- 1Department of Rehabilitation, Hunan Provincial People’s Hospital (The first Affiliated Hospital of Hunan Normal University), Changsha, China
- 2Department of Neurological Rehabilitation, Hunan Rehabilitation Hospital, Changsha, China
- 3School of Rehabilitation Medicine, Capital Medical University, Beijing, China
- 4Music Therapy Center, China Rehabilitation Research Center, Beijing, China
Introduction: Musical sensory orientation training (MSOT) is an innovative technique to improve the state of consciousness and cognitive function. Compared with traditional arousal therapies, MSOT offers a non-invasive, safe, and easily operable alternative with no side effects. This study aimed to conduct a preliminary investigation into the effect of MSOT in improving consciousness levels in patients with DoC (Disorders of Consciousness), as well as the feasibility of its clinical application, thereby providing reference for future large-sample randomized controlled studies.
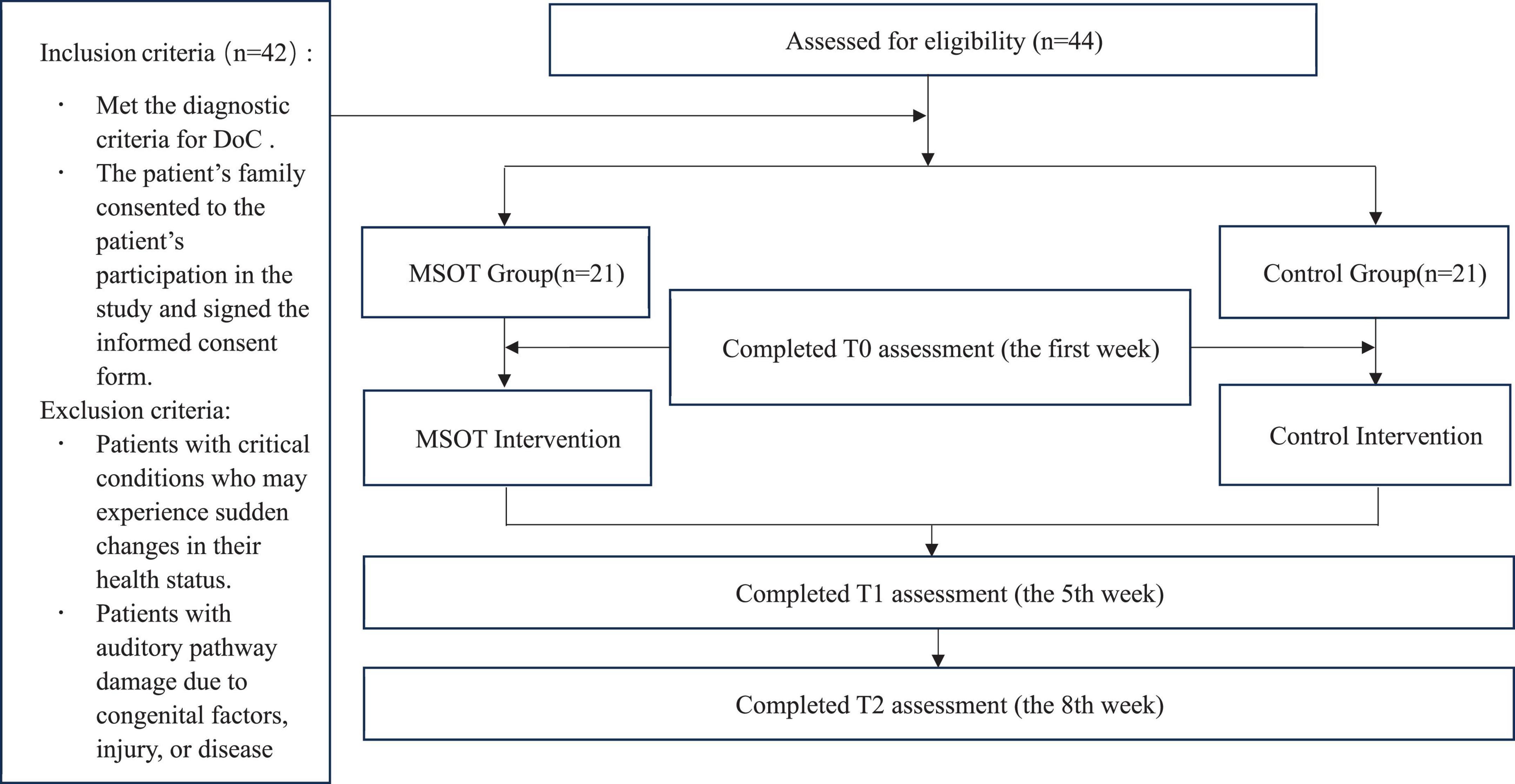
Methods: We recruited 42 participants between March 2024 to March 2025, dividing them into two groups: a control group of 21 patients who received conventional treatment for DoC and watched videos of family/friends’ activities and short videos, and an intervention group of 21 patients who received MSOT along with conventional treatment. Patients in both groups were assessed at baseline, week 5 and week 8 of the intervention.
Results: The MSOT group showed significant improvement in Coma Recovery Scale—Revised (CRS-R) subscale and total scores over time (baseline, week 5, week 8). At week 8, the MSOT group demonstrated significantly higher CRS-R scores in communication function and arousal level compared to the control group. Behavioral observations in the MSOT group revealed significantly higher frequencies of name response, sound source tracking, and command-following behaviors.
Conclusion: The results of this study demonstrate that MSOT exhibits certain effect in improving consciousness levels in patients with DoC and demonstrates feasibility in clinical implementation. Extending the intervention duration in future studies may amplify its therapeutic effects.
Introduction
Disorders of consciousness (DoC) are states of impaired consciousness resulting from serious brain injuries, and includes coma, vegetative state, and minimally conscious state, characterized by reduced levels of arousal and alterations in the content of consciousness (Bender et al., 2023). Patients with DoC face long-term, complex medical and caregiving challenges, presenting one of the most pressing issues in the field of neurorehabilitation. In recent years, several arousal techniques have been developed in the field of DoC rehabilitation, such as pharmacotherapy, hyperbaric oxygen therapy, and brain neuromodulation techniques, which have achieved some success in the treatment of coma (Edlow et al., 2021; Yang et al., 2020). While pharmacologic interventions (e.g., amantadine, zolpidem) have shown promise in enhancing arousal in chronic DoC, their utility is limited by tachyphylaxis, adverse effects (e.g., agitation, insomnia), and variable efficacy across injury endotypes (Giacino et al., 2018; Edlow et al., 2021). Placebo-controlled trials in this vulnerable population also raise ethical concerns, as withholding potential therapies may delay recovery (Fins, 2015). Furthermore, heterogeneity in structural and functional connectivity among DoC patients leads to inconsistent treatment responses, underscoring the need for personalized, non-invasive approaches (Edlow et al., 2021; Thibaut et al., 2019). Moreover, there is insufficient evidence-based support for their use in the arousal treatment of some patients with chronic DoC, and most of the treatments have certain risks (Yao et al., 2023).
With the advancement of neuroscience, neurologic music therapy has been established as a distinctive treatment for DoC. Music, as a sensory stimulus transmitted through auditory receptors, exerts varying effects on patients’ attention and auditory perception depending on its style, tonality, and tempo (Zhang et al., 2021; Liu et al., 2022; O’Kelly et al., 2013). Musical sensory orientation training (MSOT) is an emerging technique of neurologic music therapy that aims to improve the state of consciousness and cognitive function. In recent years, MSOT has gradually been implemented in clinical practice, and research into its mechanisms of action has commenced (Xiao et al., 2023). MSOT utilizes music as a medium to stimulate the sensory systems, thereby facilitating the rehabilitation of patients with DoC. Its fundamental principle is to stimulate the auditory, visual, tactile and motor sensory systems of patients through the rhythm, melody, pitch, and timbre of music, stimulating their sensory perception and motor function (Thaut and Hoemberg, 2014). Compared with traditional arousal therapies, MSOT is non-invasive, safe, and easy to operate, with no side effects. The technique leverages recorded music or live music performances to improve attention retention, enhance the execution of simple commands, and improve cognitive function by engaging patients in simple musical activities, either passively or actively. Various elements of music activate cognitive functions such as working memory, episodic memory, language processing, mental imagery, and attention (Boltzmann et al., 2021). Music therapy interventions employ live music, where therapists improvise on the keyboard with varying rhythms, melodies, and sound effects, eliciting emotional fluctuations of tension, anticipation, and humor (Lichtensztejn et al., 2014). Therapists incorporate various musical elements into patients’ responses, creating opportunities for meaningful interactions.
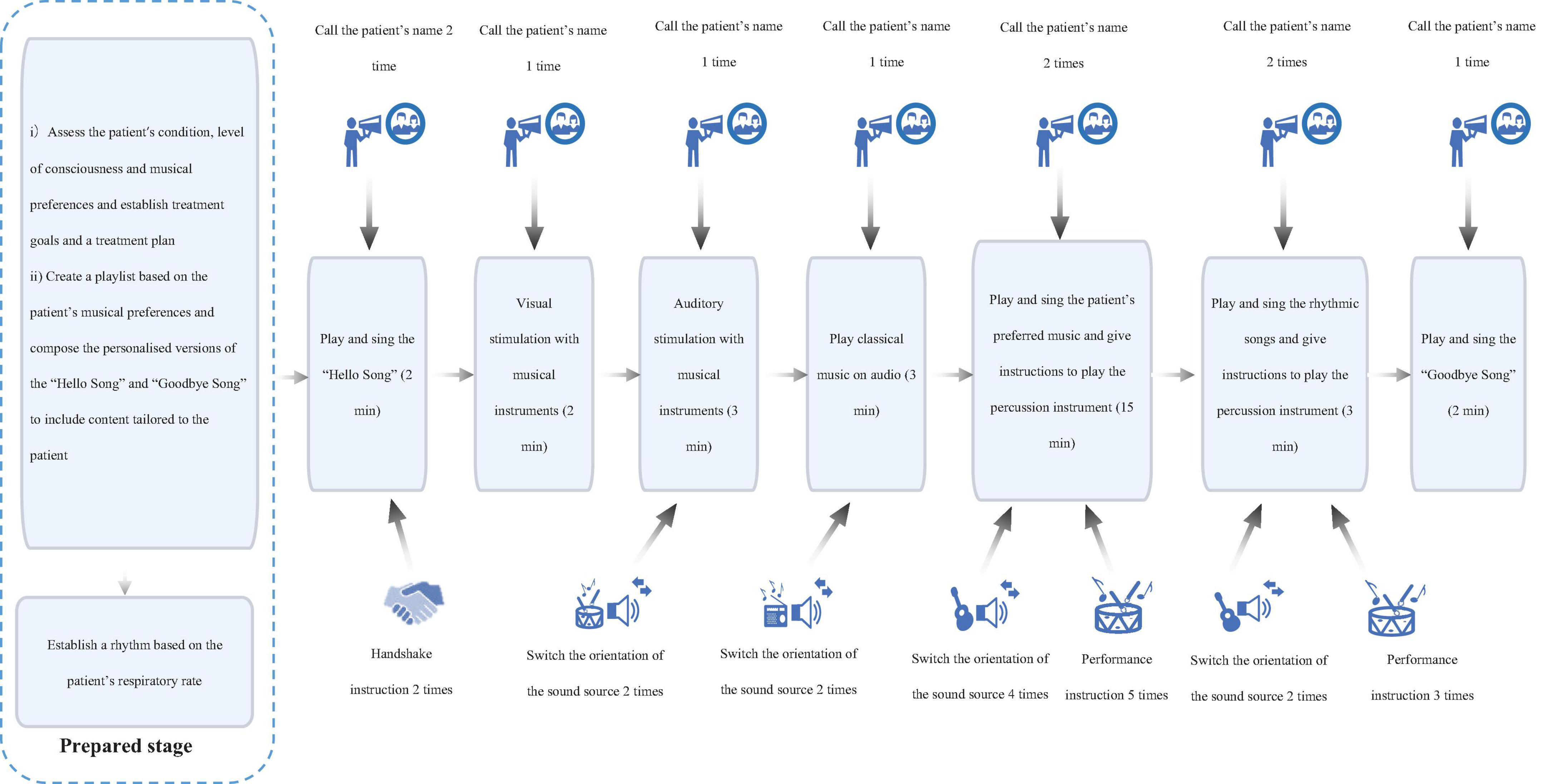
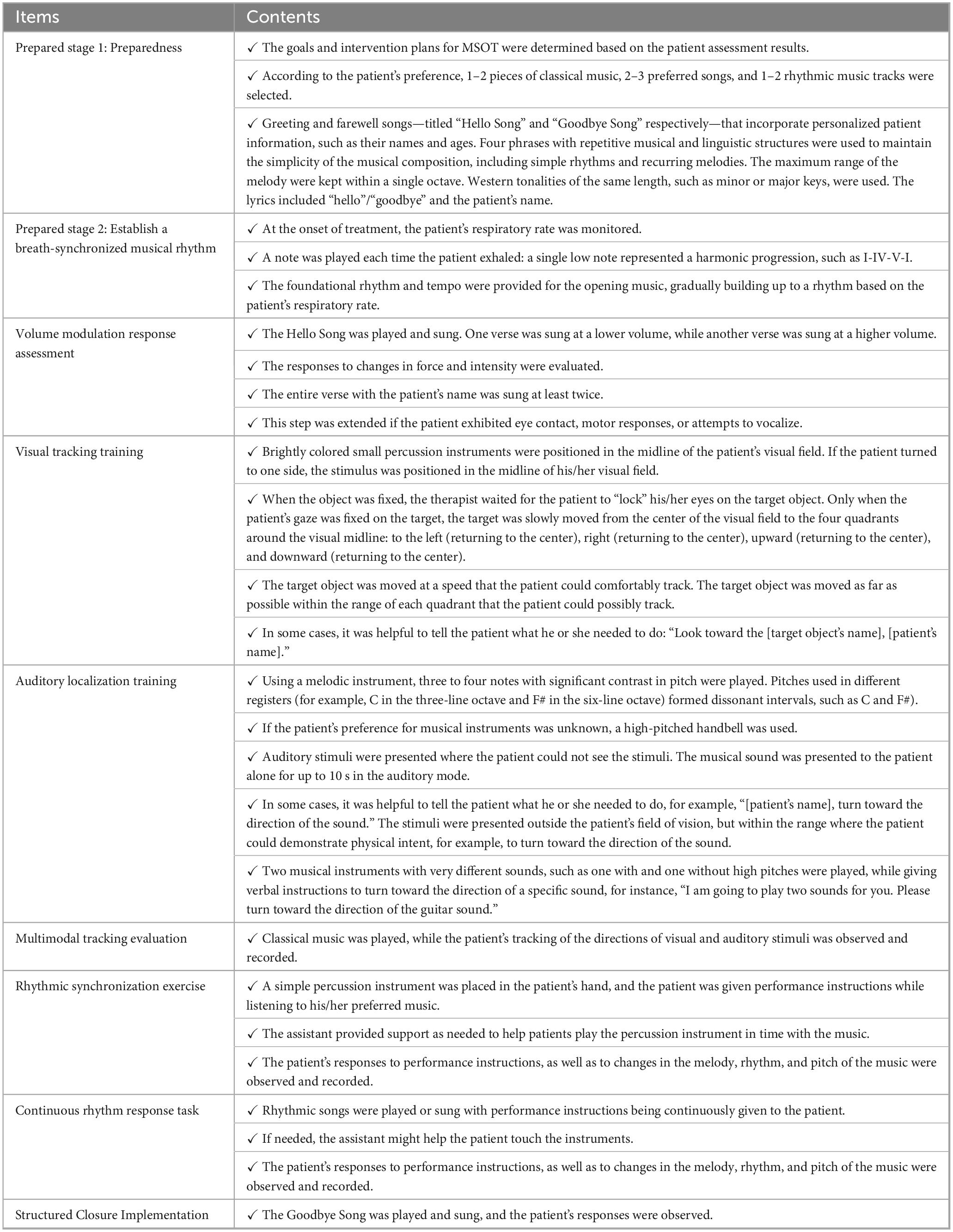
The study is significant in several areas. Firstly, in the fields of neurology and rehabilitation medicine, DoC is a major challenge and quite difficult to manage. Patients with DoC typically exhibit a range of cognitive, sensory, and motor impairments that severely affect their physical functioning and quality of life (Bender et al., 2023). Effective interventions are crucial to improving the level of consciousness of the patients. Secondly, MSOT is a promising approach that shows potential in improving the prognosis of patients with DoC (Thaut and Hoemberg, 2014; Boltzmann et al., 2021; Lichtensztejn et al., 2014). Further exploration of the efficacy of MSOT could contribute to the development of evidence-based medical interventions. Thirdly, the implementation of MSOT currently lacks standardized guidelines and protocols. Our study integrated auditory, visual, and sensory stimuli through the use of musical elements. During the treatment, the assessment method of the music therapy for DoC was adopted, allowing for concurrent treatment and evaluation. By combining the listening of preferred music with live improvised music interventions, the specific steps of the MSOT were formulated, thereby concretizing the MSOT approach. Therefore, this pilot study prospectively evaluated the therapeutic efficacy of MSOT for consciousness enhancement in DoC, while systematically assessing its clinical implementation feasibility, thereby establishing an empirical foundation for subsequent phase III randomized controlled trials.
Materials and methods
Individuals
Given the absence of prior research implementing MSOT in patients with DoC, the expected effect size remains uncertain. We conservatively assume a medium-to-large effect size range (Cohen’s *d* = 0.5–0.8). For the generalized estimating equation (GEE) analysis [α = 0.05; power (1-β) = 0.80], with intervention condition (MSOT vs. video-based multisensory stimulation) as the between-subject factor and time [week 1 (t0), week 5 (t1), week 8 (t2)] as the within-subject factor, we targeted 80% statistical power (corresponding to effect size *f* = 0.30). Power calculations using G*Power 3 indicated that an effective sample size of *n* = 17 per group would achieve 80% power for an effect size of *d* = 0.65 (within the projected medium-to-large range), yielding a total sample size of n = 34. To account for an anticipated 10% attrition rate due to data missingness (e.g., invalid questionnaires or participant dropout), we inflated the per-group sample size to 22, resulting in a final total of n = 44. This sample size aligns with comparable randomized controlled trials (e.g., Zhang et al., 2021; n = 40) and ensures sufficient power to detect effects on primary outcome measures.
The study enrolled patients diagnosed with DoC admitted to Hunan Provincial People’s Hospital between March 2024 and March 2025. Convenience sampling initially identified 44 candidates, of whom 42 met the eligibility criteria following the exclusion of two ineligible patients (Figure 1). Inclusion criteria required: (1) met the diagnostic criteria for DoC according to international consensus guidelines; (2) age ≥ 18 years. Exclusion criteria comprised: (1) acute critical illnesses with imminent risk of clinical deterioration; (2) neuroimaging-confirmed structural auditory pathway lesions (congenital malformations, traumatic injuries, or acquired pathologies).
A crucial team member, a doctor of the Department of Rehabilitation Medicine, assisted in presenting the study to potential participants. Posters were displayed in the wards and clinics, detailing the study’s purpose, content, risks and benefits. Written informed consent was obtained from all patients’ legally authorized representatives prior to participation. Participants were allocated to either the intervention (n = 21) or control group (n = 21).
Intervention
Patients in the intervention group underwent structured MSOT sessions five times weekly, each comprising 30 min of music-mediated multisensory training, over an 8-week period (Figure 2). Specific implementation steps for MSOT showed in Table 1. The MSOT was developed through a systematic synthesis of evidence from prior neurorehabilitation studies (Raglio et al., 2014; Binzer et al., 2016; Magee, 2018). The core component of MSOT is the development of an individualized treatment plan based on patient assessment, a dynamic adjustment process through breath synchronization, multi-sensory stimulation (visual tracking/auditory localization), structured musical interactions (customized greetings/farewells tracks), and rhythmic synchronized performance combined with real-time observational feedback. General treatment principles of MSOT showed in Supplemental material 1. All sessions were jointly administered by a certified neurologic music therapist (NMT) and a trained research assistant, with both personnel completing a 20-h competency-based training program in DoC-specific music intervention protocols prior to study initiation.
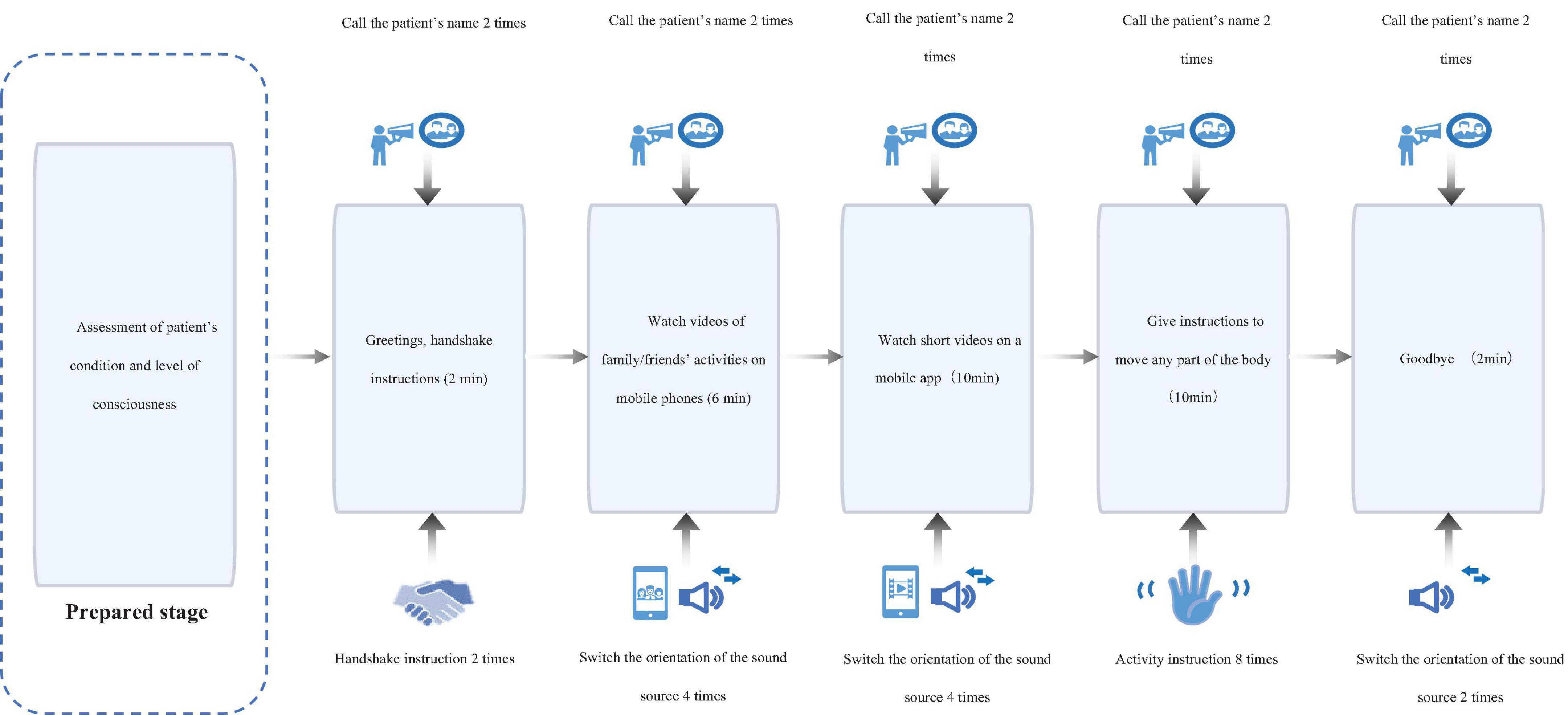
In addition to conventional treatment, patients in the control group were exposed to video-based multisensory stimulation consisting of two components: (i) customized audiovisual recordings of family/friends’ daily activities; (ii) passive viewing of neutral short videos via a tablet device (e.g., nature scenes, abstract animations). To standardize tactile input, neutral objects including a plastic comb, textured rubber ball, and silicone massage stick were passively placed in patients’ palms for non-directed tactile exploration during sessions. Interventions were administered in 30-min sessions five times weekly over 8 weeks, with each session jointly supervised by a certified rehabilitation therapist from the research team and the patient’s primary caregiver to ensure protocol adherence (Figure 3).
Outcome measures
Coma Recovery Scale-Revised (CRS-R) (Giacino et al., 2004): The CRS-R consists of six subscales assessing the auditory function, visual function, motor function, oromotor function, communication, and arousal of the patient. Based on subscale scores, patients were diagnosed with unresponsive wakefulness syndrome, minimally conscious state (MCS), which includes two subcategories known as MCS + and MCS-, or emergence from MCS. To minimize the risk of misdiagnosis, two experienced clinicians conducted the CRS-R assessments twice daily for five consecutive days. The best result from these evaluations was used for the diagnosis (Wannez et al., 2017).
Frequency of behavioral observations: After reviewing the literature (Magee, 2018; Bower et al., 2023), we identified several behavioral parameters for systematic monitoring during therapeutic interventions, including: (a) frequency of onymous response manifestations (head turning, eye blinking, gaze orientation toward auditory stimuli, facial grimacing, and vocalizations upon name recognition); (b) frequency of acoustic source localization through directional gaze orientation; (c) frequency of spontaneous object/instrument manipulation; and (d) frequency of instructional compliance in performing percussive motor sequences. To ensure precise documentation of MSOT-induced responses, all sessions were video-recorded following acquisition of informed consent, with trained evaluators subsequently quantifying response frequencies through frame-by-frame video analysis. According to the calculation, the Cronbach’sα coefficient for the behavioral observation scale was 0.958.
The CRS-R assessments were conducted twice a day for five consecutive days in week 1 (T0), week 5 (T1), and week 8 (T2) of the intervention. The best score from each assessment period was used. Other behavioral assessments were conducted by comparing the cumulative behavioral frequencies at T0, T1, and T2.
Patient and public involvement statement
This study engaged patients with Disorders of Consciousness (DoC) during the intervention phase. The Musical Sensory Orientation Training (MSOT) protocol was individualized to reflect patients’ musical preferences. Recruitment adhered to strict ethical protocols, with informed consent secured. Throughout the intervention, trained researchers systematically monitored behavioral responses (e.g., name recognition, sound tracking) to refine sensory stimulation in real time. Outcomes were analyzed and communicated within the clinical research team to guide future rehabilitation strategies.
Statistical analysis
Statistical analyses were performed using SPSS 22.0 for Windows (SPSS, Chicago, IL, United States). The Kolmogorov–Smirnov test was used to test the normality of the data. Normally distributed data were expressed as mean (standard deviation) and non-normally distributed data were expressed as median (interquartile range). The t-test and chi-square test were used to assess the balance of the baseline characteristics of the patients between the two groups. A generalized estimating equation model was developed to assess the longitudinal changes in outcome indicators, with outcome indicators at each time point as the dependent variable, and intervention, time, and the interaction between treatment and time as the independent variables. Multiple comparisons were conducted using the Bonferroni method, with statistical significance defined as p < 0.05.
Results
Participants’ characteristics
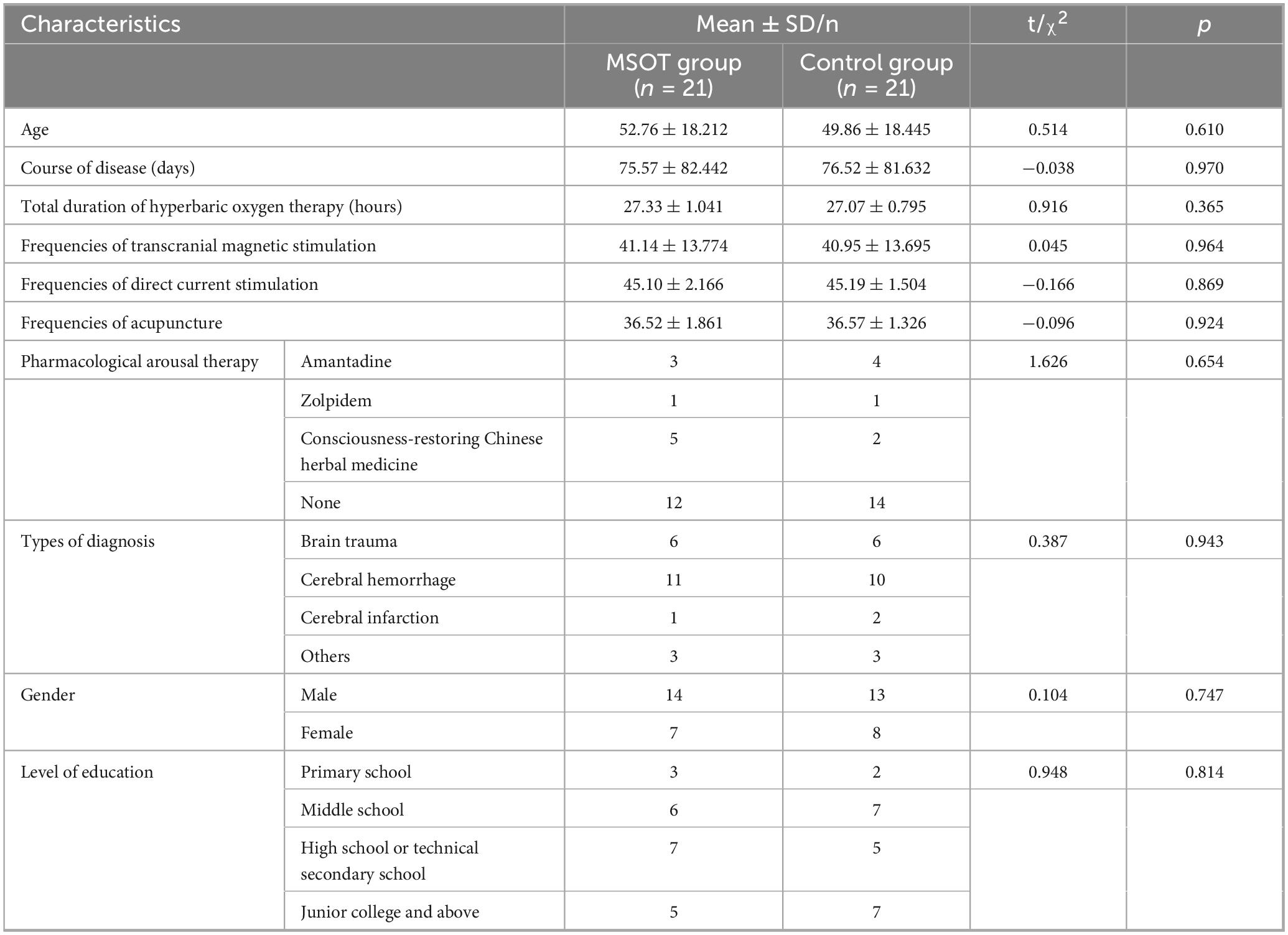
A comparative analysis was performed between the two groups regarding age, gender, educational level, disease diagnosis, disease course (defined as days from onset to enrollment), the type of arousal medication used and other arousal-promoting interventions (including duration/frequency of such treatments). No statistically significant differences were observed between the groups (p > 0.05; see Table 2).
Table 2 presents the baseline characteristics of the intervention (MSOT) and control groups, demonstrating their comparability at the study outset. Both groups had similar demographic and clinical profiles, with no significant differences in age (52.76 ± 18.21 vs. 49.86 ± 18.45 years, p = 0.610), disease duration (75.57 ± 82.44 vs. 76.52 ± 81.63 days, p = 0.970), or total hyperbaric oxygen therapy hours (27.33 ± 1.04 vs. 27.07 ± 0.80, p = 0.365). Frequencies of adjunct therapies (e.g., transcranial magnetic stimulation, acupuncture) were also balanced (p > 0.05). Pharmacological arousal therapies and diagnosis types (e.g., brain trauma, cerebral hemorrhage) were similarly distributed (p > 0.05). Gender (male: 14 vs. 13) and education levels (e.g., junior college and above: 5 vs. 7) showed no disparities (p > 0.05). This homogeneity supports the validity of subsequent outcome comparisons, as confounding variables were minimized.
Intervention effects on outcomes
Interaction effects of generalized estimating equations
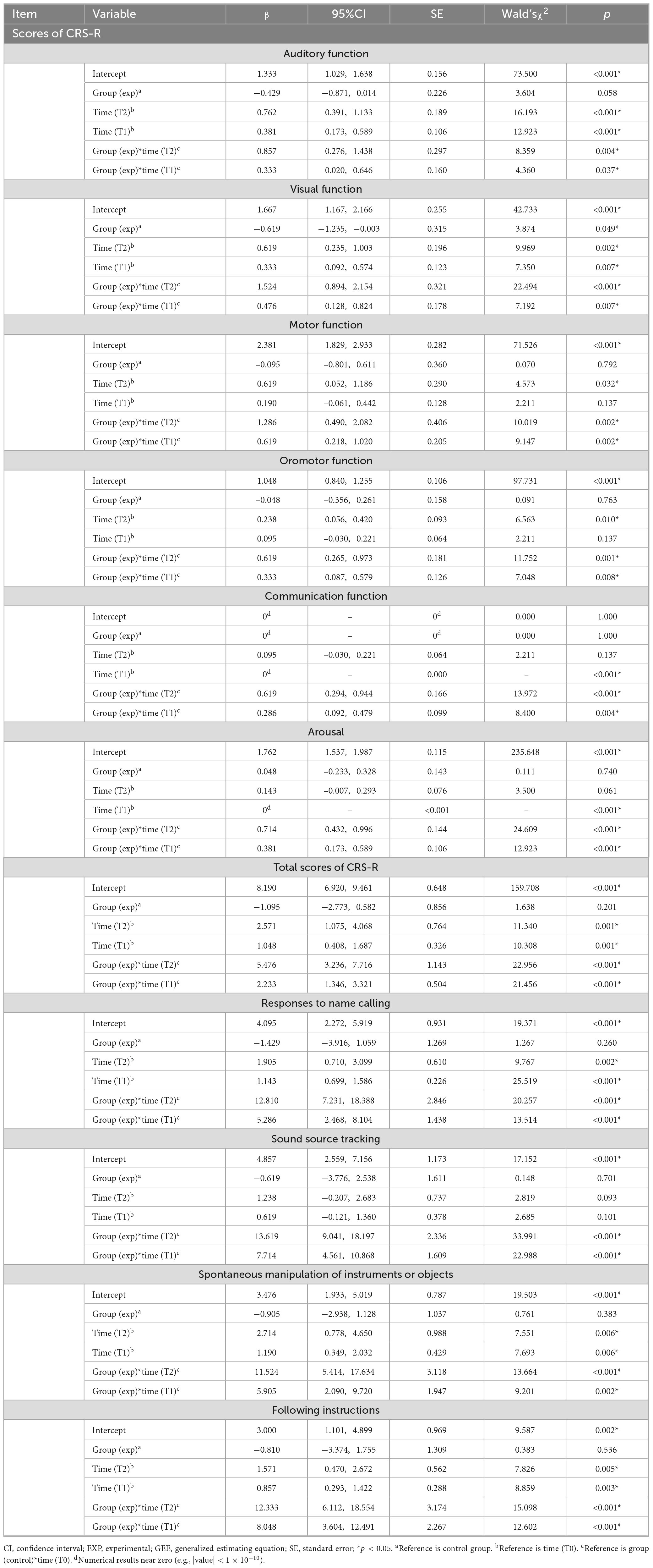
Table 3 presents the results of the generalized estimating equation (GEE) analysis, which evaluates the longitudinal effects of the intervention across multiple timepoints (T0: baseline; T1: mid-intervention; T2: post-intervention). The analysis reveals significant group-by-time interactions (p < 0.05) for all assessed Coma Recovery Scale-Revised (CRS-R) subscales (auditory, visual, motor, oromotor, communication, arousal) and total score, as well as all behavioral observation frequencies (responses to name calling, sound source tracking, spontaneous manipulation of instruments or objects, following instructions), at both T1 and T2 follow-ups. The significant interactions indicate that the trajectory of improvement over time differed significantly between the intervention group and the control group, with the intervention group demonstrating substantially greater improvements.
For instance, the significant interaction for auditory function at T1 (β = 0.333, p = 0.037) indicates that the intervention group achieved a greater mean improvement from baseline than the control group, with an adjusted difference of 0.333 points (95% CI: 0.020–0.646) at T1. Meanwhile, the interaction effect for at T2 was more substantial (β = 0.857, p = 0.004), indicating that the intervention group achieved a mean score increase 0.857 points (95% CI: 0.276–1.438) greater than the control group at T2 relative to T0 baselines.
Similarly, significant effects were also found for visual function (T2:β = 1.524, p < 0.001; T1:β = 0.476, p = 0.007), motor function (T2:β = 1.286, p = 0.002; T1:β = 0.619, p = 0.002), oromotor function (T2:β = 0.619, p = 0.001; T1:β = 0.333, p = 0.008), communication function (T2:β = 0.619, p < 0.001; T1:β = 0.286, p = 0.004), arousal (T2:β = 0.714, p < 0.001; T1:β = 0.381, p < 0.001), and total CRS-R score (T2:β = 5.476, p < 0.001; T1:β = 2.233, p < 0.001), as well as frequencies of behavioral observation, including responses to name calling (T2:β = 12.810, p < 0.001; T1:β = 5.286, p < 0.001), sound source tracking (T2:β = 13.619, p < 0.001; T1:β = 7.714, p < 0.001), spontaneous manipulation of instruments or objects (T2:β = 11.524, p < 0.001; T1:β = 5.905, p = 0.002), following instructions (T2:β = 12.333, p < 0.001; T1:β = 8.048, p < 0.001). These findings collectively suggest that the intervention not only accelerates functional recovery across sensory, motor, and communicative domains but also leads to significantly greater enhancements in complex behavioral responsiveness compared to the control condition, which are critical for patients with disorders of consciousness.
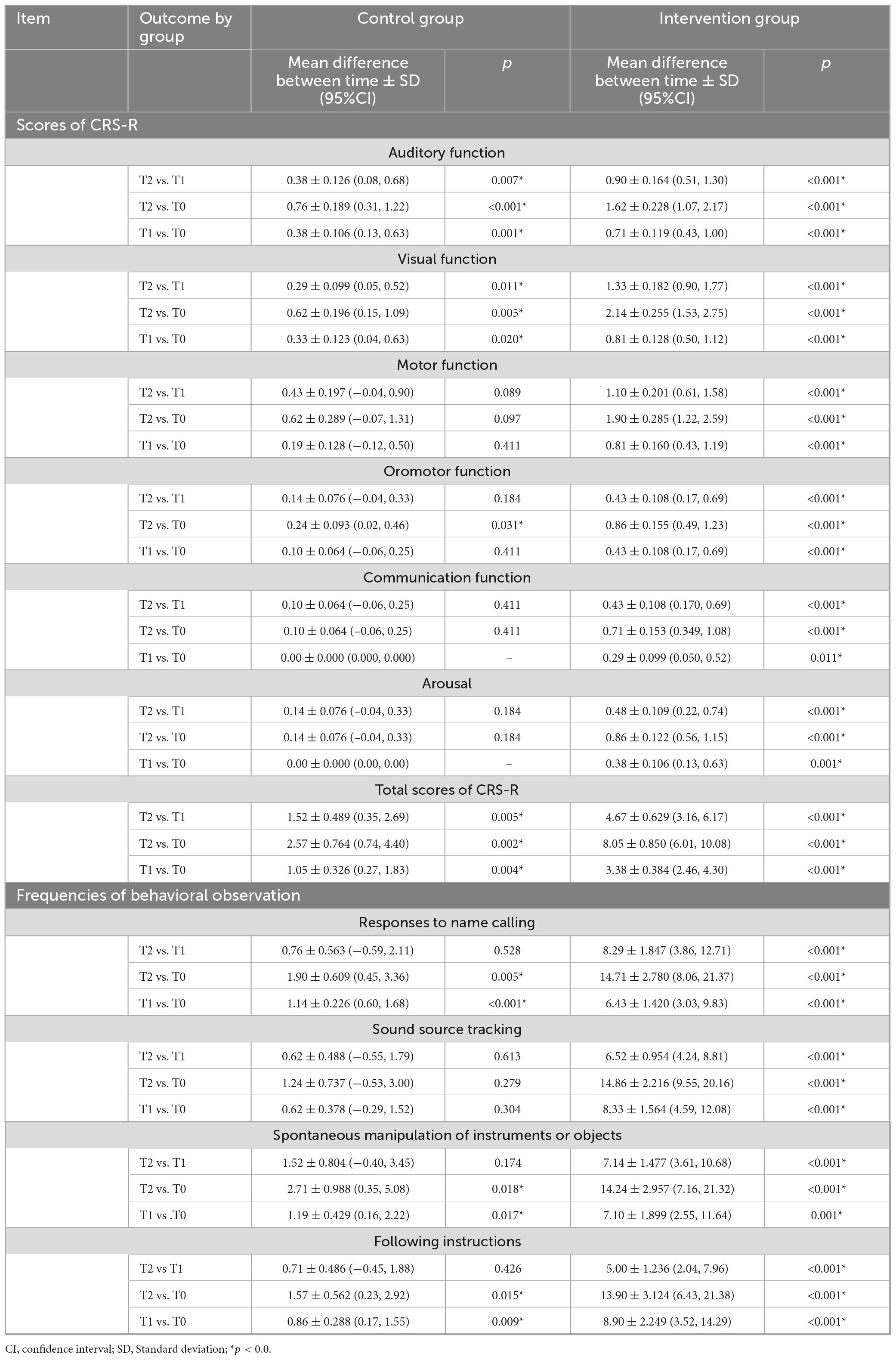
Simple effects analysis of time
Given the statistically significant group-by-time interaction effect, further analyses examined simple effects. Tables 4, 5 provides a detailed comparison of within-group and between-group changes across the three timepoints. Table 4 presents the results of a simple effects analysis examining within-group changes over time (T0; T1; T2) using Generalized Estimating Equations (GEE). The intervention group demonstrated significantly greater improvements across all outcomes compared to the control group. For example, in auditory function, the intervention group showed a significant increase of 1.62 points from T0 to T2 (95% CI: 1.07–2.17, p < 0.001), whereas the control group had a smaller but also significant increase of 0.76 points (95% CI: 0.31–1.22, p < 0.001). Similar patterns emerged for visual function, responses to name calling, spontaneous manipulation of objects, and instruction-following (all p < 0.05).
Critically, motor function improvements were significant in the intervention group (1.90 points, 95% CI: 1.22–2.59, p < 0.001) but non-significant in the control group (0.62 points, 95% CI: −0.07–1.31, p = 0.097). The same pattern of significant was observed for oromotor function, communication, arousal, and sound source tracking. This divergence confirmed the effectiveness of the intervention. Importantly, the intervention group sustained improvement from T1 (10.48 ± 0.761) to T2 (15.14 ± 1.153), as evidenced by total CRS-R scores (increase of 4.67 points, p < 0.001), which far exceeded the concurrent gains in the control group (1.52 points, p = 0.005). These results underscore the superiority of the intervention in driving both functional and behavioral recovery, with significant implications for clinical practice.
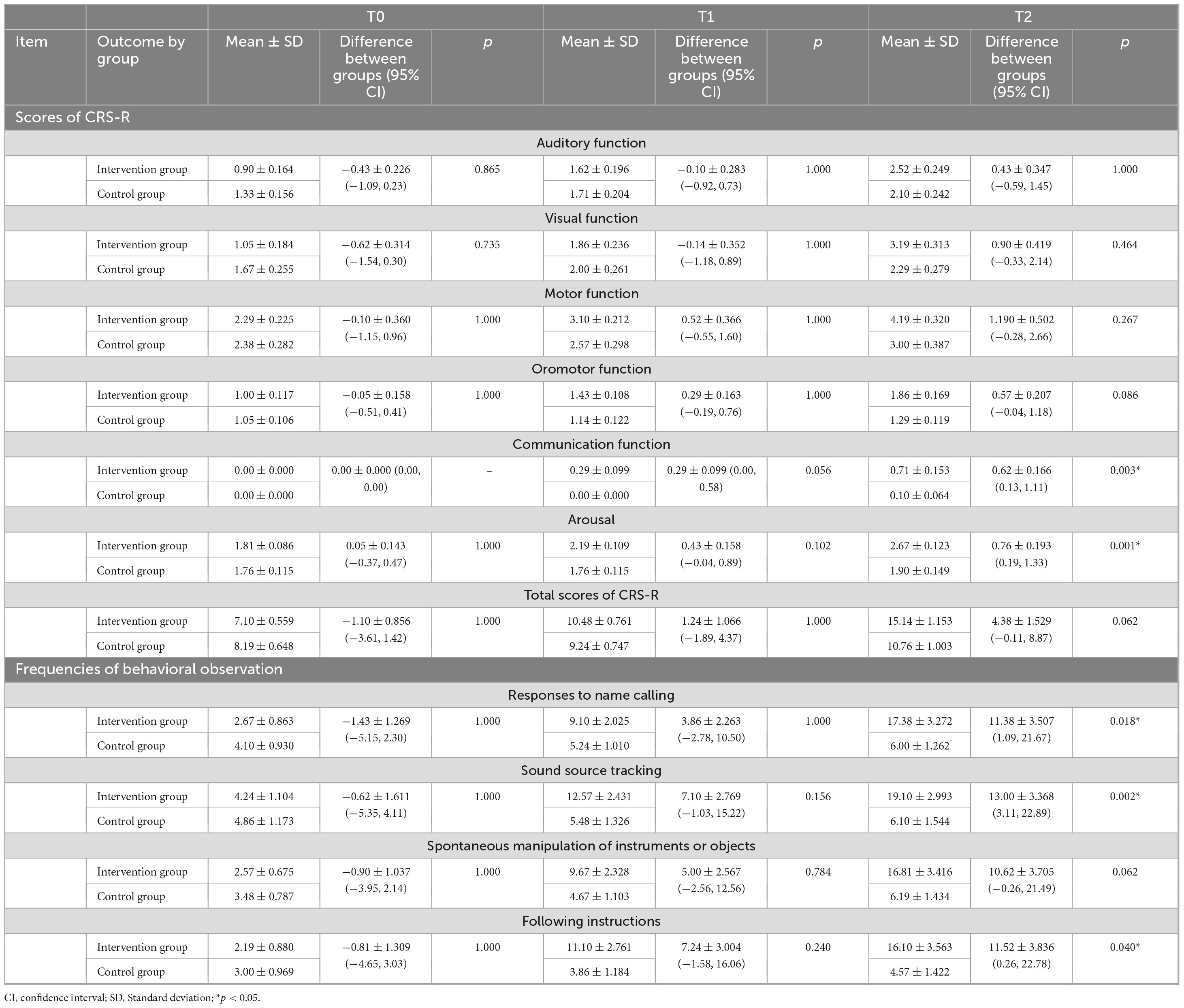
Simple effects analysis of group
Intergroup comparisons demonstrated no significant differences in CRS-R subscales (auditory, visual, motor, oromotor), total score, or behavioral frequencies at baseline (T0) and week 5 (T1) (all p > 0.05). By week 8 (T2), the MSOT group exhibited significantly greater improvements versus controls in: communication function (mean difference = 0.62, 95% CI: 0.13–1.11; p = 0.003), arousal (0.76, 95% CI: 0.19–1.33; p = 0.001), responses to name-calling (11.38, 95% CI: 1.09–21.67; p = 0.018), sound source tracking (13.00, 95% CI: 3.11–22.89; p = 0.002), and following instructions (11.52, 95% CI: 0.26–22.78; p = 0.040). Conversely, no significant intervention effects were detected for auditory function, visual function, motor function, oromotor function, spontaneous manipulation of instruments or objects or CRS-R composite scores at any assessment point, including T2 (p > 0.05), details in Table 5.
Discussion
MSOT, as an innovative treatment, is of great significance for the rehabilitation of patients with DoC. The results of this study showed that with the increased duration of MSOT intervention, patients with DoC showed significant improvements in all subscale scores of the CRS-R and the total CRS-R score, as well as in the frequency of behavioral observations. These findings suggest that MSOT is effective in improving the consciousness levels of patients with DoC, which is consistent with the results of previous studies on the effect of live music on improving consciousness in patients with DoC (Liu et al., 2022; O’Kelly et al., 2013; Raglio et al., 2014; Formisano et al., 2001; Binzer et al., 2016). Research suggests that musical stimuli may elicit responses more effectively than verbal stimuli in patients with DoC (Magee et al., 2023). In live improvisational performances, the appropriate adjustment of musical elements such as rhythm, pitch, mode, and volume to support and match some of the behaviors exhibited by patients such as unconscious manipulation of small instruments, blinking, and finger movements significantly encourages patient engagement in musical interaction (O’Connor and Gray, 2022). In addition, the use of the patient’s preferred music can also enhance the expression of residual functions in patients with DoC (Heine et al., 2017). Therefore, in this study, the intervention protocol of MSOT fully considered the selection of musical pieces and the patients’ musical preferences. The patients with DoC were engaged actively or passively through the use of arousal music, live performances of their preferred music, and improvised songs, which effectively improved their behavioral responses.
The results of this study also revealed no significant differences in all outcome measures between the MSOT and control groups at week 5 of the intervention. However, at week 8 of the intervention, the MSOT group showed significant improvements in communication and arousal scores of the CRS-R, as well as in the frequencies of responses to name-calling, sound source tracking, and instruction-following behaviors compared with the control group. These findings indicate that the duration of MSOT intervention affects its efficacy, with improvements becoming more pronounced over time. Furthermore, the MSOT intervention was significantly more effective than the control in improving communication function, arousal level, and behavioral responses in patients. The advantages of music therapy in improving the level of consciousness in patients with DoC lie in its ability to enhance arousal levels and attention, as well as provide opportunities for communicative interaction (Magee et al., 2022). Improvements in name response/sound tracking (behavioral metrics) reflect arousal and attention, which may precede recovery of higher-order functions (e.g., motor execution). CRS-R subscales like “auditory function” require consistent command-following, whereas behavioral metrics capture transient responses. Total CRS-R improvements likely stem from cumulative gains across subscales, even if individual domains (e.g., motor) lacked significance. The findings of this study corroborate this perspective. In the MSOT intervention, improvised music is introduced which contains the name of the patient and has a rhythm based on the patient’s respiratory rate (Magee, 2018). The presentation of preferred music provides a predictable patient behavioral response that can be adapted during live performance to meet individual needs. This approach reduces overstimulation, while maximizing opportunities for musical interaction, thereby reducing the likelihood of understimulation. However, the 8-week MSOT intervention did not show a significant advantage in improving auditory, visual, motor, and oromotor functions in patients with DoC compared with the control group. This lack of significant improvement in these specific domains is likely attributable to the insufficient duration of the intervention, which may not have been long enough to translate gains in arousal and attention into measurable functional recovery in motor and oromotor systems. Research suggests that for patients with motor dysfunction following stroke or traumatic brain injury, an intervention duration exceeding three months is recommended (Daly et al., 2019; Morris et al., 2018; Kwakkel et al., 2023). However, most studies indicate that the training period required for the rehabilitation of cognitive and speech functions might be even longer (Merceur et al., 2024; Axmadjon, 2024). Therefore, based on evidence from comparable rehabilitation paradigms targeting motor and cognitive recovery, future MSOT trials aiming to capture effects on motor, oromotor, and higher-order cognitive functions should consider a minimum intervention duration of 3 months, with potentially longer durations (e.g., ≥ 6 months) required to adequately assess speech and complex cognitive outcomes.
The observed temporal pattern of treatment response—with significant improvements emerging only at week 8 (T2) rather than week 5 (T1)—suggests two potential neurobiological mechanisms. First, MSOT’s multisensory integration may require prolonged exposure to induce structural neuroplasticity in thalamocortical circuits. Animal models demonstrate that combined auditory-somatosensory stimulation over ≥ 4 weeks upregulates synaptic density in the medial geniculate body and primary sensory cortices, particularly after traumatic axonal injury (Fernández-Espejo et al., 2015; Edlow et al., 2021). This aligns with human fMRI studies showing music-enhanced functional connectivity between auditory cortices and prefrontal regions only after 6–8 weeks of intervention in DoC patients (Boltzmann et al., 2021). Second, behavioral conditioning through repetitive musical cues (e.g., pairing patient’s name with specific melodic phrases) may strengthen associative learning in preserved hippocampal-cortical networks. Classical conditioning paradigms in MCS patients require 100–150 trials over 3–4 weeks to establish reliable stimulus-response patterns (Schiff et al., 2009), matching our 40-session protocol. These mechanisms collectively suggest MSOT operates through both bottom-up sensory pathway modulation and top-down cognitive retraining—a dual-process framework supported by recent thalamic deep brain stimulation studies (Chudy et al., 2018).
The quantitative analysis revealed statistically significant improvements in CRS-R following MOST intervention, with 7/21 patients (33.3%) transitioning from MCS-to sMCS, and 5/21 (23.8%) transitioning from VS/MCS- to MCS + neurobehavioral thresholds. Operational viability was confirmed through protocol adherence rates exceeding 90% across all intervention cohorts.
Conclusion
The results of this study demonstrate that MOST appears effective in improving consciousness levels in patients with DoC and demonstrates feasibility in clinical implementation. Extending the intervention duration in future studies may amplify its therapeutic effects.
Limitations
This study has several limitations. Firstly, the study was limited by factors such as manpower, environment, and treatment duration, resulting in reliability that is inferior to that of a large-scale randomized controlled trial (RCT). Secondly, the duration of the intervention was constrained exploration of the effects of a longer intervention period. Thirdly, all outcome measures used were subjective assessment indicators, and the results were, to some extent, influenced by subjective factors. Fourthly, and critically in light of the control condition, the use of video-based multisensory stimulation as the control intervention, while a reasonable ethical compromise for this population, is not a fully inert placebo or matched “sham” version of the MSOT. This design choice means it may not adequately control for non-specific therapeutic effects, such as the attention received from researchers, the novelty of the experience, or the general sensory activation provided by the video content. Consequently, the observed differences between groups might partially reflect these non-specific factors rather than solely the specific therapeutic elements of the active MSOT intervention, potentially impacting the internal validity of the findings regarding the specific efficacy of MSOT itself. Future research should incorporate objective outcome measures (e.g., near-infrared spectroscopy, electroencephalogram analysis) and employ more rigorous control conditions, such as carefully matched sham interventions or active control groups controlling for non-specific factors, to further investigate the specific effects and mechanisms of MSOT intervention in larger-scale RCTs.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Hunan Provincial People’s Hospital’s Ethics Committee (Approval No. 2024-105). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JG: Data curation, Methodology, Resources, Writing – original draft, Writing – review & editing. WL: Data curation, Methodology, Project administration, Writing – review & editing. SZ: Investigation, Resources, Visualization, Writing – review & editing. LQ: Data curation, Investigation, Writing – review & editing. YD: Data curation, Investigation, Writing – review & editing. CF: Data curation, Supervision, Writing – review & editing. XZ: Methodology, Project administration, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Capital’s Funds for Health Improvement and Research, CFH 2024-2-6011, National Natural Science Foundation of China (NSFC) No. T2341003, National Key Research and Development Program of China (Nos. 2022YFC3600300 and 2022YFC3600305), Health Research Projects of Hunan Provincial Health Commission No. W20243094 and Hunan Province Cerebrovascular Disease Rehabilitation Research Centre.
Acknowledgments
We would like to thank the participants for their time and efforts in this study. We appreciate the supports from Hunan Provincial People’s Hospital.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnins.2025.1610811/full#supplementary-material
References
Axmadjon, A. I. (2024). Rehabilitation of stroke patients. Ethiopian Int. J. Multidisciplinary Res. 11, 250–257.
Bender, A., Eifert, B., Rubi-Fessen, I., Jox, R., Maurer-Karattup, P., and Müller, F. (2023). The neurological rehabilitation of adults with coma and disorders of consciousness. Dtsch. Arztebl. Int. 120, 605–612. doi: 10.3238/arztebl.m2023.0159
Binzer, I., Schmidt, H., Timmermann, T., Jochheim, M., and Bender, A. (2016). Immediate responses to individual dialogic music therapy in patients in low awareness states. Brain Inj 30, 919–925. doi: 10.3109/02699052.2016.1144082
Boltzmann, M., Schmidt, S., Gutenbrunner, C., Krauss, J., Stangel, M., Höglinger, G., et al. (2021). Auditory stimulation modulates resting-state functional connectivity in unresponsive wakefulness syndrome patients. Front. Neurosci. 15:554194. doi: 10.3389/fnins.2021.554194
Bower, J., Magee, W., Catroppa, C., and Baker, F. (2023). Content validity and inter-rater reliability of the music interventions in pediatric DoC behavior observation record. J. Music Ther. 60, 13–35. doi: 10.1093/jmt/thac013
Chudy, D., Deletis, V., Šagi, I., Rosenzweig, M. R., and Vukić, M. (2018). Deep brain stimulation for the early treatment of the minimally conscious state and vegetative state: Experience in 14 patients. World Neurosurg. 110, e595–e606. doi: 10.3171/2016.10.JNS161071
Daly, J., McCabe, J., Holcomb, J., Monkiewicz, M., Gansen, J., and Pundik, S. (2019). Long-dose intensive therapy is necessary for strong, clinically significant, upper limb functional gains and retained gains in severe/moderate chronic stroke. Neurorehabil. Neural Repair. 33, 523–537. doi: 10.1177/1545968319846120
Edlow, B. L., Sanz, L. R. D., Polizzotto, L., Pouratian, N., Rolston, J., Snider, S., et al. (2021). Therapies to restore consciousness in patients with severe brain injuries: A gap analysis and future directions. Neurocrit. Care 35, 68–85. doi: 10.1007/s12028-021-01227-y
Fernández-Espejo, D., Rossit, S., and Owen, A. M. (2015). A thalamocortical mechanism for the absence of overt motor behavior in covertly aware patients. JAMA Neurol. 72, 1442. doi: 10.1001/jamaneurol.2015.2614
Fins, J. J. (2015). Disorders of consciousness and disordered care: Families, caregivers, and narratives of necessity. Arch. Phys. Med. Rehabil. 96, 1384–1390. doi: 10.1016/j.apmr.2012.12.028
Formisano, R., Vinicola, V., Penta, F., Matteis, M., Brunelli, S., and Weckel, J. (2001). Active music therapy in the rehabilitation of severe brain injured patients during coma recovery. Ann. Ist Super Sanita 37, 627–630.
Giacino, J. T., Katz, D. I., Schiff, N. D., Whyte, J., Ashman, E. J., Ashwal, S., et al. (2018). Practice guideline update recommendations summary: Disorders of consciousness: Report of the guideline development, dissemination, and implementation subcommittee of the American Academy of Neurology; the American Congress of Rehabilitation Medicine; and the National Institute on Disability, Independent Living, and Rehabilitation Research. Neurology 91, 450–460. doi: 10.1212/WNL.0000000000005926
Giacino, J., Kalmar, K., and Whyte, J. (2004). The JFK coma recovery scale-revised: Measurement characteristics and diagnostic utility. Arch. Phys. Med. Rehab. 85, 2020–2029. doi: 10.1016/j.apmr.2004.02.033
Heine, L., Tillmann, B., Hauet, M., Juliat, A., Dubois, A., Laureys, S., et al. (2017). Effects of preference and sensory modality on behavioural reaction in patients with disorders of consciousness. Brain Inj 31, 1307–1311. doi: 10.1080/02699052.2017.1306108
Kwakkel, G., Stinear, C., Essers, B., Munoz-Novoa, M., Branscheidt, M., Cabanas-Valdés, R., et al. (2023). Motor rehabilitation after stroke: European Stroke Organisation (ESO) consensus-based definition and guiding framework. Eur. Stroke J. 8, 880–894. doi: 10.1177/23969873231191304
Lichtensztejn, M., Macchi, P., and Lischinsky, A. (2014). Music therapy and disorders of consciousness: Providing clinical data for differential diagnosis between vegetative state and minimally conscious state from music-centred music therapy and neuroscience perspectives. Music Therapy Perspect. 32, 47–55. doi: 10.1093/mtp/miu001
Liu, Z., Liu, Y., Zhao, L., Li, M., Liu, C., Zhang, C., et al. (2022). Short-term efficacy of music therapy combined with alpha binaural beat therapy in disorders of consciousness. Front. Psychol. 13:947861. doi: 10.3389/fpsyg.2022.947861
Magee, W. (2018). Music in the diagnosis, treatment and prognosis of people with prolonged disorders of consciousness. Neuropsychol. Rehabil. 28, 1331–1339. doi: 10.1080/09602011.2018.1494003
Magee, W., Lipe, A., Ikeda, T., and Siegert, R. (2022). Exploring the clinical utility of the music therapy assessment tool for awareness in disorders of consciousness (MATADOC) with people with end-stage dementia. Brain Sci. 12:1306. doi: 10.3390/brainsci12101306
Magee, W., Narayanan, A., O’Connor, R., Haughey, F., Wegener, E., Chu, B., et al. (2023). Validation of the music therapy assessment tool for awareness in disorders of consciousness with the Coma recovery scale-revised. Arch. Phys. Med. Rehabil. 104:1107. doi: 10.1016/j.apmr.2023.03.010
Merceur, M., Reilly, K., Bonan, I., Holé, J., Hummel, E., Cogné, M., et al. (2024). A systematic review of rehabilitation programmes for cognitive impairment related to breast cancer: Different programmes at different times? Ann. Phys. Rehab. Med. 67:101832. doi: 10.1016/j.rehab.2024.101832
Morris, T., Costa-Miserachs, D., Rodriguez-Rajo, P., Finestres, J., Bernabeu, M., Gomes-Osman, J., et al. (2018). Feasibility of aerobic exercise in the subacute phase of recovery from traumatic brain injury: A case series. J. Neurol. Phys. Ther. 42, 268–275. doi: 10.1097/NPT.0000000000000239
O’Connor, R., and Gray, D. (2022). Exploring the effectiveness of music therapy intervention as part of interdisciplinary assessment and treatment for patients with prolonged disorders of consciousness. Music Med. 14, 125–132. doi: 10.47513/mmd.v14i2.833
O’Kelly, J., James, L., Palaniappan, R., Taborin, J., Fachner, J., Magee, W., et al. (2013). Neurophysiological and behavioural responses to music therapy in vegetative and minimally conscious states. Front. Human Neurosci. 7:884. doi: 10.3389/fnhum.2013.00884
Raglio, A., Guizzetti, G., Bolognesi, M., Antonaci, D., Granieri, E., Baiardi, P., et al. (2014). Active music therapy approach in disorders of consciousness: A controlled observational case series. J. Neurol. 261, 2460–2462. doi: 10.1007/s00415-014-7543-0
Schiff, N. D., Giacino, J. T., and Fins, J. J. (2009). Deep brain stimulation, neuroethics, and the minimally conscious state—moving beyond proof of principle. Arch. Neurol. 66, 697–702. doi: 10.1001/archneurol.2009.79
Thaut, M., and Hoemberg, V. (2014). Handbook of Neurologic Music Therapy. Oxford: Oxford University Press.
Thibaut, A., Schiff, N., Giacino, J., Laureys, S., and Gosseries, O. (2019). Therapeutic interventions in patients with prolonged disorders of consciousness. Lancet Neurol. 18, 600–614. doi: 10.1016/S1474-4422(19)30031-6
Wannez, S., Heine, L., Thonnard, M., Gosseries, O., and Laureys, S. (2017). The repetition of behavioral assessments in diagnosis of disorders of consciousness. Ann. Neurol. 81, 883–889. doi: 10.1002/ana.24962
Xiao, X., Chen, W., and Zhang, X. (2023). The effect and mechanisms of music therapy on the autonomic nervous system and brain networks of patients of minimal conscious states: A randomised controlled trial. Front. Neurosci. 17:182181. doi: 10.3389/fnins.2023.1182181
Yang, Y., Xie, Q., and He, J. (2020). Interpretation of “Diagnoses and treatments of prolonged disorders of consciousness: The Chinese experts consensus”. J. Clin. Neurosurg. 17, 601–604. doi: 10.3969/j.issn.1672-7770.2020.06.001
Yao, S., Tang, Y., and Li, S. (2023). Research progress of music therapy assisting the rehabilitation of patients with disorders of consciousness. Chinese J. Rehab. Med. 38, 427–431. doi: 10.3969/j.issn.1001-1242.2023.03.026
Keywords: disorders of consciousness, MSOT, music therapy, CRS-R, pilot study
Citation: Gu J, Long W, Zeng S, Qin L, Dong Y, Fang C and Zhang X (2025) The effect of musical sensory orientation training in improving consciousness level in patients with disorders of consciousness: a pilot study. Front. Neurosci. 19:1610811. doi: 10.3389/fnins.2025.1610811
Received: 13 April 2025; Accepted: 25 June 2025;
Published: 24 July 2025.
Edited by:
Teresa Lesiuk, University of Miami, United StatesReviewed by:
Isabella Fioravante, Pontificia Universidad Católica de Chile, ChileBrooke Murtaugh, Madonna Rehabilitation Hospital, United States
Copyright © 2025 Gu, Long, Zeng, Qin, Dong, Fang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoying Zhang, Q2hldW5neGlhb3lpbmdAcXEuY29t
 Jiayi Gu
Jiayi Gu Wei Long1
Wei Long1