- 1Department of Breast Surgery, West China Hospital of Sichuan University, Chengdu, China
- 2Engineering Research Center of Medical Information Technology, Ministry of Education, West China Hospital, Sichuan University, Chengdu, China
- 3Information Technology Center, West China Hospital of Sichuan University, Chengdu, China
- 4Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Department of Hepatobiliary and Pancreatic Surgery Unit I, Peking University Cancer Hospital and Institute, Beijing, China
- 5Northern Jiangsu People's Hospital, Clinic Medical College, Yangzhou University, Yangzhou, China
- 6Department of Liver Surgery and Liver Transplantation Centre, State Key Laboratory of Biotherapy and Cancer Center, West China Hospital, Sichuan University, Chengdu, China
To explore the updated evaluation about the obstetrical and perioperative outcomes of laparoscopic appendicectomy (LA) for pregnancy appendicitis compared with open appendicectomy (OA). Two reviewers independently searched the PubMed, the Cochrane Central Register of Controlled Trials, EMBASE, and Web of Science databases to screen eligible studies up to December 2020. Only clinical researches, no < 10 cases for LA and OA group were included. Twenty retrospective studies with 7,248 pregnant women, evaluating LA and OA in surgical and obstetrical outcomes, were included. The weighted mean difference (WMD) with 95% CI and odds ratio (OR) was used to compare continuous and dichotomous variables. It seems LA was connected with significantly shorter hospital time and lower wound infection [mean difference (MD), −0.57 days; 95% CI, −0.96 to −0.18; p = 0.004 and OR, 0.34; 95% CI, 0.18 to 0.62; p = 0.0005, respectively]. The incidence of fetal loss after LA was higher than OA (OR,1.93; 95% CI, 1.39–2.69; p < 0.0001). It was almost similar in the rate of preterm delivery (OR, 0.80; 95% CI, 0.48 to 1.34; p = 0.40) and other perioperative and obstetrical complications (p > 0.05). Our results indicated that the occurrence of fetal loss after LA should not be ignored. Caution, skillful operation, and thoroughly informed consent about the advantages and disadvantages of laparoscopy are necessary.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/#recordDetails, identifier: CRD42021233150.
Introduction
Acute appendicitis, the most common cause of non-obstetric acute abdomen, affecting 1.8–41 per 10,000 pregnancies and one in nearly 1,000 births (1, 2), accounts for 25% of non-obstetric procedures performed in the prenatal period (3). Acute appendicitis during pregnancy possesses a unique treatment challenge because of the high probability of Appendix translocation and the presence of the fetus limiting the applicability of imaging techniques (4). In addition, the symptoms and signs of appendicitis usually include lower abdominal pain, nausea, and lack of appetite, occasionally similar to the onset of pregnancy or parturition (5). Delayed diagnosis and treatment both increase the threats of perforation and intraabdominal infection that is associated with growing motherly morbidity and fetal mortality (6). For suspected pregnant appendicitis, open or laparoscopic appendectomy (LA) is the mainstay of treatment strategy (7, 8).
According to previous reports, patients with LA had less wound infection, less post-operative ache, and get back faster to work than those with open appendectomy (OA) (9, 10). Laparoscopies give a clearer visualization of the whole abdomen than OA. The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) guidelines currently is inclined to LA as the routine therapy for pregnant appendicitis (11). However, some large-scale studies have pointed out that LA has a non-ignorable influence on fetal loss and pre-term labor (12, 13). The optimal surgical procedure is still equivocal for pregnancy appendicitis. Acute simple appendicitis tends to occur in the first and second trimesters, whereas perforation is more inclined toward the third trimester (5, 6, 14). However, in clinical practice, LA and OA both have been performed in patients, whether it is the early or the third trimester. Many systematic reviews have been published to evaluate the effects of the two surgical methods on the fetus and pregnant women, but until now there have been no consistent conclusions (15–17). In the past 2 years, some clinical studies evaluating the two operations have tended to show no significant difference in obstetric outcomes, such as fetal loss and pre-term delivery (18, 19). It is likely that the obstetric outcomes may have improved with recent progress in perioperative care and laparoscopic technique. To illustrate these issues, we implemented a systematic review and updated meta-analysis to evaluate the obstetric and operational outcomes of LA and OA during pregnancy.
Methods
Materials and Methods
The study has been conducted on the basis of the PRISMA guidelines (20) and registered with a registration number at PROSPERO (CRD42021233150). Institutional Review Board approval is not required as this article is a systematic review and not an experimental study.
Search Strategy
A literature retrieval was conducted on December 23, 2020. Major electronic literature databases, PubMed, Web of Science, EMBASE, and the Cochrane Central Register of Controlled Trials, were roundly screened by two independent investigators (J Zhang and MY Wang) using the following search terms: pregnancy, laparoscopic, open, appendicectomy and appendicitis. The particular search strategies are in Appendix. To prevent missing relevant studies, the references of literature and publications were manually searched. We used the endnote X9 to remove the duplicated articles.
Inclusion and Exclusion
Two investigators (J Zhang and MY Wang) reviewed the currently available literature and independently viewed all titles and abstracts for eligible studies. Included in the standard were the following: (I) research on LA and OA for pregnancy appendicitis; (II) randomized controlled trials (RCTs), case-control studies, retrospective studies, and cohort studies; (III) pregnant patients with acute appendicitis. Exclusion criteria included the following: (I) editorials, reviews, letters, comments, animal studies, or case reports; (II) non-English studies; (III) studies < 10 patients per group; (IV) data that were unrecognizable and incomplete.
Data Extraction and Evaluation
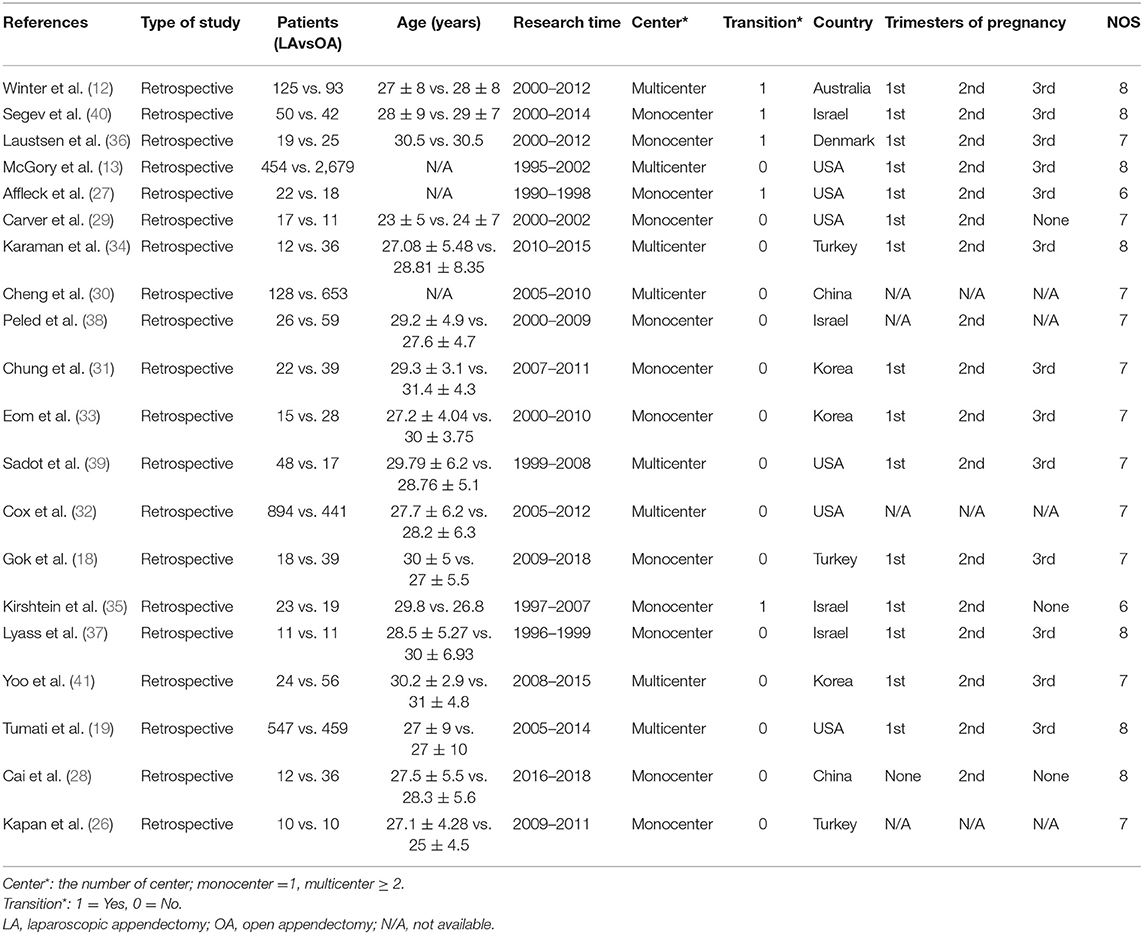
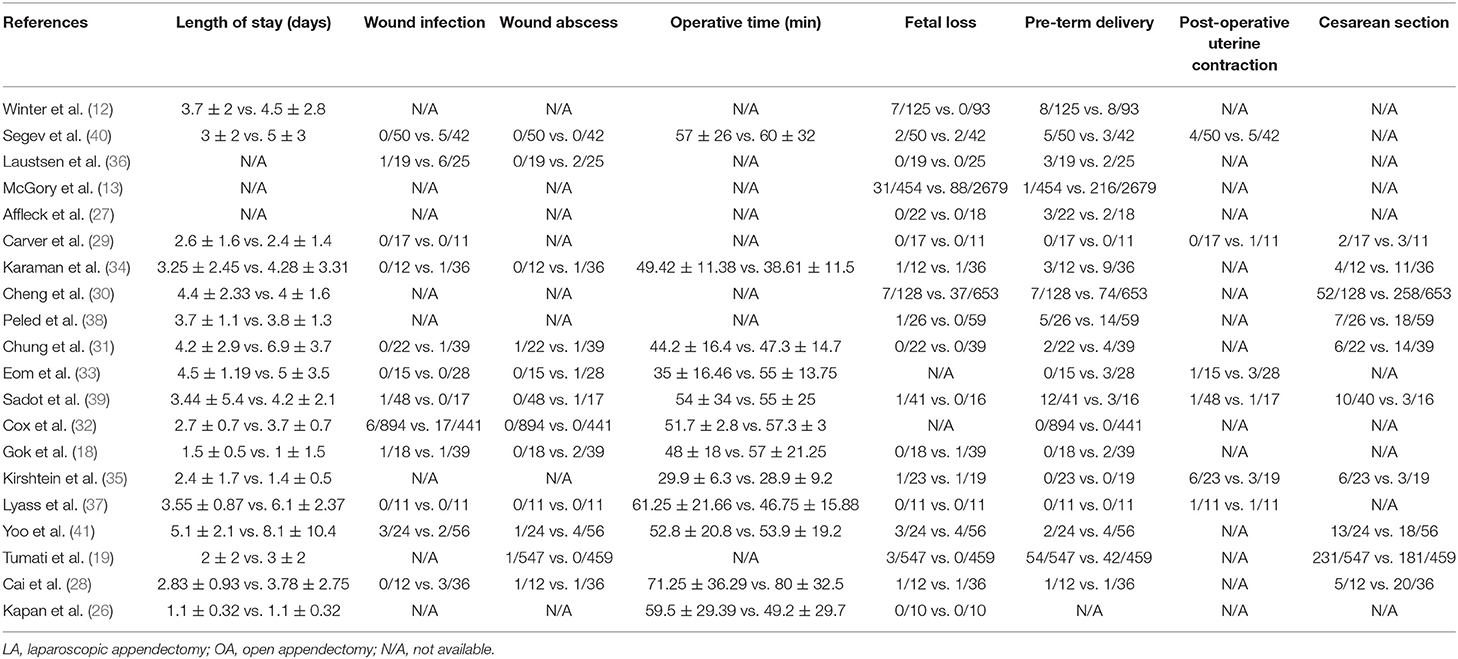
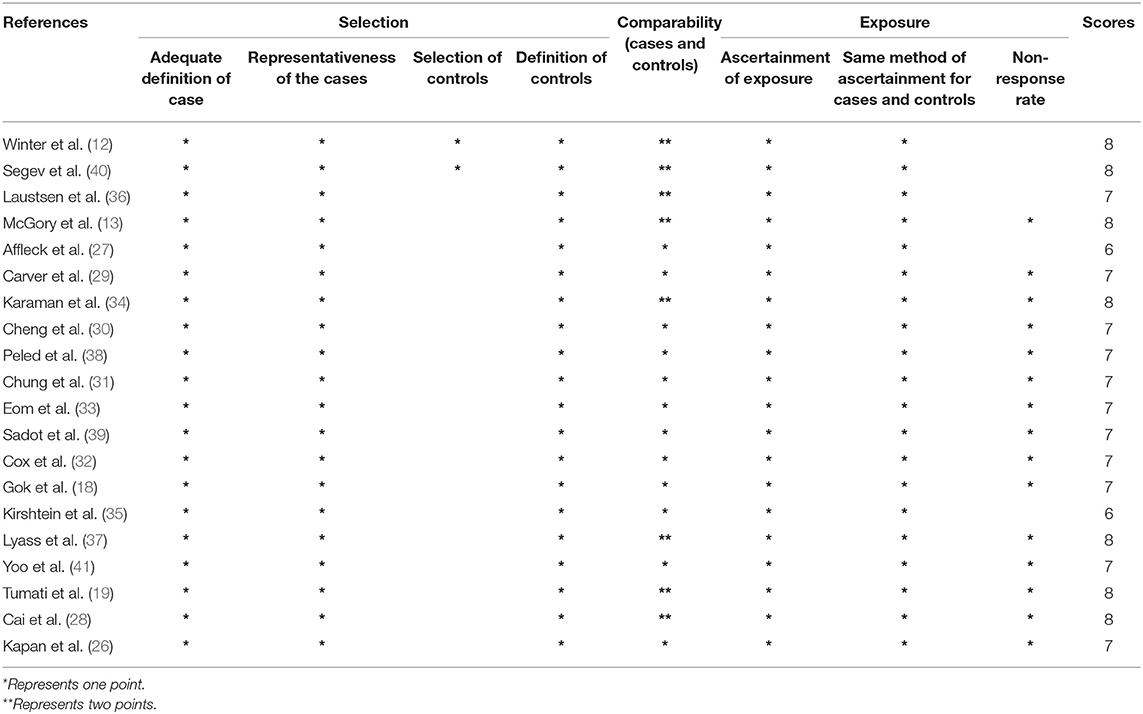
Data extraction included the following items: study and patient traits, which included the year of publication, first author, type of study, sample sizes, average age, research time, gestational age at surgery, conversion to OA, country, trimesters, pathology of appendicitis; operative and obstetrical outcomes, which included fetal loss, pre-term delivery, cesarean section, surgery time, length of stay (LOS), wound infection, abscess, and post-operative uterine contraction. The primary outcomes were fetal loss and pre-term delivery, the secondary outcomes included cesarean section, LOS, operative time, wound infection, abscess, and post-operative uterine contraction. Two reviewers (J Zhang and MY Wang) independently extracted the information using a uniform format, and if there was any ambiguity, a third observer (QB Feng) joined to reach a consensus. We utilized the Newcastle–Ottawa Scale (NOS) to comprehensively evaluate included studies as all eligible studies were retrospective (21). Every study was independently evaluated by two reviewers (J Zhang and MY Wang), and a NOS score of ≥ 6 is considered a sign of high quality.
Statistical Analysis
We used Review Manager 5.3 Software to analyze the data. The weighted mean difference (WMD) with the 95% CI and odds ratio (OR) was used to compare continuous and dichotomous variables. Studies reporting median results for continuous data were converted to mean and SD if the median range and sample volume were recorded (22). The diverse heterogeneity of the included studies was evaluated by the I2-test. If I2 < 50%, the heterogeneity was considered slight, and the fixed-effect model was wielded to perform pooled OR and WMD (23); if not, the random-effects model was used (24). The funnel plot was adopted to assess the publication bias (25). For excluding the potential influence of individual studies on the main results, we step by step exclude individual studies to analyze their impact on the overall results.
Results
Retrieved Results and Features of the Appropriate Studies
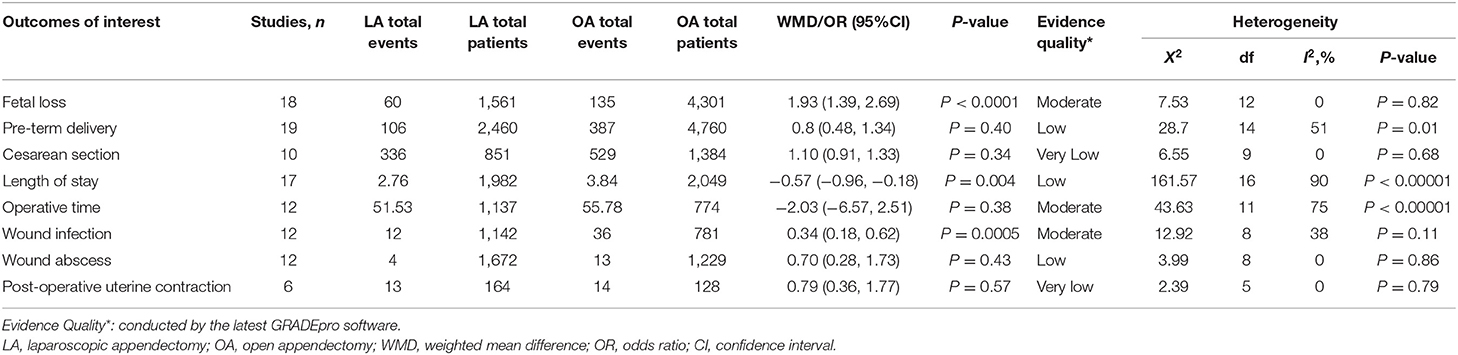
The literature retrieval outputted 1,466 correlative English publications from the multifarious electronic databases, of which 20 retrospective studies (12, 13, 18, 19, 26–41) comparing in a total of 7,248 pregnant women (2,477 and 4,771 patients underwent LA and OA, severally) were screened for farther analysis. The flow diagram of our analysis schedule is presented in Figure 1. The primary characteristics of the included 20 studies are shown in Table 1, whereas the surgical and obstetrical results of the included papers are listed in Table 2. All results of our systematic review are presented in Table 3. Meanwhile, the quality evaluation of included studies with the Newcastle Ottawa Scale is presented as a summary in Table 4.
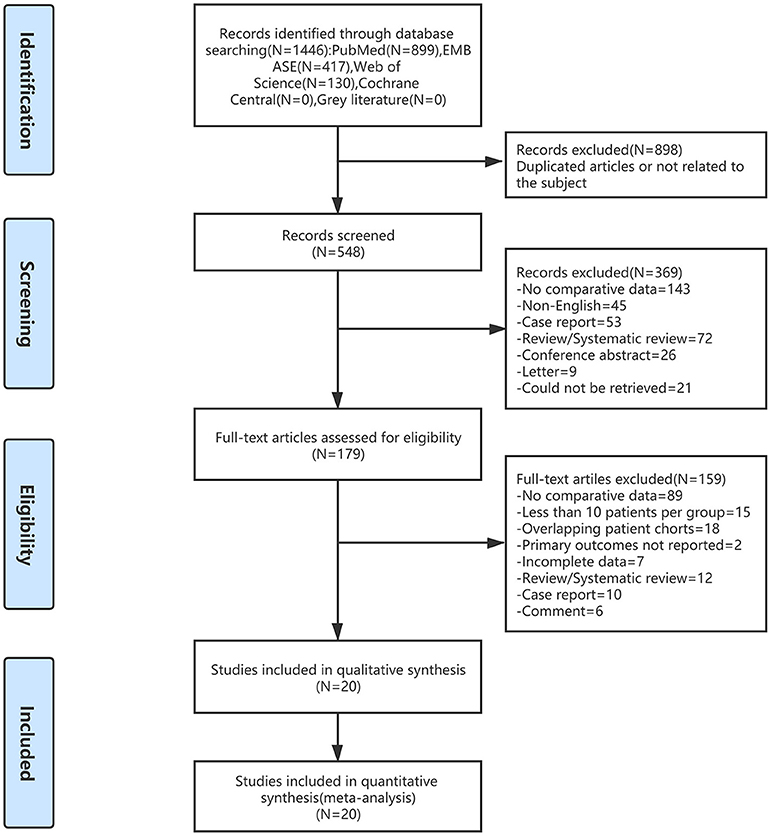
Figure 1. Flow diagram of study identification and selection. LA, laparoscopic appendectomy; OA, open appendectomy.
Meta-Analysis Outcomes
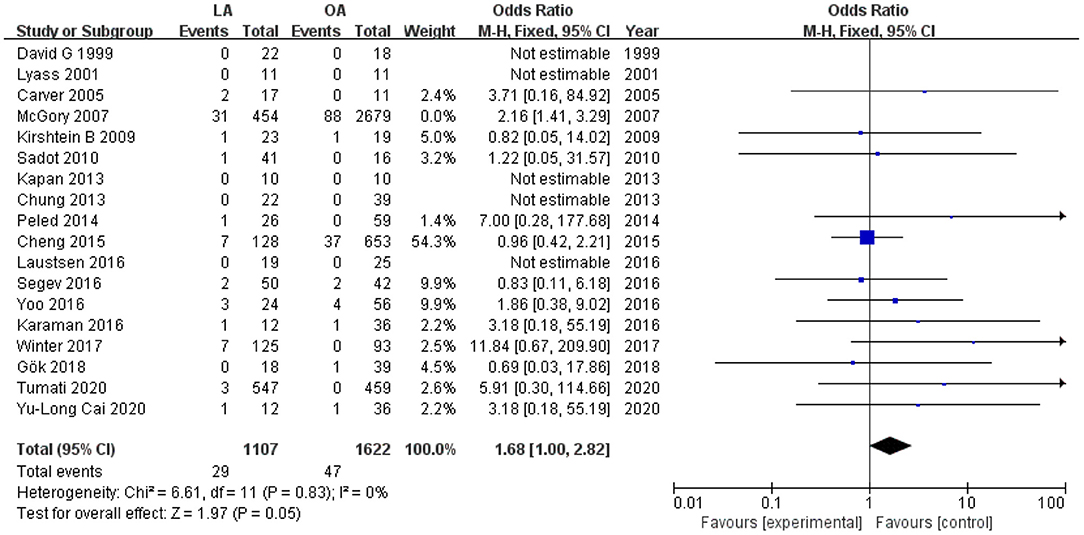
Fetal Loss
Eighteen studies (12, 13, 18, 19, 26–31, 34–41) with a total of 5,862 patients (1,561 who underwent LA and 4,301 who underwent OA) recorded fetal loss. The pooled results suggested that there were 60 (3.8%) fetal losses in the LA in contrast to 135 (3.1%) in the OA from eighteen trials (OR 1.93, 95% CI 1.39–2.69, P < 0.0001). Heterogeneity analysis showed no statistically significant difference (I2 = 0%); therefore, a fixed effects model (FEM) was applied (Figure 2A).
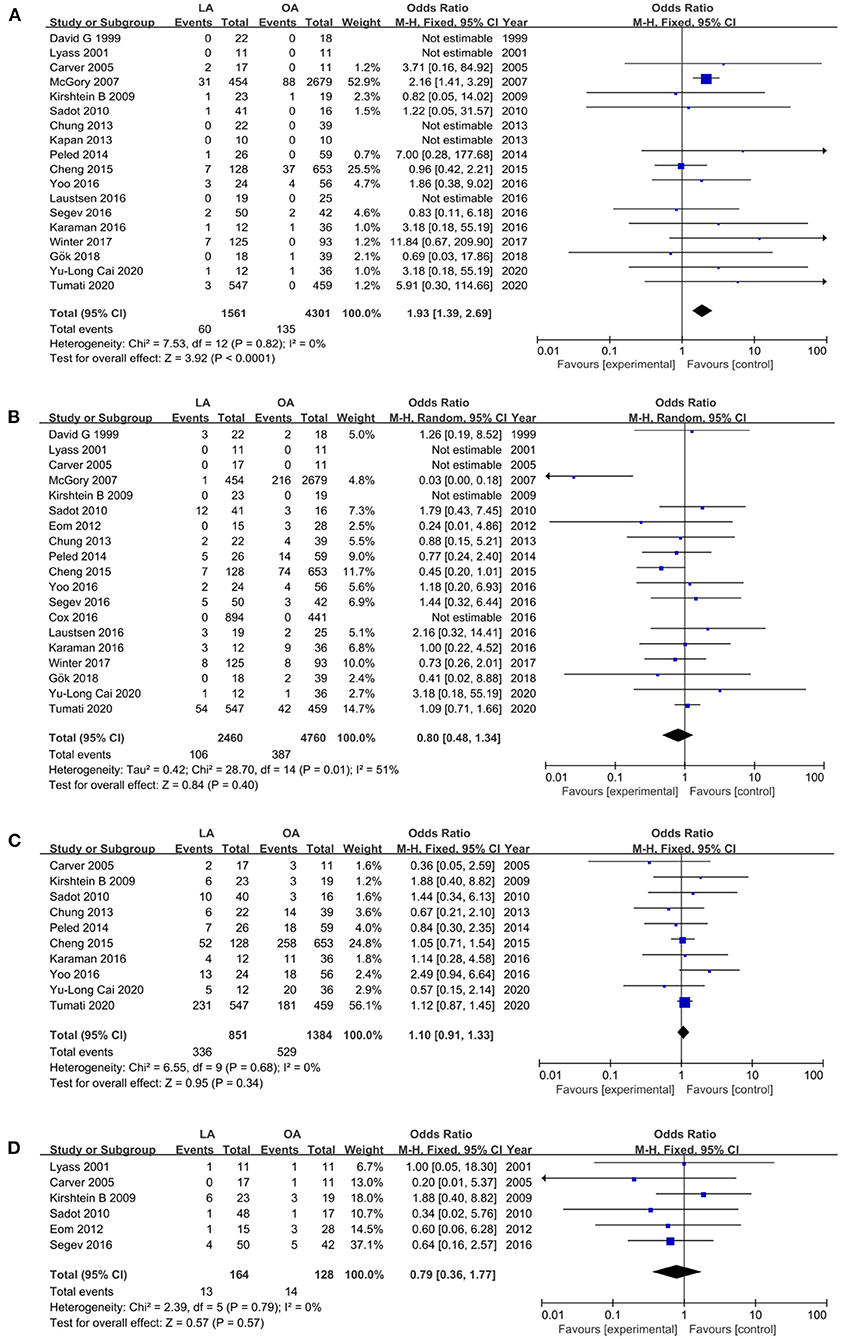
Figure 2. Forest plot of the obstetrical outcomes comparison of LA vs. OA. (A) Forest plot for fetal loss (OR 1.93, 95% CI 1.39–2.69, P < 0.0001); (B) Forest plot for pre-term delivery (OR 0.80, 95% CI 0.48–1.34, P = 0.40); (C) Forest plot for cesarean section (OR 1.10, 95% CI 0.91–1.33, P = 0.34); (D) Forest plot for post-operative uterine contraction (OR 0.79, 95% CI 0.36–1.77, p = 0.57).
Pre-term Delivery
Pre-term delivery, defined as labor before 37 gestational weeks, was assessed in 19 studies (12, 13, 18, 19, 27–41). The results suggested that there was no difference in pre-term delivery in the two groups (OR 0.80, 95% CI 0.48–1.34, P = 0.40). Heterogeneity was medium (I2 = 51%) and analyzed in a random effects model (REM) (Figure 2B).
Cesarean Section
Ten studies (19, 28–31, 34, 35, 38, 39, 41) that encompassed 2,235 patients (851 in LA and 1,384 in OA) recorded the cesarean section, and the pooled data revealed no statistical difference in cesarean section (OR 1.10, 95% CI 0.91–1.33, P = 0.34). There was no statistically significant heterogeneity (I2 = 0%) and was analyzed in FEM (Figure 2C).
Post-operative Uterine Contraction
Six trials (29, 33, 35, 37, 39, 40) reported post-operative uterine contraction, and the pooled results suggested no statistically significant difference in post-operative uterine contraction (OR 0.79, 95% CI 0.36–1.77, p = 0.57, I2 = 0%, Figure 2D).
Operative Time
Estimated operative time was assessed in 12 studies (18, 26, 28, 31–35, 37, 39–41). The pooled results showed that there was no statistical difference in operative time (MD −2.03 min, 95% CI −6.57 to 2.51, P = 0.38). Heterogeneity was high and was analyzed in the REM (I2 = 75%) (Figure 3A).
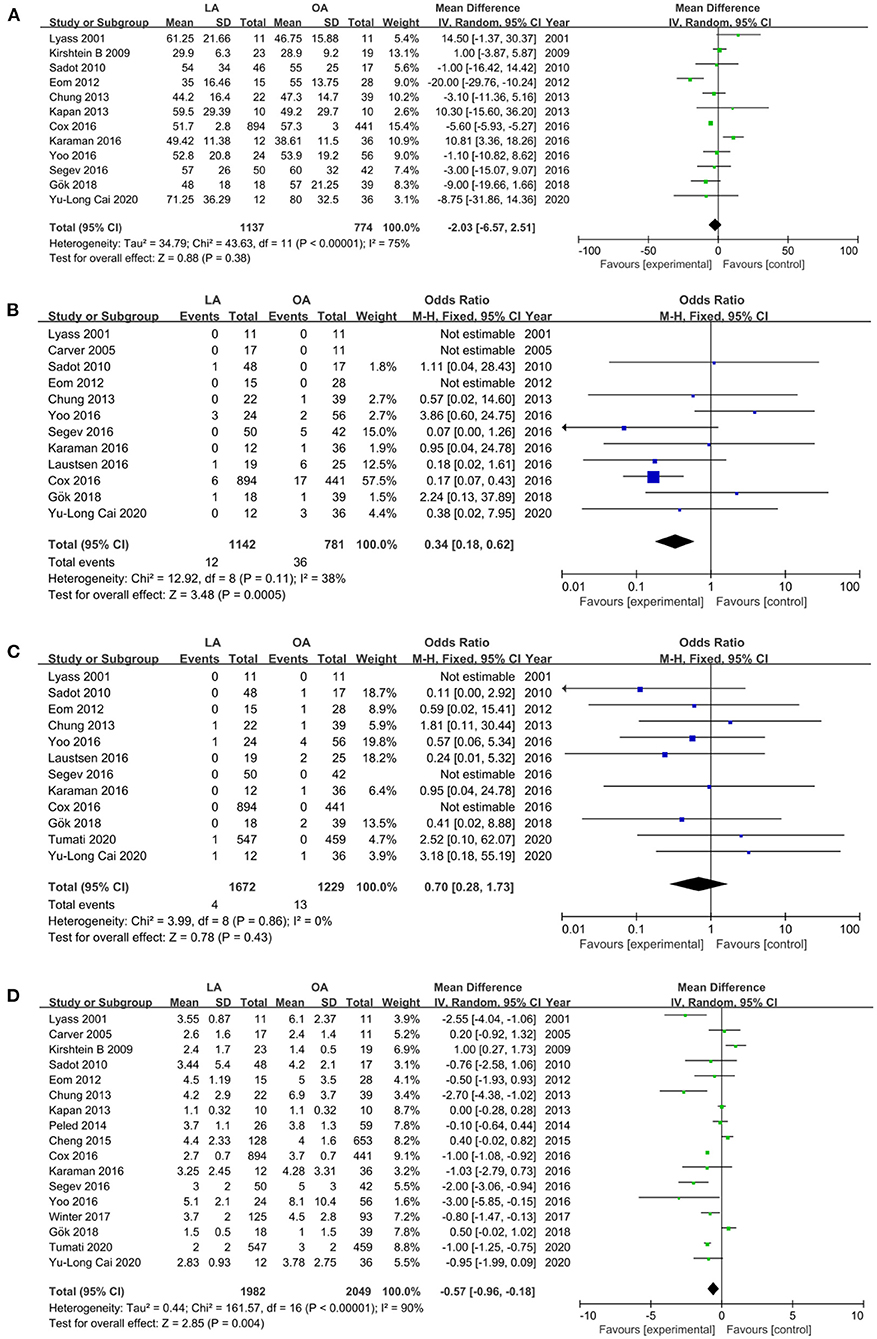
Figure 3. Forest plot of the surgical outcomes comparison of LA vs. OA. (A) Forest plot for operative time (MD −2.03 min, 95% CI −6.57 to 2.51, P = 0.38); (B) Forest plot for wound infection (OR 0.34, 95% CI 0.18– 0.62, P = 0.0005); (C) Forest plot for abscess (OR 0.70, 95% CI 0.28–1.73, p = 0.43); (D) Forest plot for LOS (MD −0.57 days, 95% CI −0.96 to −0.18, P = 0.004).
Wound Infection and Abscess
Wound infection (18, 28, 29, 31–34, 36, 37, 39–41) and abscess (18, 19, 28, 31–34, 36, 37, 39–41), two crucial perioperative outcomes, were reported in diverse 12 studies. Patients undergoing LA had lower wound infection compared with OA (OR 0.34, 95% CI 0.18–0.62, P = 0.0005, I2 = 38%, Figure 3B), whereas, there was no statistical difference in wound abscess (OR 0.70, 95% CI 0.28–1.73, p = 0.43, I2 = 0%, Figure 3C).
Length of Stay
The LOS was referred in 17 studies (12, 18, 19, 26, 28–35, 37–41) with a total of 4,031 patients (1,982 and 2,049 underwent LA and OA, respectively). The results revealed a shorter LOS in the LA (MD −0.57 days, 95% CI −0.96 to −0.18, P = 0.004) (Figure 3D). Heterogeneity was high (I2 = 90%) and analyzed in REM.
Sensitivity Analysis and Quality Assessment
The remaining parameters were not impacted after each successive exclusion of the eligible literature. All included publications had NOS scores ≥ 6, indicating a low risk of bias.
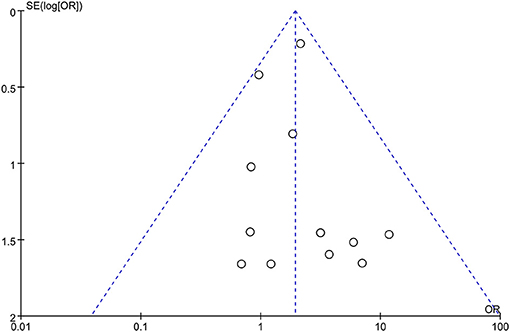
Publication Bias
Begg funnel plots were depicted for each result to estimate publication bias. All studies were within 95% CIs in the funnel plot of fetal loss (Figure 4), which suggested no obvious publication bias.
Discussion
Nowadays, there is deficient testimony to point out the optimal operation of appendicitis in pregnancy because large RCTs are difficult to conduct in pregnant women. In recent years, systematic reviews and meta-analyses also had no consensus on whether to choose LA or OA (15–17). Under such an unclear situation, further explorations for pregnant appendicitis are necessary.
This systematic review summarized the knowledge and conclusions of the current literature. In our results, LA for pregnancy appendicitis had advantages in the aspect of hospital stay and wound infection. Nevertheless, operative time and the general post-operative complications, wound abscess and post-operative uterine contractions, did not differ among LA and OA. As for obstetric outcomes, the laparoscopic operation was two times as likely to cause fetal loss as compared with OA; while pre-term delivery and cesarean section were comparable between the two operations.
The average hospital stay in the laparoscopic group was reduced by half a day, to some extent. Shorter hospital stay meant cost savings and improved patient satisfaction (42). LA had higher expenses in the terms of material cost than open appendicectomy. However, some studies had shown no obvious diversity in total hospitalization costs between the two approaches (28), reduction in hospital stay for LA might have some contribution. Compared with traditional open appendectomy, LA was a relatively rising operation, but the results of our analysis revealed that surgery time between the two operation methods was almost similar. It potentially showed the increase in experience and learning curve of laparoscopic appendectomy over the last 20 years. Laparoscopic operations had predominance in some post-operative complications such as wound infection, according to the previous experience and literatures (10, 43). This is one reason that laparoscopy is more, in general, used for treating pregnant acute appendicitis.
Fetal loss is the most devastating and frightening complication of surgical intervention for pregnancy appendicitis. In our conclusion, fetal loss in the laparoscopic group was significantly higher than OA. The pooled risk was 1.93, similar to the meta-analysis and systematic review carried out by Wilasrusmee et al. (43), in which the risk of fetal loss in LA was 1.91 times that in OA. Our study and the study by Wilasrusmee both included a large sample size study conducted by McGory et al. (13). The patient-volume of this study accounted for about 40% of our analysis. When excluded it from the included studies, Wilasrusmee et al. considered that there was no association between surgical methods and fetal loss. However, our results showed that the risk of fetal loss in LA was 1.68 times higher than that in OA after the above-mentioned large sample study was removed (p = 0.05, Figure 5). Although p = 0.05, the OR value still reminded us of a trend that laparoscopic appendectomy was linked with a higher risk and possibility of fetal loss. With the progress from simple to complicated appendicitis, which meant the increase of infection, the risk of fetal death and maternal morbidity showed an increasing trend (6). Complicated appendicitis was defined as suppurative, perforated, gangrenous appendicitis, or combined peritonitis appendicitis. We analyzed the distribution of complicated appendicitis between LA and OA groups (OR 0.69, 95% CI 0.59–0.81, p < 0.00001, Supplementary Figure 1), suggesting that complicated appendicitis in the LA group was significantly less than in the OA group. In the case of mild appendicitis infection, there was still a higher rate of fetal loss for laparoscopic appendectomy, highlighting the correlation between fetal loss and laparoscopy itself.
Therefore, it is quite necessary for patients and doctors to fully evaluate the risk of fetal loss associated with LA. Perioperative and operational management should be enhanced and executed by a multidisciplinary team. In addition to skilled and prudent operation, the signing of informed consent is also very significant. The increase of fetal loss during LA may be closely related to ascending intraperitoneal pressure and fetal carbon dioxide acidosis caused by CO2 pneumoperitoneum (44). The potential harm to the pregnant uterus during trocar passage and operation also possibly led to abortion (37, 45). Increasing abdominal pressure along with Trendelenburg's position also had the potential risk of affecting the infant by leading to maternal hypercapnia and hypoxemia (46). Pneumoperitoneum status for individual study, including the magnitudes of intraabdominal pressure and the types of pneumoperitoneum, are presented in Supplementary Table 1. Almost all included studies mentioned that laparoscopic appendectomy was performed in pneumoperitoneum circumstances. Ten studies explicitly stated that the pneumoperitoneum was produced by CO2, and nine of them showed the specific range of intraabdominal pressure, all of which ranged from 10 to 15 mmHg. Recent SAGES guidelines inclined to 10–15 mmHg CO2 injection as a relatively safe procedure for laparoscopy in pregnant patients (8). Controlling the pressure and gas may be a feasible way to reduce the probability of fetal loss; however, large-scale and well-designed studies were required to demonstrate this perspective.
Post-operative uterine contraction, correlated with pre-term delivery, is one of the common complications after appendicectomy for pregnant women. In our results, pre-term delivery and post-operative uterine contraction were both fairly comparable among the two operations, which might illustrate that there was no noteworthy correlation between surgical methods and these two indicators.
Calculating the overall rate of pre-term delivery in all 20 studies (R = 54 + 42/547 + 459 * 100% = 9.5%), we found it was almost similar to the global incidence of pre-term birth (47). Spontaneous abortion accounted for 10–20% of all pregnancies worldwide. However, the fetal loss among all pregnancy appendicitis in our systematic review was much lower, at about 3.3%. This might be because the fetal loss in this study was only related to surgical and infectious factors, whereas spontaneous abortion in the world was related to various factors such as genes, endocrine, immunity, and environment.
To avoid data loss and the influence of unnecessary confounding factors, two authors independently searched the literature. Meanwhile, setting the criteria that study < 10 patients per group and studies that appendectomy was mixed with other operations and could not be differentiated were excluded. Even so, there were many inherent limitations in the present analysis. First, all the 20 including trials were retrospective studies, implying inevitable follow-up bias and selective bias. Second, the time interval of the included literature was quite long (20 years), and the management philosophy of pregnant appendicitis patients evolved over time. In addition, the comparability between our present research and the anterior study by Wilasrumsee et al. seemed to be another limitation. Third, for third-trimester patients, doctors and patients were more inclined to choose open appendectomy, as the insertion and operation of laparoscopic devices could cause damage to the enlarged uterus (40). Our review also showed that the gestational age at surgery in the open group was significantly higher than laparoscopy (MD = −3.31, 95% CI −4.27 to −2.35; P < 0.00001, Supplementary Figure 2). Therefore, the distribution of trimesters in the two groups potentially generated bias between them. In addition, the weights and pre-existing abdominal incisions of the patient, the choice of surgeons, and their experience were all likely to affect the final procedure. The included studies did not provide outcomes in different trimesters, impeding to get definitive results of the optimal and feasible surgical procedure in the three diverse trimesters (Table 1). Fourth, in the included studies, there were cases where LA was converted to open; about 11 out of the 2,477 patients of LA were transformed to OA. Six, nearly half of the 11 cases, were still classified as LA. Those transformations have possibly taken confounders to the outcomes. When we retrieved databases, we found vast clinical studies about laparoscopic appendectomy for pregnant appendicitis, partly reflecting that LA has widely been used in clinical practice. The applicability and feasibility of LA could be naturally interpreted to some degree.
Conclusion
Laparoscopic appendectomy is safe in experienced hands, with the admitted advantages of minimally invasive surgery, especially in hospital stays and the common post-operative complications. However, the obvious increase in fetal loss compared with OA should never be ignored. All in all, laparoscopic appendectomy should be undertaken by a comprehensive team, and it is essential for patients to be thoroughly informed about the merits and demerits of the available surgical methods. Further, larger-scale and well-designed studies are demanded to elucidate the reasons for the high incidence of fetal loss after laparoscopic appendectomy.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author Contributions
JZ: data collection, data analysis, and writing. QF: study design and modification. PL: data collection. MW: make form. ZX: data collection and make form. All authors contributed to the article and approved the submitted version.
Funding
Model research and application demonstration of hierarchical coordination within health alliance based on a cloud platform (Project No.: 2020YFS0092).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2021.720351/full#supplementary-material
Supplementary Figure 1. Forest plot for the distribution of complicated appendicitis between LA and OA groups.
Supplementary Figure 2. Forest plot for the gestational age at the surgery between LA and OA groups.
Supplementary Table 1. Pneumoperitoneum status of included studies.
Appendix. The particular search strategy.
References
1. Zingone F, Sultan AA, Humes DJ, West J. Risk of acute appendicitis in and around pregnancy: a population-based cohort study from England. Ann Surg. (2015) 261:332–7. doi: 10.1097/SLA.0000000000000780
2. Nakashima M, Takeuchi M, Kawakami K. Clinical outcomes of acute appendicitis during pregnancy: conservative management and appendectomy. World J Surg. (2021) 45:1717–24. doi: 10.1007/s00268-021-06010-w
3. Gilo NB, Amini D, Landy HJ. Appendicitis and cholecystitis in pregnancy. Clin Obstet Gynecol Dec. (2009) 52:586–96. doi: 10.1097/GRF.0b013e3181c11d10
4. Freeland M, King E, Safcsak K, Durham R. Diagnosis of appendicitis in pregnancy. Am J Surg Dec. (2009) 198:753–8. doi: 10.1016/j.amjsurg.2009.05.023
5. Pastore PA, Loomis DM, Sauret J. Appendicitis in pregnancy. J Am Board Fam Med Nov-Dec. (2006) 19:621–6. doi: 10.3122/jabfm.19.6.621
6. Yilmaz HG, Akgun Y, Bac B, Celik Y. Acute appendicitis in pregnancy–risk factors associated with principal outcomes: a case control study. Int J Surg Jun. (2007) 5:192–7. doi: 10.1016/j.ijsu.2006.05.005
7. Ball E, Waters N, Cooper N, Talati C, Mallick R, Rabas S, et al. Evidence-based guideline on laparoscopy in pregnancy commissioned by the british society for gynaecological endoscopy (BSGE) endorsed by the royal college of obstetricians & gynaecologists (RCOG). Facts Views Vis Obgyn. (2019) 11:5–25.
8. Pearl JP, Price RR, Tonkin AE, Richardson WS, Stefanidis D. SAGES guidelines for the use of laparoscopy during pregnancy. Surg Endosc Jun. (2017) 31:3767–82. doi: 10.1007/s00464-017-5637-3
9. Frazee RC, Roberts JW, Symmonds RE, Snyder SK, Hendricks JC, Smith RW, et al. A prospective randomized trial comparing open versus laparoscopic appendectomy. Ann Surg. (1994) 219:725–8; discussion 728–31. doi: 10.1097/00000658-199406000-00017
10. Yaghoubian A, Kaji AH, Lee SL. Laparoscopic versus open appendectomy: outcomes analysis. Am Surg Oct. (2012) 78:1083–6. doi: 10.1177/000313481207801016
11. Korndorffer JR, Fellinger E, Reed W. SAGES guideline for laparoscopic appendectomy. Surg Endosc Apr. (2010) 24:757–61. doi: 10.1007/s00464-009-0632-y
12. Winter NN, Guest GD, Bozin M, Thomson BN, Mann GB, Tan SBM, et al. Laparoscopic or open appendicectomy for suspected appendicitis in pregnancy and evaluation of foetal outcome in Australia. ANZ J Surg May. (2017) 87:334–8. doi: 10.1111/ans.13750
13. McGory ML, Zingmond DS, Tillou A, Hiatt JR, Ko CY, Cryer HM. Negative appendectomy in pregnant women is associated with a substantial risk of fetal loss. J Am Coll Surg Oct. (2007) 205:534–40. doi: 10.1016/j.jamcollsurg.2007.05.025
14. Reedy MB, Kallen B, Kuehl TJ. Laparoscopy during pregnancy: a study of five fetal outcome parameters with use of the Swedish Health Registry. Am J Obstet Gynecol Sep. (1997) 177:673–9. doi: 10.1016/S0002-9378(97)70163-7
15. Chakraborty J, Kong JC, Su WK, Gourlas P, Gillespie C, Slack T, et al. Safety of laparoscopic appendicectomy during pregnancy: a systematic review and meta-analysis. ANZ J Surg Oct. (2019) 89:1373–8. doi: 10.1111/ans.14963
16. Prodromidou A, Machairas N, Kostakis ID, Molmenti E, Spartalis E, Kakkos A, et al. Outcomes after open and laparoscopic appendectomy during pregnancy: a meta-analysis. Eur J Obstet Gynecol Reprod Biol. (2018) 225:1–31. doi: 10.1016/j.ejogrb.2018.04.010
17. Lee SH, Lee JY, Choi YY, Lee JG. Laparoscopic appendectomy versus open appendectomy for suspected appendicitis during pregnancy: a systematic review and updated meta-analysis. BMC Surg. (2019) 19:41–53. doi: 10.1186/s12893-019-0505-9
18. Gok AFK, Soydas Y, Bayraktar A, Emirikçi S, Ilhan M, Koltka AK, et al. Laparoscopic versus open appendectomy in pregnancy: a single center experience. Ulus Travma Acil Cerrahi Derg. (2018) 24:552–6. doi: 10.5505/tjtes.2018.26357
19. Tumati A, Yang J, Zhang X, Su J, Ward CA, Hong J, et al. Pregnant patients requiring appendectomy: comparison between open and laparoscopic approaches in NY State. Surg Endosc. (2021) 35:4681–90. doi: 10.1007/s00464-020-07911-y
20. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol Oct. (2009) 62:e1–34. doi: 10.1016/j.jclinepi.2009.06.006
21. Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers' to authors' assessments. BMC Med Res Methodol. (2014) 14:45. doi: 10.1186/1471-2288-14-45
22. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. (2005) 5:13. doi: 10.1186/1471-2288-5-13
23. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. (1986) 7:177–88. doi: 10.1016/0197-2456(86)90046-2
24. DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. (2007) 28:105–14. doi: 10.1016/j.cct.2006.04.004
25. Souza JP, Pileggi C, Cecatti JG. Assessment of funnel plot asymmetry and publication bias in reproductive health meta-analyses: an analytic survey. Reprod Health. (2007) 4:3. doi: 10.1186/1742-4755-4-3
26. Kapan S, Bozkurt MA, Turhan AN, Gönenç M, Aliş H. Management of acute appendicitis in pregnancy. Ulus Travma Acil Cerrahi Derg. (2013) 19:20–4. doi: 10.5505/tjtes.2013.81889
27. Affleck DG, Handrahan DL, Egger MJ, Price RR. The laparoscopic management of appendicitis and cholelithiasis during pregnancy. Am J Surg. (1999) 178:523–9. doi: 10.1016/S0002-9610(99)00244-5
28. Cai YL, Yang SS, Peng DZ, Jia QB, Li FY, Ye H, et al. Laparoscopic appendectomy is safe and feasible in pregnant women during second trimester: a retrospective study in a top-level Chinese center. Medicine (Baltimore). (2020) 99:e21801. doi: 10.1097/MD.0000000000021801
29. Carver TW, Antevil J, Egan JC, Brown CV. Appendectomy during early pregnancy: what is the preferred surgical approach? Am Surg. (2005) 71:809–12. doi: 10.1177/000313480507101002
30. Cheng HT, Wang YC, Lo HC, Su LT, Soh KS, Tzeng CW, et al. Laparoscopic appendectomy versus open appendectomy in pregnancy: a population-based analysis of maternal outcome. Surg Endosc. (2015) 29:1394–9. doi: 10.1007/s00464-014-3810-5
31. Chung JC, Cho GS, Shin EJ, Kim HC, Song OP. Clinical outcomes compared between laparoscopic and open appendectomy in pregnant women. Can J Surgt. (2013) 56:341–6. doi: 10.1503/cjs.022112
32. Cox TC, Huntington CR, Blair LJ, Prasad T, Lincourt AE, Augenstein VA, et al. Laparoscopic appendectomy and cholecystectomy versus open: a study in 1999 pregnant patients. Surg Endosc. (2016) 30:593–602. doi: 10.1007/s00464-015-4244-4
33. Eom JM, Hong JH, Jeon SW, Choi JS, Lee JH, Kim HO, et al. Safety and clinical efficacy of laparoscopic appendectomy for pregnant women with acute appendicitis. Ann Acad Med Singap. (2012) 41:82–6.
34. Karaman E, Aras A, Cim N, Kolusari A, Kiziltan R, Çelik S, et al. Maternal and fetal outcomes after laparoscopic vs. Open appendectomy in pregnant women: data from two tertiary referral centers. Ginekol Pol. (2016) 87:98–103. doi: 10.17772/gp/58752
35. Kirshtein B, Perry ZH, Avinoach E, Mizrahi S, Lantsberg L. Safety of laparoscopic appendectomy during pregnancy. World J Surg Mar. (2009) 33:475–80. doi: 10.1007/s00268-008-9890-4
36. Laustsen JF, Bjerring OS, Johannessen Ø, Qvist N. Laparoscopic appendectomy during pregnancy is safe for both the mother and the fetus. Dan Med J. (2016) 63:A5259.
37. Lyass S, Pikarsky A, Eisenberg VH, Elchalal U, Schenker JG, Reissman P. Is laparoscopic appendectomy safe in pregnant women? Surg Endosc. (2001) 15:377–9. doi: 10.1007/s004640000368
38. Peled Y, Hiersch L, Khalpari O, Wiznitzer A, Yogev Y, Pardo J. Appendectomy during pregnancy–is pregnancy outcome depending by operation technique? J Matern Fetal Neonatal Med. (2014) 27:365–7. doi: 10.3109/14767058.2013.818131
39. Sadot E, Telem DA, Arora M, Butala P, Nguyen SQ, Divino CM. Laparoscopy: a safe approach to appendicitis during pregnancy. Surg Endosc. (2010) 24:383–9. doi: 10.1007/s00464-009-0571-7
40. Segev L, Segev Y, Rayman S, Shapiro R, Nissan A, Sadot E. Appendectomy in pregnancy: appraisal of the minimally invasive approach. J Laparoendosc Adv Surg Tech A. (2016) 26:893–7. doi: 10.1089/lap.2016.0280
41. Yoo KC, Park JH, Pak KH, Kim KY, Lee BH, Kim BC, et al. Could laparoscopic appendectomy in pregnant women affect obstetric outcomes? A multicenter study. Int J Colorectal Dis. (2016) 31:1475–81. doi: 10.1007/s00384-016-2584-8
42. Ball CG, Kortbeek JB, Kirkpatrick AW, Mitchell P. Laparoscopic appendectomy for complicated appendicitis: an evaluation of postoperative factors. Surg Endosc. (2004) 18:969–73. doi: 10.1007/s00464-003-8262-2
43. Wilasrusmee C, Sukrat B, McEvoy M, Attia J, Thakkinstian A. Systematic review and meta-analysis of safety of laparoscopic versus open appendicectomy for suspected appendicitis in pregnancy. Br J Surg. (2012) 99:1470–8. doi: 10.1002/bjs.8889
44. Hunter JG, Swanstrom L, Thornburg K. Carbon dioxide pneumoperitoneum induces fetal acidosis in a pregnant ewe model. Surg Endosc. (1995) 9:272–7; discussion 277–9. doi: 10.1007/BF00187767
45. Moreno-Sanz C, Pacual-Pedreno A, Picazo-Yeste JS, Seoane-Gonzalez JB. Laparoscopic appendectomy during pregnancy: between personal experiences and scientific evidence. J Am Coll Surg. (2007) 205:37–42. doi: 10.1016/j.jamcollsurg.2007.01.068
46. O'Rourke N, Kodali BS. Laparoscopic surgery during pregnancy. Curr Opin Anaesthesiol. (2006) 19:254–9. doi: 10.1097/01.aco.0000192817.30612.b3
Keywords: appendicitis, laparoscopic appendectomy, open appendectomy, pregnant, fetal loss
Citation: Zhang J, Wang M, Xin Z, Li P and Feng Q (2021) Updated Evaluation of Laparoscopic vs. Open Appendicectomy During Pregnancy: A Systematic Review and Meta-Analysis. Front. Surg. 8:720351. doi: 10.3389/fsurg.2021.720351
Received: 04 June 2021; Accepted: 16 August 2021;
Published: 23 September 2021.
Edited by:
Gabriel Sandblom, Karolinska Institutet (KI), SwedenReviewed by:
Shang Yu Wang, Linkou Chang Gung Memorial Hospital, TaiwanPelle Lindqvist, Karolinska Institutet (KI), Sweden
Baris Mantoglu, Sakarya Egitim ve Araştirma Hastanesi, Turkey
Copyright © 2021 Zhang, Wang, Xin, Li and Feng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qingbo Feng, ZnFiOTE3NWRvY0AxNjMuY29t
†These authors have contributed equally to this work
 Jia Zhang
Jia Zhang Miye Wang2,3†
Miye Wang2,3† Zechang Xin
Zechang Xin Qingbo Feng
Qingbo Feng