- 1Department of Epidemiology, Dalla Lana School of Public Health, University of Toronto, Toronto, ON, Canada
- 2Department of Pediatrics, Yale School of Medicine, New Haven, CT, United States
- 3Child Study Center, Yale School of Medicine, New Haven, CT, United States
- 4Division of Pediatric Neurology, Department of Neurology, University of Virginia Medical Center, Charlottesville, VA, United States
- 5Department of Physical Therapy, Tufts University, Medford, MA, United States
- 6Department of Neurology, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States
- 7Department of Neurology, New York-Presbyterian NYP/Columbia University Irving Medical Center, New York, NY, United States
- 8Connecticut Chapter, National Multiple Sclerosis Society, Hartford, CT, United States
- 9Department of Neurology, Yale School of Medicine, New Haven, CT, United States
- 10Trinity Health of New England, Hartford, CT, United States
- 11Department of Orthopedics and Rehabilitation, Yale School of Medicine, New Haven, CT, United States
- 12Yale New Haven Health Old Saybrook Medical Center, Old Saybrook Medical Center, New Haven, CT, United States
- 13Yale MS Center, North Haven, CT, United States
- 14Division of Pain & Palliative Medicine, Connecticut Children’s Medical Center, Hartford, CT, United States
- 15Department of Pediatrics, University of Connecticut School of Medicine, Farmington, CT, United States
- 16Department of Paediatrics, Temerty Faculty of Medicine, University of Toronto, Toronto, ON, Canada
- 17Division of Neuroscience and Mental Health, Department of Paediatrics (Neurology), Hospital for Sick Children, SickKids Research Institute, Toronto, ON, Canada
Introduction: Pain in multiple sclerosis (MS) is common, but literature on pain in children with MS remains scarce. Pain has physical, psychological, and social implications in MS, and both comprehensive assessment and interdisciplinary management approaches are needed. We sought to develop an interdisciplinary interim guideline for the assessment and management of pain in children with MS.
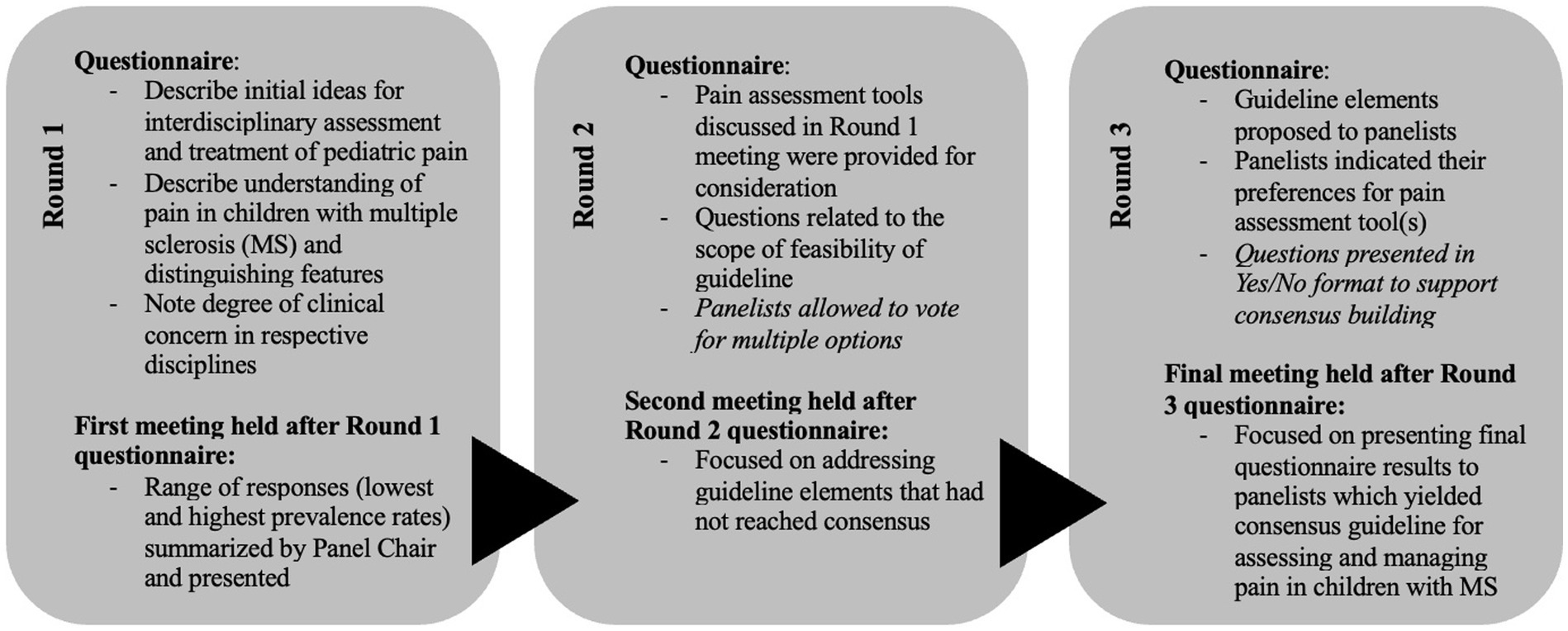
Methods and materials: We convened a modified Delphi panel composed of 13 experts in pediatric and adult MS neurology, physiotherapy, pain, patient lived-experience, advanced practice nursing, psychology, physiatry, and MS research. A survey was sent to panelists for anonymous completion. The panel discussed survey themes extracted by the panel chair. The process was repeated twice.
Results: Thirteen assessment and treatment recommendations were produced regarding pain in children with MS.
Discussion: Future studies will assess implementation of these pain assessment and treatment guidelines in the clinical setting.
1. Introduction
Multiple sclerosis (MS) is an autoimmune disease associated with demyelination, neurodegeneration, and chronic inflammation of the central nervous system (Vargas-Lowy and Chitnis, 2012; Filippi et al., 2016; Brenton et al., 2020). While most often diagnosed in adulthood, approximately 2–10% of individuals with MS experience their first clinical symptom(s) before age 18 (Vargas-Lowy and Chitnis, 2012; Jancic et al., 2016; Narula, 2016; Nikolić et al., 2020).
The reported prevalence of pain in people with MS ranges from 29 and 86% (Jancic et al., 2016; Urits et al., 2019; Yilmazer et al., 2020). Several types of pain have been observed in people with MS. Among these, neuropathic pain is the most commonly reported, occurring in as many as 86% of patients (Urits et al., 2019; Yilmazer et al., 2020). Generalized back pain, tonic spasms or spasticity, L’Hermitte’s symptom, visceral pain, and trigeminal neuralgia are other types of pain that are also observed in adults with MS (Ferraro et al., 2017; Aboud and Schuster, 2019; Yilmazer et al., 2020). Similar pain presentations are also observed in children (Wang and Greenberg, 2018). The wide range of pain types and their varying presentations (Wang et al., 2017; Bosma et al., 2018; Urits et al., 2019) may make the assessment and management of pain challenging. Pain, however, affects the day to day lives of patients with MS. For example, pain flares reported in adults (Aboud and Schuster, 2019) are strongly correlated with quality of life (QoL) to a greater extent in people with MS than in people with other neurological conditions (Ferraro et al., 2017; Marck et al., 2017; Yilmazer et al., 2020).
Given the burden of pain in MS, comprehensive recommendations for children with MS are needed (Wang and Greenberg, 2018). Herein, we propose an interim guideline for pain assessment in children with MS based on the results of a modified Delphi process.
2. Materials and methods
2.1. Study design
We conducted a modified Delphi study to develop an interim guideline for the assessment and management of pain in children with MS. Our approach is modified because it included face-to-face meetings which were not included in the original Delphi methods (Dalkey and Helmer-Hirschberg, 1962). Measuring consensus expert opinion through Delphi and modified Delphi processes are models for establishing guidelines that has been applied for other conditions affecting children such as new onset refractory status epilepticus (NORSE), febrile infection related epilepsy syndrome (FIRES), and anti-NMDA receptor encephalitis (Hirsch et al., 2018; Nosadini et al., 2021; Wickström et al., 2022). It is especially useful for conditions for which there is limited research, such as pain assessment and management among children with MS (Wickström et al., 2022). We assessed expert opinions regarding pain metrics (e.g., pain frequency, pain intensity, pain sensation), pain assessment tools, intervention considerations, and application of interdisciplinary approaches to care. Consistent with other Delphi studies, consensus agreement was defined as at least 75% agreement (Diamond et al., 2014).
2.2. Ethics statement
The project was deemed exempt from review (#2000027448) by the Yale University Institutional Review Board (IRB).
2.3. Expert panel
The principal investigator (NM) and Delphi panel chair (CS) identified a sample of experts in the field of MS and/or pain research. Investigators recruited interdisciplinary representatives with the following expertise: child MS neurology, adult MS neurology, physiotherapy, pediatric pain medicine, patient lived-experience, nursing, social work and pediatric psychology, physiatry and rehabilitation medicine, and MS research. Thirteen experts participated in each round of this Delphi study. Informed consent was provided through the experts’ responses confirming participation via email. A social worker was replaced by a pediatric psychologist after Round 1 due to scheduling conflicts. Many panelists provided expertise in two areas (e.g., pediatric neurology and research). Six panelists work exclusively in a pediatric context.
2.4. Procedure
There were three rounds of Delphi surveys and panel discussions. For each round, a series of statements were sent to the panelists via electronic survey using REDCap which were followed by discussion rounds with the panel. The responses were anonymized except for questions asking panelists to describe their expert roles. All participants responded and were able to meet to discuss guidelines at each round. The number of respondents (N), the level of agreement (LA) and level of disagreement (LD) for the final recommendations are reported. A summary of the matters discussed in each round can be found in Figure 1.
3. Results
The Delphi panelists concluded that assessment of pain in children with MS involves three major considerations: (1) Children with MS report a variety of pain types, including neuropathic pain, spasticity-related pain, and various forms of headaches, (2) Pain symptoms in children with MS can vary widely with periods of remission followed by flares that impact quality of life and activities of daily life, and (3) Differences exist between children and adults in their ability to accept, manage, and articulate their pain’s characteristics and functional impact. Panelists estimated that recurrent, MS-related occurred in 25–50% of children in their own clinical practices. A summary of the assessment and treatment guidelines is in Table 1.
3.1. Assessment guidelines
3.1.1. Child-friendly assessment of pain locations, sensation, and intensity
3.1.1.1. Recommendations
1. Patients should be asked to describe their pain intensity (e.g., mild, moderate, severe), and location(s) in their own words whenever possible (N = 13; LA = 100%; LD = 0%)
2. A list of adjectives can be provided such as through The Adolescent Pediatric Pain Tool (APPT) to describe pain sensation and intensity (N = 13; LA = 100%; LD = 0%)
3. A visual pain scale, such as the Faces Pain Scale, can be provided to describe their pain intensity (N = 13; LA = 100%; LD = 0%)
4. Body map diagrams can be provided to describe pain location(s) (N = 13; LA = 100%; LD = 0%)
The panelists agreed that asking patients to describe their pain in their own words was preferred whenever possible. Tools such as The Adolescent Pediatric Pain Tool (APPT) (ages 8–17 years old) (Jacob et al., 2014) may help patients and providers describe pain in a developmentally appropriate manner (e.g., instead of just listing “neuropathic pain,” list words such as, “burning”). Pain intensity descriptors such as, “typical” “worst” and “best” are helpful to frame current symptoms in the context of the patient’s typical experience. The Faces Pain Scale-Revised (FSP-R) (ages 4-17 years old), is a helpful option for younger children or children with learning disabilities (Hicks et al., 2001; Tsze et al., 2013). Panelists agreed that patients could show where their pain is located on a body map diagram (von Baeyer et al., 2011).
3.1.2. Functionality and activities of daily living
3.1.2.1. Recommendation
The impact of pain on activities of daily life (ADLs) can be assessed by the Functional Disability Index (FDI) (ages 8-18 years old) (Daffin et al., 2020); Patient Reported Outcomes Measurement Information System (PROMIS) Pediatric Pain Interference Short Form (ages 8–17 years old; parent proxy form available for children ages 5–17 years old) (Varni et al., 2010; PROMIS, 2023); and/or the Child Activity Limitations Interview (CALI-21) (ages 8–18 years old) (Palermo et al., 2008) (N = 13; LA = 100%; LD = 0%).
Considering the lack of a validated instrument for the pediatric MS setting and the variation of instrument preference amongst panelists, the panelists agreed all three instruments are viable options for assessing functionality and ADLs.
3.1.3. Psychosocial
3.1.3.1. Recommendation
Mental health screening should be completed, followed by appropriate referral for further psychological assessment, general psychotherapy, and/or health behavior intervention (N = 13; LA = 100%; LD = 0%).
Mental health is an important consideration in any comprehensive guideline for pain assessment and management, as pain is a biopsychosocial experience. There is a bidirectional relationship between chronic pain and mental health. A thorough assessment of school attendance, school-based supports, sleep quality and quantity, and functional disability is important. The panel recommended that psychological and psychosocial wellness should be assessed at the initial visit and follow-up visits, with referrals as appropriate.
3.1.4. Headache
3.1.4.1. Recommendation
Patients’ headache experience should be assessed, and a referral to a headache specialist should be made when needed (N = 13; LA = 92.3%; LD = 7.7%).
Children with MS presenting with headaches require a thorough headache evaluation to determine whether it is a primary headache disorder, secondary headache due to MS, or result of underlying non-MS pathology. Headache merits a separate guideline, given its complexities. The panelists agreed that clinicians should ask patients about headaches and can make a referral to a headache specialist if indicated.
3.1.5. Frequency of pain assessment
3.1.5.1. Recommendations
1. Pain will be assessed during all initial MS consultations (N = 13; LA = 100%; LD = 0%)
2. Pain will be assessed in follow-up visits as needed (N = 13; LA = 100%; LD = 0%)
Panelists agreed that pain should be assessed in all children with MS as part of the initial clinical assessment. Pain assessment questionnaires could be sent to patients ahead of time for electronic completion at home to promote efficiency of pain assessment in visit.
3.2. Treatment guidelines
3.2.1. Holistic care team
3.2.1.1. Recommendation
The treatment of pain in children with MS requires an interdisciplinary approach (N = 13; PA = 100%; PD = 0%).
Interdisciplinary care is essential for pain management. An interdisciplinary team may involve physicians, physiotherapists, nurses, psychologists, and social workers. Patients are important decision makers and members of their own pain treatment team.
3.2.2. Pharmaceutical
3.2.2.1. Recommendations
1. In general, over-the-counter pharmaceuticals should be tried before introducing prescription medications (N = 13; LA = 100%; LD = 0%)
2. Wherever possible, therapeutic agents should be targeted for the patient’s specific type of pain (N = 13; LA = 100%; LD = 0%)
Panelists agreed that, whenever possible, providers should first recommend over-the-counter analgesics, such as acetaminophen or ibuprofen. Prescription agents that target specific pain symptoms including anticonvulsants (e.g., gabapentin), serotonin and norepinephrine reuptake inhibitor (e.g., duloxetine), or tricyclic antidepressants (e.g., amitriptyline) should be employed if over-the-counter agents are ineffective or not indicated for the pain type (e.g., neuropathic pain).
3.2.3. Psychosocial
3.2.3.1. Recommendation
Behavior pain treatments should be recommended and for all patients with pain at baseline and continued as indicated (N = 13; LA = 100%; LD = 0%).
Adopting a biopsychosocial approach to pain management has been demonstrated to lead to improved outcomes among patients with chronic pain (Eucker et al., 2022). All panelists agreed that incorporating non-pharmaceutical treatments into a balanced treatment plan should be encouraged. These can include cognitive behavioral therapy for pain, biofeedback-assisted relaxation training, guided imagery, and mindfulness.
4. Discussion
Herein, we propose interim guidelines for the assessment and treatment of pain in children with MS which we developed using a modified Delphi panel. There are different types of pain in MS, which may fluctuate due to the progressive and relapsing nature of the disease (Jeong et al., 2019). Repeated, thorough assessments may allow for early detection and appropriate pain management intervention for children with MS which has been observed in adults with MS being assessed for neuropathic pain (Ferraro et al., 2017).
Pain treatment should be specific to the pain presentation and may include pharmaceutical and non-pharmaceutical. In a study in adults, approximately 15% of people with MS were on a pharmaceutical regimen for chronic pain (Ferraro et al., 2017). Gabapentin (33.3%), pregabalin (28.0%), duloxetine (21.0%) and amitriptyline (16.0%) were the most prescribed medications (Ferraro et al., 2017). Another 5.6% of patients had been prescribed cannabinoid-based medication for spasticity, 42.1% were taking non-steroidal anti-inflammatory drugs as treatment, and 3.1% patients were prescribed and utilized opioid medication (Ferraro et al., 2017). Slightly more than 10% of patients were prescribed greater than one medication for their pain symptoms (Ferraro et al., 2017). The optimal treatment of different pain types in children warrants further study.
Pain can interfere with physical, social, and psychological domains of functioning, potentially to a greater extent than other neurological disorders, which highlights the need for an interdisciplinary approach (Drulovic et al., 2015; Huang et al., 2017; Yilmazer et al., 2020). One study found that pain interference is associated with changes in the pain-processing connectome as detected by reduced beta power on magnetoencephalography (MCG), particularly in the thalamus and posterior insula, suggesting a potential biological mechanism for the pain experience in MS (Kim et al., 2018). People with MS experience greater pain-related interference in daily life the longer they have the disease (Yilmazer et al., 2020), highlighting the importance of recognizing and treating pain early in pediatric MS to support good quality of life. Several psychosocial treatment modalities have been studied in adult MS patients and other chronic pain populations which merit further study in the pediatric MS population. These include cognitive behavioral therapy (Ostojic et al., 2021), biofeedback-assisted relaxation training (Ostojic et al., 2021), and mindfulness (Senders et al., 2018).
Our study has some limitations. First, all panelists were from academic institutions in North America. This could affect generalizability of the guideline across cultures. Of note, the recommended instruments are available in an array of languages to allow for broad use. Further, the recommended instruments have not been validated in this population. However, the instruments have been validated in several pediatric populations with similar risk factors for pain as children with MS, including abdominal pain, musculoskeletal pain syndromes, back pain, headache, chronic kidney disease-related pain, Crohn’s disease-related pain, amongst others (Palermo et al., 2008; Kashikar-Zuck et al., 2011; Forrest et al., 2020). Lastly, the panel did not include a pediatric MS patient, though we did include an adult patient.
5. Conclusion
Pain in children with MS may negatively impact quality of life. Therefore, these proposed guidelines are essential for identifying, assessing, and treating pain in this population. Chronic pain is multifaceted, making interdisciplinary care critical. Future studies could assess the acceptability of the proposed guidelines amongst children with MS, the feasibility of implementing the guidelines in the clinical setting, as well as the validation of the proposed assessment tools in childhood MS. Other mental health aspects of pain are important to evaluate, but beyond the scope of the present study. Future guidelines should provide recommendations for psychological and social assessment, as well as a comprehensive screening battery involving pain, psychological, and social assessments.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
CS and NM designed the study. CS, AV, and NM drafted the initial manuscript. All authors reviewed the manuscript for important intellectual content and contributed edits.
Funding
This work was supported, in part, by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health award number K23NS101099. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Makhani is also supported by a Harry Weaver Neuroscience Scholar Award from the National MS Society and a Child Health Research Award from the Charles H. Hood Foundation.
Conflict of interest
Makhani is a consultant for the Institute for Advanced Clinical Trials for Children.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aboud, T., and Schuster, N. M. (2019). Pain management in multiple sclerosis: a review of available treatment options. Curr. Treat. Options Neurol. 21:62. doi: 10.1007/s11940-019-0601-2
Bosma, R. L., Kim, J. A., Cheng, J. C., Rogachov, A., Hemington, K. S., Osborne, N. R., et al. (2018). Dynamic pain connectome functional connectivity and oscillations reflect multiple sclerosis pain. Pain 159, 2267–2276. doi: 10.1097/j.pain.0000000000001332
Brenton, J. N., Kammeyer, R., Gluck, L., Schreiner, T., and Makhani, N. (2020). Multiple sclerosis in children: current and emerging concepts. Semin. Neurol. 40, 192–200. doi: 10.1055/s-0040-1703000
Daffin, M., Gibler, R. C., and Kashikar-Zuck, S. (2020). Measures of juvenile fibromyalgia. Arthritis Care Res (Hoboken). 72, 171–182. doi: 10.1002/acr.24197
Dalkey, NC, and Helmer-Hirschberg, O. (1962). An experimental application of the Delphi method to the use of experts. RAND Corporation. Available at: https://www.rand.org/pubs/research_memoranda/RM727z1.html.
Diamond, I. R., Grant, R. C., Feldman, B. M., Pencharz, P. B., Ling, S. C., Moore, A. M., et al. (2014). Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J. Clin. Epidemiol. 67, 401–409. doi: 10.1016/j.jclinepi.2013.12.002
Drulovic, J., Basic-Kes, V., Grgic, S., Vojinovic, S., Dincic, E., Toncev, G., et al. (2015). The prevalence of pain in adults with multiple sclerosis: a multicenter cross-sectional survey. Pain Med. 16, 1597–1602. doi: 10.1111/pme.12731
Eucker, S. A., Knisely, M. R., and Simon, C. (2022). Nonopioid treatments for chronic pain—integrating multimodal biopsychosocial approaches to pain management. JAMA Netw. Open 5:e2216482. doi: 10.1001/jamanetworkopen.2022.16482
Ferraro, D., Plantone, D., Morselli, F., Dallari, G., Simone, A. M., Vitetta, F., et al. (2017). Systematic assessment and characterization of chronic pain in multiple sclerosis patients. Neurol. Sci. 39, 445–453. doi: 10.1007/s10072-017-3217-x
Filippi, M., Rocca, M. A., Ciccarelli, O., De Stefano, N., Evangelou, N., Kappos, L., et al. (2016). MRI criteria for the diagnosis of multiple sclerosis: MAGNIMS consensus guidelines. Lancet Neurol. 15, 292–303. doi: 10.1016/s1474-4422(15)00393-2
Forrest, C. B., Forrest, K. D., Clegg, J. L., de la Motte, A., Amaral, S., Grossman, A. B., et al. (2020). Establishing the content validity of promis pediatric pain interference, fatigue, sleep disturbance, and sleep-related impairment measures in children with chronic kidney disease and Crohn’s disease. J. Patient Reported Outcomes 4:11. doi: 10.1186/s41687-020-0178-2
Hicks, C. L., von Baeyer, C. L., Spafford, P. A., van Korlaar, I., and Goodenough, B. (2001). The faces pain scale – revised: toward a common metric in pediatric pain measurement. Pain 93, 173–183. doi: 10.1016/s0304-3959(01)00314-1
Hirsch, L. J., Gaspard, N., van Baalen, A., Nabbout, R., Demeret, S., Loddenkemper, T., et al. (2018). Proposed consensus definitions for new-onset refractory status epilepticus (norse), febrile infection-related epilepsy syndrome (fires), and related conditions. Epilepsia 59, 739–744. doi: 10.1111/epi.14016
Huang, W.-J., Chen, W.-W., and Zhang, X. (2017). Multiple sclerosis: pathology, diagnosis and treatments. Exp. Ther. Med. 13, 3163–3166. doi: 10.3892/etm.2017.4410
Jacob, E., Mack, A. K., Savedra, M., Van Cleve, L., and Wilkie, D. J. (2014). Adolescent pediatric pain tool for multidimensional measurement of pain in children and adolescents. Pain Manag. Nurs. 15, 694–706. doi: 10.1016/j.pmn.2013.03.002
Jancic, J., Nikolic, B., Ivancevic, N., Djuric, V., Zaletel, I., Stevanovic, D., et al. (2016). Multiple sclerosis in pediatrics: current concepts and treatment options. Neurol. Therapy 5, 131–143. doi: 10.1007/s40120-016-0052-6
Jeong, A., Oleske, D. M., and Holman, J. (2019). Epidemiology of pediatric-onset multiple sclerosis: a systematic review of the literature. J. Child. Neurol 34, 705–712. doi: 10.1177/0883073819845827
Kashikar-Zuck, S., Flowers, S. R., Claar, R. L., Guite, J. W., Logan, D. E., Lynch-Jordan, A. M., et al. (2011). Clinical utility and validity of the functional disability inventory among a multicenter sample of youth with chronic pain. Pain 152, 1600–1607. doi: 10.1016/j.pain.2011.02.050
Kim, J. A., Bosma, R. L., Hemington, K. S., Rogachov, A., Osborne, N. R., Cheng, J. C., et al. (2018). Neuropathic pain and pain interference are linked to alpha-band slowing and reduced beta-band magnetoencephalography activity within the dynamic pain connectome in patients with multiple sclerosis. Pain 160, 187–197. doi: 10.1097/j.pain.0000000000001391
Marck, C. H., De Livera, A. M., Weiland, T. J., Jelinek, P. L., Neate, S. L., Brown, C. R., et al. (2017). Pain in people with multiple sclerosis: associations with modifiable lifestyle factors, fatigue, depression, anxiety, and mental health quality of life. Front. Neurol. 8:8. doi: 10.3389/fneur.2017.00461
Narula, S. (2016). Pediatric multiple sclerosis: updates in epidemiology, clinical features and management. Neurodegener. Dis. Manag. 6, 3–7. doi: 10.2217/nmt-2016-0046
Nikolić, B., Ivančević, N., Zaletel, I., Rovčanin, B., Samardžić, J., and Jančić, J. (2020). Characteristics of pediatric multiple sclerosis: a tertiary referral center study. PLoS One 15:e0243031. doi: 10.1371/journal.pone.0243031
Nosadini, M., Thomas, T., Eyre, M., Anlar, B., Armangue, T., Benseler, S. M., et al. (2021). International consensus recommendations for the treatment of pediatric NMDAR antibody encephalitis. Neurol Neuroimmunol Neuroinflamm 8:e1052. doi: 10.1212/NXI.0000000000001052
Ostojic, K., Sharp, N., Paget, S., Khut, G., and Morrow, A. (2021). BrightHearts: a pilot study of biofeedback assisted relaxation training for the Management of Chronic Pain in children with cerebral palsy. Paediatric Neonatal Pain. 4, 34–43. doi: 10.1002/pne2.12062
Palermo, T. M., Lewandowski, A. S., Long, A. C., and Burant, C. J. (2008). Validation of a self-report questionnaire version of the child activity limitations interview (CALI): the CALI-21. Pain 139, 644–652. doi: 10.1016/j.pain.2008.06.022
PROMIS. (2023). “HealthMeasures.” List of Parent Proxy Measures, 3 May 2023. Available at: www.healthmeasures.net/explore-measurement-systems/promis/intro-to-promis/list-of-parent-proxy-measures
Senders, A., Borgatti, A., Hanes, D., and Shinto, L. (2018). Association between pain and mindfulness in multiple sclerosis: a cross-sectional survey. Int J MS Care 20:12018, 28–34. doi: 10.7224/1537-2073.2016-076
Tsze, D. S., von Baeyer, C. L., Bulloch, B., and Dayan, P. S. (2013). Validation of self-report pain scales in children. Pediatrics 132, e971–e979. doi: 10.1542/peds.2013-1509
Urits, I., Adamian, L., Fiocchi, J., Hoyt, D., Ernst, C., Kaye, A. D., et al. (2019). Advances in the understanding and management of chronic pain in multiple sclerosis: a comprehensive review. Curr. Pain Headache Rep. 23, 1–11. doi: 10.1007/s11916-019-0800-2
Vargas-Lowy, D., and Chitnis, T. (2012). Pathogenesis of pediatric multiple sclerosis. J. Child Neurol. 27, 1394–1407. doi: 10.1177/0883073812456084
Varni, J. W., Stucky, B. D., Thissen, D., DeWitt, E. M., Irwin, D. E., Lai, J. S., et al. (2010). PROMIS pediatric pain interference scale: an item response theory analysis of the pediatric pain item bank. J. Pain 11, 1109–1119. doi: 10.1016/j.jpain.2010.02.005
von Baeyer, C. L., Lin, V., Seidman, L. C., Tsao, J. C., and Zeltzer, L. K. (2011). Pain charts (body maps or manikins) in assessment of the location of pediatric pain. Pain Manag. 1, 61–68. doi: 10.2217/pmt.10.2
Wang, I.-C., Chung, C.-Y., Liao, F., Chen, C.-C., and Lee, C.-H. (2017). Peripheral sensory neuron injury contributes to neuropathic pain in experimental autoimmune encephalomyelitis. Sci. Rep. 7, 1–14. doi: 10.1038/srep42304
Wang, C. X., and Greenberg, B. M. (2018). Pediatric multiple sclerosis: from recognition to practical clinical management. Neurol. Clin. 36, 135–149. doi: 10.1016/j.ncl.2017.08.005
Wickström, R., Taraschenko, O., Dilena, R., Payne, E. T., Specchio, N., Nabbout, R., et al. (2022). International consensus recommendations for management of new onset refractory status epilepticus (Norse) including febrile infection-related epilepsy syndrome (fires): summary and clinical tools. Epilepsia 63, 2827–2839. doi: 10.1111/epi.17391
Keywords: pain, pediatrics, multiple sclerosis, clinical guideline, Delphi panel
Citation: Stratton C, Vassilopoulos A, Brenton JN, Potter K, Vargas W, Rumm H, Bartels A, Bailey M, Odonkor C, Stoll S, Zempsky EWT, Yeh EA and Makhani N (2023) Interim guidelines for the assessment and treatment of pain in children with multiple sclerosis. Front. Neurosci. 17:1235945. doi: 10.3389/fnins.2023.1235945
Edited by:
Filipe Palavra, University of Coimbra, PortugalReviewed by:
Mafalda Sampaio, Centro Hospitalar Universitário de São João (CHUSJ), PortugalTeresa Painho, Hospital de Dona Estefânia, Portugal
Copyright © 2023 Stratton, Vassilopoulos, Brenton, Potter, Vargas, Rumm, Bartels, Bailey, Odonkor, Stoll, Zempsky, Yeh and Makhani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Catherine Stratton, Y2F0aGVyaW5lLnN0cmF0dG9uQG1haWwudXRvcm9udG8uY2E=; Naila Makhani, bmFpbGEubWFraGFuaUB5YWxlLmVkdQ==
 Catherine Stratton
Catherine Stratton Areti Vassilopoulos
Areti Vassilopoulos J. Nicholas Brenton
J. Nicholas Brenton Kirsten Potter5
Kirsten Potter5 Charles Odonkor
Charles Odonkor E. William T. Zempsky
E. William T. Zempsky E. Ann Yeh
E. Ann Yeh Naila Makhani
Naila Makhani