- 1Barts and the London School of Medicine and Dentistry, William Harvey Research Institute, Queen Mary University of London, London, United Kingdom
- 2Sir William Dunn School of Pathology, University of Oxford, Oxford, United Kingdom
- 3Department of Drug Science and Technology, University of Turin, Turin, Italy
- 4Department of Basic Medical Sciences, School of Medicine, Al-Balqa Applied University, As-Salt, Jordan
- 5Diabetes Complication Research Centre, School of Medicine, UCD Conway Institute, University College Dublin, Dublin, Ireland
- 6Department of Intensive Care and Intermediate Care, RWTH University Hospital Aachen, Aachen, Germany
A Correction on
RvE1 attenuates polymicrobial sepsis-induced cardiac dysfunction and enhances bacterial clearance
By Chen J, Purvis GSD, Collotta D, Al Zoubi S, Sugimoto MA, Cacace A, Martin L, Colas RA, Collino M, Dalli J and Thiemermann C (2020). Front. Immunol. 11:2080. doi: 10.3389/fimmu.2020.02080
There was a mistake in Figure 3A as published. The previous image of Figure 3A (MHCII vs. SSC-A scatter plot) was selected from a mouse in the 24-hour post-CLP group that had received RvE1 treatment, as we initially understood that RvE1-treated mice were also subjected to 24-hour CLP. However, to avoid any further confusion, we have now replaced this scatter plot with an image from a mouse subjected to CLP without RvE1 treatment. This change more accurately reflects the legend of Figure 3A: “(A) Flow cytometry gating strategy of mouse peritoneal immune cells 24 h post-CLP”. The corrected Figure 3 and its caption appear below.
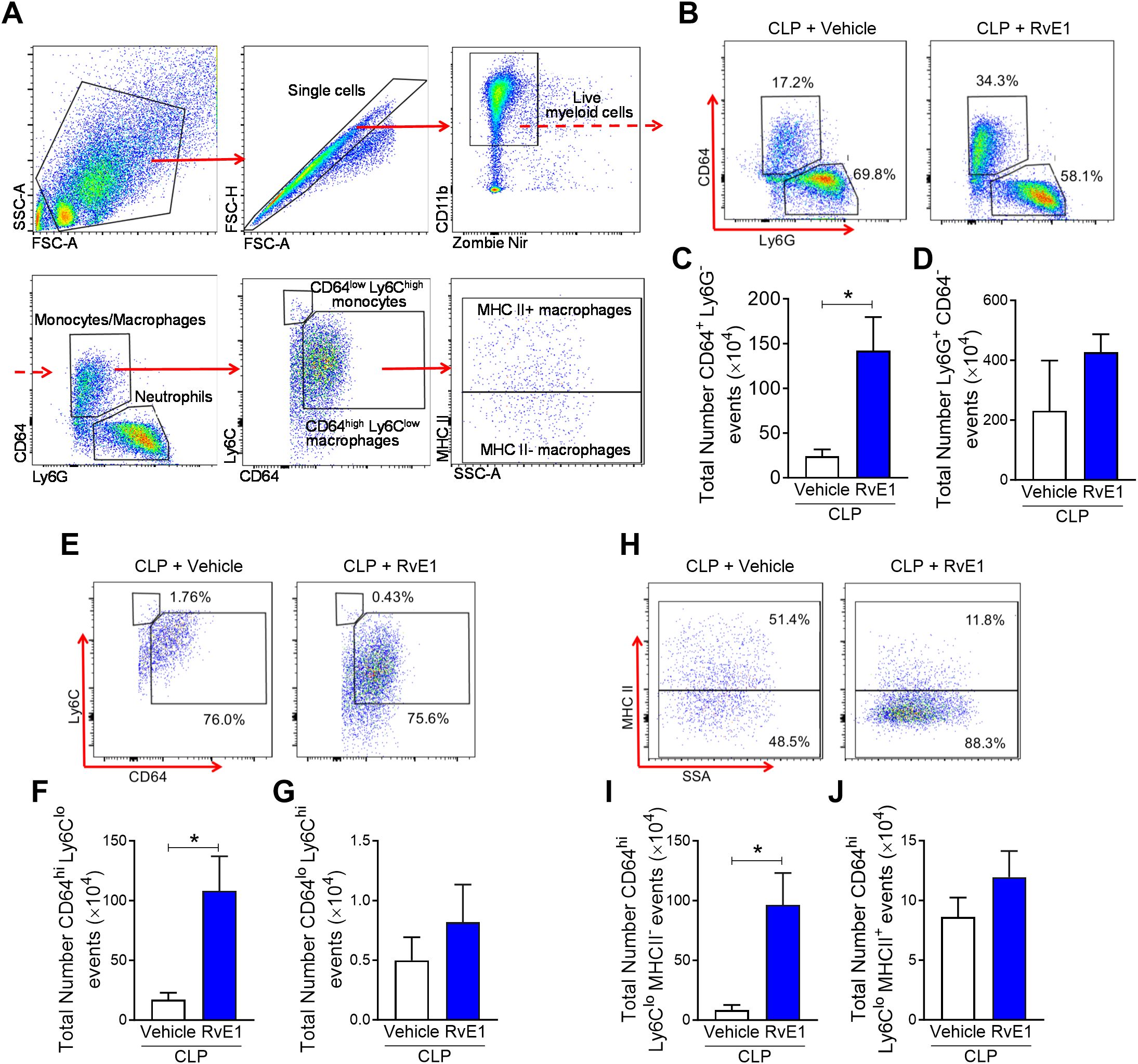
Figure 3. RvE1 treatment enhances MHC II- macrophage recruitment in peritoneal cavity. Mice underwent CLP surgery. One hour after CLP, mice were treated with either RvE1 (1 μg/mouse i.v.) or vehicle (100 μl PBS, 0.1% Ethanol). (A) Flow cytometry gating strategy of mouse peritoneal immune cells 24 h post-CLP. (B) Scattergrams illustrating monocyte/macrophage (identified as Ly6G-CD64+) and neutrophil (identified as Ly6G+CD64-) positive events in peritoneal lavages from CLP mice with vehicle or RvE1 treatment. (C, D) Cumulative data for peritoneal CD64+ monocytes/macrophages and Ly6G+ neutrophils. (E) Scattergrams illustrating macrophage (identified as CD64highLy6Clow) and monocyte (identified as CD64lowLy6Chigh) positive events in peritoneal lavages from CLP mice with vehicle or RvE1 treatment. (F, G) Cumulative data for peritoneal CD64highLy6Clow macrophages and CD64lowLy6Chigh monocytes. (H) Scattergrams illustrating MHC II- macrophage and MHC II+ macrophage positive events in peritoneal lavages from CLP mice with vehicle or RvE1 treatment. (I, J) Cumulative data for peritoneal MHC II- macrophages and MHC II+ macrophages. Data are expressed as mean ± SEM of four mice for vehicle group and five mice for RvE1 treatment group. Data were analyzed by unpaired Student’s t-test. *P< 0.05 versus CLP + Vehicle group.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Keywords: polymicrobial sepsis, resolvin E1, bacterial clearance, immune response, cardiomyopathy
Citation: Chen J, Purvis GSD, Collotta D, AI Zoubi S, Sugimoto MA, Cacace A, Martin L, Colas RA, Collino M, Dalli J and Thiemermann C (2025) Correction: RvE1 attenuates polymicrobial sepsis-induced cardiac dysfunction and enhances bacterial clearance. Front. Immunol. 16:1659224. doi: 10.3389/fimmu.2025.1659224
Received: 03 July 2025; Accepted: 18 July 2025;
Published: 31 July 2025.
Edited and Reviewed by:
Niccolo Terrando, Duke University, United StatesCopyright © 2025 Chen, Purvis, Collotta, AI Zoubi, Sugimoto, Cacace, Martin, Colas, Collino, Dalli and Thiemermann. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianmin Chen, amlhbm1pbi5jaGVuQHFtdWwuYWMudWs=; Christoph Thiemermann, Yy50aGllbWVybWFubkBxbXVsLmFjLnVr
 Jianmin Chen
Jianmin Chen Gareth S. D. Purvis
Gareth S. D. Purvis Debora Collotta
Debora Collotta Sura AI Zoubi
Sura AI Zoubi Michelle A. Sugimoto
Michelle A. Sugimoto Antonino Cacace1,5
Antonino Cacace1,5 Lukas Martin
Lukas Martin Massimo Collino
Massimo Collino Jesmond Dalli
Jesmond Dalli Christoph Thiemermann
Christoph Thiemermann