Abstract
Fibrin sealants have recently been thoroughly studied in several surgical specialties; however, results are conflicting. We aimed to examine the safety and efficacy of fibrin sealant patients having thyroidectomies. A thorough, systematic literature search was carried out using the terms thyroidectomy and fibrin sealant using PubMed, Cochrane Library, and Clinicaltrials.gov on December 25, 2022. The primary outcome of interest in this review was the amount of drainage, whereas hospitalization, the length of drain retention, and temporary dysphonia were secondary outcomes. Our meta-analysis (n = 249) showed that application of fibrin sealant is associated with lesser total drainage [SMD −2.76 (−4.83, −0.69); P = 0.009; I2 97%], but not with retention time of drainage [SMD −2.35 (−4.71, 0.01); P = 0.05; I2 98%], hospitalization time [SMD −1.65 (−3.70, 0.41); P = 0.12; I2 97%], and transient dysphonia [RR 1.01 (0.27, 3.82); P = 0.99; I2 0%]. The systematic review found that the use of fibrin sealant in thyroid surgery is positive in total volume drainage but not with the retention time of drainage, hospitalization time, and transient dysphonia. It is notable to remember that this interpretation is complicated by uneven, occasionally subpar technique and trial reporting, according to this systematic review's findings.
1. Introduction
Thrombin and fibrinogen make up the two components of fibrin sealant (1). The final stable form of the substance, insoluble fibrin, is produced by the conversion of fibrinogen by thrombin in the presence of minute amounts of calcium and factor XIII. These products are used to seal biological tissues as two-component (i.e., fibrinogen and thrombin) liquid glue or as a two-component dry patch. Liquid glue formulations include Tisseel or Tissucol, Evicel, and dry patch products such as Tachosil and Tachocomb (2, 3). One of the earliest fibrin sealants among these products, Tisseel/Tissucol has been available for more than 30 years—it was originally offered on the European market in 1978 (4). There are two main active component groups in Tisseel. The first is the human thrombin and calcium chloride; the second is the human thrombin, synthetic aprotinin (anti-fibrinolytic), and Factor XIII (5, 6). When the two are combined and applied to tissue, the fibrinogen and thrombin create a fibrin clot that clings to the tissue, stops bleeding, and serves as bio glue.
Even though bleeding following thyroid surgery is uncommon, it can be fatal and necessitate an immediate reoperation. This fear makes surgeons do routine drains following any thyroid surgery (7). Although the presence of vascularized remnant tissue in partial thyroidectomy or Graves’ disease may increase the risk of bleeding, postoperative bleeding has been documented to occur as infrequently as 0.3% to 1% after thyroidectomy (8, 9).
The potential clinical benefits of fibrin sealant to patients and healthcare organizations are significant, which include a decrease in the frequency of postoperative complications (such as the formation of haematomas or seromas and infections) and a decrease in surgical wound drainage, which can reduce or eliminate the need for surgical drains (1). Woods et al. showed in a comprehensive review and meta-analysis of wound drain used following thyroid surgery that they were not always necessary and increased infection rates, postoperative pain, and length of hospital stay (10). On the other hand, there is a worry that some forms of fibrin sealants may have negative consequences, such as leaving deadly air pockets inside the body. Warnings have been issued by the Food and Drug Administration (FDA) in the USA regarding the development of potentially fatal air or gas emboli following the use of fibrin sealant aerosol sprays during surgery (11). The risks of employing sprays too closely to exposed tissue surfaces and at pressures higher than those advised by the makers have been made clear to users of the goods. Nevertheless, there is a lack of information from RCTs about damages despite safety concerns. In a multicenter RCT carried out in three institutions in Italy, the rate of unfavorable outcomes was compared in a group of patients receiving fibrin sealants as an adjuvant for preventing air leaks in patients having lung resection (12). Following these surgeries, broncopleural fistulas and air leaks are also frequent side effects (13, 14). The researchers discovered that there was no statistically significant difference in the rate of adverse events between patients who received fibrin sealant and those who did not, with a follow-up duration of 30—40 days (12).
Three published systematic studies have mainly addressed tonsillectomy and rhytidectomy when discussing tissue adhesives, not always fibrin sealant, in soft-tissue surgery of the head and neck (15–17). The most current systematic analysis on the use of tissue adhesives in rhytidectomy revealed that their usage considerably decreased the rate of haematoma formation and decreased the volume of surgical drainage (16). Results, however, have needed to be more consistent and frequently unfairly impacted by poor study design. To address these concerns, we conducted this systematic review and meta-analysis. We aimed to examine the safety and efficacy of fibrin sealant in patients undergoing thyroidectomies.
2. Materials and methods
This systematic review and meta-analysis adhered to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and was conducted manually (18). However, we did not register our study to the PROSPERO. A thorough, systematic literature search was carried out using the terms thyroidectomy and fibrin sealant using PubMed, Cochrane Library, and Clinicaltrials.gov. Table 1 displays specific search queries from each database. All authors did the literature search on December 25, 2022. Two authors (H.S. and V.S.) read the titles and abstracts and evaluated the possibly eligible papers using the inclusion and exclusion criteria. We settled any disagreements that arose during this procedure.
Table 1
| Electronic database | Search terms |
|---|---|
| PubMed | (“fibrin tissue adhesive"[MeSH Terms] OR (“fibrin"[All Fields] AND “tissue"[All Fields] AND “adhesive"[All Fields]) OR “fibrin tissue adhesive"[All Fields] OR (“fibrin"[All Fields] AND “sealant"[All Fields]) OR “fibrin sealant"[All Fields]) AND (((“thyroid gland"[MeSH Terms] OR (“thyroid"[All Fields] AND “gland"[All Fields]) OR “thyroid gland"[All Fields] OR “thyroid"[All Fields] OR “thyroid usp"[MeSH Terms] OR (“thyroid"[All Fields] AND “usp"[All Fields]) OR “thyroid usp"[All Fields] OR “thyroids"[All Fields] OR “thyroid s"[All Fields] OR “thyroidal"[All Fields] OR “thyroideal"[All Fields] OR “thyroidism"[All Fields] OR “thyroiditis"[MeSH Terms] OR “thyroiditis"[All Fields] OR “thyroiditides"[All Fields]) AND (“surgery"[MeSH Subheading] OR “surgery"[All Fields] OR “surgical procedures, operative"[MeSH Terms] OR (“surgical"[All Fields] AND “procedures"[All Fields] AND “operative"[All Fields]) OR “operative surgical procedures"[All Fields] OR “general surgery"[MeSH Terms] OR (“general"[All Fields] AND “surgery"[All Fields]) OR “general surgery"[All Fields] OR “surgery s"[All Fields] OR “surgerys"[All Fields] OR “surgeries"[All Fields])) OR (“thyroidectomy"[MeSH Terms] OR “thyroidectomy"[All Fields] OR “thyroidectomies"[All Fields]) OR (“hemithyroidectomies"[All Fields] OR “hemithyroidectomy"[All Fields])) |
| Cochrane Library | Fibrin sealant AND thyroid surgery OR thyroidectomy OR hemithyroidectomy |
| ClinicalTrials.gov | Fibrin sealant AND thyroid surgery OR thyroidectomy OR hemithyroidectomy |
Search strategy performed in each electronic database.
We included any published randomized clinical trials (RCTs) comparing fibrin sealant to control group, published in any year, written in any language, and having adult patients of any gender or ethnicity undergoing thyroid surgery that would typically necessitate the insertion of a surgical drain. RCTs with patients with fibrin sealant were used to cover the surgical dead space to reach underlying structures. Studies that were conference papers or abstracts-only publications, non-research letters, reviews, and editorial or commentaries were excluded.
The primary outcome of interest in this review was the amount of drainage, whereas hospitalization, the length of drain retention, and temporary dysphonia were secondary outcomes. We extracted the following details from each eligible study: first author, study design, fibrin sealant information, sample size, type of thyroid surgery, age, sex, and complications rate. We used a spreadsheet with predetermined column titles for each data entry to gather data. Formal requests were made to the principal investigators of included studies in cases where crucial information was missing.
We assessed the risk of bias independently, adhering to the Cochrane Risk of Bias (RoB) Assessment version 2 for RCTs. Any discrepancies were resolved by discussion.
We employed the inverse variance approach to evaluate continuous variables, and the pooled effect estimate was presented as standardized mean differences (SMD) with its standard deviation (SD). The risk ratios (RRs) and 95% confidence intervals (CIs) for dichotomous variables were calculated using the Mantel-Haenszel algorithm. In this meta-analysis, all p values were two-tailed, and the statistical threshold for significance was set at 0.05 (regardless of the heterogeneity, which is set at 0.10). To determine the origin of heterogeneity, We conducted a leave-one-out sensitivity analysis. Inverted funnel-plot analysis was used to evaluate the risk of publication bias qualitatively.
3. Results
After eliminating duplicate results, 206 records were left from the initial search's 363 records. We disregarded one hundred forty-eight records after title/abstract screening. We eliminated seven full-text articles after 11 full-text articles were assessed for eligibility due to the following reasons: did not report the key interests, not RCT, papers that reported other procedures, and an abstract published in a journal's supplementary file as it is presented in a conference. A total of 249 patients from 4 RCTs were included in this systematic review and meta-analysis (19–22). The most significant result was from Kim et al. (n = 78) showing the largest total drainage (93.5 ± 30.7 vs. 105.7 ± 31.2 ml for control and intervention group, respectively). However, the time to remove the drain was not shortened by the utilization of fibrin sealant (20). The PRISMA flow is depicted in Figure 1, and detailed characteristics of included studies are shown in Table 2.
Figure 1

PRISMA flow diagram for this systematic review and meta-analysis.
Table 2
| Study ID | Total cohort (n) | Total male (n) | Intervention details | Control details | Age (years) | Total thyroidectomy (n) | Total drainage (ml) | Funding |
|---|---|---|---|---|---|---|---|---|
| Vidal-Pérez 2016 | 30 vs. 30 | 5 vs. 9 | Tissucol FS | No FS | 52 ± 8 vs. 50 ± 7 | 30 vs. 30 | 51 (29–72) vs. 110 (74–132) | |
| Uwiera 2005 | 26 vs. 30 | 4 vs. 11 | Tisseel FS | No FS | 49 (27–73) vs. 50 (26–66) | 16 vs. 9 | 53.4 ± 7.5 vs. 24.5 ± 4.6 | |
| Kim 2012 | 38 vs. 40 | 6 vs. 13 | Berplast P FS | No FS | 47.8 ± 9.6 vs. 50.8 ± 10.8 | 38 vs. 40 | 93.5 ± 30.7 vs 105.7 ± 31.2 | Samsung Medical Center |
| NCT01226914 | 28 vs. 27 | 4 vs. 3 | Evicel FS | Saline Placebo | 48.8 ± 15.2 vs. 51.9 ± 11.5 | 18 vs. 17 | 96.3 (73.3–139.3) vs 120 (68.8–161.5) | Ethicon, Inc. |
Summary characteristics of included studies (n = 249).
Our meta-analysis showed that application of fibrin sealant is associated with lesser total drainage [SMD −2.76 (−4.83, −0.69); P = 0.009; I2 97%], but not with retention time of drainage [SMD −2.35 (−4.71, 0.01); P = 0.05; I2 98%], hospitalization time [SMD −1.65 (−3.70, 0.41); P = 0.12; I2 97%], and transient dysphonia [RR 1.01 (0.27, 3.82); P = 0.99; I2 0%]. Meta-analyses can be seen in Figures 2–5 for total drainage, retention time of drainage, hospitalization time, and transient dysphonia, respectively.
Figure 2
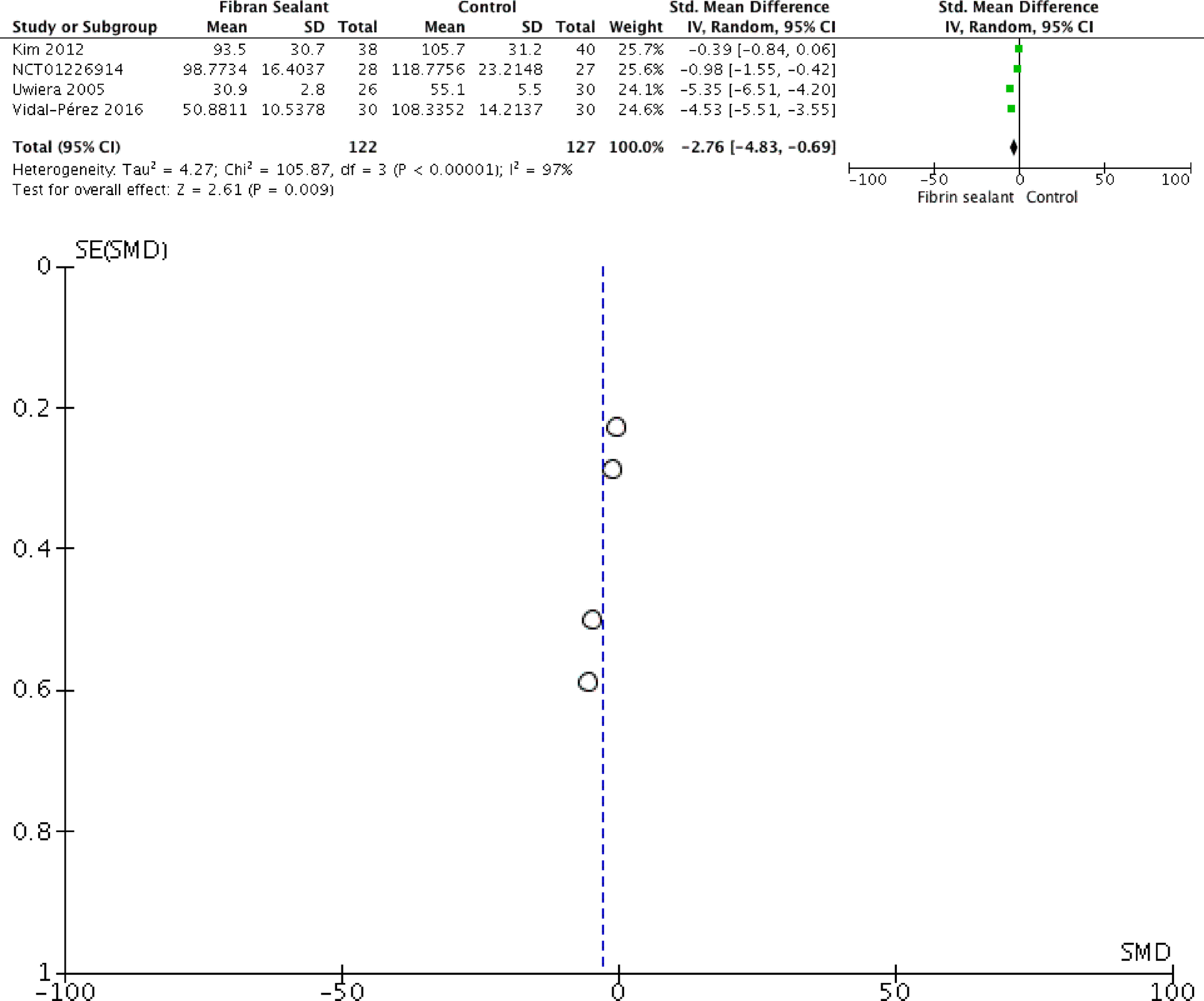
Forest and funnel plot for total drainage.
Figure 3

Meta-analysis for retention time of drainage between intervention and control arm.
Figure 4

Meta-analysis for hospitalization time.
Figure 5
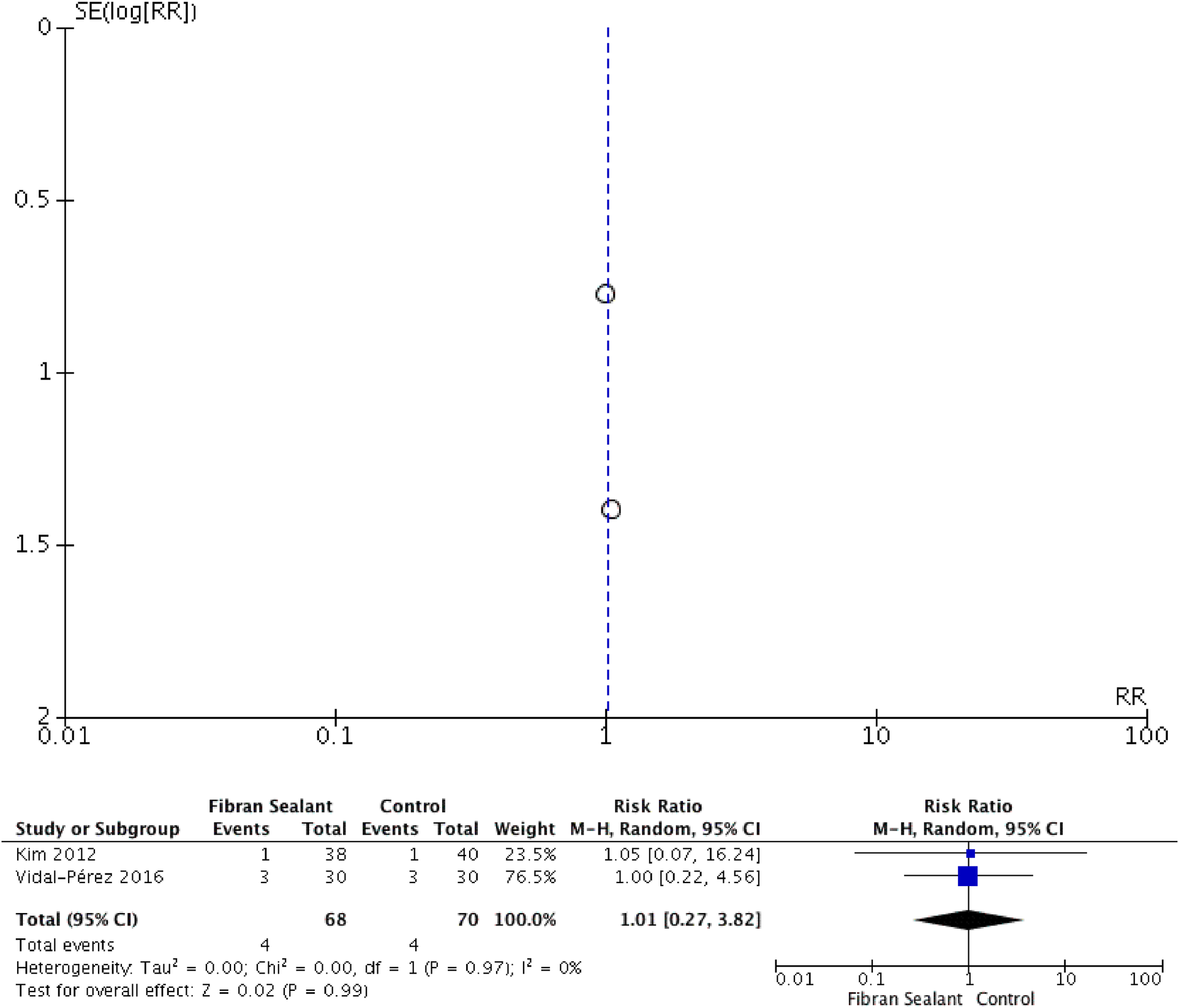
Forest plot and meta-analysis for patients experiencing transient dysphonia.
3.1. Risk of bias
The relationship between fibrin sealant and thyroidectomy was visualized using a funnel-plot analysis as a qualitatively symmetrical inverted funnel-plot. Our Risk of Bias Cochrane version 2 also showed that all included RCTs were of low risk of bias. Detailed risk of bias were represented in Figure 6.
Figure 6
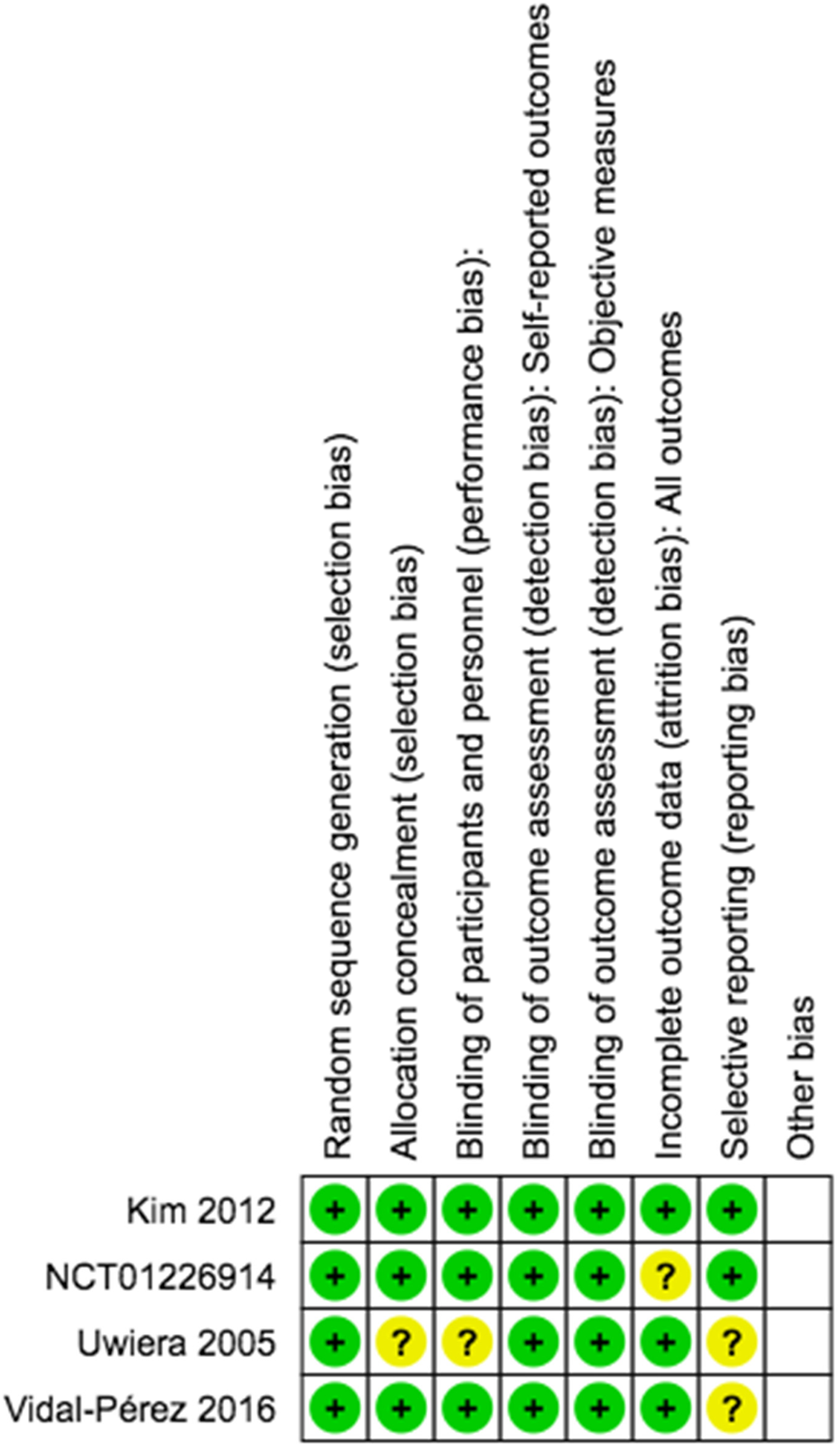
Risk of bias assessment version 2.
4. Discussions
Most surgical procedures have traditionally employed drains (23, 24). It has been a standard procedure to drain wounds following thyroid and parathyroid surgery. However, in neck surgeries, the likelihood of a significant postoperative haemorrhage is relatively low and does not appear to rise in the absence of drains (25, 26). The primary uses of a drain have historically been to prevent postoperative problems by removing lymphatic or postoperative bleeding and notifying the surgeon of any early postoperative bleeding. A surgeon typically inserts drains to stop bleeding and detect it early after thyroid surgeries. However, drain implantation increases the risk of infection and lengthens the hospital stay (27, 28). Patients are typically released from the hospital on the day of surgery because it is known that the risk of respiratory failure brought on by a haematoma is highest in the first six hours following thyroid surgery (29). Additionally, the drains may cause more drainage because of the inflammation they cause by simply being there (30, 31). The lymphatics may not be able to shut off due to the vacuum caused by the drain's negative pressure, which would increase seroma production and drainage. According to Schoretsanitis et al., the non-drained group's VAS score is reduced by about 50%. Most of the non-drained patients in this trial also saw a significant reduction in postoperative pain, particularly on postoperative day 1 (32). These findings demonstrated that drain placement might be directly related to the patient's postoperative discomfort by raising postoperative pain. The last concern is about the incidence of hematomas or seromas formation following thyroidectomy. Surgeons have become interested in having no drainage after thyroid surgery. However, the volume that drains spontaneously after surgery could not be predicted, therefore research to date have been constrained. An interesting study by Woo et al. from South Korea revealed that there was no increase in the likelihood of hematoma or seroma formation when a negative pressure drain was used to improve drainage during the first 24–48 h postoperatively (31).
Our study showed that applying fibrin sealant is associated with lesser overall drainage. A prospective RCT conducted by Docimo et al. assess the various hemostatic approaches in patients undergoing total thyroidectomy. In the intervention cohort receiving hemostatic agent was found to be effective at reducing postsurgical drain output and provides a complementary hemostatic approach in patients undergoing total thyroidectomy (48 ± 19.2 vs. 98.3 ± 23.1 ml in intervention and control group, respectively; 95% CI −63.2 to −31.2; p-value < 0.0001) (33). While other outcomes of interest, which include retention time of drainage, hospitalization time, and transient dysphonia, did not result in a statistically significant manner. Previous research revealed that the first 6 h following thyroid surgery have the highest risk of respiratory failure due to hemorrhage, which makes it discouraged to discharge patients on the day of surgery (34, 35). The length of hospitalization is a key factor in cost analysis, and numerous studies have demonstrated the connection between the length of hospitalization and the use of drains (18, 35, 36). In contrast to their potential to shorten hospital stays and increase discomfort, drains have not demonstrated the ability to reduce postoperative complications.
Regarding mean total drainage volume, there was significant statistical heterogeneity in the sub-group analysis of thyroidectomy trials. The different cut-off volumes may have caused this heterogeneity for drain removal used in the studies by Hornig et al. and Uwiera et al. (10 ml/8 hr and 10 ml/24 hr, respectively) (19, 21). The considerable statistical heterogeneity tempers the significant reduction of 36.36 ml in the mean total drainage volume for thyroidectomy in the fibrin sealant arm compared to the control. In contrast to a meta-analysis which showed that not using drains was safe and may even be beneficial, Hornig et al. and Uwiera et al. reported a mean total drainage volume ranging from about 70 — 120 ml (21). One would expect 70 — 120 ml in the anterior neck to be clinically apparent and require aspiration or evacuation. It is unknown whether this discrepancy results from the wound's closed suction drain's stimulating impact. It is challenging to make a case for employing fibrin sealant because Woods et al. have demonstrated that drains are not typically necessary in thyroid surgery (10). According to the current meta-analysis, fibrin sealant may reduce drainage volume, but this has yet to result in a noticeably different clinical outcome (both in the pooled and individual study analysis) (37). Other than stating that fibrin sealant is safe to employ, the study's findings do little to alter the practices of surgeons who already do drainless surgery. The use of fibrin sealant in patients more susceptible to problems needs more research.
In thyroid and parathyroid surgery, fibrin sealants offer a comparative advantage over under-flap suction. The agony patients experience when a drain is removed is also avoided using fibrin glue, which is also less expensive. According to Patel et al., the use of fibrin glue led to a statistically significant reduction in the number of time patients needed to spend in the hospital after undergoing both forms of surgery (124 patients who had undergone thyroidectomy and 47 patients who had undergone parathyroidectomy; p = 0.022 and 0.033, respectively). Another crucial point is that a pyriform sinus fistula-caused instance of recurrent suppurative thyroiditis was successfully treated by injecting fibrin glue (38).
4.1. Adverse reactions
Adverse events suspected to be connected to fibrin sealants were reported in several RCTs in different surgical specialities. Death following the use of fibrin sealant may be connected to the use of fibrin sealant in upper GI tract surgery caused by a significant bleed; however, there was no evidence of bleeding at the intended bleeding site. Various modest adverse events, such as mild cellulitis and mild seroma, anaemia, urine extravasation, incision site problems, and a slight generalized skin rash, were also mentioned in other RCTs. Excessive discomfort, scar pain, testicular pain hydrocele, and post-procedural hemorrhage antibodies all had varying degrees of severity. The severity of adverse events or their relationship to the use of fibrin sealant was not disclosed. After surgery, unfavourable outcomes happened instantly, after two hours, after 24 h, after 14 days, and 32 days (39).
4.2. Clinical implication
Human fibrinogen and its various constituent parts create fibrin glue, a sticky biological substance (40). By boosting homeostasis and angiogenesis and inducing macrophages, which play a role in fibroblast proliferation and collagen formation at the wound site, fibrin glue aids in wound healing (41, 42). In thyroid and parathyroid surgery, fibrin sealants offer a comparative advantage over under-flap suction (43–45). The agony patients experience when a drain is removed is also avoided using fibrin glue, which is also less expensive.
4.3. Limitation
The publication bias shown by the funnel plot represents a limitation of this systematic review and meta-analysis due to the small number of studies included. Due to the novelty and dearth of RCTs using fibrin sealant, the sample size was similarly modest. Although fibrin sealant tended to shorten hospital stays, this was not statistically significant and was confounded by solid statistical heterogeneity. It could not do a meta-analysis of postoperative pain because none of the included studies covered it. Lastly, we were not able to conduct a cost-benefit analysis.
In conclusion, the systematic review found that the use of fibrin sealant in thyroid surgery is positive in total volume drainage but not with the retention time of drainage, hospitalization time, and transient dysphonia. It is notable to remember that this interpretation is complicated by uneven, occasionally subpar technique and trial reporting, according to this systematic review's findings. As a result, it is inescapably difficult to draw definitive conclusions from meta-analyses. Additional clinical trials using sound methodology are required. This is especially true for lateral neck dissection, where there are few randomized data and where the potential for the most significant benefit is there.
Statements
Author contributions
All authors were responsible for the conception and design of the work and the drafting of the manuscript; JH analyzed the data; HS and VS revised the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Noori A Ashrafi SJ Vaez-Ghaemi R Hatamian-Zaremi A Webster TJ . A review of fibrin and fibrin composites for bone tissue engineering. Int J Nanomedicine. (2017) 12:4937–61. 10.2147/IJN.S124671
2.
Nativ O Patel B Shen J Batiller J Horn S Hart JC . Safety and hemostatic efficacy of fibrin pad in partial nephrectomy: results of an open-label phase I and a randomized, standard-of-care-controlled phase I/II study. BMC Nephrol. (2012) 13:147. 10.1186/1471-2369-13-147
3.
Tavilla G Bruggemans EF Gielen CLI Brand A van den Hout WB Klautz RJM et al Multicentre randomized clinical trial to investigate the cost-effectiveness of an allogeneic single-donor fibrin sealant after coronary artery bypass grafting (FIBER study). Br J Surg. (2015) 102:1338–47. 10.1002/bjs.9877
4.
Fortelny RH Petter-Puchner AH Glaser KS Redl H . Use of fibrin sealant (tisseel/tissucol) in hernia repair: a systematic review. Surg Endosc. (2012) 26:1803–12. 10.1007/s00464-012-2156-0
5.
Su Y-Y Lin Y-S Yang L-Y Pan Y-B Huang Y-T Weng CH et al Use of human fibrin glue (Tisseel) versus suture during transvaginal natural orifice ovarian cystectomy of benign and non-endometriotic ovarian tumor: a retrospective comparative study. BMC Surg. (2021) 21:49. 10.1186/s12893-021-01061-1
6.
Villalonga JF Solari D Guizzardi G Scala MR Campero A . Fat and fibrin glue: quo vadis?Turk Neurosurg. (2021) 31:238–46. 10.5137/1019-5149.JTN.29712-20.2
7.
Pino A Frattini F Sun H Zhang D Wu C Kim H et al Use of vivostat® autologous fibrin sealant in thyroid surgery. Surg Technol Online. (2021) 38:57–61. 10.52198/21.STI.38.SO1441
8.
Dixon JL Snyder SK Lairmore TC Jupiter D Govednik C Hendricks JC . A novel method for the management of post-thyroidectomy or parathyroidectomy hematoma: a single-institution experience after over 4,000 central neck operations. World J Surg. (2014) 38:1262–7. 10.1007/s00268-013-2425-7
9.
Contin P Gooßen K Grummich K Jensen K Schmitz-Winnenthal H Büchler MW et al ENERgized vessel sealing systems versus CONventional hemostasis techniques in thyroid surgery—the ENERCON systematic review and network meta-analysis. Langenbeck’s Arch Surg. (2013) 398:1039–56. 10.1007/s00423-013-1137-7
10.
Woods RSR Woods JFC Duignan ES Timon C . Systematic review and meta-analysis of wound drains after thyroid surgery. Br J Surg. (2014) 101:446–56. 10.1002/bjs.9448
11.
O’Hanlan KA Bassett P . Exploring adverse events and utilization of topical hemostatic agents in surgery. JSLS J Soc Laparoendosc Surg. (2022) 26(3):e2022.00033. 10.4293/JSLS.2022.00033
12.
Cardillo G Carleo F Carbone L De Massimi AR Lococo A Santini PF et al Adverse effects of fibrin sealants in thoracic surgery: the safety of a new fibrin sealant: multicentre, randomized, controlled, clinical trial. Eur J Cardio-Thoracic Surg. (2012) 41:657–62. 10.1093/ejcts/ezr083
13.
Ramot Y Steiner M Lavie Y Ezov N Laub O Cohen E et al Safety and efficacy of sFilm-FS, a novel biodegradable fibrin sealant, in Göttingen minipigs. J Toxicol Pathol. (2021) 34:319–30. 10.1293/tox.2021-0030
14.
Mahmoodzadeh H Rahimi-Movaghar E Omranipour R Shirkhoda M Jalaeefar A Miri SR et al The effect of fibrin glue on the postoperative lymphatic leakage after D2-lymphadenectomy and gastrectomy in patients with gastric cancer. BMC Surg. (2021) 21:155. 10.1186/s12893-021-01168-5
15.
Por Y-C Shi L Samuel M Song C Yeow VK-L . Use of tissue sealants in face-lifts: a metaanalysis. Aesthetic Plast Surg. (2009) 33:336–9. 10.1007/s00266-008-9280-1
16.
Killion EA Hyman CH Hatef DA Hollier LH Reisman NR . A systematic examination of the effect of tissue glues on rhytidectomy complications. Aesthetic Surg J. (2015) 35:229–34. 10.1093/asj/sju078
17.
Sproat R Radford P Hunt A . Hemostatic glues in tonsillectomy: a systematic review. Laryngoscope. (2016) 126:236–42. 10.1002/lary.25256
18.
Rosen P Bailey L Manickavel S Gentile C Grayson J Buczek E . Ambulatory surgery vs overnight observation for total thyroidectomy: cost analysis and outcomes. OTO open. (2021) 5:2473974X21995104. 10.1177/2473974X21995104
19.
Hornig JD Gillespie MB Lentsch EJ Fuller CW Condrey J Nguyen SA . Fibrin sealant use in thyroidectomy: a prospective, randomized, placebo-controlled double blind trial using EVICEL. Otorhinolaryngol Neck Surg. (2016) 1:21–4. 10.15761/OHNS.1000106
20.
Kim TW Choi SY Jang M-S Lee G-G Nam M-E Son Y-I et al Efficacy of fibrin sealant for drainage reduction in total thyroidectomy with bilateral central neck dissection. Otolaryngol Neck Surg. (2012) 147:654–60. 10.1177/0194599812449315
21.
Uwiera TC Uwiera RRE Seikaly H Harris JR . Tisseel and its effects on wound drainage post-thyroidectomy: prospective, randomized, blinded, controlled study. J Otolaryngol. (2005) 34:374. 10.2310/7070.2005.34603
22.
Vidal-Pérez Ó Flores-Siguenza L Valentini M Astudillo-Pombo E Fernández-Cruz L García-Valdecasas JC . Aplicación de sellante de fibrina en pacientes operados por cáncer diferenciado de tiroides. ¿qué mejoramos?Cir Cir. (2016) 84:282–7. 10.1016/j.circir.2015.02.004
23.
Clapp B Lodeiro C Dodoo C Coleman G Sadri B Wicker E et al Trends in drain utilization in bariatric surgery: an analysis of the MBSAQIP database 2015-2017. Obes Surg. (2020) 30:569–79. 10.1007/s11695-019-04215-6
24.
Sethia R Freeman T Mead K Selhorst A Vala K Skoracki L et al Patient-Directed home drain removal in head and neck surgery. Laryngoscope. (2021) 131:2471–7. 10.1002/lary.29556
25.
Perigli G Cianchi F Badii B Staderini F Skalamera I Cupellini C et al An easier option for “invisible scar” thyroidectomy: hybrid-transoral endoscopic thyroidectomy submental access (H-TOETSA)-experience on twenty-two consecutive patients. Surg Endosc. (2021) 35:1796–800. 10.1007/s00464-020-07576-7
26.
Ramouz A Rasihashemi SZ Safaeiyan A Hosseini M . Comparing postoperative complication of LigaSure small jaw instrument with clamp and tie method in thyroidectomy patients: a randomized controlled trial [IRCT2014010516077N1]. World J Surg Oncol. (2018) 16:154. 10.1186/s12957-018-1448-9
27.
Hernández-Avendaño V Jiménez-López M . Drains after thyroid surgery. Rev Med Inst Mex Seguro Soc. (2020) 58:543–7. 10.24875/RMIMSS.M20000083
28.
Abboud B El-Kheir A . Redo thyroid surgery without drains. Surg Today. (2020) 50:1619–25. 10.1007/s00595-020-02065-9
29.
Papini E Monpeyssen H Frasoldati A Hegedüs L . 2020 European thyroid association clinical practice guideline for the use of image-guided ablation in benign thyroid nodules. Eur Thyroid J (2020) 9:172–85. 10.1159/000508484
30.
Kahaly GJ . Management of graves thyroidal and extrathyroidal disease: an update. J Clin Endocrinol Metab. (2020) 105:3704–20. 10.1210/clinem/dgaa646
31.
Woo SH Kim JP Park JJ Shim HS Lee SH Lee HJ et al Comparison of natural drainage group and negative drainage groups after total thyroidectomy: prospective randomized controlled study. Yonsei Med J. (2013) 54:204–8. 10.3349/ymj.2013.54.1.204
32.
Schoretsanitis G Melissas J Sanidas E Christodoulakis M Vlachonikolis JG Tsiftsis DD . Does draining the neck affect morbidity following thyroid surgery?Am Surg. (1998) 64:778–80.
33.
Docimo G Tolone S Conzo G Limongelli P Del Genio G Parmeggiani D et al A gelatin–thrombin matrix topical hemostatic agent (floseal) in combination with harmonic scalpel is effective in patients undergoing total thyroidectomy. Surg Innov. (2016) 23:23–9. 10.1177/1553350615596638
34.
Anuwong A Ketwong K Jitpratoom P Sasanakietkul T Duh Q-Y . Safety and outcomes of the transoral endoscopic thyroidectomy vestibular approach. JAMA Surg. (2018) 153:21–7. 10.1001/jamasurg.2017.3366
35.
Khadra H Bakeer M Hauch A Hu T Kandil E . Hemostatic agent use in thyroid surgery: a meta-analysis. Gland Surg. (2018) 7:S34–41. 10.21037/gs.2018.03.02
36.
Memeh K Ruhle B Vaghaiwalla T Kaplan E Keutgen X Angelos P . Thyroidectomy for euthyroid patients with Hashimoto thyroiditis and persisting symptoms: a cost-effectiveness analysis. Surgery. (2021) 169:7–13. 10.1016/j.surg.2020.03.028
37.
Coey JG Whittaker PJ Williams G Ikram UH Page OJR . Fibrin tissue adhesive versus nasal packing in endoscopic nasal surgery: a systematic review and meta-analysis. Rhinol J. (2019) 57(1):21–31. 10.4193/Rhin18.112
38.
Patel M Garg R Rice DH . Fibrin glue in thyroid and parathyroid surgery: is under-flap suction still necessary?Ear Nose Throat J. (2006) 85:530–2. 10.1177/014556130608500818
39.
Allotey JK King AH Kumins NH Wong VL Harth KC Cho JS et al Systematic review of hemostatic agents used in vascular surgery. J Vasc Surg. (2021) 73:2189–97. 10.1016/j.jvs.2020.10.081
40.
Montano N Giordano M Caccavella VM Ioannoni E Polli FM Papacci F et al Hemopatch® with fibrin glue as a dural sealant in cranial and spinal surgery. A technical note with a review of the literature. J Clin Neurosci. (2020) 79:144–7. 10.1016/j.jocn.2020.07.011
41.
Versteeg HH Heemskerk JWM Levi M Reitsma PH . New fundamentals in hemostasis. Physiol Rev. (2013) 93:327–58. 10.1152/physrev.00016.2011
42.
Spotnitz WD . Fibrin sealant: past, present, and future: a brief review. World J Surg (2010) 34:632–4. 10.1007/s00268-009-0252-7
43.
Sekyi-Djan N Chapple C Myuran T Hammond-Kenny A Hilger A . Corrigendum to: the use of ARTISS fibrin sealant in thyroid surgery: case series and review of the literature. Br J Surg. (2022) 109:1130–1130. 10.1093/bjs/znac303
44.
Gubitosi A Ruggiero R Docimo G Esposito A . Fibrin sealant in general surgery. Personal experience and literary review. Ann Ital Chir. (2014) 85:153–8.
45.
Page MJ McKenzie JE Bossuyt PM Boutron I Hoffmann TC Mulrow CD et al The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372:1–9. 10.1136/BMJ.N71
Summary
Keywords
fibrin sealant, thyroidectomy, randomized controlled trials, volume drainage, systematic review
Citation
Koerniawan HS, Candrawinata VS, Tjahyanto T, Wijaya NJ, Putra AW and Wijaya JH (2023) The safety and efficacy of fibrin sealant for thyroidectomy: a systematic review and meta-analysis of randomized controlled trials. Front. Surg. 10:1149882. doi: 10.3389/fsurg.2023.1149882
Received
23 January 2023
Accepted
18 May 2023
Published
20 June 2023
Volume
10 - 2023
Edited by
Rui Seabra Ferreira, São Paulo State University, Brazil
Reviewed by
Fausto Fama, University of Messina, Italy Sebastiano Bonventre, University of Palermo, Italy
Updates
Copyright
© 2023 Koerniawan, Candrawinata, Tjahyanto, Wijaya, Putra and Wijaya.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Jeremiah Hilkiah Wijaya Jeremiah.hansum6@gmail.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.