- 1Section of Neuroscience and Clinical Pharmacology, Department of Biomedical Sciences, University of Cagliari, Monserrato, Italy
- 2Section of Cytomorphology, Department of Biomedical Sciences, University of Cagliari, Monserrato, Italy
- 3Section of Physiology, Department of Biomedical Sciences, University of Cagliari, Monserrato, Italy
- 4Medical Faculty, University of Cagliari, Cagliari, Italy
Purpose: Previous studies reported a correlation between olfactory function and depression. However, in literature, no data are available for the correlation between depression and all other factors such as age, sex, olfactory, gustatory, and cognitive function in healthy subjects taken together. The aim of this study was to provide a systematic account regarding the association between those variables in a non-clinical population.
Methods: Two hundred and seventy-three participants were recruited with an age range of 19–84 years. Olfactory, gustatory, cognitive function, and depression level were evaluated by means of the following tests: the Sniffin’ Sticks test, Taste Strips test, Montreal Cognitive Assessment (MoCA), and Beck Depression Inventory (BDI).
Results: In our data, an age-related decrease in olfactory and gustatory function and a decline in cognitive functions such as attention, memory, and language were observed. Instead, no significant differences were observed for the depression level in relation to the different age ranges. However, our results indicated that the depression level could be associated to sex, odor identification impairment, and decreased attention and language.
Conclusion: Sex, the odor identification impairment, and an age-related decrease in attention and language are associated with increased level of depression in healthy subjects. Our data can be useful and informative for health care workers, that is, to have adequate preventive strategies to be used whenever these conditions are detected and recognized.
Introduction
Olfactory and gustatory function allows animals to detect smells and to locate food sources (Loy et al., 2016). In humans, olfactory function regulates food intake, emotional/motivational responses such as pleasantness and reward, anxiety, and social and reproductive behavior (Hoskison, 2013; Brai and Alberi, 2018). The olfactory function usually decreases in relation to age (Doty and Cameron, 2009; Doty and Kamath, 2014; Masala et al., 2018a) due to different age-related events such as a reduction in the expression of olfactory receptors, a decrease in neurogenic processes, an increase in the exposure to toxic environmental agents, and an increase in the ossification and/or closure of foramina on the cribriform plate (Kalmey et al., 1998). Age-related decline in olfactory function could also be associated to a decreased volume of the olfactory bulb (Buschhuter et al., 2008).
Patients with olfactory disorders show usually daily life problems in personal hygiene, safety, sexual behavior, and, particularly food intake (Croy et al., 2014a). Consequently, due to the existence of direct brain connections between olfactory bulb and limbic areas such as the amygdala and orbitofrontal cortex, patients with olfactory dysfunctions exhibited higher levels of depression (Pause et al., 2001; Croy et al., 2010, 2014a, b, c; Negoias et al., 2010). Moreover, patients with depression showed reduced activation in the orbitofrontal cortex, thalamus, and insula (Croy et al., 2014a, b, c) and also a decreased volume of the olfactory bulb (Negoias et al., 2010).
Depression is considered a common disease that affects about 8–12% worldwide people at least once in their life (Andrade et al., 2003). According to the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association [APA], 2013), depression is characterized by different symptoms: depressed mood, a decreased interest or pleasure in all things, weight gain or weight loss, fatigue, insomnia, and/or hypersomnia. Although gustatory disorders are less common among general population than olfactory ones, a connection between taste disorders and depression is also known (Hur et al., 2018); in fact, a previous study reported that alterations in taste and appetite are associated to affective disorders (Maheswaran et al., 2014). Recently, Perini et al. (2019) reported an association between cognitive disorders and depression. However, in literature, these associations with depression were studied independently in patients and no data are available for the correlation between depression and all other factors such as age and sex, and olfactory, gustatory, and cognitive function at the same time in healthy subjects.
The aim of this study was to provide a systematic account regarding the association between the effect of demographic factors (sex and age) and olfactory, gustatory, and cognitive function on the depression level in a non-clinical population.
Materials and Methods
Participants
Two hundred and seventy-three participants were recruited (177 females, mean age ± SD, 40.0 ± 18.9 years, and 96 males, mean age ± SD, 41.7 ± 18.5 years, age range 19–84). Among women, no one was pregnant, 57 (32.2%) showed menopause, 120 (67.8%) showed different phases of the menstrual cycle, and 21% (N = 37) of them used hormonal contraceptives.
In order to assess statistical differences in olfactory, gustatory, and cognitive function in relation to age, all subjects were divided into three age groups: 18–35 (N = 137), 36–55 (N = 63), and > 55 (N = 73) according to previous studies (Hummel et al., 2007; Masala et al., 2018a, b). Data collection started from September 2018 to December 2019. Exclusion criteria were a history of head or neck trauma, nasal pathology, neurodegenerative diseases, acute respiratory infections, diabetes, stroke, any systemic disease associated with smell disorders, chronic renal disease, and thyroid disorders.
Participants were instructed to drink only water 1 h prior to the experiment and not wear any scented products on the day of testing. Participants received an explanatory statement and gave their written informed consent to participate in the study (Prot. NP/2018/1630).
The clinical evaluation for each participant included age, sex, weight (kg), height (cm), body mass index (BMI), current medications, smoking history, and employment. Moreover, for each subject, olfactory, gustatory, and cognitive function and depression level were assessed.
Evaluation of the Olfactory Function
Olfactory function was evaluated using the Sniffin’ Sticks test (Burghart Messtechnik, Wedel, Germany), taking into consideration three different parameters: odor threshold (OT), odor discrimination (OD), and odor identification (OI) (Hummel et al., 1997, 2007; Oleszkiewicz et al., 2019). First, OT was determined using n-butanol with 16 stepwise dilutions. Thresholds were measured using the single-staircase technique based on a three-alternative forced-choice task (3AFC). Second, OD was measured over 16 trials (Masala et al., 2018a, b; Masala et al., 2019; Masala et al., 2020; Solla et al., 2020). For each discrimination, three pens were presented, two containing the same odor and the third containing the target odorant (3AFC task). Third, OI was measured using 16 common odors, each presented with four verbal descriptors in a multiple forced-choice format (three distractors and one target). The interval between odor presentations was 20–30 s. A total score (Threshold, Discrimination, Identification, TDI) was calculated: a score of > 30.5, between 30.5 and 16.5, and < 16.5 indicated normosmia, hyposmia, and functional anosmia, respectively (Hummel et al., 2007).
Assessment of Gustatory Function
Taste function was examined by the Taste Strips test (TST) (Mueller et al., 2003; Hummel et al., 2007; Landis et al., 2009). TST is a validated method for the evaluation of taste sensitivity using 16 spoon-shaped filter strips impregnated with four concentrations of the four basic tastes (sweet, sour, salty, and bitter). The TST strips were positioned on the tongue, and the subject was asked to identify the taste quality from a list of four descriptors (sweet, sour, salty, and bitter) in a forced-choice paradigm. Before each strip administration, the mouth was cleaned with water. The TST global score is the sum of correct identifications and defines the taste performance. A TST score ≥ 9 is considered as normogeusia and a TST score < 9 is classified as hypogeusia.
Assessment of Cognitive Function
A cognitive function evaluation was carried out using the Montreal Cognitive Assessment (MoCA), which assesses cognitive impairment in eight different domains: visual–constructional skills, executive functions, attention and concentration, memory, verbal fluency (language), conceptual thinking, calculations, and spatial orientation (Conti et al., 2015; Cecchini et al., 2019).
Depression Level Assessment
Depression level was evaluated using the self-reported Beck Depression Inventory (BDI-II) test (Beck et al., 1961), which includes 21 items with a four-point scale ranging in order of severity from 0 to 3. The depression level was classified as minimal = 0–13, mild depression = 14–19, moderate depression = 20–28, and severe depression = 29–63.
Statistics
At first, sample size calculation was performed in order to assess the required minimum number of subjects to be enrolled in the study. Based on previous studies using similar protocols (Masala et al., 2018a, b; Cecchini et al., 2019), a number of about 200–250 total subjects were considered adequate in order to detect the investigated differences. In fact, a power calculation, based on similar studies and considering a critical effect size f = 0.25 (medium effect), with 85–90% power and a 5% significance level in a standard one-way ANOVA, suggested a minimal required number of about 200 total subjects, and a power calculation considering a critical effect size d = 0.5 (medium effect), with 85–90% power, and a two-tailed 5% significance level in an unpaired t test, suggested a required minimal number of 70/80 subjects/group.
Data were presented as mean values ± standard deviation (SD). In particular, between-subjects one-way ANOVAs and post hoc analyses using multiple pairwise comparison tests with Bonferroni’s corrected alpha values were carried out to assess statistical differences in demographic information (weight, height, and BMI); olfactory, gustatory, and cognitive function; and depression level in the three different age ranges (18–35, 36–55, and > 55 years).
In addition, an effect size estimation (Cohen’s d for any significant pairwise comparison) was also reported in the Results section where appropriate (a value of 0.2, 0.5, or 0.8 indicates a small, medium, or large effect size, respectively). Differences in the frequencies of the three age groups for the depression level were assessed using the chi-square (χ2) test. In order to identify the more promising factors for the multivariate regression analyses, bivariate correlations between depression vs. sex, age, weight, BMI, and olfactory, gustatory, and cognitive functions were assessed using Pearson’s coefficient (r).
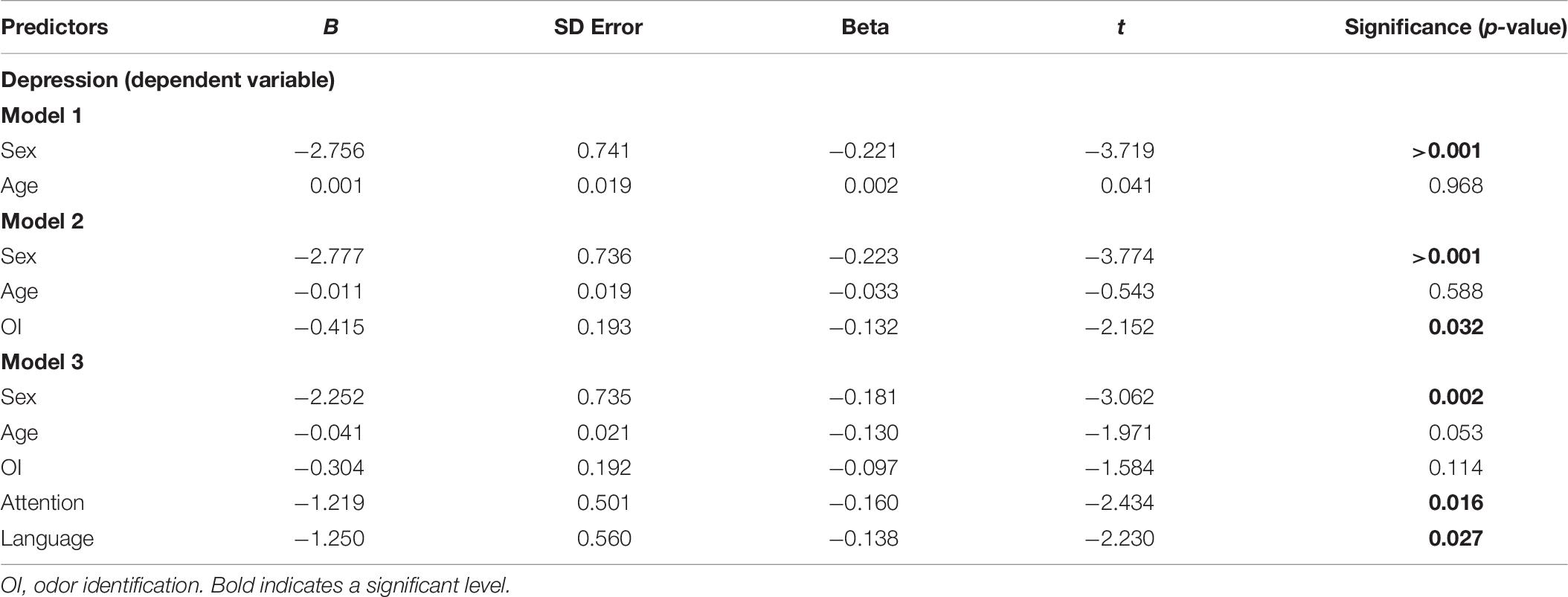
Furthermore, an exploratory stepwise multivariate linear regression analysis was performed to assess the potential contribution of each significant correlated factor (such as age, sex, OI deficit, impairment in language, and attention) on the depression level. In the multivariate linear regression analysis, the depression level (BDI score) was set as the dependent variable, while age, sex, OI, attention, and language were independent variables (predictors).
In order to perform the multivariate linear regression analysis using a stepwise selection, in model 1, we calculated the correlation between depression level with two independent variables, such as age and sex, then in model 2, we included the OI, and, finally, in model 3, we added attention and language. This stepwise method allows us to evaluate the specific role of each independent variable in the model.
Statistical analyses were performed by the SPSS software version 22 for Windows (IBM, Armonk, NY, United States). The significance level was set at p < 0.05.
Results
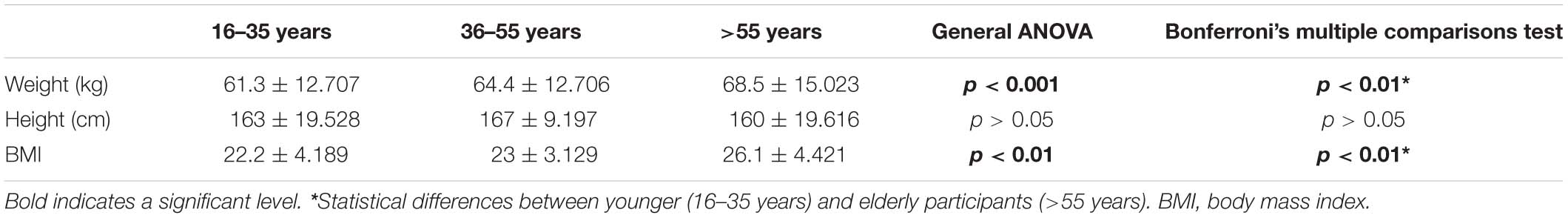
Mean values ± SD of weight, height, and BMI in the three age groups were reported in Table 1. Results showed a significant difference in weight [F(2,270) = 6.782, p < 0.001, partial η2 = 0.048] and in BMI [F(2,270) = 22.346, p < 0.01, partial η2 = 0.142]; in particular, an increase in both weight and BMI in elderly subjects (>55 years) compared to younger participants (18–35 years) (both p < 0.01, Bonferroni’s post hoc multiple comparison test; d = 0.52 and d = 0.91, for weight and BMI, respectively). Conversely, no significant differences were observed in the height between the three age groups.
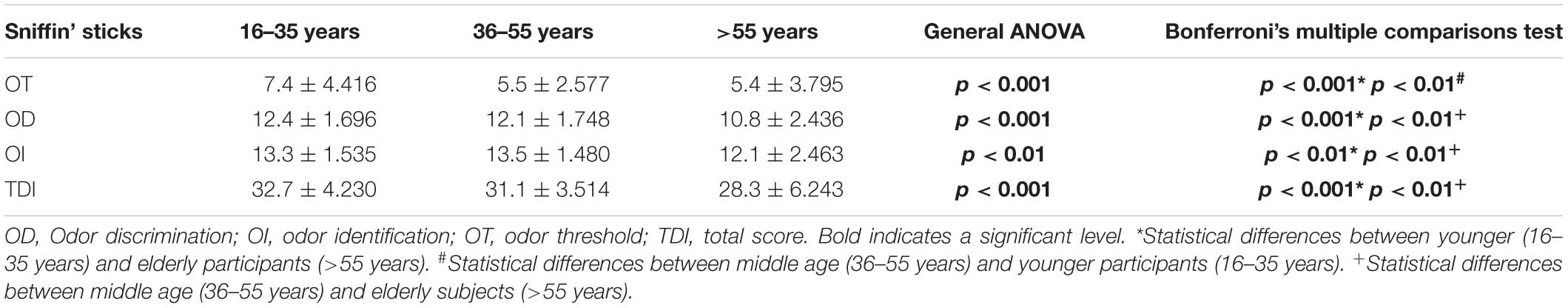
As regards the olfactory function, mean values ± SD for OT were 7.4 ± 4.416, 5.5 ± 2.577, and 5.4 ± 3.795 in the three age groups, respectively (Table 2). A significant difference in OT [F(2,270) = 8.538, p < 0.001, partial η2 = 0.059] was found, particularly an impairment in both the middle age (36–55 years) and the elderly (> 55 years) compared to the younger subjects (18–35 years) (p < 0.01 and p < 0.001, d = 0.53 and d = 0.49, respectively). Mean values ± SD were 12.4 ± 1.696, 12.1 ± 1.748, and 10.8 ± 2.436 for OD and 13.3 ± 1.535, 13.5 ± 1.480, and 12.1 ± 2.463 for OI, in the three age groups, respectively (Table 2). In the OD test, a significant performance decrease [F(2,270) = 15.852, p < 0.001, partial η2 = 0.105] was observed, in particular in elderly (age > 55 years) compared to younger (18–35 years) (p < 0.001; d = 0.77) and middle age (36–55 years) subjects (p < 0.01; d = 0.63). Statistical differences [F(2,270) = 12.122, p < 0.01, partial η2 = 0.082] were also found in the OI between both younger (16–35 years) and middle age (36–55 years) vs. elderly participants (>55 years) (both p < 0.01; d = 0.57 and d = 0.68, respectively). Consequently, a significant impairment in TDI score [F(2,270) = 20.623, p < 0.001, partial η2 = 0.133] was found, in particular, in the elderly (>55 years) compared to both the younger (18–35 years) (p < 0.001; d = 0.83) and middle age subjects (36–55 years) (p < 0.01; d = 0.56). Mean values ± SD for the TDI score were 32.7 ± 4.230, 31.1 ± 3.514, and 28.3 ± 6.243 in the three age groups, respectively (Table 2).
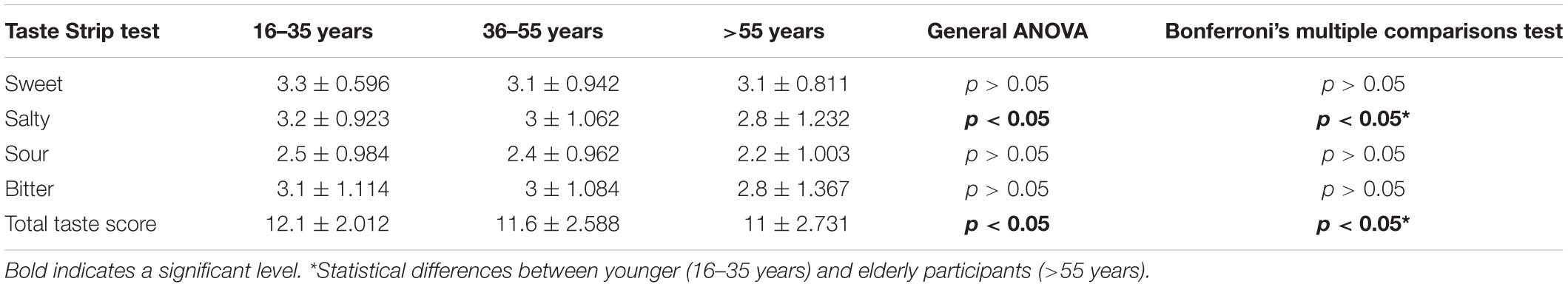
As regards gustatory function, significant differences among the three age groups were found only for the salty taste [F(2,270) = 3.037, p < 0.05, partial η2 = 0.022] and the total taste score [F(2,270) = 27.731, p < 0.01, partial η2 = 0.133] (Table 3). In particular, elderly subjects (>55 years) showed a significant decrease in salty perception and in total taste performance compared to younger participants (18–35 years) (both p < 0.05; d = 0.38 and d = 0.46, respectively). Conversely, no significant differences among the three age groups were found for sweet, sour, and bitter taste (p > 0.05).
As regards cognitive functions, mean values ± SD assessed by the MoCA test were indicated in Table 4. Mean values ± SD for memory performance were 3.7 ± 1.311, 2.8 ± 1.588, and 1.9 ± 1.545 in the three age groups, respectively (Table 4), and a significant age-related decrease was observed [F(2,270) = 35.314, p < 0.001, partial η2 = 0.207]. Statistical differences in memory scores were observed between younger (16–35 years), middle age (36–55 years), and elderly participants (>55 years) (both p < 0.001; d = 1.28 and d = 0.58, respectively). Furthermore, mean values ± SD for attention were 5.9 ± 0.296, 5.4 ± 0.752, and 5.2 ± 1.100 in the three age groups, respectively. A significant decrease in attention [F(2,270) = 19.706, p < 0.01, partial η2 = 0.127] was found, in particular, in the elderly participants (>55 years) compared to the younger ones (18–35 years) (p < 0.01; d = 0.87), while no significant differences were observed between middle aged (36–55 years) and elderly participants (>55 years). For language, mean values ± SD were 2.6 ± 0.296, 2.7 ± 0.496, and 2.1 ± 0.812 in the three age groups, respectively (Table 4). Also, in this case, significant age-related differences were detected [F(2,270) = 20.596, p < 0.01, partial η2 = 0.132], with elderly subjects (>55 years) showing a significant decrease in language function compared to the younger ones (18–35 years) (p < 0.01; d = 0.83). Conversely, no significant differences were observed in naming, abstraction, orientation, and spatial executive functions among the three age groups (all p > 0.05). Finally, according to the differences observed in memory, attention, and language MoCA subtests, differences were also detected in the total MoCA score [F(2,270) = 33.944, p < 0.001, partial η2 = 0.201], with elderly subjects (>55 years) showing a significant impairment in total cognitive functions compared to the younger ones (p < 0.001; d = 1.04). In particular, mean values ± SD for total cognitive functions (MoCA) were 27.8 ± 1.745, 26.8 ± 2.179, and 24.8 ± 3.675 in the three age groups, respectively (Table 4).
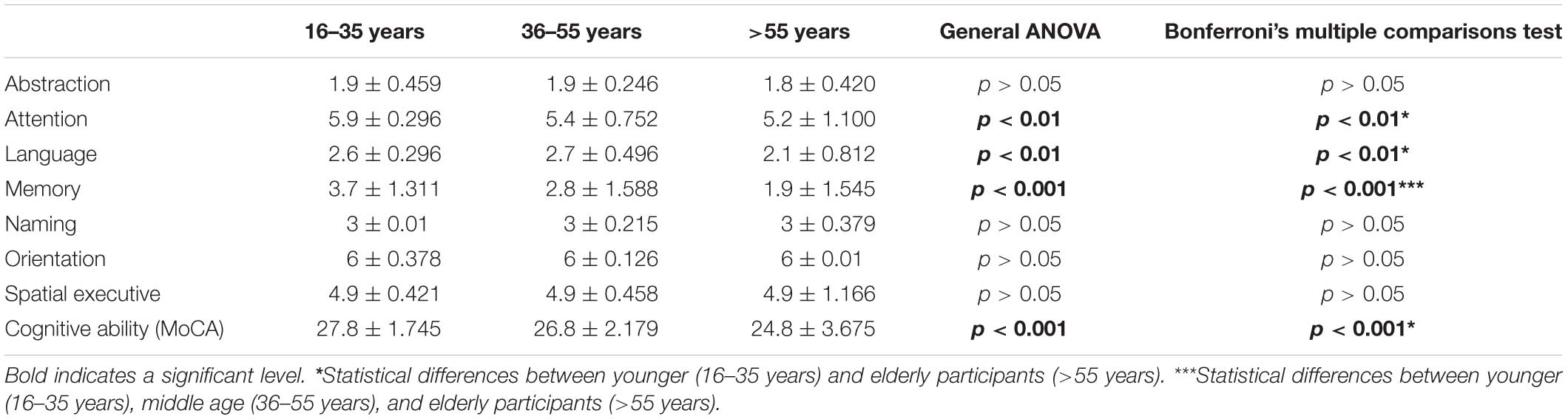
Table 4. Statistical differences for cognitive abilities (MoCA) in the three age groups (mean ± SD).
As regards the depression level, no significant differences were observed in the distribution of BDI scores among the three age groups; however, a non-significant trend (chi-square test, χ2 = 2.443, p = 0.059) was observed in the comparison between younger and elderly subjects for minimal vs. mild/moderate depression level (Table 5). In particular, among the younger group (18–35 years), 87.5% of the participants exhibited minimal depression, 9.5% showed mild depression, and only 2.9% had moderate depression (Table 5), while among the 36–55-year group, 84% of the subjects showed minimal depression, 11% exhibited mild depression, and 5% showed moderate depression. Instead, in the elderly group (>55 years), 79.4% of the participants exhibited minimal depression, 15% showed mild depression, and 5.5% exhibited moderate depression. Not one of the enrolled participants showed a severe level of depression.
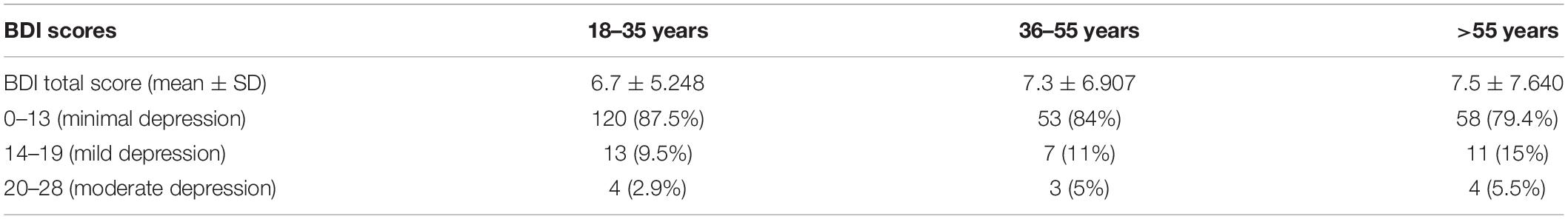
Table 5. Depression levels (mean ± SD) assessed using the Beck Depression Inventory (BDI) test and their distribution among the three age groups.
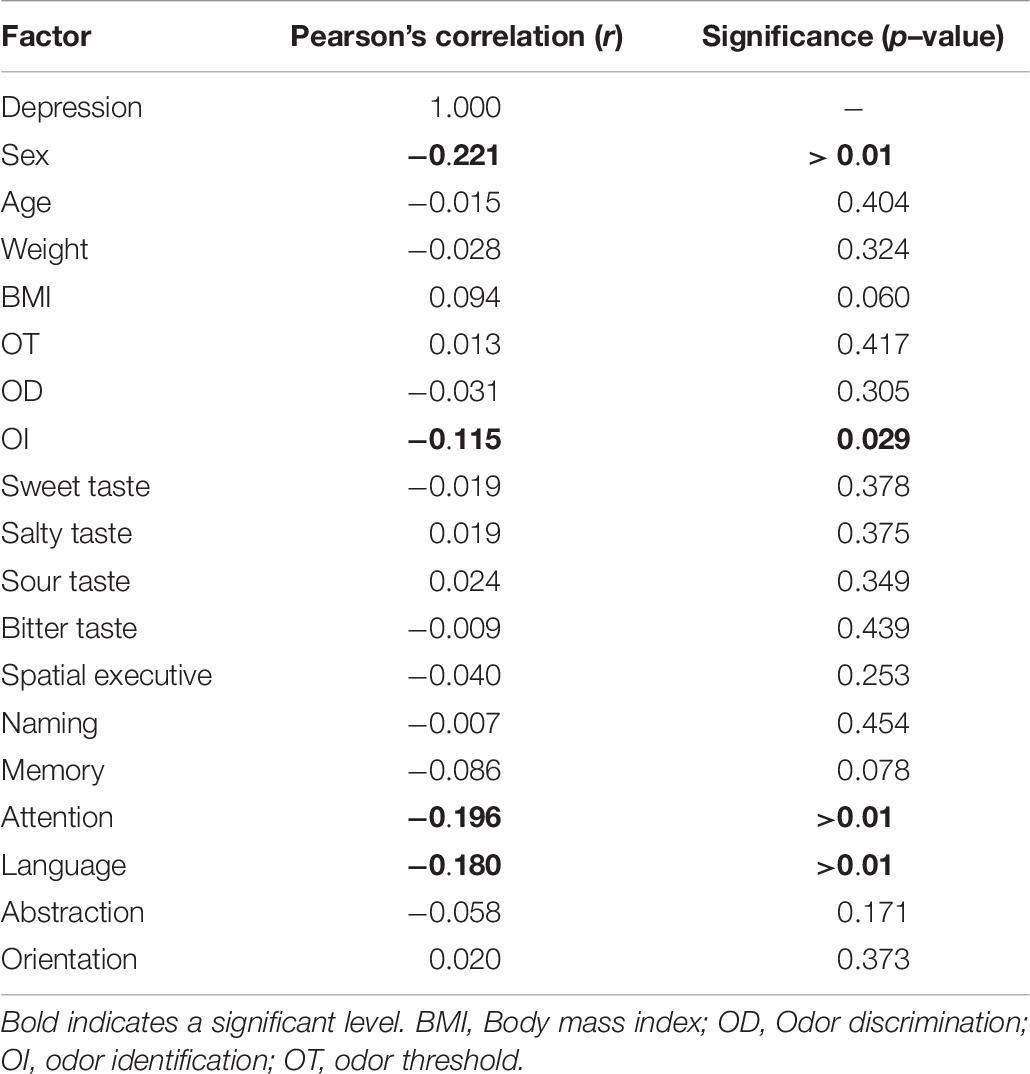
In addition, in order to evaluate all correlations between depression level and each other factor (sex, age, BMI, and olfactory, gustatory, and cognitive functions), we performed bivariate correlations. Significant negative correlations were found between the depression level vs. sex (r = −0.221, p < 0.01), OI (r = −0.115, p < 0.05), attention (r = −0.196, p < 0.01), and language (r = −0.180, p < 0.01). Conversely, no significant correlations between the depression level vs. weight, BMI, memory, spatial/executive function, orientation, abstraction, naming, OT, OD, and gustatory function were observed (Table 6).
Finally, in order to investigate the contribution of sex, age, OI, attention, and language on the depression level, an exploratory stepwise multivariate linear regression analysis was performed. The depression level was considered as the dependent variable, while in model 1, sex and age were the independent variables (predictors). A significant contribution emerged [F(2,270) = 6.948, p < 0.001] and the model explained around 5% of variance (R2 = 0.049). Instead, in model 2, a significant effect was observed for sex, age, and OI [F(2,269) = 6.238, p ≤ 0.001] with an explanation of around 7% of variance (R2 = 0.065). Finally, in model 3, a significant contribution was observed for sex, age, OI, attention, and language [F(2,267) = 6.564, p ≤ 0.001]. Model 3 explained around 11% of variance (R2 = 0.109) (Table 7).
Discussion
This study evaluated for the first time the association between depression and age-related decline in olfactory, gustatory, and cognitive function in healthy subjects. In general, our results indicated that depression could be associated to sex, OI impairment, and decreased attention and language. In line with previous studies (Altemus, 2006; Labaka et al., 2018), our data showed higher depression scores in women compared to men. A possible explanation for this gender-related difference in depression may be linked to the different levels in inflammatory cytokines (Felgel and Lotrich, 2013; Slavich and Sacher, 2019), to neurotrophic and hormonal factors (Kuehner, 2017), as well as to differences in central serotoninergic function (Gressier et al., 2016; Perry et al., 2017). Moreover, as reported in several studies (see, for example, Altemus, 2006, and references therein), women show greater influence of reproductive hormones across their life such as changes in reproductive hormones during puberty, the menstrual cycle, pregnancy, and menopause, which may alter brain function and increase the susceptibility to develop depressive conditions. In particular, hormonally induced changes in the brain levels of norepinephrine, oxytocin, prolactin, and GABA during pregnancy and lactation may induce depression (Altemus, 2006).
As regards age-related depression, our data showed no significant differences in depression level mean values among subjects in the three age ranges. A possible explanation for these data can be linked to the fact that around 80% of subjects in our sample showed depression scores between 0 and 13, so all participants showed a minimal depression level. In contrast, a previous study (Goldberg et al., 2003) reported mean depression values in elderly patients that ranged between 10 and 13. However, differences between this study and our data could be associated to general differences in sample characteristics (healthy subjects vs. medical outpatients of a behavioral medicine clinic), the diverse inclusion/exclusion criteria, or genetic, individual (such as emotional), and social (such as cultural) characteristics of participants (Laird et al., 2019).
Moreover, in line with a previous study (Starkstein and Kremer, 2001), our results showed a correlation between depression level vs. decreased attention and language. This aspect could be explained considering an age-related decrease in memory, attention, language, and total cognitive performance in elderly subjects (with >55 years). Usually, the diagnosis for age-related cognitive decline requires a reliable documentation of cognitive impairment in two or more cognitive domains such as memory, attention, and language. This deficit is classified as “age-related cognitive decline” in the DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, fourth edition (American Psychiatric Association [APA], 2000), while in the DSM-V (American Psychiatric Association [APA], 2013), it is indicated as a “neurocognitive disorder.” This age-related cognitive decline could be associated to a decrease in brain volume such as a degeneration in fronto-temporal, parietal, and occipital lobes (Peters, 2006). Moreover, the brain of elderly subjects, for at least some of these, may also show similar initial alterations as those observed in Alzheimer’s disease such as the presence of neurofibrillary tangles and senile plaques (Serrano-Pozo et al., 2011).
In addition, our results showed a significant negative association between depression and OI, while no associations were found for OT and OD. This negative correlation, as previously indicated by Zucco and Bollini (2011), could suggest a possible association between olfactory deficit in depression and impairment in cognitive function and in memory.
Our data are in line with previous studies reporting a significant association between depression and olfactory dysfunction (Atanasova et al., 2008; Croy et al., 2014a, c). This association may be explained considering the neuro-anatomical connections between olfactory, emotional, and cognitive brain areas as previously reported by Soudry et al. (2011), in view of the fact that OI is usually associated to cognitive and emotional central pathways connecting the orbitofrontal cortex, piriform cortex, hippocampal and entorhinal cortex, and the amygdala, while OT is more associated to individual differences of the nasal cavity (Masala et al., 2019). Previous studies (Doty et al., 1987; Tabert et al., 2005) indicated that the most common impairment in elderly adults without cognitive impairment is the OI deficit, which consists in the identification of a specific odor at supra-threshold concentration. Conversely, deficit in OD occurs in patients with mild cognitive impairment, or in subjects with Alzheimer’s disease and with REM sleep behavior disorder (Doty et al., 1987; Tabert et al., 2005; Galbiati et al., 2019).
In our sample, no significant associations were found between depression vs. weight and BMI. However, our results showed that elderly subjects (with >55 years) exhibited an increase in weight and BMI compared to young participants (18–35 years). These results are in line with previous studies (Reas et al., 2007; Flegal et al., 2013; Yi et al., 2015) that reported an increased prevalence of obesity in elderly subjects. A possible explanation for this result could be related to an age-related decrease in olfactory and gustatory function. As indicated in previous studies (Hummel et al., 2001; Pribitkin et al., 2003; Gudziol et al., 2007; Landis et al., 2010; Stinton et al., 2010; Boesveldt et al., 2011), patients with olfactory disorders also showed a decreased gustatory function, and this suggests the presence of mutual interactions among olfactory and gustatory senses. Different theories were reported in order to explain this age-related decrease in olfactory function such as a decrease in the number of fibers in the olfactory bulb and a reduction in the number of olfactory receptor neurons (Boyce and Shone, 2006). The age-related decline in olfactory function could also be associated to a decreased volume of the olfactory bulb (Buschhuter et al., 2008). Instead, the age-related decrease in gustatory function could be related to a reduction of the fungiform taste papillae density and to changes in salivary composition (Walliczek-Dworschak and Hummel, 2017).
Conclusion
Our data, in line with previous studies, confirm a decrease in olfactory function, an impairment in perception of salty, and a decline in memory, attention, and language related to the age. Conversely, no significant differences were observed for the depression level in relation to the different age groups. However, OI impairment and decrease in attention and language are associated with increased depression levels.
Depression is a multifactorial broadly diffused psychopathology that increases all over the world. Also, in consideration of the potential harmful consequences in people affected by depression (such as a significant negative burden in quality of life, high rates of relapse, and suicide risk), an early detection of depression becomes a factor of primary importance in the population. Our data can be useful and informative for health care workers in order to have adequate preventive strategies when depressive conditions are detected and recognized.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors under request.
Ethics Statement
The studies involving human participants were reviewed and approved by the Comitato etico Azienda Ospedaliero Universitaria di Cagliari (PROT. NP/2018/1630). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
CM and FS: conceptualization, supervision, formal analysis. CM, FL, and RP: data curation. CM: funding acquisition, project administration, validation. FL and RP: investigation, methodology. FL: software, visualization. RP and CM: writing—original draft. FS and AM: writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by a grant from the University of Cagliari (Progetti di Ricerca di Interesse Dipartimentale, PRID 2019).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Altemus, M. (2006). Sex differences in depression and anxiety disorders: potential biological determinants. Horm. Behav. 50, 534–538. doi: 10.1016/j.yhbeh.2006.06.031
American Psychiatric Association [APA] (2000). Diagnostic and Statistical Manual of Mental Disorders, 4th Edn. Arlington: American Psychiatric Association.
American Psychiatric Association [APA] (2013). Diagnostic and Statistical Manual of Mental Disorders, 5th Edn. Arlington: American Psychiatric Association.
Andrade, L., Caraveo-Anduaga, J. J., Berglund, P., Bijl, R. V., De Graaf, R., Vollebergh, W., et al. (2003). The epidemiology of major depressive episodes: results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys. Int. J. Methods Psychiatr. Res. 12, 3–21. doi: 10.1002/mpr.138
Atanasova, B., Graux, J., El Hage, W., Hommet, C., Camus, V., and Belzung, C. (2008). Olfaction: a potential cognitive marker of psychiatric disorders. Neurosci. Biobehav. Rev. 32, 1315–1325. doi: 10.1016/j.neubiorev.2008.05.003
Beck, A. T., Ward, C. H., Mendelson, M., Mock, J., and Erbaugh, J. (1961). An inventory for measuring depression. Arch. Gen. Psychiatry. 4,, 561–571. doi: 10.1001/archpsyc.1961.01710120031004
Boesveldt, S., Lindau, S. T., McClintock, M. K., Hummel, T., and Lundström, J. N. (2011). Gustatory and olfactory dysfunction in elderly adults: a national probability study. Rhinology 49, 324–330.
Boyce, J. M., and Shone, G. R. (2006). Effects of ageing on smell and taste. Postgrad. Med. J. 82, 239–241. doi: 10.1136/pgmj.2005.039453
Brai, E., and Alberi, L. (2018). Olfaction, Among the First Senses to Develop and Decline. IntechOpen: Thomas Heinbockel.
Buschhuter, D., Smitka, M., Puschmann, S., Gerber, J. C., Witt, M., Abolmaali, N. D., et al. (2008). Correlation between olfactory bulb volume and olfactory function. Neuroimage 42, 498–502. doi: 10.1016/j.neuroimage.2008.05.004
Cecchini, M. P., Federico, A., Zanini, A., Mantovani, E., Masala, C., Tinazzi, M., et al. (2019). Olfaction and taste in Parkinson’s disease: the association with mild cognitive impairment and the single cognitive domain dysfunction. J. Neural Transm. 126, 585–595. doi: 10.1007/s00702-019-01996-z
Conti, S., Bonazzi, S., Laiacona, M., Masina, M., and Coralli, M. V. (2015). Montreal Cognitive Assessment (MoCA)-Italian version: regression based norms and equivalent scores. Neurol. Sci. 36, 209–214. doi: 10.1007/s10072-014-1921-3
Croy, I., Hummel, T., Pade, A., and Pade, J. (2010). Quality of life following nasal surgery. Laryngoscope 120, 826–831. doi: 10.1002/lary.20824
Croy, I., Nordin, S., and Hummel, T. (2014a). Olfactory disorders and quality of life–an updated review. Chem. Senses 39, 185–119. doi: 10.1093/chemse/bjt072
Croy, I., Schulz, M., Blumrich, A., Hummel, C., Gerber, J., and Hummel, T. (2014b). Human olfactory lateralization requires trigeminal activation. Neuroimage 98, 289–295. doi: 10.1016/j.neuroimage.2014.05.004
Croy, I., Symmank, A., Schellong, J., Hummel, C., Gerber, J., Joraschky, P., et al. (2014c). Olfaction as a marker for depression in humans. J. Affect. Disord. 160, 80–86. doi: 10.1016/j.jad.2013.12.026
Doty, R. L., and Cameron, E. L. (2009). Sex differences and reproductive hormone influences on human odor perception. Physiol. Behav. 97, 213–228. doi: 10.1016/j.physbeh.2009.02.032
Doty, R. L., and Kamath, V. (2014). The influences of age on olfaction: a review. Front. Psychol. 7:20. doi: 10.3389/fpsyg.2014.00020
Doty, R. L., Reyes, P. F., and Gregor, T. (1987). Presence of both odor identification and detection deficits in Alzheimer’s disease. Brain Res. Bull. 18, 597–600. doi: 10.1016/0361-9230(87)90129-8
Felgel, J. C., and Lotrich, F. E. (2013). Inflammatory cytokines in depression: neurobiological mechanisms and therapeutic implications. Neuroscience 29, 199–229. doi: 10.1016/j.neuroscience.2013.04.060
Flegal, K. M., Kit, B. K., Orpana, H., and Graubard, B. I. (2013). Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 309, 71–82. doi: 10.1001/jama.2012.113905
Galbiati, A., Verga, L., Giora, E., Zucconi, M., and Ferini-Strambi, L. (2019). The risk of neurodegeneration in REM sleep behavior disorder: a systematic review and meta-analysis of longitudinal studies. Sleep Med. Rev. 43, 37–46. doi: 10.1016/j.smrv.2018.09.008
Goldberg, J. H., Breckenridge, J. N., and Sheikh, J. I. (2003). Age differences in symptoms of depression and anxiety: examining behavioral medicine outpatients. J. Behav. Med. 26, 119–132.
Gressier, F., Calati, R., and Serretti, A. (2016). 5-HTTLPR and gender differences in affective disorders: a systematic review. J. Affect. Disord. 15, 193–207. doi: 10.1016/j.jad.2015.09.027
Gudziol, H., Rahneberg, K., and Burkert, S. (2007). Anosmics are more poorly able to taste than normal persons. Laryngorhinootologie 86, 640–643.
Hoskison, E. E. (2013). Olfaction, pheromones and life. J. Laryngol. Otol. 127, 1156–1159. doi: 10.1017/s0022215113002545
Hummel, T., Kobal, G., Gudziol, H., and Mackay-Sim, A. (2007). Normative data for the “Sniffin’ Sticks” including tests of odor identification, odor discrimination, and olfactory thresholds: an upgrade based on a group of more than 3000 subjects. Eur. Arch. Otorhinolaryngol. Suppl. 264, 237–243. doi: 10.1007/s00405-006-0173-0
Hummel, T., Nesztler, C., Gallert, S., Bende, M., Kobal, G., and Nordin, S. (2001). Gustatory Sensitivity in patients with anosmia. Chem. Senses 22, 39–52.
Hummel, T., Sekinger, B., Wolf, S. R., Pauli, E., and Kobal, G. (1997). ‘Sniffin’ Sticks’: olfactory performance assessed by the combined testing of odour identification, odour discrimination and olfactory threshold. Chem. Senses 22, 39–52. doi: 10.1093/chemse/22.1.39
Hur, K., Choi, J. S., Zheng, M., Shen, J., and Wrobel, B. (2018). Association of alterations in smell and taste with depression in older adults. Laryngoscope Investig. Otolaryngol. 3, 94–99. doi: 10.1002/lio2.142
Kalmey, J. K., Thewissen, J. G., and Dluzen, D. E. (1998). Age-related size reduction of foramina in the cribriform plate. Anat. Rec. 251, 326–329. doi: 10.1002/(SICI)1097-0185(199807)251:3<326::AID-AR7>3.0.CO;2-T
Kuehner, C. (2017). Why is depression more common among women than among men? Lancet Psychiat. 4, 146–158. doi: 10.1016/s2215-0366(16)30263-2
Labaka, A., Goñi-Balentziaga, O., Lebeña, A., and Pérez-Tejada, J. (2018). Biological sex differences in depression: a systematic review. Biol. Res. Nurs. 20, 383–392. doi: 10.1177/1099800418776082
Laird, K. T., Krause, B., Funes, C., and Lavretsky, H. (2019). Psychobiological factors of resilience and depression in late life. Translat. Psychiatry 9:88.
Landis, B. N., Scheibe, M., Weber, C., Berger, R., Brämerson, A., Bende, M., et al. (2010). Chemosensory interaction: acquired olfactory impairment is associated with decreased taste function. J. Neurol. 257, 1303–1308. doi: 10.1007/s00415-010-5513-8
Landis, B. N., Welge-Luessen, A., Brämerson, A., Bende, M., Mueller, C. A., Nordin, S., et al. (2009). “Taste strips” a rapid, lateralized, gustatory bedside identification test based on impregnated filter papers. J. Neurol. 256, 242–248. doi: 10.1007/s00415-009-0088-y
Loy, F., Solari, P., Isola, M., Crnjar, R., and Masala, C. (2016). Morphological and electrophysiological analysis of tarsal sensilla in the medfly Ceratitis capitata (Wiedemann, 1824) (Diptera: Tephritidae). Ital. J. Zool. 83, 456–468.
Maheswaran, T., Abikshyeet, P., Sitra, G., Gokulanathan, S., Vaithiyanadane, V., and Jeelani, S. (2014). Gustatory dysfunction. J. Pharm. Bioallied. Sci. 6, S30–S33.
Masala, C., Käehling, C., Fall, F., and Hummel, T. (2019). Correlation between olfactory function, trigeminal sensitivity, and nasal anatomy in healthy subjects. Eur. Arch. Otorhinolaryngol. 276, 1649–1654. doi: 10.1007/s00405-019-05367-y
Masala, C., Loy, F., Piras, R., Liscia, A., Fadda, L., Moat, A., et al. (2020). Effect of olfactory and gustatory dysfunction and motor symptoms on body weight in patients with Parkinson’s disease. Brain Sci. 10:218. doi: 10.3390/brainsci10040218
Masala, C., Saba, L., Cecchini, M. P., Solla, P., and Loy, F. (2018a). Olfactory function and age: a Sniffin’ Sticks extended test study performed in sardinia. Chemosens. Percept. 11, 19–26. doi: 10.1007/s12078-017-9233-7
Masala, C., Solla, P., Liscia, A., Defazio, G., Saba, L., Cannas, A., et al. (2018b). Correlation among olfactory function, motors’ symptoms, cognitive impairment, apathy, and fatigue inpatients with Parkinson’s disease. J. Neurol. 265, 1764–1771. doi: 10.1007/s00415-018-8913-9
Mueller, C., Kallert, S., Renner, B., Stiassny, K., Temmel, A. F., Hummel, T., et al. (2003). Quantitative assessment of gustatory function in a clinical context using impregnated “taste strips”. Rhinology 41, 2–6.
Negoias, S., Croy, I., Gerber, J., Puschmann, S., Petrowski, K., Joraschky, P., et al. (2010). Reduced olfactory bulb volume and olfactory sensitivity in patients with acute major depression. Neuroscience 169, 415–421. doi: 10.1016/j.neuroscience.2010.05.012
Oleszkiewicz, A., Schriver, V. A., Croy, I., Hähner, A., and Hummel, T. (2019). Updated Sniffin’ Sticks normative data based on an extended sample of 9139 subjects. Eur. Arch. Otorhinolaryngol. 276, 719–728. doi: 10.1007/s00405-018-5248-1
Pause, B. M., Miranda, A., Goder, R., Aldenhoff, J. B., and Ferstl, R. (2001). Reduced olfactory performance in patients with major depression. J. Psychiatr. Res. 35, 271–277. doi: 10.1016/s0022-3956(01)00029-2
Perini, G., Cotta Ramusino, M., Sinforiani, E., Bernini, S., Petrachi, R., and Costa, A. (2019). Cognitive impairment in depression: recent advances and novel treatments. Neuropsychiatr. Dis. Treat. 15, 1249–1258. doi: 10.2147/ndt.s199746
Perry, L. A. M., Goldstein-Piekarski, A. N., and Williams, A. M. (2017). Sex differences modulating serotonergic polymorphisms implicated in the mechanistic pathways of risk for depression and related disorders: a mini-review: sex modulation of genes in depression. J. Neurosci. Res. 95, 737–762. doi: 10.1002/jnr.23877
Pribitkin, E., Rosenthal, M. D., and Cowart, B. J. (2003). Prevalence and causes of severe taste loss in a chemosensory clinic population. Ann. Otol. Rhinol. Laryngol. 112, 971–978. doi: 10.1177/000348940311201110
Reas, D. L., Nygård, J. F., Svensson, E., Sørensen, T., and Sandanger, I. (2007). Changes in body mass index by age, gender, and socio-economic status among a cohort of Norwegian men and women (1990–2001). BMC. Public Health 7:269. doi: 10.1186/1471-2458-7-269
Serrano-Pozo, A., Frosch, M. P., Masliah, E., and Hyman, B. T. (2011). Neuropathological alterations in Alzheimer Disease. Cold Spring Harb. Perspect. Med. 1:a006189. doi: 10.1101/cshperspect.a006189
Slavich, G. M., and Sacher, J. (2019). Stress, sex hormones, inflammation, and major depressive disorder: extending social signal transduction theory of depression to account for sex differences in mood disorders. Psychopharmacology (Berl.) 236, 3063–3079. doi: 10.1007/s00213-019-05326-9
Solla, P., Masala, C., Liscia, A., Piras, R., Ercoli, T., Fadda, L., et al. (2020). Sex-related differences in olfactory function and evaluation of possible confounding factor among patients with Parkinson’s disease. J. Neurol. 267, 57–63. doi: 10.1007/s00415-019-09551-2
Soudry, Y., Lemogne, C., Malinvaud, D., Consoli, S. M., and Bonfils, P. (2011). Olfactory system and emotion: common substrates. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 128, 18–23. doi: 10.1016/j.anorl.2010.09.007
Starkstein, S. E., and Kremer, J. L. (2001). Cerebral aging: psychological, radiological, and metabolic correlates. Dialogues Clin. Neurosci. 3, 218–228.
Stinton, N., Muhammad, A. A., Barkat, N., and Doty, R. L. (2010). Influence of smell loss on taste function. Behav. Neurosci. 124, 256–264. doi: 10.1037/a0018766
Tabert, M. H., Liu, X., Doty, R. L., Serby, M., Zamora, D., Pelton, G. H., et al. (2005). A 10-item smell identification scale related to risk for Alzheimer’s disease. Ann. Neurol. 58, 155–160. doi: 10.1002/ana.20533
Walliczek-Dworschak, U., and Hummel, T. (2017). The human sense of olfaction. Facial Plast. Surg. 33, 396–404. doi: 10.1055/s-0037-1603828
Yi, S. W., Ohrr, H., Shin, S. A., and Yi, J. J. (2015). Sex-age-specific association of body mass index with all-cause mortality among 12.8 million Korean adults: a prospective cohort study. Int. J. Epidemiol. 44, 1696–1705. doi: 10.1093/ije/dyv138
Keywords: smell, taste, depression, age, gender differences, olfaction, cognitive function
Citation: Sanna F, Loy F, Piras R, Moat A and Masala C (2021) Age-Related Cognitive Decline and the Olfactory Identification Deficit Are Associated to Increased Level of Depression. Front. Neurosci. 15:599593. doi: 10.3389/fnins.2021.599593
Received: 27 August 2020; Accepted: 18 January 2021;
Published: 22 February 2021.
Edited by:
Rufin VanRullen, Centre National de la Recherche Scientifique (CNRS), FranceReviewed by:
Enrico Giora, Vita-Salute San Raffaele University, ItalyEmanuele Brai, BrainFit4Life, Switzerland
Copyright © 2021 Sanna, Loy, Piras, Moat and Masala. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Carla Masala, Y21hc2FsYUB1bmljYS5pdA==
 Fabrizio Sanna
Fabrizio Sanna Francesco Loy
Francesco Loy Raffaella Piras3
Raffaella Piras3 Carla Masala
Carla Masala