Precision cardiovascular medicine: shifting the innovation paradigm
- Frontiers in Science
- Article hubs
- Transforming cardiovascular medicine with precision approaches
- Explainer
Explainer
Front Sci, 07 October 2025
This explainer is part of an article hub, related to lead article https://doi.org/10.3389/fsci.2025.1474469
Cardiovascular diseases (CVDs) are the leading cause of death globally.
Yet despite improved public health guidance on lifestyle factors—as well as new drug therapies—heart disease deaths continue to rise. For example, 19 million people died from CVDs in 2020, and by 2030 this is expected to reach 26 million.
We now know that CVDs are highly complex and diverse conditions, which means that conventional "one-size-fits-all" treatments do not work for everyone.
In their Frontiers in Science article, Aikawa et al. outline the challenges in treating CVDs, and the scientific advances and innovations in precision medicine that could overcome them. This explainer summarizes the article’s main points.
What are the challenges in treating CVD?
CVD is an umbrella term consisting of dozens of different heart and blood vessel conditions, such as heart failure, arrhythmias, high blood pressure, stroke, and blood clots.
However, even patients with identical diagnoses exhibit varied symptoms and treatment response. This is influenced by unique combinations of genetic, environmental, and lifestyle factors.
This diversity extends all the way down to how CVDs progress at the cellular level. Diseases may involve different components of the immune system, changes in metabolism, or altered stress responses. This makes it difficult to find treatments that will work reliably across the many patients who have CVDs.
A key example of this problem can be seen in a drug class called statins, which treat high cholesterol levels. While statins can successfully lower cholesterol and thus heart disease risks in many patients, they do not work for everyone.
Whether this is due to differences in genetics, cells, the drugs themselves, or a combination of factors, it suggests that current treatments are not enough to address the full range of CVDs.
How can precision medicine improve treatments for CVD?
Precision medicine is an approach that allows doctors to personalize treatments for individual patients. It aims to use the right treatments for the right patients at the right time.
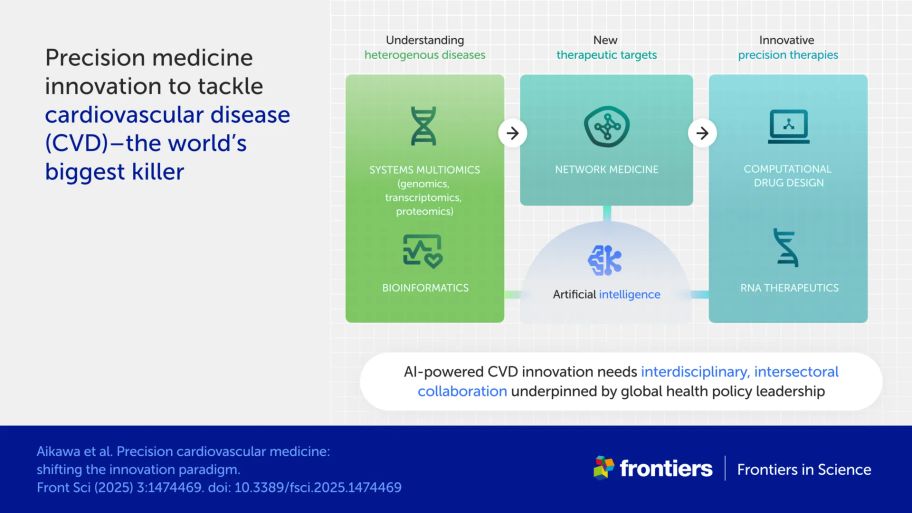
Aikawa et al. argue that the complexity of CVDs means scientists must move beyond studying single drug candidates and instead embrace a new era of precision medicine. They highlight the potential benefits of systems biology, which looks at how networks of genes and proteins interact to shape disease.
Systems biology helps scientists find biological markers that let clinicians diagnose and treat diseases.
Biomarkers can also help scientists predict how effective drugs will be each disease, and identify which genes and proteins could act as effective targets for new drugs.
What can omics technologies reveal about CVD?
New technologies called “omics” are letting scientists categorize the molecules within cells with unprecedented detail.
“Proteomics,” for instance, identifies all the proteins present in cells. The technique can help drug developers find new biomarkers and drug targets for CVD.
Single-cell “transcriptomics” shows which genes are active in individual cells, rather than averaging results across a whole tissue sample. It has revealed that cell types are more diverse than expected, often consisting of multiple subsets.
This helps scientists see the unique roles each subset plays in disease progression. For example, a highly inflammatory subset might promote arterial disease.
“Multiomics,” which refers to combining different omics techniques, each with a unique set of strengths, can help us to further understand disease progression at the cellular level.
For example, multiomics has let researchers create detailed “atlases” that map the various kinds of cells within organs, clarifying the picture of how they work in health and disease.
These techniques will help to identify new drug targets and biomarkers for precision cardiovascular medicine. Research in this area is already showing that differences between cell types can help explain why diseases affect people in different ways. These cell-level variations may be a key reason why some patients get sicker than others or respond differently to the same treatment.
How can AI enhance precision cardiovascular medicine?
Artificial intelligence (AI) is already enhancing cardiovascular medicine and drug development. For example, it can improve how doctors predict disease progression and patient outcomes. It can also spot difficult-to-see abnormalities on patient scans.
AI can cluster patients into groups based on their disease types, which may help to develop better precision treatment pathways. Researchers are also using AI to understand enormous datasets from electronic health records, omics analyses, and drug trials.
In addition, AI now lets scientists design new drugs that hit newly discovered CVD targets, and helps to predict their effect and safety in individual patients. Doing this digitally before lab and human testing can rapidly accelerate drug development.
How can new therapeutics deliver precision medicine for CVDs?
Conventionally, “small molecule” drugs are used to treat most CVDs. These drugs disrupt the actions of proteins involved in disease, but many protein targets cannot be reached this way and are considered “undruggable.”
Newer classes of therapeutics could overcome this challenge, signposting more drug targets.
Pioneering drugs that target specific genes are showing particular promise in cardiovascular medicine. Known as RNA therapeutics, these drugs silence the RNA messages that produce harmful proteins involved in CVDs, including some previously considered undruggable. These therapies may also be quicker to develop than conventional medicines, and RNA therapeutics have already lowered cholesterol levels in some patients.
Scientists are also investigating the therapeutic potential of other kinds of RNA that don’t make proteins but regulate cell functions. Many of these “non-coding RNAs” are linked to CVDs, and research is ongoing to understand their role and test possible drugs that target them.
How can we implement precision cardiovascular medicine?
Aikawa et al. stress that transforming cardiovascular medicine using precision approaches requires global collaboration between many stakeholders across countries, disciplines, and sectors.
They argue for a new way of developing medicines in which scientists work together on the cutting-edge technologies described in their article. This paradigm will involve stronger partnerships between scientists and companies to ensure that new drug targets are successfully translated into medicines that reach patients. Data science and AI will be crucial throughout this process so that patients can benefit from the large and complex datasets generated by omics technologies.
The authors also call on global health policy leaders to support this transformation equitably so that its benefits reach everyone globally. This can be done through better funding opportunities, data organization, new clinical trial methods, drug regulation, and patient access policies.