Abstract
Objective:
Multi-disciplinary team (MDT) collaboration enables hepatocellular carcinoma (HCC) patients to achieve better survival through precise diagnosis and individualized treatment. This study aimed to further investigate the effect of MDT care program (MDT-CP) on quality of life (QoL), anxiety and depression in HCC patients after surgery.
Methods:
Totally, 150 postoperative HCC patients were enrolled and randomized in a 1:1 ratio into the MDT-CP group (N = 76) to receive MDT care for 6 months and the normal care program (N-CP) group (N = 74) to receive routine care for 6 months.
Results:
Quality of Life Questionnaire-Core 30 (QLQ-C30) global health status score at 1 month (M1), M3 and M6, QLQ-C30 functions score at M3 and M6 elevated while QLQ-C30 symptom score at M1 and M3 decreased in MDT-CP group compared with N-CP group (all P < 0.05). In addition, Hospital Anxiety and Depression Scale (HADS)-Anxiety score at M3 and M6, anxiety occurrence rate at M6, anxiety degree at M6, were all reduced in MDT-CP group compared with N-CP group (all P < 0.05). HADS-Depression score at M6, and depression occurrence rate at M3, were both lessened in MDT-CP group compared to N-CP group (both P < 0.05), while there was no distinction of depression degree at any time points between groups.
Conclusion:
MDT-CP improves QoL, relieves anxiety and depression to a certain extent in HCC patients after surgery.
Introduction
Hepatocellular carcinoma (HCC) is the most common form of liver cancer and accounts for 8.3% of the world's cancer deaths (1–3). Studies have identified the major risk factors for HCC, including Hepatitis B virus (HBV), hepatitis C virus, alcoholic and nonalcoholic fatty liver disease (4). In addition, co-infection of hepatitis D virus (HDV) and HBV significantly increases the risk of HCC recurrence in patients undergoing living donor liver transplantation (5). Together with the progresses in early detection and treatment of HCC, the morbidity and mortality of HCC have been reduced to some extent (6). However, HCC still imposes a huge financial and life burden on patients (7). These burdens often reduce quality of life (QoL) and cause anxiety and depression in HCC patients.
The nursing management of QoL, anxiety and depression in HCC patients is highly concerned in recent years (8, 9). One recent study illustrates that the model of 5A nursing intervention is a new nursing model that offers nursing intervention through inquiry, suggestion, evaluation, help, and follow-up with patients, which could elevate QoL in HCC patients after surgery (10). Meanwhile, a comprehensive education and care program improves QoL, anxiety and depression, and prolongs survival in patients with HCC undergoing surgical resection (11). In addition, our previous study also illustrates reminiscence therapy-based care ameliorates QoL, anxiety and depression in elderly patients with HCC (12). Considering that poor QoL, anxiety and depression are still prevalent and positively associated with HCC mortality (13–15), it is necessary to explore novel intervention to manage the QoL, anxiety, and depression in HCC patients.
Multi-disciplinary team (MDT) is the collaboration of multiple specialists from different disciplines to achieve coordinated management (16), which aims to delay disease progression, prolong survival, and maintain an acceptable QoL in patients (17). A previous study shows MDT collaborative nursing model can elevate QoL, alleviate anxiety, depression and other negative emotions in the postoperative advanced pancreatic cancer patients (18). Moreover, other studies illustrate that MDT also improve QoL, anxiety, depression in patients with cervical cancer and gastric cancer (19, 20). However, the impact of MDT management on QoL and mental health in HCC patients is still unclear.
Thus, we designed an MDT care program (MDT-CP) in this randomized, controlled study, aiming to compare the effect of MDT-CP versus normal care program (N-CP) on QoL and mental health in HCC patients after surgery.
Methods
Patients
A total of 150 primary HCC patients who underwent tumor resection from February 2019 to March 2021 were consecutively enrolled in this randomized, controlled study. The inclusion criteria contained: (a) pathologically diagnosed as HCC; (b) older than 18 years; (c) underwent tumor resection; (d) were voluntary for participation and willing for complying with the study protocol. The exclusion criteria contained: (a) had other malignancies; (b) complicated with a severe mental disorder or cognitive impairment that unable to comply with the study assessment; (c) had psychological intervention history. The study was permitted by Ethics Committee of The Central Hospital of Wuhan, Tongji Medical College, Huazhong University of Science and Technology. Written informed consent was gained from each patient.
Random assignment
Included patients were randomly assigned according to a 1:1 ratio using the block randomization method with a block size of 4 (21). Briefly, scratch cards were made to record patients’ randomization information and were distributed to patients when they were deemed eligible for inclusion. Based on the first 37 blocks, patients were assigned to two groups with 74 patients in each group; while based on the last block (38th block), 2 patients were both assigned to the MDT-CP group. Therefore, the included patients were assigned to two groups: 76 in the MDT-CP group and 74 in the N-CP group.
Intervention
For the N-CP group, routine care was provided, and routine verbal and written discharge instructions were given, including dietary and medication instructions and precautions related to HCC. For the first 6 months after discharge, patients were regularly admitted to the hospital for follow-up once a month. During the follow-up period, the patient's condition was monitored and health guidance was provided.
For the MDT-CP group, patients received MDT-CP on the basis of normal care, and the specific methods are as follows: (a) a multi-disciplinary team was formed, consisting of 2 attendings from the department of hepatobiliary and pancreatic surgery, 2 nutritionists from nutrition department, 2 rehabilitation physicians from rehabilitation department, 2 psychiatrists from psychiatry department, and 4 nursing staff from nursing department; (b) an MDT-CP was developed: a thorough assessment of the patient's physical, psychological, environmental, and health behaviors was conducted, then a rational plan of care was discussed with the patient's family to clarify the patient's needs; (c) the program was implemented: patients were followed up weekly by telephone and monthly by home visits or outpatient visits, during the follow-up, the following nursing measures were implemented according to the patient's actual condition: (1) the department of hepatobiliary and pancreatic surgery was mainly responsible for observing patients’ physiological indications, changes in their condition, recovery of liver function, and postoperative functional recovery, in order to improve patient's condition and promote disease recovery; (2) the nutrition department was responsible for developing a nutritional plan and encouraging patients to have a rational diet; (3) the rehabilitation department was responsible for developing a training plan based on the patient's physical condition and tolerance level; (4) the psychiatry department was responsible for psychological intervention according to the patient's condition, encouraging the patient to communicate emotionally and relieving the patient's bad mood; (5) the nursing department was responsible for training relevant staff and supporting the whole program (22, 23).
Follow-up and assessment
Following the patient's discharge from the hospital, outpatient or telephone follow-up was performed for 6 months. Quality of Life Questionnaire-Core 30 (QLQ-C30) and Hospital Anxiety and Depression Scale (HADS) scores were assessed on discharge (M0), at 1 month after discharge (M1), at 3 months after discharge (M3), and at 6 months after discharge (M6). The QLQ-C30 score was used to assess patients’ quality of life (24). The HADS scale was used to assess anxiety and depression, with no being 0–7 scores, mild being 8–10 scores, moderate being 11–14 scores, and severe being 15–21 scores (25).
Statistics
The sample size was determined by assuming that the mean QLQ-C30 global health status score for the MDT-CP group was 85 with a standard deviation (SD) of less than 20 and the mean QLQ-C30 global health status score for the N-CP group was 75 with an SD of less than 20 at M6 (26). The minimum sample size for each group was 63 at a significance (α) level of 0.05 and a power of 85%, which was then adjusted for a 15% dropout rate and increased to 73. SPSS v.26.0 (IBM Corp., America) was used for analysis. GraphPad Prism v.9.0 (GraphPad Software Inc., America) was used for graphing. Kolmogorov-Smirnov test was utilized for normality determination. The normal distributed continuous variables (age, QLQ-C30 score, and HADS score) were displayed as mean ± SD and analyzed using Student's t-test. The skewed distributed continuous variables (liver function indexes) were presented as median and inter-quartile range (IQR) and analyzed using Mann-Whitney U test. The binary categorized variables and unordered categorical variables (gender, smoke, marriage status, employment status before surgery, location, chronic comorbidities, ECOG PS score, Child-Pugh stage, tumor nodule number, largest tumor size, anxiety occurrence, and depression occurrence) were expressed as count (percentage) and analyzed using Chi-Square test. The ordinal categorical variables (level of education, BCLC stage, CNLC stage, anxiety degree, and depression degree) were expressed as count (percentage) and analyzed using Mann-Whitney U test. P < 0.05 was considered significant.
Results
Study flow
A total of 164 primary HCC patients who underwent tumor resection were invited, while 14 of them were excluded from this study, including 9 patients who either met the exclusion criteria or did not meet the inclusion criteria, and 5 patients who refused to participate. The remaining 150 patients were then randomized as 1:1 ratio into N-CP group (N = 74) and MDT-CP group (N = 76) to receive N-CP and MDT-CP interventions for 6 months, respectively. During follow-up, 5 (6.8%) patients in N-CP group withdrew, including 1 (1.4%) patient who lost to follow-up and 1 (1.4%) patient who was willing for dropout at M1, 2 (2.7%) patients who lost to follow-up at M3, and 1 (1.4%) patient who lost to follow-up at M6. In MDT-CP group, 9 (11.8%) patients withdrew, which included 3 (3.9%) patients who lost to follow-up and 2 (2.6%) patients who was willing for dropout at M1, 1 (1.3%) patient who lost to follow-up and 1 (1.3%) patient who was willing for dropout at M3, and 2 (2.6%) patients who lost to follow-up at M6. In both groups, QLQ-C30 and HADS scores were evaluated at M0, M1, M3, and M6, respectively. Finally, all available data were included with ITT principle (Figure 1).
Figure 1
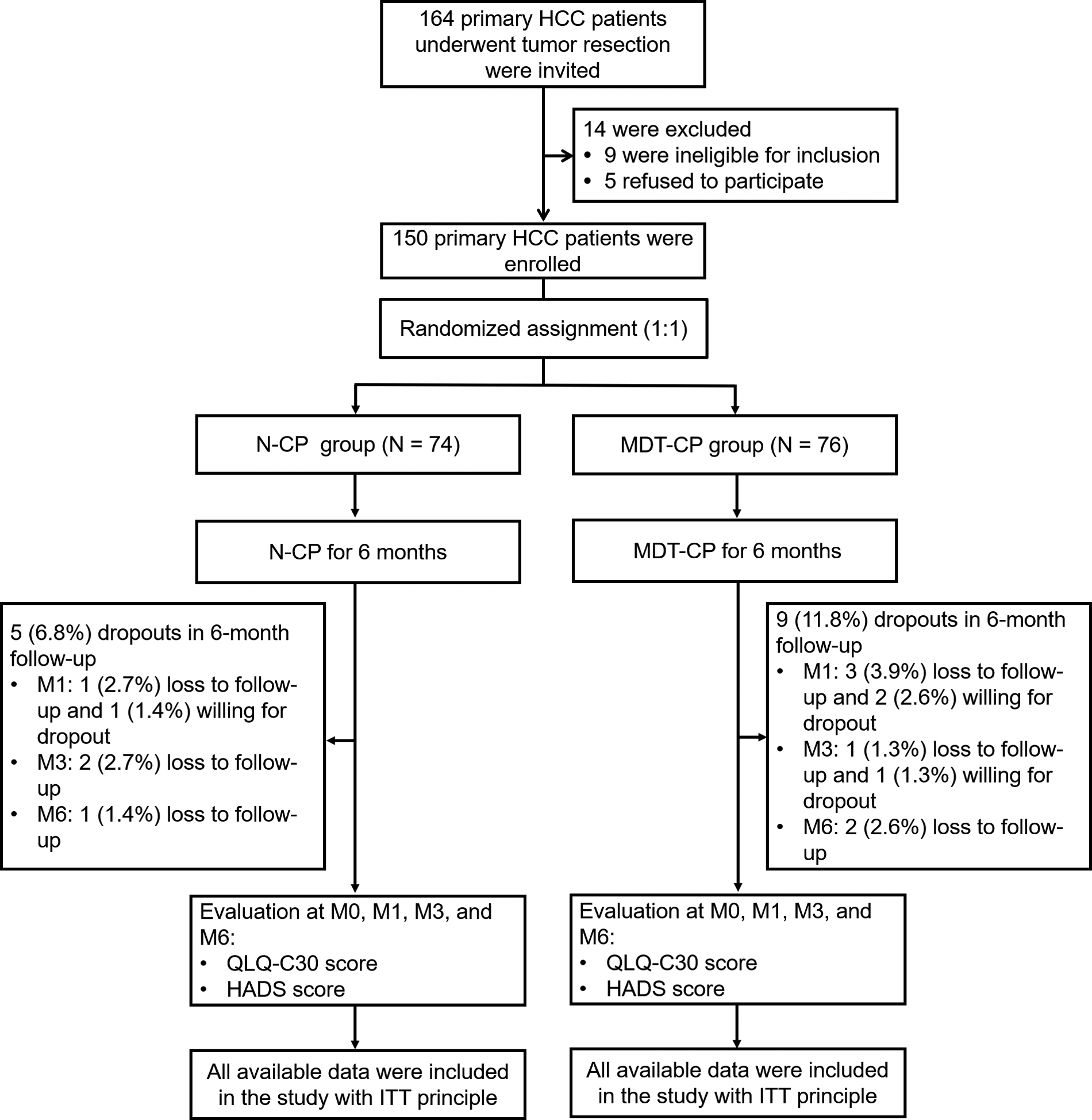
Study flow chart.
Comparison of baseline characteristics between groups
The mean age was 57.4 ± 9.8 and 56.8 ± 9.3 years respectively in MDT-CP and N-CP groups. Meanwhile, there were 8 (10.8%) females in MDT-CP group and 12 (15.8%) females in N-CP group, accordingly. Further comparison analysis showed that no discrepancy was observed in clinical characteristics, including demographic characteristics, chronic comorbidities, and disease features between MDT-CP and N-CP group (all P > 0.05) (Table 1). Moreover, it was found that there was no difference in the level of liver function indexes and tumor markers between MDT-CP group and N-CP group (all P > 0.05) (Table 2).
Table 1
| Items | N-CP group (N = 74) | MDT-CP group (N = 76) | P value |
|---|---|---|---|
| Demographics | |||
| Age (years), mean ± SD | 56.8 ± 9.3 | 57.4 ± 9.8 | 0.696 |
| Gender, No. (%) | 0.370 | ||
| Female | 8 (10.8) | 12 (15.8) | |
| Male | 66 (89.2) | 64 (84.2) | |
| Smoke, No. (%) | 0.944 | ||
| Never | 32 (43.2) | 33 (43.4) | |
| Former | 18 (24.3) | 20 (26.3) | |
| Current | 24 (32.4) | 23 (30.3) | |
| Marriage status, No. (%) | 0.771 | ||
| Married | 57 (77.0) | 57 (75.0) | |
| Single/Divorced/Widowed | 17 (23.0) | 19 (25.0) | |
| Employment status before surgery, No. (%) | 0.750 | ||
| Employed | 36 (48.6) | 35 (46.1) | |
| Unemployed | 38 (51.4) | 41 (53.9) | |
| Level of education, No. (%) | 0.712 | ||
| Primary school or less | 8 (10.8) | 5 (6.6) | |
| High school | 36 (48.6) | 43 (56.6) | |
| Undergraduate | 24 (32.4) | 22 (28.9) | |
| Graduate or above | 6 (8.1) | 6 (7.9) | |
| Location, No. (%) | 0.658 | ||
| Rural | 8 (10.8) | 10 (13.2) | |
| Urban | 66 (89.2) | 66 (86.8) | |
| Chronic comorbidities | |||
| History of HB, No. (%) | 61 (82.4) | 61 (80.3) | 0.733 |
| History of liver cirrhosis, No. (%) | 53 (71.6) | 57 (75.0) | 0.640 |
| History of hypertension, No. (%) | 26 (35.1) | 31 (40.8) | 0.476 |
| History of hyperlipidemia, No. (%) | 12 (16.2) | 19 (25.0) | 0.184 |
| History of diabetes, No. (%) | 7 (9.5) | 12 (15.8) | 0.244 |
| Disease features | |||
| ECOG PS score, No. (%) | 0.927 | ||
| Score 0 | 56 (75.7) | 58 (76.3) | |
| Score 1 | 18 (24.3) | 18 (23.7) | |
| Child-pugh stage, No. (%) | 0.938 | ||
| Stage A | 60 (81.1) | 62 (81.6) | |
| Stage B | 14 (18.9) | 14 (18.4) | |
| Tumor nodule number, No. (%) | 0.255 | ||
| Unifocal | 35 (47.3) | 43 (56.6) | |
| Multifocal | 39 (52.7) | 33 (43.4) | |
| Largest tumor size, No. (%) | 0.191 | ||
| <5.0 cm | 41 (55.4) | 34 (44.7) | |
| ≥5.0 cm | 33 (44.6) | 42 (55.3) | |
| BCLC stage, No. (%) | 0.754 | ||
| Stage 0 | 0 (0.0) | 1 (1.3) | |
| Stage A | 34 (45.9) | 37 (48.7) | |
| Stage B | 22 (29.7) | 20 (26.3) | |
| Stage C | 18 (24.3) | 18 (23.7) | |
| CNLC stage, No. (%) | 0.422 | ||
| Stage Ia | 13 (17.6) | 9 (11.8) | |
| Stage Ib | 27 (36.5) | 36 (47.4) | |
| Stage IIa | 22 (29.7) | 23 (30.3) | |
| Stage IIb | 12 (16.2) | 8 (10.5) | |
Clinical characteristics.
N-CP, normal care program; MDT-CP, multi-disciplinary team care program; SD, standard deviation; HB, hepatitis B; ECOG PS, eastern cooperative oncology group performance status; BCLC, barcelona clinic liver cancer; CNLC, Chinese liver cancer.
Table 2
| Items | N-CP group (N = 74) | MDT-CP group (N = 76) | P value |
|---|---|---|---|
| ALT (U/L), median (IQR) | 31.3 (23.9–44.9) | 32.0 (20.6–48.0) | 0.987 |
| AST (U/L), median (IQR) | 40.5 (29.2–54.0) | 40.0 (26.8–53.3) | 0.632 |
| ALP (U/L), median (IQR) | 101.8 (72.5–157.0) | 91.4 (73.5–122.8) | 0.228 |
| TBIL (μmol/L), median (IQR) | 15.3 (10.5–25.0) | 14.8 (10.2–21.2) | 0.622 |
| CEA (ng/ml), median (IQR) | 4.7 (2.7–6.2) | 4.1 (2.9–7.0) | 0.545 |
| CA199 (U/ml), median (IQR) | 24.9 (14.6–43.7) | 24.7 (14.9–41.6) | 0.897 |
| AFP (ng/ml), median (IQR) | 229.3 (10.4–874.8) | 111.1 (9.6–1104.1) | 0.912 |
Liver function indexes and tumor markers.
N-CP, normal care program; MDT-CP, multi-disciplinary team care program; ALT, alanine aminotransferase; IQR, interquartile range; AST, aspartate aminotransferase; ALP, alkaline phosphatase; TBIL, total bilirubin; CEA, carcinoembryonic antigen; CA199, carbohydrate antigen 199; AFP, alpha-fetoprotein.
Comparison of QoL between groups
There was no distinction of QLQ-C30 global health status score between MDT-CP group and N-CP group at M0 (P = 0.412), while it was higher in MDT-CP group compared to N-CP group at M1 (P = 0.014), M3 (P = 0.017) and M6 (P = 0.013) (Figure 2A). Simultaneously, the QLQ-C30 function score did not differ between groups at M0 (P = 0.410) or M1 (P = 0.080), whereas it was increased in MDT-CP group compared to N-CP group at M3 (P = 0.020) and M6 (P = 0.033) (Figure 2B). Regarding QLQ-C30 symptoms score, no gap was found between groups at M0 (P = 0.552) or M6 (P = 0.368), but it was decreased in MDT-CP group compared to N-CP group at M1 (P = 0.030) and M3 (P = 0.013) (Figure 2C).
Figure 2
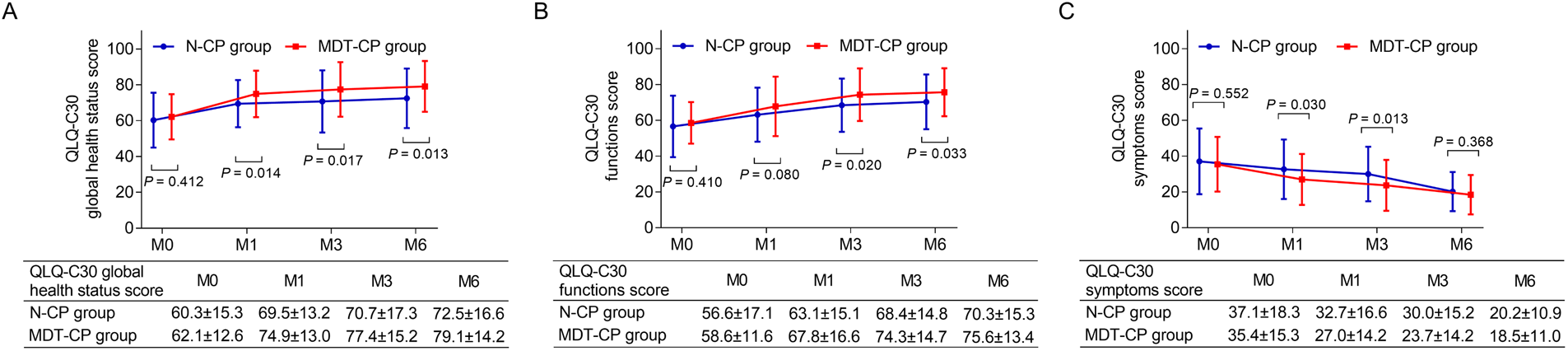
Qol was elevated in MDT-CP group compared to N-CP group. QLQ-C30 global health status score (A) and QLQ-C30 functional score (B) were elevated, whereas QLQ-C30 symptom score (C) was reduced in MDT-CP group compared with N-CP group.
Comparison of HADS-A score and HADS-D score between groups
HADS-A score was reduced in MDT-CP group compared with N-CP group at M3 (P = 0.038) and M6 (P = 0.026), but it remained similar between groups at M0 (P = 0.639) and M1 (P = 0.122) (Figure 3A). In addition, no difference in HADS-D score was found between groups at M0 (P = 0.587), M1 (P = 0.116) or M3 (P = 0.059), however, it was lower in MDT-CP group compared with N-CP group at M6 (P = 0.049) (Figure 3B).
Figure 3
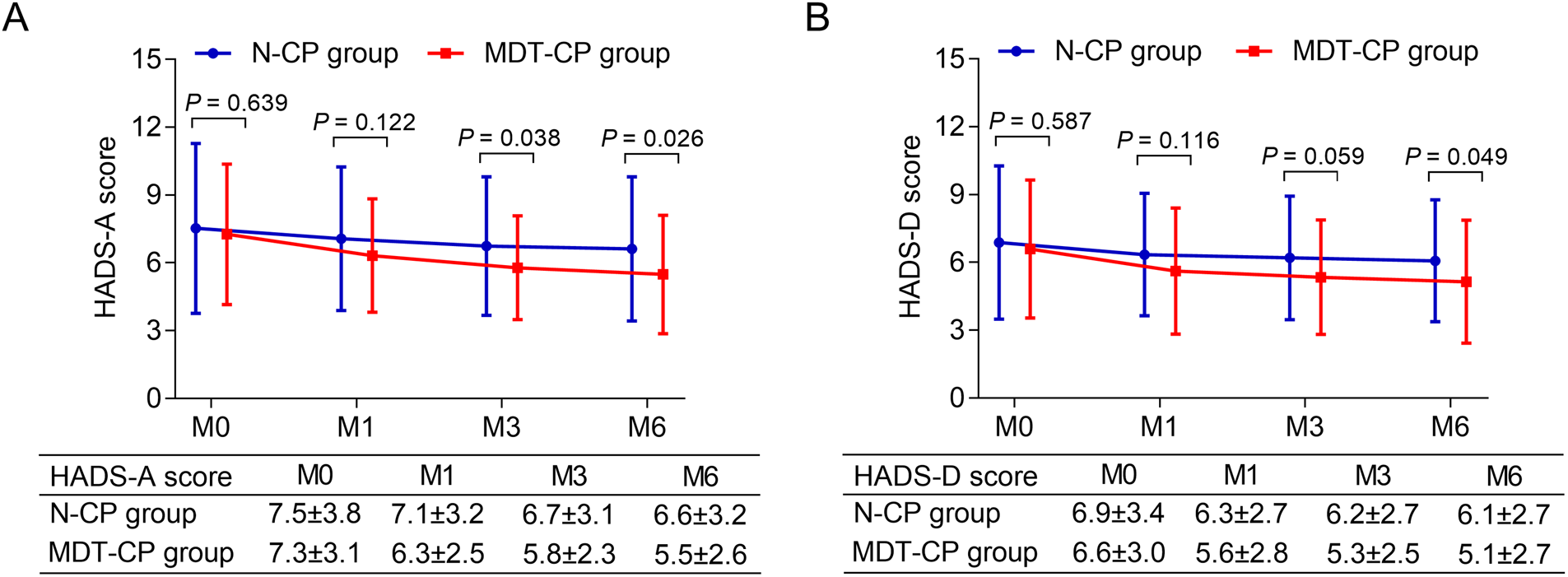
Anxiety and depression were reduced in MDT-CP group compared to N-CP group. HADS-A score (A) and HADS-D score (B) were decreased in MDT-CP group compared to N-CP group.
Comparison of anxiety occurrence rate and degree between groups
No difference in anxiety occurrence rate was observed between MDT-CP group and N-CP group at M0 (P = 0.643), M1 (P = 0.406), or M3 (P = 0.196), while it was decreased in MDT-CP group than that in N-CP group at M6 (17.9% vs. 33.3%, P = 0.040) (Supplementary Table S1). In addition, there was no distinction of anxiety degree between MDT-CP group and N-CP group at M0 (P = 0.580), M1 (P = 0.284) or M3 (P = 0.117), but it was lower in MDT-CP group than that in N-CP group at M6 (P = 0.035) (Supplementary Table S2).
Comparison of depression occurrence rate and degree between groups
In terms of depression occurrence rate, no difference was found at M0 (P = 0.417), M1 (P = 0.189), or M6 (P = 0.156) between MDT-CP group and N-CP group, whereas it was reduced in MDT-CP group compared with N-CP group at M3 (14.9% vs. 24.6%, P = 0.044) (Supplementary Table S3). Besides, there was no difference of depression degree between MDT-CP group and N-CP group at M0, M1, M3, or M6 (all P > 0.05) (Supplementary Table S4).
Discussion
HCC has a profound negative impact on patients’ QoL (27). In addition, the fear of recurrence, especially after surgery or liver transplantation, also seriously affects this (28). Previous studies show that MDT improves QoL of many patients with cancers (18–20, 29), however, the effect of MDT on QoL in HCC patients after surgery is unclear. Our results illustrated that MDT-CP elevated QoL of HCC patients who underwent surgery, especially in terms of global health status and functions, which might be because MDT-CP made a comprehensive and reasonable care plan according to the needs of HCC patients, including (1) Nutrition plans which were formulated by nutritionists to make patients ingest adequate nutrition, and thus improved the patients’ immunity and recovery; (2) Physical training plans according to the patients’ physical conditions, which were made by rehabilitation physicians to enhance the patients’ physical status. Therefore, global health conditions and functions of HCC patients were elevated by MDT-CP. However, comparing with N-CP, the symptoms score in QLQ-C30 was only lower at M1 and M3 by MDT-CP, but there was no difference at M6, which might be because MDT-CP could promote the recovery of patients after surgery in a short time; but with the increase of time, the symptoms of HCC patients in N-CP group were also relieved.
HCC patients who underwent surgery have a high incidence of anxiety and depression (30, 31). One study shows that about 48% of HCC patients who underwent surgery experienced anxiety and about 18% experienced depression (32). This is slightly different from our results, in our study, about 37% of HCC patients developed anxiety and 32% of HCC patients developed depression at M0. The differences of anxiety and depression between the previous study (32) and our study might be due to the differences in assessment populations. The reasons for the high incidence of anxiety and depression in HCC patients after surgery might be that they had enormous pressure, such as worries about their own health status, and a huge financial burden (33, 34). In addition, fear of cancer recurrence was also one of the factors affecting the mental health of postoperative HCC patients. Our study suggested that HCC patients still had a high incidence of anxiety and depression after surgery, therefore, more nursing methods were needed to manage the mental health of HCC patients.
The high incidence of anxiety and depression in HCC patients is a key issue (35). MDT has been shown to alleviate anxiety and depression in patients with various cancers (18–20, 36), while the effect of MDT on mental health in HCC patients is unclear. Our study showed that MDT-CP relieved anxiety and alleviated depression to a certain extent in postoperative HCC patients. This might result from that MDT-CP had a multidisciplinary team of specialists including (1) Professional attending physicians who learned about the condition of disease timely alleviated the patient's fear of recurrence [which was positively associated with the incidence of anxiety and depression (37)]. (2) Psychiatrists who provided psychological interventions on patients relieved their negative emotions. (3) Nursing staffs who provided care to patients during the nursing period might improve their mental health (11). Thus, MDT-CP could relief anxiety and depression of HCC patients.
In the current study, we used a block randomization method with a block size of 4 to randomize 150 patients (21). And there were 38 scratch cards made to record patients’ randomization information. The first 37 scratch cards randomly divided patients into two groups. At this time, there were 74 patients in N-CP and MDT-CP, respectively (148 in total). However, the number of people included was two less than we expected. When the 38th scratch card was opened, two patients just fell into the MDT-CP group. Therefore, there were 76 patients in the MDT-CP group and 74 patients in the N-CP group. This difference in a small number of patients is normal in studies with the block randomization method (38, 39).
There were some limitations in this study: (1) This study was a single-center study, which led to the selection bias. (2) The intervention period was only 6 months; thus, a longer-term intervention was needed to evaluate the effect of long-term MDT-CP on QoL, anxiety and depression in HCC patients. (3) Our study only included HCC patients who underwent surgery. However, many HCC patients were unable to undergo surgery, who even had a poorer QoL and a higher incidence of anxiety and depression. Future studies should elaborate on the effect of MDT-CP in these patients.
In conclusion, MDT-CP improves QoL, mitigates anxiety and depression to a certain degree in HCC patients who underwent surgery. Our findings suggest that MDT-CP could be an effective caring option for the postoperative management of HCC, while a larger-scale study is needed for verification.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of The Central Hospital of Wuhan, Tongji Medical College, Huazhong University of Science and Technology. The patients/participants provided their written informed consent to participate in this study.
Author contributions
JW substantially contributed to the conception and the design of the study. LY and CY were responsible for the acquisition, analysis and interpretation of the data. All authors contributed to manuscript drafting and critical revisions of the intellectual content. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by Wuhan Municipal Health Commission with project number WX21Q21.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.1045003/full#supplementary-material.
References
1.
Llovet JM Kelley RK Villanueva A Singal AG Pikarsky E Roayaie S et al Hepatocellular carcinoma. Nat Rev Dis Primers. (2021) 7(1):6. 10.1038/s41572-020-00240-3
2.
Sagnelli E Macera M Russo A Coppola N Sagnelli C . Epidemiological and etiological variations in hepatocellular carcinoma. Infection. (2020) 48(1):7–17. 10.1007/s15010-019-01345-y
3.
Sung H Ferlay J Siegel RL Laversanne M Soerjomataram I Jemal A et al Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71(3):209–49. 10.3322/caac.21660
4.
Kulik L El-Serag HB . Epidemiology and management of hepatocellular carcinoma. Gastroenterology. (2019) 156(2):477–91.e1. 10.1053/j.gastro.2018.08.065
5.
Baskiran A Akbulut S Sahin TT Koc C Karakas S Ince V et al Effect of HBV-HDV co-infection on HBV-HCC co-recurrence in patients undergoing living donor liver transplantation. Hepatol Int. (2020) 14(5):869–80. 10.1007/s12072-020-10085-3
6.
Singal AG El-Serag HB . Hepatocellular carcinoma from epidemiology to prevention: translating knowledge into practice. Clin Gastroenterol Hepatol. (2015) 13(12):2140–51. 10.1016/j.cgh.2015.08.014
7.
Zou H Li M Lei Q Luo Z Xue Y Yao D et al Economic burden and quality of life of hepatocellular carcinoma in greater China: a systematic review. Front Public Health. (2022) 10:801981. 10.3389/fpubh.2022.801981
8.
Zhang L Zhang X Cui Z Zhou L Qu K Wang N . Effects of high-quality nursing care on psychological outcomes and quality of life in patients with hepatocellular carcinoma: a protocol of systematic review and meta-analysis. Medicine. (2020) 99(35):e21855. 10.1097/MD.0000000000021855
9.
Yuan Y Li Y Yang G Zhang L Ye J . Effect of comprehensive nursing approach in perioperative stage of patients with hepatocellular carcinoma interventional therapy. Evid Based Complement Alternat Med. (2022) 2022:6862463. 10.1155/2022/6862463
10.
Zhang X Lai M Wu D Luo P Fu S . The effect of 5A nursing intervention on living quality and self-care efficacy of patients undergoing chemotherapy after hepatocellular carcinoma surgery. Am J Transl Res. (2021) 13(6):6638–45.
11.
Wang J Yan C Fu A . A randomized clinical trial of comprehensive education and care program compared to basic care for reducing anxiety and depression and improving quality of life and survival in patients with hepatocellular carcinoma who underwent surgery. Medicine. (2019) 98(44):e17552. 10.1097/MD.0000000000017552
12.
Li T Li B Tan L Lv B . Reminiscence therapy as a potential method to improve psychological health and quality of life in elderly hepatocellular carcinoma patients: a randomized, controlled trial. Front Surg. (2022) 9:873843. 10.3389/fsurg.2022.873843
13.
Sternby Eilard M Hagstrom H Mortensen KE Wilsgaard T Vagnildhaug OM Dajani O et al Quality of life as a prognostic factor for survival in hepatocellular carcinoma. Liver Int. (2018) 38(5):885–94. 10.1111/liv.13593
14.
Wang YH Li JQ Shi JF Que JY Liu JJ Lappin JM et al Depression and anxiety in relation to cancer incidence and mortality: a systematic review and meta-analysis of cohort studies. Mol Psychiatry. (2020) 25(7):1487–99. 10.1038/s41380-019-0595-x
15.
Pinquart M Duberstein PR . Depression and cancer mortality: a meta-analysis. Psychol Med. (2010) 40(11):1797–810. 10.1017/S0033291709992285
16.
Taberna M Gil Moncayo F Jane-Salas E Antonio M Arribas L Vilajosana E et al The multidisciplinary team (MDT) approach and quality of care. Front Oncol. (2020) 10:85. 10.3389/fonc.2020.00085
17.
Cohen GS Black M . Multidisciplinary management of hepatocellular carcinoma: a model for therapy. J Multidiscip Healthc. (2013) 6:189–95. 10.2147/JMDH.S41206
18.
Ma W Zhang L Wang C Xu X . Effect of multidisciplinary team collaborative nursing model combined with mind mapping teaching method on postoperative complications and mental health of patients with advanced pancreatic cancer. Iran J Public Health. (2022) 51(3):535–43. 10.18502/ijph.v51i3.8929
19.
Han D Wang D Yang J Li X . Effect of multidisciplinary collaborative continuous nursing on the psychological state and quality of life of patients with cervical cancer. Am J Transl Res. (2021) 13(6):6654–61.
20.
Rui A Xu Q Yang X . Effect of multidisciplinary cooperative continuous nursing on the depression, anxiety and quality of life in gastric cancer patients. Am J Transl Res. (2021) 13(4):3316–22.
21.
Yang HL Wu XB Mao C . Block randomization in clinical trials. Zhonghua Yu Fang Yi Xue Za Zhi. (2019) 53(4):437–40. 10.3760/cma.j.issn.0253-9624.2019.04.022
22.
Wang H Xu C Zhang C . Application effect of continuous nursing based on multidisciplinary treatment model in postoperative patients with liver cancer. Chin Nurs Res. (2019) 33(7):1202–6.
23.
Liu L Wang J Ren L . Study on the effect of multidisciplinary collaborative nursing model on self-perceived burden and quality of life of patients with recurrence of primary liver cancer after operation. Tianjin J Nurs. (2021) 29(3):292–5.
24.
Aaronson NK Ahmedzai S Bergman B Bullinger M Cull A Duez NJ et al The European organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. (1993) 85(5):365–76. 10.1093/jnci/85.5.365
25.
Zigmond AS Snaith RP . The hospital anxiety and depression scale. Acta Psychiatr Scand. (1983) 67(6):361–70. 10.1111/j.1600-0447.1983.tb09716.x
26.
Nottelmann L Groenvold M Vejlgaard TB Petersen MA Jensen LH . A parallel-group randomized clinical trial of individually tailored, multidisciplinary, palliative rehabilitation for patients with newly diagnosed advanced cancer: the pal-rehab study protocol. BMC Cancer. (2017) 17(1):560. 10.1186/s12885-017-3558-0
27.
Norman EML Weil J Philip J . Hepatocellular carcinoma and its impact on quality of life: a review of the qualitative literature. Eur J Cancer Care. (2022) 31(6):e13672. 10.1111/ecc.13672
28.
Akbulut S Ozer A Saritas H Yilmaz S . Factors affecting anxiety, depression, and self-care ability in patients who have undergone liver transplantation. World J Gastroenterol. (2021) 27(40):6967–84. 10.3748/wjg.v27.i40.6967
29.
Lu L Yang J Zheng J Zhang C Yang Y Huang J . The effect of MDT collaborative nursing combined with hierarchical nursing management model on the quality of life and comfort of patients with gallbladder stones combined with acute cholecystitis after surgery. Comput Math Methods Med. (2022) 2022:8696084. 10.1155/2022/8696084
30.
Liu J Zong G Zhang C Li C Chen X Zhang Y . Anxiety and serum catecholamines as predictors of survival and recurrence in hepatocellular carcinoma. Psychooncology. (2017) 26(9):1347–53. 10.1002/pon.4305
31.
Akada K Koyama N Miura Y Aoshima K . Nationwide database analysis of insomnia, depression, and sleeping pill prescriptions in hepatocellular carcinoma patients. Curr Med Res Opin. (2022) 38(8):1333–9. 10.1080/03007995.2022.2081451
32.
Feldbrugge L Langenscheidt A Krenzien F Schulz M Krezdorn N Kamali K et al Health-related quality of life and mental health after surgical treatment of hepatocellular carcinoma in the era of minimal-invasive surgery: resection versus transplantation. Healthcare. (2021) 9(6):694. 10.3390/healthcare9060694
33.
Szelei A Dome P . Cancer and depression: a concise review. Orv Hetil. (2020) 161(22):908–16. 10.1556/650.2020.31759
34.
Shin JY Lim JW Shin DW Kim SY Yang HK Cho J et al Underestimated caregiver burden by cancer patients and its association with quality of life, depression and anxiety among caregivers. Eur J Cancer Care. (2018) 27(2):e12814. 10.1111/ecc.12814
35.
Lee HH Chiu CC Lin JJ Wang JJ Lee KT Sun DP et al Impact of preoperative anxiety and depression on quality of life before and after resection of hepatocellular carcinoma. J Affect Disord. (2019) 246:361–7. 10.1016/j.jad.2018.12.085
36.
Wang S Qian X . Effect of multidisciplinary team care on the management of cirrhotic patients with upper gastrointestinal bleeding: a retrospective cohort study. Ann Palliat Med. (2021) 10(3):3050–8. 10.21037/apm-21-85
37.
Liu J Peh CX Simard S Griva K Mahendran R . Beyond the fear that lingers: the interaction between fear of cancer recurrence and rumination in relation to depression and anxiety symptoms. J Psychosom Res. (2018) 111:120–6. 10.1016/j.jpsychores.2018.06.004
38.
Efird J . Blocked randomization with randomly selected block sizes. Int J Environ Res Public Health. (2011) 8(1):15–20. 10.3390/ijerph8010015
39.
Matts JP Lachin JM . Properties of permuted-block randomization in clinical trials. Control Clin Trials. (1988) 9(4):327–44. 10.1016/0197-2456(88)90047-5
Summary
Keywords
multi-disciplinary team care program, quality of life, anxiety, depression, hepatocellular carcinoma
Citation
Yang L, Yan C and Wang J (2023) Effect of multi-disciplinary team care program on quality of life, anxiety, and depression in hepatocellular carcinoma patients after surgery: A randomized, controlled study. Front. Surg. 9:1045003. doi: 10.3389/fsurg.2022.1045003
Received
15 September 2022
Accepted
08 November 2022
Published
06 January 2023
Volume
9 - 2022
Edited by
Sami Akbulut, İnönü University, Turkey
Reviewed by
Arif Emre, Kahramanmaras Sütçü Imam University, Turkey Alexander Reinisch, University of Giessen, Germany
Updates
Copyright
© 2023 Yang, Yan and Wang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Jingjing Wang jingjiu17855689543@163.com
These authors have contributed equally to this work
Specialty Section: This article was submitted to Surgical Oncology, a section of the journal Frontiers in Surgery
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.