- 1Department of Orthopedics, Gatam Institute, Tangerang, Indonesia
- 2Department of Orthopedic Surgery, Fatmawati Hospital, Jakarta, Indonesia
- 3Department of Orthopedic Surgery, Premier Bintaro Hospital, Tangerang, Indonesia
- 4Department of Orthopedic Surgery, Faculty of Medicine, Universitas Trisakti, Jakarta, Indonesia
Introduction: Robotic-assisted techniques in minimally invasive spine surgery are recognized for their potential to enhance surgical precision, minimize intraoperative complications, and improve clinical outcomes. A significant advantage of robotics in oblique lateral interbody fusion (OLIF) is the capability to perform single-position surgery, allowing simultaneous anterior and posterior procedures without the need to reposition the patient.
Methods: A retrospective review of 25 consecutive patients who underwent robotic-navigated single-position OLIF spine surgery was performed. Data collected included back and leg pain scores (VAS), screw placement accuracy, operative time, estimated blood loss, postoperative length of stay, and surgical complications.
Results: In total, 116 screws were placed robotically in 25 patients, with a mean age of 62.2 ± 8.9 years. Diagnoses included grade 1 (10 patients) or grade 2 (7 patients) spondylolisthesis and degenerative disc disease (8 patients). The mean operative time from incision to closure was 101.2 ± 7.2 min, with an estimated intraoperative blood loss of 90.0 ± 16.6 ml. VAS scores for leg and back pain improved from preoperative to six months postoperative (from 3.6 to 1 for leg pain and 5.3 to 1 for back pain). Two major vein complications and one retrograde ejaculation.
Conclusion: Single-position OLIF shows promising results, with robotic guidance offering substantial benefits, including reduced bleeding, fewer surgical complications, and shorter operative times, all without flipping the patient. Robotic assistance in OLIF holds great potential and broad application prospects in spine surgery.
Introduction
Spine surgery has significantly evolved over the past decade, moving from conventional open procedures to minimally invasive spine surgery, which has now become the standard approach for managing various spinal pathologies (1). Minimally invasive spine surgery reduces soft tissue damage around the surgical site, resulting in smaller incisions, decreased blood loss, and quicker recovery to normal activities (1, 2). Surgeons utilize percutaneous pedicle screws and specialized posterior or lateral lumbar retractors to accomplish these objectives. While minimally invasive surgery has shown favorable outcomes, it should be noted that there is radiation exposure to patients, surgeons, and operating room personnel (3).
Robotic navigation in spine surgery addresses concerns about radiation exposure by enabling real-time instrument and pedicle screw tracking without radiation (4). Spinal surgery is complex because it is close to nerves and major blood vessels, making precision and accuracy essential. Robotic assistance can enhance accuracy and minimize human error (5).
Lateral lumbar surgery is one of the surgical techniques that is benefited by robotic navigation technology. Traditionally, surgeons need to flip the patient from the lateral decubitus position to the prone after the implantation of the interbody cage for fusion; this flip will lengthen the surgical time, increase patient exposure to the anesthetic agent, and increase hospital operating room time, which could increase the total unit cost. Recently, the Oblique Lateral Interbody Fusion (OLIF) technique has gained attention for its advantages, particularly its retroperitoneal approach, which eliminates the need to divide the psoas major muscle while reducing the risk of injury to major vessels, the ureter, and the lumbar plexus.
The current retrospective study aimed to investigate the feasibility of a robot-assisted OLIF procedure for degenerative disc disease of the lumbar spine.
Material and methods
This is a retrospective cohort study of 25 patients who underwent an oblique lateral interbody fusion with robotic navigation percutaneous screw fixation. A team of four spine surgeons performed all surgeries from September to December 2022. All data were obtained through the extraction of inpatient medical records.
The inclusion criteria were: (1) Patients diagnosed varied from grade 1 or 2 degenerative spondylolisthesis and degenerative disc disease. (2) Patients with conservative treatment showed no significant effects after 3–6 months.
We evaluate clinical outcomes after surgery in the form of visual analog scale (VAS) back pain and leg pain, the screw accuracy, operating time, estimated blood loss, postoperative length of stay (LOS), and complications after surgery. The VAS 0 indicated no pain, and 10 represented the worst pain. These scores were collected preoperatively, one, three, and six months post-surgery. Screw accuracy was assessed using a post-operative CT scan. The operative time was counted as the interval from the initial skin incision to the skin closure. Estimated blood loss (EBL) was measured intraoperatively from a suction bottle and gauze. Postoperative LOS was the hospitalization period from hospital administration to postoperative without the need for analgesics. Complications were measured intraoperative, postoperative, and during follow-up time.
Surgical technique
Registration
The ExclesiusGPS robotic platform (Globus Medical; Audubon, PA, USA) is securely attached to both the bed and the patient's spine at the posterior superior iliac spine. Two fluoroscopic images align the patient's anatomical position with the preoperative segmented CT images. It is crucial to minimize any patient movement to avoid errors in the registration process.
Anesthesia and position
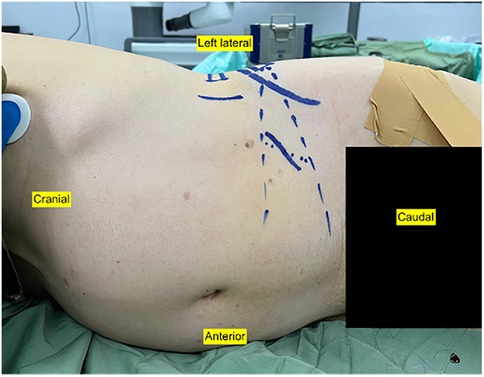
The patient is positioned in the lateral decubitus position with the left side up under general anesthesia (Figure 1). This position allowed the surgeons to work simultaneously from anterior and posterior, OLIF from the anterior side, and percutaneous robotic navigated screw from the posterior side.
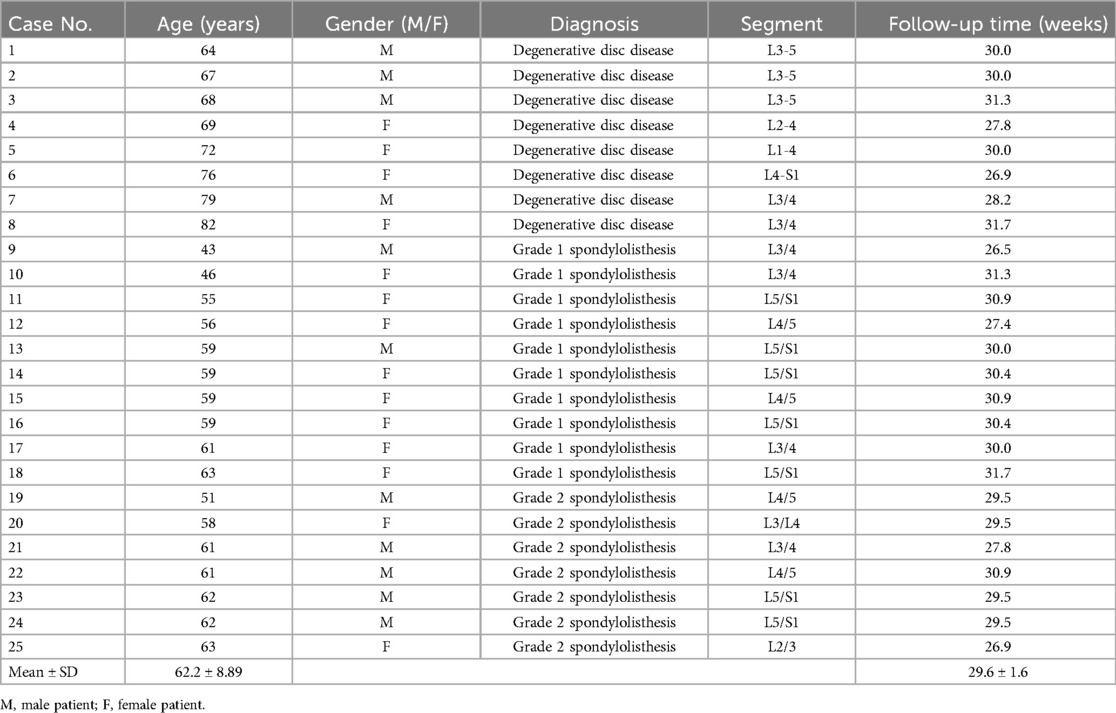
Software planning
The ExcelsiusGPS planning software sets targets and designs construct trajectories based on the patient's preoperative or intraoperative CT scans. Successful planning with the CT scans and the ExcelsiusGPS system includes meticulous instrument registration and precise screw trajectory mapping to minimize potential complications (Figure 2).
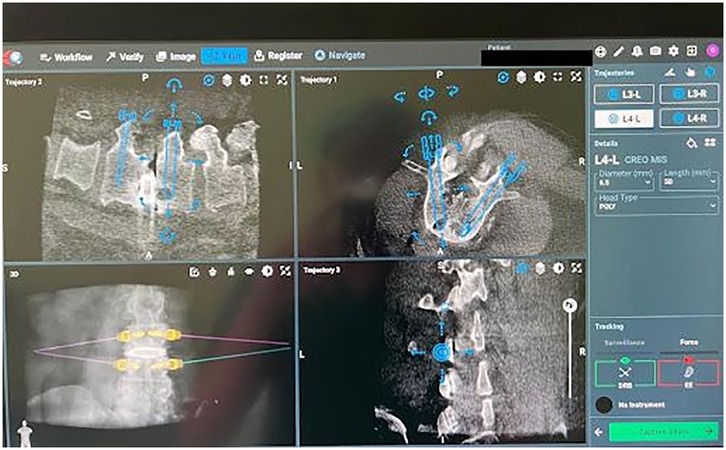
Figure 2. ExcelsiusGPS software screw planning includes entry points, trajectories, screw length, and width.
Posterior procedure
Insertion of the percutaneous posterior screw was navigated by the robotic system (Figure 3). We implemented a preoperative workflow that involved registering the preoperative CT scan into the Excelsius GPS system and merging the intraoperative C-arm images with the CT scan. Dynamic reference frames and surveillance markers were affixed to the iliac wing to prevent obstruction during procedures, whether utilizing the robot or performing the OLIF. A single midline skin incision was made. The robotic-assisted technique for screw placement initiates with the insertion of a robotic knife down to the bone, followed by the navigated dilator and cannula. Subsequently, the navigated drill, tap, and pedicle screw are advanced along the robotic arm. Screw placement is performed from proximal to distal to enhance accuracy and minimize errors. The right side is addressed first to facilitate the downward drainage of any incisional bleeding; starting with the left side could lead to obscuration of surgical field by blood later on. Once all screws were positioned, the anterior surgeon performed the discectomy as decompression procedure and cage placement. After completing these steps, the pedicle screws were then secured.
Anterior procedure
The robotic arm is aligned with pre-planned disc spaces, marking the skin to guide the surgical corridor. In OLIF, incisions were placed 5–7 cm from the center of the disc, depending on the level of the pathology. External oblique, internal oblique and transversal fascia were split until we saw the peritoneum and retroperitoneal fat (Figure 4). The peritoneum was released from surrounding tissue by finger dissection until we could palpate the psoas muscle. The robotic arm assists in posterior screw placement while the anterior surgeon exposes the disc spaces. It is crucial to avoid patient movement to prevent errors in robotic guidance. If the posterior surgeon is still working, the L5-S1 disc is exposed first through an oblique corridor, followed by L4–5 and L3–4. Once screw placement is complete, the anterior surgeon proceeds with discectomy, dilating, and the cage is inserted in a standard OLIF fashion (Figures 5, 6). Closure begins simultaneously as the posterior surgeon finishes.
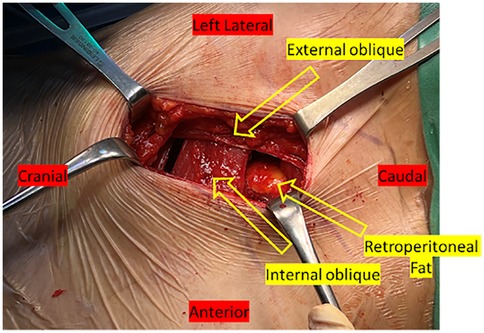
Figure 4. An intraoperative image displays retroperitoneal fat visible following the division of the muscles and fascia.

Figure 6. The intraoperative C-arm image displays the interbody cage placement. The implant should span the entire apophyseal ring.
Results
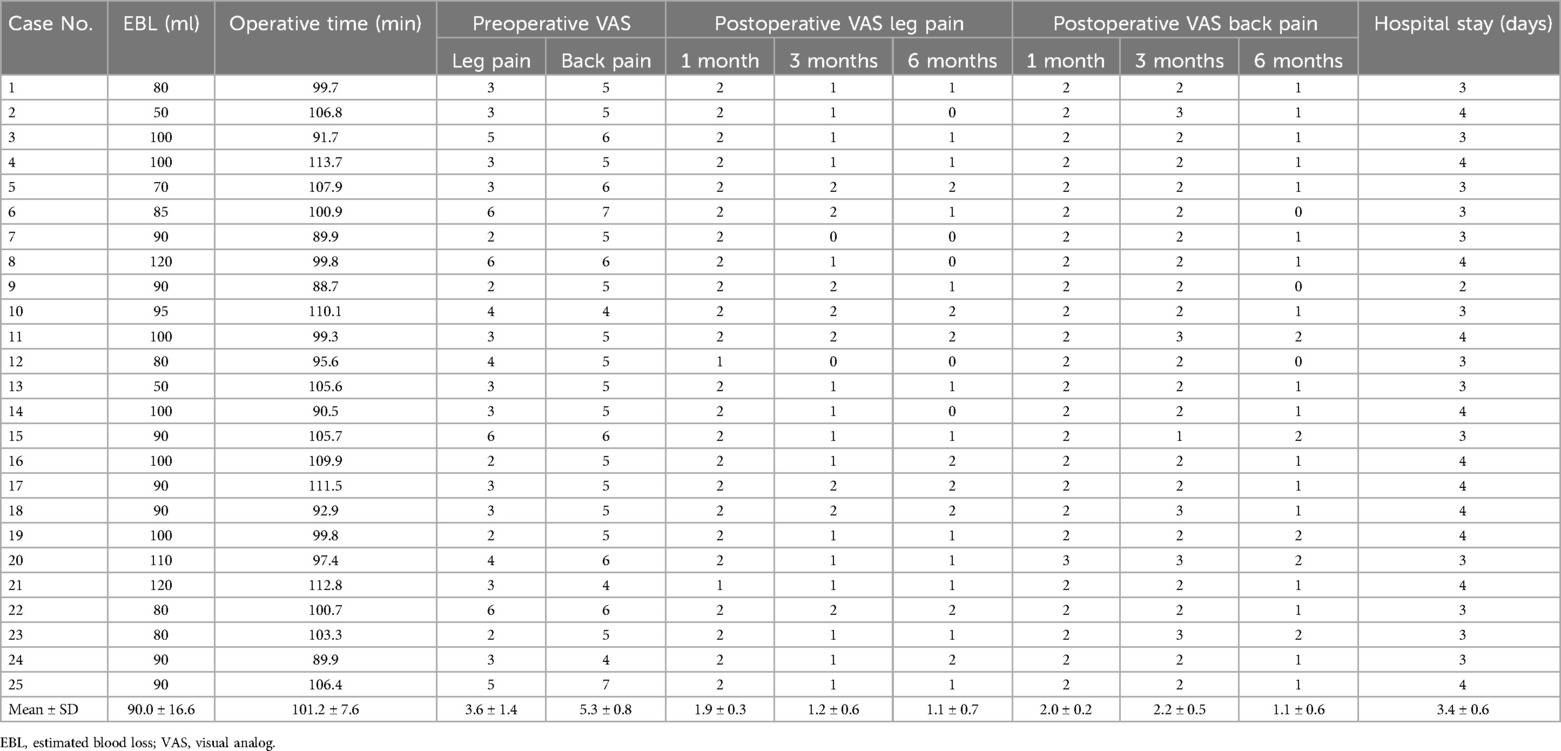
A total of 25 patients were included in the study. The diagnosis was grade 1 spondylolisthesis (10 patients), grade 2 spondylolisthesis (7 patients), and degenerative disc disease (8 patients). Their mean age was 62.2 years old (range 43–82 years), with an average follow-up of 29.6 ± 1.6 weeks after surgery (Table 1). The mean preoperative VAS of leg pain was 3.6, and the mean VAS of back pain was 5.3. The outcomes of this study are as follows; further details can be found in Table 2.
VAS (leg pain and back pain)
The mean of postoperative VAS of back pain at 1 (2.0 ± 0.2), 3 (2.2 ± 0.5), and 6 (1.1 ± 0.6) months postoperatively were lower compared to the preoperative. Median leg pain VAS scores were 1 (1.9 ± 0.3), 3 (1.2 ± 0.6), and 6 (1.1 ± 0.7) months postoperatively.
Screw accuracy
A total of 116 screws were inserted using robotic navigation. There was only one lateral breach (0.8%) and one superior breach (0.8%). No medial or inferior breaches were observed during the follow-up period.
Operating time
The operating time for single-position OLIF and percutaneous screw insertion from skin incision until skin closure was 101.2 ± 7.16 min (Table 2). The operation was divided into four steps. The first is the application of dynamic reference based on the iliac wing and registering the CT scan data into the Excelcius GPS; this procedure took around 31.3 ± 8.5 min. The second procedure was the insertion of percutaneous pedicle screws; every single screw needed 3.4 ± 1.6 min, and the total time for single-level percutaneous screws was 13.6 ± 8.5 min. The third step was doing the OLIF procedure; it took around 41.5 ± 8.2 min for a single level, and for every other level above or below, it needed an additional 20.2 ± 4.3 min. The final step was inserting the rod into the screw; it took around 8.3 ± 2.3 min for bilateral rod placement.
Estimated blood loss
The estimated blood loss was 90.0 ± 16.6 ml (range 50–120 ml).
Post operative length of stay (LOS)
The mean hospital stay for each patient was 3.4 ± 0.6 days; all patients were discharged after being fully mobile without any walking aid and without the need for high doses or strong analgesics.
Complications
There were two (8%) vascular complications during surgery; the common iliac vein was accidentally torn during mobilization for access to the L4/5 disc. It was managed using absorbable hemostatic application over the ruptured vein. One patient (4%) had retrograde ejaculation after fusion of L5/S1; the symptom resolved within 3 months after the surgery. In this study, the patient who experienced retrograde ejaculation is different with the patient who experienced major venous bleeding. Of the 116 screws that were inserted using robotic navigation, there were one lateral breach (0.8%) and one superior breach (0.8%). No medial or inferior breaches were observed during the follow-up period.
Illustrative case
Case 1
A 53-year-old male underwent an L2–4 OLIF for chronic low back pain due to degenerative disc disease (Figures 7A–D). Preoperatively, he reported a VAS score of 2 for leg pain and 5 for back pain. A robotic-assisted OLIF procedure was performed with a lateral decubitus approach. No intra and postoperative complications were found in this patient. The patient's symptoms resolved until 6 months after surgery (Figures 7E–H).

Figure 7. (A) X-ray image in lateral extension showing disc narrowing in L3/4 before surgery. (B) CT scan showing disc narrowing in L3/L4. (C,D) MRI showed disc narrowing at the level of L3/4. Postoperative x-ray (E,F) and MRI (G,H) showed that the intervertebral cage was well positioned without displacement.
Case 2
A 70-year-old female underwent a one-level L4/5 robotic-assisted OLIF surgery. She had been experiencing leg pain and lower back pain for the past 3.5 years, with moderate to severe preoperative leg pain (VAS 6) and back pain (VAS 7). Imaging studies, including plain radiographs and a CT scan, revealed spondylolisthesis at L4/5 (Figures 8A–D). After thorough consideration, a robotic-assisted OLIF procedure was performed using a lateral decubitus approach. The patient's hospital stay was 3 days. Postoperative imaging confirmed a successful surgery with no evidence of any breaches (Figures 8E–H). At a follow-up visit 6.2 months later, her leg and back pain had significantly improved, with VAS scores of 1.2 and 0, respectively. No complications were reported intraoperatively or postoperatively.
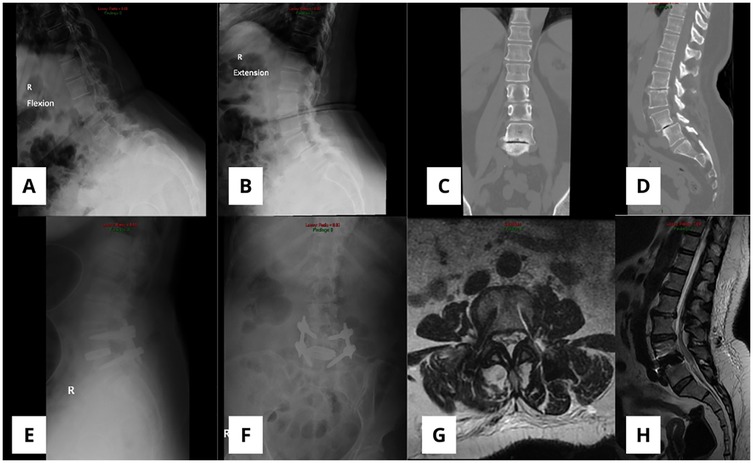
Figure 8. (A,B) X-ray image in lateral flexion and extension showing spondylolisthesis L4/5 before surgery. (C,D) CT scan showed disc narrowing at the level of L5/S1. Postoperative x-ray (E,F) and MRI (G,H) showed that the intervertebral cage was well positioned without displacement.
Discussion
Robotic surgery has become widely accepted as a treatment modality in medicine. Spine surgery is also part of the medical field that has already accepted the technology (6). All surgeries included in this retrospective study were performed by a single surgeon, using a consistent technique throughout. A small margin of error for pedicle screw insertion that could lead to devastated neurologic or vascular injury is the reason why this technology is becoming more and more popular in the field of spine surgery (7). Robotic navigation offers two key benefits in lateral lumbar surgery. First, it allows the surgeon to easily insert percutaneous pedicle screws in the lateral position without the need for a C-arm. Second, it can be used with robotic instruments for endplate preparation and interbody cage implantation. A robotic arm can also function as a retractor holder, providing more excellent stability than a table-mounted retractor.
Navigation spine surgery with a robotic arm could increase time efficiency during operation (8). Traditionally, the interbody cage was inserted in a lateral decubitus position for OLIF or XLIF procedure, and the patient was flipped to prone for insertion of a pedicle screw (9). The robotic arm provides a rigid platform that enables to perform pedicle screw insertion in the lateral decubitus position. In this study, we did not compare the operating time between a single position and lateral then prone (bipedal position). However, time efficiency had already been shown by another study by Ziino et al., which showed a statistically significant time difference between the two procedures (10). A study comparing robotic-assisted OLIF in single vs. bipedal positions found that the single position resulted in a shorter operative time, higher screw accuracy at the A level, and lower back pain VAS scores at one week postoperatively compared to the bipedal position (11). Tong et al. found a significantly different VAS between robotic and freehand in three days postoperative. However, no significant difference was found in the three- and six-month follow-ups (12).
Our data found that no medial pedicle breaches were using robotic spine navigation. Laine et al. categorized pedicle screw breaches into four types: medial, lateral, superior, and inferior, based on the location of the breach (13). Due to the anatomical proximity between the pedicle and the corresponding nerve root, medial or inferior breaches carry a high risk of nerve injury (14). In contrast, lateral or superior breaches pose a lower risk (15).
Another data comparing free hand and navigated screw insertion showed that the possibility of misplacement in the free hand group is relatively high, ranging from 3% to 55% in the thoracic spine and 5%–41% in the lumbar spine (16–18). Pedicle wall breaches in the lateral and superior parts could be caused by soft tissue pressure in the robotic instrument or skiving of the pilot drill on the lateral wall of the facet joint (19). The haptic feedback that is received from the instrument, combined with the trajectory in the navigation monitor, is essential in maintaining accuracy in pedicle screw insertion (20).
Intraoperative blood loss is reduced in robotic-assisted OLIF surgery compared to the freehand technique due to the smaller incisions required in robotic-assisted procedures. The freehand technique typically involves longer operative times, contributing to increased estimated blood loss (21). Similarly, Several studies have demonstrated that OLIF enables aggressive correction of spinal deformities, reduces postoperative back pain, achieves higher fusion rates with thorough disc space clearance, and decreases blood loss (22–24).
The most commonly reported complications of OLIF surgery in the literature include vascular, ureteral, and nerve damage, as well as lower extremity weakness (25). Other complications reported include male sexual dysfunction, cerebrovascular accidents, peritoneal laceration, ileus, psoas paresis, and groin numbness (22). In our cases, there were two vascular complications during surgery and one instance of retrograde ejaculation post-surgery. While significant vascular injuries are rare in OLIF, careful preoperative planning that takes vascular anatomy into account is essential to prevent such catastrophic events (26). Bifurcation of the abdominal aorta occurs commonly on the L4 level (67%–83%), but various anatomies can be found at the L3 vertebral body level (27, 28). As a result, the iliac artery is already present at level L4 and lies near the psoas major muscle. During procedures, mobilization is made to change the patient's position, which can cause venous bleeding. The surgeon manages the bleeding using patch methods, and the bleeding stops (29).
Retrograde ejaculation, believed to result from injury to the superior hypogastric nerve plexus, is rarely reported. To minimize the risk of postoperative sexual dysfunction, especially in male patients, meticulous blunt dissection and gentle retraction of structures within the great vessel bifurcation are essential (30). Tannoury et al. reported on 940 patients and 2,429 fusion levels using the OLIF technique. The overall surgical complication rate was 8.2%, with no instances of major vascular injury (31). Xiao-guang, et al. reported complications associated with robotic-assisted OLIF procedures. These complications included sympathetic nerve injury and transient thigh flexion weakness or numbness, all of which resolved within the first three months. These issues arose due to the anatomical positioning of the lumbar plexus, lumbar sympathetic trunk, and segmental arteries located laterally in front of the lumbar vertebrae, making them vulnerable to irritation or injury (32).
Although single-position surgery is not a new concept and is widely practiced in lateral or prone positions across many hospitals, integrating robotic assistance in oblique lateral interbody fusion (OLIF) significantly enhances surgical precision, safety, and efficiency. Robotic guidance allows accurate preoperative planning and real-time navigation, which is especially important given the complex retroperitoneal anatomy near the psoas, major vessels, and lumbar plexus. It improves implant accuracy, minimizes risk to critical structures, reduces radiation exposure, and supports minimally invasive techniques for better outcomes.
This study has several limitations. First, the absence of a control group restricts the ability to draw comparative conclusions or establish causality. The primary objective was to assess trends and feasibility within a specific patient population, making a control group beyond the study's scope. Second, validated outcome measures like the Oswestry Disability Index (ODI) were not used due to inconsistent data availability, limiting standardized assessment of functional outcomes. Additionally, the relatively short follow-up period may not capture long-term complications. The surgeries were also performed by four different spine surgeons, introducing potential variability in technique and outcomes. Future studies should include longer follow-up, larger sample sizes, and standardized measures to enhance result reliability. Lastly, this study did not include statistical analysis. The primary objective was to describe the surgical technique and evaluate the feasibility and safety of robotic-assisted oblique lumbar interbody fusion (OLIF), rather than to perform hypothesis-driven comparisons.
Conclusions
Single-position OLIF shows favorable results, with robotic guidance offering substantial benefits, including reduced bleeding, fewer surgical complications, lower VAS, and shorter operative times without repositioning the patient.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Research Ethics Committee, Trisakti University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
AR: Writing – original draft, Writing – review & editing, Conceptualization, Project administration, Resources. LG: Conceptualization, Project administration, Writing – original draft, Writing – review & editing. AA: Conceptualization, Resources, Writing – original draft, Writing – review & editing. OL: Conceptualization, Resources, Writing – original draft, Writing – review & editing. PP: Writing – original draft, Writing – review & editing. HM: Writing – original draft, Writing – review & editing. SH: Writing – original draft, Writing – review & editing. KG: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. MM: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. EK: Data curation, Project administration, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We thank Maharani Asmara Putri from Mapson Arya Parahita for the technical support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Yoon JW, Wang MY. The evolution of minimally invasive spine surgery: JNSPG 75th anniversary invited review article. J Neurosurg Spine. (2019) 30(2):149–58. doi: 10.3171/2018.11.SPINE181215
2. Park J, Ham DW, Kwon BT, Park SM, Kim HJ, Yeom JS. Minimally invasive spine surgery: techniques, technologies, and indications. Asian Spine J. (2020) 14(5):694–701. doi: 10.31616/asj.2020.0384
3. Jenkins NW, Parrish JM, Sheha ED, Singh K. Intraoperative risks of radiation exposure for the surgeon and patient. Ann Transl Med. (2021) 9(1):84. doi: 10.21037/atm-20-1052
4. Vaccaro AR, Harris JA, Hussain MM, Wadhwa R, Chang VW, Schroerlucke SR, et al. Assessment of surgical procedural time, pedicle screw accuracy, and clinician radiation exposure of a novel robotic navigation system compared with conventional open and percutaneous freehand techniques: a cadaveric investigation. Glob Spine J. (2020) 10(7):814–25. doi: 10.1177/2192568219879083
5. Kalidindi KKV, Sharma JK, Jagadeesh NH, Sath S, Chhabra HS. Robotic spine surgery: a review of the present status. J Med Eng Technol. (2020) 44(7):431–7. doi: 10.1080/03091902.2020.1799098
6. Reddy K, Gharde P, Tayade H, Patil M, Reddy LS, Surya D. Advancements in robotic surgery: a comprehensive overview of current utilizations and upcoming frontiers. Cureus. (2023) 15(12):e50415. doi: 10.7759/cureus.50415
7. Naik A, MacInnis BR, Shaffer A, Krist DT, Smith AD, Garst JR, et al. Trends in technology for pedicle screw placement: a temporal meta-analysis. Spine (Phila Pa 1976). (2023) 48(11):791–9. doi: 10.1097/BRS.0000000000004604
8. Lee YS, Cho DC, Kim KT. Navigation-guided/robot-assisted spinal surgery: a review article. Neurospine. (2024) 21(1):8–17. doi: 10.14245/ns.2347184.592
9. Wong AXJ, Tang DH, Kaliya-Perumal AK, Oh JYL. The evolution of lateral lumbar interbody fusion: a journey from past to present. Medicina (Kaunas). (2024) 60(3):378. doi: 10.3390/medicina60030378
10. Ziino C, Konopka JA, Ajiboye RM, Ledesma JB, Koltsov JCB, Cheng I. Single position versus lateral-then-prone positioning for lateral interbody fusion and pedicle screw fixation. J Spine Surg (Hong Kong). (2018) 4(4):717–24. doi: 10.21037/jss.2018.12.03
11. Zhao W, Wang Y, Zhang H, Guo J, Han J, Lin A, et al. Analysis of the screw accuracy and postoperative efficacy of screw placement in single position and bipedal position in robot-assisted oblique lumbar interbody fusion: preliminary results of mazor X stealth usage. Orthop Surg. (2024) 16(2):401–11. doi: 10.1111/os.13972
12. Tong M, Zhang S, Zhang W, Mou L, Dong Z, Wang R, et al. Efficacy and safety of navigation robot-assisted versus conventional oblique lateral lumbar interbody fusion with internal fixation in the treatment of lumbar degenerative diseases: a retrospective study. Medicine (Baltimore). (2024) 103(32):e39261. doi: 10.1097/MD.0000000000039261
13. Laine T, Lund T, Ylikoski M, Lohikoski J, Schlenzka D. Accuracy of pedicle screw insertion with and without computer assistance: a randomised controlled clinical study in 100 consecutive patients. Eur Spine J. (2000) 9(3):235–40. doi: 10.1007/s005860000146
14. Castro WHM, Halm H, Jerosch J, Malms J, Steinbeck J, Blasius S. Accuracy of pedicle screw placement in lumbar vertebrae. Spine (Phila Pa 1976). (1996) 21(11):1320–4. doi: 10.1097/00007632-199606010-00008
15. Herkowitz HN, Steinmann JC, El-Kommos H, Wesolowski DP. Spinal pedicle fixation. Confirmation of an image-based technique for screw placement. Spine (Phila Pa 1976). (1993) 18(13):1856–61. doi: 10.1097/00007632-199310000-00022
16. Gautschi OP, Schatlo B, Schaller K, Tessitore E. Clinically relevant complications related to pedicle screw placement in thoracolumbar surgery and their management: a literature review of 35,630 pedicle screws. Neurosurg Focus. (2011) 31(4):E8. doi: 10.3171/2011.7.FOCUS11168
17. Perna F, Borghi R, Pilla F, Stefanini N, Mazzotti A, Chehrassan M. Pedicle screw insertion techniques: an update and review of the literature. Musculoskelet Surg. (2016) 100(3):165–9. doi: 10.1007/s12306-016-0438-8
18. Kosmopoulos V, Schizas C. Pedicle screw placement accuracy: a meta-analysis. Spine (Phila Pa 1976). (2007) 32(3):E111–20. doi: 10.1097/01.brs.0000254048.79024.8b
19. Ito M, Ueno J, Torii Y, Iinuma M, Yoshida A, Tomochika K, et al. Utility of a navigated high-speed drill in robotic-assisted screw placement for spine surgery. Cureus. (2024) 16(1):e52779. doi: 10.7759/cureus.52779
20. Nakdhamabhorn S, Pillai BM, Chotivichit A, Suthakorn J. Sensorless based haptic feedback integration in robot-assisted pedicle screw insertion for lumbar spine surgery: a preliminary cadaveric study. Comput Struct Biotechnol J. (2024) 24:420–33. doi: 10.1016/j.csbj.2024.05.022
21. Feng S, Tian W, Wei Y. Clinical effects of oblique lateral interbody fusion by conventional open versus percutaneous robot-assisted minimally invasive pedicle screw placement in elderly patients. Orthop Surg. (2020) 12(1):86–93. doi: 10.1111/os.12587
22. Silvestre C, Mac-Thiong JM, Hilmi R, Roussouly P. Complications and morbidities of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine J. (2012) 6(2):89–97. doi: 10.4184/asj.2012.6.2.89
23. Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kishida S, et al. Mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for lumbar spinal degeneration disease. Yonsei Med J. (2015) 56(4):1051–9. doi: 10.3349/ymj.2015.56.4.1051
24. Walker CT, Harrison Farber S, Cole TS, Xu DS, Godzik J, Whiting AC, et al. Complications for minimally invasive lateral interbody arthrodesis: a systematic review and meta-analysis comparing prepsoas and transpsoas approaches. J Neurosurg Spine. (2019) 30(4):446–60. doi: 10.3171/2018.9.SPINE18800
25. Han J, Han S, Meng S, Zhao X, Zhang H, Guo J, et al. Application of the oblique lateral interbody fusion technique in salvage surgery: technical note and case series. Front Surg. (2023) 10:1144699. doi: 10.3389/fsurg.2023.1144699
26. Kim H, Chang BS, Chang SY. Pearls and pitfalls of oblique lateral interbody fusion: a comprehensive narrative review. Neurospine. (2022) 19(1):163–76. doi: 10.14245/ns.2143236.618
27. Chithriki M, Jaibaji M, Steele RD. The anatomical relationship of the aortic bifurcation to the lumbar vertebrae: a MRI study. Surg Radiol Anat. (2002) 24(5):308–12. doi: 10.1007/s00276-002-0036-3
28. Lee CH, Seo BK, Choi YC, Shin HJ, Park JH, Jeon HJ, et al. Using MRI to evaluate anatomic significance of aortic bifurcation, right renal artery, and conus medullaris when locating lumbar vertebral segments. Am J Roentgenol. (2004) 182(5):1295–300. doi: 10.2214/ajr.182.5.1821295
29. Diaz-Aguilar LD, Shah V, Himstead A, Brown NJ, Abraham ME, Pham MH. Simultaneous robotic single-position surgery (SR-SPS) with oblique lumbar interbody fusion: a case series. World Neurosurg. (2021) 151:e1036–43. doi: 10.1016/j.wneu.2021.05.043
30. Orita S, Shiga Y, Inage K, Eguchi Y, Maki S, Furuya T, et al. Technical and conceptual review on the L5-S1 oblique lateral interbody fusion surgery (OLIF51). Spine Surg Relat Res. (2021) 5(1):1–9. doi: 10.22603/ssrr.2020-0086
31. Tannoury T, Kempegowda H, Haddadi K, Tannoury C. Complications associated with minimally invasive anterior to the psoas (ATP) fusion of the lumbosacral spine. Spine (Phila Pa 1976). (2019) 44(19):E1122–9. doi: 10.1097/BRS.0000000000003071
Keywords: robotic-assisted, OLIF, minimal invasive surgery, single position, surgical technique
Citation: Rizki Gatam A, Gatam L, Ajiantoro A, Luthfi O, Phedy P, Mahadhipta H, Husin S, Gani KS, Mitchel M and Kholinne E (2025) The feasibility of robotic navigation in single position oblique lateral spine surgery. A technical note and a retrospective study. Front. Surg. 12:1582889. doi: 10.3389/fsurg.2025.1582889
Received: 25 February 2025; Accepted: 11 June 2025;
Published: 25 June 2025.
Edited by:
Mario Ganau, Oxford University Hospitals NHS Trust, United KingdomReviewed by:
Moiz Khan, MathWorks, United StatesRodolfo Maduri, Hôpital Riviera-Chablais (HRC), Switzerland
Copyright: © 2025 Rizki Gatam, Gatam, Ajiantoro, Luthfi, Phedy, Mahadhipta, Husin, Gani, Mitchel and Kholinne. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Erica Kholinne, ZXJpY2FAdHJpc2FrdGkuYWMuaWQ=
 Asrafi Rizki Gatam1,2,3
Asrafi Rizki Gatam1,2,3 Karina Sylvana Gani
Karina Sylvana Gani Mitchel Mitchel
Mitchel Mitchel Erica Kholinne
Erica Kholinne