Abstract
Background:
We conducted this cohort study to assess the differences in the learning curve of bipolar transurethral plasma enucleation of the prostate (B-TUEP) associated with prostatic peripheral zone thickness (PZT) under MRI quantitative measurements.
Methods:
For the study, 60 patients with benign prostatic hyperplasia (BPH) were involved. PZT are defined as “Thin” (<7 mm), “Thick” (>10 mm), and “Medium” (in between), with 20 patients in each group. Learning stages were defined as Group 1 (No. 1–20), Group 2 (No. 21–40), and Group 3 (No. 41–60). We measured parameters of the prostate, such as PZT and transitional zone thickness (TZT), with MRI. A learner with no experience in enucleation performed the operations. Statistical analyses were performed to compare the differences. Pearson correlation analysis and multiple linear regression analysis evaluated the relationship between characteristics of patients. P < 0.05 was deemed statistically significant.
Results:
One-Way ANOVA revealed different enucleation efficiency (0.811 ± 0.18 vs. 0.748 ± 0.14 vs. 0.634 ± 0.16), prostate volume (58.9 ± 15.33 vs. 57.3 ± 15.58 vs. 46.6 ± 14.10), and thickness of transition zone (44.45 ± 7.60 vs. 42.45 ± 6.08 vs. 34.78 ± 6.04) among Thin, Medium, and Thick groups. The enucleation efficiency is different between groups divided by learning stages (Group 1 vs. Group 3, 0.658 vs. 0.783; Group 2 vs. Group 3, 0.751 vs. 0.783). Pearson correlation analysis reveals that PZT was negatively correlated with prostate volume (r = −0.427), resection weight (r = −0.35), enucleation efficiency (r = −0.445), and TZT (r = −0.533), and was positively correlated with Q-max (r = 0.301) and bladder outlet obstruction index (BOOI) (r = 0.388). The regression coefficients of PZT, TZT, prostate volume, and Q-max were −0.012, 0.008, 0.007, and 0.013, respectively (all P < 0.05).
Conclusion:
Lower PZT is independent of higher enucleation efficiency, larger adenoma, and higher TZT. PZT may be an important factor on the learning curve of B-TUEP. Higher TZT, prostate volume. and Q-max may also relate to higher enucleation efficiency. For B-TUEP learners, it seems easier to perform the operation when the PZT is low, though more care should be taken with the capsule perforation. Further, the capsule plane should be maintained more attentively if the PZT is high.
Introduction
Benign prostatic hyperplasia (BPH), as a disease which progresses with age, is one of the most important factors of lower urinary tract symptom (LUTS) in elderly men (1, 2). Anatomical endoscopic enucleation of the prostate (AEEP) is a popular technique for the surgical intervention of severe BPH, and has been widely accepted and recommended by many urologists (3). Less blood loss, shorter postoperative hematuria time, less diluted hyponatremia, and higher prostate adenoma removal rate are considered as significant advantages of this technique (4–6). At present, BPH is thought to be caused by hyperplasia of the transitional zone (7), which makes the adenoma of the transitional zone more circular under pressure (8). At the same time, the peripheral zone becomes thinner and forms the anatomical level of enucleation technology (9, 10). However, AEEP is considered to have a certain learning curve because of the requirement of higher operation skills (3, 11).
In order to help surgeons get through the learning curve more quickly, our center has run courses on bipolar plasma transurethral enucleation of prostate (B-TUEP) for urologists from other centers. We found that some characteristics may affect the efficiency of mastering this technique during teaching. On the other hand, our surgeons with enough experience in B-TUEP noticed that patients with thinner prostate peripheral zones seem to have a clearer capsule plane during AEEP procedure, which seems to be more beneficial to learners. Thus, we conducted a cohort study to assess the differences in the learning curve of B-TURP associated with different prostatic PZT, attempting to provide a theoretical basis for suitable patient selection.
Patients and Methods
Study Design
Sixty men diagnosed with BPH were designed to be included, and were numbered 1–60 according to the sequence of receiving operations. All of the patients were admitted because of severe LUTS, severe hematuria, bladder calculus formation, or refractory urinary retention. Exclusion criteria was a diagnosis or history of prostate cancer, prior prostate surgery, urethral strictures, and neurogenic bladder. We also excluded patients who had developed acute prostatitis within the last 6 months and whose prostate volumes were over 90 ml, because we considered that these situations would create serious difficulty for beginners. All the patients stopped their anticoagulation and antiplatelet medicine and received subcutaneous low-molecular heparin until 12 h before surgery, because their factors have been proven to increase hospital stay and complications (12). The preoperative evaluation of patients included serum prostate specific antigen (PSA), f-PSA, urine analysis, ultrasound, and prostatic multi-parameter 3.0MRI. Ultrasound-guided transrectal prostate biopsies were performed on patients suspected of prostate cancer due to elevated PSA, results of digital rectal examination, or imaging examination. Subjective and objective micturition parameters include preoperative international prostate symptom score (IPSS), quality of life score (Qol), Q-max, voiding detrusor pressure at Q-max, bladder outlet obstruction index (BOOI), and post-voiding residual volume (PVRV). Q-max, voiding detrusor pressure at Q-max, and BOOI were measured with urodynamic examination. PVRV was measured with ultrasound. All patients provided written informed consent. The study protocol was approved by the Institutional Review Board of our hospital in compliance with the Declaration of Helsinki. The length, width, and height of the prostate were measured by a radiologist using MRI, and the prostate volume was estimated by the widely accepted prostate volume calculation formula (prostate volume = length * width * height *π/6). According to the description of Kwon et al. (1), peripheral zone thickness (PZT) is defined as the longest distance between the outer and inner edge of the peripheral zone when a straight line is drawn from the center of the transitional zone to the outer edge of the peripheral zone on the level of the largest transitional zone. Transition zone thickness (TZT) is the maximum straight distance between the two edges of the transition zone passing through the center. We measured the thickness bilaterally and took the average values as PZT and TZT, respectively.
We defined PZT <7 mm as “Thin,” over 10 mm as “Thick,” and the thickness between them as “Medium.” Patients were included in these groups according to different thicknesses, until we got 20 cases in each group. In addition, the No.1–20, 21–40, and 41–60 patients in the sequence of receiving surgery were divided into Group 1, Group 2, and Group 3, respectively, which represented different learning stages.
The enucleation time refers to time from the first incision to enucleation of the entire adenoma and complete hemostasis, which demands the condition of no active hemorrhage without fluid perfusion. According to Netsch et al. (13), the enucleation efficiency is defined as the resected weight/enucleation time (g/min). All surgeries were performed by one resident surgeon (surgeon A), who has completed more than 1 year's training in transurethral endoscopy in our hospital. However, he lacked experience in AEEP surgery, and has only performed resection and coagulation after enucleation performed by other surgeons in about 30 cases of B-TUEP. Surgeon B, who is the tutor of surgeon A, is experienced, and has performed more than 1,000 cases of B-TUEP. By watching surgeon B's operations and surgery videos, as well as discussing and consulting with surgeon B, surgeon A gained enough theoretical basis. Surgeon A had performed 10 B-TUEP operations with the help of surgeon B before. These 10 patients were excluded from the research.
The operation was performed with a bipolar plasma kinetic system, using 28Fr bipolar resectoscope and electrode loop. The PK system used 160W for cutting and 80W for coagulation. Normal saline was used as irrigation fluid. The operation was performed according to Liu et al.'s (14) report. Anatomical marks such as verumontanum, prostate, external urethral sphincter, and bilateral ureteral orifice were identified before beginning. A “λ”-shape incision was made close to the verumontanum to expose the surgical capsule. The adenoma was pushed from 6:00 position to both sides to form a transverse groove in the capsule plane. From 6:00 position in the groove, the adenoma was pried upward to the 12:00 direction while the plane was extended to both sides until the endoscope broke through at the bladder neck. The middle lobe was then nearly enucleated. The bilateral lobes of adenoma were then detached clockwise or counter-clockwise from 5:00 or 7:00 position of the apex until reaching the 12:00 position at bladder neck in a spiral manner. Then the adenoma was pushed toward the midline to separate adhesion from the bladder neck. After that, we could see the residual urethral mucosa connected to the prostatic apex at 12:00 position, which might contain parts of the external urethral sphincter. Then a horizontal incision was made as close as possible to the adenoma at the apex to keep more urethral mucosa. Then the capsule was fully enucleated except for a little fixation at 5:00 position, which was convenient for morcellation with electrode loop. During the whole operation, if bleeding or obvious blood vessels were seen, electrocoagulation was started to stop or prevent bleeding immediately. If the surgical field was not clear, it was first considered if there were bleeding points in or out of the visible field, or factors affecting irrigation. The resected tissue was fully flushed out and weighed. After meticulous hemostasis, a 20Fr three-lumen silicone catheter was indwelled.
Statistical Analysis
Statistical analysis was performed using the statistical software program SPSS (IBM SPSS Statistics 25.0, Chicago, USA). P-P diagram, Q-Q diagram, histogram, and K-S test were used to identify normality of variables. Some variables with partial skewness distribution were transformed to normal distribution after natural logarithmic transformation. Continuous variables with normal distribution are described with mean ± standard deviation (SD). Differences in continuous variables between groups were analyzed via One-Way ANOVA. Post-hoc Multiple Comparisons were carried out by the LSD method. The variables with skew distribution are described with median (interquartile distance), whose comparison between groups and ordered variable are analyzed with Kruskal-Wallis H's test. Correlation analysis of continuous variables was performed by Pearson correlation analysis. A multiple linear regression analysis with stepwise selection of the variables was performed to quantify the relative contribution R2 of these parameters (IPP, sequence of receiving operation, PSA, f-PSA, PSAD, Q-max, PVRV, IPSS-T, IPSS-S, IPSS-V, Qol, voiding detrusor pressure at Q-max, BOOI, BMI, age, prostate volume, TZT, and PZT) to the variance of the dependent variable (enucleation efficiency). A stepwise approach was selected, integrating independent parameters sequentially. Collinearity was tested with the variance inflation factor (VIF). VIF > 5 indicated existence of collinearity. Durbin-Watson value close to 2 indicates that there is no autocorrelation in the model and no correlation between sample data. A significance level of P < 0.05 was deemed statistically significant.
Results
All sixty patients went through operations successfully, without conversion to open surgery or traditional transurethral resection of prostate (TURP) and perioperative death. None of the patients developed severe post-operation dilutional hyponatremia. Fifty-three patients had their catheters removed successfully 3 days after surgery, while the other seven patients developed urinary retention and were catheterized again until 1 week after operation. Twelve patients developed mild stress urinary incontinence for a short time (<1 month) after surgery; moreover, all of them developed no or little leakage on the 3-month follow-up. Two patients suffered from hematuria after discharge that may be due to constipation, and one patient got successful hemostasis after re-catheterization and continuous bladder irrigation. One patient developed bladder tamponade, which required blood clots evacuation and electrocoagulation to stop the bleeding, but no blood transfusion was required. The general trends of efficiency of enucleation are elevation with the gradual study, which is higher in the Thin group (Figure 1).
Figure 1
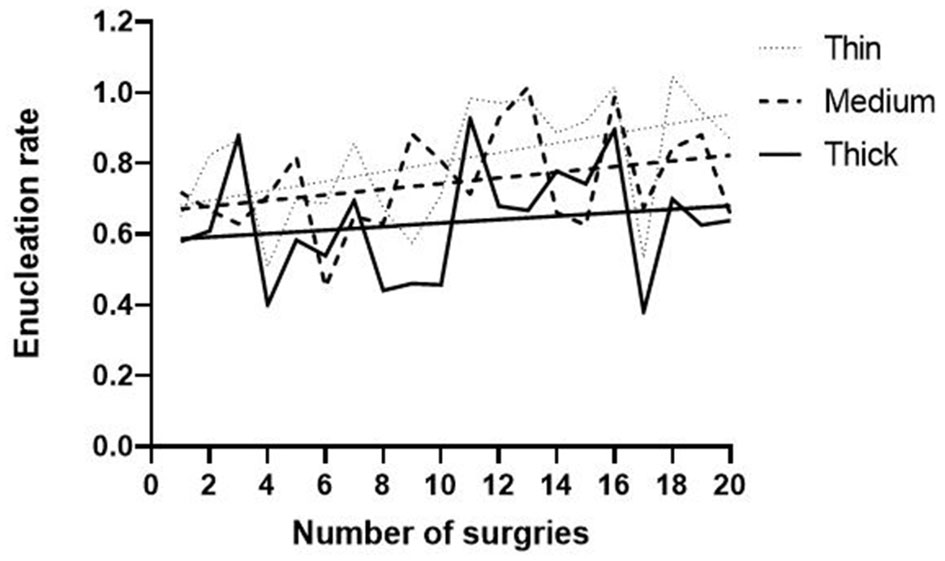
Learning curve of enucleation rate with different peripheral zones.
There is no difference in surgical sequence, age, height, body weight, BMI, PSA, f-PSA, PSAD, IPSS-S, IPSS-V, IPSS-T, Qol, PVR, Q-max, voiding detrusor pressure at Q-max, BOOI, enucleation time, or resection weight among the three groups. However, there are significant differences in efficiency, volume, and TZT of the three groups (Table 1). As a result, it is noticed that the thinner the PZT is, the higher the enucleation efficiency (0.811 ± 0.18 vs. 0.748 ± 0.14 vs. 0.634 ± 0.16, P = 0.004), the larger the prostate volume (58.9 ± 15.33 vs. 57.3 ± 15.58 vs. 46.6 ± 14.10, P = 0.025), and the thicker TZT are (44.45 ± 7.60 vs. 42.45 ± 6.08 vs. 34.78 ± 6.04, P < 0.001). In Post-hoc Multiple Comparisons (Supplementary Material 1), there are differences in resected tissue weight (50.0 ± 14.56 vs. 39.2 ± 13.48, P = 0.018), PSAD [0.091 (0.085) vs. 0.144 (0.168), P = 0.039], and age (72.6 ± 5.63 vs. 68.5 ± 5.39, P = 0.025) between the Thin group and Thick group.
Table 1
| Thin (n = 20) | Medium (n = 20) | Thick (n = 20) | F-value | P-value | |
|---|---|---|---|---|---|
| Surgical sequence | 34 ± 16.74 | 25 ± 15.68 | 32 ± 19.22 | 1.643 | 0.202 |
| Age (y) | 71.0 ± 5.86 | 72.6 ± 5.63 | 68.5 ± 5.39 | 2.691 | 0.076 |
| Weight (kg) | 73.2 ± 12.51 | 70.3 ± 10.76 | 71.1 ± 8.47 | 0.377 | 0.688 |
| Height (cm) | 170.6 ± 5.38 | 171.9 ± 5.01 | 172.3 ± 4.42 | 0.645 | 0.529 |
| BMI (kg/m2) | 25.1 ± 4.09 | 23.9 ± 3.97 | 23.9 ± 2.22 | 0.854 | 0.431 |
| Prostate volume (ml) | 58.9 ± 15.33 | 57.3 ± 15.58 | 46.6 ± 14.10 | 3.942 | 0.025 |
| IPP | 7.46 ± 8.72 | 7.82 ± 8.70 | 8.88 ± 10.12 | 0.128 | 0.880 |
| * PSA (ng/dl) | 4.935 (5.980) | 4.785 (7.702) | 5.715 (8.493) | 0.637 | 0.533 |
| * f-PSA (ng/dl) | 0.980 (1.108) | 0.860 (1.001) | 1.130 (0.940) | 0.170 | 0.844 |
| * PSAD | 0.091 (0.085) | 0.099 (0.077) | 0.144 (0.168) | 2.675 | 0.078 |
| Q-max (ml/s) | 2.8 (4.4) | 1.9 (5.2) | 3.9 (6.0) | 0.561 | |
| Voiding detrusor pressure at Q-max (cm H2O) | 65.4 ± 27.47 | 84.4 ± 34.37 | 82.5 ± 32.32 | 1.649 | 0.204 |
| BOOI | 67.6 ± 23.27 | 74.0 ± 39.08 | 87.9 ± 31.92 | 1.167 | 0.324 |
| PVRV (ml) | 112.5 (223.7) | 44.5 (150.3) | 96 (395) | 0.598 | |
| IPSS-T | 29 (11.2) | 33.5 (10.5) | 31 (7.7) | 0.325 | |
| IPSS-S | 12 (4.7) | 15.0 (4.7) | 13.5 (4.0) | 0.394 | |
| IPSS-V | 16.5 (8.7) | 18.5 (6.7) | 19 (7.2) | 0.562 | |
| Qol | 5 (1.0) | 5 (2.0) | 5 (1.7) | 0.971 | |
| TZT (mm) | 44.45 ± 7.60 | 42.45 ± 6.08 | 34.78 ± 6.04 | 11.929 | <0.001 |
| PZT (mm) | 5.67 ± 1.26 | 8.27 ± 0.71 | 11.98 ± 2.34 | 79.791 | <0.001 |
| Tissue weight (g) | 50.0 ± 14.56 | 46.3 ± 14.07 | 39.2 ± 13.48 | 3.085 | 0.053 |
| Enucleation time (min) | 61.0 ± 8.55 | 60.8 ± 10.23 | 61.0 ± 10.01 | 0.002 | 0.998 |
| Enucleation efficiency (g/min) | 0.811 ± 0.18 | 0.748 ± 0.14 | 0.634 ± 0.16 | 6.040 | 0.004 |
Clinical data of patients in different PZT groups.
Continuous variables with normal distribution are represented by mean ± SD, while ones with skewed distribution are represented by median (interquartile distance).
The variables are tested for homogeneity of variance, and then the F-value was calculated by One-way ANOVA test. Ordered variables are analyzed with Kruskal-Wallis H's test.
P < 0.05 indicated significant statistical significance.
The variables present normal distribution after natural logarithmic transformation and F and P-value are calculated according to the transformed data.
There is no significant difference in the above parameters among the three groups divided by the learning progress (Supplementary Material 2). In fact, the enucleation efficiency of Group 3 is significantly higher than that of Group 1 (0.783 vs. 0.658, P = 0.024) and Group 2 (0.783 vs. 0.751, P = 0.031) in the Post-hoc Multiple Comparisons (Supplementary Material 3).
In addition, Pearson correlation analysis (Table 2) gives the result that PZT was negatively correlated with prostate volume (r = −0.427), resection weight (r = −0.35), and enucleation efficiency (r = −0.445) in moderate intensity, and strongly negatively correlated with TZT (r = −0.533). On the contrary, it was moderately positively correlated with Q-max (r = 0.301) and BOOI (r = 0.388), which were statistically significant.
Table 2
| r | P-value | |
|---|---|---|
| Prostate volume (ml) | −0.427 | 0.001 |
| Tissue weight (g) | −0.35 | 0.006 |
| Enucleation efficiency (g/min) | −0.445 | <0.001 |
| TZT | −0.533 | <0.001 |
| BOOI | 0.388 | 0.021 |
| * PSA | −0.004 | 0.976 |
| * f-PSA | 0.029 | 0.824 |
| * PSAD | 0.239 | 0.066 |
Pearson correlation analysis of PZT.
r: correlation coefficient.
P <0.05 indicates statistical significance.
Fits normal distribution after natural logarithmic transformation.
We also conducted multiple linear regression analysis. As can be seen from Table 3, TZT, PZT, prostate volume, and Q-max are finally included in the model as independent variables affecting the enucleation efficiency. The model formula is that enucleation efficiency = 0.041 + 0.008 * TZT − 0.012 * PZT + 0.007 * volume + 0.013 * Q-max (R2= 0.932). This means that TZT, PZT, prostate volume, and Q-max can explain the 93.2% change of enucleation efficiency, and the model fitting degree is high. The F test (F = 48.050, P < 0.001) shows that at least one of these variables has a significant influence on the enucleation efficiency. In addition, the VIF values in the model are all less than five, which means that there is no collinearity among independent variables. Moreover, the D-W value is very close to 2, which shows that there is no autocorrelation in the model and correlation between the sample data. The regression coefficients of TZT, prostate volume, and Q-max were 0.008 (t = 3.597, P = 0.001), 0.007 (t = 7.275, P < 0.001), and 0.013 (t = 2.538, P = 0.017), respectively. The regression coefficient of PZT is −0.012 (t = −2.080, P = 0.046). According to the analysis, TZT, prostate volume, and Q-max have a significant positive influence on the gouging efficiency, while PZT has a significant negative influence.
Table 3
| Unstandardized | Standardized coefficients | t | P | VIF | R 2 | Adjusted R2 | F | ||
|---|---|---|---|---|---|---|---|---|---|
| coefficients | |||||||||
| B | Std. Error | Beta | |||||||
| Constant | 0.041 | 0.101 | – | 0.410 | 0.685 | – | 0.932 | 0.851 | F = 48.050, P < 0.001 |
| TZT | 0.008 | 0.002 | 0.334 | 3.597 | 0.001** | 1.907 | |||
| PZT | −0.012 | 0.006 | −0.150 | −2.080 | 0.046* | 1.150 | |||
| Prostate Volume | 0.007 | 0.001 | 0.646 | 7.275 | <0.001** | 1.746 | |||
| Q-max | 0.013 | 0.005 | 0.173 | 2.538 | 0.017* | 1.026 | |||
Multiple linear regression analysis.
Dependent Variable: Enucleation Efficiency.
Durbin-Watson: 2.136.
P < 0.05,
P < 0.01.
Discussion
B-TUEP has been recognized to provide symptom relief for BPH patients with prostates of almost any size, with definite efficacy and safety (15). Moreover, some researchers have confirmed that the incidence of body pain/discomfort, decreased physical pleasure, and difficulty in ejaculation of patients after B-TUEP is lower than that of holmium laser enucleation of prostate (HoLEP) (16). The overall enucleation efficiency in our study is similar to previous published articles about learning curves of different AEEP techniques (13, 17, 18). Clinically we found that some special characteristics of prostates are not suitable for doctors who have just started to learn enucleation technology, as they may affect their confidence in mastering this technology and limit its wide application. It is helpful for them to start with easier cases and be aware of complications that are more likely to occur in different PZT groups.
In our study, we firstly divided the patients into groups according to PZT. It was revealed that the enucleation efficiency of adenoma with PZT <7 mm was significantly higher than that of adenoma with PZT over 10 mm (Figure 1). This indicated that lower PZT may be more adequate for beginners' learning curves in the aspect of enucleation efficiency. Moreover, it is interesting that the enucleation efficiency of the Medium group is obviously higher than that of the Thick group, while there is no difference in resected tissue weight between the two groups in Post-hoc Multiple Comparisons (Supplementary Material 1). This proves that PZT may be an important factor for enucleation efficiency.
In the comparison of groups according to learning stages, the enucleation efficiency in the early stage is similar to that of middle stage, and obviously increases at the late stage (Figure 2). That indicates that enucleation efficiency is supposed to be a quantitative indicator of mastery of B-TUEP technique.
Figure 2
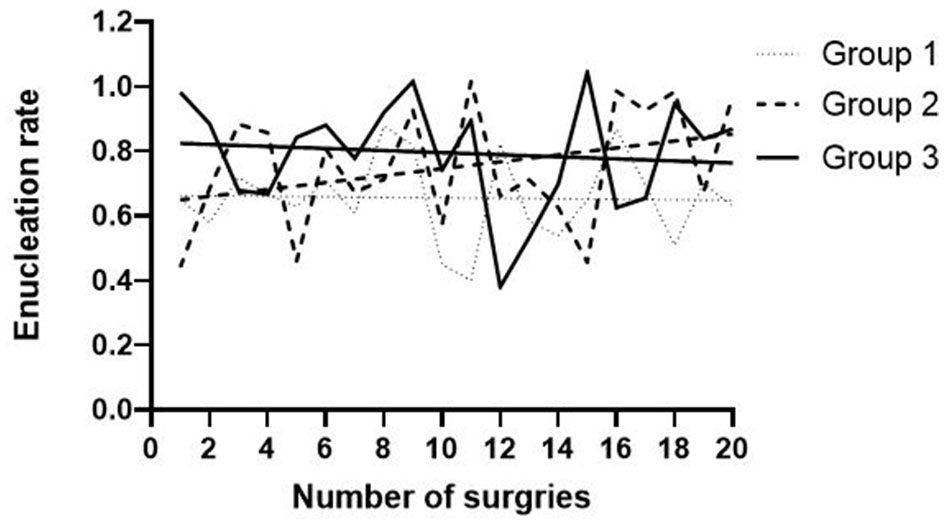
Learning curve of enucleation rate in different learning stages.
Our conclusion was further confirmed by multiple linear regression analysis. We found that when all the factors mentioned above were analyzed in stepwise approach, only TZT, PZT, prostate volume, and Q-max were proved to have the most significant influence on enucleation efficiency, which could explain 93.2% of enucleation efficiency changes. Moreover, the above variables do not display collinearity, suggesting that they are all independent factors, in which the increase of TZT, prostate volume, and Q-max can increase the enucleation efficiency, while the increase of PZT can decrease it. Our conclusion is in accordance with the work of Carolina Bebi et al. in which they found a larger prostate provided better enucleation efficiency.
It is worth noting that thin PZT seem to be more prone to developing capsule perforation during operation (Thin vs. Medium vs. Thick, 30 vs. 10 vs. 15%) (Table 4). We speculate that the peripheral zone is too thin to maintain the pressure during AEEP. When giving courses, we found that beginners' manual strength control is unstable and inexperienced. Especially when learners forget to change the direction of pushing, it will lead to the increase of pressure on the capsule. In this way, thinner capsules are more likely to be perforated, while thicker capsules may give them more opportunities to make mistakes. Well-defined planes greatly affect the development of perforation. However, more plane losses occurred in Group 3 than Group 1 and 2, which indicated that low PZT may be a greater risk factor for perforation. On the other hand, adenoma with high PZT seems to be more likely to develop multiple layers of capsule plane during enucleation (Thin vs. Medium vs. Thick, 20 vs. 15 vs. 40%), interfering with enucleation progress. However, Chi-square test cannot be performed due to the small sample size, so this conclusion needs to be confirmed by a larger sample study.
Table 4
| Clavien-Dindo group | Group 1 (n = 20) | Group 2 (n = 20) | Group 3 (n = 20) | |
|---|---|---|---|---|
| Intraoperative complications | ||||
| Wrong capsule plane | – | 4 (20%) | 3 (15%) | 8 (40%) |
| Capsule perforation | I | 6 (30%) | 2 (10%) | 3 (15%) |
| Postoperative complications | ||||
| Continuous hematuria | I | – | 1 (5%) | – |
| Hematuria requiring surgically intervention | IIIa | 1 (5%) | – | – |
| Hematuria requiring blood transfusion | II | – | – | – |
| Acute urinary retention after removal of the urethral catheter | I | 1 (5%) | 2 (10%) | 4 (20%) |
| Short term stress urinary incontinence after removal of the urethral catheter | I | 4 (20%) | 5 (25%) | 3 (15%) |
Intraoperative and postoperative complications.
Regarding the PZT, a previous study showed no tendency of thickening with age (7). It is also a meaningful anatomical factor and is related to prostate volume and micturition parameters (1). As BPH develops, the proliferation of the transitional zone has compression effects on urethra, peripheral zone, bladder, and surrounding tissue (1), thereby causing urinary tract obstruction and thinning of peripheral zone and intravesical prostatic protrusion (IPP). However, the compression effect on the peripheral zone could be low when the prostate volume is small, resulting in the lack of a well-defined mature layer formation that is crucial to identify surgical plane during enucleation (19). The result of our study indicates PZT may become thinner under pressure with the increase of age and the aggravation of BPH, due to the fact that patients in the Medium group are older than those in the Thick group. In our study, PZT was negatively correlated with prostate volume, tissue weight and TZT, and was positively correlated with Q-max. Therefore, our research is in common with the conclusion of Kwon et al. (1), that is, PZT of BPH patients may reflect the hyperplasia degree of prostate and the pressure on the peripheral zone, which may reveal the extent of urethral obstruction and voiding symptoms.
Conclusion
Measurement of PZT under MRI is related to the learning curve of B-TUEP, so it can provide information for learners in selecting adequate patients pre-operationally. Better patient selection can help learners to go through the curve of B-TUEP faster. Prostates with lower PZT tend to be related to higher enucleation efficiency, larger adenoma, and higher TZT. In addition, higher TZT, prostate volume, and Q-max may be independently related to higher enucleation efficiency as well. For B-TUEP learners, the operation seems easier to perform when the PZT of prostate is low, though more care should be given with the capsule perforation. The capsule plane should be maintained more attentively if the PZT is high. Surgeons can estimate the difficulty of operation by measuring PZT before operation, so as to select more suitable patients at the beginning.
Limitation
We divided patients into groups due to different PZT experimentally, because the cut-off points were never described in previous studies. Stratification of PZT may be improved by further studies. However, our results proved that PZT had an effect on the learning curve of B-TUEP. Our study was based on the learning process of Surgeon A, which may lack representativeness. We noticed that there are also some published studies that involved just a single surgeon (17, 19), and we consider it is valuable to share this experience with more surgeons who want to learn B-TUEP.
We did not describe postoperative parameters including length of hospital stay and postoperative irrigation. This is because we plan to discharge most patients 3 days after operation if they do not develop severe hematuria or other severe complications. Some patients still needed indwelling catheters when they left our hospital, and required moving to local hospitals and clinics.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of the Second Affiliated Hospital of Dalian Medical University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
QW is responsible for collecting data and writing articles. RA is responsible for reviewing articles and proofreading English. YH is responsible for the conception and statistical analysis of the article. LW is responsible for the revision of manuscripts. YY is responsible for the revision of manuscripts and interpretation of statistical analysis results. BY is the tutor of QW and RA and the surgical instructor in the article. All authors contributed to the article and approved the submitted version.
Acknowledgments
We appreciate Mr. Yang's teaching as a responsible tutor, and his effort on the AEEP surgery so that we could summarize his experience from it.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2021.795705/full#supplementary-material
- AEEP
Anatomical endoscopic enucleation of prostate
- BPH
Benign prostatic hyperplasia
- B-TUEP
Bipolar transurethral plasma enucleation of the prostate
- MRI
Magnetic resonance imaging
- PSA
Prostate specific antigen
- f-PSA
free prostatic specific antigen
- PASD
Prostate specific antigen density
- IPSS
International Prostatic Symptom Score
- Qol
Quality of life
- BOOI
Bladder outlet obstruction index
- PVRV
Post-voiding residual volume
- PZT
Peripheral zone thickness
- TZT
Transition zone thickness.
Abbreviations
References
1.
Kwon JK Han JH Choi HC Kang DH Lee JY Kim JH et al . Clinical significance of peripheral zone thickness in men with lower urinary tract symptoms/benign prostatic hyperplasia. BJU Int. (2016) 117:316–22. 10.1111/bju.13130
2.
Zhang Y Wang XD Song Y Peng R Tang T Li M et al . Epidemiology of frequent/urgent urination in older adults in China: a multicenter, cross-sectional study. Front Public Health. (2021) 9:669070. 10.3389/fpubh.2021.669070
3.
Teoh JY Cho CL Wei Y Isotani S Tiong HY Ong TA et al . Surgical training for anatomical endoscopic enucleation of the prostate. Andrologia. (2020) 52:e13708. 10.1111/and.13708
4.
Kim KH Yang HJ Heo NH Kim SH Kim DS Lee CH et al . Comparison study of learning curve using cumulative sum analysis between holmium laser enucleation of the prostate and transurethral resection of the prostate: is holmium laser enucleation of the prostate a difficult procedure for beginner urologists?J Endourol. (2021) 35:159–64. 10.1089/end.2020.0492
5.
Abdulwahab Al-Radhi M Lun LK Safi M Al-Danakh A Al-Kohlany KM Al-Najar A et al . Can bipolar transurethral enucleation of the prostate be a better alternative to the bipolar transurethral resection of the prostate? : a prospective comparative study. Medicine. (2021) 100:e25745. 10.1097/MD.0000000000025745
6.
Pallauf M Kunit T Ramesmayer C Deininger S Herrmann TRW Lusuardi L . Endoscopic enucleation of the prostate (EEP). the same but different-a systematic review. World J Urol. (2021) 39:2383–96. 10.1007/s00345-021-03705-6
7.
Matsugasumi T Fujihara A Ushijima S Kanazawa M Yamada Y Shiraishi T et al . Morphometric analysis of prostate zonal anatomy using magnetic resonance imaging: impact on age-related changes in patients in Japan and the USA. BJU Int. (2017) 120:497–504. 10.1111/bju.13823
8.
Watanabe H . New concept of BPH: PCAR theory. Prostate. (1998) 37:116–25. 10.1002/(SICI)1097-0045(19981001)37:2<116::AIDPROS8>3.0.CO;2-E
9.
Guzman JA Sharma P Smith LA Buie JD de Riese WT . Histological changes of the peripheral zone in small and large prostates and possible clinical implications. Res Rep Urol. (2019) 11:77–81. 10.2147/RRU.S182781
10.
Weaver PE Smith LA Sharma P Keesari R Al Mekdash H de Riese WT . Quantitative measurements of prostate capsule and gland density and their correlation to prostate size: possible clinical implications in prostate cancer. Int Urol Nephrol. (2020) 52:1829–37. 10.1007/s11255-020-02527-6
11.
Enikeev D Morozov A Taratkin M Misrai V Rijo E Podoinitsin A et al . Systematic review of the endoscopic enucleation of the prostate learning curve. World J Urol. (2021) 39:2427–38. 10.1007/s00345-020-03451-1
12.
Boeri L Capogrosso P Ventimiglia E Fontana M Sampogna G Zanetti SP et al . Clinical comparison of holmium laser enucleation of the prostate and bipolar transurethral enucleation of the prostate in patients under either anticoagulation or antiplatelet therapy. European Urol Focus. (2020) 6:720–28. 10.1016/j.euf.2019.03.002
13.
Netsch C Bach T Herrmann TR Neubauer O Gross AJ . Evaluation of the learning curve for Thulium VapoEnucleation of the prostate (ThuVEP) using a mentor-based approach. World J Urol. (2013) 31:1231–8. 10.1007/s00345-012-0894-1
14.
Liu C Zheng S Li H Xu K . Transurethral enucleation and resection of prostate in patients with benign prostatic hyperplasia by plasma kinetics. J Urol. (2010) 184:2440–5. 10.1016/j.juro.2010.08.037
15.
Bebi C Turetti M Lievore E Ripa F Rocchini L Spinelli MG et al . Bipolar Transurethral Enucleation of the Prostate: Is it a size-independent endoscopic treatment option for symptomatic benign prostatic hyperplasia?PLoS One. (2021) 16:e0253083. 10.1371/journal.pone.0253083
16.
Bebi C Turetti M Lievore E Ripa F Bilato M Rocchini L et al . Sexual and ejaculatory function after holmium laser enucleation of the prostate and bipolar transurethral enucleation of the prostate: a single-center experience. Int J Impot Res. (2020). 10.1038/s41443-020-00366-8
17.
Kim KH Kim KT Oh JK Chung KJ Yoon SJ Jung H et al . Enucleated weight/enucleation time, is it appropriate for estimating enucleation skills for holmium laser enucleation of the prostate? A consideration of energy consumption. World J Mens Health. (2018) 36:79–86. 10.5534/wjmh.17039
18.
Bae J Oh SJ Paick JS . The learning curve for holmium laser enucleation of the prostate: a single-center experience. Korean J Urol. (2010) 51:688–93. 10.4111/kju.2010.51.10.688
19.
Feng L Song J Zhang D Tian Y . Evaluation of the learning curve for transurethral plasmakinetic enucleation and resection of prostate using a mentor-based approach. Int Braz J Urol. (2017) 43:245–55. 10.1590/s1677-5538.ibju.2016.0237
Summary
Keywords
AEEP, benign prostatic hyperplasia, peripheral zone, learning curve, bipolar
Citation
Wang Q, Alshayyah R, He Y, Wen L, Yu Y and Yang B (2022) Is the Peripheral Zone Thickness an Indicator of a Learning Curve in Bipolar Transurethral Plasma Enucleation of the Prostate?—A Single Center Cohort Study. Front. Surg. 8:795705. doi: 10.3389/fsurg.2021.795705
Received
15 October 2021
Accepted
24 December 2021
Published
02 February 2022
Volume
8 - 2021
Edited by
Guiming Liu, Case Western Reserve University, United States
Reviewed by
Bogdan Geavlete, St. John Hospital Emergency Clinic, Romania; Nicolo' Schifano, San Raffaele Hospital (IRCCS), Italy; Luca Boeri, University of Milan, Italy
Updates
Copyright
© 2022 Wang, Alshayyah, He, Wen, Yu and Yang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bo Yang dymnyb@hotmail.com
This article was submitted to Genitourinary Surgery, a section of the journal Frontiers in Surgery
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.