- 1College of Acupuncture and Orthopedics, Hubei University of Chinese Medicine, Wuhan, China
- 2Department of Osteology, Huanggang Hospital of Traditional Chinese Medicine Affiliated to Hubei University of Chinese Medicine, Huanggang, China
- 3School of Medicine, Hubei Minzu University, Enshi, China
- 4Department of Surgery, Huanggang Hospital of Traditional Chinese Medicine Affiliated to Hubei University of Chinese Medicine, Huanggang, China
Introduction: The Achilles tendon is the largest tendon in the human body and is prone to rupture when subjected to excessive dorsiflexion trauma of the ankle joint. The primary goal of treatment is to restore limb function; however, there remains considerable debate regarding the optimal management strategy.
Patient concerns: We report a patient presenting with chronic Achilles tendon rupture accompanied by calcification of the tendon, which caused persistent pain and functional limitation of the affected limb.
Diagnosis: Chronic Achilles tendon rupture with associated tendon calcification, with a tendon defect measuring approximately 6 cm on preoperative imaging, confirmed by clinical examination and imaging evaluation.
Interventions: The patient underwent surgical removal of the calcified lesion, followed by reconstruction of the tendon defect using a gastrocnemius aponeurosis flap combined with the Achilles tendon sheath.
Outcomes: Postoperative recovery was favorable, and at the 6-month follow-up, the patient achieved satisfactory ankle function with an AOFAS score of 89, a VISA-A score of 91, and an ATRS score of 90. At the 12-month follow-up, functional outcomes remained stable, with an AOFAS score of 95, a VISA-A score of 96, and an ATRS score of 94, confirming sustained recovery and tendon integrity.
Conclusion: This case highlights a feasible surgical strategy for chronic Achilles tendon rupture with calcification, which may provide an alternative approach for tendon reconstruction in patients with sheath proliferation and calcified lesions.
1 Introduction
Achilles tendon rupture is a common tendon injury that is usually easy to diagnose; nevertheless, previous studies have documented a misdiagnosis rate as high as 25% (1). Early misdiagnosis or missed diagnosis may progress to chronic injury, which significantly increases the difficulty of treatment and worsens the prognosis, thereby causing considerable distress to patients' daily life and work (2). Chronic Achilles tendon rupture complicated with calcification is relatively rare in clinical practice (3). In this case, we performed calcified lesion debridement combined with suture anchor fixation, gastrocnemius aponeurosis flap, and Achilles tendon sheath reconstruction. This approach utilizes proliferative Achilles tendon sheath tissue as an autologous material, avoiding the need for distant tendon graft harvesting and thereby reducing donor-site morbidity. By combining the gastrocnemius aponeurosis flap with the thickened sheath, this technique provides sufficient mechanical strength for defect repair while minimizing additional trauma. The case is reported as follows.
2 Case presentation
The patient was an 18-year-old male who developed left ankle pain after falling to the ground following a jump while playing basketball on June 20, 2024. He initially sought care at a local hospital, where he was diagnosed with a “ankle sprain” and treated with plaster immobilization. After three weeks, the patient removed the plaster by himself and continued weight-bearing ambulation with a limp. Given the patient's young age, the presence of marked tendon calcification was considered unusual; possible causes such as previous minor injury, local chronic inflammation, or metabolic factors were taken into account.
On August 15, 2024, he presented to our hospital due to worsening pain in the left ankle. Physical examination revealed mild swelling of the left heel without obvious erythema, ulceration, or abnormal skin temperature. There was localized tenderness on the posterior aspect of the left ankle and slightly limited heel-raising movement.
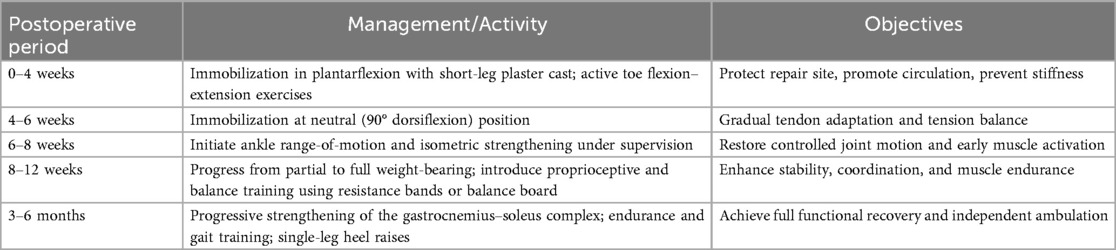
Imaging studies, including x-ray and MRI, demonstrated thickening of the left Achilles tendon with intratendinous calcification and tendon rupture, with a tendon gap measuring approximately 6 cm as shown on preoperative MRI. Based on these findings, the diagnosis of chronic rupture of the left Achilles tendon with tendon defect and calcification was established (Figures 1a–d). Surgical treatment was recommended.
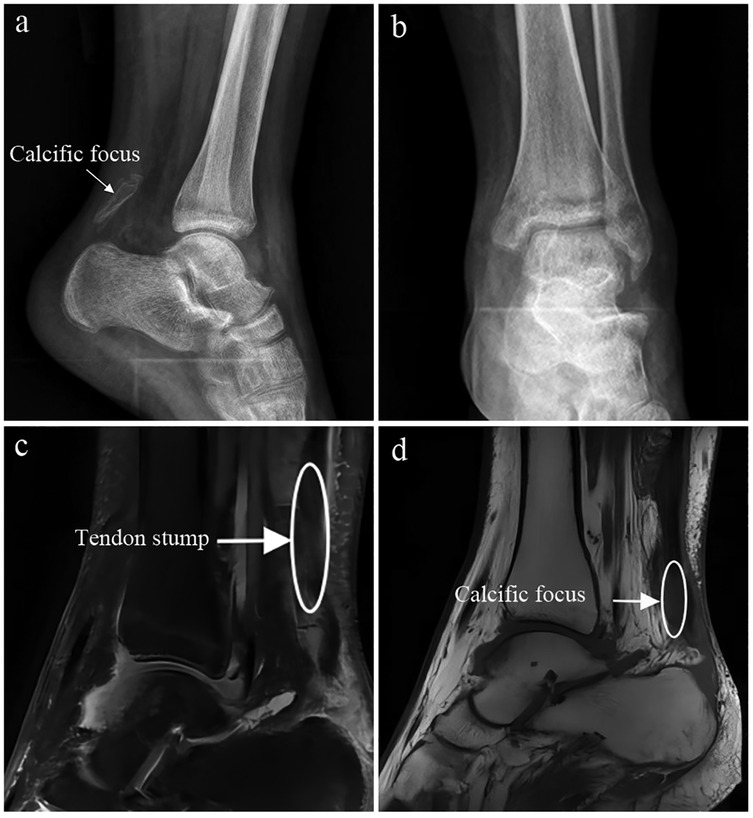
Figure 1. (a–d) Preoperative x-ray and magnetic resonance imaging (MRI) showing chronic rupture and defect of the left Achilles tendon with calcification.
3 Treatment
Three days after admission, the patient underwent “debridement of calcified lesion of the left Achilles tendon combined with suture anchor fixation, reconstruction with gastrocnemius aponeurosis flap and Achilles tendon sheath, and plaster immobilization.” Intraoperative exploration revealed that the gastrocnemius aponeurosis and Achilles tendon sheath were structurally intact but exhibited marked fibrotic thickening. The Achilles tendon was shortened, with an approximately 6-cm defect between the proximal and distal stumps (Figures 2a,b). The calcified lesion was located at the distal stump and demonstrated indistinct demarcation from the adjacent tendon tissue. After complete excision of the calcified portion, the tendon sheath was evaluated and found to be sufficiently thick and mechanically robust to serve as autologous reinforcement material. A gastrocnemius aponeurosis flap measuring approximately 8 cm in length and 3 cm in width, together with a thickened Achilles tendon sheath of about 6 cm in length, was harvested and prepared for reconstruction. The aponeurosis flap was then reversed and longitudinally interwoven with the thickened tendon sheath to reconstruct the defect. The construct was anchored to the calcaneal tuberosity using a suture anchor (Figures 2c,d). This approach was selected because it provided adequate coverage and tensile support without the need for distant tendon graft harvesting. Alternative options, including peroneus brevis transfer and allograft tendon reconstruction, were considered but deemed unnecessary given the adequate local tissue quality. The proximal and distal tendon stumps were re-approximated under appropriate tension and secured with a modified Kessler suture technique. Intraoperative passive ankle motion demonstrated smooth force transmission of the reconstructed tendon without excessive tension.
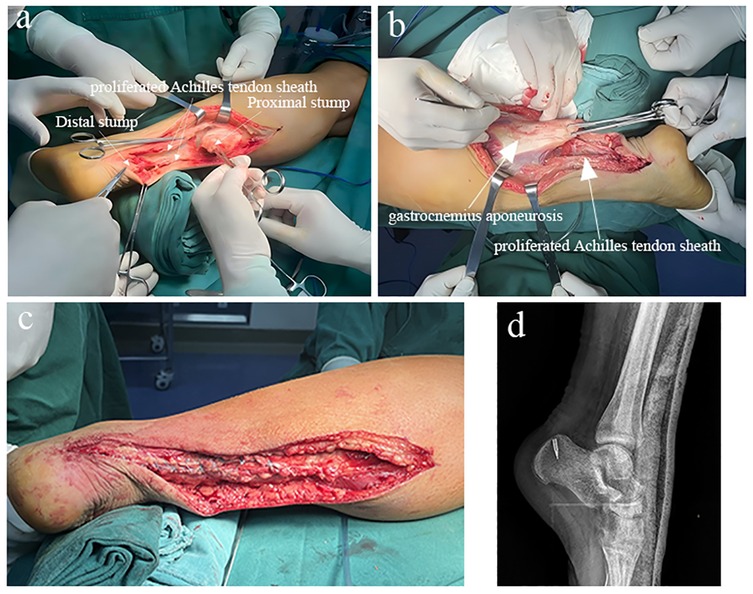
Figure 2. (a,b) Intraoperative exploration showing intact gastrocnemius aponeurosis and achilles tendon sheath with marked scar hyperplasia, and shortening of the Achilles tendon stumps. (c) The gastrocnemius aponeurosis flap and proliferated Achilles tendon sheath were folded and sutured into a cord-like structure resembling the native Achilles tendon. (d) Postoperative digital radiograph demonstrating appropriate placement of the suture anchor.
Postoperatively, the affected limb was immobilized in plantarflexion with a short-leg plaster cast for 4 weeks, followed by neutral (90° dorsiflexion) immobilization for 2 weeks. During the immobilization period, the patient was instructed to perform active toe flexion–extension exercises to promote venous return and prevent stiffness. After cast removal at 6 weeks, supervised physiotherapy was initiated, including ankle range-of-motion training and isometric strengthening exercises. Partial weight-bearing ambulation was permitted at 8 weeks postoperatively, progressing to full weight-bearing by 12 weeks as tolerated. Between 10 and 12 weeks, proprioceptive and balance training were introduced using a balance board and resistance bands. From 3 to 6 months, progressive strengthening of the gastrocnemius–soleus complex and endurance training were conducted. By 6 months postoperatively, the patient achieved full weight-bearing walking and could perform single-leg heel raises, indicating satisfactory functional recovery. The detailed rehabilitation schedule is summarized in Table 1.
At the 6-month follow-up, the patient showed restoration of ankle flexion and extension function (Figures 3a,b), with an AOFAS score of 89, a VISA-A score of 91, and an ATRS score of 90, indicating good short-term recovery. At the 12-month follow-up, the patient demonstrated stable and sustained improvement, achieving an AOFAS score of 95, a VISA-A score of 96, and an ATRS score of 94, with no pain, weakness, or limitation in daily activities. Follow-up ultrasonography confirmed continuous tendon integrity and satisfactory remodeling at the reconstruction site, suggesting durable functional outcomes.
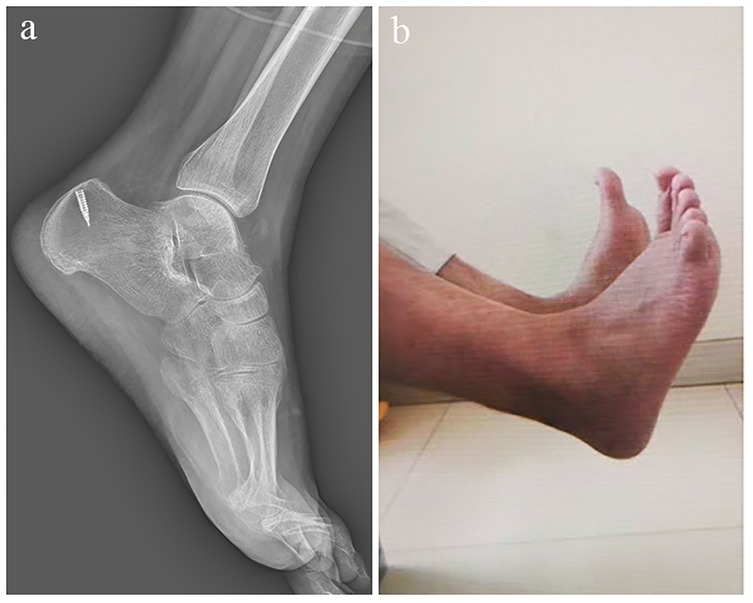
Figure 3. (a,b) At 6 months postoperatively, the patient demonstrated satisfactory recovery of ankle flexion and extension function.
4 Discussion
The Achilles tendon is the largest tendon in the human body, and rupture may occur when direct trauma or sudden excessive tensile force exceeds its structural limit. Due to the compensatory action of the posterior tibial muscle group, some patients with Achilles tendon rupture may still retain ankle flexion and extension, which often leads to underestimation by patients themselves and insufficient physical examination by clinicians. These are the main reasons for misdiagnosis and missed diagnosis.
For chronic Achilles tendon rupture, conservative treatment is generally unsatisfactory, and surgical intervention is usually required (4). Various surgical techniques have been described, with the choice of procedure largely determined by the size of the tendon defect (5). In recent years, minimally invasive techniques have been increasingly applied in Achilles tendon repair (6). However, concerns remain regarding the tensile strength of sutures in minimally invasive settings, and freshening of tendon ends in chronic ruptures is technically challenging under minimally invasive approaches (7). Allograft tendons and synthetic grafts have been reported as alternatives for reconstructing Achilles tendon defects, but their reliability requires further clinical validation (8). Autologous tendon or fascial grafting provides dependable biomechanical strength, yet is associated with greater donor-site morbidity. In the present case, the Achilles tendon defect measured approximately 6 cm. For defects of this magnitude, fascial or tendon transfer remains a commonly employed and effective reconstructive method (9).
Among the established surgical techniques, V–Y tendon advancement and flexor hallucis longus (FHL) tendon transfer are two widely recognized options. V–Y advancement, typically used for small to moderate defects, allows direct lengthening of the proximal tendon stump but may be limited by reduced tendon elasticity and proximal weakness (10). In contrast, FHL transfer provides a strong and vascularized autologous tendon for reconstruction, offering reliable biomechanical strength and promoting early rehabilitation (11–13). However, it involves sacrificing a functional toe flexor, which can result in loss of great toe plantarflexion strength. In addition to these methods, the use of gastrocnemius aponeurosis or paratenon tissue has been reported as an effective alternative for chronic Achilles tendon reconstruction. Recent studies have demonstrated that gastrocnemius aponeurosis flaps can provide sufficient mechanical strength and favorable biological integration for medium-to-large tendon defects while avoiding donor-site morbidity (14, 15). Similarly, the paratenon, when thickened or proliferative, offers an autologous vascularized tissue layer that enhances tendon gliding and healing (16). These reports collectively support the feasibility of utilizing local tissues in reconstruction, which aligns with the technique described in our case. Compared with these methods, our approach utilizes locally proliferated Achilles tendon sheath tissue in combination with a gastrocnemius aponeurosis flap, thereby preserving donor tendon function and reducing iatrogenic morbidity while maintaining adequate mechanical strength for repair.
Compared with conventional autologous or allograft tendon transfers, the current technique demonstrates several advantages. First, by utilizing locally proliferated Achilles tendon sheath tissue together with a gastrocnemius aponeurosis flap, this approach eliminates the need for distant tendon harvesting and consequently reduces donor-site morbidity. Second, the combination of fibrotic sheath tissue and aponeurosis provides adequate tensile strength and biological continuity, facilitating graft integration while minimizing additional trauma. Third, the reconstruction preserves the native anatomical alignment and maintains physiological tension of the Achilles tendon, which may contribute to faster functional recovery. Nevertheless, this technique has several limitations. This report describes a single case, which restricts the generalizability of the findings. Although the 12-month follow-up demonstrated favorable short-term outcomes, it remains insufficient to evaluate the long-term integrity and functional durability of the reconstructed tendon. Notably, postoperative ultrasonography or magnetic resonance imaging was not performed to confirm structural tendon integration. Future prospective studies with larger sample sizes, longer follow-up periods, and imaging-based assessments are warranted to further validate the efficacy and durability of this technique.
To minimize postoperative scar formation and adhesion, meticulous intraoperative tissue handling was emphasized to preserve the paratenon and reduce unnecessary soft-tissue trauma. Postoperatively, early functional rehabilitation—including controlled range-of-motion exercises after cast removal—was implemented to prevent adhesion formation and stiffness. In addition, scar management measures such as gentle massage, silicone gel application, and regular physiotherapy were employed to promote tissue remodeling and maintain tendon gliding. These steps were essential for optimizing functional recovery after such extensive dissection.
In summary, this case provides several important clinical insights. First, some patients with Achilles tendon rupture may present with atypical symptoms, and retained ankle motion can contribute to misdiagnosis. Therefore, careful clinical examination is crucial. The heel-rise test and Thompson (Simmonds–Thompson) calf-squeeze test provide high specificity, and when rupture is suspected, MRI or ultrasonography should be performed to ensure accurate evaluation and reduce missed diagnoses (17). Second, although the Achilles tendon sheath (paratenon) is typically too thin to serve as graft material, proliferative thickening of the sheath—as observed in this patient—may offer a valuable autologous source for reconstruction. This technique obviates the need for distant autograft harvesting, thereby reducing donor-site morbidity and iatrogenic trauma. Third, once a chronic Achilles tendon rupture is recognized, early surgical intervention is recommended to prevent progressive calcification and further enlargement of the tendon defect. Finally, the possible association between tendon sheath proliferation and calcification remains hypothetical and should be interpreted with caution; future studies with histopathological and molecular investigations are warranted to clarify this potential mechanism.
5 Conclusion
This report describes a patient with chronic Achilles tendon rupture complicated by intratendinous calcification. Intraoperatively, marked proliferation of the Achilles tendon sheath was observed. Although the potential relationship between tendon sheath proliferation and tendon calcification remains unclear, the proliferated sheath provided valuable autologous tissue for reconstruction. In combination with a gastrocnemius aponeurosis flap, it allowed for robust repair of the tendon defect. While this single case is not representative, it offers valuable insight into surgical options under such specific conditions and provides evidence-based guidance for treatment strategies in similar anatomical scenarios.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the Biomedical Research Ethics Committee of Affiliated Huanggang Hospital of Traditional Chinese Medicine. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
ST: Writing – review & editing, Investigation, Writing – original draft. ZL: Writing – review & editing, Methodology, Writing – original draft. MX: Writing – review & editing, Writing – original draft, Methodology. WZ: Validation, Writing – original draft, Writing – review & editing. YS: Writing – review & editing, Supervision, Writing – original draft.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This work was supported by Research Fund Project of Huanggang Science and Technology Bureau (YBXM20240010-3).
Acknowledgments
We would like to express our gratitude to the patient for granting permission to use their clinical data in this paper and for the publication of this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Maffulli N, Via AG, Oliva F. Chronic Achilles tendon rupture. Open Orthop J. (2017) 11:660–9. doi: 10.2174/1874325001711010660
2. Deng H, Cheng X, Yang Y, Fang F, He J, Tian Y, et al. Rerupture outcome of conservative versus open repair versus minimally invasive repair of acute Achilles tendon ruptures: A systematic review and meta-analysis. PLoS One. (2023) 18(5):e0285046. doi: 10.1371/journal.pone.0285046
3. Sullivan D, Pabich A, Enslow R, Roe A, Borchert D, Barr K, et al. Extensive ossification of the Achilles tendon with and without acute fracture: a scoping review. J Clin Med. (2021) 10(16):3480. doi: 10.3390/jcm10163480
4. Schweitzer KJ, Dekker TJ, Adams SB. Chronic Achilles ruptures: reconstructive options. J Am Acad Orthop Surg. (2018) 26(21):753–63. doi: 10.5435/JAAOS-D-17-00158
5. Den Hartog BD. Surgical strategies: delayed diagnosis or neglected Achilles’ tendon ruptures. Foot Ankle Int. (2008) 29(4):456–63. doi: 10.3113/FAI.2008.0456
6. Grassi A, Amendola A, Samuelsson K, Svantesson E, Romagnoli M, Bondi A, et al. Minimally invasive versus open repair for acute Achilles tendon rupture: meta-analysis showing reduced complications, with similar outcomes, after minimally invasive surgery. J Bone Joint Surg Am. (2018) 100(22):1969–81. doi: 10.2106/JBJS.17.01364
7. Lui TH. Endoscopic-assisted Achilles tendon repair with Plantaris tendon augmentation. Arthroscopy. (2007) 23(5):551–6. doi: 10.1016/j.arthro.2006.07.053
8. Shoaib A, Mishra V. Surgical repair of symptomatic chronic Achilles tendon rupture using synthetic graft augmentation. Foot Ankle Surg. (2017) 23(3):179–82. doi: 10.1016/j.fas.2016.04.006
9. Chen C, Hunt KJ. Open reconstructive strategies for chronic Achilles tendon ruptures. Foot Ankle Clin. (2019) 24(3):425–37. doi: 10.1016/j.fcl.2019.04.002
10. Feng SM, Maffulli N, Oliva F, Saxena A, Hao YF, Hua YH, et al. Surgical management of chronic Achilles tendon rupture: evidence-based guidelines. J Orthop Surg Res. (2024) 19:132. doi: 10.1186/s13018-024-04559-5
11. Karaismailoglu B, Ghandour S, Hendriks J, Eftekhari M, Eltouny E, Waryasz G, et al. Systematic review and meta-analysis comparing open FHL tendon transfer, hamstring transfer, and turndown flaps to treat chronic Achilles tendon ruptures. Foot Ankle Int. (2025) 46(7):784–93. doi: 10.1177/1071100725
12. Xu Y, Wang X, Li H, et al. Long-term outcome of flexor Hallucis longus tendon transfer for chronic Achilles tendon rupture with large defect. Medicine (Baltimore). (2023) 102(39):e35265.37773871
13. Rashid RH, Fayyaz U, Qadir R, et al. Flexor Hallucis longus transfer and V-Y plasty for chronic Achilles tendon rupture: outcomes and considerations. Cureus. (2023) 15(9):e.
14. Zhou J, Chen J, Li Z, et al. Reconstruction of chronic Achilles tendon rupture using gastrocnemius aponeurosis flap: a retrospective study and mid-term follow-up. BMC Musculoskelet Disord. (2023) 24:312.37081473
15. Mohamed M, AlQahtani SM, AlHussainy S, et al. Outcomes of gastrocnemius aponeurosis turndown flaps for chronic Achilles tendon defects: a systematic review and meta-analysis. Foot Ankle Surg. (2024) 30(1):18–26.
16. Xu Y, Zhang H, Wu J, et al. Paratenon-based reconstruction for chronic Achilles tendon rupture: a case series and literature review. J Orthop Surg Res. (2024) 19:201.38532441
Keywords: Achilles tendon, calcification, chronic rupture, suture anchor, case report
Citation: Tu S, Li Z, Xiao M, Zhu W and Shao Y (2025) Combined flexor sheath and gastrocnemius aponeurosis flap for the treatment of chronic calcified Achilles tendon rupture: a case report. Front. Surg. 12:1687970. doi: 10.3389/fsurg.2025.1687970
Received: 18 August 2025; Accepted: 11 November 2025;
Published: 21 November 2025.
Edited by:
S. W. Kong, Asia Medical Specialists, Hong Kong SAR, ChinaReviewed by:
Mengcun Chen, University of Pennsylvania, United StatesZongchao Liu, Southwest Medical University, China
Copyright: © 2025 Tu, Li, Xiao, Zhu and Shao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wensheng Zhu, MTU2OTY1NzczMzdAMTYzLmNvbQ==; Yi Shao, MzkxNTI2ODYwM0BxcS5jb20=
†These authors have contributed equally to this work and share first authorship
 Shuangqiang Tu1,2,†
Shuangqiang Tu1,2,† Zhongshan Li
Zhongshan Li Wensheng Zhu
Wensheng Zhu Yi Shao
Yi Shao