the views of those participating in a trial investigating acute post-traumatic benign paroxysmal positional vertigo? A qualitative study. Brain Inj. (2025) 39:400–9. doi: 10.1080/02699052.2024.2435952,
21.
Pisani V Mazzone S Di Mauro R Giacomini PG Di Girolamo S . A survey of the nature of trauma of post-traumatic benign paroxysmal positional vertigo. Int J Audiol. (2015) 54:329–33. doi: 10.3109/14992027.2014.989454,
22.
Chen G Li Y Si J Zhao X Zhang T Dai X et al . Treatment and recurrence of traumatic versus idiopathic benign paroxysmal positional vertigo: a meta-analysis. Acta Otolaryngol. (2019) 139:727–33. doi: 10.1080/00016489.2019.1632484,
23.
Kim CH Kim H Jung T Lee DH Shin JE . Clinical characteristics of benign paroxysmal positional vertigo after traumatic brain injury. Brain Inj. (2024) 38:341–6. doi: 10.1080/02699052.2024.2310790,
24.
Bashir K Yousuf A Zaki HA Elmoheen A . Benign paroxysmal positional vertigo (BPPV) after concussion in two adolescent players during a rugby game. Cureus. (2023) 15:e33402. doi: 10.7759/cureus.33402,
25.
Gokler O Kocak I Aydogan E Karanfil I Bas C . Evaluation of benign paroxysmal positional vertigo in American football players. J Int Adv Otol. (2018) 14:295–8. doi: 10.5152/iao.2018.4384,
26.
Warming N Andersen SB Hougaard DD . Soccer and benign paroxysmal positional vertigo. Case Rep Otolaryngol. (2023) 2023:3744863. doi: 10.1155/2023/3744863,
27.
Bashir K Yousuf A Elmoheen A . Benign paroxysmal positional vertigo after mandibular fractures. Cureus. (2022) 14:e24442. doi: 10.7759/cureus.24442,
28.
Maslovara S Kosec A Pajic Matic I Sestak A . A rare case of posttraumatic bilateral BPPV presentation. Case Rep Otolaryngol. (2021) 2021:8636676. doi: 10.1155/2021/8636676,
29.
Dundar MA Derin S Aricigil M Eryilmaz MA Arbag H . Post-traumatic refractory multiple canal benign paroxysmal positional vertigo: a case report. North Clin Istanb. (2016) 3:229–32. doi: 10.14744/nci.2015.36349,
30.
Dutta KK Neupane AK Lodha V . Diagnosis and management of trauma induced unilateral horizontal canal BPPV with apogeotropic nystagmus in an adolescent. Indian J Otolaryngol Head Neck Surg. (2024) 76:5959–63. doi: 10.1007/s12070-024-05014-x,
31.
Harrell RG Manetta CJ Whitney SL . Relationship between location of focal traumatic brain injury and canal involved in benign paroxysmal positional vertigo. J Am Acad Audiol. (2023) 34:127–31. doi: 10.1055/s-0044-1790261,
32.
Aron M Lea J Nakku D Westerberg BD . Symptom resolution rates of posttraumatic versus nontraumatic benign paroxysmal positional vertigo: a systematic review. Otolaryngol Head Neck Surg. (2015) 153:721–30. doi: 10.1177/0194599815594384,
33.
Lee JM Lee HJ . Different clinical course of BPPV according to the medical conditions. Sci Rep. (2024) 14:12941. doi: 10.1038/s41598-024-63882-3,
34.
Kim H Ha J Lee JH Jang JH Park HY Choung YH . Early management for traumatic benign paroxysmal positional vertigo in traumatically injured patients. Injury. (2022) 53:198–203. doi: 10.1016/j.injury.2021.07.042,
Summary
Keywords
post-traumatic benign paroxysmal positional vertigo, benign paroxysmal positional vertigo, canalith repositioning maneuver, head trauma, clinical pathway
Citation
Kong TH and Seo YJ (2026) Post-traumatic benign paroxysmal positional vertigo: mechanisms, clinical phenotypes, and a structured clinical pathway for management. Front. Neurol. 17:1784282. doi: 10.3389/fneur.2026.1784282
Received
09 January 2026
Revised
22 January 2026
Accepted
22 January 2026
Published
03 February 2026
Volume
17 - 2026
Edited by
Leonardo Manzari, MSA ENT Academy Center, Italy
Reviewed by
Francesco Comacchio, University Hospital Sant’Antonio, Italy
Cristiano Balzanelli, Vertigo Center San Bernardino Polyclinic, Italy
Updates
Copyright
© 2026 Kong and Seo.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Young Joon Seo, okas2000@yonsei.ac.kr
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.