- 1School of Physical Education and Sports Science, Guangzhou Sport University, Guangzhou, China
- 2LFE Research Group, Department of Health and Human Performance, Universidad Politécnica de Madrid, Madrid, Spain
- 3School of Dance and Martial Arts, Capital University of Physical Education and Sports, Beijing, China
- 4Centre for Active Living and Learning, University of Newcastle, Callaghan, NSW, Australia
- 5Postgraduate School, University of Harbin Sport, Harbin, China
Background: Previous studies have shown that physical activity interventions positively affect core symptoms and executive functioning in children with attention-deficit/hyperactivity disorder (ADHD). However, comparisons between different physical activity interventions still need to be made. This study is the first to analyze the effects of 10 different types of physical activity on children with ADHD through a network meta-analysis.
Methods: PubMed, Embase, Web of Science, and Cochrane Library databases were searched for randomized controlled trials on the effects of physical activity interventions on children with ADHD. The search time frame was from database creation to October 2022. Two investigators independently performed literature screening, extraction, and quality assessment. Network meta-analysis was performed with Stata 15.1.
Results: A total of 31 studies were included, and the results indicated that perceptual-motor training was the most effective in terms of motor ability and working memory (SUCRA = 82.7 and 73.3%, respectively). For attention problems and cognitive flexibility, aquatic exercise was the most effective (SUCRA = 80.9 and 86.6%, respectively). For social problems, horsemanship was the most effective (SUCRA = 79.4%). For inhibition switching, cognitive-motor training was the most effective (SUCRA = 83.5%).
Conclusion: Our study revealed that aquatic exercise and perceptual-motor training had a superior overall performance. However, the effects of various physical activity interventions on different indicators in children with ADHD can vary depending on the individual and the intervention’s validity. To ensure an appropriate physical activity intervention is selected, it is important to assess the severity of symptoms exhibited by children with ADHD beforehand.
1. Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a neurodevelopmental disorder that affects approximately 7.2% of children worldwide (Thomas et al., 2015; Thapar et al., 2017). Its primary characteristics are inattention, impulsivity, and hyperactivity (American Psychiatric Association [APA], 2013), and can be divided into three distinct subtypes: inattentive, hyperactive-impulsive, and combined inattentive and hyperactive-impulsive (American Psychiatric Association [APA], 2013). It has been shown that children with ADHD often develop diverse problems, including sleep disturbances, distractibility, motor deficits, decreased social skills, and decreased academic performance (Kim et al., 2011; Konicarova et al., 2014; Schneider et al., 2016; Yu et al., 2019). These issues are also persistent, frequently remaining when patients reach puberty and adulthood (Edition, 2013). Therefore, it is highly detrimental to the development of pediatric patients and hurts their physical and mental health, academic growth, and socialization process.
Given this, the treatment of pediatric patients with ADHD is of utmost importance. The most commonly used treatment modality is medication, such as methylphenidate (MPH) (Barkley and Poillion, 1994; Welsch et al., 2021), but it may cause side effects such as headache, stomach pain, and decreased appetite (De Sousa and Kalra, 2012). Meanwhile, in the past two decades, non-pharmacological interventions for ADHD have been rapidly developed and used (Cortese et al., 2022), such as physical activity interventions, neurofeedback interventions, and cognitive interventions (Jensen and Kenny, 2004; Sánchez-López et al., 2015; Sani et al., 2022), due to concerns about the side effects and long-term effects of pharmacological treatments (Coghill, 2019). Physical activity interventions, in particular, have gained traction due to their lower cost, ease of implementation, capacity to improve physical fitness, and additional benefits (Cornelius et al., 2017).
Previous research has uncovered a strong link between physical activity and various functions in individuals with ADHD. Barnard-Brak et al. (2011) utilized data from the Early Childhood Longitudinal Study, Kindergarten cohort (ECLS-K) to demonstrate that structured physical activity was associated with a decrease in ADHD symptoms over time. This may be due to the stimulation of the catecholamine system, which is known to be impaired in individuals with ADHD (Barnard-Brak et al., 2011).
A recent study conducted by Fard et al. (2022) investigated the impact of physical activity on the physical and mental health of children and adolescents with ADHD, with self-esteem as a moderating factor. The results indicated that physical activity and health levels are integral components of well-being for this population and that self-esteem could be a potential mediator for the connection between physical activity and health outcomes (Fard et al., 2022). Some previous meta-analyzes have also shown evidence of better efficacy of physical activity in patients with ADHD. Cerrillo-Urbina et al. (2015) explored the impact of physical activity on core symptoms of attention, impulsivity, anxiety, and executive functioning in patients with ADHD. The results showed that physical activity was more effective than non-physical activity, particularly aerobic exercise (Cerrillo-Urbina et al., 2015). Zang (2019) assessed the effects of physical activity interventions compared to non-physical activity interventions in children with ADHD. The findings indicated that physical activity interventions had a significant positive effect on anxiety and depression, aggressive behavior, thinking, and social problems in children with ADHD (Zang, 2019). Lambez et al. (2020) performed a meta-analysis evaluating the effects of non-pharmacological treatments for ADHD on cognitive functioning. The interventions studied included neurofeedback, cognitive behavioral therapy, cognitive training, and physical exercise. Physical exercise was found to have the greatest mean effect size, particularly for inhibition (Lambez et al., 2020). Seiffer et al. (2022) studied the efficacy of moderate to vigorous exercise (MVPA) on children with attention deficit hyperactivity disorder (ADHD), focusing on the intensity component of physical activity. The study indicated that MVPA was the most effective treatment for ADHD and that it might be used as an alternative (Seiffer et al., 2022). Collectively, these findings suggest that physical exercise may be an effective treatment option for ADHD patients.
However, previous meta-analyzes have largely compared physical and non-physical activity, without examined the potential distinctions between different types of physical activity interventions. The types of physical activity are diverse and include many types of aquatic exercise, ball games, mind-body exercise, and high-intensity interval training. Therefore, what specific types of physical activity provide the most significant benefit to pediatric patients with ADHD? Through a network meta-analysis of randomized controlled trial studies of physical activity in pediatric patients with ADHD, this study provides valuable information for selecting the best physical activity for treating pediatric patients with ADHD.
2. Materials and methods
2.1. Protocol and registration
The meta-analysis was conducted using the Cochrane Handbook for Systematic Reviews of Interventions, and the findings were reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyzes (PRISMA) statement (Higgins et al., 2019; Page et al., 2021). This network meta-analysis was prospectively registered in PROSPERO (CRD 42022363255).
2.2. Data sources and search strategy
We conducted a comprehensive search of four databases (PubMed, Web of Science, Embase, and the Cochrane Library) to identify relevant studies. Search strings included physical activity interventions, age ranges, and outcomes related to patients with ADHD. The search was performed up to October 2022. Supplementary Appendix A shows the detailed search strings for this search.
2.3. Study selection
Following guidelines, two authors (DW and DL) independently assessed the search results and vetted the publications retrieved from databases and reference lists. The titles and abstracts of the research were first used to determine their relevance. Then, relevant full-text studies were retrieved and evaluated for inclusion. Any disagreements were resolved through discussion and consensus.
2.4. Inclusion and exclusion criteria
This systematic review employed specified inclusion criteria. Each study met the following criteria:
(1) Only randomized controlled trials were included, and observational and cross-sectional studies were excluded.
(2) The range of age participants in the sample must be 18 years or less.
(3) The physical activity intervention had to contain a sports or physical activity component. Studies without physical activity intervention were excluded.
(4) The study must report data on indicators of motor skills, attention problems, social problems, cognitive flexibility, inhibitory switching, and working memory in children with ADHD before and after the intervention. Studies that do not report on these indicators must be excluded.
(5) Presented original data.
(6) We only analyzed papers written in English and excluded papers written in other languages.
2.5. Data extraction
The data were extracted to a standardized Excel spreadsheet. Two authors collected the required data separately from the included studies. Disagreements encountered during the process were resolved through discussion with the group. The following data were extracted from the final study: author, year, country, subject characteristics, intervention characteristics, and ADHD-related outcome indicators.
2.6. Quality assessment
The risk of bias was assessed using the Cochrane System Risk of Bias Assessment tool via Review Manager 5.4 software, which evaluates the studies’ quality on seven indicators: 1. Random sequence generation; 2. Allocation concealment; 3. Blinding of participants and personnel; 4. Blinding of outcome assessment; 5. Incomplete outcome data; 6. Selective reporting; and 7. Other bias.
2.7. Statistical analysis
We computed the standardized mean difference (SMD) and 95% CIs for continuous outcomes. The P-value of the chi-square test and the I2 index from the heterogeneity test were used to express the level of statistical heterogeneity. Different effect models were selected according to the level of heterogeneity of the test data. When the level of heterogeneity was low, a fixed-effects model (P ≥ 0.1 and I2 ≤ 50%) was used to analyze the data. Otherwise, a random-effects model (P < 0.1 or I2 values >50%) was used (Higgins et al., 2003).
According to the PRISMA NMA recommendations, we aggregated and analyzed NMA data using Markov chain Monte Carlo simulation chains in a Bayesian-based framework and Stata software (version 15.1) (Moher et al., 2015; Vats et al., 2019). We will employ the nodal method to quantify and demonstrate the congruence between indirect and direct comparisons, as obtained by Stata software instructions. If the p-value is greater than 0.05, the agreement test is passed.
Network meta-analysis was performed by employing a Bayesian model. The data were preprocessed using network group commands, and a mesh evidence map was drawn. The dots in the mesh evidence plot represent one intervention type, and the larger the area of its dots represents, the more significant the number of patients included in the study for the intervention. The line connecting the two dots is a direct comparison of the two interventions, and the thickness of the line represents the number of included studies. The larger the number of included studies, the thicker the line (Chaimani et al., 2013). The effects of the different movement methods were ranked. The effects of the different exercise modalities were ranked, the surface under the cumulative ranking curve (SUCRA) was obtained, and the probability ranking was plotted in a table. SUCRA is expressed as a percentage. The larger the percentage, the more effective the intervention. Additionally, to check for publication bias and minor sample study effects, we generated funnel plots for outcome indicators with study numbers >10 and used symmetry criteria to check (Khera et al., 2016). Stata15.1 was used to perform all statistical analyzes.
3. Results
3.1. Trial selection
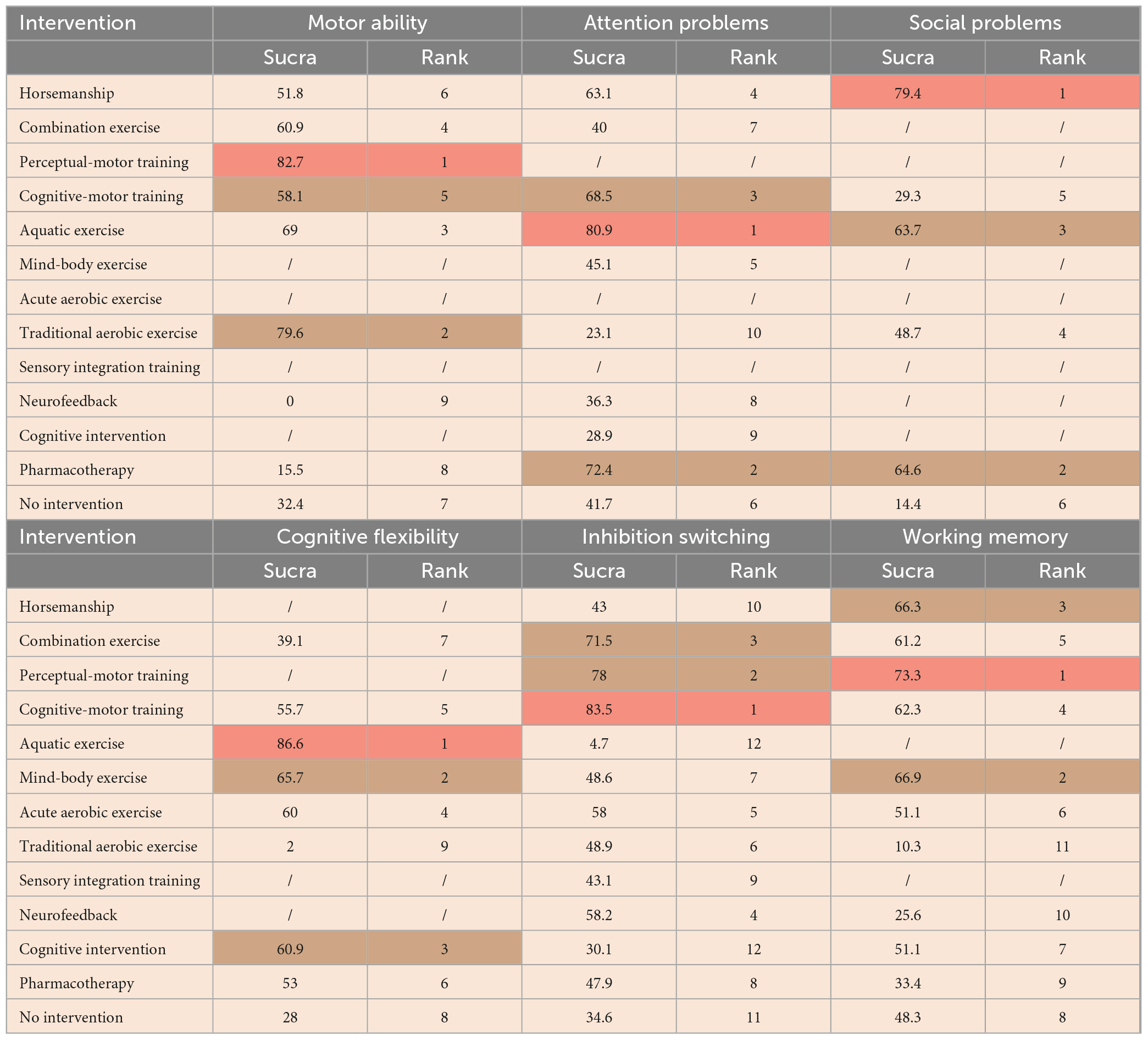
A total of 3,052 citations are yielded in the initial search of electronic databases, and an additional seven documents were manually searched. After removing duplicate studies (n = 1,129), 1,930 relevant papers remained. Subsequently, through screening, 1,809 papers were removed, and 121 papers suitable for full-text review remained, of which 90 were further eliminated. Finally, 31 studies were adopted for quantitative synthesis (Figure 1).
Figure 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyzes flow diagram of the study process.
3.2. Trial characteristics
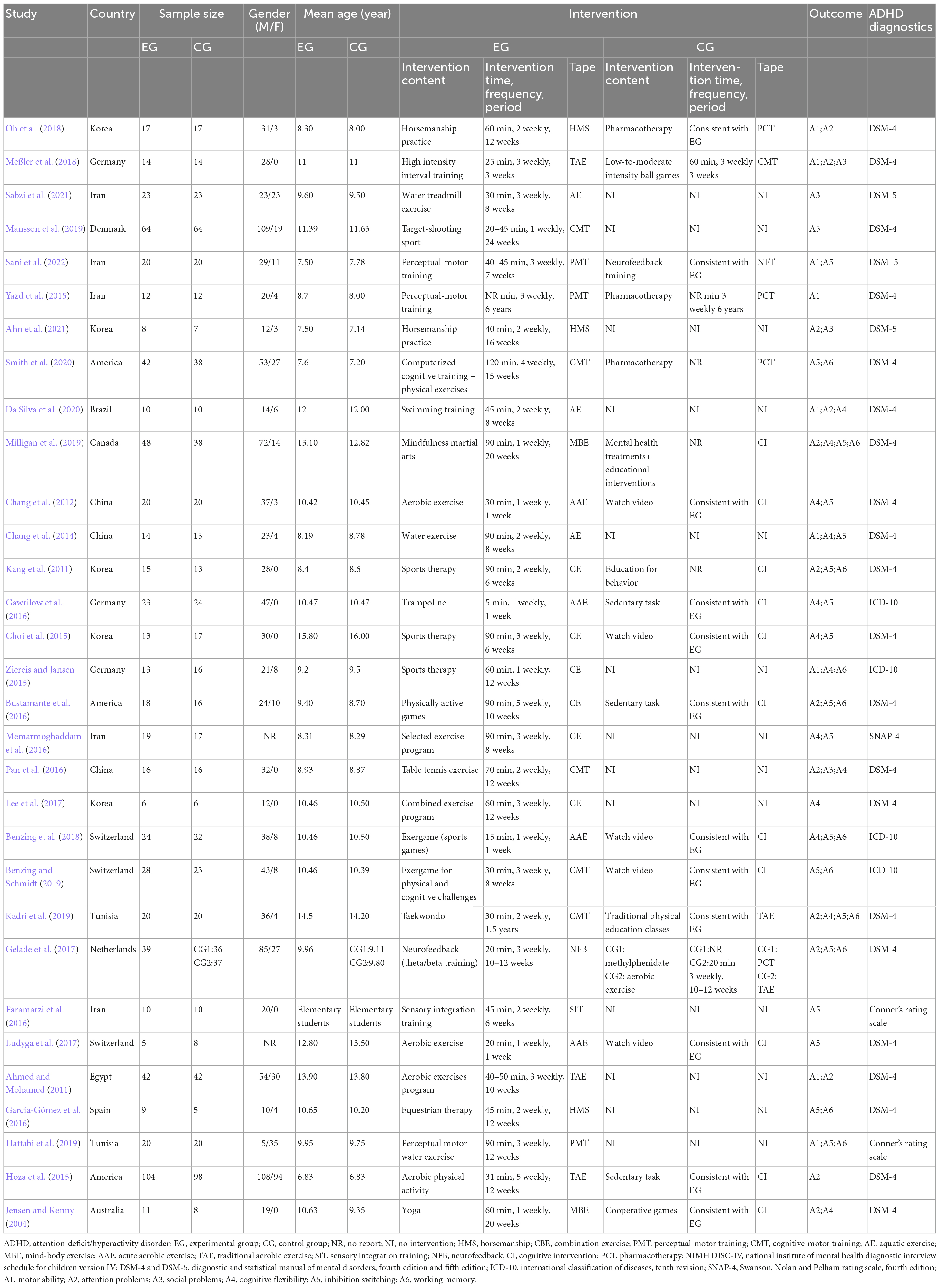
Characteristics of studies adopted are shown in Table 1, all of which were published between 2004 and 2022. The country with the highest number of included studies was Iran, with a total number of five papers. The sample size ranged from 5 to 104 for the experimental group and 5–98 for the control group, with relatively more men in the included studies. The included experimental and control groups’ mean age was less than or equal to 16 years. Interventions included cognitive-motor training (6 studies) (Hoza et al., 2015; Pan et al., 2016; Meßler et al., 2018; Benzing and Schmidt, 2019; Kadri et al., 2019; Mansson et al., 2019), combination exercise (6 studies) (Kang et al., 2011; Choi et al., 2015; Ziereis and Jansen, 2015; Bustamante et al., 2016; Memarmoghaddam et al., 2016; Lee et al., 2017), traditional aerobic exercise (5 studies) (Ahmed and Mohamed, 2011; Hoza et al., 2015; Gelade et al., 2017; Meßler et al., 2018; Kadri et al., 2019), acute aerobic exercise (4 studies) (Chang et al., 2012; Gawrilow et al., 2016; Ludyga et al., 2017; Benzing et al., 2018), aquatic exercise (3 studies) (Chang et al., 2014; Da Silva et al., 2020; Sabzi et al., 2021), horsemanship (3 studies) (García-Gómez et al., 2016; Oh et al., 2018; Ahn et al., 2021), perceptual-motor training (3 studies) (Yazd et al., 2015; Hattabi et al., 2019; Sani et al., 2022), mind-body exercise (2 studies) (Jensen and Kenny, 2004; Milligan et al., 2019), as well as sensory integration training (1 study) (Faramarzi et al., 2016). The outcome indicators for ADHD consisted of motor ability, social problems, attention problems, cognitive flexibility, inhibition switching, as well as the working memory.
3.3. Risk of bias
Eighteen studies (58.1%) had a low risk of bias with respect to random sequence generation. Twenty-one studies (67.7%) had a low risk of bias with respect to allocation concealment. Sixteen studies (51.6%) had a low risk of bias with respect to the blinding of participants and personnel. Twenty-four studies (77.4%) had a low risk of bias with respect to the blinding of outcome assessments. Twenty-nine studies (93.5%) had a low risk of bias with respect to incomplete outcome data. Thirty studies (96.8%) had a low risk of bias with respect to selective reporting. Other biases are not known. Details of the evaluation of bias results for the included literature are shown in Figures 2A, B.
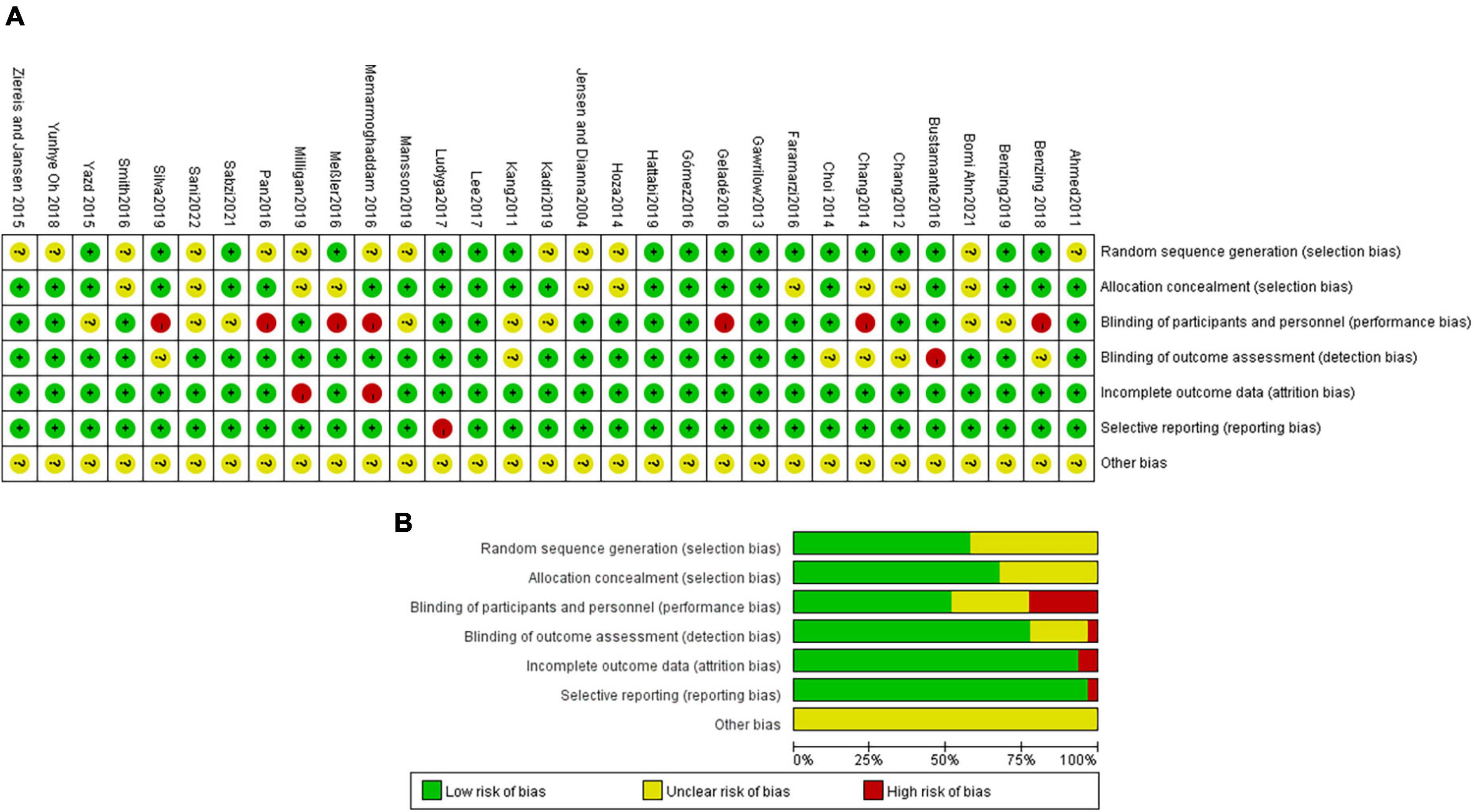
Figure 2. (A) Methodological quality of included studies. (B) The distribution of the methodological quality of included studies.
3.4. Network meta-analysis
The complete NMA figure will be presented in Supplementary Appendixes B1–6.
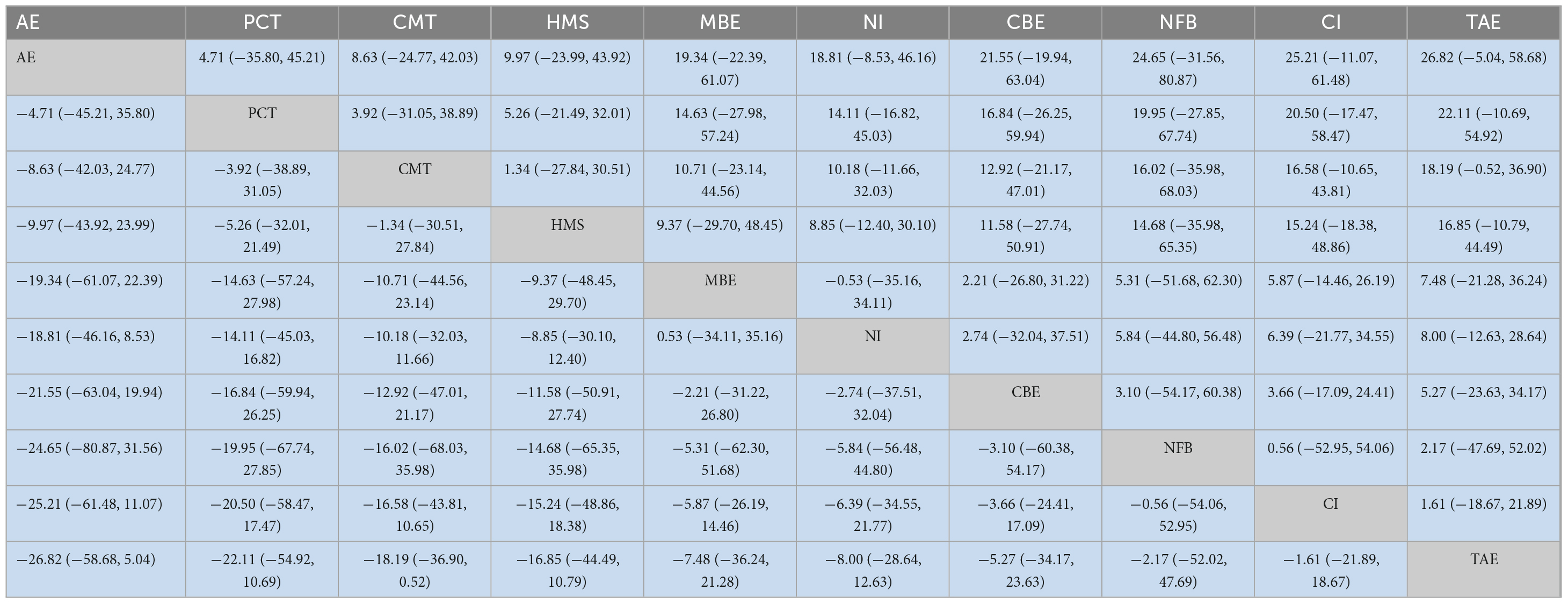
3.4.1. Motor ability
Seven studies (Chang et al., 2014; Yazd et al., 2015; Pan et al., 2016; Meßler et al., 2018; Oh et al., 2018; Da Silva et al., 2020; Sani et al., 2022) reported on the motor ability of children with ADHD, and a total of nine interventions are involved. As shown in Table 2, the statistically significant results of the network meta-analysis were as follows: Perceptual-motor training [MD = 5.26, 95% CI = (1.14, 9.38)], traditional aerobic exercise [MD = 4.74, 95% CI = (0.31, 9.16)], and aquatic exercise [MD = 3.66, 95% CI = (0.73, 6.60)], which were more effective than that with no intervention. Compared with pharmacotherapy, perceptual-motor training [MD = 9.76, 95% CI = (4.92, 14.60)], traditional aerobic exercise [MD = 9.23, 95% CI = (1.76, 16.70)], aquatic exercise [MD = 8.16, 95% CI = (1.18, 15.15)], combination exercise [MD = 7.38, 95% CI = (0.17, 14.59)] were more effective. Compared with neurofeedback, perceptual-motor training [MD = 28.68, 95% CI = (18.20, 39.15)], traditional aerobic exercise [MD = 28.15, 95% CI = (16.07, 40.23)], aquatic exercise [MD = 27.08, 95% CI = (15.46, 38.70)], combination exercise [MD = 26.30, 95% CI = (14.54, 38.05)], cognitive-motor training [MD = 26.11, 95% CI = (13.27, 38.96)], and horsemanship [MD = 24.91, 95% CI = (11.12, 38.70)] were more effective. In SUCRA, perceptual-motor training ranked first in terms of the probability of the effect of different interventions on motor performance (SUCRA: 82.7%, as shown in Supplementary Appendix C1).
3.4.2. Attention problems
Fourteen studies (Jensen and Kenny, 2004; Ahmed and Mohamed, 2011; Kang et al., 2011; Hoza et al., 2015; Bustamante et al., 2016; García-Gómez et al., 2016; Janssen et al., 2016; Pan et al., 2016; Meßler et al., 2018; Oh et al., 2018; Kadri et al., 2019; Milligan et al., 2019; Da Silva et al., 2020; Ahn et al., 2021) reported on the attention problems of children with ADHD, and a total of ten interventions are involved. As shown in Table 3, there is no statistical significance for each intervention in the network meta-analysis results. In SUCRA, aquatic exercise ranked first in terms of the probability of the effect of different interventions on the reduction of attention problems (SUCRA: 80.9%, as shown in Supplementary Appendix C2).
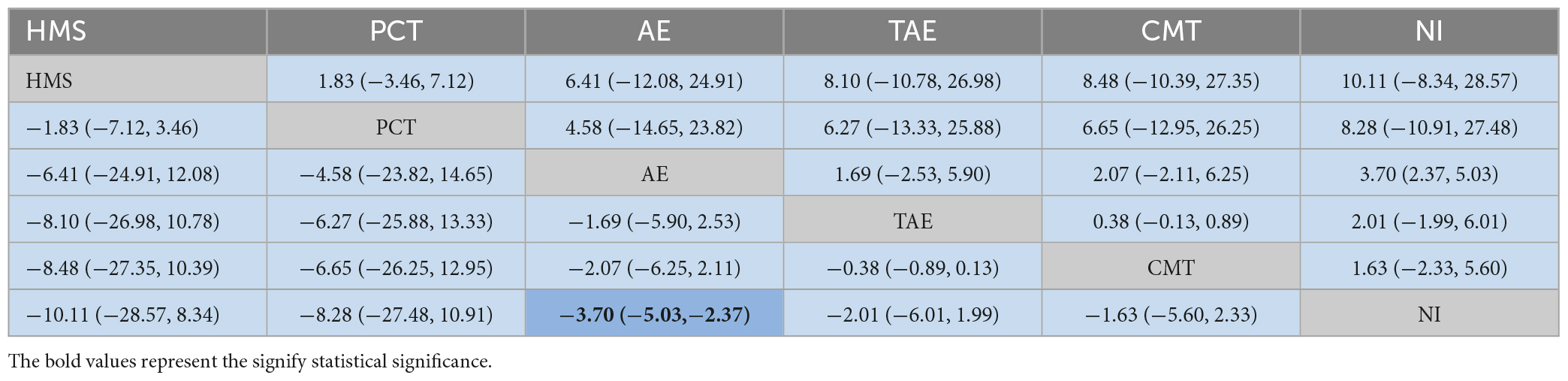
3.4.3. Social problems
Five studies (Pan et al., 2016; Meßler et al., 2018; Oh et al., 2018; Ahn et al., 2021; Sabzi et al., 2021) reported on the social problems of children with ADHD, and a total of six interventions are involved. As shown in Table 4, the statistically significant results of the network meta-analysis were as follows: Aquatic exercise [MD = −3.70, 95% CI = (−5.03, −2.37)] was more effective than that with no intervention. In the SUCRA, aquatic exercise ranked first in terms of the probability of the effect of different interventions on the reduction of social problems (SUCRA: 79.4%, as shown in Supplementary Appendix C3).
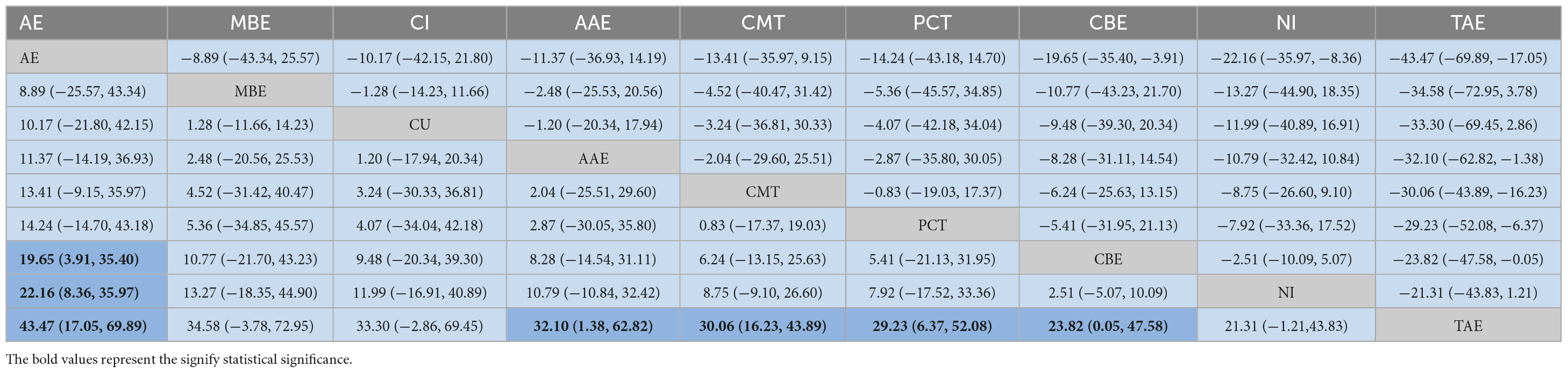
3.4.4. Cognitive flexibility
Fourteen studies (Jensen and Kenny, 2004; Kang et al., 2011; Chang et al., 2012, 2014; Hoza et al., 2015; Ziereis and Jansen, 2015; Gawrilow et al., 2016; Memarmoghaddam et al., 2016; Pan et al., 2016; Lee et al., 2017; Benzing et al., 2018; Kadri et al., 2019; Milligan et al., 2019; Da Silva et al., 2020) reported on the cognitive flexibility of children with ADHD, and a total of nine interventions are involved. As shown in Table 5, the statistically significant results of the network meta-analysis were as follows: Aquatic exercise [MD = 19.65, 95% CI = (3.91, 35.40)] was more effective than combination exercise. Aquatic exercise [MD = 22.16, 95% CI = (8.36, 35.97)] was more effective than that with no intervention. Compared to traditional aerobic exercise, aquatic exercise [MD = 43.47, 95% CI = (17.05, 69.89)], acute aerobic exercise [MD = 32.10, 95% CI = (1.38, 62.82)], and cognitive-motor training [MD = 30.06, 95% CI = (16.23, 43.89)] were more effective. In SUCRA, aquatic exercise ranked first in terms of the probability of the effect of different interventions on cognitive flexibility (SUCRA: 86.6%, as shown in Supplementary Appendix C4).
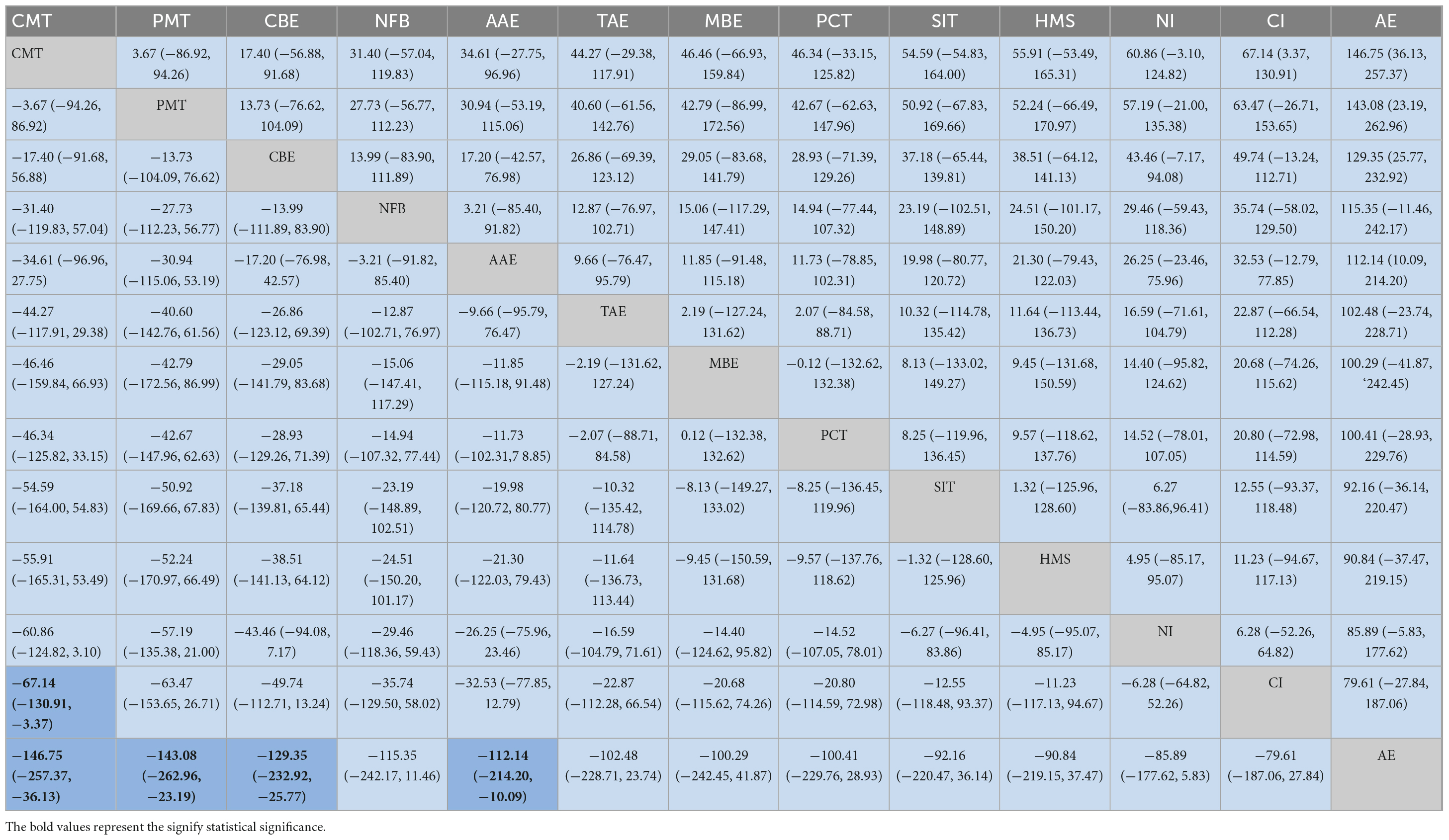
3.4.5. Inhibition switching
Eighteen studies (Kang et al., 2011; Chang et al., 2012, 2014; Choi et al., 2015; Hoza et al., 2015; Bustamante et al., 2016; Faramarzi et al., 2016; García-Gómez et al., 2016; Gawrilow et al., 2016; Janssen et al., 2016; Memarmoghaddam et al., 2016; Ludyga et al., 2017; Benzing et al., 2018; Benzing and Schmidt, 2019; Hattabi et al., 2019; Kadri et al., 2019; Mansson et al., 2019; Milligan et al., 2019; Sani et al., 2022) reported the inhibition switching of children with ADHD, and a total of 13 interventions are involved. As shown in Table 6, the statistically significant results of the network meta-analysis were as follows: Cognitive-motor training [MD = −67.14, 95% CI = (−130.91, −3.37)] was more effective than cognitive intervention. Compared with aquatic exercise, cognitive-motor training [MD = −146.75, 95% CI = (−257.37, 36.13)], perceptual-motor training [MD = −143.08, 95% CI = (−262.96, 23.19)], combination exercise [MD = −129.35, 95% CI = (−232.92, 25.77)], and acute aerobic exercise [MD = −112.14, 95% CI = (−214.20, 10.09)] were more effective. In SUCRA, cognitive-motor training ranked first in the probability of the effect of different interventions on inhibition switching (SUCRA: 83.5%, as shown in Supplementary Appendix C5).
3.4.6. Working memory
Ten studies (Kang et al., 2011; Hoza et al., 2015; Ziereis and Jansen, 2015; Bustamante et al., 2016; Janssen et al., 2016; Benzing et al., 2018; Benzing and Schmidt, 2019; Hattabi et al., 2019; Kadri et al., 2019; Milligan et al., 2019) reported on the working memory of children with ADHD, and a total of nine interventions are involved. As shown in Table 7, the statistically significant results of the network meta-analysis were as follows: cognitive-motor training [MD = 9.45, 95% CI = (2.39, 16.51)] was more effective than traditional aerobic exercise. In SUCRA, perceptual-motor training ranked first in terms of the probability of effectiveness of different interventions on working memory (SUCRA: 73.3%, as shown in Supplementary Appendix C6).
3.5. Publication bias
As is vividly shown in Supplementary Appendix D, funnel plots were employed to detect publication bias, while no significant publication bias was revealed by the visual inspection of funnel plots for all indicators.
4. Discussion
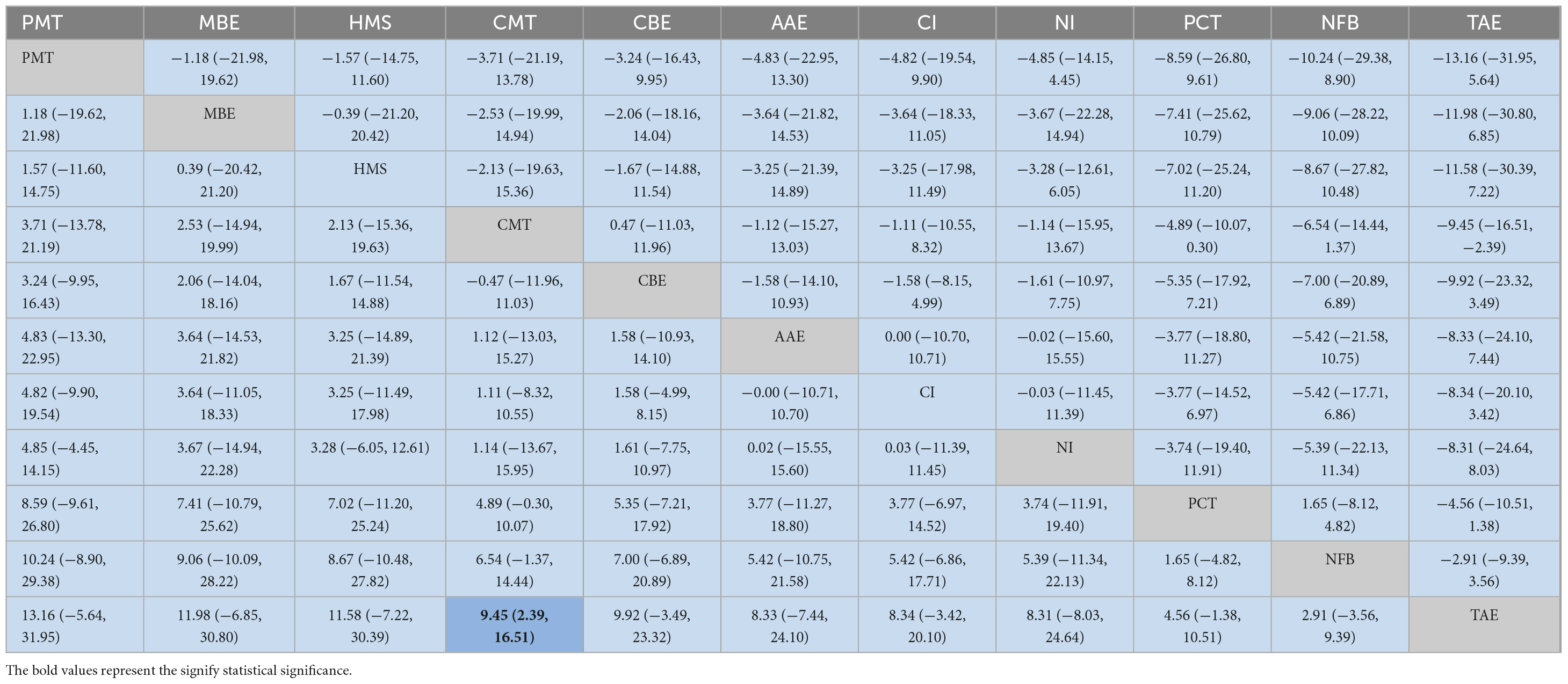
In this study, motor ability, attention problems, social problems, cognitive flexibility, inhibition switching, and working memory are adopted as outcome indicators to compare the effects of different interventions on each outcome indicator. As shown in Table 8, it has been shown in our current study that perceptual-motor training, traditional aerobic exercise, as well as aquatic exercise were the top three interventions for benign development in motor ability. When it comes to attention problems, aquatic exercise, pharmacotherapy, and cognitive-motor training were the top three interventions to reduce attention problems. As for the indicator of the social problem, horsemanship, pharmacotherapy, and aquatic exercise were the top three interventions in reducing social problems. In terms of cognitive flexibility, aquatic exercise, mind-body exercise, and cognitive intervention were the top three interventions to increase cognitive flexibility. For inhibition switching, cognitive-motor training, perceptual-motor training, and combination exercise were the top three interventions to reduce inhibition switching time. Finally, in terms of working memory indicators, perceptual-motor training, pharmacotherapy, and horsemanship were the top three interventions for enhancing working memory. It has been shown in our findings that there is no single intervention most effective across all outcome indicators, and different interventions may be more effective for different outcomes.
Perceptual-motor training is the best physical activity intervention for children with ADHD regarding motor ability and working memory. This type of training combines physical activities such as coordination, balance, and strength with perceptual tasks (Hattabi et al., 2019). Previous research has demonstrated a strong correlation between motor behavior and underlying perceptual processes (Chu and Reynolds, 2007). In particular, when physical activity is designed to improve attention, it will contribute to developing executive functions (Piek et al., 2004; Hung et al., 2013). By combining training activities with perceptual tasks, there is potential for an overall improvement in motor ability and working memory in children with ADHD (Mandich et al., 2001).
The aquatic exercise was the intervention with the highest frequency (4 sessions) in the top three rankings for all outcome indicators and the best physical activity intervention in terms of both attention problems and cognitive flexibility. Aquatic exercise is a form of physical activity in which the training process is completed in an aquatic environment. Due to the fluid nature of water, physical activity in an aquatic environment requires participants to constantly pay attention to the environment’s fluctuations (Vivas et al., 2011). At the same time, the buoyancy effect of water provides an auxiliary force, resistance, or support, which makes physical activity in the water environment safer, and children’s activity can be more active (Broach and Dattilo, 1996). For example, swimming in water sports is a highly coordinated and lateralized sport requiring control of the upper and lower limbs in an aquatic environment (Colgate and Lynch, 2004). This feature may allow for further activation of brain regions in the prefrontal cortex and amygdala, thus contributing to improved attentional problems and cognitive flexibility (Faw, 2003).
Horsemanship is the best physical activity intervention in terms of indicators of social problems. Horsemanship is a physical activity modality through learning activities with horses as a vehicle (Kern et al., 2011). It has been shown that because equestrian learning requires participants to establish trust and frequent interaction with the horse, it contributes to developing participants’ social competence (Hauge et al., 2014) and self-efficacy (Bizub et al., 2003). With this mutual relationship with the horse, children experience the horse’s feelings, which are then internalized in their behavior, enabling further development of empathy. This change will likely transfer to human interactions (Granados and Agis, 2011). At the same time, the horse’s rhythmic activity also improves the participants’ physiological responses to stress and impulsivity (Tyler, 1994; Jang et al., 2015).
Cognitive-motor training is the best physical activity intervention for inhibiting conversion indicators. Cognitive-motor training is an intervention that integrates cognitive and motor tasks to promote an individual’s physical and mental health (Amini et al., 2022). It has been shown that performing two or more cognitive-motor tasks simultaneously, such as computation in postural training and movement under computer games, will contribute more to improvements in cognitive domains compared to single-task training (van der Niet et al., 2016; Luder et al., 2018; Schmidt et al., 2020) while reducing reaction time (Wollesen et al., 2020). Cognitive-motor training requires participants to use both skill and cognitive effort to cope with unpredictable stimuli from the external environment (Chuang et al., 2015). Therefore, some researchers have suggested that this may improve participants’ executive functioning, including improvements in inhibitory switching (Kunstler et al., 2018; Gao et al., 2019).
In conclusion, physical activity interventions have varying levels of effect on different indicators related to the symptoms of children with ADHD. This impact is dependent on the components, characteristics, and settings of the intervention. Nevertheless, physical activity interventions have been found to have numerous advantages across multiple indicators.
5. Strengths and limitations
One advantage of our current study is that we are the first network meta-analysis of the effects of physical activity on symptoms related to children with ADHD, which provides some scientific reference for selecting appropriate physical activity therapy for children with ADHD. The second advantage is that this study explored the effects of different physical activities on different symptom indicators in children with ADHD, which can provide some scientific reference for targeted treatment. The third advantage is that the current study only included studies from randomized controlled trials and excluded observational and cross-sectional studies, which helped to enhance the reliability of the findings. However, our reticulated meta-analysis also has some limitations that may affect the interpretation of the results. First, the relatively small number of available studies and the limited number and sample size of studies included in the analysis makes it difficult to give a particularly robust conclusion. Second, the outcome indicators that could be included are still limited. In the future, more outcome indicators of symptoms related to children with ADHD should be included based on an adequate number of studies. Finally, findings should be interpreted with caution because of the small number of studies and the limited evidence for direct comparisons of some interventions. Relevant studies should be further expanded to provide evidence with higher confidence.
6. Conclusion
Our current study showed that the overall performance of aquatic exercise and perceptual-motor training was better. However, different physical activity interventions have different validity and individual differences regarding their effects on different indicators in children with ADHD. Therefore, to ensure that the most suitable physical activity intervention is chosen, it is essential to accurately assess each child’s specific ADHD symptoms before implementation.
Author contributions
CL and DL conceived and designed the study. DL and DW collected the data. DL, DW, and WC analyzed and interpreted the data. DL drafted the manuscript. JY and WZ revised the manuscript. All authors have read and agreed to the published version of the manuscript, and contributed to the study conception and design.
Acknowledgments
We would like to thank the researchers and study participants for their contributions.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnins.2023.1139263/full#supplementary-material
References
Ahmed, G., and Mohamed, S. (2011). Effect of regular aerobic exercises on behavioral, cognitive and psychological response in patients with attention deficit-hyperactivity disorder. Life Sci. 8, 392–397.
Ahn, B., Joung, Y., Kwon, J., Lee, D., Oh, S., Kim, B., et al. (2021). Effects of equine-assisted activities on attention and quality of life in children with cerebral palsy in a randomized trial: Examining the comorbidity with attention-deficit/hyperactivity disorder. BMC Pediatr. 21:135. doi: 10.1186/s12887-021-02597-0
American Psychiatric Association [APA] (2013). Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: American psychiatric association. doi: 10.1176/appi.books.9780890425596
Amini, A., Vaezmousavi, M., and Shirvani, H. (2022). The effectiveness of cognitive-motor training on reconstructing cognitive health components in older male adults, recovered from the COVID-19. Neurol. Sci. 43, 1395–1403. doi: 10.1007/s10072-021-05502-w
Barkley, R., and Poillion, M. (1994). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment. Behav. Disord. 19, 150–152. doi: 10.1177/019874299401900205
Barnard-Brak, L., Davis, T., Sulak, T., and Brak, V. (2011). The association between physical education and symptoms of attention deficit hyperactivity disorder. J. Phys. Act. Health 8, 964–970. doi: 10.1123/jpah.8.7.964
Benzing, V., and Schmidt, M. (2019). The effect of exergaming on executive functions in children with ADHD: A randomized clinical trial. Scand. J. Med. Sci. Sports 29, 1243–1253. doi: 10.1111/sms.13446
Benzing, V., Chang, Y., and Schmidt, M. (2018). Acute physical activity enhances executive functions in children with ADHD. Sci. Rep. 8:12382. doi: 10.1038/s41598-018-30067-8
Bizub, A., Joy, A., and Davidson, L. (2003). “It’s like being in another world”: Demonstrating the benefits of therapeutic horseback riding for individuals with psychiatric disability. Psychiatr. Rehabil. J. 26, 377–384. doi: 10.2975/26.2003.377.384
Broach, E., and Dattilo, J. (1996). Aquatic therapy: A viable therapeutic recreation intervention. Ther. Recreation J. 30, 213–229.
Bustamante, E., Davis, C., Frazier, S., Rusch, D., Fogg, L., Atkins, M., et al. (2016). Randomized Controlled Trial of Exercise for ADHD and Disruptive Behavior Disorders. Med. Sci. Sports Exerc. 48, 1397–1407. doi: 10.1249/MSS.0000000000000891
Cerrillo-Urbina, A., García-Hermoso, A., Sánchez-López, M., Pardo-Guijarro, M., Santos Gómez, J., and Martínez-Vizcaíno, V. (2015). The effects of physical exercise in children with attention deficit hyperactivity disorder: A systematic review and meta-analysis of randomized control trials. Child Care Health Dev. 41, 779–788. doi: 10.1111/cch.12255
Chaimani, A., Higgins, J., Mavridis, D., Spyridonos, P., and Salanti, G. (2013). Graphical tools for network meta-analysis in STATA. PLoS One 8:e76654. doi: 10.1371/journal.pone.0076654
Chang, Y., Hung, C., Huang, C., Hatfield, B., and Hung, T. (2014). Effects of an aquatic exercise program on inhibitory control in children with ADHD: A preliminary study. Arch. Clin. Neuropsychol. 29, 217–223. doi: 10.1093/arclin/acu003
Chang, Y., Liu, S., Yu, H., and Lee, Y. (2012). Effect of acute exercise on executive function in children with attention deficit hyperactivity disorder. Arch. Clin. Neuropsychol. 27, 225–237. doi: 10.1093/arclin/acr094
Choi, J., Han, D., Kang, K., Jung, H., and Renshaw, P. (2015). Aerobic exercise and attention deficit hyperactivity disorder: Brain research. Med. Sci. Sports Exerc. 47, 33–39. doi: 10.1249/MSS.0000000000000373
Chu, S., and Reynolds, F. (2007). Occupational therapy for children with attention deficit hyperactivity disorder (ADHD), part 1: A delineation model of practice. Br. J. Occup. Ther. 70, 372–383. doi: 10.1177/030802260707000902
Chuang, L., Hung, H., Huang, C., Chang, Y., and Hung, T. (2015). A 3-month intervention of Dance Dance Revolution improves interference control in elderly females: A preliminary investigation. Exp. Brain Res. 233, 1181–1188. doi: 10.1007/s00221-015-4196-x
Coghill, D. (2019). Debate: Are stimulant medications for attention-deficit/hyperactivity disorder effective in the long term?(For). J. Am. Acad. Child Adolesc. Psychiatry 58, 938–939. doi: 10.1016/j.jaac.2019.07.002
Colgate, J., and Lynch, K. (2004). Mechanics and control of swimming: A review. IEEE J. Ocean. Eng. 29, 660–673. doi: 10.1109/JOE.2004.833208
Cornelius, C., Fedewa, A., and Ahn, S. (2017). The effect of physical activity on children with ADHD: A quantitative review of the literature. J. Appl. Sch. Psychol. 33, 136–170. doi: 10.1080/15377903.2016.1265622
Cortese, S., Sabe, M., Chen, C., Perroud, N., and Solmi, M. (2022). Half a century of research on attention-deficit/hyperactivity disorder: A scientometric study. Neurosc. Biobehav. Rev. 140:104769. doi: 10.1016/j.neubiorev.2022.104769
Da Silva, L., Doyenart, R., Salvan, P., Rodrigues, W., Lopes, J., Gomes, K., et al. (2020). Swimming training improves mental health parameters, cognition and motor coordination in children with Attention Deficit Hyperactivity Disorder. Int. J. Environ. Health Res. 30, 584–592. doi: 10.1080/09603123.2019.1612041
De Sousa, A., and Kalra, G. (2012). Drug therapy of attention deficit hyperactivity disorder: Current trends. Mens Sana Monogr. 10:45. doi: 10.4103/0973-1229.87261
Edition, F. (2013). Diagnostic and statistical manual of mental disorders. Am. Psychiatr. Assoc. 21, 591–643.
Faramarzi, S., Rad, S., and Abedi, A. (2016). Effect of sensory integration training on executive functions of children with attention deficit hyperactivity disorder. Neuropsychiatr. Neuropsychol. 11, 1–5.
Fard, F., Baniasadi, T., Ahmadi, T., Biyabani, P., and Mofrad, S. (2022). Effects of physical activity on wellbeing among children with ADHD: A mediation by self-esteem. J. Hum. Ins. 6, 1–6.
Faw, B. (2003). Pre-frontal executive committee for perception, working memory, attention, long-term memory, motor control, and thinking: A tutorial review. Conscious. Cogn. 12, 83–139. doi: 10.1016/S1053-8100(02)00030-2
Gao, Z., Zeng, N., Pope, Z., Wang, R., and Yu, F. (2019). Effects of exergaming on motor skill competence, perceived competence, and physical activity in preschool children. J. Sport Health Sci. 8, 106–113. doi: 10.1016/j.jshs.2018.12.001
García-Gómez, A., Rodriguez-Jimenez, M., Guerrero-Barona, E., Rubio-Jimenez, J., Garcia-Pena, I., and Moreno-Manso, J. (2016). Benefits of an experimental program of equestrian therapy for children with ADHD. Res. Dev. Disabil. 59, 176–185. doi: 10.1016/j.ridd.2016.09.003
Gawrilow, C., Stadler, G., Langguth, N., Naumann, A., and Boeck, A. (2016). Physical activity, affect, and cognition in children with symptoms of ADHD. J. Atten. Disord. 20, 151–162. doi: 10.1177/1087054713493318
Gelade, K., Bink, M., Janssen, T., van Mourik, R., Maras, A., and Oosterlaan, J. (2017). An RCT into the effects of neurofeedback on neurocognitive functioning compared to stimulant medication and physical activity in children with ADHD. Eur. Child Adolesc. Psychiatry 26, 457–468. doi: 10.1007/s00787-016-0902-x
Granados, A., and Agis, I. (2011). Why children with special needs feel better with hippotherapy sessions: A conceptual review. J. Altern. Complement. Med. 17, 191–197. doi: 10.1089/acm.2009.0229
Hattabi, S., Bouallegue, M., Ben Yahya, H., and Bouden, A. (2019). Rehabilitation of ADHD children by sport intervention: A Tunisian experience. La Tunis. Med. 97, 874–881.
Hauge, H., Kvalem, I., Berget, B., Enders-Slegers, M., and Braastad, B. (2014). Equine-assisted activities and the impact on perceived social support, self-esteem and self-efficacy among adolescents–an intervention study. Int. J. Adolesc. Youth 19, 1–21. doi: 10.1080/02673843.2013.779587
Higgins, J., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M., et al. (2019). Cochrane handbook for systematic reviews of interventions. Hoboken, NJ: John Wiley & Sons. doi: 10.1002/9781119536604
Higgins, J., Thompson, S., Deeks, J., and Altman, D. (2003). Measuring inconsistency in meta-analyses. BMJ 327, 557–560. doi: 10.1136/bmj.327.7414.557
Hoza, B., Smith, A., Shoulberg, E., Linnea, K., Dorsch, T., Blazo, J., et al. (2015). A randomized trial examining the effects of aerobic physical activity on attention-deficit/hyperactivity disorder symptoms in young children. J. Abnorm. Child Psychol. 43, 655–667. doi: 10.1007/s10802-014-9929-y
Hung, C., Chang, Y., Chan, Y., Shih, C., Huang, C., and Hung, T. (2013). Motor ability and inhibitory processes in children with ADHD: A neuroelectric study. J. Sport Exerc. Psychol. 35, 322–328. doi: 10.1123/jsep.35.3.322
Jang, B., Song, J., Kim, J., Kim, S., Lee, J., Shin, H., et al. (2015). Equine-assisted activities and therapy for treating children with attention-deficit/hyperactivity disorder. J. Altern. Complement. Med. 21, 546–553. doi: 10.1089/acm.2015.0067
Janssen, T., Bink, M., Geladé, K., Van Mourik, R., Maras, A., and Oosterlaan, J. (2016). A randomized controlled trial investigating the effects of neurofeedback, methylphenidate, and physical activity on event-related potentials in children with attention-deficit/hyperactivity disorder. J. Adolesc. Psychopharmacol. 26, 344–353. doi: 10.1089/cap.2015.0144
Jensen, P., and Kenny, D. (2004). The effects of yoga on the attention and behavior of boys with attention-deficit/hyperactivity disorder (ADHD). J. Atten. Disord. 7, 205–216. doi: 10.1177/108705470400700403
Kadri, A., Slimani, M., Bragazzi, N., Tod, D., and Azaiez, F. (2019). Effect of taekwondo practice on cognitive function in adolescents with attention deficit hyperactivity disorder. Int. J. Environ. Res. Public Health 16:204. doi: 10.3390/ijerph16020204
Kang, K., Choi, J., Kang, S., and Han, D. (2011). Sports therapy for attention, cognitions and sociality. Int. J. Sports Med. 32, 953–959. doi: 10.1055/s-0031-1283175
Kern, J., Fletcher, C., Garver, C., Mehta, J., Grannemann, B., Knox, K., et al. (2011). Prospective Trial of Equine-assisted Activities in Autism Spectrum Disorder. Altern. Ther. Health Med. 17, 14–20.
Khera, R., Murad, M., Chandar, A., Dulai, P., Wang, Z., Prokop, L., et al. (2016). Association of pharmacological treatments for obesity with weight loss and adverse events: A systematic review and meta-analysis. JAMA 315, 2424–2434. doi: 10.1001/jama.2016.7602
Kim, J., Mutyala, B., Agiovlasitis, S., and Fernhall, B. (2011). Health behaviors and obesity among US children with attention deficit hyperactivity disorder by gender and medication use. Prev. Med. 52, 218–222. doi: 10.1016/j.ypmed.2011.01.003
Konicarova, J., Bob, P., and Raboch, J. (2014). Balance deficits and ADHD symptoms in medication-naive school-aged boys. Neuropsychiatr. Dis. Treat. 10, 85–88. doi: 10.2147/NDT.S56017
Kunstler, E., Finke, K., Gunther, A., Klingner, C., Witte, O., and Bublak, P. (2018). Motor-cognitive dual-task performance: Effects of a concurrent motor task on distinct components of visual processing capacity. Psychol. Res. 82, 177–185. doi: 10.1007/s00426-017-0951-x
Lambez, B., Harwood-Gross, A., Golumbic, E., and Rassovsky, Y. (2020). Non-pharmacological interventions for cognitive difficulties in ADHD: A systematic review and meta-analysis. J. Psychiatr. Res. 120, 40–55. doi: 10.1016/j.jpsychires.2019.10.007
Lee, S., Song, J., and Park, J. (2017). Effects of combination exercises on electroencephalography and frontal lobe executive function measures in children with ADHD: A pilot study. Biomed. Res. 2017, S455–S460.
Luder, B., Kiss, R., and Granacher, U. (2018). Single- and dual-task balance training are equally effective in youth. Fronti. Psychol. 9:912. doi: 10.3389/fpsyg.2018.00912
Ludyga, S., Brand, S., Gerber, M., Weber, P., Brotzmann, M., Habibifar, F., et al. (2017). An event-related potential investigation of the acute effects of aerobic and coordinative exercise on inhibitory control in children with ADHD. Dev. Cogn.Neurosci. 28, 21–28. doi: 10.1016/j.dcn.2017.10.007
Mandich, A., Polatajko, H., Macnab, J., and Miller, L. (2001). Treatment of children with developmental coordination disorder: What is the evidence?. Phys. Occup. Ther. Pediatr. 20, 51–68. doi: 10.1300/J006v20n02_04
Mansson, A., Elmose, M., Mejldal, A., Dalsgaard, S., and Roessler, K. (2019). The effects of practicing target-shooting sport on the severity of inattentive, hyperactive, and impulsive symptoms in children: A non-randomised controlled open-label study in Denmark. Nord. J. Psychiatry 73, 233–243. doi: 10.1080/08039488.2019.1612467
Memarmoghaddam, M., Torbati, H., Sohrabi, M., Mashhadi, A., and Kashi, A. (2016). Effects of a selected exercise programon executive function of children with attention deficit hyperactivity disorder. J. Med. Life 9, 373–379.
Meßler, C., Holmberg, H.-C., and Sperlich, B. (2018). Multimodal therapy involving high-intensity interval training improves the physical fitness, motor skills, social behavior, and quality of life of boys with ADHD: A randomized controlled study. J. Atten. Disord. 22, 806–812. doi: 10.1177/1087054716636936
Milligan, K., Sibalis, A., McKeough, T., Lackner, C., Schmidt, L., Pun, C., et al. (2019). Impact of mindfulness martial arts training on neural and behavioral indices of attention in youth with learning disabilities and co-occurring mental health challenges. Mindfulness 10, 2152–2164. doi: 10.1007/s12671-019-01161-3
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., et al. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 4, 1–9. doi: 10.1186/2046-4053-4-1
Oh, Y., Joung, Y., Jang, B., Yoo, J., Song, J., Kim, J., et al. (2018). Efficacy of hippotherapy versus pharmacotherapy in attention-deficit/hyperactivity disorder: A randomized clinical trial. J. Alternat. Complement. Med. 24, 463–471. doi: 10.1089/acm.2017.0358
Page, M., McKenzie, J., Bossuyt, P., Boutron, I., Hoffmann, T., Mulrow, C., et al. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 88:105906. doi: 10.1016/j.ijsu.2021.105906
Pan, C., Chu, C., Tsai, C., Lo, S., Cheng, Y., and Liu, Y. (2016). A racket-sport intervention improves behavioral and cognitive performance in children with attention-deficit/hyperactivity disorder. Res. Dev. Disabil. 57, 1–10. doi: 10.1016/j.ridd.2016.06.009
Piek, J., Dyck, M., Nieman, A., Anderson, M., Hay, D., Smith, L., et al. (2004). The relationship between motor coordination, executive functioning and attention in school aged children. Arch. Clin. Neuropsychol. 19, 1063–1076. doi: 10.1016/j.acn.2003.12.007
Sabzi, A., Dana, A., Salehian, M., and Yekta, H. (2021). The effect of water treadmill exercise on children with attention deficit hyperactivity disorder. Int. J. Pediatr. 9, 13671–13681.
Sánchez-López, M., Pardo-Guijarro, M., Del Campo, D., Silva, P., Martínez-Andrés, M., Gulías-González, R., et al. (2015). Physical activity intervention (Movi-Kids) on improving academic achievement and adiposity in preschoolers with or without attention deficit hyperactivity disorder: Study protocol for a randomized controlled trial. Trials 16:456. doi: 10.1186/s13063-015-0992-7
Sani, N., Akbarfahimi, M., Akbari, S., Zarei, M., and Taghizadeh, G. (2022). Neurofeedback training versus perceptual-motor exercises interventions in visual attention for children with attention-deficit/hyperactivity disorder: A randomized controlled trial. Basic Clin. Neurosci. 13, 215–224. doi: 10.32598/bcn.2021.563.2
Schmidt, M., Mavilidi, M., Singh, A., and Englert, C. (2020). Combining physical and cognitive training to improve kindergarten children’s executive functions: A cluster randomized controlled trial. Contemp. Educ. Psychol. 63:101908. doi: 10.1016/j.cedpsych.2020.101908
Schneider, H., Lam, J., and Mahone, E. (2016). Sleep disturbance and neuropsychological function in young children with ADHD. Child Neuropsychol. 22, 493–506. doi: 10.1080/09297049.2015.1018153
Seiffer, B., Hautzinger, M., Ulrich, R., and Wolf, S. (2022). The efficacy of physical activity for children with attention deficit hyperactivity disorder: A meta-analysis of randomized controlled trials. J. Atten. Disord. 26, 656–673. doi: 10.1177/10870547211017982
Smith, S. D., Vitulano, L. A., Katsovich, L., Li, S., Moore, C., Li, F. et al. (2020). A randomized controlled trial of an integrated brain, body, and social intervention for children with ADHD. J. Atten. Disord. 24, 780–794. doi: 10.1177/1087054716647490
Thapar, A., Cooper, M., and Rutter, M. (2017). Neurodevelopmental disorders. Lancet Psychiatry 4, 339–346. doi: 10.1016/S2215-0366(16)30376-5
Thomas, R., Sanders, S., Doust, J., Beller, E., and Glasziou, P. (2015). Prevalence of attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. Pediatrics 135, e994–e1001. doi: 10.1542/peds.2014-3482
Tyler, J. (1994). Equine psychotherapy - worth more than just a horse laugh. Women Ther. 15, 139–146. doi: 10.1300/J015v15n03_11
van der Niet, A., Smith, J., Oosterlaan, J., Scherder, E., Hartman, E., and Visscher, C. (2016). Effects of a cognitively demanding aerobic intervention during recess on children’s physical fitness and executive functioning. Pediatr. Exerc. Sci. 28, 64–70. doi: 10.1123/pes.2015-0084
Vats, D., Flegal, J., and Jones, G. (2019). Multivariate output analysis for Markov chain Monte Carlo. Biometrika 106, 321–337. doi: 10.1093/biomet/asz002
Vivas, J., Arias, P., and Cudeiro, J. (2011). Aquatic therapy versus conventional land-based therapy for Parkinson’s disease: An open-label pilot study. Arch. Phys. Med. Rehabil. 92, 1202–1210. doi: 10.1016/j.apmr.2011.03.017
Welsch, L., Alliott, O., Kelly, P., Fawkner, S., Booth, J., and Niven, A. (2021). The effect of physical activity interventions on executive functions in children with ADHD: A systematic review and meta-analysis. Ment. Health Phys. Act. 20:100379. doi: 10.1016/j.mhpa.2020.100379
Wollesen, B., Wildbredt, A., van Schooten, K., Lim, M., and Delbaere, K. (2020). The effects of cognitive-motor training interventions on executive functions in older people: A systematic review and meta-analysis. Eur. Rev. Aging Phys. Act. 17:9. doi: 10.1186/s11556-020-00240-y
Yazd, S., Ayatizadeh, F., Dehghan, F., Machado, S., and Wegner, M. (2015). Comparing the effects of drug therapy, perceptual motor training, and both combined on the motor skills of school-aged attention deficit hyperactivity disorder children. CNS Neurol Disord. Drug Targets 14, 1283–1291. doi: 10.2174/1871527315666151111123501
Yu, C., Chueh, T., Hsieh, S., Tsai, Y., Hung, C., Huang, C., et al. (2019). Motor competence moderates relationship between moderate to vigorous physical activity and resting EEG in children with ADHD. Ment. Health Phys. Act. 17:100302. doi: 10.1016/j.mhpa.2019.100302
Zang, Y. (2019). Impact of physical exercise on children with attention deficit hyperactivity disorders: Evidence through a meta-analysis. Medicine 98:e17980. doi: 10.1097/MD.0000000000017980
Keywords: physical activity, children, ADHD, neurodevelopmental disorders, network meta-analysis
Citation: Li D, Wang D, Cui W, Yan J, Zang W and Li C (2023) Effects of different physical activity interventions on children with attention-deficit/hyperactivity disorder: A network meta-analysis of randomized controlled trials. Front. Neurosci. 17:1139263. doi: 10.3389/fnins.2023.1139263
Received: 06 January 2023; Accepted: 17 February 2023;
Published: 20 March 2023.
Edited by:
Zhe-an Shen, Xinjiang Institute of Technology, ChinaReviewed by:
Wan-Chun Su, National Institutes of Health (NIH), United StatesXiaofang Wang, Zhejiang University School of Medicine, China
Miriam Kessi, Xiangya Hospital, Central South University, China
Copyright © 2023 Li, Wang, Cui, Yan, Zang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chenmu Li, NTEyMjlAZ3pzcG9ydC5lZHUuY24=
 Dong Li
Dong Li Deng Wang2
Deng Wang2 Wenlai Cui
Wenlai Cui