- 1Department of Anesthesiology, Third Hospital of Shanxi Medical University, Shanxi Bethune Hospital, Shanxi Academy of Medical Sciences, Tongji Shanxi Hospital, Taiyuan, China
- 2Department of Anesthesiology, Shanxi Medical University, Taiyuan, China
- 3Department of Nephrology, Third Hospital of Shanxi Medical University, Shanxi Bethune Hospital, Shanxi Academy of Medical Sciences, Tongji Shanxi Hospital, Taiyuan, China
Uremia is the advanced stage of chronic kidney disease (CKD), characterized by the accumulation of metabolic waste products in the blood as a result of the kidneys' inability to meet the body's metabolic demands. Patients with uremia frequently experience a range of complications, including renal anemia, osteoporosis, and cardiovascular disease, all of which significantly impair their quality of life. Chronic kidney disease-associated pruritus (CKD-aP) is a common comorbidity in uremic patients, particularly among those undergoing hemodialysis, with prevalence rates ranging from 10 to 77%. This case report enrolled three patients diagnosed with chronic kidney disease-associated pruritus (CKD-ap) who underwent ultrasound-guided sympathetic nerve blockade procedures. The results demonstrated significant reductions in pruritus intensity concurrent with measurable enhancements in sleep quality and daily functioning.
1 Introduction
Uremia is the advanced stage of chronic kidney disease (CKD), characterized by the accumulation of metabolic waste products in the blood as a result of the kidneys' inability to meet the body's metabolic demands (Levey et al., 2003). Patients with uremia frequently experience a range of complications, including renal anemia, osteoporosis, and cardiovascular disease, all of which significantly impair their quality of life (Joseph et al., 2020; Sulková et al., 2021; Coronado Daza et al., 2015). Chronic kidney disease-associated pruritus (CKD-aP) is a common comorbidity in uremic patients, particularly among those undergoing hemodialysis, with prevalence rates ranging from 10 to 77% (Makar et al., 2021). Research has indicated that the deposition of metabolic waste products, neurological dysfunction, microinflammation, and immune system imbalance are closely associated with the development of CKD-aP (Kimmel et al., 2006; Agarwal et al., 2021).
The role of sympathetic nerves has garnered significant attention in the investigation of the pathogenesis of CKD-aP. Sympathetic nerves are a critical component of the autonomic nervous system and are involved in the regulation of both acute and chronic pain through mechanisms such as neurological and endocrine interactions, as well as modulation of nutrition and immunity (Doroshenko et al., 2024). It has been proposed that abnormal sympathetic nerve activity is closely linked to pruritus, particularly in the context of neuropathic itch, with dysregulation of this activity potentially contributing to the intensification of itch, thereby exacerbating cutaneous symptoms (Tong et al., 2022).
For CKD-aP, optimal treatment remains unclear (Simonsen et al., 2017). Clinically, gabapentin and naltrexone are the most commonly prescribed medications for alleviating CKD-aP. However, these drugs frequently cause adverse effects such as dizziness, leading to poor patient compliance. Alternative therapies, including phototherapy and acupuncture, often require prolonged treatment durations and exhibit slow onset of efficacy, which can impose significant financial burdens on patients (Siemens et al., 2014; Mettang and Kremer, 2015). Clinicians typically utilize either single or combination therapies, considering the severity of symptoms to achieve the most effective therapeutic outcomes. Sympathetic nerve block, a well-established treatment, has been proven safe and effective in managing conditions such as complex regional pain syndrome, post-traumatic stress disorder, and cardiac arrhythmias (O'Connell et al., 2016; Lipov and Ritchie, 2015; Witt et al., 2017). We hypothesized that sympathetic blockade might alleviate pruritus by suppressing abnormal sympathetic nerve activity in CKD-aP patients, thereby improving their quality of life. To test this hypothesis, we recruited three uremic patients suffering from pruritus, with the expectation that their responses could provide new insights into the treatment of CKD-aP.
2 Case report
2.1 Case 1
The patient was a 70-year-old female with chronic renal failure in the uremic stage, complicated by grade 2 hypertension, type 2 diabetes mellitus, severe anemia, and several other underlying conditions. She was admitted to our hospital for hemodialysis due to progressively elevated serum creatinine, electrolyte disturbances, and acid-base imbalances. During hemodialysis, she experienced episodes of nosebleeds, as well as adverse reactions including nausea, vomiting, and insomnia. Prior to treatment, the patient suffered from persistent pruritus, particularly at night, affecting multiple areas such as the face, trunk, and limbs. Additionally, she often experienced difficulty falling asleep, sleep disturbances, and poor blood pressure control, which required increased doses of antihypertensive medication. When the pruritus symptoms became severe, the patient was administered gabapentin orally for symptomatic management. However, the therapeutic response was unsatisfactory. Prior to undergoing sympathetic nerve block therapy, the patient had discontinued the medication for 2 weeks.
2.2 Case 2
The patient, a 61-year-old male, was in the uremic stage of chronic renal failure, complicated by grade 3 hypertension, type II diabetes mellitus, diabetic nephropathy, renal anemia, renal bone disease, and multiple other comorbidities. In recent years, he had experienced persistent pruritus, generalized fatigue, recurrent bilateral lower extremity edema, intermittent morning nausea, and other symptoms, all of which were accompanied by progressively elevated blood creatinine, hyperkalemia, and repeated peritoneal dialysis treatments. Recent refinement of the peritoneal balance test indicated inadequate dialysis, leading to adjustments in the patient's peritoneal dialysis regimen. Subsequently, venous fistuloplasty was performed, and it was recommended that the patient transition to hemodialysis once the arteriovenous fistula matured. Prior to treatment, the patient exhibited significant pruritus on his back and face, with visible signs of scratching upon examination. The symptoms were exacerbated during dialysis and significantly aggravated by cold, heat, and increased stress. No corresponding symptomatic treatment was administered to the patient for the pruritus symptoms.
2.3 Case 3
The patient is a 70-year-old female who, in 2017, developed generalized edema without an obvious causative factor. Laboratory tests revealed elevated blood creatinine levels, leading to a diagnosis of chronic renal failure. She has since been undergoing regular dialysis treatment and has progressed to the uremic stage. The patient also has a comorbid diagnosis of type II diabetes mellitus. Prior to treatment, she experienced significant pruritus in the limbs and back, which was initially alleviated by hydration agents but became progressively less effective over time. The persistent pruritus severely impacted her sleep quality, leading to mood swings and irritability, which significantly compromised her overall quality of life.
3 Results and discussions
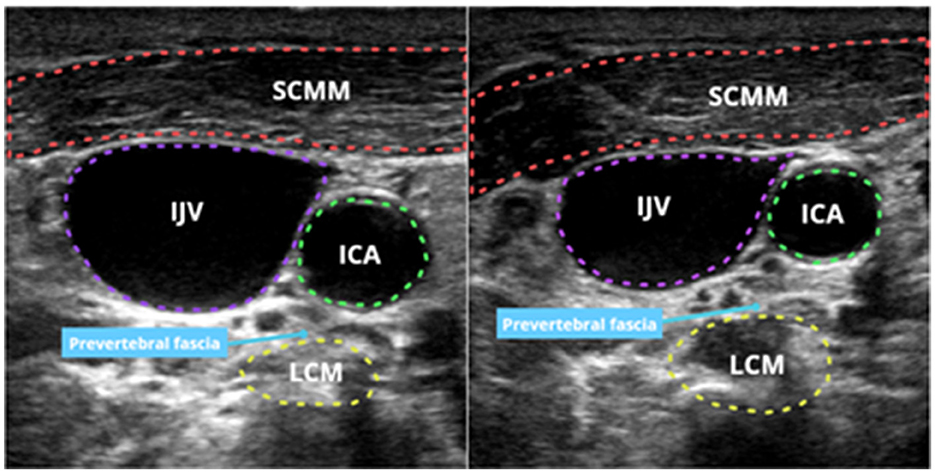
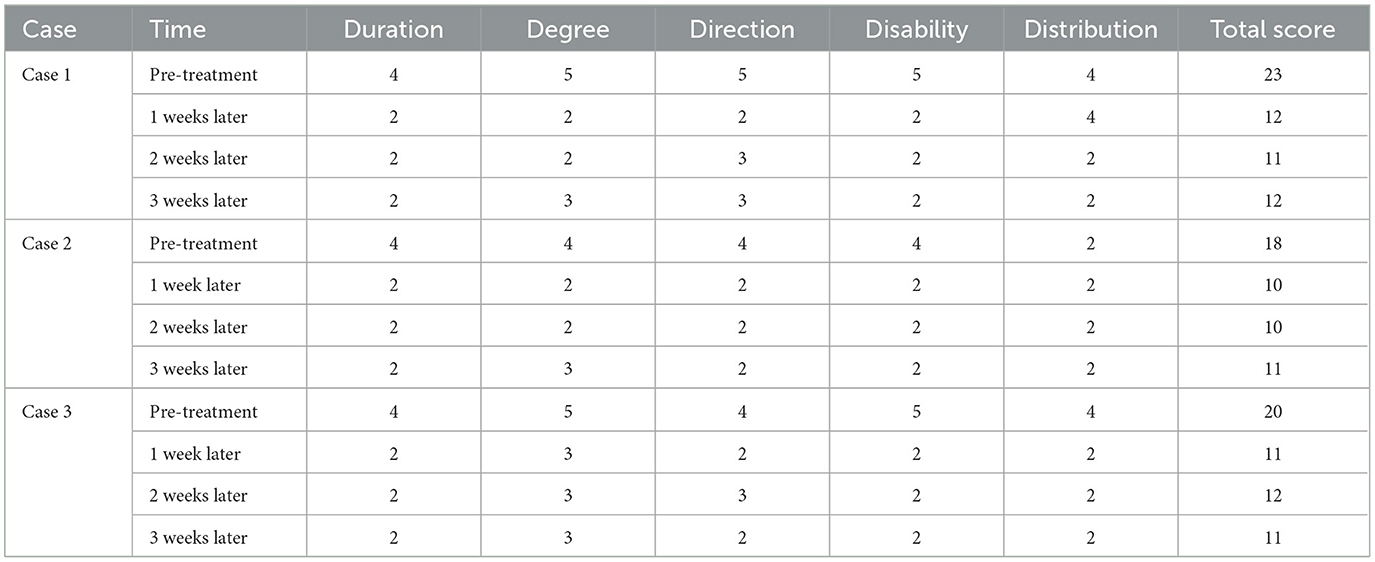
All three patients presented with severe pruritus, which was not observed prior to the diagnosis of CKD. The intensity of their pruritic symptoms worsened with the progression of renal disease, prompting a diagnosis of CKD-aP (Verduzco and Shirazian, 2020). Following full informed consent, we performed a sympathetic nerve block under the guidance of one of our experienced anesthesiologists. The procedure was conducted as follows (Figure 1): under ultrasound guidance, a needle was inserted near the 6th cervical vertebra, targeting the anterior ramus of the transverse process at a depth of 3.0–3.5 cm. After confirming the absence of blood, cerebrospinal fluid, and gas, 5 mL of 0.5% ropivacaine was injected slowly. Successful blockade was indicated by the occurrence of Horner's syndrome postoperatively. Nerve blocks were administered on the contralateral side every other day, with a total of six treatments. Dynamic assessments were conducted before the treatment, after 1 week, after 2 weeks, and after 3 weeks. The patients' pruritus was evaluated using the 5-D Pruritus Scale, assessing itch duration, severity, direction of progression, incapacitation, and distribution, the results are shown in Table 1. There was further supplemented with the Peak Pruritus Numerical Rating Scale and the Twelve-Item Pruritus Scale, the results are presented in the Supplementary material (Elman et al., 2010; Jang et al., 2020). Additionally, the impact of the treatment on sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI; Buysse et al., 1989), with results shown in the following tables and figures. Throughout the treatment and follow-up periods, we closely monitored the patients for adverse effects, such as localized pain and nerve injury. However, among the three participants in this study, only transient Horner's syndrome was observed following the nerve block, with no other adverse effects reported. These findings suggest that this therapeutic approach is associated with a high level of safety.
During the follow-up period, the severity of the patient's symptoms and their impact on quality of life were assessed. The results of the study indicated that after six sessions of sympathetic nerve block treatment, all patients experienced a significant reduction in itch scores and an improvement in sleep quality. These findings suggest that sympathetic nerve block is clinically effective in improving symptoms of CKD-aP.
Sympathetic blockade has been demonstrated to be a safe and effective therapeutic approach, primarily through its mechanism of inhibiting the release of chemical signals associated with various disease states by blocking sympathetic nerve conduction (Baig et al., 2017; Lipov et al., 2017). By disrupting the conduction of sympathetic nerve signals, it effectively reduces the transmission of pain signals to the central nervous system, thereby alleviating pain perception. Moreover, by inhibiting the release of neurotransmitters such as norepinephrine from sympathetic nerve terminals, sympathetic blockade can further reduce pain perception, showing efficacy in conditions like neuropathic pain and cancer pain (Zhang et al., 2022; Lipov et al., 2009). Sympathetic blockade also exerts regulatory effects on the cardiovascular system, including decreasing heart rate, reducing myocardial contractility, and promoting vasodilation, which in turn reduces cardiac workload and alleviates symptoms associated with cardiovascular disorders (King et al., 2007; Wang et al., 2023). Additionally, sympathetic blockade can modulate immune system function by interrupting sympathetic innervation to immune organs, offering therapeutic potential in immune-related conditions such as ulcerative colitis (Lipov et al., 2020). It also has therapeutic applications in managing vasodilatory abnormalities associated with spasms, as well as in alleviating symptoms like hot flashes during menopause (Feigin et al., 2023). Sympathetic nerve block techniques are now widely used in clinical practice. With ultrasound-guided visualization, the safety of this procedure is significantly enhanced.
There is limited experimental evidence to demonstrate the effectiveness of sympathetic nerve block therapy in alleviating pruritus in patients with uremia. Our study may provide new insights into the potential clinical application of this therapy. We hypothesize that its mechanism of action may involve several factors. In patients with uremia, impaired renal function prevents the timely removal of metabolic waste products, leading to the accumulation of substances such as urea, creatinine, and uric acid in the bloodstream. This accumulation not only damages organs such as the liver and kidneys but may also affect both central and peripheral nervous systems, potentially stimulating cutaneous nerve endings and triggering pruritus (Wang et al., 2016). Sympathetic nerve block alleviates pruritus by interrupting sensory signal transmission in nerve endings. Furthermore, immune dysregulation plays a crucial role in CKD-aP, with levels of inflammatory mediators such as histamine, IL-2, and IL-6 being significantly elevated in patients with CKD-aP compared to healthy individuals (Ko et al., 2023). Immune organs are heavily innervated by sympathetic fibers, and sympathetic blockade modulates immune system activity by interrupting sympathetic innervation to these organs, thereby influencing the levels of both pro-inflammatory cytokines (e.g., IL-6, TNF-α) and anti-inflammatory cytokines (e.g., IL-10, TNF-β; Lipov et al., 2020). Immune cells express both α-adrenergic and β-adrenergic receptors, and the expression levels of these receptors vary depending on the cellular state, maturity, or activation status. Studies have demonstrated that adrenergic receptors functionally influence immune cell activities, particularly their migration, activation, and cytokine production (Schiller et al., 2021).
This case report has several limitations that warrant consideration. Notably, the absence of standardized quality-of-life assessment instruments, particularly the SF-36 or EQ-5D scales, may have compromised the objective quantification of the intervention's overall therapeutic efficacy. Future investigations should prioritize the implementation of large-scale, adequately powered, multicenter randomized controlled trials to establish comparative effectiveness between this therapeutic modality and conventional treatment paradigms. Furthermore, extending the follow-up duration to encompass several months or years would facilitate a comprehensive evaluation of the long-term clinical outcomes associated with sympathetic nerve blockade in the management of pruritus symptoms.
In conclusion, sympathetic nerve blockade represents a novel therapeutic strategy that offers a promising approach for the management of CKD-associated pruritus (CKD-ap). Although limited by a small sample size, our preliminary findings demonstrate clinically meaningful improvements in both pruritus severity and sleep quality among treated patients. However, additional experimental research and well-designed clinical trials are required to substantiate the safety and efficacy of this intervention before its widespread clinical application.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethics Review Committee of Shanxi Bethune Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YL: Conceptualization, Investigation, Methodology, Visualization, Writing – original draft. YC: Conceptualization, Data curation, Formal analysis, Writing – original draft. JN: Conceptualization, Data curation, Methodology, Writing – original draft. XH: Data curation, Validation, Writing – original draft. WZ: Conceptualization, Funding acquisition, Supervision, Visualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the scientific research project of Shanxi Provincial Health Commission 253 (#2022068), the basic research general project of Shanxi Provincial Department of Science and Technology (#202203021221245), and China Zhongguancun Precision Medicine Science and Technology Foundation (#Z-2021-002).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnins.2025.1529183/full#supplementary-material
References
Agarwal, P., Garg, V., Karagaiah, P., Szepietowski, J. C., Grabbe, S., Goldust, M., et al. (2021). Chronic kidney disease-associated pruritus. Toxins 13:527. doi: 10.3390/toxins13080527
Baig, S., Moon, J. Y., and Shankar, H. (2017). Review of sympathetic blocks: anatomy, sonoanatomy, evidence, and techniques. Reg. Anesth. Pain Med. 42, 377–391. doi: 10.1097/AAP.0000000000000591
Buysse, D. J., Reynolds, C. F. 3rd, Monk, T. H., Berman, S. R., and Kupfer, D. J. (1989). The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213. doi: 10.1016/0165-1781(89)90047-4
Coronado Daza, J., Martí-Carvajal, A. J., Ariza García, A., Rodelo Ceballos, J., Yomayusa González, N., Páez-Canro, C., et al. (2015). Early vs. delayed erythropoietin for the anaemia of end-stage kidney disease. Cochrane Database Syst. Rev. 2015:Cd011122. doi: 10.1002/14651858.CD011122
Doroshenko, M., Turkot, O., Dua, A., and Horn, D. B. (2024). Sympathetic Nerve Block. Statpearls. Treasure Island (FL) ineligible companies: StatPearls Publishing.
Elman, S., Hynan, L. S., Gabriel, V., and Mayo, M. J. (2010). The 5-D itch scale: a new measure of pruritus. Br. J. Dermatol. 162, 587–593. doi: 10.1111/j.1365-2133.2009.09586.x
Feigin, G., Velasco Figueroa, S., Englesakis, M. F., D'Souza, R., Hoydonckx, Y., Bhatia, A., et al. (2023). Stellate ganglion block for non-pain indications: a scoping review. Pain Med. 24, 775–781. doi: 10.1093/pm/pnad011
Jang, Y. H., Kim, S. M., Eun, D. H., Park, K. D., Park, G. H., Kim, B. S., et al. (2020). Validity and reliability of itch assessment scales for chronic pruritus in adults: a prospective multicenter study. J. Am. Acad. Dermatol. 82, 80–86. doi: 10.1016/j.jaad.2019.06.043
Joseph, M. S., Palardy, M., and Bhave, N. M. (2020). Management of heart failure in patients with end-stage kidney disease on maintenance dialysis: a practical guide. Rev. Cardiovasc. Med. 21, 31–39. doi: 10.31083/j.rcm.2020.01.24
Kimmel, M., Alscher, D. M., Dunst, R., Braun, N., Machleidt, C., Kiefer, T., et al. (2006). The role of micro-inflammation in the pathogenesis of uraemic pruritus in haemodialysis patients. Nephrol. Dial. Transplant. 21, 749–755. doi: 10.1093/ndt/gfi204
King, A. J., Osborn, J. W., and Fink, G. D. (2007). Splanchnic circulation is a critical neural target in angiotensin II salt hypertension in rats. Hypertension 50, 547–556. doi: 10.1161/HYPERTENSIONAHA.107.090696
Ko, M. J., Peng, Y. S., and Wu, H. Y. (2023). Uremic pruritus: pathophysiology, clinical presentation, and treatments. Kidney Res. Clin. Pract. 42, 39–52. doi: 10.23876/j.krcp.21.189
Levey, A. S., Coresh, J., Balk, E., Kausz, A. T., Levin, A., Steffes, M. W., et al. (2003). National kidney foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann. Intern. Med. 139, 137–147. doi: 10.7326/0003-4819-139-2-200307150-00013
Lipov, E., Gluncic, V., Lukić, I. K., and Candido, K. (2020). How does stellate ganglion block alleviate immunologically-linked disorders? Med. Hypotheses 144:110000. doi: 10.1016/j.mehy.2020.110000
Lipov, E., and Ritchie, E. C. A. (2015). Review of the use of stellate ganglion block in the treatment of PTSD. Curr. Psychiatry Rep. 17:599. doi: 10.1007/s11920-015-0599-4
Lipov, E. G., Candido, K., and Ritchie, E. C. (2017). Possible reversal of PTSD-related DNA methylation by sympathetic blockade. J. Mol. Neurosci. 62, 67–72. doi: 10.1007/s12031-017-0911-3
Lipov, E. G., Joshi, J. R., Sanders, S., and Slavin, K. V. A. (2009). Unifying theory linking the prolonged efficacy of the stellate ganglion block for the treatment of chronic regional pain syndrome (CRPS), hot flashes, and posttraumatic stress disorder (PTSD). Med. Hypotheses 72, 657–661. doi: 10.1016/j.mehy.2009.01.009
Makar, M., Smyth, B., and Brennan, F. (2021). Chronic kidney disease-associated pruritus: a review. Kidney Blood Press. Res. 46, 659–669. doi: 10.1159/000518391
Mettang, T., and Kremer, A. E. (2015). Uremic pruritus. Kidney Int. 87, 685–691. doi: 10.1038/ki.2013.454
O'Connell, N. E., Wand, B. M., Gibson, W., Carr, D. B., Birklein, F., Stanton, T. R., et al. (2016). Local anaesthetic sympathetic blockade for complex regional pain syndrome. Cochrane Database Syst. Rev. 7:Cd004598. doi: 10.1002/14651858.CD004598.pub4
Schiller, M., Ben-Shaanan, T. L., and Rolls, A. (2021). Neuronal regulation of immunity: why, how and where? Nat. Rev. Immunol 21, 20–36. doi: 10.1038/s41577-020-0387-1
Siemens, W., Xander, C., Meerpohl, J. J., Antes, G., and Becker, G. (2014). Drug treatments for pruritus in adult palliative care. Dtsch. Arztebl. Int. 111, 863–870. doi: 10.3238/arztebl.2014.0863
Simonsen, E., Komenda, P., Lerner, B., Askin, N., Bohm, C., Shaw, J., et al. (2017). Treatment of uremic pruritus: a systematic review. Am. J. Kidney Dis. 70, 638–655. doi: 10.1053/j.ajkd.2017.05.018
Sulková, S. D., Pokorná, A., Šafránek, R., Pavlíková, L., and Palička, V. (2021). [Bone disesase in end-stage kidney disease - renal and non-renal components]. Vnitr. Lek. 67, 258–263. doi: 10.36290/vnl.2021.072
Tong, F., He, Q., Du, W. J., Yang, H., Du, D., Pu, S., et al. (2022). Sympathetic nerve mediated spinal glia activation underlies itch in a cutaneous T-cell lymphoma model. Neurosci. Bull. 38, 435–439. doi: 10.1007/s12264-021-00805-6
Verduzco, H. A., and Shirazian, S. (2020). CKD-associated pruritus: new insights into diagnosis, pathogenesis, and management. Kidney Int. Rep. 5, 1387–1402. doi: 10.1016/j.ekir.2020.04.027
Wang, C. P., Lu, Y. C., Tsai, I. T., Tang, W. H., Hsu, C. C., Hung, W. C., et al. (2016). Increased levels of total p-cresylsulfate are associated with pruritus in patients with chronic kidney disease. Dermatology 232, 363–370. doi: 10.1159/000445429
Wang, Y., Anesi, J., Maier, M. C., Myers, M. A., Oqueli, E., Sobey, C. G., et al. (2023). Sympathetic nervous system and atherosclerosis. Int. J. Mol. Sci. 24:13132. doi: 10.3390/ijms241713132
Witt, C. M., Bolona, L., Kinney, M. O., Moir, C., Ackerman, M. J., Kapa, S., et al. (2017). Denervation of the extrinsic cardiac sympathetic nervous system as a treatment modality for arrhythmia. Europace 19, 1075–1083. doi: 10.1093/europace/eux011
Keywords: CKD-aP, uremia, sympathetic nerve block, chronic kidney disease, autonomic nervous system
Citation: Li Y, Chen Y, Nie J, Huang X and Zhang W (2025) Case Report: Sympathetic nerve block treat chronic kidney disease-associated pruritus. Front. Neurosci. 19:1529183. doi: 10.3389/fnins.2025.1529183
Received: 16 November 2024; Accepted: 31 March 2025;
Published: 16 April 2025.
Edited by:
Vitor Engracia Valenti, São Paulo State University, BrazilReviewed by:
Mohamed Essameldin Abdelgawad, Wake Forest University, United StatesPuneet Agarwal, Sawai ManSingh Medical College, India
Copyright © 2025 Li, Chen, Nie, Huang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weiwei Zhang, emhhbmd3d0BzeG11LmVkdS5jbg==
 Ying Li
Ying Li Yaohua Chen1
Yaohua Chen1 Weiwei Zhang
Weiwei Zhang